Summary
The Japanese government recommended hospitalization of patients on dialysis once they tested positive because of their high COVID-19 mortality rate and definite need for periodic dialysis. However, after experiencing the Delta variant surge, strategic changes towards outpatient care for mild or asymptomatic cases, along with strengthening emergency preparedness were needed. Facing the Omicron surge, the Tokyo Metropolitan Government introduced two novel schemes: i) a temporary medical facility with a dialysis center for infected patients on hemodialysis, which started admitting patients on dialysis on January 20, 2022, to provide additional bed capacity and access to hemodialysis and ii) a transportation scheme for patients who need travel to maintenance dialysis facilities from their homes, which was introduced on February 5. The Tokyo Metropolitan Government, cooperating with some nephrology experts, announced these schemes and urged local dialysis facilities to change strategies, providing information regarding infection prevention measures and treatments in online seminars on February 3 and 7. Consequently, promoting outpatient care did not lead to an increase in the case fatality ratio (CFR) in patients on dialysis with COVID-19 in Tokyo during the first Omicron surge (January 7 to February 10, 8.2%; February 11 to March 31, 5.5%). Furthermore, after an additional online seminar on July 20, the CFR dramatically declined in the second Omicron surge (July 8 to September 8, 1.2%). Implementation of public health intervention and careful communication with local dialysis facilities were both crucial to the strategic changes. To maintain essential health services, emergency preparedness should be cultivated during regular times.
Keywords: policy, maintaining essential health services, emergency preparedness
Introduction
Patients receiving dialysis have an increased risk for severity of COVID-19 and a higher mortality rate than the general population (1). Considering the enhanced vulnerability of patients receiving dialysis to COVID-19 and their need for periodic hemodialysis, the Japanese government policy recommends that patients receiving dialysis with COVID-19 be hospitalized, even if they have only mild symptoms or are asymptomatic. However, when newly diagnosed cases were drastically increasing, hospitalization of each infected dialysis patient was, despite the governmental policy, unfeasible owing to hospital overload.
The surge in Delta variant infection struck Tokyo in the summer of 2021, and hospitals were overcrowded with moderate to severe cases. The COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians, Japanese Society for Dialysis Therapy, and Japanese Society of Nephrology reported that it was "nearly impossible" to find a transfer destination even if an inpatient's condition worsened (2).
Emergency preparedness in dialysis facilities before the Omicron era
Having experienced recurrent shortages of hospital beds, however, not a small number of dialysis facilities were still unwilling to perform dialysis for patients with asymptomatic or mild COVID-19. It can be assumed that, for one thing, this was due to the potential risks of nosocomial infection. Concerning infection control measures, the Japanese Association of Dialysis Physicians published guidelines for preventing infection in maintenance hemodialysis facilities (3). However, according to a national questionnaire survey, from October to November 2020, some dialysis facilities performed inadequate infection control measures, including personal protective equipment use (especially face shields or eye guards), bed spacing, and exchanging bed linens (4).
In such a situation, the Task Force Committee, taking the leadership, had been releasing requests to physicians working at dialysis facilities for flexibly dealing with fluid COVID-19 situations and advocating for several strategies regarding preparedness and responses to such public health emergencies (2,5,6). These strategies included cooperative work with authorities such as prefectural governments, efficient triage and effective use of hospital beds, patient education, promoting vaccination, proactive use of neutralizing antibody treatments, and implementation of infection control measures at each dialysis facility. In line with those strategies, after the Delta wave, we, the public health officials of the Tokyo Metropolitan Government, cooperating with nephrology experts including the chairperson of the Task Force Committee, reviewed the medical provision system and attempted to make improvements by, for instance, hosting online discussion seminars with local dialysis hospitals and asking to increase bed capacity in preparation for probable upcoming larger waves of infection.
Nevertheless, in January 2022 with the advent of the Omicron variant, an acceleratingly increasing number of new positive cases in Tokyo immediately threatened the local medical provision system and patients needing dialysis.
Two novel schemes aiming to change the strategy of outpatient dialysis in response to the Omicron BA.1 surge
In response to the first Omicron surge, the Tokyo Metropolitan Government set up two novel schemes: i) a temporary medical facility with a dialysis center for infected patients who needed hemodialysis and ii) a transportation scheme utilizing specialized negative pressure vehicles for outpatients needing transport from home to their maintenance dialysis facilities (Figure 1). The temporary medical facility could offer additional local bed capacity for patients needing dialysis. In particular, the hospital bed turnover rate could be improved by accommodating already hospitalized patients who still need isolation despite their symptoms being relieved (Figure 1A). Thus, the temporary medical facility enabled more efficient and effective use of medical resources. The transportation scheme provided access to maintenance dialysis facilities for patients with COVID-19 who could not use public transportation, as mentioned in the World Health Organization guidance for maintaining essential health services (7). Apart from these newly introduced schemes, the Tokyo Metropolitan Government had established another scheme to provide neutralizing antibody treatment for indicated outpatients with COVID-19 by transporting them to existing temporary medical facilities (without dialysis functions) (8). This scheme could also be adapted for patients on dialysis (Figure 1B). As a whole, clarifying the division of roles and responsibilities for local stakeholders (authorities, hospitals, and clinics), these schemes made strategic changes, from hospitalization of all positive patients needing dialysis to outpatient care if the patients were asymptomatic or had mild COVID-19 symptoms. In doing so, hospital beds could be allocated for patients with more severe conditions.
Figure 1.
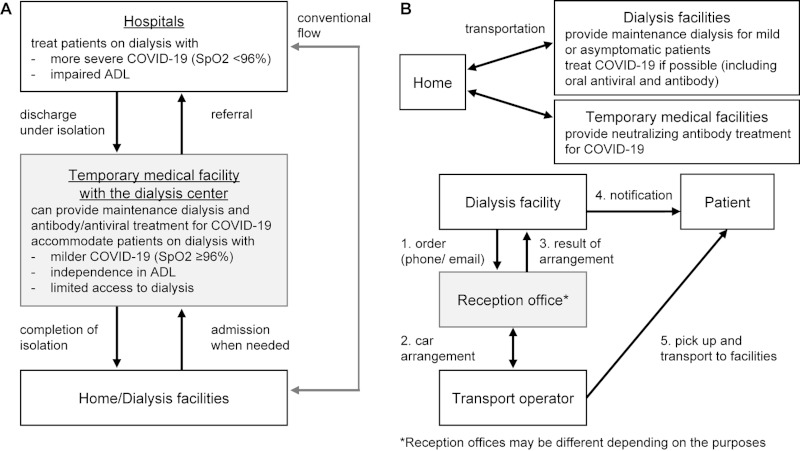
Schematic images of the temporary medical facility with the dialysis center (A) and the transportation scheme for patients on dialysis (B). Figure 1A illustrates how the temporary medical facility with the dialysis center could provide an additional capacity of beds between hospitals and homes. Figure 1B shows the scheme of transportation of patients needing dialysis from their homes to maintenance dialysis facilities (mainly clinics) or other temporary medical facilities.
Implementation of the temporary medical facility with the dialysis center and its functions
The temporary medical facility, with the dialysis center, which had a maximum capacity of 150 beds exclusively for patients with COVID-19, was established on December 28, 2021, by repurposing an old building that used to be a private dialysis hospital (9). At first, only non-dialysis patients were admitted to the facility, and it started to admit patients receiving dialysis on January 20, 2022. The dialysis center was installed within the facility, where 10 dialysis machines and the same number of exclusive beds were prepared. Therefore, if two cycles of dialysis were performed for each bed, up to 20 patients could receive dialysis daily. Dialysis could be performed four days a week. Doctors (at least one nephrologist when dialysis was performed), clinical engineers, nurses (especially those who had been unemployed to not put a burden on hospitals), nurse assistants, and administrative officers worked at the facility. Some over-the-counter medicines, prescribed medicines for symptomatic treatment, and medication for performing dialysis and oxygen (only used in an emergency for patients on dialysis) were available. Treatments with neutralizing antibodies and oral antivirals for COVID-19 (sotrovimab and molnupiravir) could also be performed for indicated patients. Only minimum necessary clinical testing was available, such as blood gas analysis. The facility was not equipped for chest radiography. Therefore, the temporary medical facility with the dialysis center was fundamentally no more than a temporary accommodation where dialysis and isolation were possible. Given that patients receiving dialysis have a higher risk of severe COVID-19, those showing deterioration (such as oxygen saturation < 96%) are not basically admitted and should be immediately transferred to the hospital. To secure a hospital referral, several local hospitals, including university hospitals, were designated as backup hospitals. However, when hospitals were particularly overcrowded, patients on dialysis who were in relatively severe condition could only be admitted to the temporary medical facility for a short time until an appropriate hospital was found.
The schematic of the temporary medical facility with the dialysis center is shown in Figure 1A. The facility could accommodate the following patients: those already hospitalized who still required isolation despite their symptoms being resolved, patients isolated at home who had difficulty receiving maintenance dialysis at their regular dialysis facilities, and patients receiving dialysis who called an ambulance for COVID-19 symptoms but could not find a transfer destination. In addition, patients seeking antibody treatment could also be admitted to other temporary medical facilities in the same way. When admitting and discharging patients receiving dialysis, it was crucial to cooperate with the patients' maintenance dialysis facilities or hospitals in case they were being hospitalized. Accordingly, patient information could be shared regarding the dialysis conditions, clinical course of COVID-19, and schedule for returning to regular dialysis at maintenance dialysis facilities after completing isolation.
We hosted an online seminar on February 3, 2022, inviting all dialysis hospitals in Tokyo. The seminar announced the newly established temporary medical facility with the dialysis center. Hospitals were requested to consider transferring their inpatients who still required days of isolation despite their symptoms being already resolved. In total, 94 of 172 dialysis hospitals (54.7%) attended the seminar.
Implementation of the transportation scheme and announcement of the strategic changes for dialysis facilities
Figure 1B shows the overview of the transportation scheme. This transportation system, introduced on February 5, 2022, enabled each dialysis clinic to order specialized negative pressure vehicles for its patients, encouraging it to perform outpatient dialysis for those with mild or asymptomatic COVID-19. Furthermore, patients with mild COVID-19 symptoms who need dialysis could be transferred to temporary medical facilities (either the one with the dialysis center or others) to receive sotrovimab. This strategy could expectedly reduce the risk of the condition worsening, at least for those infected with the Omicron BA.1 subvariant (10,11); in addition, it could not only ensure the facilitation of outpatient dialysis but also alleviate the burden on the whole medical provision system.
We hosted another online seminar on February 7, 2022. We invited almost all dialysis facilities in Tokyo, including clinics, to announce these schemes and to call on the strategic changes, emphasizing the importance of the division of roles and responsibilities for all. Among 442 dialysis facilities in Tokyo, 258 (there could be double-counts) attended the seminar. At the workshop, we encouraged dialysis facilities to prescribe oral antivirals (molnupiravir) upon diagnosis of COVID-19 if indicated. Furthermore, some lectures were provided based on the guidelines (3) to prevent nosocomial infection among patients with COVID-19 during dialysis at such facilities. After that seminar, the Tokyo Metropolitan Government began the subsidy program that covered the cost of infection prevention, such as personal protective equipment, as financial incentives for maintenance dialysis facilities performing outpatient dialysis for patients who tested positive for COVID-19.
Facing the second Omicron surge that began in early July, we hosted a similar online seminar on July 20 again. Of 447 dialysis hospitals and clinics, 233 (52.1%) attended this seminar.
Effects of these schemes and the strategic changes on the case fatality ratio (CFR) in patients on dialysis during the Omicron BA.1/2 and BA.5 surges
Figure 2 shows the weekly new positive cases and deaths in patients on dialysis from January to early September 2022 in Tokyo. The registry data of national patients needing dialysis with COVID-19, publicly released by the Task Force Committee, were collected from the websites of the Japanese Association of Dialysis Physicians and another related organization (12). There were two waves of infection during that period (so-called "sixth and seventh wave"), which were caused mainly by the Omicron BA.1/BA.2 and BA.5 subvariants, respectively. Notably, there was a dramatic decrease in the number of reported deaths in the seventh wave.
Figure 2.
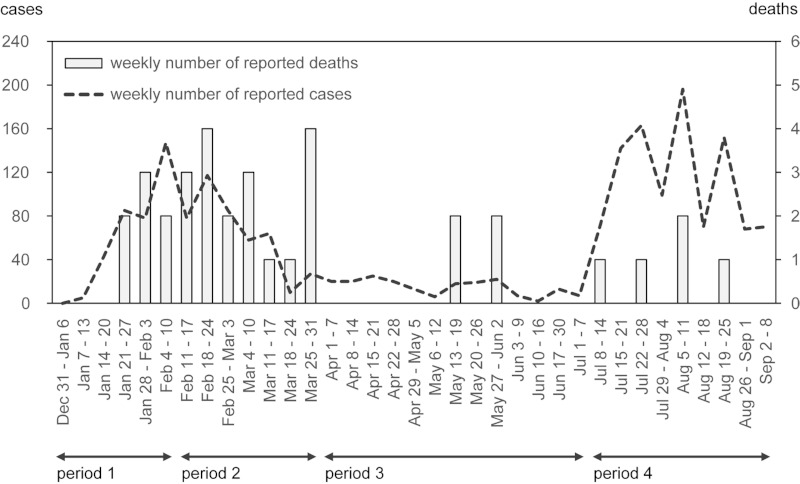
Weekly new positive cases and deaths in patients on dialysis from January to early September 2022 in Tokyo. The weekly number of reported deaths (bar) and new positive cases (dotted line) is shown from the beginning of the first Omicron surge to the second surge. The temporary medical facility with the dialysis center started admitting patients on dialysis on January 20, 2022 and the transportation scheme started on February 5, and they were subsequently announced on February 3 and 7. Four periods for calculating the case fatality ratio are indicated. Data were derived from weekly cumulative data released by the Task Force Committee. The number of weekly new positives (deaths) was calculated by comparing the cumulative numbers of positives (deaths) in consecutive weeks.
To calculate the CFR, we separated the study period into four different periods: period 1, before the strategic changes, from January 7 to February 10; period 2, the rest of the sixth wave, after the strategic changes, from February 11 to March 31; period 3, between the waves, from April 1 to July 7; period 4, during the seventh wave, from July 8 to September 8 (Figure 2). Since the calculation of the CFR from the registry data was a real-time estimation, the CFR could be underestimated when cases were increasing owing to the time delay from onset to death (13). To mitigate the bias, we exploited an alternate formula for the CFR, where the number of reported deaths was divided by the sum of the number of reported deaths and cases recovered from the disease (14).
The reported number of deaths and recovery over those periods was respectively as follows: period 1, seven and 78; period 2, 18 and 308; period 3, four and 150; period 4, five and 426. The CFRs during periods 1-4 were 8.2%, 5.5%, 2.6% and 1.2%, respectively. Using R software version 4.2.0 (The R Foundation for Statistical Computing, Vienna, Austria) (15), we conducted Fisher's exact test with the number of reported deaths and recovery to compare period 1 and other periods. Two-sided p-values were 0.32 for period 1 vs. period 2, 0.057 for period 1 vs. period 3 and 0.0010 for period 1 vs. period 4. Even though there was a matter of multiple comparisons, the p-value of period 1 vs. period 4 could be interpreted as statistically significant. Note that these figures could be biased owing to the reported time delay; for instance, if it takes longer to report patients' recovery than their death from the time of diagnosis, the CFR of period 1 can be overestimated. Additionally, we could not rule out the possibility that more death cases had been unreported during period 4 than during periods 1 and 2.
Having said that, there seemed to be a striking difference in CFR between these two waves. The number of hospital beds for patients receiving dialysis was not increased so much during those periods. One possible explanation could be that our public health measures were fairly effective, although it took a few months to fully produce the effect because the strategic changes required several processes in each dialysis facility including making procedure documents, procuring equipment, education and registering for prescription antivirals. The mechanism of how promoting outpatient dialysis can improve CFR in COVID-19 patients can be considered to be, for one thing, associated with improved accessibility to dialysis, which contributed to minimizing the disruption of dialysis schedules of patients. Skipping regular hemodialysis and not receiving dialysis for three days or more can impose excessive risk on patients, probably leading to deterioration in COVID-19 patients. Another explanation for reduced CFR may involve vaccination status. Unfortunately, data on COVID-19 vaccination coverage, specifically in patients on dialysis, were not available. Yet we instead collected data on vaccine coverage among people aged ≥ 65 years in Tokyo (16). At the beginning of period 1 (January 7), only 0.2% of people aged ≥ 65 years had received third shots. On February 25 (nearly in the middle of the sixth wave), the coverage ratio reached 50%. Regarding the coverage ratio of the fourth dose in the same population, 10.1% had received fourth shots at the beginning of period 4 (July 8). As early as August 8, the figure exceeded 50%, although this just coincided with the peak of the surge of infection. Therefore, the size of the immunized population might be smaller during periods 1 and 2 than during period 4; this factor could contribute to the improved CFR in period 4 to a certain degree. Other possible factors, which could affect CFRs include differences in herd immunity and viral pathogenicity between these two waves. Since available data and evidence are currently limited, future studies are needed to discuss these factors.
Conclusions
In this study, we observed a dramatic decrease in CFR in patients on dialysis during the seventh wave of COVID-19. Although the major contributing factor to this change has not been defined and needs further investigations, we believe, at least in part, our public health measures had an important role. Through our practices, we reconfirmed the importance of not only supplying necessary resources but also careful communication with local dialysis facilities. In particular, describing the situations with data, the definite need for the strategic changes and appropriate infection prevention measures were all important to collectively respond to the crisis.
Providing appropriate medical care for patients receiving dialysis with COVID-19 amid the surge of infection has been a formidable challenge. Not only does hospitalization become more challenging, but dialysis access can be seriously limited. To sustain the local medical provision system for them, effective hospital bed use, maintaining dialysis sessions and proactive treatments such as oral antivirals and neutralizing antibodies for indicated patients are of paramount importance. For that purpose, the combined strategies of improving the dialysis provision system and reducing demands, including efforts to prevent the spread of infection at each facility during regular times, are needed. Such emergency preparedness for maintaining essential health services, namely maintenance dialysis, should be cultivated to respond better to emergencies.
Funding: None.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. Terada M, Ohtsu H, Saito S, Hayakawa K, Tsuzuki S, Asai Y, Matsunaga N, Kutsuna S, Sugiura W, Ohmagari N. Risk factors for severity on admission and the disease progression during hospitalisation in a large cohort of patients with COVID-19 in Japan. BMJ Open. 2021; 11:e047007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kikuchi K, Yamakawa T, Ryuzaki M, Nangaku M; COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians, the Japanese Society for Dialysis Therapy, and the Japanese Society of Nephrology. The notification about the current situation of hospitalization arrangement for dialysis patients infected with COVID-19 and requests to dialysis facilities. http://www.touseki-ikai.or.jp/htm/03_info/doc/20210802_current_status_of_hospitalization_adjustment.pdf (accessed September 15, 2022). (in Japanese) .
- 3. The Japanese Association of Dialysis Physicians. Guidelines for Standard Hemodialysis Procedure and Prevention of Infection in Maintenance Hemodialysis Facilities (5th edition). http://www.touseki-ikai.or.jp/htm/05_publish/doc_m_and_g/20200430_infection%20control_guideline.pdf (accessed September 15, 2022). (in Japanese) .
- 4. Sugawara Y, Iwagami M, Kikuchi K, Yoshida Y, Ando R, Shinoda T, Ryuzaki M, Nakamoto H, Sakai K, Hanafusa N, Kashihara N, Nangaku M; COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians, the Japanese Society for Dialysis Therapy, and the Japanese Society of Nephrology. Infection prevention measures for patients undergoing hemodialysis during the COVID-19 pandemic in Japan: a nationwide questionnaire survey. Ren Replace Ther. 2021; 7:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kikuchi K, Yamakawa T, Ryuzaki M, Nangaku M; COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians, the Japanese Society for Dialysis Therapy, and the Japanese Society of Nephrology. Recommendations for ensuring medical care for dialysis patients with COVID-19 in Japan. http://www.touseki-ikai.or.jp/htm/03_info/doc/20210120_dialysis_medical_care_2.pdf (accessed September 15, 2022). (in Japanese) .
- 6. Kikuchi K, Yamakawa T, Ryuzaki M, Nangaku M; COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians, the Japanese Society for Dialysis Therapy, and the Japanese Society of Nephrology. The notification about use of antibody cocktail therapy for COVID-19 at clinics without beds. http://www.touseki-ikai.or.jp/htm/03_info/doc/20211001_0_use_of_antibody_cocktail_therapy.pdf (accessed September 15, 2022). (in Japanese) .
- 7. World Health Organization. Maintaining essential health services: operational guidance for the COVID-19 context, interim guidance, June 1 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2 (accessed September 15, 2022).
- 8. Ohmagari N. How did the Tokyo Metropolitan Government respond to COVID-19? Glob Heal Med. 2022; 4:67-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tokyo Metropolitan government. The 2746th press release. https://www.metro.tokyo.lg.jp/tosei/hodohappyo/press/2021/12/24/21.html (accessed September 15, 2022). (in Japanese) .
- 10. Jonny, Violetta L, Kartasasmita AS, Amirullah Roesli RM, Rita C. Pharmacological treatment options for coronavirus disease-19 in renal patients. Int J Nephrol. 2021; 2021:4078713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hoffmann M, Krüger N, Schulz S, Cossmann A, Rocha C, Kempf A, Nehlmeier I, Graichen L, Moldenhauer AS, Winkler MS, Lier M, Dopfer-Jablonka A, Jäck HM, Behrens GMN, Pöhlmann S. The Omicron variant is highly resistant against antibody-mediated neutralization: Implications for control of the COVID-19 pandemic. Cell. 2022; 185:447-456. e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. The Japanese Association of Dialysis Physicians. Information. http://www.touseki-ikai.or.jp/ (accessed September 15, 2022). (in Japanese) .
- 13. Nishiura H. Real-time estimation of the case fatality ratio and risk factors of death. Handbook of Statistics. 2017; 36:167-174. [Google Scholar]
- 14. World Health Organization. Estimating mortality from COVID-19. https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19 (accessed September 15, 2022).
- 15. R Core Team (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/ (accessed September 15, 2022).
- 16. Tokyo Metropolitan government. COVID-19 vaccination coverage. https://www.fukushihoken.metro.tokyo.lg.jp/iryo/kansen/coronavaccine/jisseki.html (accessed September 12, 2022). (in Japanese) .


