Abstract
Objective
There is a high prevalence of burnout in nurses. This systematic review investigates the use of music to manage burnout in nurses.
Data Source
MEDLINE (Ovid), MEDLINE InProcess/ePubs, Embase, APA PsycINFO, the Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov databases were searched.
Study Inclusion and Exclusion Criteria
Full-text articles were selected if the study assessed the use of music to manage burnout in nurses. Burnout was defined according to the International Classification of Diseases 11th Revision.
Data Extraction
Data were extracted using an Excel sheet. The second and third authors independently extracted study characteristics, frequency and type of music engagement, measures of burnout, and burnout outcomes (occupational stress, coping with stress, and related symptoms such as anxiety).
Data Synthesis
Study and outcome data were summarized.
Results
The literature search resulted in 2210 articles and 16 articles were included (n = 1205 nurses). All seven cross-sectional studies reported upon nurses’ self-facilitated use of music including music listening, playing instruments, and music entertainment for coping or preventing stress, supporting wellbeing, or enhancing work engagement. Externally-facilitated music engagement, including music listening, chanting, percussive improvisation, and song writing, was reported in the four randomized controlled trials and five cohort studies with reductions in burnout outcomes.
Conclusions
Self-facilitated and externally-facilitated music engagement can help to reduce burnout in nurses.
Keywords: burnout, music, nurses, stress, wellbeing
Introduction
Burnout is a syndrome resulting from prolonged workplace stress that has not been managed effectively.1 It is classified as an occupational phenomenon in the International Classification of Diseases 11th Revision.1 Adverse influences on mental health may be described by three characteristics: lack of energy or exhaustion, decreased motivation or cynical feelings related to one’s job, and reduced work performance.1 Consequences can also include physical issues, such as headaches, type 2 diabetes, and cardiovascular problems.2-4
Many studies have reported an increased risk for and high prevalence of burnout in healthcare workers, including nurses.5-10 Nurses make up the largest group of workers in the healthcare system,5 and are essential to its proper functioning.11 Higher levels of burnout in nurses may give rise to medical errors, decreased patient satisfaction, higher rates of patient mortality, and higher rates of nosocomial infections.5,12-16 Given that the adverse effects of burnout on nurses may also impact the quality of patient care, it is important to examine effective coping mechanisms for nurses to manage their occupational stress.15,17-20 Major sources of work-related stress in nurses may include workload, leadership and management, professional conflict, lack of reward, and emotional labour.6,21 Previous studies have explored various strategies for managing the occupational stress of healthcare workers.22 However, there is an absence of studies that examine the use of music to manage burnout in nurses, despite the amount of research supporting music’s efficacy for reducing stress.23 According to one systematic review and two meta-analyses, both passive and active engagement in music have been reported to reduce stress.23 A narrative literature review of music intervention studies in the workplace reported that psychological factors, communication, rehabilitative outcomes, and cognitive work performance seem to be the principal areas of interest in the field of music and occupational medicine, with possible economic benefits.24 The narrative literature review included 14 articles, but only three reported upon healthcare professionals. A study conducted to explore recreational music-making with nursing students resulted in statistically significant improvements in multiple burnout and mood dimensions, and potential annual cost savings of $16,800 were projected for the nursing program and $322,000 for the acute care hospital.25 Considering the prevalence of burnout in nurses and its impact on patient care and the healthcare system, and the positive impact of music on stress, a review of the use of music in relation to burnout in nurses could inform non-pharmacological support for the wellbeing of nurses.
Objective
This study will report upon the type of music utilized, how it is implemented, and the outcomes in relation to burnout in nurses. This review will be inclusive of cross-sectional studies, cohort studies, and randomized controlled trials (RCTs) providing reports from both nurses and researchers about the use of music in relation to burnout. Prevention of unmanaged occupational stress is integral to reducing burnout and further research is needed in this area.22 Previous findings from a review of a diversity of occupations suggest that music can have a positive impact on occupational health.24 Given the high levels of burnout in nurses and the reported benefits of music, a review of the literature specific to the use of music to manage burnout in nurses is warranted and may provide insight into the use of music to prevent burnout. Music interventions have been shown to positively impact the mental health of adults by enhancing emotional wellbeing, decreasing stress levels, inducing relaxation, and reducing depression.26-33 Music may be easily implemented in a cost-effective manner both in daily life and in medical settings, making it a viable option to help manage burnout in nurses.23
Methods
Study Design and Registration
The protocol of this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO; CRD42021268840). This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline.34
Search Strategy
MEDLINE (Ovid), MEDLINE InProcess/ePubs, Embase, APA PsycINFO, the Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov databases were searched systematically. Results were limited to the English language, and searches started from the initial coverage of the respective database to July 2021. The search strategy is described in Supplemental Appendix: Table A1. Backward and forward citation searching of included full-text articles was conducted using Google Scholar to identify relevant articles missed through database searching. Backward citation searching involved examining the reference lists of included full-text articles, while forward citation searching involved identifying articles that cited an included full-text article. Continued literature surveillance was done through July 2021.
Study Selection and Data Extraction
The second and third authors individually conducted title and abstract screening using Rayyan.35 They also independently conducted full-text evaluation, data extraction, and quality assessment. Full-text articles were selected according to the following inclusion criteria: the study assessed the use of music to manage burnout in nurses. Burnout was defined according to the International Classification of Diseases 11th Revision.1 This definition of burnout is inclusive of chronic workplace stress that has not been successfully managed. Thus, the outcomes of occupational stress, coping with stress, and related symptoms such as anxiety were included. Reviews, case reports, conference proceedings, dissertations, and book chapters were excluded. Demographics and outcome data were extracted using an Excel sheet. Any conflicts between the reviewers were resolved by the last author.
Extracted study characteristics included the year of publication, country, study design, age, gender, sample size, intervention, comparison, and delivery methods. The type and frequency of music engagement were also extracted. The primary outcome was burnout, inclusive of the use of music as a coping strategy and other indicators of wellbeing.
Quality Assessment
The quality of the included studies was assessed by the second and third authors independently using the Newcastle-Ottawa Scale (NOS) and the Joanna Briggs Institute’s (JBI) critical appraisal tools.36-38 The NOS quality assessment forms were used to assess cohort studies and cross-sectional studies.36,37 The NOS checklist contains three sections: selection, comparability, and outcomes. The JBI critical appraisal checklist was used for RCTs.38 This checklist appraises the appropriateness of study design, study population, outcomes, and statistical analysis. The reviewers met to discuss the results of their appraisal and any disagreements were resolved by the last author.
Results
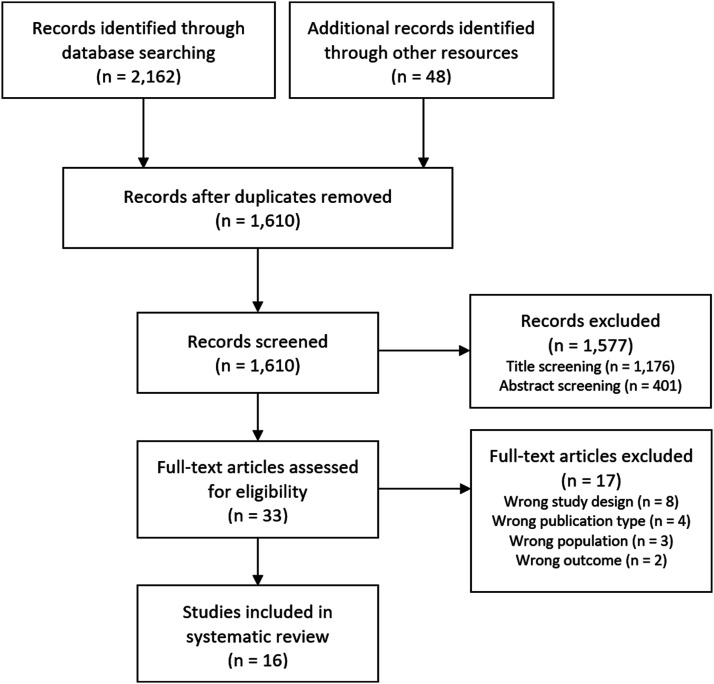
The literature search resulted in 2210 articles (Figure 1). After removing duplicates, 1610 titles and abstracts were screened resulting in 1577 studies being excluded. Of the remaining 33 studies, 17 full-text articles were excluded.39-55 The reasons for exclusion are provided in Supplemental Appendix: Table A2. Sixteen studies met the inclusion criteria.56-71 The included studies contained a total of 1205 participants across eight different countries: Australia,57,59,60,67,68 United States,56,58,61,65 Turkey,64,69 Finland,70 Greece,66 India,71 Taiwan,62 and the United Kingdom.63 The studies were published between 2005 to 2021.
Figure 1.
PRISMA flow diagram.
Study Characteristics
The demographics of the included studies are summarized in Table 1. The average age of participants was 40 ± 7 years, and 7% were male. In total, this review includes seven cross-sectional studies (43.8%),58,60,61,63,67,68,70 five cohort studies (31.3%),56,57,59,65,69 and four RCTs (25.0%).62,64,66,71 The seven cross-sectional studies collected reports directly from nurses.58,60,61,63,67,68,70 The four RCTs reported upon different uses of music for burnout: (1) self-selected music listening,62 (2) researcher-selected music listening during progressive muscle relaxation,64 (3) chanting,71 and (4) percussive improvisation.66 One cohort study implemented song writing65 and four cohort studies used directed music listening to induce relaxation during progressive muscle relaxation, aromatherapy massage, or mindfulness activities.56,57,59,69 The seven cross-sectional studies distributed surveys,58,61 interviews,60,63,67,68 or questionnaires.70 The RCTs and cohort studies utilized validated scales such as the Copenhagen Burnout Inventory – 19 Items,56 Perceived Occupational Stress Scale,57,59 Perceived Stress Scale – 10 Items,64 Fatigue Severity Scale,64 Faces Anxiety Scale,57,59 Professional Quality of Life Scale – 30 Items,56,65,69 Visual Analogue Scale,62 and Hospital Anxiety and Depression Scale.72 Two studies (12.5%) employed biomarkers to measure stress such as heart rate, finger temperature, serum cortisol, dehydroepiandrosterone sulfate, and salivary alpha-amylase.62,71
Table 1.
Characteristics of included studies.
| Study (Year) | Country | Study Design | Age (Mean ± SD Years) | Gender (% Male) | Sample Size (N) |
|---|---|---|---|---|---|
| Davis (2005)59 | Australia | Cohort | 36.4 | 18.2 | 68 |
| Rose (2006)67 | Australia | Cross-sectional | 30 - 50 | 0 | 5 |
| Cooke (2007)57 | Australia | Cohort | 37.5 | 20.5 | 79 |
| Cutshall (2010)58 | US | Cross-sectional | Various | NR | 49 |
| Rose (2010)68 | Australia | Cross-sectional | NR | 0 | 16 |
| Lai (2011)62 | Taiwan | RCT | 23.4 ± 2.5 | 0 | 54 |
| Happell (2013)60 | Australia | Cross-sectional | NR | NR | 38 |
| Jordan (2016)61 | US | Cross-sectional | 41.0 ± 10.8 | 4 | 120 |
| Tuisku (2016)70 | Finland | Cross-sectional | 44.9 | 5.8 | 530 |
| Oates (2018)63 | UK | Cross-sectional | Various | 18.5 | 27 |
| Ploukou (2018)66 | Greece | RCT | NR | 4.2 | 48 |
| Ceravolo (2019)56 | US | Cohort | NR | NR | 12 |
| Ozgundondu (2019)64 | Turkey | RCT | 26.2 ± 3.9 | 0 | 56 |
| Phillips (2020)65 | US | Cohort | 38.2 ± 10.7 | 4.7 | 43 |
| Semerci (2020)69 | Turkey | Cohort | 40.2 ± 4.3 | 0 | 30 |
| W.J (2021)71 | India | RCT | 28.5 ± 3.6 | 0 | 30 |
Abbreviations: NR, not reported; RCT, randomized controlled trial; SD, standard deviation; UK, United Kingdom; US, United States.
Cross-Sectional Studies
Seven of the 16 studies (43.8%) were cross-sectional and collected self-reported data from nurses about their general use of music for burnout.58,60,61,63,67,68,70 The seven cross-sectional studies reported: (1) 61% of nurses used music therapy as a coping strategy,58 (2) music listening was the second most common activity for coping with stress,61 (3) music listening and playing instruments was one of the four activities reported by nurses to support wellbeing,63 (4) 20% of the nurses in the study used music listening as a coping mechanism,67 (5) music was used to cope with stress,68 (6) music on the wards was one of the 11 suggestions by nurses to reduce occupational stress,60 and (7) nurses who participated in cultural activities provided by their employer (such as music entertainment) rated their work engagement to be significantly increased compared to non-participants.70
Nurses experiencing moderate stress ranked music therapy as their most utilized complementary and alternative medicine therapy.58 No description of how music was used within music therapy was provided. Although nurses who engaged in cultural activities (including music entertainment) rated their work engagement to be significantly increased compared to non-participants, no change in burnout (perceived stress) was reported.70 No descriptions that identified which participants specifically attended each type of cultural activity were provided.
In total, five cross-sectional studies (71.4%) reported upon self-directed use of music for coping with stress or supporting wellbeing.58,61,63,67,68 One study (14.3%) suggested music on the wards as a stress prevention strategy.60 One study (14.3%) reported that nurses who attended employer-provided cultural events (such as music entertainment) rated their work engagement to be significantly increased.70 A summary of the outcomes of included studies is provided in Table 2.
Table 2.
Summary of outcomes.
| Study (Year) | Sample Size (N) | Type of Music Engagement | Frequency of Music Engagement | Reporting Method | Measure | Effect of Music on Burnout Outcomes |
|---|---|---|---|---|---|---|
| Cross-sectional studies | ||||||
| Rose (2006)67 | 5 | Self-directed music listening | NR | Self-reported | Oral narrative/storytelling and reflective journaling | 1/5 (20%) reported using music as a coping strategy |
| Cutshall (2010)58 | 49 | Music therapy (undescribed) | NR | Self-reported | Written survey | 61% reported using music therapy as a coping strategy |
| Rose (2010)68 | 16 | Music (undescribed leisure activities) | NR | Self-reported | Semi-structured interviews/storytelling and reflective journaling | Music was used as a coping strategy |
| Happell (2013)60 | 38 | Self-directed music listening | NR | Self-reported | Six focus group interviews | Music on the wards was listed as one of 11 stress prevention strategies (the number of nurses that suggested this is unknown) |
| Jordan (2016)61 | 120 | Self-directed music listening | NR | Self-reported | Survey | Music listening was rated as the second most common activity (46%) for coping with work-related stress |
| Tuisku (2016)70 | 530 | Employer-provided opportunities to attend cultural events, including music entertainment | 29 nurses (5%) reported participating in cultural activities three times or more, 45 (9%) reported participating twice, 141 (27%) reported participating once, 313 (59%) reported no participation, and 2 (.4%) did not report participation in a 6-month period | Self-reported | Digital questionnaire & 5-point Likert Scale | Nurses who participated in cultural activities rated their work engagement to be significantly increased compared to non-participants. It was not reported how often nurses participated in any cultural activities that were music entertainment |
| Oates (2018)63 | 27 | Self-directed music listening and playing an instrument alone or with others in musical bands | NR | Self-reported | Semi-structured interviews | Music was one of four activities reported by nurses to support wellbeing |
| Cohort studies | ||||||
| Davis (2005)59 | 68 | Researcher-directed music listening (new-age music) in conjunction with aromatherapy massage | 15-minute sessions, once a week for 12 weeks | Observed | POSS & FAS | No significant difference for job satisfaction and occupational stress (POSS). 86% reported reduced anxiety (FAS) |
| Cooke (2007)57 | 79 | Researcher-directed music listening (new-age music) in conjunction with aromatherapy massage | 15-minute sessions, once a week for 12 weeks, one period during summer and one period during winter | Observed | POSS & FAS | No significant difference for job satisfaction and occupational stress. 92% reported that music and aromatherapy massage reduced anxiety |
| Ceravolo (2019)56 | 12 | Researcher-directed music listening (‘soft’ music), aromatherapy, using a singing bowl, and mindfulness | 60-minute session once weekly for 8 weeks | Observed | ProQOL-30, CBI-19 | Significant increase in compassion satisfaction scores and significant reductions in risk for burnout scores (ProQOL-30); significant reductions in personal burnout and work-related burnout scores (CBI-19) |
| Phillips (2020)65 | 43 | Song writing once a week for 4 weeks. Weeks 1-4: Story Development, Week 5: Song Development - song recording and performance; Week 6: Debriefing Session - final writing session and experience debriefing | Week 1-4 (Story Development): 1-1.5 hours once weekly, Week 5 (Song Development): 4 hours, Week 6: NR | Observed | ProQOL-30 | Significant reductions in burnout and secondary traumatic stress scores; significant increase in compassion satisfaction scores |
| Semerci (2020)69 | 30 | Researcher-directed music listening (relaxation music) in conjunction with progressive muscle relaxation | 25-30-minute session once weekly for 8 weeks | Observed | ProQOL-30 | Significant reductions in burnout and compassion fatigue scores |
| Randomized controlled trials | ||||||
| Lai (2011)62 | 54 | Self-selected music listening with headphones. Music selections included: piano music (n = 20, 37%), slow jazz (n = 13, 24.1%), harp music (n = 11, 20.4%), Western orchestral (n = 5, 9.3%), and Chinese orchestral music (n = 5, 9.3%) during chair rest | 30 minutes of music listening | Observed | VAS, heart rate, mean arterial pressure, finger temperature, serum cortisol | Significant reduction in self-perceived stress scores, heart rate, mean arterial pressure, and cortisol. Significantly increased finger temperature; significant correlations between music preference and heart rate, mean arterial pressure, finger temperature, and self-perceived stress |
| Ploukou (2018)66 | 46 | Percussion improvisation sessions. Instruments included: Bongo drum, Djembe, Doumbek and in some cases maraca, castanets, triangle, wood block, ratchet and tambourine | 60-minute session once a week for one month | Observed | HADS, PILL | Significant reductions in depression & anxiety (HADS), and psychosomatic symptoms (PILL) |
| Ozgundondu (2019)64 | 56 | Researcher-directed music listening (music: Daniel Kobialka) in conjunction with progressive muscle relaxation | 20-minute session once weekly for 8 weeks | Observed | FSS, PSS | Significant reductions in stress (PSS) and fatigue (FSS) at weeks 8 and 12. Significant improvements were reported for self-distraction, acceptance, instrumental support, emotional support, and venting |
| W.J (2021)71 | 30 | Mahamantra chanting | 20 minutes each day (during any personally convenient time) for 45 days | Observed | VAS, heart rate, mean arterial pressure, finger temperature, serum cortisol | Significant reductions in serum cortisol and SAA and a non-significant increase in DHEA-S |
Abbreviations: CBI-19, Copenhagen Burnout Inventory - 19 Items; DHEA-S, dehydroepiandrosterone sulfate; FAS, Faces Anxiety Scale; FSS, Fatigue Severity Scale; HADS; Hospital Anxiety and Depression Scale; NR, not reported; PILL, Pennebaker Inventory of Limbic Languidness; POSS, Perceived Occupational Stress Scale; ProQOL-30, Professional Quality of Life Scale - 30 Items; PSS, Perceived Stress Scale - 10 Items; SAA, salivary alpha-amylase; VAS, Visual Analogue Scale.
Cohort Studies
Five of the 16 studies (31.3%) were cohort studies which reported different uses of music for burnout: (1) researcher-directed music listening with aromatherapy massage,57,59 (2) researcher-directed music listening with mindfulness activities,56 (3) researcher-directed music listening with progressive muscle relaxation,69 and (4) facilitated song writing.65 Two of the cohort studies (40.0%) combined music listening with aromatherapy massage.57,59 In both studies, nurses were offered 15-minute aromatherapy massages while listening to new-age music once a week over a 12-week period. One of these two studies compared two 12-week periods, one in the summer and one in the winter.57 Both studies reported that music with aromatherapy massage led to no significant difference in job satisfaction or occupational stress pre- and post-intervention. However, 86-92% of the nurse participants reported reduced anxiety.57,59 One study (20%) combined researcher-directed music listening with progressive muscle relaxation.69 Nurses participated in group sessions for 25-30 minutes once a week for eight weeks. This led to a significant reduction in burnout and compassion fatigue.69 One study (20%) implemented researcher-directed music listening with mindfulness activities.56 Nurses participated in the mindfulness activities while listening to soft music once a week for eight weeks. This led to a significant increase in compassion satisfaction and a significant reduction in scores for risk for burnout, personal burnout, and work-related burnout.56 One study (20%) implemented a six-week facilitated song writing activity that occurred once weekly.65 This study reported that music-related activities led to a significant reduction in burnout and secondary traumatic stress; a significant reduction in depression, insomnia, and loneliness; and a significant increase in self-compassion and self-awareness. In addition, music-related activities resulted in a significant increase in compassion satisfaction.65
All five cohort studies included an external facilitator for the use of music and occurred in a group setting. Duration of the interventions varied from 15 minutes over 12 weeks (music with aromatherapy massage),57,59 25-30 minutes over eight weeks (music with progressive muscle relaxation),69 and approximately 1.5 hours each week for four weeks (song writing).65 Four of the cohort studies (80.0%) investigated the use of music in conjunction with another activity (progressive muscle relaxation, aromatherapy massage, or mindfulness activities) and implemented researcher-directed music listening.56,57,59,69 Of these four studies, two reported a significant reduction specifically in burnout,65,69 and two reported significant reductions in anxiety but no significant change in occupational stress.57,59 One of the cohort studies (20.0%) investigated the use of song writing and reported significant reductions in burnout.65
Randomized Controlled Trials
Four of the 16 studies (25.0%) were RCTs and each reported upon different uses of music for burnout: (1) self-selected music listening,62 (2) percussive improvisation,66 (3) researcher-directed music listening with progressive muscle relaxation,64 and (4) chanting.71 In one of the RCTs (25.0%), nurses engaged in self-directed music listening for 30 minutes and reported significantly reduced self-perceived stress scores, reduced heart rate, mean arterial pressure, and cortisol; significantly increased finger temperature; and significant correlations between music preference and self-perceived stress.62 Additionally, 88.9% of the participants reported engaging in music listening to reduce stress. The music listening options included: piano music (n = 20, 37%), slow jazz (n = 13, 24.1%), harp music (n = 11, 20.4%), Western orchestral music (n = 5, 9.3%), and Chinese orchestral music (n = 5, 9.3%). One study (25.0%) implemented 60-minute drumming classes once weekly for four weeks and reported significant reductions in depression, anxiety, and psychosomatic symptoms.66 One study (25.0%) implemented pre-determined music listening during 20-minute progressive muscle relaxation sessions that occurred once weekly for eight weeks.64 Participants in the intervention group reported a significant reduction in perceived stress and fatigue severity scores at weeks 8 and 12; and significant improvements for self-distraction, acceptance, instrumental support, emotional support, and venting.64 One study (25.0%) engaged nurses in chanting and reported significant reductions in serum cortisol and salivary alpha-amylase, and an insignificant increase in dehydroepiandrosterone sulfate.71
All four RCTs included an external facilitator for the use of music. In total, one study (25.0%) reported upon self-selected music listening,62 two (50.0%) reported upon active music engagement (chanting, improvised percussion),66,71 and one (25.0%) reported upon researcher-directed music listening in conjunction with progressive muscle relaxation for burnout.64
Types of Music Engagement
The sixteen studies in this review reported upon eight different types of music engagement: (1) self-directed music listening (25.0%);60-62,67 (2) self-directed playing of music instruments and/or self-selected music listening (6.3%);63 (3) song writing (6.3%);65 (4) chanting (6.3%);71 (5) percussive improvisation (6.3%);66 (6) music entertainment (6.3%);70 (7) researcher-directed music listening in conjunction with progressive muscle relaxation (12.5%),64,69 aromatherapy massage (12.5%),57,59 or mindfulness activities (6.3%);56 and (8) music without description (12.5%).58,68
Quality Assessment
The NOS scores of the five included cohort studies ranged from 4 – 6 out of a possible score of 9 (Supplemental Appendix: Table A3).56,57,59,65,69 The five cohort studies were of poor quality. The NOS scores of the seven included cross-sectional studies ranged from 2 – 6 out of a possible score of 10 (Supplemental Appendix: Table A4).58,60,61,63,67,68,70 According to the Agency for Healthcare Research and Quality (AHRQ) standards, one study70 was satisfactory and six studies58,60,61,63,67,68 were unsatisfactory. The JBI critical appraisal checklist was used to assess the four RCTs.62,64,66,71 The scores ranged from 8 – 10 out of a possible score of 13 (Supplemental Appendix: Table A5), resulting in the inclusion of all four studies.
Discussion
To the best of our knowledge, this is the first systematic review to report upon the use of music to manage burnout in nurses. Drawing upon the World Health Organization’s definition of burnout, unmanaged occupational stress is the main indicator of burnout. The 16 studies in this review reported upon eight different uses of music for burnout in nurses including managing occupational stress. It is not possible to make any conclusive statements about the use of music for burnout in nurses, not only due to the differences in study designs, but the differences in the types of music, frequency, duration, control groups and comparisons. To report upon the use of music for burnout with confidence, larger sample sizes are required, comparisons between the different uses of music are required, and controls need to be in place for variables such as facilitator and group effects. Additionally, the cultural use of music needs to be explored. In this review, studies were conducted across eight different countries. The findings, in relation to the type of music used, may be specific to the cultural demographics of the study. Despite the heterogeneity of the use of music in these studies, music has been shown to have a positive impact on the outcome of burnout. The results of the included studies primarily suggest that there were two mechanisms of music engagement that nurses used to manage their occupational burnout: (1) self-facilitated engagement and (2) externally-facilitated engagement.
Self-Facilitated Music Engagement
All seven cross-sectional studies reported upon nurses’ self-facilitated use of music including music listening, playing instruments, and music entertainment for coping or preventing stress, supporting wellbeing, or enhancing work engagement. Music may be easily utilized in daily life and medical settings and is thus accessible to nurses to manage stress and burnout, and to promote wellbeing.33,57,59-61,63,66-68 According to four cross-sectional studies, nurses were proactively engaging in self-selected music listening.60,61,63,67 When provided the opportunity to engage in music entertainment, they reported their work engagement to be significantly increased, even though there was no change in their perceived stress.70 Music entertainment may encourage work engagement through communication and collective participation.70 Additionally, feeling connected to others can enhance wellbeing as a preventative measure.73 This was also noted for the playing of musical instruments, such as participating in an ensemble which may encourage feelings of connectedness.63 Self-use of music may be effective for instant mood regulation through distraction and for improving perceived levels of anxiety by shifting one’s attention from stressful environmental stimuli to auditory information.63,74,75 The cross-sectional studies did not reveal how often nurses are listening to music, or the preferences of music. However, it appears that nurses are self-selecting music, which aligns with previous studies supporting the use of preferred music to induce relaxation and reduce physical and perceived stress.62,76,77 The importance of preferred music, or personalized use of music, is also highlighted in the cross-sectional study conducted by Cutshall and colleagues.58 Data collection through surveys and storytelling sessions provide the opportunity to report upon the strategies that nurses employed to manage burnout. A common theme was the use of self-directed music (music listening, playing an instrument, or undefined) to cope with occupational stress. Considering the accessibility of music listening, and the research supporting the use of music listening for reducing stress,78 health promotion practitioners may want to consider advocating for the use of music listening in healthcare settings.
Externally-Facilitated Music Engagement
Externally-facilitated music engagement, including music listening, chanting, percussive improvisation, and song writing, was reported in the four RCTs and five cohort studies with reductions in burnout outcomes. Systems-level facilitators can improve the mental wellbeing of nurses by providing external aid and access to music sessions instructed by trained professionals. These external facilitators can include the government, unit managers, and other stakeholders that determine the allocation of healthcare financial resources. The high prevalence of burnout among nurses necessitates the involvement of external facilitators to manage nurses’ occupational stress. The studies included in this review point towards positive outcomes of participation in music sessions facilitated by trained professionals. For instance, musical participation through cultural or religious events, including chanting and drum circles, may be effective to promote nurses’ mental and physical health.66,71,79,80 This type of active music engagement often requires a trained facilitator and often occurs in a group setting which can promote social cohesion. In this review, five of the studies used facilitated music in conjunction with another intervention; therefore, the results of the study do not solely reflect the use of music. Through music facilitation, nurses were able to learn musical skills to engage in song writing, chanting, and drumming regardless of their background in music. Song writing in a group setting may reduce loneliness through the sharing of experiences and enhanced self-awareness. Music-related activities, such as improvised drumming, may provide nurses with an opportunity to express their feelings, resulting in reduced burnout and improved wellbeing and patient care.66 Healthcare settings may want to consider providing nurses the opportunity to actively engage in making music with a facilitator to reduce outcomes of burnout.
Related Research
A review of music in the workplace suggests that music can positively influence psychological symptoms, work-related stress, and burnout and improve work performance and cognitive outcomes.24 The review did not include cross-sectional studies or target the nurse population specifically, but it does support similar findings to our systematic review which included studies that demonstrated a positive impact of music on burnout.56-71 A study of music listening for workplace stress stated that daily music listening could reduce work-related stress and that the effects may be related to individual musical preferences and familiarity.78 This is a similar finding to this current systematic review which reports upon the self-directed use of music listening among nurses, and the ability of preferred music to induce relaxation and reduce physical and perceived stress.57,59-64,66-68 A study exploring both music listening and music therapy interventions in relation to pain reported both modes as equally effective for stress and anxiety reduction.81 In the current systematic review, studies using both music interventions56,57,59-71 and a music therapy intervention58 reported the positive impact of music on burnout or related outcomes. However, Bradt et al.81 also reported that 77.4% of the participants preferred music therapy for future treatments. The preferences for music therapy were due to therapeutic relationships, interactive music-making, and the possibility of emotional expression.81-83 None of the included studies in the current systematic review compared the effectiveness, feasibility, and preferences of music and music therapy interventions. Development of standards for music therapy interventions and research comparing music and music therapy interventions may be necessary for further investigation.
Future Directions
Further research is needed to collect samples with rigorous randomization and the use of control groups. It may be important to determine whether the effectiveness of music may be influenced by anticipation of its benefits and daily use of music.62 In addition, investigating associations between variables such as personal characteristics and the impact of music on burnout may be necessary.57,66 Longitudinal studies are required to determine the long-term effects of various music interventions on burnout in nurses.63,64,69,71 Further research is needed to incorporate accepted complementary therapies in control groups to provide context for the effectiveness of music on burnout in nurses compared to other interventions.71
Limitations
This systematic review has several limitations. Among the 16 included studies, seven studies (43.8%) had a cross-sectional study design.58,60,61,63,67,68,70 From these studies, it was not possible to determine the direct impact of music on burnout and stress in nurses. Various scales were used56,57,59,62,64,65,69,70 and thus a meta-analysis was not conducted. Moreover, 11 studies (68.8%) were unsatisfactory or of poor quality according to AHRQ standards.56,58-61,63,65,67-69 Small sample size,56,61,65,66 homogeneous nature of the sample,56,59,61,66,68 non-randomized group assignment,65 convenience sampling,65 low response rate,61,63,70 voluntary bias,62 inherent bias,64 and response bias were reported.61 Poor representativeness may reduce the generalizability of conclusions.
Conclusions
Self-reports from nurses indicate the use of self-facilitated music for coping with stress, preventing stress, supporting wellbeing, or enhancing work engagement. Data collected from RCTs and cohort studies indicate that externally-facilitated music engagement can reduce burnout in nurses. This systematic review demonstrates the utility of music as an intervention to reduce burnout and promote mental health in nurses.
SO WHAT? Implications for Health Promotion Practitioners and Researchers
What is already known on this topic?
There is a high prevalence of burnout in nurses. According to one systematic review and two meta-analyses, both passive and active engagement in music have been reported to reduce stress.
What does this article add?
To the best of our knowledge, this is the first systematic review that evaluates the use of music to manage burnout in nurses. It provides insight into nurses’ current use of music for coping with stress, an aspect of burnout, and describes the externally-facilitated music that has been implemented to reduce burnout in nurses.
What are the implications for health promotion practice or research?
This systematic review demonstrates the utility of music as an intervention to reduce burnout and promote mental health in nurses. Considering the prevalence of burnout in nurses and its impact on patient care and the healthcare system, this review could inform non-pharmacological support for the wellbeing of nurses.
Supplemental Material
Supplemental Material for The Use of Music to Manage Burnout in Nurses: A Systematic Review by Rachael Finnerty, Katherine Zhang, Rina A. Tabuchi, and Kevin Zhang in American Journal of Health Promotion
Author Contributions: Study concept and design: Kevin Zhang, Rachael Finnerty. Acquisition, analysis, and interpretation of data: all authors. Writing of manuscript: all authors. Critical review and approval of manuscript: all authors.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental Material for this article is available online.
ORCID iDs
Rachael Finnerty https://orcid.org/0000-0003-1131-2918
Kevin Zhang https://orcid.org/0000-0003-1183-5743
References
- 1.World Health Organization . Burn-out an “occupational phenomenon”: International classification of diseases. Published online May 28, 2019. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases
- 2.Leiter MP, Hakanen JJ, Ahola K, Toppinen-Tanner S, Koskinen A, Väänänen A. Organizational predictors and health consequences of changes in burnout: A 12-year cohort study. J Organ Behav. 2013;34(7):959-973. doi: 10.1002/job.1830 [DOI] [Google Scholar]
- 3.Lubbadeh T. Job burnout: A general literature review. Int Rev Manag Market. 2020;10(3):7-15. doi: 10.32479/irmm.9398 [DOI] [Google Scholar]
- 4.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatr. 2016;15(2):103-111. doi: 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friganović A, Selič P, Ilić B, Sedić B. Stress and burnout syndrome and their associations with coping and job satisfaction in critical care nurses: A literature review. Psychiatr Danub. 2019;31(suppl 1):21-31. [PubMed] [Google Scholar]
- 6.Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J Psychiatr Res. 2020;123:9-20. doi: 10.1016/j.jpsychires.2019.12.015 [DOI] [PubMed] [Google Scholar]
- 7.Myhren H, Ekeberg Ø, Stokland O. Job satisfaction and burnout among intensive care unit nurses and physicians. Critical Care Research and Practice. 2013;2013:1-6. doi: 10.1155/2013/786176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lasebikan VO, Oyetunde MO. Burnout among nurses in a Nigerian general hospital: Prevalence and associated factors. International Scholarly Research Network Nursing. 2012;2012:402157. doi: 10.5402/2012/402157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aiken LH, Clarke SP, Sloane DM, et al. Nurses’ reports on hospital care in five countries. Health Aff. 2001;20(3):43-53. doi: 10.1377/hlthaff.20.3.43 [DOI] [PubMed] [Google Scholar]
- 10.Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286-3302. doi: 10.1111/jan.14839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fawaz M, Anshasi H, Samaha A. Nurses at the front line of COVID-19: Roles, responsibilities, risks, and rights. Am J Trop Med Hyg. 2020;103(4):1341-1342. doi: 10.4269/ajtmh.20-0650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pérez-Francisco DH, Duarte-Clíments G, del Rosario-Melián JM, Gómez-Salgado J, Romero-Martín M, Sánchez-Gómez MB. Influence of workload on primary care nurses’ health and burnout, patients’ safety, and quality of care: Integrative review. Healthcare. 2020;8(1):12. doi: 10.3390/healthcare8010012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeung DY, Kim C, Chang SJ. Emotional labour and burnout: A review of the literature. Yonsei Med J. 2018;59(2):187-193. doi: 10.3349/ymj.2018.59.2.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hersch RK, Cook RF, Deitz DK, et al. Reducing nurses’ stress: A randomized controlled trial of a web-based stress management program for nurses. Appl Nurs Res. 2016;32:18-25. doi: 10.1016/j.apnr.2016.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Welp A, Meier LL, Manser T. Emotional exhaustion and workload predict clinician-rated and objective patient safety. Front Psychol. 2015;5:1573. doi: 10.3389/fpsyg.2014.01573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care–associated infection. Am J Infect Control. 2012;40(6):486-490. doi: 10.1016/j.ajic.2012.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Oliveira SM, de Alcantara Sousa LV, Vieira Gadelha MdS, do Nascimento VB. Prevention actions of burnout syndrome in nurses: An integrating literature review. Clin Pract Epidemiol Ment Health. 2019;15:64-73. doi: 10.2174/1745017901915010064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reith TP. Burnout in United States healthcare professionals: A narrative review. Cureus. 2018;10(12):e3681. doi: 10.7759/cureus.3681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Med Care. 2007;45(12):1195-1204. doi: 10.1097/MLR.0b013e3181468ca3 [DOI] [PubMed] [Google Scholar]
- 20.Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med. 2002;346(22):1715-1722. doi: 10.1056/NEJMsa012247 [DOI] [PubMed] [Google Scholar]
- 21.McVicar A. Workplace stress in nursing: A literature review. J Adv Nurs. 2003;44(6):633-642. doi: 10.1046/j.0309-2402.2003.02853.x [DOI] [PubMed] [Google Scholar]
- 22.De Giorgi R, Dinkelaar BM. Strategies for preventing occupational stress in healthcare workers: Past evidence, current problems. BJPsych Adv. 2021;27(3):205-210. doi: 10.1192/bja.2020.90 [DOI] [Google Scholar]
- 23.de Witte M, Spruit A, van Hooren S, Moonen X, Stams GJ. Effects of music interventions on stress-related outcomes: A systematic review and two meta-analyses. Health Psychol Rev. 2020;14(2):294-324. doi: 10.1080/17437199.2019.1627897 [DOI] [PubMed] [Google Scholar]
- 24.Raglio A, Oddone E, Morotti L, et al. Music in the workplace: A narrative literature review of intervention studies. J Compl Integr Med. 2020;17(4). doi: 10.1515/jcim-2017-0046 [DOI] [PubMed] [Google Scholar]
- 25.Bittman BB, Snyder C, Bruhn KT, et al. Recreational music-making: An integrative group intervention for reducing burnout and improving mood states in first year associate degree nursing students: Insights and economic impact. Int J Nurs Educ Scholarsh. 2004;1(1). doi: 10.2202/1548-923X.1044 [DOI] [PubMed] [Google Scholar]
- 26.Chanda ML, Levitin DJ. The neurochemistry of music. Trends Cognit Sci. 2013;17(4):179-193. doi: 10.1016/j.tics.2013.02.007 [DOI] [PubMed] [Google Scholar]
- 27.Heiderscheit A, Chlan L, Donley K. Instituting a music listening intervention for critically ill patients receiving mechanical ventilation: Exemplars from two patient cases. Music Med. 2011;3(4):239-245. doi: 10.1177/1943862111410981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koelsch S. Music-evoked emotions: principles, brain correlates, and implications for therapy: Functional neuroanatomy of music-evoked emotions. Ann NY Acad Sci. 2015;1337(1):193-201. doi: 10.1111/nyas.12684 [DOI] [PubMed] [Google Scholar]
- 29.Bradt J, Dileo C. Music interventions for mechanically ventilated patients. Cochrane Database Syst Rev. 2014;2014(12):CD006902. doi: 10.1002/14651858.CD006902.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamioka H, Mutoh Y, Yamada M, et al. Effectiveness of music therapy: A summary of systematic reviews based on randomized controlled trials of music interventions. Patient Prefer Adherence. 2014;8:727-754. doi: 10.2147/PPA.S61340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nilsson U. The anxiety- and pain-reducing effects of music interventions: A systematic review. Assoc Perioperat Register Nurse J. 2008;87(4):780-807. doi: 10.1016/j.aorn.2007.09.013 [DOI] [PubMed] [Google Scholar]
- 32.Daykin N, Mansfield L, Meads C, et al. What works for wellbeing? A systematic review of wellbeing outcomes for music and singing in adults. Persp Pub Health. 2018;138(1):39-46. doi: 10.1177/1757913917740391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Witte M, Spruit A, van Hooren S, Moonen X, Stams GJ. Effects of music interventions on stress-related outcomes: A systematic review and two meta-analyses. Health Psychol Rev. 2020;14(2):294-324. doi: 10.1080/17437199.2019.1627897 [DOI] [PubMed] [Google Scholar]
- 34.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed June 21, 2021
- 37.Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. Bio Med Central Pub Health. 2013;13(1):154. doi: 10.1186/1471-2458-13-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joanna Briggs Institute . Critical appraisal tools. Published online n.d. https://jbi.global/critical-appraisal-tools Accessed August 27, 2021
- 39.Field T, Quintino O, Henteleff T, Wells-Keife L, Delvecchio-Feinberg G. Job stress reduction therapies. Altern Ther Health Med. 1997;3(4):54-56. [PubMed] [Google Scholar]
- 40.Lambert VA, Lambert CE, Ito M. Workplace stressors, ways of coping and demographic characteristics as predictors of physical and mental health of Japanese hospital nurses. Int J Nurs Stud. 2004;41(1):85-97. doi: 10.1016/S0020-7489(03)00080-4 [DOI] [PubMed] [Google Scholar]
- 41.Tracy MF, Lindquist R, Savik K, et al. Use of complementary and alternative therapies: A national survey of critical care nurses. Am J Crit Care. 2005;14(5):404-415. doi: 10.4037/ajcc2005.14.5.404 [DOI] [PubMed] [Google Scholar]
- 42.Chang EM, Daly JW, Hancock KM, et al. The relationships among workplace stressors, coping methods, demographic characteristics, and fealth in Australian nurses. J Prof Nurs. 2006;22(1):30-38. doi: 10.1016/j.profnurs.2005.12.002 [DOI] [PubMed] [Google Scholar]
- 43.Repar PA, Patton D. Stress reduction for nurses through arts-in-medicine at the university of New Mexico hospitals. Holist Nurs Pract. 2007;21(4):182-186. doi: 10.1097/01.HNP.0000280929.68259.5c [DOI] [PubMed] [Google Scholar]
- 44.Schwarzkopf R, Brown C, Silkin R, Toby-Harris L, Torres M, Voss D. Caring for self: Promoting personal wellness for nursing leaders in the hospital environment. Nurse Leader. 2007;5(5):34-46. doi: 10.1016/j.mnl.2007.07.010 [DOI] [Google Scholar]
- 45.Rose J, Glass N. An investigation of emotional wellbeing and its relationship to contemporary nursing practice. Collegian. 2009;16(4):185-192. doi: 10.1016/j.colegn.2009.08.001 [DOI] [PubMed] [Google Scholar]
- 46.Van der Colff JJ, Rothmann S. Occupational stress, sense of coherence, coping, burnout and work engagement of registered nurses in South Africa. SA J Ind Psychol. 2009;35(1):423. doi: 10.4102/sajip.v35i1.423 [DOI] [Google Scholar]
- 47.Brooks DM, Bradt J, Eyre L, Hunt A, Dileo C. Creative approaches for reducing burnout in medical personnel. Arts Psychother. 2010;37(3):255-263. doi: 10.1016/j.aip.2010.05.001 [DOI] [Google Scholar]
- 48.Logid J. The healing power of art: Is it just for patients? Creativ Nurs. 2011;17(3):118-119. doi: 10.1891/1078-4535.17.3.118 [DOI] [PubMed] [Google Scholar]
- 49.Sonke J, Pesata V, Arce L, Carytsas FP, Zemina K, Jokisch C. The effects of arts-in-medicine programming on the medical-surgical work environment. Arts Health. 2015;7(1):27-41. doi: 10.1080/17533015.2014.966313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karpavičiūtė S, Macijauskienė J. The impact of arts activity on nursing staff well-being: An intervention in the workplace. Int J Environ Res Publ Health. 2016;13(4):435. doi: 10.3390/ijerph13040435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Phillips C, Welcer B. Songs for the soul: A program to address a nurse’s grief. Clin J Oncol Nurs. 2017;21(2):145-146. doi: 10.1188/17.CJON.145-146 [DOI] [PubMed] [Google Scholar]
- 52.Catlin A, Cobbina M, Dougherty R, Laws D. Music, spirituality, and caring science: The effect of a cappella song on healthcare staff in medical–surgical units. Int J Hum Caring. 2019;23(3):234-241. doi: 10.20467/1091-5710.23.3.234 [DOI] [Google Scholar]
- 53.Veiga G, Dias Rodrigues A, Lamy E, Guiose M, Pereira C, Marmeleira J. The effects of a relaxation intervention on nurses’ psychological and physiological stress indicators: A pilot study. Compl Ther Clin Pract. 2019;35:265-271. doi: 10.1016/j.ctcp.2019.03.008 [DOI] [PubMed] [Google Scholar]
- 54.Bianchini C, Copeland D. The use of mindfulness-based interventions to mitigate stress and burnout in nurses. J Nurses Prof Dev. 2021;37(2):101-106. doi: 10.1097/NND.0000000000000708 [DOI] [PubMed] [Google Scholar]
- 55.Zamanifar S, Bagheri-Saveh MI, Nezakati A, Mohammadi R, Seidi J. The effect of music therapy and aromatherapy with chamomile-lavender essential oil on the anxiety of clinical nurses: A randomized and double-blind clinical trial. J Med Life. 2020;13(1):87-93. doi: 10.25122/jml-2019-0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ceravolo D, Raines DA. The impact of a mindfulness intervention for nurse managers. J Holist Nurs. 2019;37(1):47-55. doi: 10.1177/0898010118781620 [DOI] [PubMed] [Google Scholar]
- 57.Cooke M, Holzhauser K, Jones M, Davis C, Finucane J. The effect of aromatherapy massage with music on the stress and anxiety levels of emergency nurses: Comparison between summer and winter. J Clin Nurs. 2007;16(9):1695-1703. doi: 10.1111/j.1365-2702.2007.01709.x [DOI] [PubMed] [Google Scholar]
- 58.Cutshall S, Derscheid D, Miers AG, et al. Knowledge, attitudes, and use of complementary and alternative therapies among clinical nurse specialists in an academic medical center. Clin Nurse Spec. 2010;24(3):125-131. doi: 10.1097/NUR.0b013e3181d86cd1 [DOI] [PubMed] [Google Scholar]
- 59.Davis C, Cooke M, Holzhauser K, Jones M, Finucane J. The effect of aromatherapy massage with music on the stress and anxiety levels of emergency nurses. Australas Emerg Nurs J. 2005;8(1-2):43-50. doi: 10.1016/j.aenj.2005.05.001 [DOI] [PubMed] [Google Scholar]
- 60.Happell B, Dwyer T, Reid-Searl K, Burke KJ, Caperchione CM, Gaskin CJ. Nurses and stress: Recognizing causes and seeking solutions. J Nurs Manag. 2013;21(4):638-647. doi: 10.1111/jonm.12037 [DOI] [PubMed] [Google Scholar]
- 61.Jordan TR, Khubchandani J, Wiblishauser M. The impact of perceived stress and coping adequacy on the health of nurses: A pilot investigation. Nurs Res Pract. 2016;2016:1-11. doi: 10.1155/2016/5843256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lai HL, Li YM. The effect of music on biochemical markers and self-perceived stress among first-line nurses: A randomized controlled crossover trial: Music reduces stress. J Adv Nurs. 2011;67(11):2414-2424. doi: 10.1111/j.1365-2648.2011.05670.x [DOI] [PubMed] [Google Scholar]
- 63.Oates J. What keeps nurses happy? Implications for workforce well-being strategies. Nurs Manag. 2018;25(1):34-41. doi: 10.7748/nm.2018.e1643 [DOI] [PubMed] [Google Scholar]
- 64.Ozgundondu B, Gok Metin Z. Effects of progressive muscle relaxation combined with music on stress, fatigue, and coping styles among intensive care nurses. Intensive Crit Care Nurs. 2019;54:54-63. doi: 10.1016/j.iccn.2019.07.007 [DOI] [PubMed] [Google Scholar]
- 65.Phillips CS, Volker DL, Davidson KL, Becker H. Storytelling through music: A multidimensional expressive arts intervention to improve emotional well-being of oncology nurses. JOC Oncol Pract. 2020;16(4):e405-e414. doi: 10.1200/JOP.19.00748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ploukou S, Panagopoulou E. Playing music improves well-being of oncology nurses. Appl Nurs Res. 2018;39:77-80. doi: 10.1016/j.apnr.2017.11.007 [DOI] [PubMed] [Google Scholar]
- 67.Rose J, Glass N. Community mental health nurses speak out: The critical relationship between emotional wellbeing and satisfying professional practice. Collegian. 2006;13(4):27-32. doi: 10.1016/S1322-7696(08)60537-5 [DOI] [PubMed] [Google Scholar]
- 68.Rose J, Glass N. An Australian investigation of emotional work, emotional well-being and professional practice: An emancipatory inquiry. J Clin Nurs. 2010;19(9-10):1405-1414. doi: 10.1111/j.1365-2702.2009.02997.x [DOI] [PubMed] [Google Scholar]
- 69.Semerci R, Öztürk G, Akgün Kostak M, Elmas S, İhsan Danacı A, Musbeg S. The effect of progressive muscle relaxation exercises on compassion satisfaction, burnout, and compassion fatigue of nurse managers. Perspect Psychiatr Care. 2020;57(3):1250-1256. doi: 10.1111/ppc.12681 [DOI] [PubMed] [Google Scholar]
- 70.Tuisku K, Pulkki-Råback L, Virtanen M. Cultural events provided by employer and occupational wellbeing of employees: A cross-sectional study among hospital nurses. Work. 2016;55(1):93-100. doi: 10.3233/WOR-162389 [DOI] [PubMed] [Google Scholar]
- 71.Niva WJ, Sekar L, Manikandan A, et al. Mahamantra chanting as an effective intervention for stress reduction among nursing professionals—A randomized controlled study. Adv Integrat Med. 2020;8(1):27-32. doi: 10.1016/j.aimed.2020.05.007 [DOI] [Google Scholar]
- 72.Djukanovic I, Carlsson J, Årestedt K. Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65–80 years old? A psychometric evaluation study. Health Qual Life Outcome. 2017;15(1):193. doi: 10.1186/s12955-017-0759-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Martino J, Pegg J, Frates EP. The connection prescription: Using the power of social interactions and the deep desire for connectedness to empower health and wellness. Am J Lifestyle Med. 2017;11(6):466-475. doi: 10.1177/1559827615608788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee D, Henderson A, Shum D. The effect of music on preprocedure anxiety in Hong Kong Chinese day patients. J Clin Nurs. 2004;13(3):297-303. doi: 10.1046/j.1365-2702.2003.00888.x [DOI] [PubMed] [Google Scholar]
- 75.Thaut MH, Davis WB. The influence of subject-selected versus experimenter-chosen music on affect, anxiety, and relaxation. J Music Ther. 1993;30(4):210-223. doi: 10.1093/jmt/30.4.210 [DOI] [Google Scholar]
- 76.Lai HL. Music preference and relaxation in Taiwanese elderly people. Geriatr Nurs. 2004;25(5):286-291. doi: 10.1016/j.gerinurse.2004.08.009 [DOI] [PubMed] [Google Scholar]
- 77.Pelletier CL. The effect of music on decreasing arousal due to stress: A meta-analysis. J Music Ther. 2004;41(3):192-214. doi: 10.1093/jmt/41.3.192 [DOI] [PubMed] [Google Scholar]
- 78.Raglio A, Bellandi D, Gianotti M, et al. Daily music listening to reduce work-related stress: A randomized controlled pilot trial. J Publ Health. 2019;42(1):e81-e87. doi: 10.1093/pubmed/fdz030 [DOI] [PubMed] [Google Scholar]
- 79.Amin A, Kumar SS, Rajagopalan A, et al. Beneficial effects of OM chanting on depression, anxiety, stress and cognition in elderly women with hypertension. Indian J Clin Anat Physiol. 2016;3(3):253. doi: 10.5958/2394-2126.2016.00056.6 [DOI] [Google Scholar]
- 80.Smith C, Viljoen JT, McGeachie L. African drumming: A holistic approach to reducing stress and improving health? J Cardiovasc Med. 2014;15(6):441-446. doi: 10.2459/JCM.0000000000000046 [DOI] [PubMed] [Google Scholar]
- 81.Bradt J, Potvin N, Kesslick A, et al. The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: A mixed methods study. Support Care Cancer. 2015;23(5):1261-1271. doi: 10.1007/s00520-014-2478-7 [DOI] [PubMed] [Google Scholar]
- 82.de Witte M, Pinho AdS, Stams GJ, Moonen X, Bos AER, van Hooren S. Music therapy for stress reduction: A systematic review and meta-analysis. Health Psychol Rev. 2020;2020:1-26. Published online November 12. doi: 10.1080/17437199.2020.1846580 [DOI] [PubMed] [Google Scholar]
- 83.Gutgsell KJ, Schluchter M, Margevicius S, et al. Music therapy reduces pain in palliative care patients: A randomized controlled trial. J Pain Symptom Manag. 2013;45(5):822-831. doi: 10.1016/j.jpainsymman.2012.05.008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for The Use of Music to Manage Burnout in Nurses: A Systematic Review by Rachael Finnerty, Katherine Zhang, Rina A. Tabuchi, and Kevin Zhang in American Journal of Health Promotion