Abstract
Plain language summary available online
Dear Editor, As of 15 February 2020, the novel coronavirus (2019‐nCoV) has rapidly spread throughout China and across the world, with more than 60 000 laboratory‐confirmed cases. Due to the current lack of specific treatment and the risk of transmission during the viral incubation period, infection prevention and control of 2019‐nCoV are both urgent and critical to global health. In this article we aim to highlight the necessity of implementing protective measures, and recommend how to set in place proper emergency management plans for preventing and controlling nosocomial infection of 2019‐nCoV in dermatology departments.
A cluster of unexplained cases of pneumonia was initially reported in Wuhan, China in December 2019. The pathogen, a novel coronavirus named 2019‐nCoV, was isolated from lower‐respiratory‐tract samples of infected patients, and the resultant disease was termed COVID‐19 (Coronavirus Disease 2019). Of note, the transmission of 2019‐nCoV may occur during an incubation period that may be as long as 14 days.1,2 Currently, infection prevention and control are urgent and critical due to the lack of specific treatment and heightened risk of spreading during the incubation period.
During the outbreak of COVID‐19, it was discovered that 78% of infected professionals worked in general wards,3 which indicates the strong transmissibility of COVID‐19 and reminds us of the high risk of nosocomial transmission in general departments. Since the outbreak, the Chinese government has implemented a series of strict prevention and control measures; however, it is still possible to miss infected patients in the asymptomatic incubation period. Additionally, both awareness of protection and protective facilities are generally lacking in medical departments, including dermatology. Moreover, most patients in dermatology department have skin lesions, which makes it easier for 2019‐nCoV to transmit via indirect contact. Therefore, dermatology departments could be at relatively high risk for COVID‐19 outbreaks, and it is necessary to set in place emergency management protocols to prevent and control the nosocomial infection of COVID‐19 in dermatology departments.
Located in the infected centre, our hospital has set up pre‐examination and triage stations both at the hospital entrance and in the outpatient department of each subdepartment. In addition, a dermatologist is assigned to cooperate with nurses at the dermatology triage stations to evaluate patients further if necessary. Triage to the fever clinic is necessary when patients with skin disorders have fevers or are suspected of being infected with COVID‐19 (Figure 1).1 When the fever is considered to be caused by a skin disease, the dermatologist participates in the consultation. For patients determined to be free of viral infection, confirmed as noninfected or discharged by the designated department, the dermatology clinic is then made accessible.
Figure 1.
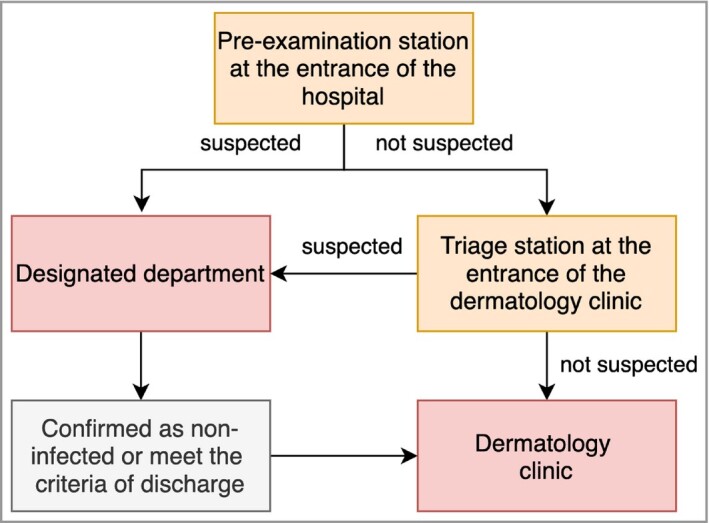
Flow diagram of pre‐examination triage for outpatients with skin disease. Note: for the diagnostic criteria for confirmed cases, suspected cases and discharge, refer to reference [2]
Wearing of N95 masks and hand hygiene need to be performed correctly by care providers and patients during consultation.4 For patients requiring hospitalization, transfer to wards will be permitted only if the results of blood routine tests and chest computed tomography scans identify the patient's illness to be unassociated with COVID‐19.1
Online consultation for nonemergency patients and those with mild conditions has obviously decreased the number of patients in dermatology clinics during the epidemic period, which reduces the probability of nosocomial infection of 2019‐nCoV.
Emergency management procedures for inpatients suspected of having COVID‐19 have been put in place. Although strict measures are implemented in the outpatient department, patients in the asymptomatic incubation period might still be admitted to the dermatology ward. Therefore, emergency management for inpatients should be carried out urgently when an inpatient has symptoms associated with COVID‐19 during hospitalization. Experienced staff trained about COVID‐19 should be organized immediately to set up a contingency group to prevent and control the outbreak of COVID‐19. This group should discuss daily and report the updated conditions of patients with suspected infection. This group should then communicate with the experts in the respiratory intensive care and radiology departments in a timely manner to evaluate whether the patient needs further examination and treatment to exclude COVID‐19. The above measures will stabilize the order of wards and avoid the nosocomial infection of 2019‐nCoV.
Isolation, reporting and transfer of suspected patients must be conducted following local infection control policies and processes.
Patients’ skin disorders might be neglected in the quarantine ward. For this reason, we first recommend sending pictures of skin lesions to the dermatologist via email or teleconference to analyse the patient's condition. If the condition is still unclear, the dermatologist should go to the clean area of the isolation ward for a multidisciplinary consultation. When none of the above works, it is the responsibility of the dermatologist to consult at the patient's bedside. The information about the patient, such as the primary disease, evolution of skin disease, medication, related examinations and other special medical history, should be provided to the dermatologist in advance. By this method, the exposure time of the dermatologist to the patient and the infection risk can be greatly reduced.
Although our hospital is in an infected centre, no infected patients have been detected in our departments, owing to heightened surveillance. Most of our recommendations are based on integrating current clinical practice with previous experiences during similar coronavirus outbreaks. With the accumulation of clinical evidence and the development of science and technology, these management principles will be modified continually.
References
- Jin YH, Cai L, Cheng ZS. et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019‐nCoV) infected pneumonia (standard version). Mil Med Res 2020; 7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothe C, Schunk M, Sothmann P. et al. Transmission of 2019‐nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020; 382:970–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Hu B, Hu C. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA 2020; 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson T, Del Mar C, Dooley L. et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev 2011: CD006207. [DOI] [PMC free article] [PubMed] [Google Scholar]


