Abstract
Background
COVID-19 continues to disproportionately impact families of children with developmental disabilities (DD). There is an urgent need to understand these families’ experiences, particularly those that face economic or social marginalization. This qualitative study sought to identify the experiences of families of children with DD during the COVID-19 pandemic.
Methods
Using phenomenology, in-depth interviews (IDIs) were conducted with caregivers and health care providers of children with DD living in a large urban Canadian city. Interviews were recorded, transcribed, and coded using inductive coding methods by two independent coders. Transcripts were analyzed within and across stakeholder groups using thematic analysis.
Results
A total of 25 IDIs were conducted in 2020. 3 main themes and 7 sub-themes emerged related to the experiences of parents and health care providers for children with DD: families reported difficulty adhering to public health measures leading to isolation and increased parental stress; restricted access to in-person services worsened behaviour and development; and worsened household financial security in already marginalized families.
Conclusions
Our study demonstrates that families of children with DD have been negatively impacted by the evolving environment from the COVID-19 pandemic, and even more so in those who face social and economic challenges. Public health restrictions have impaired the daily lives of these families and our study suggests that limitations to accessing in-person services may have long-lasting impacts on the well-being of families of children with DD. It is imperative that the unique needs of these families be considered and centred for future interventions.
Keywords: Caregiver, Children, COVID-19 pandemic, Developmental disabilities, Lived experiences
INTRODUCTION
One in 16 children in Canada has a developmental disability (DD) impacting motor, cognitive, language, and behavioural developmental domains (1). DD refers to a wide range of conditions, including autism spectrum disorder (ASD), cerebral palsy (CP), intellectual disability, attention deficit hyperactivity disorder (ADHD), and metabolic-genetic disorders (2). Children with DD rely on a delicate patchwork of services from health care providers, therapists (behavioural therapists, occupational therapists, physiotherapists, speech-language therapists), respite services, and family support services (3). During the COVID-19 pandemic, many services were abruptly cancelled or severely restricted (4,5). While challenges in accessing services are not new, they were magnified during the pandemic and continue to persist (4,5).
As seen in previous humanitarian crises, research since the onset of the pandemic reveals significant negative impacts of the COVID-19 pandemic on families of children with DD (FCDD) compared to other families (4–8). FCDD are twice as likely to be living in poverty compared to the general population. Children and youth living in poverty have been significantly impacted by COVID-19, with an increased risk of poor mental health outcomes (2,8,9).
To best support FCDD, interventions should address their identified family and community needs, for example, delivering programs in the community instead of requiring travel (10). However, few studies have engaged FCDD to understand their specific needs and develop tailored interventions during the COVID-19 pandemic. In this formative research study, we explored the experiences of FCDD to understand the impact of the COVID-19 pandemic on their well-being and functioning, with the intent of informing a future community-based intervention.
METHODS
Study design and location
This was a formative research study using phenomenology as our primary qualitative methodology, which explores the lived experiences of individuals who have shared a common experience (11). Our study took place in a large, Canadian hospital that provides outpatient, multidisciplinary care for FCDD, many of whom face social barriers. In addition, our study included community agencies that have a strong working relationship with the department.
Sampling and recruitment
Using a non-random purposive sampling framework, 15 caregivers and 10 care providers were invited to participate in in-depth interviews (IDIs) conducted virtually by telephone. The number of participants was in accordance with recommended sample sizes for phenomenological studies (12). Caregivers were included if they had a child with a diagnosed DD that had been previously assessed in the clinic and were informed of the study by a social worker or service navigator within their circle of care. Types of DDs included can be found in Table 2. Care providers who work with children with DD were identified by publicly available means (e.g., hospital and clinic websites, listservs). Care providers were included in the study if they currently worked or supported children and families with DD. These included physicians, social workers, nurses, occupational therapists, dietitians, and early childhood educators. All participants provided consent to participate, were 18 years of age or older, and had access to a telephone. Caregivers who wished to participate but did not speak English consented to an interview with a trained researcher with a medical interpreter. Caregivers were provided a $50 grocery store gift card for their participation in the study.
Table 2.
Demographics of caregivers (n=15)
| N (%) | |
|---|---|
| Relationship to child | |
| Biological mother | 13 (87%) |
| Biological father | 2 (13%) |
| Households with ≥2 children | 13 (87%) |
| Age of children in household | |
| School age (2007–2016) | 14 (93%) |
| Adolescents (2006 and earlier) | 1 (7%) |
| Households with ≥1 child with diagnosis | |
| Autism spectrum disorder (ASD) | 11 (73%) |
| Attention deficit hyperactivity disorder (ADHD) | 4 (27%) |
| Developmental delay | 5 (33%) |
| Other (i.e., cerebral palsy, learning disabilities, mood disorder) | 6 (40%) |
| Parent immigration status | |
| Canadian/Permanent resident | 12 (80%) |
| Refugee/Refugee Claimant | 3 (20%) |
| Length of time in Canada | |
| >5 years | 9 (60%) |
| ≤5 years | 6 (40%) |
| Spoken language preference | |
| English | 10 (67%) |
| Other | 5 (33%) |
| Total household income | |
| <$60 K | 9 (60%) |
| ≥$60 K | 4 (27%) |
| Not reported | 2 (13%) |
| Full-time employment | |
| Pre-pandemic | 5 (33%) |
| During pandemic | 3 (20%) |
| Part-time employment | |
| Pre-pandemic | 4 (27%) |
| During pandemic | 2 (13%) |
| Not employed | |
| Pre-pandemic | 6 (40%) |
| During pandemic | 10 (67%) |
| Housing | |
| House (market rent/own) | 3 (20%) |
| Apartment (market rent/own) | 9 (60%) |
| Subsidized housing | 2 (13%) |
| Not reported | 1 (7%) |
| Number of Internet-enabled devices at home | |
| <5 | 9 (60%) |
| ≥5 | 6 (40%) |
| Monthly household Internet costs | |
| >$100 | 12 (80%) |
| <$100 | 3 (20%) |
| Not reported | 2 (13%) |
Data collection
IDIs were conducted by telephone between June and August 2020. Interviews were conducted by 2 trained female researchers (T.F., P.K.B.) and were overseen by principal investigators (S.S., R.S.M.), who were female and male, respectively. The authors conducting interviews were not involved in patient care or clinic procedures and did not have an established relationship with any participants. Participants were introduced to T.F. and P.K.B. as research assistants. A semi-structured interview guide was iteratively developed and pilot tested. All interviews were recorded and transcribed verbatim, and field notes were made during and after interviews. Interviews ranged from 30 minutes to 2 hours. A demographic questionnaire was completed after each interview, which identified children’s diagnoses, age, and household factors, including language, income, employment and immigration status for caregivers and gender identity, occupation, and length of practice for health care providers.
Data analysis
A codebook was created inductively by the research team (T.F. and S.S.) by identifying, classifying, and labelling the primary patterns in the interview transcripts. Inductive coding uses a bottom-up approach, allowing emerging themes to come from stakeholder sentiments to drive the creation of codes. Transcripts were coded by 2 independent coders (T.F. and S.S.). Iterative testing was conducted, and the codebook was modified accordingly until a pooled kappa coefficient of 0.85 was reached, demonstrating high inter-rater reliability (13). Dedoose qualitative software was used for data management during coding and analysis (14). Themes were explored within and between stakeholder groups and verified using group discussion with the research team. Redundancy was reached in thematic analysis, indicating data saturation (15,16). Preliminary findings were summarized and presented at research team meetings (in July and August 2020) to provide an opportunity to solicit feedback from stakeholders (i.e., participant checking). This study complied with the Consolidated Criteria for Reporting Qualitative Research (COREQ) Checklist (17). This study was approved by the St. Michael’s Hospital Research Ethics Board (REB #: 20-127).
RESULTS
Demographics
A total of 25 interviews were conducted: 15 caregivers (Table 1) and 10 care providers (Table 2). All 15 caregivers reported being the birth parent of their child with DD. Five caregivers (33%) had arrived in Canada less than 5 years ago. The most common DD was ASD (66%), followed by ADHD, developmental delay, CP, and speech impairment. Nine families (60%) had a total household income of less than $60,000 per year, of which most were below the low-income cut-off (LICO) for a family of 4 (18). Most caregivers (66%) spoke English as their primary language. Before the pandemic, 6/15 (40%) were unemployed, which increased to 10/15 (66%) after the pandemic began.
Table 1.
Demographics of care providers (n=10)
| N (%) | |
|---|---|
| Gender identity | |
| Female | 10 (100%) |
| Professional designation | |
| Dietitian | 1 (10%) |
| Early Childhood Educator | 1 (10%) |
| Occupational Therapist | 1 (10%) |
| Physician | 3 (30%) |
| Registered Nurse | 2 (20%) |
| Social Worker | 2 (20%) |
| Length of time working with children with developmental disabilities (DD) | |
| 1–10 | 3 (30%) |
| 10+ | 7 (70%) |
| Practice setting | |
| Community health centre or public health agency | 4 (40%) |
| Hospital-based ambulatory care or community agency providing direct developmental services | 5 (50%) |
| Family health team | 1 (10%) |
| Virtual services | |
| Yes | 10 (100%) |
| Virtual service modality | |
| Telephone | 10 (100%) |
| Zoom/Skype | 4 (40%) |
| Ontario Telemedicine Network (OTN) | 5 (50%) |
| Webex | 2 (20%) |
A variety of care providers were interviewed, including a dietician, early childhood educator, occupational therapist, physicians, registered nurses, and social workers. Of the care providers, most (7/10) had worked with children with DD for over 10 years. In terms of practice setting, half (5/10) were based out of a hospital, 4 were community-based, and 1 worked in both settings. All care providers were female.
Thematic analysis
We identified 3 main themes and 7 sub-themes related to the impact of COVID-19 on FCDD (Supplementary Table).
Families of children with DD had difficulty adhering to public health measures which increased isolation and stress
Both caregivers and providers reported difficulty coping with the increased isolation and stress that resulted from adhering to public health measures. They found it difficult to leave their homes; some reported that they felt they were not allowed to leave while others found it too challenging to manage their children’s behaviours and comply with public health measures (Q1–4, Supplementary Table). Most caregivers felt it was more stressful to try to leave home with their children and therefore, opted to spend more time indoors than they previously would have. Caregivers also noted that it was difficult to engage their children in virtual school and programming, especially while working from home (Q5–8, Supplementary Table). With increased demands on caregivers, lack of support, and changing work environments, many felt stressed and unproductive, unable to work efficiently and balance the needs of their children (Q9–11, Supplementary Table). Care providers felt that families had no routines at home during lockdown, which they believe led to increased behavioural challenges amongst children (Q12–13, Supplementary Table).
Reduced access to therapies and services impacted child behaviour and development
Caregivers and care providers reported that children with DD displayed behavioural changes throughout the pandemic. Before the pandemic, caregivers observed gains in their children’s behavioural, social, and language development, all of which slowed or regressed during the pandemic (Q14–17, Supplementary Table). Difficulties with sleeping and higher levels of stress were also noted. There were also reported difficulties in receiving therapy and services due to the abrupt closure of services (Q18–22, Supplementary Table). Caregivers were worried their children were missing critical therapeutic windows for intervention and had decreased opportunities for socialization, leading to mental health and developmental challenges. A few caregivers and care providers reported that their children’s social skills improved while at home, as caregivers were able to spend more time with their children in a controlled environment (Q23–25, Supplementary Table).
The pandemic negatively impacted family financial security
Both caregivers and care providers discussed the financial challenges that families experienced. Firstly, caregivers reported increased costs of having their children at home, as they needed to provide more food for them and invest in supplies for activities to keep them busy (Q26, Supplementary Table). In addition, caregivers and care providers noted challenges with receiving funding (Q27, Supplementary Table). For many, funding that had previously been confirmed was delayed. Those that were in the process of applying for funding or needed to contact funding offices experienced major barriers due to office closures. However, many caregivers did note the beneficial impact of government programs like Canadian Emergency Response Benefit (CERB) (Q28, Supplementary Table). They found this support to be very helpful and important for their well-being. Care providers discussed the financial impact that job loss had on the families they were working with (Q29, Supplementary Table).
DISCUSSION
Our study highlighted the experiences of FCDD who also face social and economic barriers during the COVID-19 pandemic. Caregivers said that public health measures meant they stayed home and were isolated, and many reported that their child’s previous programming became virtual or stopped altogether, consistently highlighting the difficulties their children had with virtual programming. While many caregivers reported that their child’s behavioural progress slowed or regressed, some children with social anxiety may have experienced improvement. Most reported exceptional challenges to balance caring for a child with DD while also managing other roles at home, including working and managing other children, and many reported increased stress.
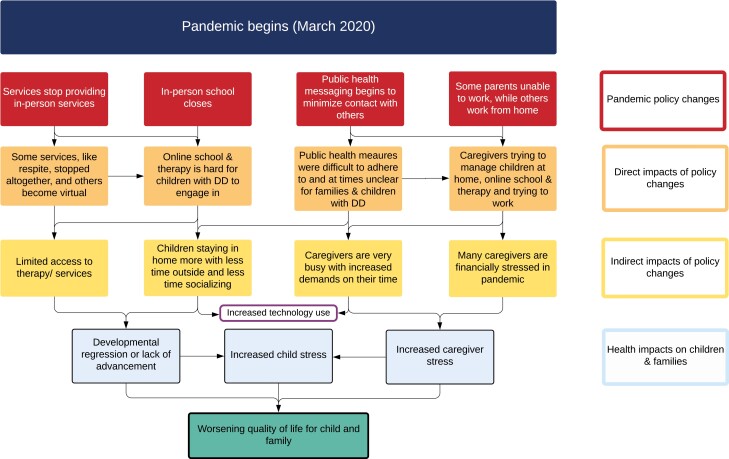
Our study findings highlight the indirect and direct impact of the COVID-19 and resultant public health measures on service disruptions for children with DD and family stress (Figure 1). This has been seen in previous humanitarian and localized crises; for example, in Hurricane Ike, services were severely restricted, leading to lack of access to therapy and children with DD experienced behavioural, academic, and social skill regressions, as was noted in our current study (6). Although public health restrictions related to COVID-19 continue to change, it is important to recognize that the impact of service disruption was profound for these families.
Figure 1.
Conceptual model of direct and indirect pandemic policy changes on families of children with DD.
Caregivers reported considerable frustration and difficulty with accessing services virtually. While virtual care and therapy were sometimes available for children with DD, caregivers felt it to be much less effective for children, and many opted out of these options, effectively leaving children and families without access to therapy at all. Many therapeutic services, such as physiotherapy, occupational therapy, and behavioural therapy, require specialized equipment that is not available at home, warranting in-person appointments (19). As virtual programming was akin to a cessation of therapies and services, this has led to caregiver burnout and family stress, which was also endorsed by the participants in our study (4). Although virtual care has been touted as a way to increase access to health services for a number of populations, it may be challenging for children and youth with DD who receive treatment from therapists (20). Therefore, it is important that service providers recognize that children and youth with DD may not benefit from virtual services, and it is important that steps be taken to ensure that their access to in-person care is safeguarded, redefining these services as “essential” (21).
In addition to losing services, families reported worsening financial status in our study. Other studies have also shown that in the current pandemic, food insecurity has worsened due to a number of factors, including loss of income, lack of low-cost food supply, and public health messaging to self-isolate and stay home, disproportionately affecting FCDD (22). All of these factors can lead to increased familial and caregiver stress. Caregiver stress profoundly impacts children’s development (23,24) and is associated with decreased efficacy of behavioural interventions for children with DD (24). Caregiver stress may lead to children’s difficulty with emotion regulation and social skills (23). Moreover, caregiver stress can manifest as worsening mental health, a known adverse childhood experience, and yet another downstream impact of the COVID-19 pandemic (25). The impact of adverse childhood experiences (ACEs) and toxic stress on the developing brain is well known to be deleterious, and the impact is even more magnified in children with DD. Mitigating these factors is therefore not only important for the family unit, but for the health and well-being of children long-term.
Our study findings suggest that the impact of the pandemic had cascading effects on the development, family functioning, and quality of life for FCDD (Figure 1). While public policies had to be developed rapidly throughout the pandemic to contain the spread of COVID-19, they may have indirectly contributed to fewer services and increased stress for FCDD, impacting their quality of life. It is our intent to use these findings to build a community intervention that centres on the specific needs of the families of these children with DD. While this paper highlights experiences throughout the COVID-19 pandemic, children with DD have been commonly isolated, neglected, and excluded from responses in other humanitarian crises, which has repeated itself throughout history (26). Families who are impacted by these policy decisions often do not have a seat at the table to help develop inclusive public health strategies (10). Health providers and policymakers alike must include FCDD in decision making, particularly when considering how to ensure their safety and well-being (27).
Limitations
There are some limitations to our study. First, caregivers were all recruited from one institutional site, an urban, inner-city setting. While they and their children all lived and accessed programs in different areas of the city, their views may be different from other caregivers of children who access care in different settings. Second, while our sample size was appropriate for phenomenological studies and reached data saturation, our findings may not be generalizable in other contexts. Thirdly, we only have included a subset of illustrative quotes for primary themes which are most descriptive of the theme but do not include quotes from every interview. Fourth, the experiences captured in this study occurred early in the COVID-19 pandemic. Experiences may have shifted as the pandemic has evolved, and future research should seek to better understand the short- and long-term trajectory that the pandemic changes have had on the lives of FCDD. Lastly, the identities and lived experiences of the research team are important to acknowledge as they may have influenced the interview experience.
CONCLUSION
The pandemic has impacted FCDD in multiple areas, including behaviour, development, financial security, and overall well-being. Our study findings suggest that the impact of the early phases of the pandemic has had cascading effects on family functioning and quality of life for children with DD and their families, which may remain for years to come. To deliver truly patient-centred services for FCDD, there is an urgent need for responsive programming that is co-developed with caregivers and providers. Future research should explore potential solutions to the many barriers experienced by families during pandemic/crisis settings.
Supplementary Material
Contributor Information
Tali Filler, Women and Children’s Health Program, St. Michael’s Hospital, Unity Health Toronto, Toronto, Ontario, Canada; Temerty Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada.
Pardeep Kaur Benipal, Women and Children’s Health Program, St. Michael’s Hospital, Unity Health Toronto, Toronto, Ontario, Canada.
Ripudaman Singh Minhas, Women and Children’s Health Program, St. Michael’s Hospital, Unity Health Toronto, Toronto, Ontario, Canada; Department of Pediatrics, Temerty Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada; Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, Ontario, Canada.
Shazeen Suleman, Women and Children’s Health Program, St. Michael’s Hospital, Unity Health Toronto, Toronto, Ontario, Canada; Department of Pediatrics, Temerty Faculty of Medicine, University of Toronto, Toronto, Ontario, Canada; Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, Ontario, Canada; MAP Centre for Urban Health Solutions, St. Michael's Hospital, Unity Health Toronto, Toronto, ON, Canada.
FUNDING
This work was supported by St. Michael’s Hospital Association Innovation Fund [SMH 21-008].
POTENTIAL CONFLICTS OF INTEREST
S.S. is a member of this journal’s editorial board. She was not involved in the editing or review of this manuscript. There are no other disclosures. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
REFERENCES
- 1. Berrigan P, Scott CWM, Zwicker JD.. Employment, education, and income for Canadians with developmental disability: Analysis from the 2017 Canadian Survey on Disability. J Autism Dev Disord 2020. doi: 10.1007/s10803-020-04603-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Majenemer A, McGrath PJ, Bambusch J, et al. Time to be counted: COVID-19 and intellectual and developmental disabilities. Royal Society of Canada. 1 June 2021. https://rsc-src.ca/en/covid-19-policy-briefing/time-to-be-counted-covid-19-and-intellectual-and-developmental-disabilities
- 3. Rollins M, Milone F, Suleman S, Vojvoda D, Sgro M, Barozzino T.. Patient navigators: Mapping the route toward accessibility in health care. Paediatr Child Health 2019;24:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Young E, Milligan K, Henze M, Johnson S, Weyman K.. Caregiver burnout, gaps in care, and COVID-19: Effects on families of youth with autism and intellectual disability. Can Fam Physician 2021;67:506–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fontanesi L, Marchetti D, Mazza C, Di Giandomenico S, Roma P, Verrocchio MC.. The effect of the COVID-19 lockdown on parents: A call to adopt urgent measures. Psychol Trauma 2020;12:S79–81. [DOI] [PubMed] [Google Scholar]
- 6. McAdams Ducy E, Stough LM.. Exploring the support role of special education teachers after Hurricane Ike: Children with significant disabilities. J Fam Issues 2011;32:1325–45. [Google Scholar]
- 7. Bussières EL, Malboeuf-Hurtubise C, Meilleur A, et al. . Consequences of the COVID-19 pandemic on children’s mental health: A meta-analysis. Front Psychiatry 2021;12:691659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jenkins EK, McAuliffe C, Hirani S, et al. . A portrait of the early and differential mental health impacts of the COVID-19 pandemic in Canada: Findings from the first wave of a nationally representative cross-sectional survey. Prev Med 2021;145:106333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fegert JM, Vitiello B, Plener PL, Clemens V.. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health 2020;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vanderbom KA, Eisenberg Y, Tubbs AH, Washington T, Martínez AX, Rauworth A.. Changing the paradigm in public health and disability through a knowledge translation center. Int J Environ Res Public Health 2018;15:328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches, 3rd edn. Thousand Oaks, CA: Sage Publications, 2009. [Google Scholar]
- 12. Iwamoto DK, Negi NJ, Partiali RN, Creswell JW.. The racial and ethnic identity formation process of second-generation Asian Indian Americans: A phenomenological study. J Multicult Couns Devel 2013;41:224–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McHugh ML. Interrater reliability: The kappa statistic. Biochem Med 2012;22:276–82. [PMC free article] [PubMed] [Google Scholar]
- 14. SocioCultural Research Consultants, LLC. Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data. Los Angeles, CA: SocioCultural Research Consultants, LLC. 2018. Available from: www.dedoose.com [Google Scholar]
- 15. Vasileiou K, Barnett J, Thorpe S, Young T.. Characterising and justifying sample size sufficiency in interview-based studies: Systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 2018;18:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 17. Tong A, Sainsbury P, Craig J.. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. [DOI] [PubMed] [Google Scholar]
- 18. Statistics Canada. Table 11-10-0241-01. Low income cut-offs (LICOs) before and after tax by community size and family size, in current dollars [Internet]. 2022. Available from: 10.25318/1110024101-eng [DOI]
- 19. Warner M, Lloyd CM.. Considerations for building post-COVID early care and education systems that serve children with disabilities: Child trends; 2020. 2022. https://www.childtrends.org/publications/considerations-for-building-post-covid-early-care-and-education-systems-that-serve-children-with-disabilities (Accessed August 15, 2022).
- 20. Aishworiya R, Kang YQ.. Including children with developmental disabilities in the equation during this COVID-19 pandemic. J Autism Dev Disord 2021;51:2155–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Suleman S, Ratnani Y, Stockley K, et al. . Supporting children and youth during the COVID-19 pandemic and beyond: A rights-centred approach. Paediatr Child Health 2020;25:333–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Loopstra R. Vulnerability to Food Insecurity since the COVID-19 Lockdown. The Food Foundation, 2020. https://foodfoundation.org.uk/publication/vulnerability-food-insecurity-covid-19-lockdown> [Google Scholar]
- 23. Crnic KA, Neece CL, McIntyre LL, Blacher J, Baker BL.. Intellectual disability and developmental risk: Promoting intervention to improve child and family well-being. Child Dev 2017;88:436–45. [DOI] [PubMed] [Google Scholar]
- 24. Osborne LA, McHugh L, Saunders J, Reed P.. Parenting stress reduces the effectiveness of early teaching interventions for autistic spectrum disorders. J Autism Dev Disord 2008;38:1092–103. [DOI] [PubMed] [Google Scholar]
- 25. Calvano C, Engelke L, Di Bella J, Kindermann J, Renneberg B, Winter SM.. Families in the COVID-19 pandemic: Parental stress, parent mental health and the occurrence of adverse childhood experiences—Results of a representative survey in Germany. Eur Child Adolesc Psychiatry 2022;31:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. UNICEF. The state of the world's children 2013: Children with Disabilities. November 2013. https://www.unicef.org/reports/state-worlds-children-2013 (Accessed August 15, 2022). [Google Scholar]
- 27. Ronoh S, Gaillard J, Marlowe J.. Children with disabilities in disability-inclusive disaster risk reduction: Focussing on school settings. Policy Futures Educ 2017;15:380–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.