Abstract
Objective
Due to the COVID-19 pandemic, burnout among healthcare workers has significantly increased. This study evaluated rates of burnout in neuropsychologists one year into the COVID-19 pandemic.
Method
A survey invitation was sent across five neuropsychology-related listservs in April 2021. Burnout was assessed with the Copenhagen Burnout Inventory (CBI; Kristensen, T. S., Borritz, M., Villadsen, E., & Christensen, K. B. (2005). The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress, 19 (3), 192–207) and differences in Personal, Work, and Client burnout scores were evaluated across patient population and work setting.
Results
57.3% and 51.5% of respondents (N = 130) endorsed moderate-to-high levels of personal and work-related burnout, respectively. In the Personal domain, respondents working with pediatric patients had higher mean scores and a higher proportion of respondents endorsed moderate-to-high levels of burnout.
Conclusion
More than half of the survey respondents endorsed elevated levels of personal and work-related burnout. This is concerning as burnout is associated with personal challenges and diminished patient care. Potential organizational interventions are discussed.
Keywords: COVID-19, Burnout, Clinical practice, Neuropsychologists
Burnt Out: Rate of Burnout in Neuropsychology Survey Respondents During the COVID-19 Pandemic
“By far, this has been the most physically and mentally exhausting year of my entire career I am without a doubt experiencing burn out. Pressing pause is very difficult because of the high demand for services. I am currently planning a leave of absence due to burn out.” Survey Respondent, 2021.
First described in the 1970s, burnout is a well-described concept and a syndrome now recognized by the World Health Organization (WHO) (Freudenberger, 1974; Maslach, 1976; World Health Organization, 2020). Burnout, which results from chronic, unmanaged workplace stress, is characterized by exhaustion, mental and emotional distancing from one’s job, and a reduction in work-place efficacy (WHO, 2020). Though conceptualized as an “occupational phenomenon” by the WHO, burnout is associated with adverse physical (e.g., pain, sleep disorders), emotional (e.g., depression, increased alcohol consumption), and cognitive (e.g., executive functioning, attention, memory) difficulties that affect individuals outside of the workplace (Azam, Khan, & Alam, 2017; Deligkaris, Panagopoulou, Montgomery, & Masoura, 2014).
Burnout is world-wide phenomena, ubiquitous across occupational settings (Golembiewski, Boudreau, Sun, & Luo, 1998; Maslach, Schaufeli, & Leiter, 2001). The COVID-19 pandemic has resulted in an increase in burnout, especially among healthcare workers who face concerns of work-related infection, increased work demands, and shortages of personal protective equipment (Denning et al., 2021). For example, a large multi-national study that included 3537 healthcare workers found that 67% of respondents screened positive for burnout, with anxiety and depression as top predictors of burnout (Denning et al., 2021). To date, most studies evaluating burnout during the COVID-19 pandemic have focused on medical doctors, nursing staff, and midwives. While studies have documented emotional concerns and distress among neuropsychologists during the early stages of the pandemic (e.g., Zane, Thaler, Reilly, Mahoney, & Scarisbrick, 2021), no study has specifically evaluated burnout in neuropsychologists. The pandemic has brought about unique challenges by forcing neuropsychologists to determine which aspects of their services are urgent, critical, and feasible in virtual or in-person environments while considering the varying levels of cognitive impairment and technology proficiency among their patients (e.g., Marra, Hoelzle, Davis, & Schwartz, 2020). Elucidating burnout rates amongst neuropsychologists can inform institutional efforts to better support clinicians as they provide critically important patient care.
Materials and Methods
The present survey study was approved by institutional review board and completed in accordance with the Helsinki Declaration. On April 20th, 2021, an electronic invitation to complete a survey assessing changes in clinical practice due to the COVID-19 pandemic was distributed across neuropsychology member organizations listservs. Specifically, the sampling frame included the member listservs: AACN Boarded, AACN Community, AACN Peds Interest, and NPSYCHPEDNPSY. The population of interest was any independent and licensed clinician providing neuropsychological services. No follow-up emails or reminders to complete the survey were disseminated. All responses were anonymous. Survey respondents completed a Qualtrics survey that contained 60 multiple-choice and free-response questions assessing current clinical practices in neuropsychology (data not reported in this paper) and an additional survey assessing burnout.
The Copenhagen Burnout Inventory (CBI; Kristensen, Borritz, Vlladsen, & Christensen, 2005) is a 19-item survey used to assess burnout. This survey was developed to overcome criticisms of the widely used Maslach Burnout Inventory and is in the public domain (https://nfa.dk/-/media/NFA/Vaerktojer/Spoergeskemaer/CBI/CBI-scales.ashx?la=da). The CBI assesses burnout across three domains: personal burnout, work-related burnout, and client-related burnout. The Personal burnout domain consists of six items that assess both physical and psychological fatigue (e.g., How often do you feel tired? How often do you feel emotionally exhausted?). The Work burnout domain consists of seven items that assess fatigue related to work (e.g., Are you exhausted in the morning at the thought of another day at work? Does your work frustrate you?). Lastly, the Client burnout domain consists of six items that assess fatigue related to working with clients/patients (e.g., Does it drain your energy to work with clients? Do you sometimes wonder how long you will be able to work with clients?).
Respondents report how often they experience each burnout symptom (e.g., “always,” “often,” “sometimes,” “seldom”, “almost never”). Each response is transformed into a numerical value (i.e., 0, 25, 50, 75, 100), with higher values indicating more burnout. The scores for every question within each domain are averaged together to create a total domain score. Norms are derived from initial studies of individuals in the health and human service industry (e.g., doctors, nurses, social workers) in Copenhagen and a total domain score of 50 points or higher is considered a moderate-to-high degree of burnout (Kristensen et al., 2005). All responses were optional, and a respondent could skip any question. Respondents could also provide additional comments at the end of the survey.
The CBI has high internal consistency (Cronbach’s alpha .85–.87), has been translated into multiple languages, and is used in studies across the world (see Kristensen et al., 2005). Notably, initial standardization of the CBI had survey questions embedded among other questions not assessing burnout. For transparency and to reduce the amount of time respondents spent completing the questionnaire, all questions of the survey were presented with no additional items and the questionnaire was labeled as an instrument to evaluate burnout. This methodological decision may have introduced bias, potentially leading respondents to under or overreport their actual level of burnout.
A 2 × 3 between-group multivariate analysis of variance (MANOVA) was performed on three dependent variables: Personal, Work, and Client Burnout. Independent variables were patient populations (adult, pediatric, both) and work settings (private practice/university, hospital/medical center, VA/government/prisons). Chi-square analyses examined the proportion of respondents who endorsed high degree of burnout based on the patient population and work setting stratifications.
Results
A total of 131 respondents completed the CBI. One respondent completed the domain evaluating Personal burnout but did not complete the remaining 13 questions. This respondent was dropped from subsequent analyses. There were no other nonresponders (i.e., not answering three or more questions per scale) or missing data. Internal consistency for the domain of personal burnout was excellent (Cronbach’s alpha = 0.91), work domain was acceptable (Cronbach’s alpha = 0.79), and client domain was good (Cronbach’s alpha = 0.88).
Most of the survey respondents (n = 25, 95.4%) indicated that their clinical practice was in the United States and a small minority (n = 6, 4.6%) practiced in Canada. Of the respondents from the United States, n = 39 (29.8%) practiced in the Northeast, n = 28 (21.4%) practiced in the Southeast, n = 34 (26%) practiced in the Midwest, n = 19 (14.5%) practiced in the West, and n = 5 (3.8%) practiced in the Southwest.
Of the respondents, n = 31 (23.7%) worked primarily with pediatric patients, n = 73 (55.7%) worked primarily with adult patients, and n = 27 (20.6%) reported working with both patient populations. Most respondents worked in a hospital/medical center (n = 67, 51%) or a private practice/University setting (n = 49, n = 37.4%). A smaller percentage of respondents worked in a VA, government, or prison setting (n = 13, 9.92%) or listed their primary work setting as “other” (n = 2, 1.5%). Due to the small cell sizes, the latter two groups were merged for further analyses.1
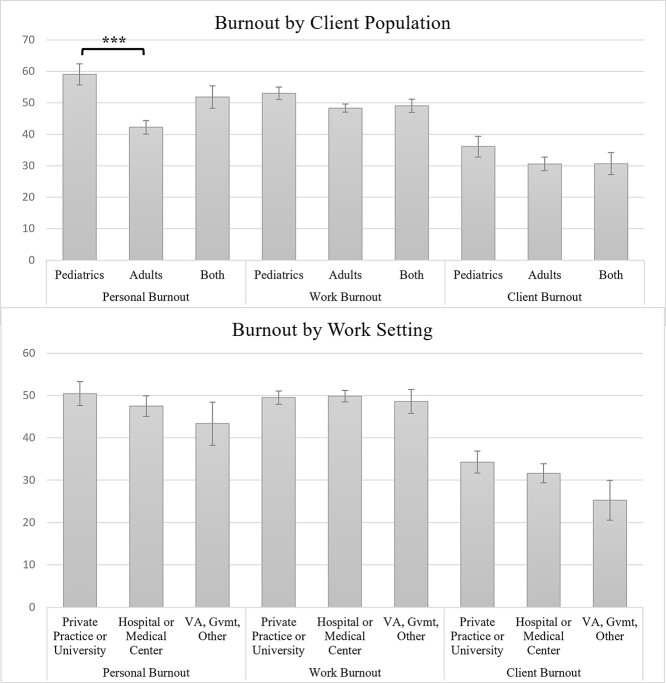
The interaction of the 2 × 3 (Patient Population × Work Setting) MANOVA failed to reach significance (F(9, 292.20) = 1.40, p = .187; Wilk’s Λ = .902, partial η2 = .034). The main effect for mean Burnout scores based on work setting (i.e., private practice/university, hospital/medical center, VA/government/prisons) failed to reach significance (F(6, 240) = 0.472, p = .829; Wilk’s Λ = .977, partial η2 = .012). The main effect for self-reported Burnout scores across patient population (Pediatric, Adult, Both) was significant (F(6, 240) = 3.32, p = .004; Wilk’s Λ = .853, partial η2 = .077). Univariate analyses showed that group differences across patient population were seen for the domain of Personal burnout (F(2, 122) =7.464, p < .001, partial η2 = .109), but not Work or Client burnout (p’s < .05). Bonferroni post-hoc analyses indicated that respondents who worked primarily with pediatric populations endorsed higher Personal Burnout than respondents who worked with adult populations (p < .001). See Table 1 and Figure 1 for marginal means and univariate analyses.
Table 1.
Burnout in neuropsychologists
| Overall | Pediatric | Adult | Both | Test Parameter | Private Practice, University | Hospital, Medical Center | VA, Gvmt, Other | Test Parameter | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n | 130 | 30 | 73 | 27 | 49 | 66 | 15 | |||
| Mean (Std. Dev.) |
Personal | 48.11 (19.66) | 59.03 (17.30) | 42.24 (19.03) + | 51.85 (18.25) | F(2,122) = 7.46*** | 50.42 (20.10) | 47.45 (20.41) | 43.33 (13.06) | F(2,122) = 0.76 |
| Work | 49.57 (10.92) | 53.03 (9.83) | 48.34 (10.73) | 49.07 (12.14) | F(2, 122) = 2.01 | 49.49 (11.32) | 49.86 (11.04) | 48.60 (9.69) | F(2, 122) = 0.08 | |
| Client | 31.89 (18.23) | 36.11 (18.61) | 30.59 (17.36) | 30.71 (20.05) | F(2, 122) = 1.03 | 34.27 (19.25) | 31.63 (18.00) | 25.28 (14.90) | F(2, 122) = 0.57 | |
| % High Burnout | Personal | 57.7 | 76.7 | 46.58 | 66.67 | ꭓ2(2) = 9.01* | 63.27 | 58.21 | 33.3 | ꭓ2(2) = 4.23 |
| Work | 51.5 | 70.00 | 46.58 | 44.44 | ꭓ2(2) = 5.36 | 46.94 | 53.03 | 60.00 | ꭓ2(2) = 0.90 | |
| Client | 18.5 | 23.33 | 17.81 | 14.81 | ꭓ2(2) = 0.732 | 20.41 | 19.70 | 6.70 | ꭓ2(2) = 1.58 |
Note: * = p < .05, ** = p < .01, *** = p < .001; + = significant differences between groups after Bonferroni post-hoc analyses.
VA = Veterans Administration; Gvmt = Government.
Fig. 1.
Burnout in clinical neuropsychologists.Note: * = p < .05, ** = p < .01, *** = p < .001; . = significant differences between groups after Bonferroni post-hoc analyses. CBI = Copenhagen Burnout Inventory; VA = Veterans Administration; Gvmt = Government
Across the whole sample, more than half of respondents endorsed a high degree of Personal burnout (57.7%) and Work burnout (51.8%) (see Table 1). Fewer respondents endorsed a high degree of Client burnout (18.5%). Mirroring the analyses above, the proportion of respondents indicating a high degree of burnout was largely independent of patient population and work setting. Only respondents working with pediatric populations endorsed a high degree of Personal burnout at a higher proportion (76.7%) than respondents working with adult populations (46.58%) (ꭓ2(2) = 9.01, p = .011).
Discussion
The present study evaluated burnout in a convenience sample of neuropsychologists one year into the COVID-19 pandemic. A majority of respondents reported a moderate-to-high degree of Personal (57.3%) and Work (51.5%) burnout. These findings extend emerging research that has documented a high degree of burnout in other healthcare workers during the COVID-19 pandemic (e.g., Denning et al., 2021; Jalili, Niroomand, Hadayand, Zeinlani, & Foutouhi, 2021).
In this study, burnout was largely independent of patient population and work setting. Interestingly, the only consistent difference was that respondents who worked primarily with pediatric populations endorsed a higher degree of Personal burnout compared with respondents who worked primarily with adult populations. This finding may be an exacerbation of prepandemic difficulties for pediatric specialist (Sweet, Benson, Nelson, & Moberg, 2015). For example, in their professional practice survey, Sweet et al. (2015) found that 81% of pediatric neuropsychologists indicated that establishing and maintaining a family life was a significant obstacle to job satisfaction. Another possibility is that pediatric neuropsychologists are much more likely to be women (Sweet et al., 2015), and the COVID-19 pandemic has disproportionately affected women in the workforce. For example, women were much more likely to be the sole providers of childcare as schools were shut down, and women were more likely to report reducing their working hours to provide childcare (Zamaro, Perez-Arce, & Prados, 2020). This is exemplified by one respondent who qualified their survey responses by stating, “Fatigue questions sometimes related to toddler at home and competing demands of family and work.” This, among other burdens that disproportionately affected women (e.g., higher job loss, less work output; Zamaro et al., 2020), may have led to higher Personal burnout. However, demographic information from study participants weas not collected; thus, the gender hypothesis could not be tested.
The high rate of significant burnout reported by neuropsychologists is concerning given the adverse physical, affective, and cognitive difficulties associated with burnout (Azam et al., 2017; Deligkaris et al., 2014). As found in prior research related to COVID-19 burnout in other professions, the high rate of work-related burnout found in this sample (51.5%) may be related to concerns for risk of exposure, lack of proper training and personal protective equipment, and financial instability (Sasangohar, Jones, Masud, Vahidy, & Kash, 2020). Related, our prior research found that nearly 90% of neuropsychologists in private practice reporting reduced work or pay in the early stages of the pandemic, and nearly a third of respondents reported ethical concerns due to organizational pressure or poor organizational communication (Citation Removed to Maintain Anonymity, 2020). Numerous survey respondents added comments to the survey indicating work-related concern, such as, “It is not burnout from the actual clients - it is the organization/management that has been awful throughout the pandemic with no concern for clinician wellbeing and constantly pushing for more work with less reimbursement/pay” and “Much of my burn out (sic) has more to do with running a small group practice at this time- having to figure all of this out and take care of everyone and being overwhelmed with referrals and unable to find sufficient help in the form of hiring additional neuropsychologists.”
Encouragingly, less than 20% of respondents reported significant client-related burnout. Nonetheless, burnout, in general, is associated with decreased patient care, decreased patient satisfaction, and increased likelihood for medical error (De Hert, 2020). Thus, to protect patients and clinicians, addressing the widespread burnout of neuropsychologists should be a priority for institutional organizations and affiliated leadership. A recent meta-analysis found that institutionally based interventions were associated with a moderate reduction in burnout scores (De Simone, Vargas, & Servillo, 2021). Effective organizational factors to reduce burnout include improving work schedules, promoting self-management, teaching self-care, and mindfulness-based stress control activities. Providing counseling, support systems, and support meetings for COVID treatment teams have also been effective (Sharifi, Asadi-Pooya, & Mousavi-Roknabadi, 2021). Reviewing these interventions and its applicability to neuropsychologists is beyond the scope of this paper but should be further investigated.
Limitations
This study has a few notable limitations. First, there is no published data on the number of individuals who are members of the listservs nor is there information on the number of individuals who subscribe to multiple listservs. Therefore, an accurate response rate could not be calculated, and the “true” prevalence rate of burnout cannot be established. Rather, the results are best conceptualized as a “snapshot” of burnout in a convenience sample of neuropsychologists. Furthermore, in an effort to maintain respondents’ anonymity, pertinent demographic variables such as gender, race, and number of years in clinical practice were not collected. As such, the generalizability of our findings is unclear and hypothesis testing on predictors of burnout was not feasible. The anonymity of survey respondents also meant that we could not confirm respondents’ credentials as licensed practitioners or ensure that multiple responses were not made, though it seems unlikely that inappropriate survey responses would occur at a rate that would meaningfully alter our findings. In addition, the nonstandard nature of CBI administration (i.e., not interspersing non-CBI questions) may have led to stereotyped responding or over/underreporting of burnout symptoms. For example, the relatively low rate of client-related burnout may be due to respondents not wanting to acknowledge feeling tired/frustrated working with their patients, though this cannot be confirmed. Finally, respondents who were experiencing burnout may have been more likely to participate in this survey, potentially inflating the rates of significant burnout.
Since this study is cross-sectional and there has been no prior research on burnout in neuropsychologists, we cannot know the extent to which the COVID-19 pandemic has contributed to the rates of burnout in this population. However, a recent meta-analysis estimated the prevalence of emotional exhaustion (an aspect of burnout) to be 40% among mental health practitioners (O’Connor, Neff, & Pitman, 2018). While it cannot be tested from the present data, this may suggest a slight increase in burnout as more than half of the respondents endorsed moderate-to-high levels of personal and work-related burnout.
Future Directions
As new variants of the SARS-CoV-2 virus emerge and societal responses to the virus evolves, continued monitoring and follow-up studies assessing burnout in neuropsychologists is needed. Particularly, future research should prospectively follow neuropsychologists over time to evaluate changes in burnout and well-being. Future research should seek to identify how psychological aspects (e.g., depression/anxiety; Denning et al., 2021), personal circumstances (e.g., simultaneously working remotely and caring for children; Kerr, Fanning, Huynh, Botto, & Kim, 2021), gender differences (e.g., rates of job loss and caregiving responsibility; Viglione, 2020; Zamarro, Perez-Arce, & Prados, 2020), and environmental circumstances (e.g., lack of PPE or institutional support; Denning et al., 2021) interact to increase risk of burnout in neuropsychologist. More importantly, the efficacy of intervention for burnout should be formally evaluated.
Conflict of Interest
There are no conflicts of interest to report.
Footnotes
The pattern of results did not differ when the “Other” respondents were considered separately, combined, or omitted from analyses.
Contributor Information
David E C Marra, Department of Psychology, VA Boston Healthcare System, Boston, MA, USA; Department of Psychiatry, Boston University School of Medicine, Boston, MA, USA.
Mary U Simons, Department of Psychology, Marquette University, Milwaukee, WI, USA.
Eben S Schwartz, Department of Neurology, University of Wisconsin School of Medicine and Public Health, Madison, WI, USA.
Elizabeth A Marston, AMITA Health Neurosciences Institute, Chicago, IL, USA.
James B Hoelzle, Department of Psychology, Marquette University, Milwaukee, WI, USA.
Funding
There are no funding sources for this study.
References
- Azam, K., Khan, A., & Alam, M. T. (2017). Causes and adverse impact of physician burnout: a systematic review. Journal of the College of Physicians and Surgeons–Pakistan, 27(8), 495–501. https://doi.org/2678. [PubMed] [Google Scholar]
- De Hert, S. (2020). Burnout in healthcare workers: prevalence, impact and preventative strategies. Local and Regional Anesthesia, 13, 171–183. 10.2147/LRA.S240564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Simone, S., Vargas, M., & Servillo, G. (2021). Organizational strategies to reduce physician burnout: a systematic review and meta-analysis. Aging Clinical and Experimental Research, 33(4), 883–894. 10.1007/s40520-019-01368-3. [DOI] [PubMed] [Google Scholar]
- Deligkaris, P., Panagopoulou, E., Montgomery, A. J., & Masoura, E. (2014). Job burnout and cognitive functioning: a systematic review. Work & Stress, 28(2), 107–123. [Google Scholar]
- Denning, M., Goh, E. T., Tan, B., Kanneganti, A., Almonte, M., Scott, A. et al. (2021). Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS One, 16(4), e0238666. 10.1371/journal.pone.0238666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenberger, H. J. (1974). Staff burn-out. Journal of Social Issues, 30(1), 159–165. 10.1111/j.1540-4560.1974.tb00706.x. [DOI] [Google Scholar]
- Golembiewski, R. T., Boudreau, R. A., Sun, B. C., & Luo, H. (1998). Estimates of burnout in public agencies: worldwide, how many employees have which degrees of burnout, and with what consequences? Public Administration Review, 58, 59–65. 10.2307/976890. [DOI] [Google Scholar]
- Jalili, M., Niroomand, M., Hadavand, F., Zeinali, K., & Fotouhi, A. (2021). Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. International Archives of Occupational and Environmental Health, 94, 1345–1352. 10.1007/s00420-021-01695-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr, M. L., Fanning, K. A., Huynh, T., Botto, I., & Kim, C. N. (2021). Parents' self-reported psychological impacts of COVID-19: Associations with parental burnout, child behavior, and income. Journal of Pediatric Psychology, 46(10), 1162–1171. 10.1093/jpepsy/jsab089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen, T. S., Borritz, M., Villadsen, E., & Christensen, K. B. (2005). The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress, 19(3), 192–207. 10.1080/02678370500297720. [DOI] [Google Scholar]
- Marra, D. E., Hoelzle, J. B., Davis, J. J., & Schwartz, E. S. (2020). Initial changes in neuropsychologists clinical practice during the COVID-19 pandemic: a survey study. The Clinical Neuropsychologist, 34(7–8), 1251–1266. 10.1080/13854046.2020.1800098. [DOI] [PubMed] [Google Scholar]
- Maslach, C. (1976). Burned-out. Human Behavior, 5, 16–22. [Google Scholar]
- Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52(1), 397–422. 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- O’Connor, K., Neff, D. M., & Pitman, S. (2018). Burnout in mental health professionals: A systematic review and meta-analysis of prevalence and determinants. European Psychiatry, 53, 74–99. 10.1016/j.eurpsy.2018.06.003. [DOI] [PubMed] [Google Scholar]
- Sasangohar, F., Jones, S. L., Masud, F. N., Vahidy, F. S., & Kash, B. A. (2020). Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesthesia and Analgesia, 131(1), 106–111. 10.1213/ANE.0000000000004866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi, M., Asadi-Pooya, A. A., & Mousavi-Roknabadi, R. S. (2021). Burnout among healthcare providers of COVID-19; a systematic review of epidemiology and recommendations. Archives of Academic Emergency Medicine, 9(1), e7. 10.22037/aaem.v9i1.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet, J. J., Benson, L. M., Nelson, N. W., & Moberg, P. J. (2015). The American Academy of Clinical Neuropsychology, National Academy of Neuropsychology, and Society for Clinical Neuropsychology (APA Division 40) 2015 TCN Professional Practice and ‘Salary Survey’: Professional Practices, Beliefs, and Incomes of U.S. Neuropsychologists. The Clinical Neuropsychologist, 29(8), 1069–1162. 10.1080/13854046.2016.1140228. [DOI] [PubMed] [Google Scholar]
- Viglione, G. (2020). Are women publishing less during the pandemic? Here's what the data say. Nature, 581(7809), 365–366. 10.1038/d41586-020-01294-9. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020). International statistical classification of diseases and related health problems (11th ed.). https://icd.who.int/
- Zamarro, G., Perez-Arce, F., & Prados, M. J. (2020). Gender differences in the impact of COVID-19. Working Paper. Switzerland: Frontiers in Public Health. Retrieved from https://tinyurl.com/CESRGenderDiffs. [Google Scholar]
- Zane, K. L., Thaler, N. S., Reilly, S. E., Mahoney, J. J., III, & Scarisbrick, D. M. (2021). Neuropsychologists’ practice adjustments: The impact of COVID-19. The Clinical Neuropsychologist, 35(3), 490–517. 10.1080/13854046.2020.1863473. [DOI] [PMC free article] [PubMed] [Google Scholar]