Abstract
Background and aims
Play is used by practitioners from across disciplinary backgrounds as a natural and enjoyable context for providing intervention and support in early childhood. In the case of autism interventions, many therapies are based on the association between social play and the development of social skills, language development, and communication skills, as these are often particular areas of challenge for autistic children. However, play is a wide-ranging concept and the extant literature on play-based interventions is large and heterogeneous. This means it is challenging for practitioners and families to navigate the evidence base and make choices about differing intervention strategies. This review aims to provide a comprehensive map of the research on this topic and to develop a conceptual framework to inform clinical decision-making.
Methods
An initial stakeholder consultation confirmed the relevance of the topic to practitioners and autistic people. A scoping review methodology (preregistered) was used to identify relevant literature. We systematically searched seven databases to find peer-reviewed primary intervention studies of play-based approaches targeting language, social and communication outcomes for autistic children aged 2-8 years. We then summarised the literature using narrative synthesis and Evidence Gap Maps (EGMs). The literature was summarised according to a range of characteristics, including study design, population characteristics, agent of intervention and outcomes measured, among others. These summaries were then used to develop a framework for some key considerations for practitioners appraising play-based approaches.
Results
388 studies met inclusion criteria. Approximately 21% of studies were RCTs, and over 50% had ≤10 participants. Over 45% of studies reported multiple relevant outcomes, with social play skills being the most common single intervention target. Girls and minority background groups are under-represented. A range of intervention types were identified, and some high-level categorisations are proposed.
Main contribution: On the basis of the evidence synthesis we suggest important dimensions for appraisal of play-based interventions, including the role of play within an intervention (as a context, a key developmental mechanism, or a component of a larger approach), the underpinning philosophy (e.g. behaviourist or developmental), and the role of the practitioner (providing parent feedback, 1:1 intervention, group facilitation).
Conclusions
The wide range of approaches uncovered by this review is a testament to the wonderful diversity inherent to both play and autism. However, research could usefully focus on consolidating the evidence base for existing approaches, rather than aiming for further diversification.
Implications: The conceptual framework proposed in this review can help practitioners appraise the literature and aid their advice to families when making shared intervention decisions.
Keywords: Autism, play, intervention, language & communication
Introduction
There is increasing research and clinical interest in the role of play in children’s linguistic and social development (Gibson, Fink, et al., 2020; O’Connor & Stagnitti, 2011; Stagnitti et al., 2016; Toseeb et al., 2020). For typically developing children, it is well-documented that early pretend play appears around the end of first year of life, coinciding with the emergence of first words (Quinn et al., 2018; Toth et al., 2006). Other aspects of playful interactions have also been related to broader social competences known to support communicative development, such as joint attention, reciprocal initiations, imitation, and, the giving and reading of nonverbal cues (Godin et al., 2019a; Radley et al., 2014).
Play is often characterised as activities or behaviours that are non-literal, voluntary and fun or rewarding (Miller, 2017). Play takes on a wide range of forms, such as pretence, physical play, sports and digital play and has also been conceptualised as a dispositional trait or stage, i.e. ‘playfulness’ (Bundy, 2012; Fink et al., 2020; Skard & Bundy, 2008) or ‘playful engagement’ (Godin et al., 2019a). Children with autism spectrum disorder (ASD) show broad differences in the frequency and nature of play behaviours compared to children with typical development or with other cognitive or developmental conditions (Boutot et al., 2005; Francis et al., 2019). Autistic children’s play may be characterised by the presence of repetitive behaviours (Wing et al., 1977) and they may show qualitative differences in imaginative or pretend play relative to other children (Jarrold, 2003). Furthermore, as social and communication difficulties form part of the core diagnostic criteria for ASD (American Psychiatric Association, 2013), it is not surprising that differences in social play have been documented in this population and have been used to inform diagnostic assessments (Gibson et al., 2011; Lord et al., 2000).
The social and communication difficulties experienced by autistic children are associated with a range of negative outcomes including various aspects of daily or adaptive functioning and mood disorder symptomatology (Chang et al., 2012; Rai et al., 2018). Long-term impacts of these difficulties include poorer adaptive and social functioning (e.g. friendships (Magiati et al., 2014) and depression into adulthood (Rai et al., 2018)). Therefore, interventions targeting the development of such skills are considered a priority by autistic individuals and their families (Autistica, n.d.).
The significance of play in the development of communication and social skills, coupled with its inherent ‘enjoyableness’ as a mode of learning in childhood, has inspired practitioners to develop a range of play-based interventions to foster these skills in autistic children. The research on these play-based interventions, however, varies greatly. Differences are found in underpinning philosophies, modes of delivery and conceptualisations of play, as well as in the designs used to assess their effectiveness. Some approaches take a more instrumental approach, e.g. using a game as a vehicle to learn and practice pragmatic communication skills (Murphy et al., 2019), while others emphasise following a child’s voluntary play interests.
The extent of heterogeneity makes navigating this burgeoning field a challenge from many perspectives, from that of the clinician or family wanting to choose an intervention that is right for a particular child, to the researcher hoping to learn more about the nature of the relations between play and communication in autistic children. The present scoping review aims to address this issue by providing an accessible and comprehensive overview of research on this topic and suggesting new conceptual dimensions that could be used in future appraisal of play-based interventions that target social and communication outcomes.
Reviews of play-based interventions
Before outlining the methodology used in the current review, we highlight some relevant reviews identified during our preliminary literature searches. Broadly, reviews of play-based interventions for improving social communication skills in autism can be divided into those that focus on improving social play skills in their own right, and those that use playful methods to target other social outcomes.
Kuhaneck and colleagues (Kuhaneck et al., 2020) conducted a systematic review of Occupational Therapy interventions and examined which therapeutic strategies were more effective in improving play skills. The authors found evidence supporting a range of strategies including environmental modification and adult-led imitation. Although the authors acknowledge the variety of play behaviours and meaning, the approach is mainly focused on improving play skills in-line with typical developmental expectations. In a similar vein, Kent and colleagues (Kent et al., 2020) reviewed interventions related to play skills. In their systematic review, play-based interventions were included if they met crucial elements of intrinsic motivation, internal control, and the freedom to suspend reality alongside evidence of a ‘play frame’ identified by playful exchanges of social play cues (Bundy, 2012). Using these criteria, 11 randomised controlled trials (RCTs) were identified. Other reviews in this area investigate the type of social play skills targeted (Kossyvaki & Papoudi, 2016), playful engagement (Godin et al., 2019b), and interventions that have involved peer-mediated approaches (Lory et al., 2018).
Reviews investigating non-play outcomes relating to social and communication development have focused on specific therapeutic approaches. For example, Lindsay et al. (2017) investigated the evidence for LEGO Therapy, while Tiede and Walton investigated Naturalistic Developmental Behavioral Interventions (NDBIs; Tiede & Walton, 2019).
Overall, the existing reviews we identified are beneficial to understanding particular methods, or types of play-based interventions that have been researched. This body of literature demonstrates some promising findings but also raises important challenges.
Firstly, as discussed by Kent et al. (2020), the definitions of play used across literature are disparate, making synthesis a challenging task. Furthermore, the operationalisation of play within an intervention setting varies widely according to the philosophy or approach underpinning different intervention types. The latter is not always acknowledged by researchers or clinicians but preliminary consultation for the present study indicated that this aspect is important to autistic individuals and their families. Related to this, we identified no existing review in the literature that could help parents and practitioners to identify and appraise the relative merits of different play-based interventions that target similar outcomes.
The present study
The present study has the following aims
To provide a comprehensive map of the research regarding play-based interventions targeting social and communication outcomes for autistic children
To develop a conceptual framework for the appraisal of play-based interventions targeting social and communication outcomes for autistic children
Methods
Approach
We adopted a scoping review methodology (Munn et al., 2018). The study design was informed by Joanna Briggs Institute guidelines (Peters et al., 2015), and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) statement (Tricco et al., 2018).
The protocol for the review was registered prospectively on the Open Science Framework (https://osf.io/ajp29), and updates, changes to this protocol (and the reasons for them) are recorded here https://osf.io/ajp29.
Community involvement
We held informal conversations with stakeholders, including autistic adults and parents and practitioners supporting autistic children, to learn more about their views on play and play-based interventions. All agreed on the importance of the topic and the need for clarification about how play can be used to support communication skills, however, conversations revealed varying personal perspectives. Some practitioners felt play was a less appropriate word as children got older, while others thought the emphasis should be on freely chosen, pleasurable activities, kept distinct from ‘work’ or ‘intervention’. Practitioners working in education noted different approaches between mainstream and specialist provision. From an autistic perspective, play was referred to as an escape that helps manage anxiety and promote communication and friendships with people with similar interests. However, autistic adults also reported that play can sometimes cause anxiety and expressed discomfort with the idea that some interventions could be rooted in a behaviourist approach.
This consultation informed our approach to evidence synthesis, as we reflected concerns of stakeholders within our framework for understanding play-based interventions. We also set up a separate, qualitative study to more systematically explore the different perspectives raised (see Gibson, de Lemos, et al., 2020 for preregistration of this study).
Eligibility criteria
To keep the scope of the review broad yet manageable, we investigated peer-reviewed research that had been published over the past 10 years, with samples of children up to the age of 8 years and concentrated on studies using quantitative or mixed-methods designs. Although some playful approaches are relevant to older children and adolescents, we restricted the search criteria to between 2-8 years of age as our preliminary searches indicated that this group is most likely to be included in play-based interventions and we did not have the resources to cover the entirety of childhood from 0-18 years of age. Resources did not permit a grey-literature search.
We adapted Bundy and colleagues’ (Bundy, 2012; Skard & Bundy, 2008) concept of playfulness, and Gibson and colleagues’ concept of social play as an optimised learning context (Gibson et al., 2020, p. 14) to inform judgements about whether an intervention could be considered play-based. According to Bundy and colleagues, playfulness consists of four elements: intrinsic motivation (a child playing simply because he or she wants to), internal control (a child feeling in control of their play-related actions), freedom to suspend reality (a child chooses how close to objective reality the play is e.g. engaging in pretend play), and framing (a child’s ability to give and read social play clues). Meanwhile, we argue that social play provides optimal conditions for the child to co-construct opportunities for practice and development of key social communication skills.
Translating this to an intervention setting, the interventionist must skilfully set the conditions for play, such that these constitute an optimised environment where affordances for learning are mapped to a child’s individual needs, providing conditions for developmental change to be enacted by children themselves. For the present review, we focused on judging whether an intervention created opportunities for intrinsic motivation, internal control and freedom to suspend reality. Most importantly, we considered a play-based intervention to be one that sets up the conditions for a child to engage in an intrinsically motivated fashion (see also Godin et al., 2019a, 2019b). As such, pure forms of discrete trial teaching (DTT)1 were not included, even where a toy was offered as a ‘reinforcer’ as this was not considered an intrinsically motivated, volitional play opportunity.
We included studies meeting the following eligibility criteria:
Sample
Children aged 2:0-7:11 years with an autism diagnosis (e.g. ASD, autistic disorder, Asperger’s syndrome or pervasive developmental disorder not-otherwise specified (PDD-NOS)). Studies of participants with autism with co-occurring conditions were included.
Intervention
Study reports a play-based intervention. This criterion can be met when play is explicitly mentioned, or if raters judge that the intervention supports intrinsic motivation, internal control, and freedom to suspend reality.
Outcomes
Study reports outcomes regarding social and communication skills, including related skills in social cognition
Study reports outcome measures that are primarily quantitative in nature
Other characteristics
Study presents original research (including published protocols)
Published in a peer-reviewed journal
Studies published since 2009
Written or translated into English or German (the languages available to the authors)
Exclusion characteristics
interventions that are too broad in nature to permit ‘isolation’ of elements relating to play
interventions solely based on animal-assisted therapies, DTT, cognitive behavioural therapy, social media, or social stories
outcomes solely related to educational achievement, sensory experience, routines, special interests, and inflexibility
outcome measures that are entirely qualitative
reviews, and meta-analyses
book chapters
Search strategy
Terms relating to autism, play-based intervention, social/communication outcomes, and those implying an intervention study were combined for the literature search (see appended example, or online protocol for full strategy). A combination of free text (across title/abstract/keyword fields) and subject heading terms were used, and the search strategy was adapted for each database.
Electronic searches using these terms were conducted on 7 and 8 November 2019 across seven electronic databases covering the period 01/01/2009 -06/11/2019: British Education Index, Child Development & Adolescent Studies, ERIC, PsycINFO, PubMed, Scopus and Web of Science Core Collection. Filtering by publication date, participant age and publication or source type (those published in academic journals), was carried out after searching. There were no restrictions by language.
For quality assurance, the Web of Science and PsycINFO searches were peer-reviewed by a research librarian using the Peer Review of Electronic Search Strategies (PRESS) checklist (McGowan et al., 2016).
The electronic database searching was supplemented by scanning the reference lists of selected relevant reviews. Authors of potentially relevant but inaccessible articles were contacted up to three times to request full text articles. Articles that remained inaccessible were excluded.
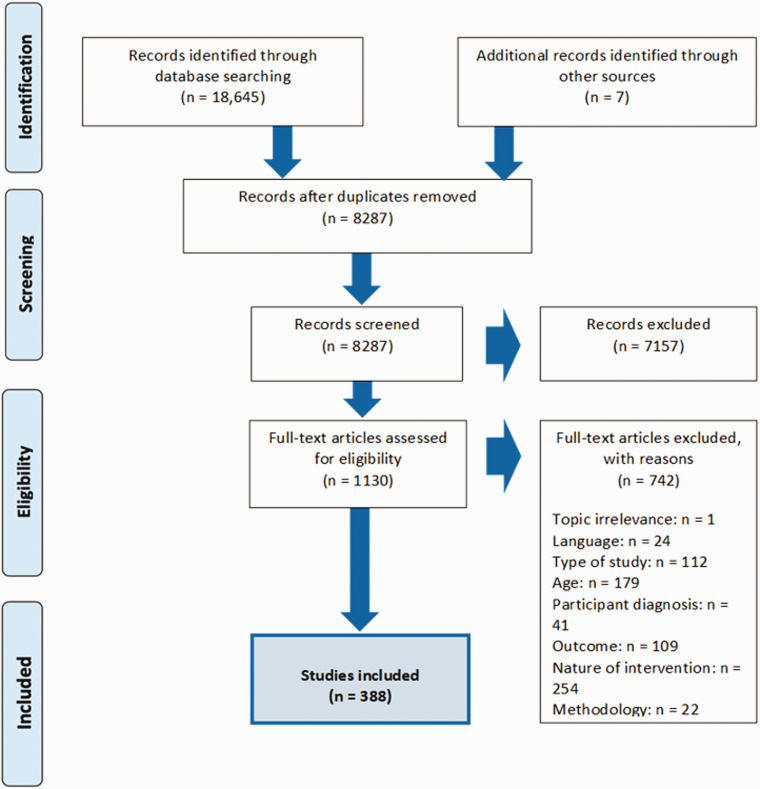
Study selection
The search yielded 18,645 papers, which we uploaded into EPPI-Reviewer 4 software (Thomas et al., 2010). Handsearching techniques yielded seven further studies. Figure 1 shows the PRISMA-ScR process diagram of study selection within this review.
Figure 1.
Study selection process.
After deduplication, 8,287 studies were screened for relevance based on title and abstract, 3% of these (248) were independently double-coded for inclusion, percentage agreement = 93.98%, Cohen’s kappa (κ) = .818 (95% CI, .646 to .990), p < .001. Any disagreements were resolved through discussion.
The remaining 1,130 articles were full-text reviewed against the study inclusion and exclusion criteria. 20% of these were double-blinded coded; 81% agreement and moderate κ = .619 (95% CI,.466 to .772), p < .001.
Charting and synthesising the data
The data charting process is the first step in summarising and synthesising across the evidence base. Aside from the codes based on the inclusion and exclusion criteria, we wished to chart important commonalities across the different studies. Therefore, creation of charting codes was an iterative process involving discussion and reflection between all authors, guided by principles set out by Gough, Oliver and Thomas (Gough et al., 2017; Thomas et al., 2017). The full data charting codes and categories are in the supplementary materials (S1).
The following data were recorded for each included study: Bibliographic data; data relevant to inclusion criteria; participant information; intervention details; aspects of play; outcome domain; agent of intervention. Classification under these different headings was double-blind coded for 20% of the 388 included studies, average κ =.75 across all codes.
Once charting was complete, we then conducted a narrative synthesis to address the second aim of developing a conceptual framework that can help practitioners and others navigate and appraise the extensive literature in this area.
Managing the high number of studies
After full-text review, 388 studies met the inclusion criteria (see Figure 1, plus list of included studies in supplementary materials S2). As this number of studies is too large to tabulate in the context of an academic paper, we took a different approach to that of scoping studies with smaller samples. We provide the full list of studies online using interactive evidence gap maps (EGMs). These allow the user to summarise charted characteristics across important dimensions, according to their own interests. In the Results section, we provide quantitative summaries of this evidence under different headings. Secondly, given our aim to provide practitioners with a useful way to navigate the evidence base, we selected a subset of interventions meeting the following criteria:
Intervention should be the subject of at least two research studies, and
be a named or ‘manualised’ intervention approach
We refer to this subset, comprising 127 studies of 19 different interventions, as the ‘named interventions’. These selection criteria were devised to give a more detailed yet accessible overview of the interventions that clinicians may more commonly encounter in practice, given the high number of novel interventions reported by just one study.
The narrative synthesis element can be found in the Discussion section of the present paper.
Deviations from protocol
Deviations from the original protocol were largely the result of pragmatic decisions to enable the work to fit with available resources, however some changes were made on the basis of reflection, consultation with stakeholders and findings of unexpected complexity in some areas where our original thoughts no longer applied. All changes from protocol are documented here https://osf.io/ajp29.
Results
A total of 388 studies met inclusion criteria. The full list of included studies is in the supplementary materials (S2) and a summary of the named interventions is presented in Table 1.
Table 1.
Summary of named interventions.
| Named intervention (n studies; % of totala) | Participant characteristics b | Study design | Intervention type | Aspects of playc | Agent of intervention | Social communication outcome |
|---|---|---|---|---|---|---|
|
Advancing Social-Communication and Play (ASAP) (n = 2, 1.57%) Boyd et al. (2018) Dykstra et al. (2012) |
Age range: 2–7 Gender: Mixed = 2 Co-occurring conditions: With co-occurring conditions = 1 Autistic-only = 1 IQ/adaptive functioning: IQ range = <50-70 VABSd = N/A |
RCT = 1 Studies meeting Indicative level criteria = 1 |
Feedback-based = 2 |
Role of play = Key mechanism Level of child- control = Guided |
Main professional: Mixed professions/ interdisciplinary teams = 2 Others involved: TA/paraprofessional = 2 |
Multiple = 2 Social play skills, Early developmental communication skills & Communication = 1 Social play skills & Early developmental communication skills = 1 |
|
Developmental, Individual- differences, Relationship-based
(DIR)/Floortime (n = 3, 2.36%) Reis et al. (2018) Carpente (2017) Liao et al. (2014) |
Age range:
2-8 Gender: Male = 1 Mixed = 2 Co-occurring conditions: Autistic-only = 3 IQ/adaptive functioning: IQ range = 51– 140 VABS = N/A |
Other study = 3 |
Feedback-based = 2 Mixed = 1 Feedback- based & Art and outdoor activity |
Role of play = Key mechanism Level of child- control = Child-led |
Main professional: Occupational therapy = 1 Arts/creative therapies = 1 Mixed professions/ interdisciplinary teams = 1 Others involved: Parent/Carer = 2 None = 1 |
Social communication severity scales = 1
Communication = 1 Multiple = 1 Social communication severity scales, Social cognition & Language |
|
Early Start Denver Model (ESDM) (n = 22,
17.32%) Geoffray et al. (2019), Rogers et al. (2019), Holzinger et al. (2019), Vivanti et al. (2019), Waddington et al. (2019), Waddington et al. (2019), Zhou et al. (2019), Colombi et al. (2018), Hernandez-Ruiz (2018), Vinen et al. (2018) Zhou et al. (2018), Touzet et al. (2017), Vivanti et al. (2016), Diamond et al. (2015), Estes et al. (2015) Fulton et al. (2014)Vivanti et al. (2014), Eapen et al. (2013), Vivanti et al. (2013),Dawson et al. (2010), Vismara, Colombi et al. (2009)Vismara, Young et al. |
Age range: 2-8 Gender: Male = 3 Mixed = 15 Not stated = 3 Co-occurring conditions: Autistic-only = 21 IQ/adaptive functioning: IQ range = <50–100 VABS = <70–114 |
RCT = 6 Quasi- experimental = 6 Studies meeting Indicative level criteria = 3 Other study = 7 |
Influenced by behaviourist
approach = 7 Mixed = 15 Feedback-based & Influenced by behaviourist approach =14 Feedback-based, Influenced by behaviourist approach & Art and outdoor activity = 1 |
Role of play = Key mechanism Level of child- control = Guided |
Main professional:
Psychology = 2 Education = 1 Non-specified = 4 Arts/creative therapies = 1 Mixed professions/ interdisciplinary teams = 14 Others involved: Parent/Carer =11 None = 11 |
Social communication severity scales = 2
Language = 2 Multiple = 18 Social communication severity scales & Language = 9 Social play skills, Early developmental communication skills & Language = 3 Language & Communication = 1 Early developmental communication skills & Communication = 1 Early developmental communication skills, Language & Communication = 1 Early developmental communication skills, Social communication severity scales, Language & Communication = 1 |
| (2009). | Social play skills, Early developmental communication skills,
Social communication severity scales &
Language = 1 Social communication severity scales,Language & Relational skills = 1 |
|||||
|
Frankfurt Early Intervention Program
(FFIP) (n = 3, 2.36%) Kitzerow et al. (2019), Kitzerow et al. (2014), Freitag et al. (2012) |
Age range: 2-8 Gender: Mixed = 3 Co-occurring conditions: Autistic-only = 3 IQ/adaptive functioning: IQ range = <50-120 VABS = <70-114 |
Quasi- experimental = 1 Other study = 2 |
Mixed = 3 Feedback-based & Influenced by behaviourist approach |
Role of play = Context Level of child- control = Guided |
Main professional:
Psychology = 3 Others involved: Parent/Carer = 3 Teacher = 3 |
Language = 1 Multiple = 2 Social communication severity scales & Language |
|
Incredible Years Parent Program(n = 2,
1.57%) Kong and Au (2018), Williams et al. (2017) |
Age range: 2-8 Gender: Mixed = 1 Co-occurring conditions: With co-occurring conditions = 1 Autistic-only = 1 IQ/adaptive functioning: N/A |
RCT = 2 | Feedback-based = 2 |
Role of play = Component Level of child- control = Child-led |
Main
professional: Psychology = 1 Non-specified = 1 Others involved:Parent/Carer = 2 |
Early developmental communication
skills = 1 Social communication severity scales = 1 |
|
Joint Attention, Symbolic Play, Engagement &
Regulation (JASPER)
(n = 21, 16.54%) Shire et al. (2019) Shire et al. (2018) Shire et al. (2017), Almirall et al. (2016), Chang, et al. (2016) Chiang et al. (2016), DiStefano, et al. (2016), Shire et al. (2016) Kasari et al. (2015), Shire et al. (2015), Gulsrud, et al. (2014) Kaale et al. (2014) |
Age range: 2-8 Gender: Male = 1 Mixed = 15 Not stated = 5 Co-occurring conditions: With co-occurring conditions = 1 Autistic-only = 21 IQ/adaptive functioning:IQ range = <50-100 VABS = N/A |
RCT = 19 Quasi- experimental = 2 |
Mixed = 21 Feedback-based & Influenced by behaviourist approach = 15 Feedback-based, Influenced by behaviourist approach & Augmentative and alternative communication = 5 Feedback-based, Influenced by behaviourist approach & Art and outdoor activity = 1 |
Role of play = Key mechanism Level of child-control = Child-led= 20 Guided = 1 |
Main professional:
Psychology = 11 Education = 2 Non-specified = 2 Mixed professions/interdisciplinary teams = 6 Others involved: Parent/Carer = 10 Teacher = 5 TA/paraprofessional = 4 None = 4 |
Early developmental communication
skills = 5 Language = 1 Communication = 2 Multiple = 13 Social play skills & Early developmental communication skills = 4 Early developmental communication skills & Communication = 2Early developmental communication skills, Social communication severity scales & Language = 2 Early developmental |
| Kasari, Kaiser et al. (2014), Kasari, Lawton et al. (2014),
Goods et al. (2013) Wong (2013), Kaale, et al. (2012), Kasari et al. (2012) Lawton and Kasari (2012a), Lawton and Kasari (2012b), Kasari et al. (2010) |
communication skills & Language = 2 Early developmental communication skills, Language & Communication = 1 Social communication severity scales, Social cognition, Language & Communication = 1 Early developmental communication skills, Social communication severity scales & Communication = 1 |
|||||
|
Reciprocal Imitation Training (n = 9,
7.09%) Penney and Schwartz (2019), Toret and Ozmen (2019), Wainer and Ingersoll (2015), Wainer and Ingersoll (2013), Ingersoll (2012) Walton and Ingersoll (2012), Cardon and Wilcox (2011), Ingersoll (2010)Ingersoll and Lalonde (2010) |
Age range: 2-7 Gender: Male = 5 Mixed = 3 Not stated = 1 Co-occurring conditions: Autistic only = 9 IQ/adaptive functioning: IQ range = N/A VABS = <70-114 |
RCT = 2 Studies meeting Indicative level criteria = 6 Other study = 1 |
Feedback-based = 8 Mixed = 1 -Feedback-based & video modelling |
Role of play = Key mechanism Level of child- control = Guided |
Main professional:
Speech and language therapy = 1 Psychology = 1 Education = 1 Non-specified = 6 Others involved: Parent/Carer = 3 Sibling = 1 None = 5 Other = 1 |
Social play skills = 2 Early developmental communication skills = 4 Multiple = 3 Social play skills, Early developmental communication skills & Language = 1 Early developmental communication skills & Social communication severity scales= 1 Early developmental communication skills, Communication & Language = 1 |
|
Responsive Teaching (n = 3, 2.36%) Alquraini et al. (2018), Yang (2016) Mahoney et al. (2014) |
Age range: 2-4 Gender: Mixed = 3 Co-occurring conditions: With co-occurring conditions = 1 Autistic only = 2 IQ/adaptive functioning: IQ range = <50-100 VABS = <70-85 |
RCT = 1 Other study = 2 |
Feedback-based = 2 Art and outdoor
activity = 1 |
Role of play = Key mechanism Level of child- control = Child-led = 2 Guided = 1 |
Main professional:
Arts & creative therapies = 1 Non-specified = 2 Others involved: Parent/Carer = 3 |
Language = 1 Multiple = 2 Social communication severity scales & Language = 1 Social play skills & Communication = 1 |
|
Kaspar (Kinesics and Synchronisation in Personal Assistant
Robotics)
(n = 3, 2.36%) Karakosta et al. (2019), Mengoni et al. (2017) Wainer et al. (2014) |
Age range: 4-8 Gender: Mixed = 2 Co-occurring conditions: Autistic-only = 2 IQ/adaptive functioning: N/A |
RCT = 1 Other study = 2 |
Robot-assisted = 2 Mixed = 1 Computer- based, Robot- assisted & Collaboration- based |
Role of play = Key mechanism Level of child- control = Adult-led |
Main professional:
Education = 1 Non-specified = 1 Other = 1 Others involved: None = 3 |
Early developmental communication
skills = 1 Social communication severity scales = 1Multiple = 1 Social play skills, Early developmental communication skills & Social communication severity scales |
|
LEGO therapy (n = 4, 3.15%) Varley et al. (2019) Hu et al. (2018), Huskens et al. (2015) Pang (2010) |
Age range: 4-8 Gender: Male = 2 Mixed = 1 Co-occurring conditions: With co-occurring conditions = 1 Autistic-only = 3 IQ/adaptive functioning: IQ range = 101-120 VABS = N/A |
RCT = 1 Studies meeting Indicative level criteria = 2 Other study = 1 |
Collaboration-based = 2 Mixed = 2 Collaboration- based & Feedback-based = 1 Robot-assisted, Collaboration- based & Feedback-based = 1 |
Role of play = Key mechanism Level of child- control = Guided = 1 Adult-led = 3 |
Main professional:
Education = 3 Non-specified = 1 Others involved: Sibling = 1 TA/paraprofessional = 1 Peer = 2 |
Social play skills = 2
Language = 1 Multiple = 1 Social communication severity scales & Communication |
|
Preschool Autism Communication Trial (PACT) (n = 5,
3.94%) Leadbitter et al. (2018), Pickles et al. (2016), Byford et al. (2015), Aldred et al. (2012), Green et al. (2010) |
Age range: 2-7 Gender: Mixed = 5 Co-occurring conditions: Autistic-only = 5 IQ/adaptive functioning: IQ range = N/A VABS = <70-85 |
RCT = 5 | Feedback-based = 5 |
Role of play = Key mechanism Level of child- control = Child-led |
Main professional:
Speech and language therapy = 5 Others involved: Parent/Carer = 5 |
Social communication severity
scales = 2 Multiple = 3 Social play skills& Social communication severity scales = 1 Social play skills, Social communication severity scales & Language = 2 |
|
Play and Language for Autistic Youngsters - PLAY
Project (n = 2, 1.57%) Mahoney and Solomon (2016), Solomon et al. (2014) |
Age range: 2-7 Gender: Mixed = 2 Co-occurring conditions: Autistic-only = 2 IQ/adaptive functioning:N/A |
RCT = 2 | Feedback-based = 2 |
Role of play = Key mechanism Level of child- control = Child-led |
Main professional:
Mixed professions/ interdisciplinary teams = 2 Others involved: Parent/Carer = 2 |
Multiple = 2 Social play skills & Social communication severity scales = 1 Social play skills & Language = 1 |
|
Play Time/Social Time (n = 2, 1.57%) Szumski et al. (2019), Szumski et al. (2016) |
Age range: 2-8 Gender: Mixed = 1 Not stated = 1 Co-occurring conditions: Autistic-only = 2 IQ/adaptive functioning: IQ range = 71-140 VABS = N/A |
Quasi- experimental = 1 Other study = 1 |
Mixed = 2 Social skills group, Feedback-based & Influenced by behaviourist approach |
Role of play = Key mechanism Level of child- control = Guided |
Main professional:
Education = 2 Others involved: None = 2 |
Multiple = 2 Social play skills & Relational skills = 1 Social play skills, Social cognition & Relational skills = 1 |
|
Project ImPACT (Improving Parents as Communication
Teachers) (n = 5, 3.94%) Ingersoll et al. (2017), Ingersoll et al. (2016), Stadnick et al. (2015), Ingersoll and Wainer (2013a), Ingersoll and Wainer (2013b) |
Age range: 2-8 Gender: Mixed = 5 Co-occurring conditions: With co-occurring conditions = 1 Autistic-only = 4 IQ/adaptive functioning: IQ range = N/A VABS = <70-85 |
RCT = 1 Quasi- experimental = 1 Studies meeting Indicative level criteria = 3 |
Influenced by behaviourist
approach = 1 Mixed = 4 Feedback-based & Influenced by behaviourist approach |
Role of play = Key mechanism Level of child- control = Child-led |
Main professional:
Psychology = 1 Education = 1 Non-specified = 1 Mixed professions/interdisciplinary teams = 2Others involved: Parent/Carer = 4 None = 1 |
Social play
skills = 1 Multiple = 4 Social play skills, Language & Communication = 1 Early developmental communication skills & Language = 1 Early developmental communication skills, Social communication severity scales & Language = 1 Social communication severity scales & Language = 1 |
|
Pivotal Response Treatment (PRT)
(n = 23, 18.11%) |
Age range: 2-8 Gender: Male = 7 |
RCT = 4 Quasi- experimental = 4 |
Influenced by behaviourist approach = 7 | Role of play = Context |
Main professional:
Speech and language therapy = 2 Psychology = 5 Education = 2 |
Social play skills = 1 Early developmental communication skills= 2 |
| Gengoux et al. (2019). Kim (2019) Boudreau et al. (2019). Smith et al. (2019). Vernon et al. (2019). Berman et al. (2018). Fossum et al. (2018). van Straten et al. (2018). Smith et al. (2015). Ventola et al. (2015). Koegel et al. (2014), Mohammadzaheri et al. (2014) Rieth et al. (2014), Schreibman and Stahmer (2014), Ventola et al. (2014) Stock et al. (2013) Matsuzaki and Yamamoto (2012), Vernon et al. (2012) Randolph et al. (2011), Coolican et al. (2010), Smith et al. (2010), Jones (2009), Schreibman et al. (2009) |
Mixed = 15 Not stated = 1 Co-occurring conditions: With co-occurring conditions = 1 Autistic-only = 22 IQ/adaptive functioning: IQ range = <50-140 VABS = <70-114 |
Studies meeting Indicative level
criteria = 8 Other study = 7 |
Mixed = 16 Feedback-based & Influenced by behaviourist approach = 10 Early intensive intervention, Feedback-based & Influenced by behaviourist approach = 2 Early intensive intervention & Influenced by behaviourist approach = 2 Robot-assisted, Collaboration- based & Influenced by behaviourist approach = 1 Feedback-based, Influenced by behaviourist approach & Augmentative and alternative communication = 1 |
Level of child- control = Guided =21 Adult-led = 2 | Non-specified = 7 Mixed professions/interdisciplinary teams = 6 Other = 1 Others involved: Parent/Carer = 13 TA/paraprofessional = 1 Peer = 2 None = 7 |
Language = 3 Communication = 2 Multiple = 15 Social communication severity scales & Language = 7 Social play skills, Social communication severity scales & Language = 2 Language & Communication = 1 Social communication severity scales, Social cognition, Language & Communication = 1 Social play skills & Communication = 1 Relational skills & Communication = 1 Social play skills & Social communication severity scales = 1 Early developmental communication skills & Communication = 1 |
|
Remaking Recess (n = 4, 3.15%) Locke et al. (2019), Locke et al. (2019), Shih et al. (2019) Kretzmann et al. (2015) |
Age range: 4-8 Gender: Male = 1 Mixed = 3 Co-occurring conditions: Autistic-only = 4IQ/adaptive functioning: IQ range = 51-120 VABS = N/A |
RCT = 3 Other study = 1 |
Feedback-based = 4 |
Role of play = Key mechanism Level of child- control = Guided |
Main professional: Non-specified = 2 Mixed professions/ interdisciplinary teams = 2 Others involved: Teacher = 1 TA/paraprofessional = 4 Peer = 4 |
Relational skills = 4 |
|
Social ABCs (n = 2, 1.57%) Brian et al. (2017), Brian et al. (2016) |
Age range: 2-4 Gender: Mixed = 2 Co-occurring conditions: Autistic-only = 2 IQ/adaptive functioning: N/A |
RCT = 1 Other study = 1 |
Mixed = 2 Feedback-based & Influenced by behaviourist approach |
Role of play = Context Level of child- control = Guided |
Main
professional: Non-specified = 2 Others involved: Parent/Carer = 2 |
Multiple = 2 Social play skills & Social communication severity scales |
|
Stay, Play, & Talk (n = 6, 4.72%) van Rhijn et al. (2019), Maich et al. (2018) Thiemann-Bourque et al. (2018), Thiemann-Bourque, et al. (2017), Barber et al. (2016)Thiemann-Bourque et al. (2016) |
Age range:
2-7 Gender: Male = 2 Mixed = 4 Co-occurring conditions: Autistic-only = 6 IQ/adaptive functioning: IQ range = <50-100 VABS = N/A |
RCT= 1 Quasi- experimental = 1 Studies meeting Indicative level criteria = 3 Other study = 1 |
Feedback-based = 3 Mixed = 3 Feedback-based & Augmentative and alternative communication |
Role of play = Key mechanism Level of child- control = Child-led = 3 Adult-led = 3 |
Main
professional: Education = 3 Mixed professions/interdisciplinary teams = 2 Non-specified = 1 Others involved: TA/paraprofessional = 2 Peer = 6 |
Communication = 3 Multiple = 3 Language & Communication = 2 Social play skills & Relational skills = 1 |
|
Superheroes Social Skills (n = 6,
4.72%) Radley et al. (2019), Radley et al. (2017), Radley et al. (2017), Radley et al. (2016), Radley et al. (2014), Radley et al. (2014) |
Age range:
2-8 Gender: Male = 2 Mixed = 3 Not stated = 1 Co-occurring conditions: With co-occurring conditions = 1 Autistic-only = 6 IQ/adaptive functioning: IQ range = 71– 140 VABS = <70 - 85 |
Studies meeting Indicative level
criteria = 5 Other study = 1 |
Mixed = 6 Social skills group, Feedback-based & Video modelling = 4 Social skills group, Feedback-based & Influenced by behaviourist approach = 2 |
Role of play = Component Level of child- control = Child-led = 3 Guided = 2 Adult-led = 1 |
Main
professional: Psychology = 6 Others involved: Parent/Carer = 1 None = 5 |
Social play skills = 1 Relational
skills = 3
Communication = 1 Multiple = 1 Social play skills, Social communication severity scales & Relational skills |
Note: Totals may be less than or greater than expected as multiple codes have been applied to some studies for co-occurring conditions and others involved, and for protocols, gender and co-occurring conditions was not coded. For some studies, separate papers report the results based on the same initial RCT or trial. We have counted the number of RCTs per published paper rather than per study.
aN = 127.
bValues for ranges (age, IQ, VABS) represent a summary of the overall range covered across all studies within each named approach.
cSome studies have different codes for level of child-control (e.g. modified interventions) as this was coded on a paper-specific basis, rather than per intervention.
dVineland Adaptive Behavior Scales (VABS).
Below we report results of the charting and synthesis process, starting with our approach to mapping different types of play-based interventions and moving on to considering the characteristics of the evidence-base.
Play-based intervention types
To meet our first aim of providing a comprehensive map of the research regarding play-based interventions targeting social and communication outcomes, we devised categories to group together play-based interventions with a common methodological approach or aim, see Table 2. The categories are not necessarily mutually exclusive although for each study in the review we have attempted to identify the main intervention type wherever possible.
Table 2.
Types of play-based intervention.
| Intervention type | Description |
|---|---|
| Feedback-based | Practitioner provides tailored feedback to the target child and/or their interaction partner during or after play. The play partner may be a parent, other professional, or a peer. |
| Influenced by behaviourist approach | Judged as having been influenced by Applied Behaviour Analysis (ABA) principles such as discrete trial teaching and positive reinforcement, to varying degrees. May range from traditional to more developmental interpretations of ABA. |
| Computer-based | Delivered via computer (including video games). |
| Robot-assisted | Delivered via robot technologies. |
| Virtual Reality | Involve the use of virtual reality games. |
| Augmentative and alternative communication (AAC) | Low- or high-tech technologies to support successful communication. |
| Video modelling | Pre-made or individualised videos consisting of modelled targets. The child watches these and imitates the modelled target behaviours with varying support in appropriate settings. |
| Early intensive intervention | Comprehensive intervention programmes, delivered over a period of time shortly after a child receives an autism diagnosis. |
| Social skills group | Delivered to groups of children. They often support the development of holistic or specific social and communication skills. |
| Art and outdoor activity | Activity-based interventions such as aquatic or music therapy. |
| Play therapy | Typically delivered by specialist play therapists trained in child psychotherapy. |
| Activity schedule | Interventions which use a visual breakdown of steps related to a target activity to support the child’s successful or appropriate involvement. |
| Collaboration-based | Collaborative working with others for a task within an intervention to be successful. |
| Mixed | A mixture of the above intervention types. |
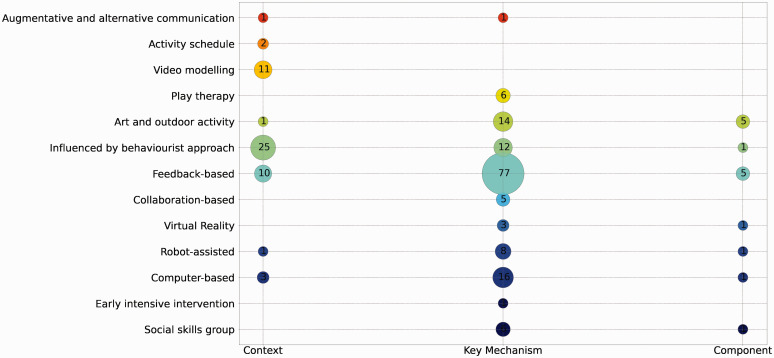
Aspects of play within interventions
We also characterised the interventions along two main dimensions relating to their conceptualisation of play:
“role of play” – the extent that playful engagement is considered the key mechanism of developmental change, and
“level of child control” – the extent to which the intervention is child-led
Codes relating to these aspects of play are shown in Table 3, and the frequency of each aspect of play by intervention type is shown in Figures 2 and 3.
Table 3.
Aspects of play coding.
| Description | |
|---|---|
| Role of play | |
| Component | An aspect of free play or structured game play is included as part of an intervention session(s), or as part of a programme that has multiple components. |
| Context | Play is conceptualised as a context for intervention. For example, it could target social engagement set in an environment conducive to play, such as a playground or play corner in a nursery. |
| Key mechanism | The intervention actively uses play within the intervention as a key mechanism for change. |
| Level of child-control | |
| Adult-led intervention | Highly structured, the adult is in control determines the target and type of play. |
| Guided intervention | A structured intervention that allows the child freedom within the limits of that structure, or a combination of adult-led and child-led play is used. |
| Child-led intervention | An intervention which allows the child to engage in free play or follows the child’s lead, for example using techniques to expand upon utterances or prolong shared attention when something has caught a child’s interest. |
Figure 2.
Frequency of role of play by intervention type.
Figure 3.
Frequency of each level of child-control by intervention type.
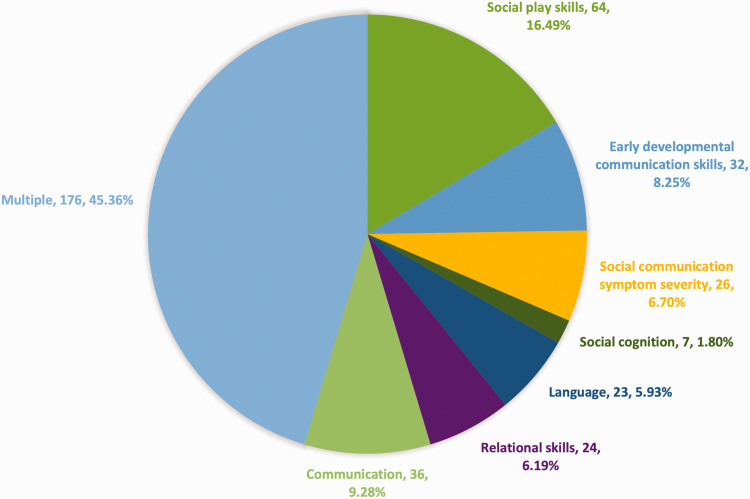
Social communication outcomes
The present review focuses on interventions targeting outcomes related to social and communication development. To summarise the vast array of potential intervention targets in these areas, we devised eight broad outcome categories that capture the main area of focus for each study (see supplemental materials S3).
Figure 4 shows the proportion of studies (N = 388) for each outcome domain. The most common category is the ‘multiple’ outcomes category, with over 45% of studies using more than one relevant outcome. Social play skills are the next most common target of play-based interventions.
Figure 4.
Proportion of studies targetting each outcome type.
Agent of intervention (AoI)
Given the scope of interdisciplinary involvement in play-based interventions, we aimed to record those who were actively involved in delivering the intervention in relation to its theorised mechanisms of change. Despite AoI-type codes being a common feature of many intervention-related reviews, this category was difficult to implement in practice for many reasons, including – multiple agency delivery or involvement, unclear reporting, the role of the main professional or others involved being complex and variable practices across interventions/studies. Two over-arching categories were developed:
‘Professional background of intervention lead’ – the background or profession of the main interventionist or clinical researcher leading the delivery of the intervention; or multidisciplinary team.
and
‘Others involved’ – individuals also actively involved in the intervention delivery who are not considered under the ‘Professional background’ category. Typically, this concerns studies in which the lead interventionist trains an individual to implement the intervention and includes a variety of non-professionals or paraprofessionals. Note that robots are not considered as part of these categories.
The frequency for each subcategory within the AoI codes is shown in Table 4.
Table 4.
Frequency for each agent of intervention category (AoI).
| AoI category | Count |
|---|---|
| Professional background of intervention lead | |
| ABA/Behaviourist training or background | 15 |
| Arts/creative therapies | 8 |
| Education | 47 |
| Mixed professions/ interdisciplinary teams | 74 |
| Non-specified | 147 |
| Occupational Therapy | 4 |
| Other | 9 |
| Play Therapy | 2 |
| Psychology | 53 |
| Speech & Language Therapy | 29 |
| Others involved | |
| None | 179 |
| Other | 3 |
| Parent/Carer | 136 |
| Peer | 32 |
| Sibling | 6 |
| Teacher | 25 |
| Teaching assistant/paraprofessional | 31 |
Participant characteristics
Three hundred and sixty-four studies (94.79%)2 included an autistic-only sample and 52 studies (13.54%) included autistic participants with co-occurring conditions. Sixty percent studied females and males, although mixed samples tended to include more males. Just 1.6% of studies looked at play-based interventions for girls only and 28.9% investigated boys only. The remaining studies did not report the gender/sex of their participants.
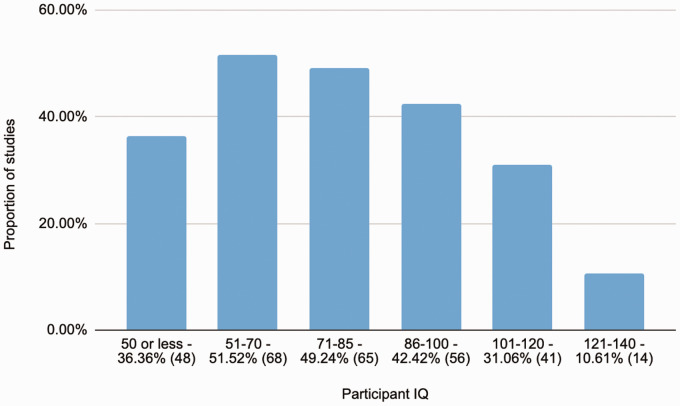
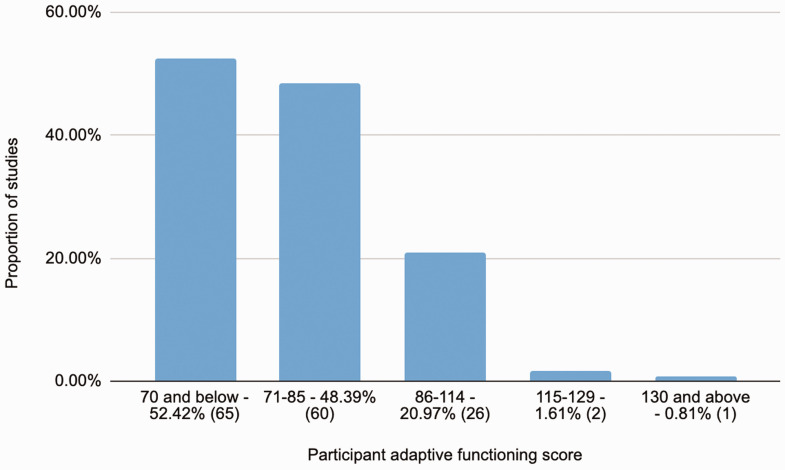
Reports of participant IQ and adaptive functioning were found in a substantial minority of studies. Figure 5 shows the breakdown for the 132 studies reporting IQ and Figure 6 shows comparable data for the Vineland Adaptive Behavior Scale (VABS) adaptive functioning scores. Table 5 shows the numbers of studies reporting these and other relevant characteristics such as language ability or autistic symptomatology scores.
Figure 5.
IQ ranges of participants in studies reporting an IQ measure (n = 132).
Figure 6.
Vineland Adaptive Behavior Scales (VABS) ranges in studies reporting this measure (n = 124).
Table 5.
Indicators of functioning.
| Functional indicator | % (n) |
|---|---|
| IQ score | 34.02 (132) |
| Adaptive functioning (VABS) score | 31.96 (124) |
| Functional description | 43.56 (169) |
| ASD symptomatology diagnostic score | 40.21 (156) |
| Language measure | 23.71 (92) |
| Developmental or mental age equivalent | 15.98 (62) |
| Not given | 8.25 (32) |
Moving to consider demographic and contextual characteristics, a substantial majority of the research has been produced in the USA, followed by Canada, Australia, and the UK. Most studies did not provide information about ethnicity (n = 239, 62.2%), family income (n = 349, 90.9%), parental occupation (n = 364, 93.8%), or maternal education levels (n = 287, 74.7%). Where reported, the most common ethnicity categories were White, Latinx/Hispanic, Black, Asian and Mixed/Other. Just five studies reported on indigenous or first nation cultures in the regions where the highest number of studies were conducted.
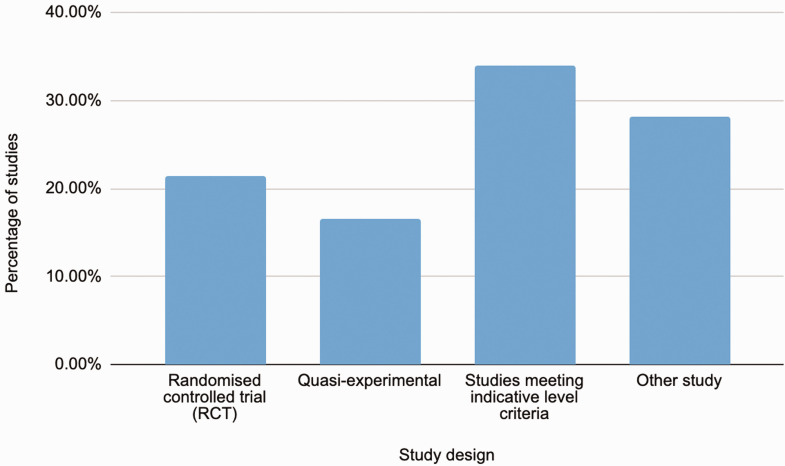
Study design
The coding of study designs, shown in Table 6, was adapted from the three ‘level of evidence’ ratings used by The Communication Trust’s Better Communication Research Project (Law et al., 2012). Note that while the study design categories give an indication of the overall quality of the evidence when it comes to intervention effectiveness, such that an RCT is considered more robust evidence than a quasi-experimental study and so on, the ‘level of evidence’ categorisation does not give any information about the quality or findings of an individual study. The percentage representation of each study design is shown in Figure 7.
Table 6.
Study design categories.
| Study design | Description |
|---|---|
| Randomised controlled trial (RCT) | Participants are fully randomly assigned to groups; an intervention group and a comparison or control group. |
| Quasi-experimental | Participants are not fully randomly assigned to intervention or control groups. |
| Studies meeting indicative level criteria | Case-series that use one of the following
approaches: 1. Control and targeted items are measured in a before and after intervention design. 2. Standardised assessments are used as comparison and control measure in a before and after design. AND one of the following research designs: 1. A case series with a multiple baseline design- in which the intervention is staggered, for example all participants have an initial baseline assessment completed, then they all begin their therapy at different times. 2. A matched control group is used in a group comparison (sample size large enough to calculate an effect size). |
| Other study | Studies that do not meet the criteria for an indicative level study. For example, case studies and case series studies that do not use a matched control group. |
Figure 7.
Frequency for each study design.
Fidelity, generalisation and follow-up
Excluding protocols (n = 4), 53.13% of studies reported some measure of treatment fidelity, while 28.09% (n = 109) reported a generalisation phase, and 39.18% (n = 152) reported longer term follow up after the immediate post-intervention measurement, eight of these studies were separate papers reporting a follow-up study from an earlier intervention, the rest report follow-up in the same paper.
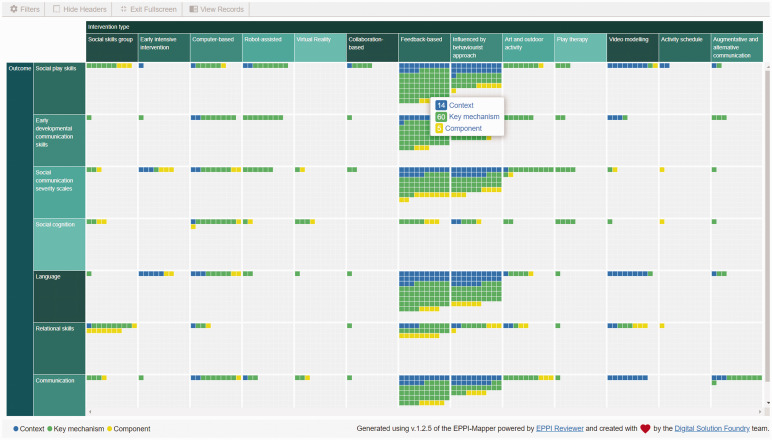
Evidence gap maps (EGMs)
Readers are strongly encouraged to explore the interactive, online EGMs (https://eppi.ioe.ac.uk/cms/Default.aspx?tabid=3787). This will allow users to investigate the features of an intervention of interest, for example if it is child-led, guided or adult-led play, or whether or not it is linked to behaviourist methods. The screenshot in Figure 8 gives an example:
Figure 8.
Screenshot of an Evidence Gap Map (EGM).
The small boxes each represent a study and, in this case, they are coloured according to the role of play code. So in the example screenshot we can see that the role of play in feedback-based interventions targeting social play skills tends to be that of a key mechanism.
Discussion
Conceptualising play-based interventions
The major contribution of the present paper is to summarise the heterogenous literature on the role of play in social and communication interventions in a way that has stakeholder relevance. The conceptualisation of the role of play within such interventions as falling within 3 broad categories of ‘context’, ‘component’ or a ‘key mechanism’ will support practitioners in reflections about their own views and practices regarding play. This approach reflects the theoretical and empirical play literature that asks questions about exactly how play activities or playful engagement might promote child development (Gibson, Fink, et al., 2020; Godin et al., 2019a; Hopkins et al., 2015; Luckett et al., 2007), as well as the literature that emphasises environmental adaptation, or ‘context-based’ therapies (Bundy et al., 2009, 2017).
Likewise, the ‘level of child control’ categories resonate with the literature on developmentalist strategies for intervention and debates around the role of guided-play vs direct instruction (Weisberg et al., 2016). The present review found that feedback-based approaches most frequently employ play as a key mechanism and are likely to be child-led. Interestingly, technology-based approaches tended to be more adult-directed, perhaps requiring a greater level of adult control to facilitate their use. More naturalistic approaches to technology use in autism have shown that free-play may be associated with higher levels of social and co-operative behaviour (Francis et al., 2019), so it is interesting to note that such approaches have not yet translated into intervention research.
The stakeholder consultation was also helpful in informing our approach to developing these two dimensions for scoping the literature. We found that play-based interventions were generally acceptable to practitioners, autistic people and the families of autistic people, although some concerns were raised from autistic individuals about the need to think carefully regarding bringing special interests into therapies and to consider the importance of autonomy. This chimes with Fletcher-Watson’s finding of a positive view of early intervention support (Fletcher-Watson et al., 2017). We hope that by reflecting on the extent to which their intervention practices are child-led and the different ways in which play underpins an intervention approach, practitioners can help autistic children and their families to make informed choices.
Types of play-based interventions
Categories for intervention types were developed reflecting the main intervention approaches that we judged would be of clinical interest. Furthermore, as some autistic stakeholders mentioned that they would be concerned about play-based therapies masking an underlying Applied Behaviour Analysis (ABA) approach, and some parents of autistic children wanted more information about ABA therapies, we also factored in information about the underlying philosophy, where this could be discerned. It is worth noting that this is not always self-evident. For example in the broader literature parent feedback models have been developed from both operant conditioning (Brookman-Frazee et al., 2006) and attachment theory perspectives (Juffer et al., 2017). In the present review, feedback approaches were one of the most common intervention types and were largely based on more naturalistic behaviourist approaches (e.g. Early Start Denver Model (ESDM)), or neuroconstructivist models (e.g. Pre-school Autism Communication Trial (PACT)). Although feedback-based approaches were mainly based on parenting interventions, there is also an emerging literature concerning peer feedback, including friends and siblings.
We also identified intervention types that are more likely to be carried out by practitioners based in schools, such as social skills groups, interest-based activity groups (e.g. music, drama) or collaborative play (e.g. LEGO-based therapy). These reflect the increasingly important role of peers in children’s learning and development as they move into the primary school years (Howe, 2009), and a move away from seeing play as a key developmental mechanism toward more of a learning context as children get older. We did not find any play-based interventions targeting social and communication outcomes that were explicitly strengths-based, by which we mean interventions acknowledging and celebrating autistic individuality in play and building on personalized preferences and contexts of play, or which view peer-peer interventions between autistic individuals as a deliberate strategy for supporting autistic communication styles (as contrasted with incidental groupings, e.g. due to school placement). This could be an interesting avenue for future play interventions, given recent findings of enhanced communication between autistic/autistic pairs, compared to autistic/non-autistic pairs (Crompton et al., 2020) and calls for strengths-based approaches from autism research organisations internationally (Huntley et al., 2019).
Having discussed the broader parameters used to scope the literature, we turn to discussion of more specific aspects of the studies reviewed, beginning with study design.
Study design
Just 21% of the included studies used an RCT design, which is typically considered the most robust way to test intervention efficacy3 (Greenhalgh, 2014). Quasi-experimental designs, using a control group but with no random allocation, accounted for a further 17%, meaning most included studies used designs that cannot provide conclusive or convincing evidence of clinical efficacy. Thus, we can conclude that the current evidence base is limited, even though we did not specifically evaluate effect-sizes/outcomes.
The lack of robust intervention studies may be because play-based interventions are a relatively new type of 'complex intervention' requiring extensive, iterative development and testing before they are worth the expense of a large trial and can be effectively taken to scale (O’Cathain et al., 2019). Choosing a study design that fits the state of knowledge in the discipline and addresses ethical or pragmatic concerns is entirely appropriate in a field in its early stages. Robot-based and computer-based interventions are good examples of approaches at an early stage. Papers classed as ‘other’ or ‘indicative’ for these types of interventions often include discussion of the development process and stakeholder consultation, important features of inclusive research (Fletcher-Watson et al., 2018).
On the other hand, it is concerning that more than half of the included studies had 10 or fewer participants, and 43% had fewer than six participants. While case-studies, case-series and small-scale observational work can provide an important foundation for intervention research, the field needs to consolidate and scale-up research efforts if widely implementable evidence-based interventions are the ultimate ambition.
Participants
Reporting of participant characteristics was piecemeal. While all studies included autistic participants, just 14% report co-occurring conditions. This is in contrast with reports of a high frequency of co-occurring conditions in the literature. In line with many other autism-related studies, girls were also under-represented despite having a potentially different social phenotype (Van Wijngaarden-Cremers et al., 2014).
Agent of intervention and outcomes
Practitioners from many backgrounds have been creative in finding ways to use play to support autistic children facing challenges in communication and social interaction. We were surprised by the relatively low number of Occupational Therapy interventions, given that the field has a long-standing tradition of play-based intervention, and also by the relative scarcity of Speech and Language Therapy studies, given the focus on communication-based outcomes in the present review. Overall, the data highlight the importance of multi-disciplinary approaches in this field (Strunk et al., 2017). Congruent with a multi-disciplinary approach, we also found that play-based interventions frequently target multiple outcomes – an approach that makes sense given the pervasive nature of social communication difficulties in autism. Social play skills were the largest single type of outcome target, measured in 16.5% of studies. This ties in with the increasing recognition that play is a crucial tool for supporting learning and development, particularly in social domains (Toseeb et al., 2020; Weisberg et al., 2013; Whitebread et al., 2009). Language development and early communication skills development were also popular as intervention targets, particularly for studies using feedback and/or behaviourist influenced approaches.
The distinction between those studies which use play as a medium for interventions targeting other outcomes, and those which target social play skills as an outcome per se, will be useful to consider when making decisions about which play-based interventions to support in future research.
Strengths and limitations
This review synthesises evidence from across a wide range of play-based interventions, allowing practitioners to position their own intervention approaches within a broader context and highlighting features of interventions that can inform clinical decision making. Furthermore, use of a pre-registered design and independent inter-rater reliability for key codes demonstrates a rigorous approach. Nevertheless, it is important to consider limitations. Firstly, due to resource constraints, we have not been able to search the grey literature and therefore could have missed important new approaches. Relatedly, we acknowledge that our criteria for selection of the 19 ‘named interventions’ is somewhat arbitrary, being based on our clinical judgement rather than an independent criterion. Readers should consult the EGMs and supplemental materials if they wish to make their own judgement. Secondly, we have not included quality appraisals or outcome syntheses, meaning that questions of intervention efficacy cannot be addressed. While this is an omission in-keeping with the decision to use scoping review methods, effectiveness data would be an important next-step for evidence synthesis in this area. Readers could refer to existing meta-analyses on early intervention for some insight into evidence of efficacy (e.g. Sandbank et al., 2020). Finally, due to the extent and variation of specific outcome measures used in autism research and clinical practice, we have not reported the exact measurement tools that studies used within these domains. An excellent review of outcome measurement tools can be found in this comprehensive report by McConachie and colleagues (McConachie et al., 2015).
Conclusions and clinical implications
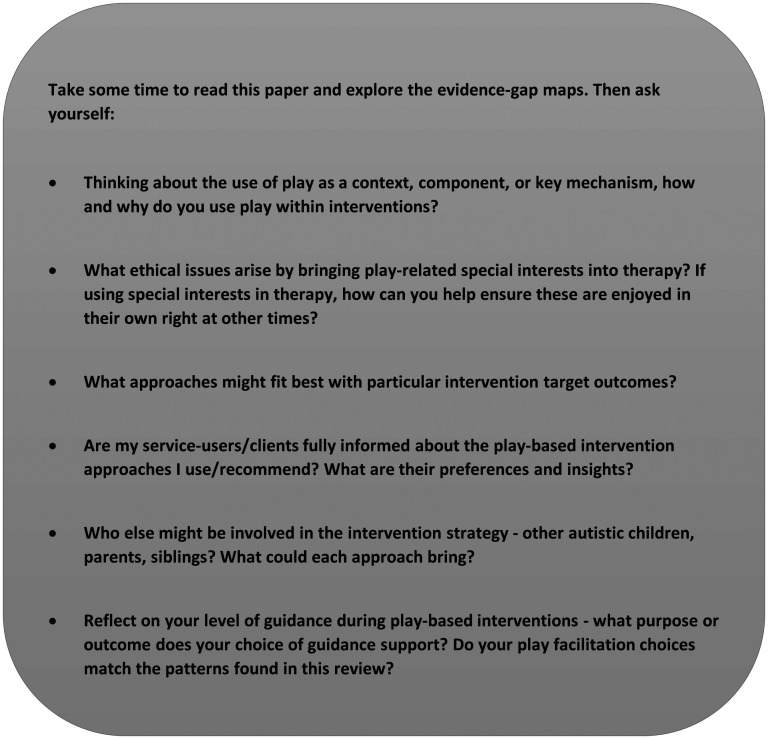
Regarding clinical implications, the conceptual framework proposed in this review can help practitioners appraise the literature and aid their advice to families when making shared intervention decisions. The observation that studies shift from play being used as a key developmental mechanism to a learning context as children get older warrants further exploration in research, when considering the public involvement feedback around the importance of play for supporting communication and friendships. Figure 9 contains some reflection and discussion prompts for practitioners to support engagement with the findings of this review.
Figure 9.
Prompts for practitioner reflection and discussion.
The stakeholder consultation and review findings reveal important dimensions for appraisal of play-based interventions, including the role of play, the underpinning philosophy (e.g. behaviourist or developmental), the role of the practitioner (providing parent feedback, 1:1 intervention, group facilitation), and the involvement of others in implementation of play-based approaches.
The wide range of approaches uncovered by this review is a testament to the wonderful diversity inherent to both play and autism. However, future research could usefully focus on consolidating the evidence base for existing play-based interventions, as the overall impression is that evidence is sparse and tending to lack robust methods. The field would also benefit from greater attention to diversity of sampling, making sure to include girls and minority background individuals, and to conduct studies in a wider range of countries from more diverse socio-economic contexts.
Supplemental Material
Supplemental material, sj-pdf-1-dli-10.1177_23969415211015840 for Play-based interventions to support social and communication development in autistic children aged 2–8 years: A scoping review by Jenny L Gibson, Emma Pritchard and Carmen de Lemos in Autism & Developmental Language Impairments
Acknowledgements
We thank Angela Cutts and the team at the Everton Library, and Isla Kuhn and the team at the Medical Library for invaluable support, advice, and peer review. Thanks to the EPPI reviewer team for their support and patience.
Notes
DTT is a teaching method often used as part of Applied Behaviour Analysis (ABA). Skills are broken down into small steps that are repeatedly ‘drilled’ in individual trials until the skill is mastered. DTT often involves the use of a reward or reinforcer after each correct trial.
Protocols cannot be coded for participant characteristics so we report results as a proportion of 384, rather than 388, studies.
Meta-analyses were not included.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: This study is funded by LEGO Foundation and therefore the authors declare a potential conflict of interest due to the inclusion of studies of LEGO-based therapy in this review. This paper is included in the special collection co-edited by author JG. It was peer reviewed via an independent editorial process, separate from that of the special collection.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: We gratefully acknowledge funding from LEGO Foundation.
ORCID iDs: Jenny L Gibson https://orcid.org/0000-0002-6172-6265
Emma Pritchard https://orcid.org/0000-0002-1967-4609
Carmen de Lemos https://orcid.org/0000-0001-5352-9432
Supplemental Material: Supplemental material for this article is available online.
References
- Aldred C., Green J., Emsley R., McConachie H. (2012). Brief report: Mediation of treatment effect in a communication intervention for pre-school children with autism. Journal of Autism and Developmental Disorders, 42(3), 447–454. [DOI] [PubMed] [Google Scholar]
- Almirall D., DiStefano C., Chang Y.-C., Shire S., Kaiser A., Lu Xi., Nahum-Shani I., Landa R., Mathy P., Kasari C. (2016). Longitudinal effects of adaptive interventions with a speech-generating device in minimally verbal children with ASD. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 45(4), 442–456. 10.1080/15374416.2016.1138407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alquraini T., Al-Odaib A., Al-Dhalaan H., Merza H., Mahoney G. (2018). Feasibility of responsive teaching with mothers and young children with autism in Saudi Arabia. Journal of Early Intervention, 40(4), 304–316. 10.1177/1053815118789176 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders : DSM-5. 10.1176/appi.books.9780890425596.744053 [DOI]
- Autistica. (n.. d.). Autistica research priorities.
- Barber A. B., Saffo R. W, Gilpin A. T., Craft L. D., Goldstein H. (2016). Peers as clinicians: Examining the impact of Stay Play Talk on social communication in young preschoolers with autism. Journal of Communication Disorders, 59, 1–15. 10.1016/j.jcomdis.2015.06.009 [DOI] [PubMed] [Google Scholar]
- Berman S., Ventola P., Gordon I. (2018). Improvements in micro level indices of social communication following Pivotal Response Treatment (PRT). Research in Autism Spectrum Disorders, 51, 56–65. 10.1016/j.rasd.2018.04.003 [DOI] [Google Scholar]
- Boudreau A. M., Lucyshyn J. M., Corkum P., Meko K., Smith I. M. (2019). Peer-mediated pivotal response treatment at school for children with autism spectrum disorder. Canadian Journal of School Psychology. 10.1177/0829573519870923 [DOI] [Google Scholar]
- Boyd B. A, Watson L. R., Reszka S. S., Sideris J., Alessandri M., Baranek G. T., Crais E. R., Donaldson A., Gutierrez A., Johnson L., Belardi K. (2018). Efficacy of the ASAP intervention for preschoolers with ASD: A cluster randomized controlled trial. Journal of Autism and Developmental Disorders, 48(9), 3144–3162. [DOI] [PubMed] [Google Scholar]
- Boutot E. A., Guenther T., Crozier S. (2005). Let’s play: Teaching play skills to young children with autism. Education and Training in Developmental Disabilities, 40, 285–292. [Google Scholar]
- Brian J. A., Smith I. M., Zwaigenbaum L., Bryson S. E. (2017). Cross-site randomized control trial of the social ABCs caregiver-mediated intervention for toddlers with autism spectrum disorder. Autism Research, 10(10), 1700–1711. 10.1002/aur.1818 [DOI] [PubMed] [Google Scholar]
- Brian J. A., Smith I. M., Zwaigenbaum L., Roberts W., Bryson S. E. (2016). The social ABCs caregiver-mediated intervention for toddlers with autism spectrum disorder: Feasibility, acceptability, and evidence of promise from a multisite study. Autism Research, 9(8), 899–912. 10.1002/aur.1582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookman-Frazee L., Stahmer A., Baker-Ericzén M. J., Tsai K. (2006). Parenting interventions for children with autism spectrum and disruptive behavior disorders: Opportunities for cross-fertilization. Clinical Child and Family Psychology Review, 9, 181–200. 10.1007/s10567-006-0010-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundy A. (2012). Children at play: Can I play too? In S. J. Lane &. A. C. Bundy (Eds.), Kids can be kids: a childhood occupations approach (pp. 28–43). F.A. Davis.
- Bundy A., Engelen L., Wyver S., Tranter P., Ragen J., Bauman A., Baur L., Schiller W., Simpson J. M., Niehues A. N., Perry G., Jessup G., Naughton G. (2017). Sydney playground project: A cluster-randomized trial to increase physical activity, play, and social skills. Journal of School Health, 87(10), 751–759. 10.1111/josh.12550 [DOI] [PubMed] [Google Scholar]
- Bundy A., Tranter P., Naughton G., Wyver S., Luckett T. (2009). Playfulness: Interactions between play contexts and child development (pp. 76–87). Oxford University Press. [Google Scholar]
- Byford S., Cary M., Barrett B., Aldred C. R., Charman T., Howlin P., Hudry K., Leadbitter K., Le Couteur A., McConachie H., Pickles A., Slonims V., Temple K. J., Green J., Bourne K., Blazey L., Holt C., Kapadia D., … The PACT Consortium. (2015). Cost-effectiveness analysis of a communication-focused therapy for pre-school children with autism: Results from a randomised controlled trial. BMC Psychiatry, 15(1). 10.1186/s12888-015-0700-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardon T. A., Wilcox M. J. (2011). Promoting imitation in young children with autism: A comparison of reciprocal imitation training and video modeling. Journal of Autism And Developmental Disorders, 41(5), 654–666. 10.1007/s10803-010-1086-8 [DOI] [PubMed] [Google Scholar]
- Carpente J. A. (2017). Investigating the effectiveness of a developmental, individual difference, relationship-based (DIR) improvisational music therapy program on social communication for children with autism spectrum disorder. Music Therapy Perspectives, 35(2), 160–174. 10.1093/mtp/miw013 [DOI] [Google Scholar]
- Chang Y. C., Quan J., Wood J. J. (2012). Effects of anxiety disorder severity on social functioning in children with autism spectrum disorders. Journal of Developmental and Physical Disabilities, 24, 235–245. 10.1007/s10882-012-9268-2 [DOI] [Google Scholar]
- Chang Y.-C., Shire S. Y., Shih W., Gelfand C., Kasari C. (2016). Preschool deployment of evidence-based social communication intervention: JASPER in the classroom. Journal of Autism and Developmental Disorders, 46(6), 2211–2223. 10.1007/s10803-016-2752-2 [DOI] [PubMed] [Google Scholar]
- Chiang C. H., Chu C. L., Lee T. C. (2016). Efficacy of caregiver-mediated joint engagement intervention for young children with autism spectrum disorders. Autism, 20(2), 172–182. 10.1177/1362361315575725 [DOI] [PubMed] [Google Scholar]
- Colombi C., Narzisi A., Ruta L., Cigala V., Gagliano A., Pioggia G., Siracusano R., Rogers S. J., Muratori F., & Prima Pietra Team. (2018). Implementation of the Early Start Denver Model in an Italian community. Autism, 22(2), 126–133. 10.1177/1362361316665792 [DOI] [PubMed] [Google Scholar]
- Coolican J., Smith I. M., Bryson S. E. (2010). Brief parent training in pivotal response treatment for preschoolers with autism. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(12), 1321–1330. 10.1111/j.1469-7610.2010.02326.x [DOI] [PubMed] [Google Scholar]
- Crompton C. J., Ropar D., Evans-Williams C. V., Flynn E. G., Fletcher-Watson S. (2020). Autistic peer-to-peer information transfer is highly effective. Autism, 24, 1704–1712. 10.1177/1362361320919286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G., Rogers S., Munson J., Smith M., Winter J., Greenson J., Donaldson A., Varley J. (2010). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics, 125(1), E17–E23. 10.1542/peds.2009-0958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond G., Ofek H., Aronson B., Viner-Ribke I., Dlugatch Y., Resnick E. (2015). Hybrid therapy for treatment of newly diagnosed toddlers with autism spectrum disorders. International Journal on Disability and Human Development, 2015. 10.1515/ijdhd-2015-0020 [DOI] [Google Scholar]
- DiStefano C., Shih W., Kaiser A., Landa R., Kasari C. (2016). Communication growth in minimally verbal children with ASD: The importance of interaction. Autism Research: Official Journal of the International Society for Autism Research, 9(10), 1093–1102. 10.1002/aur.1594 [DOI] [PubMed] [Google Scholar]
- Dykstra J. R., Boyd B. A, Watson L. R., Crais E. R., Baranek G. T. (2012). The impact of the Advancing Social-communication And Play (ASAP) intervention on preschoolers with autism spectrum disorder. Autism: The International Journal of Research & Practice, 16(1), 27–44. [DOI] [PubMed] [Google Scholar]
- Eapen V., Crnčec R., Walter A. (2013). Clinical outcomes of an early intervention program for preschool children with autism spectrum disorder in a community group setting. BMC Pediatrics, 13(1), 3. 10.1186/1471-2431-13-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A., Munson J., Rogers S. J., Greenson J., Winter J., Dawson G. (2015). Long-term outcomes of early intervention in 6-year-old children with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 54(7), 580–587. 10.1016/j.jaac.2015.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink E., Mareva S., Gibson J. L. (2020). Dispositional playfulness in young children: A cross-sectional and longitudinal examination of the psychometric properties of a new child self-reported playfulness scale and associations with social behaviour. Infant and Child Development, 29(4), e2181. 10.1002/icd.2181 [DOI] [Google Scholar]
- Fletcher-Watson S., Adams J., Brook K., Charman T., Crane L., Cusack J., Leekam, S., Milton, D., Parr, J., & Pellicano E. (2018). Making the future together: Shaping autism research through meaningful participation. Autism. 10.1177/1362361318786721 [DOI] [PMC free article] [PubMed]
- Fletcher-Watson S., Apicella F., Auyeung B., Beranova S., Bonnet-Brilhault F., Canal-Bedia R., Charman, T., Chericoni, N., Conceição, I. C., Davies, K., Farroni, T., Gomot, M., Jones, E., Kaale, A., Kapica, K., Kawa, R., Kylliäinen, A., Larsen, K., Lefort-besnard, J. … Yirmiya N. (2017). Attitudes of the autism community to early autism research. Autism, 21(1), 61–74. 10.1177/1362361315626577 [DOI] [PubMed]
- Fossum K. L., Williams L., Garon N., Bryson S. E., Smith I. M. (2018). Pivotal response treatment for preschoolers with autism spectrum disorder: Defining a predictor profile. Autism Research, 11(1), 153–165. 10.1002/aur.1859 [DOI] [PubMed] [Google Scholar]
- Francis G. A., Farr W., Mareva S., Gibson J. L. (2019). Do tangible user interfaces promote social behaviour during free play? A comparison of autistic and typically-developing children playing with passive and digital construction toys. Research in Autism Spectrum Disorders, 58, 68–82. 10.1016/j.rasd.2018.08.005 [DOI] [Google Scholar]
- Freitag C. M., Feineis-Matthews S., Valerian J., Teufel K., Wilker C. (2012). The Frankfurt early intervention program FFIP for preschool aged children with autism spectrum disorder: A pilot study. Journal of Neural Transmission, 119(9), 1011–1021. 10.1007/s00702-012-0792-0 [DOI] [PubMed] [Google Scholar]
- Fulton E., Eapen V., Crncec R., Walter A., Rogers S. (2014). Reducing maladaptive behaviors in preschool-aged children with autism spectrum disorder using the Early Start Denver Model. Frontiers In Pediatrics, 2. 10.3389/fped.2014.00040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gengoux G. W., Abrams D. A., Schuck R., Millan M. E., Libove R., Ardel C. M., Phillips J. M., Fox M., Frazier T. W., Hardan A. Y. (2019). A pivotal response treatment package for children with autism spectrum disorder: An RCT. Pediatrics, 144(3). 10.1542/peds.2019-0178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geoffray M.-M., Denis A., Mengarelli F., Peter C., Gallifet N., Beaujeard V., Grosmaitre C. J., Malo V., Grisi S., Georgieff N., Magnificat S., Touzet S. (2019). Using ESDM 12 hours per week in children with autism spectrum disorder: Feasibility and results of an observational study. Psychiatria Danubina, 31(3), 333–339. 10.24869/psyd.2019.333 [DOI] [PubMed] [Google Scholar]
- Gibson J. L., de Lemos C., Pritchard E. J. (2020). Exploring the experience of autistic play: An interpretative phenomenological analysis [OSF Registered Report]. 10.17605/OSF.IO/E8UVH [DOI]
- Gibson J. L., Fink E., Torres P. E., Browne W. V., Mareva S. (2020). Making sense of social pretense: the effect of the dyad, sex, and language ability in a large observational study of children’s behaviors in a social pretend play context. Social Development, 29, 526–543. 10.1111/sode.12420 [DOI] [Google Scholar]
- Gibson J. L., Hussain J., Holsgrove S., Adams C., Green J. (2011). Quantifying peer interactions for research and clinical use: The Manchester inventory for playground observation. Research in Developmental Disabilities, 32, 2458–2466. [DOI] [PubMed] [Google Scholar]
- Godin J., Freeman A., Rigby P. (2019. a). Conceptual clarification of the playful engagement in social interaction of preschool-aged children with autism spectrum disorder (ASD). Early Child Development and Care, 189, 430–440. 10.1080/03004430.2017.1324437 [DOI] [Google Scholar]
- Godin J., Freeman A., Rigby P. (2019. b). Interventions to promote the playful engagement in social interaction of preschool-aged children with autism spectrum disorder (ASD): A scoping study. Early Child Development and Care, 189, 1666–1681. 10.1080/03004430.2017.1404999 [DOI] [Google Scholar]
- Gough D., Oliver S., Thomas J. (2017). An introduction to systematic reviews (2nd ed.). Sage Publications Ltd.
- Goods K. S., Ishijima E., Chang Y.-C., Kasari C. (2013). Preschool based JASPER intervention in minimally verbal children with autism: Pilot RCT. Journal of Autism and Developmental Disorders, 43(5), 1050–1056. 10.1007/s10803-012-1644-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J., Charman T., McConachie H., Aldred C., Slonims V., Howlin P., Le Couteur A., Leadbitter K., Hudry K., Byford S., Barrett B., Temple K., Macdonald W., Pickles A. (2010). Parent-mediated communication-focused treatment in children with autism (PACT): A randomised controlled trial. The Lancet, 375(9732), 2152–2160. 10.1016/S0140-6736(10)60587-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T. (2014). How to read a paper: The basics of evidence-based medicine (5th ed.). BMJ Books.
- Gulsrud A. C., Hellemann G. S., Freeman S. F. N., Kasari C. (2014). Two to ten years: Developmental trajectories of joint attention in children with ASD who received targeted social communication interventions. Autism Research, 7(2), 207–215. 10.1002/aur.1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Ruiz E. (2018). Music therapy and Early Start Denver Model to teach social communication strategies to parents of preschoolers with ASD: A feasibility study. Music Therapy Perspectives, 36(1), 26–39. 10.1093/mtp/mix018 [DOI] [Google Scholar]
- Holzinger D., Laister D., Vivanti G., Barbaresi W. J., Fellinger J. (2019). Feasibility and outcomes of the Early Start Denver Model implemented with low intensity in a community setting in Austria. Journal of Developmental and Behavioral Pediatrics, 40(5), 354–363. 10.1097/DBP.0000000000000675 [DOI] [PubMed] [Google Scholar]
- Hopkins E. J., Dore R. A., Lillard A. S. (2015). Do children learn from pretense. Journal of Experimental Child Psychology, 130, 1–18. 10.1016/j.jecp.2014.09.004 [DOI] [PubMed] [Google Scholar]
- Howe C. (2009). Peer groups and children’s development. Wiley. 10.1002/9781444318098 [DOI]
- Hu X., Zheng Q., Lee G. T. (2018). Using peer-mediated LEGO® play intervention to improve social interactions for Chinese children with autism in an inclusive setting. Journal of Autism and Developmental Disorders, 48(7), 2444–2457. [DOI] [PubMed] [Google Scholar]
- Huntley M., Black M. H., Jones M., Falkmer M., Lee E., Tan T., Picen T., Thompson M., New M., Heasman B., Smith E., Bölte S., Girdler S. (2019). Action briefing: Strengths-based approaches. Autistica. https://www.autistica.org.uk/downloads/files/FINAL-Strengths-Based-Approaches-ActionBriefing.pdf [Google Scholar]
- Huskens B., Palmen A., Van der Werff M., Lourens T., Barakova E. (2015). Improving collaborative play between children with autism spectrum disorders and their siblings: The effectiveness of a robot-mediated intervention based on Lego® therapy. Journal of Autism and Developmental Disorders, 45(11), 3746–3755. [DOI] [PubMed] [Google Scholar]
- Ingersoll B. (2010). Brief report: Pilot randomized controlled trial of reciprocal imitation training for teaching elicited and spontaneous imitation to children with autism. Journal of Autism and Developmental Disorders, 40(9), 1154–1160. 10.1007/s10803-010-0966-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B. (2012). Brief report: Effect of a focused imitation intervention on social functioning in children with autism. Journal of Autism and Developmental Disorders, 42(8), 1768–1773. 10.1007/s10803-011-1423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B., Lalonde K. (2010). The impact of object and gesture imitation training on language use in children with autism spectrum disorder. Journal of Speech, Language, and Hearing Research, 53(4), 1040–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B., Wainer A. (2013. a). Initial efficacy of Project ImPACT: A parent-mediated social communication intervention for young children with ASD. Journal of Autism and Developmental Disorders, 43(12), 2943–2952. 10.1007/s10803-013-1840-9 [DOI] [PubMed] [Google Scholar]
- Ingersoll B. R., Wainer A. L. (2013. b). Pilot study of a school-based parent training program for preschoolers with ASD. Autism: The International Journal of Research and Practice, 17(4), 434–448. 10.1177/1362361311427155 [DOI] [PubMed] [Google Scholar]
- Ingersoll B. R., Wainer A. L, Berger N. I., Walton K. M. (2017). Efficacy of low intensity, therapist-implemented Project ImPACT for increasing social communication skills in young children with ASD. Developmental Neurorehabilitation, 20(8), 502–510. 10.1080/17518423.2016.1278054 [DOI] [PubMed] [Google Scholar]
- Ingersoll B., Wainer A. L., Berger N. I., Pickard K. E., Bonter N. (2016). Comparison of a self-directed and therapist-assisted telehealth parent-mediated intervention for children with ASD: A pilot RCT. Journal of Autism and Developmental Disorders, 46(7), 2275–2284. [DOI] [PubMed] [Google Scholar]
- Jarrold C. (2003). A review of research into pretend play in autism. Autism, 7, 379–390. 10.1177/1362361303007004004 [DOI] [PubMed] [Google Scholar]
- Jones E. A. (2009). Establishing response and stimulus classes for initiating joint attention in children with Autism. Research in Autism Spectrum Disorders, 3(2), 375–389. 10.1016/j.rasd.2008.08.004 [DOI] [Google Scholar]
- Juffer F., Struis E., Werner C., Bakermans-Kranenburg M. J. (2017). Effective preventive interventions to support parents of young children: Illustrations from the video-feedback intervention to promote positive parenting and sensitive discipline (VIPP-SD). Journal of Prevention & Intervention in the Community, 45, 202–214. 10.1080/10852352.2016.1198128 [DOI] [PubMed] [Google Scholar]
- Kaale A., Fagerland M. W., Martinsen E. W., Smith L. (2014). Preschool-based social communication treatment for children with autism: 12-month follow-up of a randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(2), 188–198. 10.1016/j.jaac.2013.09.019 [DOI] [PubMed] [Google Scholar]
- Kaale A., Smith L., Sponheim E. (2012). A randomized controlled trial of preschool-based joint attention intervention for children with autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 53(1), 97–105. 10.1111/j.1469-7610.2011.02450.x [DOI] [PubMed] [Google Scholar]
- Karakosta E., Dautenhahn K., Syrdal D. S., Wood L. J., Robins B. (2019). Using the humanoid robot Kaspar in a Greek school environment to support children with Autism Spectrum Condition. Paladyn, 10(1), 298–317. 10.1515/pjbr-2019-0021 [DOI] [Google Scholar]
- Kasari C., Lawton K., Shih W., Barker T. V., Landa R., Lord C., Orlich F., King B., Wetherby A., Senturk D. (2014). Caregiver-mediated intervention for low-resourced preschoolers with autism: An RCT. Pediatrics, 134(1), e72–e79. 10.1542/peds.2013-3229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C., Gulsrud A. C., Wong C., Kwon S., Locke J. (2010). Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. Journal of Autism and Developmental Disorders, 40(9), 1045–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C., Gulsrud A., Freeman S., Paparella T., Hellemann G. (2012). Longitudinal follow-up of children with autism receiving targeted interventions on joint attention and play. Journal of the American Academy of Child and Adolescent Psychiatry, 51(5), 487–495. 10.1016/j.jaac.2012.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C., Gulsrud A., Paparella T., Hellemann G., Berry K. (2015). Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. Journal of Consulting and Clinical Psychology, 83(3), 554–563. 10.1037/a0039080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari C., Kaiser A., Goods K., Nietfeld J., Mathy P., Landa R., Murphy S., Almirall D. (2014). Communication interventions for minimally verbal children with autism: A sequential multiple assignment randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(6), 635–646. 10.1016/j.jaac.2014.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent C., Cordier R., Joosten A., Wilkes-Gillan S., Bundy A., Speyer R. (2020). A systematic review and meta-analysis of interventions to improve play skills in children with autism spectrum disorder. Review Journal of Autism and Developmental Disorders, 7, 91–118. 10.1007/s40489-019-00181-y [DOI] [Google Scholar]
- Kim S. (2019). Pivotal response treatment for prompting social behaviors of Korean American children with autism. Exceptionality, 27(1), 47–64. 10.1080/09362835.2017.1359606 [DOI] [Google Scholar]
- Kitzerow J., Teufel K., Jensen K., Wilker C., Freitag C. M. (2019). Case-control study of the low intensive autism-specific early behavioral intervention A-FFIP: Outcome after one year. Zeitschrift Für Kinder- Und Jugendpsychiatrie Und Psychotherapie. https://econtent.hogrefe.com/doi/10.1024/1422-4917/a000661 [DOI] [PubMed] [Google Scholar]
- Kitzerow J., Wilker C., Teufel K., Soll S., Schneider M., Westerwald E., Sachse M., Marinovic V., Berndt K., Valerian J., Feineis-Matthews S., Freitag C. M. (2014). Frankfurt Early Intervention Program (FFIP) for preschoolers with autism spectrum disorders (ASD): First results for language development. Kindheit und Entwicklung, 23(1), 34–41. 10.1026/0942-5403/a000133 [DOI] [Google Scholar]
- Koegel R. L., Bradshaw J. L., Ashbaugh K., Koegel L. K. (2014). Improving question-asking initiations in young children with autism using pivotal response treatment. Journal of Autism and Developmental Disorders, 44(4), 816–827. 10.1007/s10803-013-1932-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong M. M.-Y., Au T. K.-F. (2018). The incredible years parent program for Chinese preschoolers with developmental disabilities. Early Education and Development, 29(4), 494–514. 10.1080/10409289.2018.1461987 [DOI] [Google Scholar]
- Kossyvaki L., Papoudi D. (2016). A review of play interventions for children with autism at school. International Journal of Disability, Development and Education, 63, 45–63. 10.1080/1034912X.2015.1111303 [DOI] [Google Scholar]
- Kretzmann M., Shih W., Kasari C. (2015). Improving peer engagement of children with autism on the school playground: A randomized controlled trial. Behavior Therapy, 46(1), 20–28. 10.1016/j.beth.2014.03.006 [DOI] [PubMed] [Google Scholar]
- Kuhaneck H., Spitzer S. L., Bodison S. C. (2020). A systematic review of interventions to improve the occupation of play in children with autism. OTJR: Occupation, Participation and Health, 40, 83–98. 10.1177/1539449219880531 [DOI] [PubMed] [Google Scholar]
- Law J., Lee W., Roulstone S., Wren Y., Zeng B., Lindsay G. (2012). ‘ What works’: Interventions for children and young people with speech, language and communication needs. Department for Education. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/556912/DFE-RR247-BCRP10.pdf
- Lawton K., Kasari C. (2012. a). Brief report: Longitudinal improvements in the quality of joint attention in preschool children with autism. Journal of Autism and Developmental Disorders, 42(2), 307–312. 10.1007/s10803-011-1231-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton K., Kasari C. (2012. b). Teacher-implemented joint attention intervention: Pilot randomized controlled study for preschoolers with autism. Journal of Consulting and Clinical Psychology, 80(4), 687–693. 10.1037/a0028506 [DOI] [PubMed] [Google Scholar]
- Leadbitter K., Aldred C., McConachie H., Le Couteur A., Kapadia D., Charman T., Macdonald W., Salomone E., Emsley R., Green J., Barrett B., Barron S., Beggs K., Blazey L., Bourne K., Byford S., Cole-Fletcher R., Collino J., … The PACT Consortium. (2018). The Autism Family Experience Questionnaire (AFEQ): An ecologically-valid, parent-nominated measure of family experience, quality of life and prioritised outcomes for early intervention. Journal of Autism and Developmental Disorders, 48(4), 1052–1062. 10.1007/s10803-017-3350-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao S. T., Hwang Y. S., Chen Y. J., Lee P., Chen S. J., Lin L. Y. (2014). Home-based DIR/Floortime™ intervention program for preschool children with autism spectrum disorders: Preliminary findings. Physical and Occupational Therapy in Pediatrics, 34(4), 356–367. 10.3109/01942638.2014.918074 [DOI] [PubMed] [Google Scholar]
- Lindsay S., Hounsell K. G., Cassiani C. (2017). A scoping review of the role of LEGO® therapy for improving inclusion and social skills among children and youth with autism. Disability and Health Journal, 10, 173–182. 10.1016/j.dhjo.2016.10.010 [DOI] [PubMed] [Google Scholar]
- Locke J., Kang-Yi C., Pellecchia M., Mandell D. S. (2019). It’s messy but real: A pilot study of the implementation of a social engagement intervention for children with autism in schools. Journal of Research in Special Educational Needs, 19(2), 135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke J., Shih W., Kang-Yi C. D., Caramanico J., Shingledecker T., Gibson J., Frederick L., Mandell D. S. (2019). The impact of implementation support on the use of a social engagement intervention for children with autism in public schools. Autism, 23(4), 834–845. 10.1177/1362361318787802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C., Risi S., Lambrecht L., Cook E. H., Leventhal B. L., DiLavore P. C., Pickles, A., & Rutter M. (2000). The autism diagnostic observation schedule generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30, 205–223. 10.1023/A:1005592401947 [DOI] [PubMed] [Google Scholar]
- Lory C., Rispoli M., Gregori E. (2018). Play interventions involving children with autism spectrum disorder and typically developing peers: A review of research quality. Review Journal of Autism and Developmental Disorders, 5, 78–89. 10.1007/s40489-017-0124-2 [DOI] [Google Scholar]
- Luckett T., Bundy A., Roberts J. (2007). Do behavioural approaches teach children with autism to play or are they pretending? Autism, 11, 365–388. 10.1177/1362361307078135 [DOI] [PubMed] [Google Scholar]
- Magiati I., Tay X. W., Howlin P. (2014). Cognitive, language, social and behavioural outcomes in adults with autism spectrum disorders: A systematic review of longitudinal follow-up studies in adulthood. Clinical Psychology Review, 34, 73–86. 10.1016/j.cpr.2013.11.002 [DOI] [PubMed] [Google Scholar]
- Mahoney G., Wiggers B., Nam S., Kralovic S., Perales F. (2014). How depressive symptomatology of mothers of children with pervasive developmental disorders relates to their participation in relationship focused intervention. International Journal of Early Childhood Special Education, 6(2), 204–221. 10.20489/intjecse.86233 [DOI] [Google Scholar]
- Mahoney G., Solomon R. (2016). Mechanism of developmental change in the PLAY Project Home Consultation Program: Evidence from a randomized control trial. Journal of Autism and Developmental Disorders, 46(5), 1860–1871. 10.1007/s10803-016-2720-x [DOI] [PubMed] [Google Scholar]
- Maich K., Hall C. L., van Rhijn T. M., Squires K. (2018). Investigating Stay, Play, & Talk: A peer-mediated social skills intervention for young children with autism spectrum disorder and other social challenges. Exceptionality Education International, 28(2), 82–104. [Google Scholar]
- Matsuzaki A., Yamamoto J. (2012). Effects of an early intervention program on preverbal communication in a child with autism: Developmental and behavioral analysis with a multiple-baseline design. Japanese Journal of Special Education, 49(6), 657–669. 10.6033/tokkyou.49.657 [DOI] [Google Scholar]
- McConachie H., Parr J. R., Glod M., Hanratty J., Livingstone N., Oono I. P., Robalino, S., Baird, G., Beresford, B., Charman, T., Garland, D., Green, J., Gringras, P., Jones, G., Law, J., Le Couteur, A. S., Macdonald, G., McColl, E. M., Morris, C., … Williams, K. (2015). Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technology Assessment, 19, 1–538. 10.3310/hta19410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan J., Sampson M., Salzwedel D. M., Cogo E., Foerster V., Lefebvre C. (2016). PRESS peer review of electronic search strategies: 2015 guideline statement. Journal of Clinical Epidemiology, 75, 40–46. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- Mengoni S. E., Irvine K., Thakur D., Barton G., Dautenhahn K., Guldberg K., Robins B., Wellsted D., Sharma S. (2017). Feasibility study of a randomised controlled trial to investigate the effectiveness of using a humanoid robot to improve the social skills of children with autism spectrum disorder (Kaspar RCT): A study protocol. BMJ Open, 7(6), e017376. 10.1136/bmjopen-2017-017376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller L. J. (2017). Creating a common terminology for play behavior to increase cross-disciplinary research. Learning & Behavior, 45, 330–334. 10.3758/s13420-017-0286-x [DOI] [PubMed] [Google Scholar]
- Mohammadzaheri F., Koegel L. K., Rezaee M., Rafiee S. M. (2014). A randomized clinical trial comparison between Pivotal Response Treatment (PRT) and Structured Applied Behavior Analysis (ABA) intervention for children with autism. Journal of Autism and Developmental Disorders, 44(11), 2769–2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn Z., Peters M. D. J., Stern C., Tufanaru C., McArthur A., Aromataris E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy S., Joffe V., Messer D., Crafter S., Radley J., Sunthararajah S., Bell, K., Corbacho, B., Fairhurst, C., Rodgers, S., Torgerson, D., & Welch, C. (2019). Evaluating “enhancing pragmatic language skills for young children with social communication impairments” (E-PLAYS): Protocol for a feasibility randomised controlled trial study. Pilot and Feasibility Studies, 5, 75. 10.1186/s40814-019-0456-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Cathain A., Croot L., Duncan E., Rousseau N., Sworn K., Turner K. M., Yardley, L., & Hoddinott P. (2019). Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open, 9, e029954. 10.1136/bmjopen-2019-029954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor C., Stagnitti K. (2011). Play, behaviour, language and social skills: {The} comparison of a play and a non-play intervention within a specialist school setting. Research in Developmental Disabilities, 32, 1205–1211. 10.1016/j.ridd.2010.12.037 [DOI] [PubMed] [Google Scholar]
- Pang Y. (2010). Lego games help young children with autism develop social skills. International Journal of Education, 2(2), e7. [Google Scholar]
- Penney A., Schwartz I. (2019). Effects of coaching on the fidelity of parent implementation of reciprocal imitation training. Autism: The International Journal of Research & Practice, 23(6), 1497–1507. [DOI] [PubMed] [Google Scholar]
- Peters M. D. J., Godfrey C. M., Khalil H., McInerney P., Parker D., Soares C. B. (2015). Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare, 13, 141–146. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Pickles A., Le Couteur A., Leadbitter K., Salomone E., Cole-Fletcher R., Tobin H., Gammer I., Lowry J., Vamvakas G., Byford S., Aldred C., Slonims V., McConachie H., Howlin P., Parr J. R., Charman T., Green J. (2016). Parent-mediated social communication therapy for young children with autism (PACT): Long-term follow-up of a randomised controlled trial. The Lancet, 388(10059), 2501–2509. 10.1016/S0140-6736(16)31229-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn S., Donnelly S., Kidd E. (2018). The relationship between symbolic play and language acquisition: A meta-analytic review. Developmental Review, 49, 121–135. 10.1016/j.dr.2018.05.005 [DOI] [Google Scholar]
- Radley K. C., Ford W. B., Battaglia A. A., McHugh M. B. (2014). The effects of a social skills training package on social engagement of children with autism spectrum disorders in a generalized recess setting. Focus on Autism and Other Developmental Disabilities, 29, 216–229. 10.1177/1088357614525660 [DOI] [Google Scholar]
- Radley K. C., Dart E. H., Helbig K. A., Schrieber S. R., Ware M. E. (2019). An evaluation of the additive effects of lag schedules of reinforcement. Developmental Neurorehabilitation, 22(3), 180–191. 10.1080/17518423.2018.1523242 [DOI] [PubMed] [Google Scholar]
- Radley K. C., Dart E. H., Moore J. W., Lum J. D. K., Pasqua J. (2017). Enhancing appropriate and variable responding in young children with autism spectrum disorder. Developmental Neurorehabilitation, 20(8), 538–548. 10.1080/17518423.2017.1323973 [DOI] [PubMed] [Google Scholar]
- Radley K. C., Hanglein J., Arak M. (2016). School-based social skills training for preschool-age children with autism spectrum disorder. Autism, 20(8), 938–951. 10.1177/1362361315617361 [DOI] [PubMed] [Google Scholar]
- Radley K. C., Jenson W. R., Clark E., Hood J. A., Nicholas P. (2014). Using a multimedia social skills intervention to increase social engagement of young children with autism spectrum disorder. Intervention in School and Clinic, 50(1), 22–28. [Google Scholar]
- Radley K. C., Jenson W. R., Clark E., O’Neill R. E. (2014). The feasibility and effects of a parent-facilitated social skills training program on social engagement of children with autism spectrum disorders. Psychology in the Schools, 51(3), 241–255. 10.1002/pits.21749 [DOI] [Google Scholar]
- Radley K. C., O’Handley R. D., Battaglia A. A., Lum J. D. K, Dadakhodjaeva K., Ford W. B., McHugh M. B. (2017). Effects of a social skills intervention on children with autism spectrum disorder and peers with shared deficits. Education and Treatment of Children, 40(2), 233–262. [Google Scholar]
- Rai D., Culpin I., Heuvelman H., Magnusson C. M. K., Carpenter P., Jones H. J., Emond, A. M., Zammit, S., Golding, J., & Pearson, R. M. (2018). Association of autistic traits with depression from childhood to age 18 years. JAMA Psychiatry, 75, 835–843. 10.1001/jamapsychiatry.2018.1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randolph J. K., Stichter J. P., Schmidt C. T., O’Connor K. V. (2011). Fidelity and effectiveness of PRT implemented by caregivers without college degrees. Focus on Autism and Other Developmental Disabilities, 26(4), 230–238. [Google Scholar]
- Reis H. I. S., Pereira A. P. S., Almeida L. S. (2018). Intervention effects on communication skills and sensory regulation on children with ASD. Journal of Occupational Therapy Schools and Early Intervention, 11(3), 346–359. 10.1080/19411243.2018.1455552 [DOI] [Google Scholar]
- Rieth S. R., Stahmer A. C., Suhrheinrich J., Schreibman L., Kennedy J., Ross B. (2014). Identifying critical elements of treatment: Examining the use of turn taking in autism intervention. Focus on Autism and Other Developmental Disabilities, 29(3), 168–179. 10.1177/1088357613513792 [DOI] [Google Scholar]
- Rogers S. J., Estes A., Vismara L., Munson J., Zierhut C., Greenson J., Dawson G., Rocha M., Sugar C., Senturk D., Whelan F., Talbott M. (2019). Enhancing low-intensity coaching in parent implemented Early Start Denver Model intervention for early autism: A randomized comparison treatment trial. Journal of Autism and Developmental Disorders, 49(2), 632–646. [DOI] [PubMed] [Google Scholar]
- Sandbank M., Bottema-Beutel K., Crowley S., Cassidy M., Feldman J. I., Canihuante M., Woynaroski T. (2020). Intervention effects on language in children with autism: A project AIM meta-analysis. Journal of Speech, Language, and Hearing Research, 63, 1537–1560. 10.1044/2020_JSLHR-19-00167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreibman L., Stahmer A. C., Barlett V. C., Dufek S. (2009). Brief report: Toward refinement of a predictive behavioral profile for treatment outcome in children with autism. Research in Autism Spectrum Disorders, 3(1), 163–172. 10.1016/j.rasd.2008.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreibman L., Stahmer A. C. (2014). A randomized trial comparison of the effects of verbal and pictorial naturalistic communication strategies on spoken language for young children with autism. Journal of Autism and Developmental Disorders, 44(5), 1244–1251. 10.1007/s10803-013-1972-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih W., Dean M., Kretzmann M., Locke J., Senturk D., Mandell D. S., Smith T., Kasari C. (2019). Remaking recess intervention for improving peer interactions at school for children with autism spectrum disorder: Multisite randomized trial. School Psychology Review, 48(2), 133–144. [Google Scholar]
- Shire S. Y., Chang Y.-C., Shih W., Bracaglia S., Kodjoe M., Kasari C. (2017). Hybrid implementation model of community-partnered early intervention for toddlers with autism: A randomized trial. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 58(5), 612–622. 10.1111/jcpp.12672 [DOI] [PubMed] [Google Scholar]
- Shire S. Y., Goods K., Shih W., Distefano C., Kaiser A., Wright C., Mathy P., Landa R., Kasari C. (2015). Parents’ adoption of social communication intervention strategies: Families including children with autism spectrum disorder who are minimally verbal. Journal of Autism and Developmental Disorders, 45(6), 1712–1724. 10.1007/s10803-014-2329-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shire S. Y., Gulsrud A., Kasari C. (2016). Increasing responsive parent-child interactions and joint engagement: Comparing the influence of parent-mediated intervention and parent psychoeducation. Journal of Autism and Developmental Disorders, 46(5), 1737–1747. 10.1007/s10803-016-2702-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shire S. Y., Shih W., Chang Y.-C., Bracaglia S., Kodjoe M., Kasari C. (2019). Sustained community implementation of JASPER intervention with toddlers with autism. Journal of Autism and Developmental Disorders, 49(5), 1863–1875. [DOI] [PubMed] [Google Scholar]
- Shire S. Y., Shih W., Kasari C. (2018). Brief report: Caregiver strategy implementation – Advancing spoken communication in children who are minimally verbal. Journal of Autism and Developmental Disorders, 48(4), 1228–1234. 10.1007/s10803-017-3454-0 [DOI] [PubMed] [Google Scholar]
- Skard G., Bundy A. (2008). Test of playfulness. In L. D. Parham & L. S. Fazio (Eds.), Play in occupational therapy for children (2nd ed., pp. 71–93). Mosby Elsevier.
- Smith I. M., Flanagan H. E., Ungar W. J., D’Entremont B., Garon N., den Otter J., Waddell C., Bryson S. E., Tsiplova K., Léger N., Vezina F., Murray P. (2019). Comparing the 1-year impact of preschool autism intervention programs in two Canadian provinces. Autism Research, 12(4), 667–681. 10.1002/aur.2072 [DOI] [PubMed] [Google Scholar]
- Smith I. M., Flanagan H. E., Garon N., Bryson S. E. (2015). Effectiveness of community-based early intervention based on pivotal response treatment. Journal of Autism and Developmental Disorders, 45(6), 1858–1872. [DOI] [PubMed] [Google Scholar]
- Smith I. M., Koegel R. L., Koegel L. K., Openden D. A., Fossum K. L., Bryson S. E. (2010). Effectiveness of a novel community-based early intervention model for children with autistic spectrum disorder. American Journal on Intellectual and Developmental Disabilities, 115(6), 504–523. 10.1352/1944-7558-115.6.504 [DOI] [PubMed] [Google Scholar]
- Solomon R., Van Egeren L. A., Mahoney G., Huber M. S. Q., Zimmerman P. (2014). PLAY project home consultation intervention program for young children with autism spectrum disorders: A randomized controlled trial. Journal of Developmental and Behavioral Pediatrics, 35(8), 475–485. 10.1097/DBP.0000000000000096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadnick N. A., Stahmer A., Brookman-Frazee L. (2015). Preliminary effectiveness of Project ImPACT: A parent-mediated intervention for children with autism spectrum disorder delivered in a community program. Journal of Autism and Developmental Disorders, 45(7), 2092–2104. 10.1007/s10803-015-2376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stagnitti K., Bailey A., Hudspeth Stevenson E., Reynolds E., Kidd E. (2016). An investigation into the effect of play-based instruction on the development of play skills and oral language. Journal of Early Childhood Research, 14, 389–406. http://10.0.4.153/1476718X15579741 [Google Scholar]
- Strunk J., Leisen M., Schubert C. (2017). Using a multidisciplinary approach with children diagnosed with autism spectrum disorder. Journal of Interprofessional Education and Practice ( Vol. 8, pp. 60–68). Elsevier Inc. 10.1016/j.xjep.2017.03.009 [DOI] [Google Scholar]
- Stock R., Mirenda P., Smith I. M. (2013). Comparison of community-based verbal behavior and pivotal response treatment programs for young children with autism spectrum disorder. Research in Autism Spectrum Disorders, 7(9), 1168–1181. 10.1016/j.rasd.2013.06.002 [DOI] [Google Scholar]
- Szumski G., Smogorzewska J., Grygiel P., Orlando A-M. (2019). Examining the effectiveness of naturalistic social skills training in developing social skills and theory of mind in preschoolers with ASD. Journal of Autism and Developmental Disorders, 49(7), 2822–2837. 10.1007/s10803-017-3377-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szumski G., Smogorzewska J., Karwowski M. (2016). Can play develop social skills? The effects of ‘Play Time/Social Time’ programme implementation. International Journal of Developmental Disabilities, 62(1), 41–50. 10.1179/2047387715Y.0000000002 [DOI] [Google Scholar]
- Thiemann-Bourque K., Brady N., McGuff S., Stump K., Naylor A. (2016). Picture exchange communication system and pals: A peer-mediated augmentative and alternative communication intervention for minimally verbal preschoolers with autism. Journal of Speech, Language, and Hearing Research, 59(5), 1133–1145. 10.1044/2016_JSLHR-L-15-0313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiemann-Bourque K., Feldmiller S., Hoffman L., Johner S. (2018). Incorporating a peer-mediated approach into speech-generating device intervention: Effects on communication of preschoolers with autism spectrum disorder. Journal of Speech Language and Hearing Research, 61(8). 10.1044/2018_JSLHR-L-17-0424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiemann-Bourque K. S., McGuff S., Goldstein H. (2017). Training peer partners to use a speech-generating device with classmates with autism spectrum disorder: Exploring communication outcomes across preschool contexts. Journal of Speech, Language, and Hearing Research, 60(9), 2648–2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toret G., Ozmen E. R. (2019). Effects of reciprocal imitation training on social communication skills of young children with autism spectrum disorder. Egitim ve Bilim-Education and Science, 44(199), 279–296. 10.15390/EB.2019.8222 [DOI] [Google Scholar]
- Touzet S., Occelli P., Schroeder C., Manificat S., Gicquel L., Stanciu R., Schaer M., Oreve M.-J., Speranza M., Denis A., Zelmar A., Falissard B., Georgieff N., Bahrami S., Geoffray M.-M. (2017). Impact of the Early Start Denver Model on the cognitive level of children with autism spectrum disorder: Study protocol for a randomised controlled trial using a two-stage Zelen design. BMJ Open, 7(3). 10.1136/bmjopen-2016-014730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas J., Brunton J., Graziosi S. (2010). EPPI-Reviewer 4: Software for research synthesis. Social Science Research Unit, UCL Institute of Education.
- Thomas J., O’Mara-Eves A., Harden A., Newman M. (2017). Synthesis methods for combining and configuring textual or mixed methods data. In D. Gough, S. Oliver, & J. Thomas (Eds.), An introduction to systematic reviews (pp. 181–211). Sage Publications.
- Tiede G., Walton K. M. (2019). Meta-analysis of naturalistic developmental behavioral interventions for young children with autism spectrum disorder. Autism, 23, 2080–2095. 10.1177/1362361319836371 [DOI] [PubMed] [Google Scholar]
- Toseeb U., Gibson J. L., Newbury D. F., Orlik W., Durkin K., Pickles A., Conti-Ramsden G. (2020). Play and prosociality are associated with fewer externalizing problems in children with developmental language disorder: The role of early language and communication environment. International Journal of Language & Communication Disorders, 1460. 6984.12541. 10.1111/1460-6984.12541 [DOI] [PubMed] [Google Scholar]
- Toth K., Munson J., Meltzoff A. N., Dawson G. (2006). Early predictors of communication development in young children with autism spectrum disorder: Joint attention, imitation, and toy play. Journal of Autism and Developmental Disorders, 36, 993–1005. 10.1007/s10803-006-0137-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A. C., Lillie E., Zarin W., O’Brien K. K., Colquhoun H., Levac D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169, 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Van Wijngaarden-Cremers P. J. M., Van Eeten E., Groen W. B., Van Deurzen P. A., Oosterling I. J., Van Der Gaag R. J. (2014). Gender and age differences in the core triad of impairments in autism spectrum disorders: A systematic review and Meta-analysis. Journal of Autism and Developmental Disorders, 44, 627–635. 10.1007/s10803-013-1913-9 [DOI] [PubMed] [Google Scholar]
- van Rhijn T., Osborne C., Ranby S., Maich K., Hall C., Rzepecki L., Hemmerich A. (2019). Peer play in inclusive child care settings: Assessing the impact of Stay, Play, & Talk, a peer-mediated social skills program. Child Care in Practice. 10.1080/13575279.2019.1588707 [DOI] [Google Scholar]
- van Straten C. L., Smeekens I., Barakova E., Glennon J., Buitelaar J., Chen A. (2018). Effects of robots’ intonation and bodily appearance on robot-mediated communicative treatment outcomes for children with autism spectrum disorder. Personal and Ubiquitous Computing, 22(2), 379–390. 10.1007/s00779-017-1060-y [DOI] [Google Scholar]
- Varley D., Wright B., Cooper C., Marshall D., Biggs K., Ali S., Chater T., Coates E., Gilbody S., Gomez de la Cuesta G., Kingsley E., Le Couteur A., McKelvey A., Shephard N., Teare D. (2019). Investigating SOcial Competence and Isolation in children with Autism taking part in LEGO-based therapy clubs In School Environments (I-SOCIALISE): Study protocol. BMJ Open, 9(5). 10.1136/bmjopen-2019-030471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventola P., Friedman H. E., Anderson L. C., Wolf J. M., Oosting D., Foss-Feig J., McDonald N., Volkmar F., Pelphrey K. A. (2014). Improvements in social and adaptive functioning following short-duration PRT program: A clinical replication. Journal of Autism and Developmental Disorders, 44(11, SI), 2862–2870. 10.1007/s10803-014-2145-3 [DOI] [PubMed] [Google Scholar]
- Ventola P., Friedman H., Oosting D. (2015). Pivotal response treatment: Case reports. The Psychoanalytic Study of the Child, 69, 242–260. 10.1080/00797308.2016.11785530 [DOI] [PubMed] [Google Scholar]
- Vernon T. W., Holden A. N., Barrett A. C., Bradshaw J., Ko Jordan A., McGarry E. S., Horowitz E. J., Tagavi D. M., German T. C. (2019). A pilot randomized clinical trial of an enhanced pivotal response treatment approach for young children with autism: The PRISM model. Journal of Autism and Developmental Disorders, 49(6), 2358–2373. 10.1007/s10803-019-03909-1 [DOI] [PubMed] [Google Scholar]
- Vernon T. W., Koegel R. L., Dauterman H., Stolen K. (2012). An early social engagement intervention for young children with autism and their parents. Journal of Autism and Developmental Disorders, 42(12), 2702–2717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinen Z., Clark M., Paynter J., Dissanayake C. (2018). School age outcomes of children with autism spectrum disorder who received community-based early interventions. Journal of Autism and Developmental Disorders, 48(5), 1673–1683. [DOI] [PubMed] [Google Scholar]
- Vismara L. A., Colombi C., Rogers S. J. (2009). Can one hour per week of therapy lead to lasting changes in young children with autism? Autism: The International Journal of Research and Practice, 13(1), 93–115. 10.1177/1362361307098516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vismara L. A., Young G. S., Stahmer A. C., Griffith E. M., Rogers S. J. (2009). Dissemination of evidence-based practice: Can we train therapists from a distance? Journal of Autism and Developmental Disorders, 39(12), 1636–1651. 10.1007/s10803-009-0796-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vivanti G., Dissanayake C., Duncan E., Feary J., Capes K., Upson S., Bent C. A., Rogers S. J., Hudry K., Jones C., Bajwa H., Marshall A., Maya J., Pye K., Reynolds J., Rodset D., Toscano G. the Victorian ASELCC Team. (2019). Outcomes of children receiving Group-Early Start Denver Model in an inclusive versus autism-specific setting: A pilot randomized controlled trial. Autism, 23(5), 1165–1175. 10.1177/1362361318801341 [DOI] [PubMed] [Google Scholar]
- Vivanti G., Dissanayake C., & Victorian ASELCC Team. (2016). Outcome for children receiving the Early Start Denver model before and after 48 months. Journal of Autism and Developmental Disorders, 46(7), 2441–2449. 10.1007/s10803-016-2777-6 [DOI] [PubMed] [Google Scholar]
- Vivanti G., Dissanayake C., Zierhut C., Rogers S. J., & Team Victorian ASELCC. (2013). Brief report: Predictors of outcomes in the Early Start Denver Model delivered in a group setting. Journal of Autism and Developmental Disorders, 43(7), 1717–1724. 10.1007/s10803-012-1705-7 [DOI] [PubMed] [Google Scholar]
- Vivanti G., Paynter J., Duncan E., Fothergill H., Dissanayake C., Rogers S. J., & Victorian ASELCC Team. (2014). Effectiveness and feasibility of the early start Denver model implemented in a group-based community childcare setting. Journal of Autism and Developmental Disorders, 44(12), 3140–3153. 10.1007/s10803-014-2168-9 [DOI] [PubMed] [Google Scholar]
- Waddington H., van der Meer L., Sigafoos J. (2019). Supporting parents in the use of the early start Denver model as an intervention program for their young children with autism spectrum disorder. International Journal of Developmental Disabilities. 10.1080/20473869.2019.1585694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waddington H., van der Meer L., Sigafoos J., Ogilvie E. (2019). Evaluation of a low-intensity version of the early start Denver model with four preschool-aged boys with autism spectrum disorder. International Journal of Developmental Disabilities. 10.1080/20473869.2019.1569360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainer A. L., Ingersoll B. R. (2013). Disseminating ASD interventions: A pilot study of a distance learning program for parents and professionals. Journal of Autism and Developmental Disorders, 43(1), 11–24. [DOI] [PubMed] [Google Scholar]
- Wainer A. L., Ingersoll B. R. (2015). Increasing access to an ASD imitation intervention via a Telehealth Parent Training Program. Journal of Autism and Developmental Disorders, 45(12, SI), 3877–3890. 10.1007/s10803-014-2186-7 [DOI] [PubMed] [Google Scholar]
- Wainer J., Dautenhahn K., Robins B., Amirabdollahian F. (2014). A pilot study with a novel setup for collaborative play of the humanoid robot KASPAR with children with autism. International Journal of Social Robotics, 6(1), 45–65. 10.1007/s12369-013-0195-x [DOI] [Google Scholar]
- Walton K. M., Ingersoll B. R. (2012). Evaluation of a sibling-mediated imitation intervention for young children with autism. Journal of Positive Behavior Interventions, 14(4), 241–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisberg D. S., Hirsh-Pasek K., Golinkoff R. M. (2013). Embracing complexity: Rethinking the relation between play and learning: Comment on Lillard et al. (2013). Psychological Bulletin, 139, 35–39. 10.1037/a0030077 [DOI] [PubMed] [Google Scholar]
- Weisberg D. S., Hirsh-Pasek K., Golinkoff R. M., Kittredge A. K., Klahr D. (2016). Guided play. Current Directions in Psychological Science, 25, 177–182. 10.1177/0963721416645512 [DOI] [Google Scholar]
- Whitebread D., Coltman P., Jameson H., Lander R. (2009). Play, cognition and self-regulation: What exactly are children learning when they learn through play? Educational and Child Psychology, 26, 40–52. [Google Scholar]
- Wing L., Gould J., Yeates S. R., Brierley L. M. (1977). Symbolic play in severely mentally retarded and in autistic children. Journal of Child Psychology and Psychiatry, 18, 167–178. 10.1111/j.1469-7610.1977.tb00426.x [DOI] [PubMed] [Google Scholar]
- Williams M. E., Hastings R., Charles J. M., Evans S., Hutchings J. (2017). Parenting for Autism, Language, And Communication Evaluation Study (PALACES): Protocol for a pilot randomised controlled trial. BMJ Open, 7(2). 10.1136/bmjopen-2016-014524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C. S. (2013). A play and joint attention intervention for teachers of young children with autism: A randomized controlled pilot study. Autism: The International Journal of Research and Practice, 17(3), 340–357. [DOI] [PubMed] [Google Scholar]
- Yang Y.-H. (2016). Parents and young children with disabilities: The effects of a home-based music therapy program on parent-child interactions. Journal of Music Therapy, 53(1), 27–54. 10.1093/jmt/thv018 [DOI] [PubMed] [Google Scholar]
- Zhou B., Xu Q., Li H., Zhang Y., Wang Y., Rogers S. J., Xu X. (2018). Effects of parent-implemented Early Start Denver Model Intervention on Chinese toddlers with autism spectrum disorder: A non-randomized controlled trial. Autism Research, 11(4), 654–666. 10.1002/aur.1917 [DOI] [PubMed] [Google Scholar]
- Zhou V., Munson J. A., Greenson J., Hou Y., Rogers S., Estes A. M. (2019). An exploratory longitudinal study of social and language outcomes in children with autism in bilingual home environments. Autism, 23(2), 394–404. 10.1177/1362361317743251 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-dli-10.1177_23969415211015840 for Play-based interventions to support social and communication development in autistic children aged 2–8 years: A scoping review by Jenny L Gibson, Emma Pritchard and Carmen de Lemos in Autism & Developmental Language Impairments