ABSTRACT
Introduction
Military Veterans have an increased risk of suicide compared to the general population, but less is known about changes in risk with the onset of the COVID-19 pandemic, or whether any changes have been moderated by psychiatric or demographic factors. The primary objective was to test the hypothesis that the likelihood of suicide attempt or death by suicide was stable during the first year of the pandemic versus the preceding year for the full sample. A second objective was to test the hypothesis that, in contrast, risk increased for Veteran subgroups characterized by traditional risk factors (e.g., psychiatric diagnosis).
Materials and Methods
We extracted electronic health record data for 771,570 Veterans who received one or more health care visits between March 13, 2019, and March 12, 2021, at eight VA hospitals across the southwestern United States. Primary outcome measures were suicide attempts and deaths by suicide. Predictor variables included psychiatric diagnoses and demographic factors.
Results
Multivariable models indicated that the odds of death by suicide did not change during the first year of the COVID-19 pandemic, while the odds of making a suicide attempt declined. Veterans treated for major depression were at heightened risk for attempting suicide in both years, but the association was smaller during the pandemic than the year prior. In contrast, the relative risk of attempt for Veterans who were never married and Veterans treated for a non-alcohol, non-opioid substance-use disorder increased during the pandemic.
Conclusions and Relevance
The findings suggest that the pandemic has not led to an increase in suicidal behavior, which is consistent with other studies, although the degree of decline varied across diagnostic and demographic groups. Further longitudinal research is needed to evaluate whether the prolonged nature of COVID-19 may lead to changes in risk over time.
INTRODUCTION
The spread of the novel coronavirus (COVID-19) became a serious public health concern in 2020. As of September 2021, the World Health Organization estimated >224 million COVID-19 infections and 4.6 million deaths worldwide.1 In light of the pandemic impacts on physical, social,2 and psychological3 functioning, there is concern about concurrent increases in suicidality. Despite attention from researchers and media, evidence regarding COVID-19 impact on suicidal behaviors remains limited.
Prior to the pandemic, the rate of death by suicide in the United States had been increasing for 20 years and had been at its highest since the mid-1900s.4 Interestingly, national data indicate that the overall rate of death from suicide decreased from 2018 to 2019, but the decline was not consistent across the geographical region, race, or ethnicity.5 Correlates of death from suicide include lack of social connection/support, hopelessness, acute stressors, and substance use.6 Ideation-to-action theories suggest painful or traumatic events can lead individuals already experiencing ideation to habituate to the idea of suicide and increase their capacity to act on suicidal thoughts.7 These theories suggest that anxiety and lack or loss of social connection, which may occur as a result of efforts to reduce COVID-19 spread (e.g., lockdowns and social distancing),8 could increase the capability to act. Researchers have called for preventive efforts during the pandemic to mitigate these potential increases in risk.9 Given the recent changes in suicide trends, further exploration into COVID-19 trends and within specific populations is valuable.
Elevated suicide risk has been documented during previous disasters (e.g., large earthquakes, tsunamis, and pandemics). A review of 291 U.S. disasters suggested that suicide rates increased in the two subsequent years.10 Similarly, a meta-analysis found that rates of death from suicide increased in the first year post-disaster.11 Suicide rate increases have also been found during the 1910–1920 influenza pandemic12 and the influenza pandemic and in Hong Kong during the 2002–2004 severe acute respiratory syndrome (SARS) epidemic.”13 These studies indicate the multi-faceted consequences of a disaster on suicidal behaviors, although it should be noted that others have found decreased post-disaster suicide rates14,15 or increases only detectable years later.16
Multiple studies have evaluated whether rates of suicidal behavior have changed in relation to the COVID-19 pandemic. For example, one meta-analysis found that suicidal ideation and behavior increased during the pandemic,17 but another meta-analysis found no link between COVID-19 and suicidal behavior.18 Population-based studies in Japan have reported that (1) women had increased rates of suicide during the pandemic19 and (2) rates increased for both genders.20 However, studies in the United States and elsewhere have suggested a lack of change,21–23 including a recent study of U.S. Military Veterans.24 Thus, findings on suicidal behavior during COVID-19 are mixed. However, these studies generally utilized relatively small samples or included only the initial months of the pandemic, and thus may not reflect ongoing risk. In addition, evidence from population-based studies may obscure findings among subgroups, especially those disproportionately vulnerable to the impact of COVID-19.
Military Veterans are a group that may be at greater risk of the negative effects of the pandemic. Compared to the general population, Veterans have higher rates of multiple factors associated with suicide risk25 and are 1.5 times more likely to die by suicide than non-Veteran adults.26 The Veterans Health Administration (VHA) has declared suicide prevention a top priority, infusing more rigorous standards of screening and care for Veterans at risk for suicide.27 However, the extent to which such efforts can mitigate the COVID-19 impact is uncertain. Consistent with data from the Centers for Disease Control and Prevention, VHA’s 2021 National Veteran Suicide Prevention Annual report noted that clinical indicators suggest a decline in deaths from suicide in 2019 versus 2018; it also reports that indicators of suicide risk did not appear to change during the first year of the pandemic.28 However, the extent to which change may vary across risk groups is less certain and has received limited attention in the literature to date. This is an important question given the possibility that COVID-19 could exacerbate an existing risk.
Due to the critical importance of suicide prevention to clinical priority-setting, we sought to evaluate the effects of COVID-19 on documented deaths from suicide and suicide attempts in Veterans across eight VHA facilities in the southwestern United States. Given recent national and VHA data, we hypothesized that we would find no change in the overall rates of either outcome among the full sample. Secondarily, we tested whether changes in suicidal behaviors may have differed among subgroups of Veterans with certain psychiatric or demographic risk factors. In this case, we expected that factors traditionally associated with suicide risk (e.g., receiving treatment for a psychiatric diagnosis and male gender) would be associated with an increased likelihood of suicidal behavior during versus before the pandemic.
METHODS
Veterans were identified using VHA’s Corporate Data Warehouse based on having received care between March 13, 2019, and March 12, 2021, at any of the eight VHA systems encompassing southern California (Los Angeles, Long Beach, Loma Linda, and San Diego), Arizona (Phoenix, Tucson, and Prescott), and New Mexico (Albuquerque). The beginning of the pandemic was defined as March 13, 2020, the date on which the U.S. Government declared a national emergency.29 Veterans seen at multiple facilities were assigned to the facility where the most visits occurred. We included all Veterans with health care encounters during either the year preceding the pandemic (March 13, 2019–March 12, 2020; n = 636,081) or the first year of the pandemic (March 13, 2020–March 12, 2021; n = 634,117). The majority (65.6% of the sample) had encounters in both calendar years and were included separately for each year. The sample included 1,270,198 records from 771,570 unique Veterans.
Demographic (gender, age, racial and ethnic backgrounds, and marital status) and residential (zip code) data were collected from Corporate Data Warehouse and are shown in Table I. For gender, race, ethnicity, and marital status, response options included that the Veteran had declined to respond, or that it was unknown or missing (2.0% had an unknown or missing value on one or more of these variables). For each variable, these categories were combined into a declined/unknown group. Age was calculated as age in years on January 1, 2019. Socioeconomic status was estimated based on median household income in each Veteran’s residential zip code,30,31 derived from the 2018 U.S. Census Bureau’s American Community Survey.32 When zip codes were missing or invalid (3.1% of the sample), mean household income for the relevant site and year was substituted. In addition, we collected mental health diagnoses from health care visits occurring during the two study periods, indicating the diagnosis or diagnoses for which the Veteran received treatment during each visit. We counted visits by diagnoses and converted these into a series of binary variables indicating whether a Veteran had or had not been treated for a specific condition. Diagnoses were coded in the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10)33 format. Based on the measures VHA uses to estimate mental health care access and quality,34 we generated a series of binary variables indicating whether or not each Veteran had an active diagnosis in each of a series of diagnostic categories (Table I).
TABLE I.
Clinical and Demographic Characteristics of the Sample
| Variable | Descriptive statistics | |
|---|---|---|
| N | 1,270,198 person-years; 771,570 Veterans | |
| Gender | Male | 87.9% |
| Age | M = 58.7 years | SD = 17.4 |
| Race | White | 62.7% |
| Black | 11.2% | |
| Asian | 3.6% | |
| Native Hawaiian or other Pacific Islander | 1.4% | |
| American Indian or Alaska Native | 1.9% | |
| Declined to report or unknown | 19.2% | |
| Ethnicity | Latinx | 14.2% |
| Marital status | Married | 48.6% |
| Divorced | 21.9% | |
| Separated | 3.0% | |
| Widowed | 3.4% | |
| Never married | 18.0% | |
| Income | M = 66,482 | SD = 23,349 |
| Diagnostic group | ICD-10 codes | % |
| Post-Traumatic Stress Disorder (PTSD) | F43.10–F43.12 | 14.9% |
| Major depression | F32.0–F32.5, F32.9, F33.0–F33.3, F33.40–F33.42, F33.9 | 12.6% |
| Generalized anxiety disorder (GAD) | F41.1 | 2.6% |
| Other anxiety disorder (OAD) | F06.4, F40.00–F40.02, F40.10, F40.11, F40.210, F40.218, F40.220, F40.228, F40.230–F40.233, F40.240–F40.243, F40.248, F40.290, F40.291, F40.298, F40.8, F40.9, F41.0, F41.3, F41.8, F41.9, F42., F42.2, F43.2, F42.4, F42.8, F42.9, F45.20, F45.21, and F45.29 | 7.4% |
| Alcohol-use disorder (AUD) | F10.10–F10.99 | 5.3% |
| Opioid-use disorder (OUD) | F11.10–F11.99 | 0.9% |
| Any other substance-use disorder (SUD) | F12.10–F16.99, F18.10–F19.99 | 3.3% |
| Serious mental illness (SMI) | F20.0, F20.1, F20.2, F20.3, F20.5, F20.81, F20.89, F20.9, F25.0, F25.1, F25.8, F25.9, F06.0, F06.2, F22, F23, F24, F28, F29, F53, F53.1, F30.10–F30.12, F30.13, F30.2, F30.3, F30.4, F30.8, F30.9, F31.0, F31.11–F31.13, F31.2, F31.30, F31.31, F31.32, F31.4, F31.5, F31.60– F31.64, F31.70–F31.78, F31.81, F31.89, F31.9 | 3.3% |
| 1+ MH visits | 27.6% | |
VHA uses a Suicide Behavior and Overdose Report (SBOR) to document suicidal and self-harm behavior. Clinicians who learn of such behaviors add an SBOR to the medical record. We generated a list of SBORs documenting suicide attempts or deaths by suicide in the study period, attributing them to the correct Veteran record based on whether they occurred before (year = 0; March 13, 2019–March 12, 2020) or during (year = 1; March 13, 2020–March 12, 2021) the pandemic and created binary death from suicide and suicide attempt variables that were used as the primary outcome variables.
Statistical Analysis
Separate binary logistic regression models were fit for the odds of death from suicide and the odds of attempting suicide. We chose logistic regression because it better fits the data compared with alternatives (e.g., Poisson or negative binomial regression). The site of care was included as a covariate. Due to our secondary interest in the hypothesis that the changes in behavior varied as a function of clinical and demographic characteristics, initial models included terms for interactions between these characteristics and year, as well as the characteristics’ main effects. Models were tested in a backward manner; non-significant interaction terms were removed and the model was refit. Models included a consistent set of demographic predictors, including gender, race (with White as the reference group), ethnicity (not Latinx), marital status (married), age, and median household income. The latter two were mean-centered at 0. All analyses utilized Stata IC 15.1 (StataCorp, College Station, TX) with alpha = .05.
RESULTS
Preliminary Analyses
Descriptive statistics are shown in Table I. A small number of records with invalid age values (e.g., values <18 or >110) were excluded from subsequent analyses (n = 204). About one in four patients (27.6%) had at least one visit with a mental health diagnosis. The most common were Post-Traumatic Stress Disorder (PTSD), major depressive disorder, and substance-use disorders. A total of 86 deaths by suicide were reported during 2019–2020, compared with 89 in 2020–2021, a non-significant difference [χ2(1) = 0.02, P = .887]. The number of Veterans who made suicide attempts declined significantly from 2,030 in 2019–2020 to 1,722 in 2020–21 [χ2(1) = 29.44, P < .001].
Primary Analyses
As noted earlier, we evaluated predictors of the odds of death from suicide and making a suicide attempt separately. Results from both models are shown in Table II. In the model of death from suicide, all interactions with year were non-significant, indicating similar associations with the odds of dying from suicide in both years. Interaction terms were thus not retained. Several diagnostic variables were significant predictors. Receiving care for major depressive disorder (MDD) or serious mental illness (SMI) was associated with 70% and 169% greater odds of dying by suicide, respectively. Similarly, Veterans treated for opioid use disorder (OUD) were 186% more likely to die by suicide, and those with alcohol use disorder (AUD) visits were 123% more likely. The likelihood of dying by suicide was not related to whether or not Veterans had visits for PTSD, GAD or other anxiety disorders, or other substance use disorder (SUD)s. In terms of demographic variables, Veterans identified as Black were 50% less likely to die by suicide relative to those identified as White, and those who identified as Latinx were 48% less likely to die by suicide compared to those who did not. Women were 68% less likely than men to die by suicide. Being widowed was associated with 15% lower odds of death from suicide compared to being married. Neither year nor other demographic variables were related to the odds of death from suicide.
TABLE II.
Logistic Regression Models of the Odds of Death from Suicide and Making a Suicide Attempt
| Outcome | |||||||
|---|---|---|---|---|---|---|---|
| Death from suicide | Suicide attempt | ||||||
| Predictor | SE | OR | 95% CI | Predictor | SE | OR | 95% CI |
| Site | <0.01 | 1.00 | 1.00, 1.01 | Site | <0.01 | 1.00 | 1.00, 1.00 |
| Year | 0.15 | 1.00 | 0.75, 1.35 | Year | 0.05 | 0.90 | 0.81, 1.01 |
| Race | Race | ||||||
| Black | 0.15 | 0.50 | 0.28, 0.89 | Black | 0.05 | 0.95 | 0.86, 1.04 |
| Asian | 0.24 | 0.41 | 0.13, 1.29 | Asian | 0.08 | 0.87 | 0.73, 1.03 |
| NH/PI | 0.39 | 0.39 | 0.05, 2.78 | NH/PI | 0.13 | 1.10 | 0.86, 1.39 |
| AI/AN | 0.28 | 0.28 | 0.04, 2.00 | AI/AN | 0.11 | 1.11 | 0.92, 1.34 |
| Declined | 0.29 | 1.16 | 0.70, 1.90 | Declined | 0.04 | 0.71 | 0.63, 0.80 |
| Ethnicity | Ethnicity | ||||||
| Latinx | 0.14 | 0.52 | 0.30, 0.89 | Latinx | 0.04 | 0.88 | 0.80, 0.96 |
| Declined | 0.39 | 1.42 | 0.83, 2.45 | Declined | 0.09 | 1.34 | 1.17, 1.54 |
| Gender | 0.40 | 0.32 | 0.14, 0.69 | Gender | 0.05 | 0.96 | 0.86, 1.06 |
| Marital | Marital | ||||||
| Separated | 0.61 | 1.62 | 0.77, 3.41 | Separated | 0.10 | 1.28 | 1.09, 1.49 |
| Divorced | 0.19 | 0.85 | 0.55, 1.33 | Divorced | 0.05 | 1.16 | 1.06, 1.27 |
| Widowed | 0.83 | 2.50 | 1.30, 4.81 | Widowed | 0.13 | 0.93 | 0.71, 1.22 |
| Never married | 0.29 | 1.36 | 0.89, 2.07 | Never married | 0.05 | 1.01 | 0.91, 1.13 |
| Declined | 0.38 | 0.81 | 0.32, 2.05 | Declined | 0.10 | 0.75 | 0.58, 0.96 |
| Median income | 0.03 | 0.99 | 0.98, 1.00 | Marital* year | 0.02 | 1.04 | 1.01, 1.08 |
| Age | <0.01 | 1.00 | 0.99, 1.00 | Age | <0.01 | 0.96 | 0.96, 0.97 |
| PTSD | 0.17 | 0.76 | 0.49, 1.18 | Median income | 0.01 | 0.96 | 0.95, 0.98 |
| MDD | 0.36 | 1.70 | 1.12, 2.58 | PTSD | 0.07 | 1.83 | 1.70, 1.97 |
| GAD | 0.45 | 1.25 | 0.62, 2.53 | MDD | 0.29 | 5.61 | 5.07, 6.21 |
| Other anxiety | 0.27 | 1.05 | 0.63, 1.73 | MDD * year | 0.06 | 0.84 | 0.73, 0.97 |
| AUD | 0.56 | 2.23 | 1.36, 3.65 | GAD | 0.06 | 1.09 | 0.98, 1.21 |
| OUD | 1.08 | 2.86 | 1.36, 6.01 | Other anxiety | 0.05 | 1.15 | 1.07, 1.24 |
| SUD | 0.45 | 1.44 | 0.78, 2.65 | AUD | 0.10 | 2.37 | 2.19, 2.57 |
| SMI | 0.69 | 2.69 | 1.62, 4.46 | OUD | 0.11 | 1.61 | 1.41, 1.84 |
| SUD | 0.13 | 2.35 | 2.10, 2.62 | ||||
| SUD* year | 0.09 | 1.21 | 1.05, 1.40 | ||||
| SMI | 0.16 | 3.87 | 3.56, 4.20 | ||||
White was the reference group for race, not Latinx was the reference group for ethnicity, male was the reference group for gender, and married was the reference group for marital status. NH/PI = Native Hawaiian or other Pacific Islander, AI/AN = American Indian or Alaska Native. CI = confidence interval, OR = odds ratio, and SE, standard error, MDD = Major Depressive Disorder, AUD = alcohol use disorder, SUD = substance use disorder, SMI = serious mental illness. Median income was divided by 10,000 to ease interpretability and was mean-centered at 0. Age was also mean-centered at 0. Diagnostic variables are binary (0 = no visits in this category, 1 = 1+ visits in this category).
The model of the likelihood of making a suicide attempt was more nuanced. Some diagnostic variables predicted the odds of suicide attempts consistently across both 2019–2020 and 2020–2021. Receiving care for PTSD was associated with 83% greater odds of a suicide attempt, and care for other anxiety disorders was associated with 15% greater odds. Veterans with visits for SMI were 287% more likely to make a suicide attempt than those without such visits. The odds of suicide attempts were also associated with receiving care for AUD (137% greater) and OUD (61% greater). For both MDD and SUD, interactions with year were significant, indicating that the strength of the associations with suicide attempt changed from 2019–2020 to 2020–2021. Because the year was coded as 0 (2019–2020) or 1 (2020–2021), the main effects for MDD and SUD in Table II reflect the association between the variable and outcome in 2019–2020 (i.e., when year = 0). This indicates that in 2019–2020, those with MDD visits were 461% more likely to attempt suicide than those without such visits. However, the interaction term (odds ratio [OR] = 0.84 [95% confidence interval 0.73, 0.97], z = −2.44, P = .015) indicates a significant decline in the strength of this association in 2020–2021. For SUD, in 2019–2020, those with visits for other SUDs were 135% more likely than those without such visits to make a suicide attempt. In this case, the interaction term (OR = 1.21 [1.05, 1.40], z = 2.65, P = .008) indicates that the strength of the association increased significantly in 2020–2021.
The likelihood of making a suicide attempt was also associated with some demographic variables, although not with race or gender. Veterans who identified as Latinx were 12% less likely to make suicide attempts, while those whose racial identity was unknown were 29% less likely to attempt suicide. In contrast, those for whom no ethnic identity was known were 34% more likely to attempt suicide. The likelihood of making a suicide attempt was inversely associated with age and with median income in Veterans’ residential zip codes. There was a significant interaction between year and marital status (OR = 1.04 [1.01, 1.08], z = 2.55, P = .011), indicating that the relationship between marital status and suicide attempt differed for 2019–2020 versus 2020–2021. Finally, the main effect of year was not significant (OR = 0.90 [0.81, 1.01], z = −1.74, P = .081). However, given the interaction terms that were retained in the model, this indicates that the likelihood of attempted suicide did not change over time for Veterans for whom marital status, MDD, and SUD were coded as 0 (i.e., those who were married and who did not have visits for either MDD or SUD). A post hoc analysis that retained all covariates but omitted interaction terms was conducted to evaluate change in the odds of suicide attempt for the full sample; this indicated that the likelihood of a suicide attempt was 14% lower in 2020–2021 compared with 2019–2020 (OR = 0.86 [0.81, 0.92], z = −4.44, P < .001).
To better explain the interactions, the model of suicide attempts was refit separately for 2019–2020 and 2020–2021. Fig. 1 shows ORs for never married versus married, having versus not having MDD visits, and having versus not having SUD visits in both years. As the figure indicates, the odds of making a suicide attempt for never married Veterans was comparable to the odds for married Veterans in 2019–2020 but higher than married Veterans in 2020–2021. For Veterans with MDD visits, the odds of suicide attempts were significantly higher than for Veterans without MDD visits in both years, but the difference decreased in 2020–2021. In contrast, Veterans with SUD visits also had greater odds of attempted suicide in both years, but the difference increased in 2020–21 compared with the year prior.
FIGURE 1.
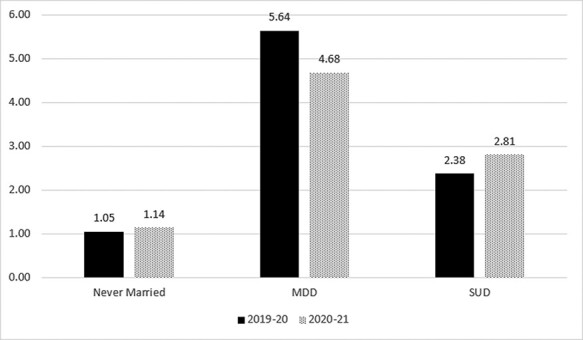
Odds of making a suicide attempt separately for 2019–2020 and 2020–2021 for predictors that interacted with time.
While Fig. 1 explains changes in the differences between these groups, it does not clarify whether changes occurred in one or both groups. For example, it is not clear whether the lower 2020–21 effect of MDD reflects declining rates of attempted suicide among Veterans with MDD visits, increasing rates among those without MDD visits, or both. To address this question, we calculated the rate of attempted suicide per 1,000 Veterans for the relevant diagnostic and demographic groups in both years, as shown in Table III. As the table makes clear, the rate of attempted suicide declined from 2019–2020 to 2020–2021 for all groups (with and without MDD visits; with and without SUD visits; currently married and never married). In other words, the interactions in the primary model of suicide attempts reflect that the decline was greater among those receiving care for MDD than those not; smaller among those receiving care for SUD than those not; and greater among those currently married than those never married.
TABLE III.
Frequency of Suicide Attempts by Diagnostic and Demographic Groups over Time
| Suicide attempt | ||||
|---|---|---|---|---|
| Group | Years | No | Yes | Rate per 1,000 Veterans |
| With MDD | 2019–2020 | 80,436 | 1,356 | 16.86 |
| 2020–2021 | 78,609 | 1,084 | 13.79 | |
| Without MDD | 2019–2020 | 554,914 | 674 | 1.21 |
| 2020–2021 | 565,214 | 638 | 1.13 | |
| With SUD | 2019–2020 | 21,450 | 684 | 31.89 |
| 2020–2021 | 19,954 | 603 | 30.22 | |
| Without SUD | 2019–2020 | 613,900 | 1,346 | 2.19 |
| 2020–2021 | 623,869 | 1,119 | 1.79 | |
| Married | 2019–2020 | 311,821 | 753 | 2.41 |
| 2020–2021 | 303,918 | 541 | 1.78 | |
| Never married | 2019–2020 | 113,208 | 512 | 4.52 |
| 2020–2021 | 113,896 | 457 | 4.01 | |
DISCUSSION
Our primary aim was to address a question critical to VHA and nationally, whether the frequency of suicidal behaviors changed during the first year of the COVID-19 pandemic. Previous findings on suicidality following disasters generally and COVID-19 specifically have been mixed. Based on previous national and VHA data, we predicted stability in the likelihood of suicide attempt and death by suicide during the period from March 13, 2020, to March 12, 2021, compared with the preceding 12 months. Indeed, we found no change in deaths from suicide and a significant reduction in suicide attempts.
Our secondary hypothesis was that even in the absence of change in the full sample, individuals possessing diagnostic and demographic suicide risk factors would experience increases in suicidal behavior. However, this was not the case. Veterans from certain demographic groups or receiving care for certain psychiatric- and substance-use disorders were more likely to die by suicide (male, White, and widowed; MDD, AUD, OUD, and SMI) and attempt suicide (PTSD, MDD, anxiety disorders, AUD, OUD, SUD, and SMI), but in most cases, the strength of the association was comparable during the first year of the pandemic and the prior 12 months. The exceptions were never married Veterans and those receiving care for non-alcohol, non-opiate SUDs. Importantly, however, this did not reflect a disproportionate increase in behavior among those with these diagnoses. Instead, it reflected a general reduction in the likelihood of suicide attempt that was more pronounced among Veterans who were currently married and Veterans who did not receive SUD care. In contrast, the odds of suicide attempt declined more steeply for Veterans receiving MDD care than for those not receiving MDD care.
In light of concerns about pandemic-induced distress and isolation described at many levels, stability and/or reduction in suicidal behavior may seem surprising. Nevertheless, multiple reports22,23,28 from multiple countries have yielded comparable results. Findings are also consistent with a smaller study of Veterans in which self-reported suicidal ideation was lower in late 2020 compared with late 2019.24 It may be that both are true: that the changes associated with COVID-19 have produced increased distress and psychiatric disorders,35 but that this has not led to an increase in suicidal behavior, at least to date. One possibility is that processes put into place within VHA may have had some protective impact, particularly for those with less severe mental health conditions. For example, since 2018 VHA has incorporated increasingly standardized risk assessment as well as safety planning for those deemed to be at increased risk. In addition, VHA increased attention to suicide risk during the pandemic by increasing outreach from suicide prevention clinicians to Veterans identified as high risk who screened positive or were tested for COVID-19.36
Preparation for the shift to telehealth and dealing with risk may also have played a positive role. VHA providers complete regular training in telehealth and management of suicide risk, enabling continuity of care with less disruption as the pandemic began. Another possibility is that the VHA population tends to be older; the average participant in the present sample was 58.7 years old at the start of the study. Older adults may be better at minimizing reactivity to stress and regulating emotions, limiting the psychological impact of the pandemic.37 This may also explain why we found that risk was lower among older Veterans, a discrepancy that increased during the pandemic. This contradicts previous evidence that suicide risk increases with age38 but matches recent suggestions that this may be changing, at least among Veterans.39
National discussion around mental health overlaid on VHA models of care may also have played a role. With frequent media discussion of the mental health impacts of COVID-19, Veterans may have been comfortable seeking help earlier, before the crisis stage, to connect with mental health services. Additional data on rates of new or reengaged patients in mental health might help elucidate this. Team-based approaches to mental health, inherent in VHA, allow for multiple providers–even remote providers–to be involved in managing emerging mental health crises, in the moment and afterward. VHA enrollees also have access to social support within the VHA, like housing support and vocational rehabilitation. Finally, VHA has expanded its offerings to connect individuals to care within the community when internal care is not readily available. All of these supports may have played a role in the finding of stable or declining rates of suicide attempts and deaths during the first year of the pandemic.
Despite evidence of a reduced incidence of death by suicide and suicide attempts to date, there are reasons to be alert to continued risk and to examine and bolster mitigation efforts. Previous studies suggest that suicide rates might not increase immediately following a disaster but instead might rise in the long term.14,15 The community, financial, and other supports that may have existed early on in the pandemic—from rent forgiveness policies to small business loans to neighborhood and non-profit-level outreach efforts to workplace leniency about childcare—may flag as the pandemic extends, and loss of these resources could lead to greater risk. There is also early evidence of potential long-term neuropsychiatric sequelae related to COVID-19 infection,40 which could impact psychiatric conditions and suicidality in the future, particularly in communities disproportionately impacted by COVID-19.
These data have limitations. First, the sample was comprised of Veterans receiving VHA care in the southwestern United States and may not generalize to the population as a whole. This is potentially important given the suggestion that the pandemic may disproportionately impact the risk of suicidality for younger individuals and women,41 who were underrepresented here. Second, data were drawn from medical records, which may have errors or be incomplete. Medical records may undercount the prevalence of death from suicide,42 although this limitation applies to both time periods in this study, and it is not clear that it would impact change over time.
Our findings suggest that the risk of death by suicide and attempted suicide remained generally stable or declined during the first year of the COVID-19 pandemic. For individuals receiving treatment for MDD, the odds of a suicide attempt declined more steeply than for individuals not being treated for MDD. In contrast, Veterans receiving treatment for certain SUDs and Veterans who had never been married had smaller reductions in the odds of suicide attempt compared to those not receiving SUD treatment and married Veterans, respectively. These groups may benefit from targeted efforts to mitigate suicide risk. Additional research is needed to determine whether these findings are replicated in non-Veteran samples and whether they remain stable throughout and following the COVID-19 pandemic.
ACKNOWLEDGMENTS
None declared.
Contributor Information
Neal Doran, VA San Diego Healthcare System and Department of Psychiatry, University of California, San Diego, CA 92161, USA.
Jenna Gress-Smith, VA Phoenix Healthcare System, Phoenix, AZ 85012, USA.
Pushpa Raja, VA Greater Los Angeles Healthcare System and Department of Psychiatry, University of California, Los Angeles, Los Angeles, CA 90073, USA.
Jack T Waddell, VA Phoenix Healthcare System, Phoenix, AZ 85012, USA.
Luther Davis, VA Loma Linda Healthcare System, 112021 Benton Street, Loma Linda, CA 92357, USA.
Sarah De La Rosa, VA New Mexico Healthcare System, Albuquerque, NM 87108, USA.
Vanessa Hurwitz, VA Long Beach Healthcare System, Long Beach, CA 90822, USA.
Kris Kratz, VA Phoenix Healthcare System, Phoenix, AZ 85012, USA.
Ryan Louis, Northern Arizona VA Healthcare System, Prescott, AZ 86301, USA.
Jeanie Moore, VA New Mexico Healthcare System, Albuquerque, NM 87108, USA.
Lana Peoples, VA Phoenix Healthcare System, Phoenix, AZ 85012, USA.
FUNDING
None declared.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. WHO coronavirus (COVID-19) dashboard. 2021. Available at https://covid19.who.int; accessed September 14, 2021.
- 2. Kawohl W, Nordt C: COVID-19, unemployment, and suicide. Lancet Psychiatry 2020; 7(5): 389–90.doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ettman C, Abdalla S, Cohen G, Sampson L, Vivier P, Galea S: Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020; 3(9): e2019686.doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Drapeau C, McIntosh J: USA suicide 2017: official final data. Education Faculty Publications, 2018. 40. https://scholar.valpo.edu/ed_fac_pubs/40; accessed August 25, 2021. [Google Scholar]
- 5. Stone D, Jones C, Mack K: Changes in suicide rates—United States, 2018-2019. MMWR Morb Mortal Wkly Rep 2021; 70(8): 261–8.doi: 10.15585/mmwr.mm7008a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chu C, Klein K, Buchman-Schmitt J, Hom M, Hagan C, Joiner T: Routinized assessment of suicide risk in clinical practice: an empirically-informed update. J Clin Psychol 2015; 71(12): 1186–200.doi: 10.1002/jclp.22210. [DOI] [PubMed] [Google Scholar]
- 7. Klonsky E, Saffer B, Bryan C: Ideation-to-action theories of suicide: a conceptual and empirical update. Curr Opin Psychol 2018; 22: 38–43.doi: 10.1016/j.copsyc.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 8. Sheffler J, Joiner T, Sachs-Ericsson N: The interpersonal and psychological impacts of COVID-19 on risk for late-life suicide. Gerontologist 2021; 61(1): 23–9.doi: 10.1093/geront/gnaa103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reger M, Stanley I, Joiner T: Suicide mortality and coronavirus disease 2019—a perfect storm? JAMA Psychiatry 2020; 77(11): 1093–4.doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- 10. Horney J, Karaye I, Abuabara A, Gearhart S, Grabich S, Perez-Patron M: The impact of natural disasters on suicide in the United States, 2003–2015. Crisis 2020; 42(5): 328–34.doi: 10.10.27/0227-5910/a000723. [DOI] [PubMed] [Google Scholar]
- 11. Safarpour H, Sohrabizadeh S, Malekyan L, et al. : Suicide death rate after disasters: a meta-analysis study. Arch Suicide Res 2020; 26: 14–27.doi: 10.1080/13811118.2020.1793045. [DOI] [PubMed] [Google Scholar]
- 12. Wasserman I: The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suic Life Threat Beh 1992; 22(2): 240–54. Available at https://pubmed.ncbi.nlm.nih.gov/1626335/. [PubMed] [Google Scholar]
- 13. Cheung Y, Chau P, Yip P: A revisit on older adult suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong. Intl J Geriatric Psychiatry 2008; 23(12): 1231–8.doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- 14. Matsubayashi T, Swada Y, Ueda M: Natural disasters and suicide: evidence from Japan. Soc Sci Med 2013; 82: 126–33.doi: 10.1016/j.socscimed.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 15. Ohto H, Maeda M, Yabe H, Yasumura S, Bromet E: Suicide rates in the aftermath of the 2011 earthquake in Japan. Lancet 2015; 385(9979): 1727.doi: 10.1016/S0140-6736(15)60890-X. [DOI] [PubMed] [Google Scholar]
- 16. Kolves K, Kolves K, DeLeo D: Natural disasters and suicidal behaviours: a systematic literature review. J Affective Dis 2013; 146(1): 1–14.doi: 10.1016/j.jad.2012.07.037. [DOI] [PubMed] [Google Scholar]
- 17. Dube J, Smith M, Sherry S, Hewitt P, Stewart S: Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res 2021; 301: 113998.doi: 10.1016/j.psychres.2021.113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Prati G, Mancini A: The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med 2021; 51(2): 201–11.doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nomura S, Kawashima T, Yoneoka D, et al. : Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Res 2021; 295: 113622.doi: 10.1016/j.psychres.2020.113622. [DOI] [PubMed] [Google Scholar]
- 20. Sakamoto H, Ishikane M, Gahaznavi C, Ueda P: Assessment of suicide in Japan during the COVID-19 pandemic vs previous years. JAMA Netw Open 2020; 4(2): e2037378.doi: 10.1001/jamanetworkopen.2020.37378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Faust J, Shah S, Du C, Li S, Lin Z, Krumhols H: Suicide deaths during the COVID-19 stay-at-home advisory in Massachusetts, March to May 2020. JAMA Netw Open 2021; 4(1): e2034273.doi: 10.1001/jamanetworkopen.2020.34273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Appleby L: What has been the effect of covid-19 on suicide rates? BMJ 2021; 372: n384.doi: 10.1136/bmj.n834. [DOI] [PubMed] [Google Scholar]
- 23. John A, Pirkis J, Gunnell D, Appleby L: Trends in suicide during the covid-19 pandemic. BMJ 2020; 371: m4352.doi: 10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]
- 24. Nichter B, Hill M, Na P, et al. : Prevalence and trends in suicidal behavior among US military veterans during the COVID-19 pandemic. JAMA Psychiatry 2021; 78(11):1218–27doi: 10.1001/jamapsychiatry.2021.2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bruce M: Suicide risk and prevention in veteran populations. Ann NY Acad Sci 2010; 1208: 98–103.doi: 10.1111/j.1749-6632.2010.05697.x. [DOI] [PubMed] [Google Scholar]
- 26. US Department of Veterans Affairs : National Veteran Suicide Prevention Annual Report. 2019. Available at https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf2019; accessed August 25, 2021.
- 27. Veterans Affairs Quality Enhancement Research Initiative : Improving uptake of the VA suicide risk identification strategy. 2020. Available at https://www.queri.research.va.gov/qnews/sept20/default.cfm?QnewsMenu=article3; accessed August 25, 2021.
- 28. Department of Veteran Affairs : 2021 National Veteran Suicide Prevention Annual Report. Office of Mental Health and Suicide Prevention, 2021. Available at https://www.mentalhealth.va.gov/docs/data-sheets/2021/2021-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-9-8-21.pdf; accessed February 16, 2022.
- 29. American Journal of Managed Care staff : COVID-19 roundup: coronavirus now a national emergency, with plans to increase testing. 2020. Available at https://www.ajmc.com/view/covid19-roundup2; accessed August 27, 2021.
- 30. Beltran S, Arenas D, Lopez-Hinojosa I, Tung E, Cronholm P: Associations of race, insurance, and zip code-level income with nonadherence diagnoses in primary and specialty diabetes care. J Am Board Fam Med 2021; 34(5): 891–7.doi: 10.3122/jabfm.2021.05.200639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chrisinger B, Gustafson J, King A, Winter S: Understanding where we are well: neighborhood-level social and environmental correlates of well-being in the Stanford Well for Life Study. Int J Environ Res Public Health 2021; 16(10): 1786.doi: 10.3390/ijerph16101786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. United States Census Bureau : American Community Survey (ACS). 2021. Available at https://census.gov/programs-surveys/acs; accessed June 11, 2021.
- 33. National Center for Health Statistics, Centers for Disease Control and Prevention : ICD-10-CM/PCS transition. 2017. Available at https://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm; accessed June 11, 2021.
- 34. Lemke S, Boden M, Kearney L, et al. : Measurement-based management of mental health quality and access in VHA: SAIL mental health domain. Psychol Serv 2017; 14(1): 1–12.doi: 10.1037/ser0000097. [DOI] [PubMed] [Google Scholar]
- 35. O’Connor R, Wetherall K, Cleare S, et al. : Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry 2021; 218(640): 326–33.doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Department of Veterans Affairs : 2021 National Veteran Suicide Prevention Annual Report. Office of Mental Health and Suicide Prevention, 2021. Available at https://https://www.mentalhealth.va.gov/docs/data-sheets/2021/2021-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-9-8-21.pdf; accessed September 14, 2021
- 37. de Bruin B: Age differences in COVID-19 risk perceptions and mental health: evidence from a national US survey conducted in March 2020. J Gerntol B Psychol Sci Soc Sci 2020; 76(2): e24–9.doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Steele I, Thrower N, Noroian P, Saleh F: Understanding suicide across the lifespan: a United States perspective of suicide risk factors, assessment and management. J Forensic Sci 2018; 63(1): 162–71.doi: 10.1111/556-4029.13519. [DOI] [PubMed] [Google Scholar]
- 39. Britton P, Ilgen M, Bohnert K, et al. : Shorter- and longer-term risk for suicide among male US military veterans in the year after discharge from psychiatric hospitalization. J Clin Psychiatry 2021; 82(2): 19m13228.doi: 10.4088/JCP.19m13228. [DOI] [PubMed] [Google Scholar]
- 40. Troyer E, Kohn J, Hong S: Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Beh Imm 2020; 87: 34–9.doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. De Berardis D, Gianfelice G, Fornaro M, et al. : A possible next COVID-19 pandemic: the violence against women and its psychiatric consequences. Front Psychiatry 2021; 12: 650671.doi: 10.3389/fpsyt.2021.650671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Palframan K, Szymanski B, McCarthy J: Ascertainment of patient suicides by Veterans Affairs facilities and associations with veteran, clinical, and suicide characteristics. Am J Publ Health 2021; 111(S2): S116–25.doi: 10.2105/AJPH.2021.306262. [DOI] [PMC free article] [PubMed] [Google Scholar]


