Abstract
A choledochal cyst (CC) is a rare congenital anomaly manifested as cystic dilatation of the biliary tree. A giant choledochal cyst is defined as a cyst with a maximum diameter of ≥ 10 cm. It is an unusual entity and rarely revealed in adulthood. We describe the case of a giant, infected CC presenting as acute pancreatitis with results of abdominal ultrasound and computed tomography consistent with a pancreatic pseudocyst. The diagnosis of CC was made on magnetic resonance cholangiopancreatography (MRCP) findings. We proceeded with cholecystectomy and the complete resection of the diverticulum after its dissection. The defect in the common bile duct was closed transversally over a T-tube. At the last follow-up two years after his admission, the patient is symptom-free with normal liver enzymes
To the best of our knowledge, this is the first case reported of giant CC complicated with both infection and pancreatitis
Keywords: general surgery, magnetic resonance cholangiopancreatography, acute pancreatitis, pancreatic pseudocyst, choledochal cyst
Introduction
A choledochal cyst (CC) is a rare congenital anomaly manifested as cystic dilatation of the biliary tree. A giant choledochal cyst is defined as a cyst with a maximum diameter of ≥ 10 cm. It is an unusual entity and rarely revealed in adulthood [1]. From 1977, the Todani classification has become the basic system of classification of choledochal cysts. Type II CC is very rare (2-3%) and appears as an extrahepatic, supraduodenal diverticulum [2].
In adults, choledochal cysts are mostly asymptomatic. Rarely, biliary perforation, hepatic abscess, biliary cirrhosis, and acute pancreatitis may be the first presentation [3]. Small CC can be easily diagnosed with radiology. However, a large CC can compress the adjoining organs such as the liver, head of the pancreas, duodenum and right kidney and appear to arise from these organs. However, accurate preoperative diagnosis is important to manage such large cysts.
We describe the case of giant, infected CC presenting as acute pancreatitis and misdiagnosed as a pancreatic pseudocyst. To the best of our knowledge, this is the first case reported in the literature, and surgeons should consider this pathology while treating pancreatic pseudocysts.
Case presentation
A 43-year-old man presented with severe abdominal pain, nausea, and vomiting for four days. The pain was dull aching in nature, paroxysmal, and unrelated to food and without jaundice. The patient has had episodic epigastric and right upper quadrant abdominal pain for the last two years, which was not explored. He was a current smoker with regular consumption of alcohol. On physical examination, he was febrile (temperature of 38.5 °Celsius), had tachycardia, and had tenderness in the epigastric and right upper quadrant. Laboratory investigations revealed leukocytosis and elevated pancreatic enzymes.
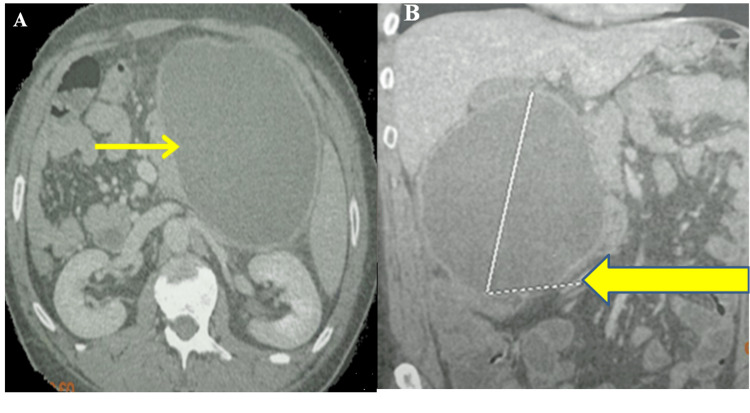
Contrast-enhanced computed tomography of the abdomen (CT) showed a round, well-circumscribed fluid collection of 17 x 10 cm with a thick enhancing wall suggestive of pancreatic pseudocyst with interstitial edematous pancreatitis (Figure 1).
Figure 1. Contrast-enhanced computed tomography showing a round, well-circumscribed fluid collection of 17 x 10 cm (yellow arrow) on axial (A) and coronal sections (B).
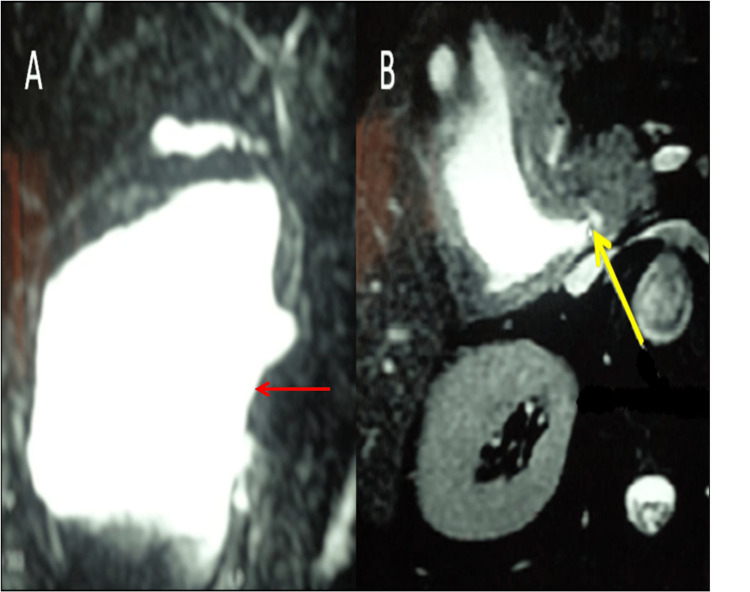
Based on the clinical and imaging findings, a provisional diagnosis of infected pancreatic pseudocyst was made. Broad-spectrum antibiotics and fluid resuscitation were started immediately and CT-guided percutaneous drainage of this collection was performed, bringing 2 liters of infected bile colonized by Staphylococcus aureus on bacteriological examination. Due to the presence of bile in the drainage fluid, we performed a magnetic resonance cholangiopancreatography (MRCP), which revealed a giant cyst of 20 x 16 cm arising from the supraduodenal extrahepatic bile duct without dilatation of extra and intrahepatic ducts suggestive of Type II CC as per Todani classification (Figure 2).
Figure 2. Magnetic resonance cholangiopancreatography showing a giant cystic formation of 20 x 16 cm arising from the supraduodenal extrahepatic bile duct (A) and the defect in the common bile duct (yellow arrow) (B).
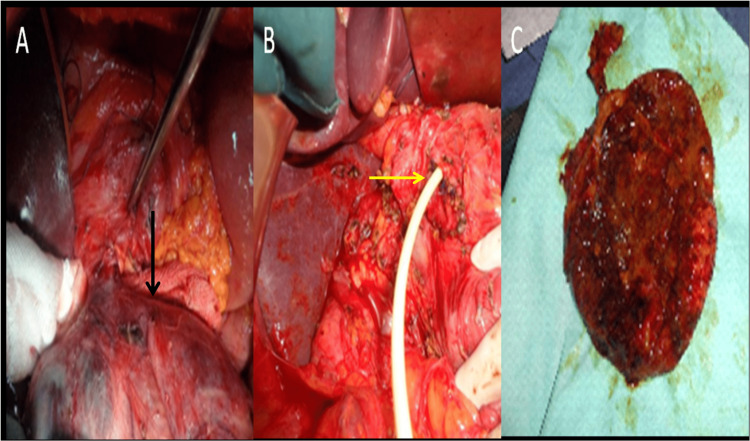
Intra-operatively, the diverticulum was located at the middle part of the extrahepatic biliary tree pushing the duodenum and the pancreas. We proceeded with cholecystectomy and the complete resection of the diverticulum after its dissection. The defect in the common bile duct was closed transversally over a T-tube (Figure 3).
Figure 3. Intra-operative images showing saccular diverticulum in the right upper quadrant (black arrow) (A); the defect in the common bile closed over a T-tube (yellow arrow) (B); and the specimen of the excised choledochal cyst (C).
The excised choledochal cyst was sent for histopathological examination and showed no evidence of malignancy. The patient was discharged after five days of hospitalization. A postoperative cholangiography showed a non-dilated common bile duct, no stones, and normal passage to the duodenum. At the last follow-up two years after his admission, the patient is symptom-free with normal liver enzymes and tumor markers.
Discussion
Todani type II choledochal cysts are very rare and account for 2-3% of all bile duct cysts. Also known as a bile duct diverticulum, saccular cysts represent a true diverticulum arising from the supraduodenal extrahepatic bile duct. They represent a predominantly pediatric pathology, but in 20% of cases, they can also be found in adults, with a higher incidence in females [3-6]. In adults, choledochal cysts are rarely symptomatic and incidentally discovered [4].
Most of the giant CCs are of type IVA and type I, according to Todani’s classification. The symptoms are more severe for giant CCs compared to non-giant CCs, and the classical triad of pain, abdominal mass, and jaundice was present in the majority of the patients with giant CCs [1,5]. Several cases of giant cysts (over 10 cm) were reported in the literature, mostly discovered in the context of a complication linked to their significant size [3, 5, 7].
Differential diagnosis of CC includes intraabdominal cystic lesion of the mesentery, peritoneum, pancreas or gastrointestinal tract [1,8]. CC can be misdiagnosed as a pancreatic cystic lesion or duodenal duplication cyst. Acute pancreatitis is rarely reported as a presentation of giant CCs in adults. Giant CCs mimicking a pancreatic pseudocyst and having complications of both infection and acute pancreatitis have not yet been reported. MRCP and the ERCP (endoscopic retrograde cholangiopancreaticography) are the most sensitive imaging studies for the diagnosis of CCs [1, 3, 5].
Surgery is the treatment choice for CCs to avoid the risk of complications such as pancreatitis, choledocholithiasis, or malignant degeneration. The surgical treatment depends on Todani classification and includes complete cyst excision (including gallbladder) with biliary-enteric anastomosis if the common bile duct is affected [1, 2,5]. The surgical procedure involves complete resection of the lesion, cholecystectomy, choledochorraphy and without biliary-enteric reconstruction. Traditionally, laparotomy is the common surgical approach to giant choledochal cysts. However, laparoscopic surgery has successful results, especially for pediatric patients [1, 6,9].
Conclusions
Giant CC is a very rare entity in the spectrum of congenital bile duct abnormality with few cases reported in the literature. The diagnosis requires high clinical suspicion and should be included in the differential diagnosis while treating a cystic pancreatic lesion. Also, to the best of our knowledge, this is the first case reported of giant CC complicated with both infection and pancreatitis.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Sahloul Hospital Ethics Committee issued approval U2347. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
References
- 1.Tactics, techniques, and challenges in the management of giant choledochal cyst in adolescents and adults: a retrospective cohort study. Kumar S, Singla S, Kumar S, Singh RK, Raj AK, Mandal M. Langenbecks Arch Surg. 2021;406:1925–1933. doi: 10.1007/s00423-021-02209-6. [DOI] [PubMed] [Google Scholar]
- 2.Challenges of surgical treatment of atypical giant choledochal cyst with the absence of gallbladder in adult patient. Rasic I, Mahmutovic N, Custovic S, Hasic N, Gavrankapetanovic A, Beciragic E, Brzika S. Case Rep Surg. 2022;2022:9605612. doi: 10.1155/2022/9605612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giant choledochal cyst in an adult at a teaching hospital in South-Western Uganda: a case report. Sikhondze MM, Cabrera Dreque C, Tayebwa E, Tumubugane G, Odongo CN, Ogwang E. Int Med Case Rep J. 2021;14:789–795. doi: 10.2147/IMCRJ.S340751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simultaneous laparoscopic removal of a Todani type II choledochal cyst and a microlithiasic cholecystitis. Grottesi A, Iacovitti S, Ciano P, Borrini F, Zippi M. Ann Hepatobiliary Pancreat Surg. 2022;26:281–284. doi: 10.14701/ahbps.22-011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ulcerated choledochocele: a case report. Ray-Offor E, Elenwo SN, Igwe PO, Ngeribara C. Int J Surg Case Rep. 2016;28:42–44. doi: 10.1016/j.ijscr.2016.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Laparoscopic resection of choledochal cysts in adults: a series from Turkey. Gündoğan E, Sümer F, Çolakoğlu MK, Çiçek E, Gökler C, Aydın MC, Kayaalp C. Turk J Surg. 2019;35:223–226. doi: 10.5578/turkjsurg.4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Open surgical treatment of choledochocele: a case report and review of literature. Yang J, Xiao GF, Li YX. World J Clin Cases. 2018;6:842–846. doi: 10.12998/wjcc.v6.i14.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.A giant retroperitoneal simple mesothelial cyst. Ergenç M, Uprak TK. ANZ J Surg. 2022;92:908–909. doi: 10.1111/ans.17195. [DOI] [PubMed] [Google Scholar]
- 9.Imaging diagnosis of a giant choledochal cyst in an infant. Grover SB, Malhotra S, Pandey S, Grover H, Kale R, Devra AG. Radiol Case Rep. 2022;17:404–411. doi: 10.1016/j.radcr.2021.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]