ABSTRACT
Studies have identified teacher effects on students’ attitudes. This study explored the differences in and associations between teachers’ and students’ COVID-19 vaccine hesitancy, and the factors that affect it. A population-based self-administered online survey was conducted to evaluate the COVID-19 vaccine hesitancy of teachers and students in a college in Taizhou, China. A total of 835 valid questionnaires were obtained. All data were analyzed using IBM SPSS statistics 26.0 software. The proportions of COVID-19 vaccine hesitancy for teachers and students were 31.7%, and 23.8%, respectively. In the binary logistic regression analysis, teachers who perceived the safety of the COVID-19 vaccine as low (OR = 6.794 , 95%CI: 1.701–27.143), did not pay continuous attention to the vaccine news (OR = 3.498, 95%CI: 1.150–10.640), and suffered chronic diseases (OR = 2.659, 95%CI: 1.135–6.227) were more likely to hesitate to get vaccinated against COVID-19. The group of students who perceived the COVID-19 vaccine safety as being low (OR = 1.805, 95%CI: 1.094–2.979) were more hesitant to get the COVID-19 vaccine. While both teachers and students were hesitant about the COVID-19 vaccine, teachers were found to be more so. Perceptions regarding the safety of COVID-19 vaccines, attention to and awareness of vaccine news, and chronic medical conditions were the main factors that influenced the hesitation regarding COVID-19 vaccines. Therefore, students’ vaccine hesitancy may depend largely on the perceptions of the vaccine’s safety rather than teachers’ vaccine hesitancy.
KEYWORDS: COVID-19, vaccine hesitancy, teachers and students, comparative studies, China
Introduction
The coronavirus disease 2019 (COVID-19) was classified as a pandemic and serious public health threat in 2020.1 Vaccination is a key preventive measure to constrain the COVID-19 pandemic, and many countries have developed free vaccination programs.2
Vaccination rates have historically varied by region and vaccine-specific characteristics, however, vaccine hesitancy remains an important factor influencing the process.3 In 2015, the World Health Organization’s (WHO) Strategic Advisory Group of Experts on Immunization (SAGE) defined vaccine hesitancy as “the delayed acceptance or refusal of vaccination despite the availability of vaccination services”4. According to recent surveys, there is a high degree of COVID-19 vaccination hesitancy worldwide.5 For example, cross-sectional surveys in the United States, Turkey, the UK, Brazil, Egypt, Sub-Saharan Africa and Italy show that the hesitation rate of the COVID-19 vaccine was 42.4% (in 2020),6 45.3% (in 2021),7 20.7% (in 2021),8 10.5% (in 2020),9 41.9% (in 2021),10 49% (in 2021),11 and 31.1% (in 2021),12 respectively. Furthermore, studies have revealed that hesitancy of the COVID-19 vaccine is common among the general population in China13 as hesitancy proportions were: 54.7% in Hong Kong (in 2020),14 19.2% in Macao (in 2021),15 35.5% in Beijing (in 2021),16 and 41.2% in Southwest China (2021).17 Vaccine hesitancy is an ongoing problem, and a better understanding of the phenomenon and its determinants in specific populations can develop more effective and targeted vaccination strategies.
The Theory of Planned Behavior (TPB) has been used to analyze individuals’ attitudes toward COVID-19 vaccination.18 According to the TPB, the attitude toward vaccination partly depends on the subjective norm, which refers to individuals’ perceptions of judgment from society members.18
Studies have shown that certain sub-populations have an increased risk of contagion, such as college students who often live and study in crowded settings.19 Teachers play significant roles in schools particularly those with boarding facilities. Studies have identified teacher effects on students’ attitudes and behaviors.20 Therefore, this study asks the following questions. To what extent does teachers’ vaccine hesitancy influence students’ vaccine hesitancy through subjective norms? What are the factors that affect vaccine hesitancies among teachers and students?
Until recently, vaccine hesitancy between teachers and students had rarely been studied. A study in the United States (in 2020) indicated that only 60% of faculty members and 45% of students expressed their readiness to receive a COVID-19 vaccine.21 Accordingly, we conducted a comparative study on COVID-19 vaccine hesitancy between teachers and students in a Chinese college, to explore the extent to which teachers’ vaccine hesitancy affects that of students’ and investigate the factors that influence vaccine hesitancy among teachers and students.
Methods and materials
Study design and population
In 2021, there were 110 colleges in Zhejiang Province, four of which were in Taizhou.22 We conducted a cross-sectional study at an occupational College in Taizhou in June 2021, which consisted of more than 11,000 students and 600 teachers. An online questionnaire was designed through the WeChat-incorporated Wen-Juan-Xing platform (Changsha Ranxing Information Technology Co., Ltd., Hunan, China), the largest online survey platform in China, and a Quick Response (QR) code was generated. A convenient sample of 246 teachers and 1963 students received the invitation for the survey through WeChat. The respondents answered the questionnaire by scanning the QR code on their mobile phones. Of those invited,167 teachers (response rate: 67.9%) and 1,237 students (response rate: 63.0%) completed the self-administered questionnaire. Subsequently, 167 teachers were matched 1:4 with students by gender.23–26 In total, 835 valid questionnaires were obtained. This study was exempted from informed consent and approved by the Ethics Committee of Taizhou Hospital of Zhejiang Province (Approval number: K20210520) in China. All procedures were performed in accordance with the guidelines of the institutional ethics committee and adhered to the tenets of the Declaration of Helsinki. The participants’ information was remained anonymous throughout.
Structured questionnaires
A self-administered questionnaire was designed for this study. The contents of the questionnaire were: (1) basic demographic information, such as age, sex, grade level, residence, and underlying diseases; (2) The respondents were asked, “Do you hesitate to get the COVID-19 vaccine for yourself (Whether you are vaccinated or not)?” (four items: very hesitant, hesitant, unhesitant, or very unhesitant); (3) perceptions of the COVID-19 vaccine, tested by two questions: “Do you think current COVID-19 vaccines are safe?” (four items: very safe, safe, unsafe, or very unsafe) and “How long do you think the protective effect will last after vaccination?” (four items: 3 months, 6 months, 12 months, others); (4) knowledge about vaccination against COVID-19, measured by: “Which of the following conditions do you think is suitable for vaccination against COVID-19?” (three items: yes, no, or unclear); (5) risk perception of COVID-19, measured by: “How do you perceive the risk of the SARS-CoV-2?” (five items: very high, high, general, low, and very low); and (6) vaccination awareness, measured by: “Have you pay attention to the news of COVID-19 vaccine constantly” (yes or no). All of the questions were closed, with checkboxes provided for responses.
Statistical analyses
The primary outcome of the survey was the hesitancies of teachers and students regarding COVID-19 vaccination. Counts and frequency distributions were displayed for classified data. The McNemar test and paired sample t-test were used to a preliminarily compare teachers’ and students’ hesitancies, and potential factors related to vaccine hesitancy, such as sex, age, residence, chronic disease, knowledge and views about the COVID-19 vaccine, and risk perceptions of COVID-19. Thereafter, χ2 (chi-square) tests were used to compare the differences between the hesitancy and no hesitancy groups in both teachers and students. The potential factors associated with their hesitancy were also assessed using the chi-square test.
Binary logistic regression was conducted to identify the factors associated with teachers’ and students’ vaccine hesitancies, with the odds ratio (OR) and a 95% confidence interval (CI) being calculated. Variables significant at the P < 0.05 level in the bivariate analyses were included in the model. All data were analyzed using IBM SPSS statistics 26.0 software (SPSS Inc., Chicago, IL, USA). A P-value of <0.05 was considered to represent a statistically significant difference or association among the test populations.
Results
A total of 835 valid questionnaires was obtained, including 167 teachers and 668 students. Among them, 37.1% of teachers and 23.8% of students were classified as hesitant to inoculate the COVID-19 vaccine (Figure 1), thus indicating that the proportion of teachers’ hesitancy regarding COVID-19 vaccination was significantly higher than that of students.
Figure 1.
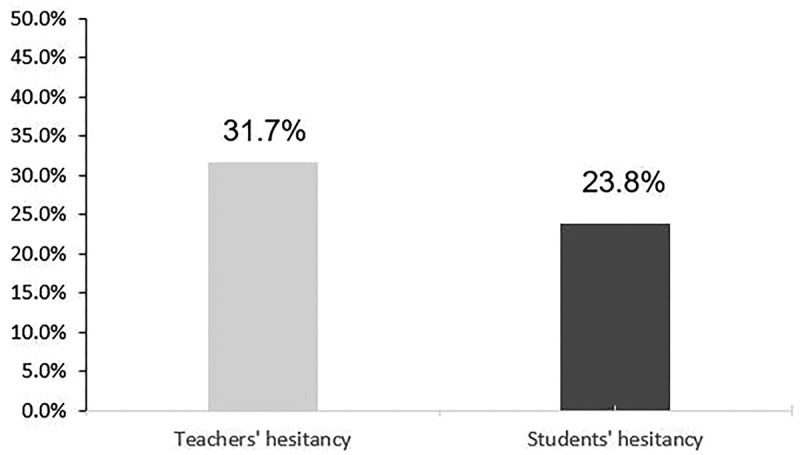
Different hesitancy between teachers and students.
Descriptive analysis
Table 1 shows the demographic information of the participants and their differences in potential factors related to COVID-19 vaccine hesitancy. Teachers were found to be older than students (teachers: 42.50 ± 8.51 years old; students: 19.13 ± 0.57 years old), include more participants living in urban areas (teachers: 95.8%; students: 24.3%), and have a higher proportion of chronic diseases (teachers: 18.6%; students: 2.4%), and are more hesitant about COVID-19 vaccination (teachers: 37.1%; students: 25.4%). Teachers were more likely than students to believe that COVID-19 vaccines are safe (92.2%; students: 87.7%), and more teachers thought that the effective time of the COVID-19 vaccine was less than or equal to six months (teachers: 59.3%; students: 50.1%). Moreover, teachers scored higher regarding knowledge of COVID-19 vaccines (total score: 22; teachers: 11.93 ± 6.19; students: 7.19 ± 5.70) and had a higher proportion of participants with low risk perceptions of COVID-19 (teachers: 59.9%; students: 55.8%). In addition, the proportion of teachers who paid attention to the news of COVID-19 vaccinations constantly was also higher than that of students (teachers: 89.8%; students: 82.0%).
Table 1.
The disparity of COVID-19 vaccine hesitancy and factors associated with hesitancy between teachers and students in a college (n = 835).
| Variables | Categories | Teachers (n=167) | Students (n=668) |
|---|---|---|---|
| Age(years)* | 42.50 ± 8.51 | 19.13 ± 0.57 | |
| Grade level | Freshman | / | 59 (8.8) |
| Sophomore | / | 457 (68.4) | |
| Junior | / | 152 (22.8) | |
| Sex | Male | 64 (38.3) | 256 (38.3) |
| Female | 103 (61.7) | 412 (61.7) | |
| Residence | Rural/Town | 7 (4.2) | 506 (75.7) |
| City | 160 (95.8) | 162 (24.3) | |
| Do you suffer from chronic diseases? | |||
| Yes | 31 (18.6) | 16 (2.4) | |
| No | 136 (81.4) | 652 (97.6) | |
| Have you ever hesitated to get the COVID-19 vaccine? | |||
| Hesitancy | 53 (31.7) | 159 (23.8) | |
| No hesitancy | 114 (68.3) | 509 (76.2) | |
| Views on the safety of the COVID-19 vaccine | |||
| High security | 154 (92.2) | 586 (87.7) | |
| Low security | 13 (7.8) | 82 (12.3) | |
| How long do you think the protective effect will last after vaccination? | |||
| ≤6 months | 99 (59.3) | 335 (50.1) | |
| > 6 months | 68 (40.7) | 333 (49.9) | |
| Score of knowledge about vaccination against COVID-19 | |||
| 11.93 ± 6.19 | 7.19 ± 5.70 | ||
| Risk perception of COVID-19 | High risk | 67 (40.1) | 295 (44.2) |
| Low risk | 100 (59.9) | 373 (55.8) | |
| Have you been pay attention to the news of COVID-19 vaccine constantly? | |||
| Yes | 150 (89.8) | 548 (82.0) | |
| No | 17 (10.2) | 120 (18.0) | |
Data were expressed as number followed by proportion in the parentheses within teachers and students.
*Data on age and score of knowledge about vaccination against COVID-19 were continuous, expressed as mean ± standard deviation (SD).
Factors affecting vaccine hesitation
As shown in Table 2, teachers’ hesitancy about the COVID-19 vaccine was related to their perception of COVID-19 vaccine safety (χ2 = 12.258, P < 0.001), whether they paid attention to the news of COVID-19 vaccine constantly (χ2 = 6.410, P = 0.020), and whether they suffered from chronic diseases (χ2 = 4.871, P = 0.027). However, students’ vaccine hesitancy was related to their residence (χ2 = 4.106, P = 0.043), perception of COVID-19 vaccine safety (χ2 = 8.422, P = 0.004), and their risk perception of COVID-19 (χ2 = 4.647, P = 0.031).
Table 2.
Bivariate analysis of factors associated with hesitancy between teachers and students (n = 835).
| Variables | Categories | Teachers (n=167) |
χ2 | P | Students (n=668) |
χ2 | P | ||
|---|---|---|---|---|---|---|---|---|---|
| Hesitancy (n=53) | No hesitancy (n=114) | Hesitancy (n=159) | No hesitancy (n=509) | ||||||
| Sex | Male | 16 (30.2) | 48 (42.1) | 2.174 | 0.140 | 51 (32.1) | 205 (40.3) | 3.446 | 0.063 |
| Female | 37 (69.8) | 66 (57.9) | 108 (67.9) | 304 (59.7) | |||||
| Age(years)* | 40.92 ± 7.366 | 43.23 ± 8.950 | 1.753 | 0.082 | 19.14 ± 0.549 | 19.13 ± 0.582 | 0.363 | 0.717 | |
| Grade level | Freshman | / | 14 (8.8) | 45 (8.8) | 0.032 | 0.984 | |||
| Sophomore | / | 108 (67.9) | 349 (68.6) | ||||||
| Junior | / | 37 (23.3) | 115 (22.6) | ||||||
| Residence | Rural/Town | 4 (7.5) | 3 (2.6) | 2.177 | 0.140 | 130 (81.8) | 376 (73.9) | 4.106 | 0.043 |
| City | 49 (92.5) | 111 (97.4) | 29 (18.2) | 133 (26.1) | |||||
| Do you suffer from chronic diseases? | |||||||||
| Yes | 15 (28.3) | 16 (14.0) | 4.871 | 0.027 | 6 (3.8) | 10 (2.0) | 1.696 | 0.193 | |
| No | 38 (71.7) | 98 (86.0) | 153 (96.2) | 499 (98.0) | |||||
| Views on the safety of the COVID-19 vaccine | |||||||||
| High security | 43 (81.1) | 111 (97.4) | 12.258 | <0.001 | 129 (81.1) | 457 (89.8) | 8.422 | 0.004 | |
| Low security | 10 (18.9) | 3 (2.6) | 30 (18.9) | 52 (10.2) | |||||
| How long do you think the protective effect will last after vaccination? | |||||||||
| ≤6 months | 37 (69.8) | 62 (54.4) | 3.566 | 0.059 | 90 (56.6) | 245 (48.1) | 3.477 | 0.062 | |
| >6 months | 16 (30.2) | 52 (45.6) | 69 (43.4) | 264 (51.9) | |||||
| Score of knowledge about vaccination against COVID-19* | |||||||||
| 11.6 ± 6.071 | 12.08 ± 6.283 | 0.460 | 0.646 | 7.24 ± 5.553 | 7.17 ± 5.754 | 0.135 | 0.893 | ||
| Risk perception of COVID-19 | High risk | 24 (45.3) | 43 (37.7) | 0.862 | 0.353 | 82 (51.6) | 213 (41.8) | 4.647 | 0.031 |
| Low risk | 29 (54.7) | 71 (62.3) | 77 (48.4) | 296 (58.2) | |||||
| Have you been pay attention to the news of COVID-19 vaccine constantly? | |||||||||
| Yes | 43 (81.1) | 107 (93.9) | 6.410 | 0.011 | 131 (82.4) | 417 (81.9) | 0.018 | 0.894 | |
| No | 10 (18.9) | 7 (6.1) | 28 (17.6) | 92 (18.1) | |||||
Data were expressed as number followed by proportion in the parentheses within hesitancy or no hesitancy between teachers and students.
*Data on age and score of knowledge about vaccination against COVID-19 were continuous, expressed as mean ± standard deviation (SD), and compared the differences between hesitancy group and no hesitancy group using t-test.
Regression analysis
Table 3 shows the regression analysis of factors affecting teachers’ and students’ COVID-19 vaccine hesitancies. Among teachers, those who perceived the COVID-19 vaccine safety to be low (OR = 6.794 , 95%CI: 1.701–27.143), did not pay attention to news regarding the COVID-19 vaccine (OR = 3.498 , 95%CI: 1.150–10.640), and had chronic diseases (OR = 2.659 , 95%CI: 1.135–6.227) were more hesitant to get the COVID-19 vaccine. Regarding students, those who perceived the COVID-19 vaccine to be less safe were more hesitant than those who perceived the vaccine as safe (OR = 1.805 , 95%CI: 1.094–2.979).
Table 3.
Binary logistic regression analysis of factors associated with hesitancy between teachers and students.
| Variables | Categories | Teachers (n=167) |
Students (n=668) |
||
|---|---|---|---|---|---|
| P | OR (95%CI) | P | OR (95%CI) | ||
| Residence | Rural/Town vs City (Ref) | / | 0.122 | 1.432 (0.908–2.259) | |
| Do you suffer from chronic diseases? | Yes vs No (Ref) | 0.024 | 2.659 (1.135–6.227) | / | |
| Views on the safety of the COVID-19 vaccine | Low vs High (Ref) | 0.007 | 6.794 (1.701–27.143) | 0.021 | 1.805 (1.094–2.979) |
| Risk perception of COVID-19 | High vs Low (Ref) | / | 0.107 | 1.350 (0.937–1.945) | |
| No vs Yes (Ref) | 0.027 | 3.498 (1.150–10.640) | / | ||
OR: odds ratio; CI: confidence interval.
Discussion
Vaccine hesitancy, which refers to the “delayed acceptance or refusal of vaccination despite the availability of vaccination services,”4 is an important factor that affects vaccination and the achieving or maintaining of herd immunity.3 Many studies have shown that people’s hesitancy of the Influenza vaccine, Measles vaccine, Varicella vaccine, and other vaccines is common.27 However, the COVID-19 vaccine, newly developed in 2020, has a limited application time,28 therefore, hesitation regarding this vaccine is more common than others’.29 According to a global systematic review, low rates of COVID-19 vaccine acceptance were reported in the Middle East, Russia, Africa, and several European countries; nevertheless, high rates were found in East and South East Asia.30 This discrepancy may be due to variations in the spread of the pandemic across the relevant countries.
In this study, COVID-19 vaccine hesitancy was found to be higher among teachers (37.1%) than students (23.8%). Thus, we can imply that students’ vaccine hesitancy may depend largely on the perceptions of the vaccine’s safety rather than subjective norms (i.e., teachers’ vaccine hesitancy).
Educational background has been found to be a factor affecting vaccination and can be applicable to the above result. Zhang et al. showed that people with higher educational backgrounds are more hesitant to inoculate the COVID-19 vaccine than those with lower educational backgrounds (i.e., the students in this study vs. the teachers).27 Furthermore, the difference in methods used to gain information between students and teachers may be further reason for the difference in hesitancies.31 At present, the hesitancy of collegial students in different countries (such as Italy, France, and Jordan) is 13.9%–42.0%32–34. Bai et al. have shown that the students’ hesitancy about COVID-19 vaccination in a Chinese university is 23.7%19. However, a study in Ethiopia established that about 59.2% of participant teachers were unwilling to accept the vaccine against the COVID-19 pandemic.35
The factors influencing vaccine hesitancy are complex and summarized by the WHO’s Strategic Advisory Group of Experts on Immunization (SAGE) as follows: 1. Background influences (such as historical, socio-cultural, economic or political factors); 2. Individual and group influences; 3. Impacts directly related to vaccines or vaccination (such as vaccination schedules, sources of supply, costs, etc.).4 In this study, the main factors influencing teachers’ hesitancy regarding the COVID-19 vaccine were found to be: their perceptions of COVID-19 vaccine’s safety, whether they paid attention to the news regarding COVID-19 vaccines, and whether they had chronic diseases. The factor that affected student COVID-19 vaccine hesitancy was the perceptions of the vaccine’s safety.
Research has shown that concerns regarding the COVID-19 vaccine’s safety in different countries and populations are gradually becoming the most prominent factor relating to the hesitancy of COVID-19 vaccine.6–29–36–41 Our study similarly found that a perception of low COVID-19 vaccine safety was a common predictor of vaccine hesitancy among teachers and students. It is concordant with the findings of Manning et al. who noted concerns about the safety and side effects of the COVID-19 vaccine to be associated with the reluctance to get vaccinated.21 Thus, it follows that a negative attitude (such as vaccine hesitancy) arises when individuals perceive the risks of the vaccination to outweigh the benefits there of.42 Furthermore, lack of knowledge about the COVID-19 vaccine is also one of the factors associated with vaccine hesitancy.43 To a certain extent, paying attention to news regarding COVID-19 and its vaccine can effectively increase public understanding, thus, reduce COVID-19 vaccine hesitancy. This aspect is well demonstrated in our regression analysis of teacher’ hesitancy as those who did not follow the COVID-19 vaccine news were more hesitant regarding vaccination (OR = 3.498 95%CI: 1.150–10.640). The social media is widely used and is an effective way to increase public awareness about COVID-19 vaccine through its instant communication and wide audience reach.44
As in the case of Abedin et al., in this study, chronic diseases were found to be a risk factor that affects teachers’ vaccine hesitancy.45 Suffering chronic diseases lowered the odds of being willing to take the vaccine, which is consistent with findings from a few developed countries such as the UK.46 In the initial analysis, we found that teachers suffering from chronic diseases were higher than students. Teachers with chronic diseases are more concerned about vaccines affecting their preexisting conditions, which might be the reason for the difference between teachers and students.
Limitations
An advantage of this study is that teachers and students were paired for comparison regarding gender; it allowed a clearer explanation of the influence of other factors on vaccine hesitancy as it controlled for gender differences. There are several limitations to this study. First, we conducted a cross-sectional study, in which teachers’ and students’ attitudes toward vaccination may change over time, especially after changes in domestic epidemics. Second, the sample in this study was selected in a particular region in China; therefore, local backgrounds may affect the generalizability of the survey results and the results may not fully represent the vaccine hesitancy of all university teachers and students nationally. Third, our questionnaire is not in the form of a scale; therefore, it is difficult to assess the reliability and validity of the study and add a scree plot. Also, there are selection bias and reporting bias in our study, which may be addressed in the future by following up on large sample sizes. Finally, other unknown confounding factors may still impact the results. These limitations should be addressed in future studies on this topic.
Conclusion
Vaccination and promotion are the basis of disease prevention and control. Our research on COVID-19 vaccine hesitancy, based on a college sample, found that teachers and students are both hesitant about the COVID-19 vaccine, and teachers have higher hesitancy than students. Perceptions about the safety of COVID-19 vaccines, awareness of and attention to vaccine news, and chronic medical conditions were the main factors that determined the hesitation of COVID-19 vaccines. Therefore, students’ vaccine hesitancy may depend largely on the perceptions of the vaccine’s safety rather than teachers’ vaccine hesitancy.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Author contributions
J.S. Z. and T.H.T. conceived the study. M.X.Z., J.S. Z. and T.H.T. designed the questionnaire. J.S. Z. collected the data. Y.C. analyzed and interpreted the data and wrote the first draft of the paper. X.Q.L. and H.W. searched, sorted, and interpreted the relevant literature. All authors edited and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Cucinotta D, Vanelli M.. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):1–7. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.King I, Heidler P, Marzo RR. The long and winding road: uptake, acceptability, and potential influencing factors of COVID-19 vaccination in Austria. Vaccines (Basel). 2021;9(7). doi: 10.3390/vaccines9070790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jacobson RM, St Sauver JL, Finney Rutten LJ. Vaccine hesitancy. Mayo Clin Proc. 2015;90(11):1562–1568. doi: 10.1016/j.mayocp.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 4.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Wang W, Wu Q, Yang J, Dong K, Chen X, Bai X, Chen X, Chen Z, Viboud C, Ajelli M, et al. Global, regional, and national estimates of target population sizes for covid-19 vaccination: descriptive study. BMJ. 2020;371:m4704. doi: 10.1136/bmj.m4704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ikiisik H, Akif Sezerol M, Tasci Y, Maral I. COVID-19 vaccine hesitancy: a community-based research in Turkey. Int J Clin Pract. 2021;75(8):e14336. doi: 10.1111/ijcp.14336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sethi S, Kumar A, Mandal A, Shaikh M, Hall CA, Kirk JMW, et al. The UPTAKE study: a cross-sectional survey examining the insights and beliefs of the UK population on COVID-19 vaccine uptake and hesitancy. [DOI] [PMC free article] [PubMed]
- 9.Moore D, Nehab MF, Camacho KG, Reis AT, Junqueira-Marinho MF, Abramov DM, et al. Low COVID-19 vaccine hesitancy in Brazil. [DOI] [PMC free article] [PubMed]
- 10.El-Sokkary RH, El Seifi OS, Hassan HM, Mortada EM, Hashem MK, Gadelrab M, et al. Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: a cross-sectional study. [DOI] [PMC free article] [PubMed]
- 11.Acheampong T, Akorsikumah EA, Osae-Kwapong J, Khalid M, Appiah A, Amuasi JH. Examining vaccine hesitancy in Sub-Saharan Africa: a survey of the knowledge and attitudes among adults to receive COVID-19 vaccines in Ghana. Vaccines. 2021;9(8):814. LID - 10.3390/vaccines9080814 [doi] LID - vaccines9080814 [pii]. doi: 10.3390/vaccines9080814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reno C, Maietti E, Fantini MP, Savoia E, Manzoli L, Montalti M, Gori D. Enhancing COVID-19 vaccines acceptance: results from a survey on vaccine hesitancy in Northern Italy. Vaccines. 2021;9(4):378. doi: 10.3390/vaccines9040378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines (Basel). 2020;8(3):482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luk TT, Zhao S, Wu Y, Wong JY, Wang MP, Lam TH. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: a population-based survey. [DOI] [PMC free article] [PubMed]
- 15.Ung COL, Hu Y, Hu H, Bian Y. Investigating the intention to receive the COVID-19 vaccination in Macao: implications for vaccination strategies. [DOI] [PMC free article] [PubMed]
- 16.Wang C, Han B, Zhao T, Liu H, Liu B, Chen L, et al. Vaccination willingness, vaccine hesitancy, and estimated coverage at the first round of COVID-19 vaccination in China: a national cross-sectional study. [DOI] [PMC free article] [PubMed]
- 17.Li M, Zheng Y, Luo Y, Ren J, Jiang L, Tang J, et al. Hesitancy toward COVID-19 vaccines among medical students in Southwest China: a cross-sectional study. [DOI] [PMC free article] [PubMed]
- 18.Fan CW, Chen I-O, Ko NA-O, Yen CF, Lin C-O, Griffiths M-O, et al. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. [DOI] [PMC free article] [PubMed]
- 19.Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, Liu R, Cheung T, Su Z, Ng CH, et al. Attitudes toward COVID-19 vaccines in Chinese college students. Int J Biol Sci. 2021;17(6):1469–1475. doi: 10.7150/ijbs.58835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blazar D, Kraft MA. Teacher and teaching effects on students’ attitudes and behaviors. Educ Eval Policy Anal. 2017;39(1):146–170. doi: 10.3102/0162373716670260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manning ML, Gerolamo AM, Marino MA, Hanson-Zalot ME, Pogorzelska-Maziarz M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nurs Outlook. 2021;69(4):565–573. doi: 10.1016/j.outlook.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Statistical bulletin on the development of education in Zhejiang Province in 2020. [accessed 2021 June 14]. http://jyt.zj.gov.cn/art/2021/6/21/art_1229266680_4667519.html.
- 23.Saoud R, Abou Heidar N, Aizen J, Andolfi C, Galansky L, Ahmed O, Shalhav AL. Long term renal function following selective angioembolization for iatrogenic vascular lesions after partial nephrectomy: a matched case-control study. Investig Clin Urol. 2021;62(3):267–273. doi: 10.4111/icu.20200510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin K-K, Lee J-S, Hou C-H, Chen W-M, Hsiao C-H, Chen Y-W, Yeh C-T, See L-C. The sociodemographic and risk factors for keratoconus: nationwide matched case-control study in Taiwan, 1998-2015. Am J Ophthalmol. 2021;223:140–148. doi: 10.1016/j.ajo.2020.09.040. [DOI] [PubMed] [Google Scholar]
- 25.R Charlier SH, Meier C, Jick SS, Meier CR, Becker C. Association between glycemic control and risk of venous thromboembolism in diabetic patients: a nested case–control study. Cardiovasc Diabetol. 2022;21(1):2. doi: 10.1186/s12933-021-01432-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim SY, Kim H-J, Lim H, Kong IG, Kim M, Choi HG. Bidirectional association between gastroesophageal reflux disease and depression: two different nested case-control studies using a national sample cohort. Sci Rep. 2018;8(1):11748. doi: 10.1038/s41598-018-29629-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang MX, Lin XQ, Chen Y, Tung TH, Zhu JS. Determinants of parental hesitancy to vaccinate their children against COVID-19 in China. Expert Rev Vaccines. 2021;20(10):1339–1349. doi: 10.1080/14760584.2021.1967147. [DOI] [PubMed] [Google Scholar]
- 28.Tregoning JS, Flight KE, Higham SL, Wang Z, Pierce BF. Progress of the COVID-19 vaccine effort: viruses, vaccines and variants versus efficacy, effectiveness and escape. Nat Rev Immunol. 2021;21(10):626–636. doi: 10.1038/s41577-021-00592-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hou Z, Tong Y, Du F, Lu L, Zhao S, Yu K, Piatek SJ, Larson HJ, Lin L. Assessing COVID-19 vaccine hesitancy, confidence, and public engagement: a global social listening study. J Med Internet Res. 2021;23(6):e27632. doi: 10.2196/27632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brauer E, Choi K, Chang J, Luo Y, Lewin B, Munoz-Plaza C, Bronstein D, Bruxvoort K. Health care providers’ trusted sources for information about COVID-19 vaccines: mixed methods study. JMIR Infodemiology. 2021;1(1):e33330. doi: 10.2196/33330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tavolacci MP, Dechelotte P, Ladner J. COVID-19 vaccine acceptance, hesitancy, and resistancy among university students in France. Vaccines (Basel). 2021;9(6). doi: 10.3390/vaccines9060654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35(8):781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sallam M, Dababseh D, Eid H, Hasan H, Taim D, Al-Mahzoum K, Al-Haidar A, Yaseen A, Ababneh NA, Assaf A, et al. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among university students in Jordan. Int J Environ Res Public Health. 2021;18(5):2407. doi: 10.3390/ijerph18052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shitu K, Wolde M, Handebo S, Kassie A. Acceptance and willingness to pay for COVID-19 vaccine among school teachers in Gondar City, Northwest Ethiopia. Trop Med Health. 2021;49(1):63. doi: 10.1186/s41182-021-00337-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Freeman D, Loe BS, Chadwick A, Vaccari C, Waite F, Rosebrock L, Jenner L, Petit A, Lewandowsky S, Vanderslott S, et al. COVID-19 vaccine hesitancy in the UK: the oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020:1–15. doi: 10.1017/S0033291720005188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luk TT, Zhao S, Wu Y, Wong JY, Wang MP, Lam TH. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: a population-based survey. Vaccine. 2021;39(27):3602–3607. doi: 10.1016/j.vaccine.2021.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yahia AIO, Alshahrani AM, Alsulmi WGH, Alqarni MMM, Abdulrahim TKA, Heba WFH, et al. Determinants of COVID-19 vaccine acceptance and hesitancy: a cross-sectional study in Saudi Arabia Hum Vaccin Immunother. 2021;17(11):4015–4020. doi: 10.1080/21645515.2021.1950506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Del Riccio M, Boccalini S, Rigon L, Biamonte MA, Albora G, Giorgetti D, et al. Factors influencing SARS-CoV-2 vaccine acceptance and hesitancy in a population-based sample in Italy. Vaccines (Basel). 2021;9(6):633. doi: 10.3390/vaccines9060633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alabdulla M, Reagu SM, Al-Khal A, Elzain M, Jones RM. COVID-19 vaccine hesitancy and attitudes in Qatar: a national cross-sectional survey of a migrant-majority population. Influenza Other Respir Viruses. 2021;15(3):361–370. doi: 10.1111/irv.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jain J, Saurabh S, Kumar P, Verma MK, Goel AD, Gupta MK, Bhardwaj P, Raghav PR. COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect. 2021;149:e132. doi: 10.1017/S0950268821001205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hudson A, Montelpare WJ. Predictors of vaccine hesitancy: implications for COVID-19 public health messaging. Int J Environ Res Public Health. 2021;18(15):8054. doi: 10.3390/ijerph18158054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Griffith J, Marani H, Monkman H. COVID-19 vaccine hesitancy in canada: content analysis of tweets using the theoretical domains framework. J Med Internet Res. 2021;23(4):e26874. doi: 10.2196/26874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Witteman HO, Zikmund-Fisher BJ. The defining characteristics of web 2.0 and their potential influence in the online vaccination debate. Vaccine. 2012;30(25):3734–3740. doi: 10.1016/j.vaccine.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 45.Abedin M, Islam MA, Rahman FN, Reza HM, Hossain MZ, Hossain MA, Arefin A, Hossain A. Willingness to vaccinate against COVID-19 among Bangladeshi adults: understanding the strategies to optimize vaccination coverage. PLoS One. 2021;16(4):e0250495. doi: 10.1371/journal.pone.0250495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bono SA, Faria de Moura Villela E, Siau CS, Chen WS, Pengpid S, Hasan MT, Sessou P, Ditekemena JD, Amodan BO, Hosseinipour MC, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low- and middle-income countries. Vaccines. 2021;9(5):515. doi: 10.3390/vaccines9050515. [DOI] [PMC free article] [PubMed] [Google Scholar]


