Abstract
Background
Ivuxolimab (PF-04518600) and utomilumab (PF-05082566) are humanized agonistic IgG2 monoclonal antibodies against OX40 and 4-1BB, respectively. This first-in-human, multicenter, open-label, phase I, dose-escalation/dose-expansion study explored safety, tolerability, pharmacokinetics, pharmacodynamics, and antitumor activity of ivuxolimab+utomilumab in patients with advanced solid tumors.
Methods
Dose-escalation: patients with advanced bladder, gastric, or cervical cancer, melanoma, head and neck squamous cell carcinoma, or non-small cell lung cancer (NSCLC) who were unresponsive to available therapies, had no standard therapy available or declined standard therapy were enrolled into five dose cohorts: ivuxolimab (0.1–3 mg/kg every 2 weeks (Q2W)) intravenously plus utomilumab (20 or 100 mg every 4 weeks (Q4W)) intravenously. Dose-expansion: patients with melanoma (n=10) and NSCLC (n=20) who progressed on prior anti-programmed death receptor 1/programmed death ligand-1 and/or anti-cytotoxic T-lymphocyte-associated antigen 4 (melanoma) received ivuxolimab 30 mg Q2W intravenously plus utomilumab 20 mg Q4W intravenously. Adverse events (AEs) were graded per National Cancer Institute Common Terminology Criteria for Adverse Events V.4.03 and efficacy was assessed using Response Evaluation Criteria in Solid Tumors (RECIST) V.1.1 and immune-related RECIST (irRECIST). Paired tumor biopsies and whole blood were collected to assess pharmacodynamic effects and immunophenotyping. Whole blood samples were collected longitudinally for immunophenotyping.
Results
Dose-escalation: 57 patients were enrolled; 2 (3.5%) patients with melanoma (0.3 mg/kg+20 mg and 0.3 mg/kg+100 mg) achieved partial response (PR), 18 (31.6%) patients achieved stable disease (SD); the disease control rate (DCR) was 35.1% across all dose levels. Dose-expansion: 30 patients were enrolled; 1 patient with NSCLC achieved PR lasting >77 weeks. Seven of 10 patients with melanoma (70%) and 7 of 20 patients with NSCLC (35%) achieved SD: median (range) duration of SD was 18.9 (13.9–49.0) weeks for the melanoma cohort versus 24.1 (14.3–77.9+) weeks for the NSCLC cohort; DCR (NSCLC) was 40%. Grade 3–4 treatment-emergent AEs were reported in 28 (49.1%) patients versus 11 (36.7%) patients in dose-escalation and dose-expansion, respectively. There were no grade 5 AEs deemed attributable to treatment. Ivuxolimab area under the concentration–time curve increased in a dose-dependent manner at 0.3–3 mg/kg doses.
Conclusions
Ivuxolimab+utomilumab was found to be well tolerated and demonstrated preliminary antitumor activity in selected groups of patients.
Trial registration number
Keywords: Therapies, Investigational; Drug Therapy, Combination; Immunomodulation; Immunotherapy
WHAT IS ALREADY KNOWN ON THIS TOPIC
Ivuxolimab (PF-04518600) and utomilumab (PF-05082566) are human, agonistic monoclonal antibodies (IgG2) specific for OX40 and 4-1BB, respectively.
Single-agent ivuxolimab or utomilumab has demonstrated safety and preliminary antitumor activity in patients with solid tumors.
This first-in-human, phase I, dose-escalation and dose-expansion study investigated the safety, tolerability, pharmacokinetics, pharmacodynamics, and antitumor activity of combination treatment with ivuxolimab and utomilumab in patients with advanced solid tumors.
WHAT THIS STUDY ADDS
Ivuxolimab in combination with utomilumab was well tolerated and demonstrated preliminary antitumor activity in selected groups of patients.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The current study supports the further assessment of this novel regimen in various combinational studies.
Introduction
Activation and expansion of tumor-specific T cells is a therapeutic strategy to enhance antitumor immune responses and improve clinical outcomes in patients with cancer.1 The tumor necrosis factor receptor superfamily members OX40 (CD134) and 4-1BB play critical roles in T-cell activation, proliferation, and survival; therefore, they represent important pathways in the development of novel cancer immunotherapies.2–14 In lymphocytes, OX40 is preferentially expressed on CD4+ T cells versus CD8+ T cells, whereas 4-1BB is expressed to a greater extent on CD8+ than CD4+ T cells.8 13 In preclinical tumor models, including melanoma, dual co-stimulation through OX40 and 4-1BB has been shown to induce clonal expansion of CD4+ and CD8+ T cells, as well as increased cytokine secretion (ie, interferon-γ and tumor necrosis factor-α), and cytotoxicity, of T cells.15–23
Ivuxolimab (PF-04518600) and utomilumab (PF-05082566) are human, agonistic monoclonal antibodies (IgG2) specific for OX40 and 4-1BB, respectively.5 7 Agonistic engagement of OX40 by ivuxolimab resulted in T-cell proliferation and cytokine secretion as well as tumor growth inhibition in preclinical models.7 The 4-1BB binding by utomilumab induced nuclear factor kappa B activation with downstream cytokine production, lymphocyte proliferation, and antitumor responses in human xenograft tumor models.5 Furthermore, ivuxolimab and utomilumab combination treatment resulted in T-cell expansion and tumor growth inhibition in a preclinical colorectal tumor model.24
A phase I study of single-agent ivuxolimab in patients with advanced solid tumors showed no dose-limiting toxicities (DLTs) at the dose levels evaluated. Furthermore, single-agent ivuxolimab induced T-cell clonal expansion in the peripheral blood and demonstrated dose-proportional exposure and preliminary antitumor activity in patients with hepatocellular carcinoma or melanoma, suggesting its suitability for combination with other cancer immunotherapies.14 Administration of single-agent utomilumab in patients with a wide range of advanced malignancies has demonstrated a tolerable safety profile with no DLTs, mostly grade 1–2 adverse events (AEs), no clinically significant hepatotoxicity (observed with another anti-4-1BB antibody, urelumab11), and preliminary antitumor activity against Merkel cell carcinoma and advanced solid tumors of gastrointestinal origin.10
In a phase Ib study, utomilumab in combination with the anti-programmed death receptor 1 (PD-1) antibody pembrolizumab was not associated with DLTs and induced durable antitumor responses in patients with advanced non-small cell lung cancer (NSCLC), small cell lung cancer, anaplastic thyroid carcinoma, renal cell carcinoma, and squamous cell carcinoma of the head and neck (HNSCC).25 In addition, utomilumab in combination with the anti-CD20 antibody rituximab demonstrated a favorable safety profile and clinical activity in patients with treatment-resistant/refractory CD20+ non-Hodgkin’s lymphoma.26 No increased or unexpected AEs were reported with utomilumab in combination with either pembrolizumab or rituximab compared with single-agent administration.25 26
In this first-in-human, phase I, dose-escalation and dose-expansion study, we investigated the safety, tolerability, pharmacokinetics (PK), pharmacodynamics, and antitumor activity of ivuxolimab in combination with utomilumab in patients with advanced solid tumors. In the dose-expansion part of the study, safety and clinical activity of this novel antibody combination were evaluated in two cohorts of previously treated patients with malignant melanoma or advanced NSCLC, including patients who had received prior immune checkpoint inhibitor therapy (ie, anti-PD-1/PD ligand 1 (PD-L1) with or without anti-cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4)) antibodies).
Patients and methods
Study design and treatment
In this multicenter, open-label, multiple-dose, phase I study, we investigated ivuxolimab in combination with utomilumab in patients with advanced solid tumors (part B), following initial assessment of single-agent ivuxolimab (part A), as previously reported.14 Briefly, in the dose-escalation portion of Part A, initial cohorts of two to four patients per dose group (0.01, 0.1, 0.3, 1.5, 3, and 10 mg/kg) were enrolled, with a staggered start, to evaluate DLTs.14 Once the DLT period for a given dose level was completed for the last enrolled patient and the next higher dose level was opened, it could have been expanded to approximately 10 patients to create a tumor biopsy backfill cohort for pharmacodynamic evaluation.14
Part B included dose-escalation and dose-expansion portions. Primary objectives of dose-escalation were to assess safety and tolerability, and to estimate the maximum tolerated doses (MTD) for the combination. Sequential, predefined dose levels of ivuxolimab (0.1, 0.3, 1.0, and 3 mg/kg) administered intravenously every 2 weeks (Q2W) were evaluated in combination with 20 mg or 100 mg of utomilumab intravenously every 4 weeks (Q4W) in adult patients with advanced bladder, gastric, or cervical cancer, melanoma (ocular, mucosal, or cutaneous), HNSCC, or NSCLC who were unresponsive to available therapies or for whom no standard therapy was available.
Primary objectives in dose expansion were to further assess safety and tolerability, and to determine the recommended phase 2 dose for the combination in patients with advanced melanoma or NSCLC. Based on the results obtained in dose escalation, the dose selected for the ivuxolimab/utomilumab expansion cohorts was ivuxolimab 30 mg (a flat dose equivalent to 0.3 mg/kg) intravenously Q2W in combination with utomilumab 20 mg intravenously Q4W. When both antibodies were given on the same day, ivuxolimab was administered at least 30 min after completing the utomilumab infusion. Patients received study drugs until disease progression, intolerable toxicity, or withdrawal of consent.
Secondary objectives were to characterize PK, immunogenicity, and preliminary antitumor activity of ivuxolimab in combination with utomilumab. Pharmacodynamic evaluations (ie, immunomodulatory effects in peripheral blood and tumor tissues) were included as exploratory objectives.
Patients
Adult patients eligible for the dose-escalation portion of the study had advanced NSCLC; HNSCC; cutaneous, mucosal, or ocular melanoma; urothelial cell carcinoma; gastric cancer; or squamous cell carcinoma of the uterine cervix and had progressed on or were intolerant to standard therapy. Eligibility criteria for patients included in the melanoma or NSCLC dose-expansion portion (with locally advanced/metastatic disease) included (a) ocular melanoma or (b) cutaneous/acral or mucosal melanoma, or (c) NSCLC with disease progression following prior treatment with immune checkpoint inhibitors (ie, anti-PD-1/PD-L1 and/or anti-CTLA-4 antibodies). Patients had to have measurable disease by Response Evaluation Criteria in Solid Tumors (RECIST) V.1.1; Eastern Cooperative Oncology Group performance status 0–1; and adequate bone marrow, renal, and hepatic functions.
Patients were not included in the study if they had known symptomatic brain metastases requiring systemic corticosteroid therapy; however, they were eligible if they had discontinued corticosteroid treatment for ≥4 weeks and were neurologically stable. Furthermore, patients were not enrolled if they had a history of active autoimmune disorders; an active bacterial, fungal, or viral infection; bleeding esophageal or gastric varices within 2 months of study enrollment; or unmanageable ascites. Patients were also excluded if they had undergone major surgery or had received radiation or systemic anticancer therapy within 4 weeks of enrollment; had clinically significant cardiac disease; had a history of grade ≥3 immune-mediated AEs related to prior immunomodulatory therapy (ie, immune checkpoint inhibitors); or required systemic immunosuppressive therapy (ie, ≥10 mg of prednisone or equivalent (≥1.5 mg of dexamethasone)) at the time of study entry. Prior treatment with an OX40 or 4-1BB agonist was not allowed.
The study followed the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice guidelines. The study was sponsored by Pfizer (registered at ClinicalTrials.gov).
Assessments
Safety and DLT
AEs were collected and characterized by type, frequency, timing, seriousness, and relationship to study treatment. The severity of the AEs occurring in treated patients was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events V.4.03.
Any of the following AEs occurring in the first two treatment cycles (28 days) was classified as DLT, unless related to the underlying disease or to disease progression: grade 4 neutropenia lasting >7 days, febrile neutropenia, grade ≥3 neutropenic infection, grade ≥3 thrombocytopenia with clinically significant bleeding, grade 4 thrombocytopenia, grade 4 anemia, grade 3 anemia related to hemolysis or autoimmune disease, and grade ≥3 maximally treated non-hematologic AEs (ie, nausea, vomiting, diarrhea) or grade ≥3 manageable, non-hematologic toxicities considered clinically significant (including cytokine release syndrome and infusion or allergic reactions). Immune-related AEs that occurred from day 29 to day 98 of assessment and met DLT criteria were considered late, immune-related DLTs.
PK and immunogenicity
Blood samples for PK analyses were collected at protocol-defined time points: day 1 (pre-dose and 1, 4, and 24 hours post-dose) and day 8 (pre-dose) in cycle 1, day 1 in cycle 2 (pre-dose and 1 hour post-dose), days 1 (pre-dose and 1 hour post-dose) and 8 (pre-dose) in cycle 3, day 1 (pre-dose and 1 hour post-dose) in cycles 4–6, day 1 in cycle 7 (pre-dose), and day 1 (pre-dose) of every other cycle thereafter. Blood samples were evaluated using validated electrochemiluminescence methods. Serum PK parameters were estimated using non-compartmental analysis.
Levels of anti-drug antibody (ADA) and neutralizing antibodies (NAb) against study drugs were determined in samples collected from treated patients at protocol-predefined time points, using a validated electrochemiluminescence assay and a cell-based assay, respectively.10
Antitumor activity
Objective tumor responses were assessed every 6 weeks in dose-escalation and every 8 weeks in dose-expansion, for 24 weeks, and then every 12 weeks until confirmed disease progression as determined using RECIST V.1.1 and immune-related RECIST (irRECIST).27 28 Responses and disease progression by irRECIST were confirmed at least 4 weeks after first documentation. Responses were summarized in terms of best overall response (BOR), duration of response, time to progression and progression.
Tumor immunohistochemistry
Paired biopsy samples were collected from patients at baseline and at cycle 4 day 1. The 4 µm slides (formalin-fixed paraffin-embedded, stained tissue sections) were stained with an anti-CD4 antibody from Leica, clone NCL-L-CD4-368; anti-CD8 antibody from Dako, clone M7103; anti-FOXP3 antibody from Abcam, clone ab20034; and anti-OX40 antibody from BD Bioscience, 555836. Tissues were analyzed for expression of CD4, CD8, FOXP3, and OX40 (in dose-escalation portion) or CD8 and OX40 (in dose-expansion portion) by automated image analysis, (Flagship automated tissue analysis CellMap0.8 software) using an algorithm developed and validated at Flagship Biosciences (Westminster, Colorado, USA).
Statistical analyses
A modified toxicity probability interval method, targeting a DLT rate of 25%, with an acceptable DLT interval of 20%–30%, was used for dose escalation. The estimated MTD was the highest tested combination dose level associated with a mean DLT rate ≤0.25 in at least nine DLT-evaluable patients.
Objective response was summarized with objective response rate (ORR) and exact, two-sided 95% CI. Time-to-event endpoints (ie, median progression-free survival) were analyzed with the Kaplan-Meier method and presented with 95% CIs.
Patient involvement statement
There were no funds or time allocated for patient and public involvement, so we were unable to involve patients.
Results
Patients
Patient demographic and baseline characteristics are summarized in table 1 for all patients on study. In the dose-escalation portion of the study, 57 patients received escalating intravenous doses of ivuxolimab (mg/kg) plus utomilumab (20 or 100 mg) in five subsequent cohorts: 0.1+20 (n=11); 0.3+20 (n=12); 0.3+100 (n=12); 1+100 (n=11); and 3+100 (n=11) (cut-off date: November 25, 2019). Patients enrolled in the dose-escalation portion had malignant melanoma (31.6%, including 4 (7%) patients with ocular melanoma) or advanced HNSCC (21.1%), gastric cancer (15.8%), urothelial cancer (12.3%), or cervical cancer (8.8%) as primary tumor diagnosis. In the two dose-expansion cohorts, 20 patients with advanced NSCLC and 10 patients with malignant melanoma (including 1 patient with choroidal melanoma and 1 patient with mucosal melanoma) received intravenous ivuxolimab 30 mg plus utomilumab 20 mg (flat doses).
Table 1.
Patient demographic and baseline characteristics
| Ivuxolimab+utomilumab | ||
| Dose escalation n=57 | Dose expansion n=30 | |
| Male : female, n (%) | 30 (52.6) : 27 (47.4) | 20 (66.7) : 10 (33.3) |
| Age, mean (range), years | 60.9 (22–85) | 61.8 (41–76) |
| ≥65 years of age, n (%) | 25 (43.9) | 13 (43.3) |
| Race, n (%) | ||
| White | 42 (73.7) | 20 (66.7) |
| Black | 0 | 1 (3.3) |
| Asian | 11 (19.3) | 4 (13.3) |
| Other | 4 (7.0) | 3 (10.0) |
| Unspecified | 0 | 2 (6.7) |
| ECOG PS, n (%) | ||
| 0 | 31 (54.4) | 12 (40.0) |
| 1 | 25 (43.9) | 18 (60.0) |
| Not reported | 1 (1.8) | 0 |
| Primary cancer diagnosis, n (%) | ||
| Bladder cancer | 7 (12.3) | 0 |
| Cervical cancer | 5 (8.8) | 0 |
| Gastric cancer | 9 (15.8) | 0 |
| HNSCC | 12 (21.1) | 0 |
| Melanoma | 18 (31.6)* | 10 (33.3)† |
| NSCLC | 6 (10.5) | 20 (66.7) |
| Prior systemic anticancer therapies | ||
| Yes, n (%) | 54 (94.7) | 29 (96.7) |
| No, n (%) | 3 (5.3) | 1 (3.3) |
| No. of prior therapies, mean (range) | 4 (1–11) | 4 (1–11) |
| Prior anti-CTLA-4 therapy, n (%) | 17 (29.8) | 5 (16.7) |
| Prior anti-PD-1 therapy, n (%) | 30 (52.6) | 27 (90.0) |
| Prior anti-PD-L1 therapy, n (%) | 6 (10.5) | 4 (13.3) |
| Prior chemotherapy, n (%) | 38 (66.7) | 19 (63.3) |
*Four patients in dose escalation had ocular melanoma.
†Includes one patient with choroidal melanoma and one patient with mucosal melanoma in dose expansion.
CTLA-4, cytotoxic T-lymphocyte-associated protein 4; ECOG PS, Eastern Cooperative Oncology Group performance status; HNSCC, head and neck squamous cell carcinoma; NSCLC, non-small cell lung cancer; PD-1, programmed death receptor 1; PD-L1, programmed death-ligand 1.
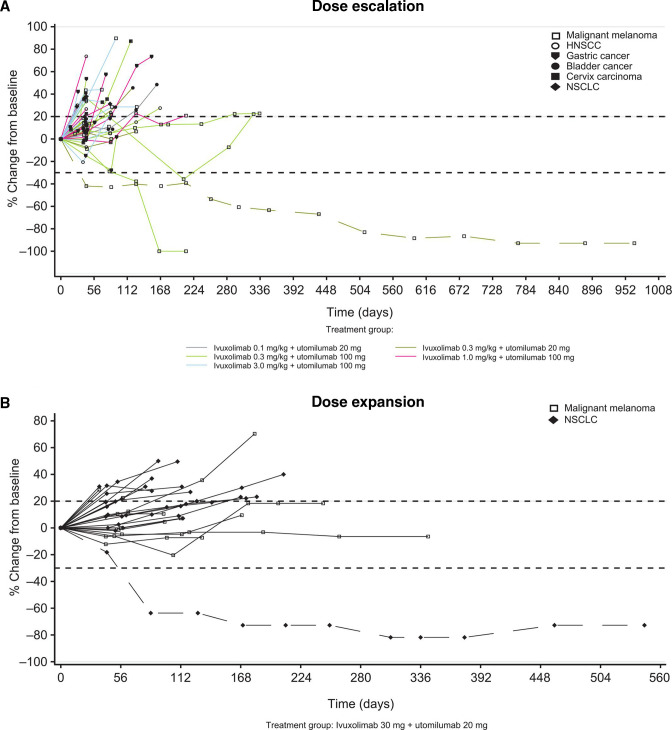
Most patients (94.7%, dose escalation; 96.7%, dose expansion) had received multiple lines of prior systemic anticancer therapy, including anti-CTLA-4, anti-PD-1, or anti-PD-L1 antibodies in the adjuvant or advanced disease setting (table 1, figure 1). Of the 30 patients with melanoma or NSCLC in the dose-expansion cohorts, 27 (90%) had been previously treated with an anti-PD-1 antibody, and 5 of 10 (50%) patients with melanoma had also received an anti-CTLA-4 antibody.
Figure 1.
Waterfall plot of tumor size change from baseline (best response) by RECIST. Dashed horizontal reference lines at 20% and –30% indicate the thresholds for RECIST V.1.1-defined objective progression and partial response, respectively. (A) Dose escalation and (B) dose expansion. CTLA-4, cytotoxic T-lymphocyte-associated protein 4; HNSCC, head and neck squamous cell carcinoma; NSCLC, non-small cell lung cancer; PD-1, programmed death receptor 1; PD-L1, PD-1 ligand 1; RECIST, Response Evaluation Criteria in Solid Tumors; uto, utomilumab.
Safety and DLT
In the dose-escalation portion of the study, grade 1–2 all-causality AEs (AEs of any causality) occurred in 23/57 (40.4%) patients and grade 3–4 AEs in 28/57 (49.1%) patients. Grade 5 events were reported in 6/57 (10.5%) patients due to disease progression (n=5) or euthanasia (n=1) (online supplemental table S1). Four (7%) of 57 patients discontinued treatment due to all-causality AEs: disease-related grade 3 pain in extremity, disease-related grade 4 hepatobiliary disorder, treatment-related grade 3 infusion-related reaction, and grade 4 colon perforation of unknown causality. In the dose-expansion portion of the study, 14/30 (46.7%) of patients had grade 1–2 all-causality AEs, and 11/30 (36.7%) grade 3–4 all-causality AEs. Five (16.7%) patients died on study due to all-causality AEs of: disease progression (n=2), pulmonary embolism (n=1), myocardial infarction (n=1), or seizure (n=1).
jitc-2022-005471supp001.pdf (4.5MB, pdf)
No DLTs were observed at the dose levels evaluated in either portion of the study (ivuxolimab ≤3 mg/kg Q2W plus utomilumab 100 mg Q4W). Administration of ivuxolimab in combination with utomilumab was generally associated with a favorable safety profile in both the dose-escalation and dose-expansion portions; most of the treatment-related AEs were grade 1–2 (table 2).
Table 2.
Treatment-related adverse events reported in ≥10% of patients (dose-expansion cohorts)*†
| AE, n (%) | Grade 1–2 | Grade 3–4 | Total |
| Any AE | 18 (60.0) | 5 (16.7) | 23 (76.7) |
| Pruritus | 6 (20.0) | 0 | 6 (20.0) |
| Anemia | 4 (13.3) | 0 | 4 (13.3) |
| Fatigue | 4 (13.3) | 0 | 4 (13.3) |
| Decreased appetite | 3 (10.0) | 0 | 3 (10.0) |
| Rash | 2 (6.7) | 1 (3.3) | 3 (10.0) |
*In addition, one patient each developed grade 3 treatment-related AEs of lymphopenia, maculopapular rash, rash erythematosus, and pustular rash. One patient experienced a grade 4, treatment-related increase in lipase. No patient had a grade 5 treatment-related AE.
†Treatment-related AEs considered immune-related included grade 4 increased lipase (n=1), grade 3 rash erythematosus (n=1), grade 3 maculopapular rash (n=1), grade 2 anemia (n=1), grade 2 pruritus (n=1), grade 1 pruritus (n=3), grade 1 rash (n=2), and grade 1 maculopapular rash (n=1).
AE, adverse event.
The most common treatment-related AEs, observed in ≥10% of patients in the dose-expansion cohorts, consisted of pruritus (20%), fatigue (13.3%), anemia (13.3%), decreased appetite (10%), and rash (10%) (table 2). One patient each developed grade 3 treatment-related AEs of lymphopenia, rash, pustular rash, immune-related rash erythematosus, and maculopapular rash. One patient with melanoma had an asymptomatic, grade 4 treatment-related and immune-related AE of increased lipase levels in cycle 5, which resolved with no change in study treatment. Other treatment-related AEs considered immune-related (grades 1–2) are listed in the footnote of table 2. None of the patients experienced a treatment-related serious AE or a treatment-related grade 5 AE.
In the dose-expansion cohorts, 2 (6.7%) patients discontinued study treatment due to an AE (grade 2 rash in a patient with melanoma and grade 3 diffuse left chest wall pain in a patient with NSCLC). Treatment interruptions due to treatment-related AEs were reported in 5 (16.7%) patients due to grade 3 rash (rash erythematosus, maculopapular rash, or rash) and grade 2 fatigue or elevation in alanine aminotransferase (n=1 each).
PK
PK and immunogenicity samples were collected from all 87 patients enrolled in dose escalation and dose expansion. Mean serum concentration profiles of ivuxolimab on cycle 1 day 1 (C1D1) and C3D1 are presented in online supplemental figure S1. Ivuxolimab PK parameters for C1D1 and C3D1 are summarized in online supplemental table S2. Following escalating intravenous doses of ivuxolimab administered in combination with utomilumab, ivuxolimab area under the concentration–time curve (AUCτ) appeared to increase in a dose-dependent manner for the 0.3 mg/kg–3 mg/kg dose range. Dose-normalized AUCτ (AUCτ(dn)) was lower at 0.1 mg/kg, consistent with that observed following ivuxolimab monotherapy in Part A, which may be in part due to target-mediated drug disposition. The variability (CV%) for AUCτ(dn) between the weight-based dosing group (0.3 mg/kg+100 mg) and flat dosing group (30 mg+20 mg) was similar. Accumulation ratio of ivuxolimab based on AUCτ ranged between 1.4 and 1.8 across the dose ranges studied, consistent with data from Part A monotherapy.
Utomilumab PK parameters summarized for C1D1 and C3D1 are presented in online supplemental table S3. AUCτ(dn) values of utomilumab following a single (C1D1) combination dosing with escalating doses of ivuxolimab appeared to be relatively similar, except for the group co-administrated with ivuxolimab 0.1 mg/kg. Following multiple-dose co-administration of utomilumab with escalating doses of ivuxolimab, AUCτ(dn) values of utomilumab exhibited relatively high variability, possibly due to the formation of ADA in some patients.
Immunogenicity
Assessment of ADA and NAb against ivuxolimab included 85 patients, of which there were 26 (30.6%) with treatment-induced ADA, 2 (2.4%) patients with treatment-boosted ADA, and 2 (2.4%) patients with NAb against ivuxolimab (both treatment-induced). Of the 28 patients with ADA against ivuxolimab, ADA responses in 19 (67.9%) patients were transient. Most ADA responses occurred at dose levels ≤0.3 mg/kg and 30 mg; there was a trend of lower rates of post-baseline ADA positivity with increasing ivuxolimab dose. The correlation between ivuxolimab Ctrough and immunogenicity status is presented in online supplemental figure S2.
The assessment of ADA and NAb against utomilumab included 80 patients; in 49 (61.3%) of these 80 patients ADA were induced post-treatment, in 5 (6.3%) patients ADA were pre-existent and boosted post-treatment. In 46 (57.5%) of the 80 patients NAb against utomilumab were detected (45 treatment-induced NAb and 1 treatment-boosted NAb). Most (64.8%) ADA responses were not persistent or transient and there was a trend for lower Ctrough in patients with ADA+ and NAb+ status (online supplemental figure S3).
Antitumor activity
In the dose-escalation portion, 2 (3.5%) of 57 patients, both with melanoma, achieved a partial response (PR), 1 in the 0.3 mg/kg+20 mg and 1 in the 0.3 mg/kg+100 mg dose group (figure 1A), whereas 18 (31.6%) patients had stable disease (SD), for a disease control rate (DCR) of 35.1% (ie, complete response (CR)+PR+SD) across all dose levels (table 3). Median duration of SD ranged from 12.3 to 23.9 weeks across dose levels. There was no difference in ORRs between RECIST and irRECIST assessments; a higher percentage of patients had immune-related SD (irSD) (45.6%) by irRECIST compared with SD by RECIST (31.6%).
Table 3.
Best overall response by RECIST
| Ivuxolimab+utomilumab | ||||||
| Dose escalation | Dose expansion | |||||
| 0.1 mg/kg +20 mg n=11 |
0.3 mg/kg +20 mg n=12 |
0.3 mg/kg +100 mg n=12 |
1 mg/kg +100 mg n=11 |
3 mg/kg +100 mg n=11 |
30 mg +20 mg N=30 |
|
| CR, n (%) | 0 | 0 | 0 | 0 | 0 | 0 |
| PR, n (%) | 0 | 1 (8.3) | 1 (8.3) | 0 | 0 | 1 (3.3) |
| SD, n (%) | 2 (18.2) | 5 (41.7) | 4 (33.3) | 4 (36.4) | 3 (27.3) | 14 (46.7) |
| PD, n (%) | 6 (54.5) | 4 (33.3) | 5 (41.7) | 6 (54.5) | 7 (63.6) | 12 (40.0) |
| Not evaluable, n (%) | 3 (27.3) | 2 (16.7) | 1 (8.3)* | 1 (9.1) | 1 (9.1) | 3 (10.0) |
| ORR, n (%) (95% exact CI) |
0 | 1 (8.3) (0.2 to 38.5) |
1 (8.3) (0.2 to 38.5) |
0 | 0 | 1 (3.3) (0.1 to 17.2) |
| DCR (CR+PR+SD), n (%) | 2 (18.2) | 6 (50.0) | 5 (41.7) | 4 (36.4) | 3 (27.3) | 15 (50.0) |
| Duration of SD, median (range), weeks | 14.9 (11.6–18.1) |
12.6 (5.9–138.1+)† |
23.9 (11.1–41.9) |
15.0 (10.9–18.3) |
12.3 (12.0–12.4) |
24.0 (13.9–77.9+)† |
*One additional patient in this dose group had indeterminate response.
†A patient with response or SD at last assessment remains on study.
CI, confidence interval; CR, complete response; DCR, disease control rate; ORR, objective response rate; PD, progressive disease; PR, partial response; RECIST, Response Evaluation Criteria in Solid Tumors; SD, stable disease.
One of the two melanoma patients with PR in the dose-escalation cohort had mucosal melanoma, whereas the other had uveal melanoma. Immune checkpoint inhibitors have low antitumor activity in these melanoma subtypes compared with cutaneous melanoma.29 The PR in the patient with metastatic mucosal melanoma lasted for >952 days (~31 months, still on study at data cut-off) (figure 2A). This patient had previously received combination therapy with ipilimumab and pembrolizumab followed by single-agent pembrolizumab for advanced disease, with BOR of PR for 9 months before progression, and thus had very limited standard treatment options. The other patient with melanoma with a PR had metastatic uveal melanoma and had not previously been treated with an immune checkpoint inhibitor. The ORR by RECIST in the 18 patients with melanoma in the dose-escalation portion of the study was 11.1% (95% exact CI 1.4% to 34.7%) and DCR was 38.9%.
Figure 2.
Tumor size change from baseline over time, by RECIST. Lines represent individual patients. Dashed horizontal reference lines at 20% and –30% indicate the thresholds for RECIST V.1.1-defined objective progression and partial response, respectively. (A) Dose escalation and (B) dose expansion. HNSCC, head and neck squamous cell carcinoma; NSCLC, non-small cell lung cancer; RECIST, Response Evaluation Criteria in Solid Tumors.
In the dose-expansion NSCLC cohort, one patient with stage IV lung adenocarcinoma achieved PR, which lasted >77 weeks (still on study at data cut-off) (figures 1B and 2B). This patient had received prior neoadjuvant chemotherapy with carboplatin/paclitaxel and nanoparticle albumin paclitaxel, and nivolumab therapy for ~19 weeks until ~10 weeks prior to start of study treatment, with a best response of SD. The ORR by RECIST in the dose-expansion NSCLC cohort (n=20) was 5% (95% exact CI 0.1% to 24.9%). In addition, 35% of patients with NSCLC achieved SD as best response, for a DCR of 40% (median duration of SD: 24.1 (range, 14.3–77.9+) weeks) (online supplemental table S4). Eleven (55%) patients in this NSCLC cohort had irSD by irRECIST, for an immune-related DCR of 60.0%.
None of the 10 patients in the dose-expansion melanoma cohort had tumor responses, whereas 70% of patients in this cohort achieved SD, with a median duration of 18.9 (range, 13.9–49.0) weeks. Comparable outcomes were observed by RECIST and irRECIST assessments of best response in this cohort.
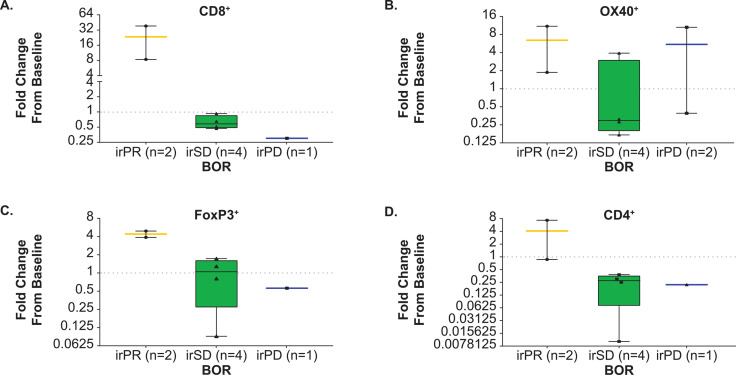
Assessment of immune cell populations in the tumor
Immunohistochemistry
Immunohistochemistry (IHC) assessments were performed using tissue from seven patients. There were two patients with a BOR or immune-related PR (irPR) included in the analysis. The first patient was a man in his mid 70s with ocular melanoma and history of prior radiotherapy, who was treated with 0.3 mg/kg ivuxolimab plus 100 mg utomilumab and achieved PR at week 18; the second patient was a woman in her mid 80s with cutaneous melanoma and history of prior pembrolizumab, who was treated with 0.3 mg/kg ivuxolimab plus 100 mg utomilumab. She initially had PD and discontinued all treatment at week 6 but achieved a delayed (unconfirmed) irPR at the next tumor assessment 5.5 months later. Consistent with the mechanism of action of the two study drugs, expression of CD8 was markedly increased in post-treatment tumors from both patients with irPR, whereas no increase of CD8 was seen in five non-responders. Similarly, expression of CD4 and FoxP3 was increased in the two patients with irPR, but not in four patients with irSD and one with immune-related PD (irPD). OX-40 was increased in both post-treatment tumors of two responders and two patients with irPD (figure 3, online supplemental figure S4).
Figure 3.
Fold-change from baseline in the percentage of immune cell types. Data are represented as the fold-change from baseline in the percent of each immune cell type, comparing the 6 weeks sample to baseline, and grouped by BOR using irRECIST criteria. The dashed horizontal line represents no change from baseline. One patient with baseline/on-treatment biopsies from different tumor sites and one patient with an indeterminate BOR were excluded from graphed analyses. For one patient with a BOR of irPD, data were evaluable for the OX40 measurement only. Paired biopsies were obtained from two patients with a BOR of irPR. Flagship automated tissue analysis was performed using the CellMap0.8 software platform. The 4 µM slides were stained with an anti-CD4 antibody from Leica, clone NCL-L-CD4-368; anti-CD8 antibody from Dako, clone M7103; anti-FOXP3 antibody from Abcam, clone ab20034; and anti-OX40 antibody from BD Bioscience, #555 836. BOR, best overall response; ir, immune-related; PD, progressive disease; PR, partial response; RECIST, Response Evaluation Criteria in Solid Tumors; SD, stable disease.
RNA expression analyses in tumors
Transcriptional profiles of bulk tumors confirmed upregulation of CD8 in patients with irPR. Gene ranking-based gene set enrichment analysis (Fast Gene Set Enrichment Analysis) on genes in order by statistics from differential analysis of the 10 paired biopsies, using the hallmark gene sets, indicated gene sets associated with immune activation and inflammation were among those most enriched (higher positive normalized enrichment score (NES)) with the lowest adjusted p values (online supplemental figure S5).
In the dose-escalation portion, differential gene expression was analyzed for 10 patients with paired biopsies across multiple doses. Paired differential analysis adjusted for tumor purity, estimated by Estimation of STromal and Immune cells in MAlignant Tumor tissues using Expression data, and comparing on-treatment (6 weeks) to baseline biopsy samples, revealed a significant upregulation of B cell immunoglobulin-heavy and immunoglobulin-light chain-related transcripts (online supplemental figure S6). In unsupervised clustering of NES of hallmark gene sets in response to treatment in each patient, the two patients who achieved PR or delayed PR (Patients 2 and 3, respectively), were most closely clustered, with increases in pro-inflammatory and immune-activation pathways at 6 weeks (online supplemental figure S7). Mutation burden at baseline was similar in patients who achieved PR or SD compared with those with PD (online supplemental figure S8).
In the dose-expansion portion, genome-wide RNA expression analysis of tissue from a subset of seven patients with NSCLC (those with an evaluable baseline biopsy) revealed a distinctly different global gene expression profile in the tumor from the patient with a PR (Patient 1) compared with the tumors of the other six patients who had objective PD or SD (online supplemental figure S9). Differential gene analysis of baseline tumor from the responding patient demonstrated lower expression of genes involved in immune-related pathways and higher expression of genes involved with biosynthesis as compared with the other six patients with NSCLC who did not have response to treatment. Based on RNA expression, the tumor from the patient with PR also had the lowest expression of FOXP3 and OX40, but not CD8. IHC analyses for OX40 and CD8 produced similar findings.
No on-treatment biopsy was available from the patient with PR; therefore, PD effects could only be evaluated for patients with SD/PD. Several patients with SD/PD had relatively small (±13%) changes in tumor size, even though substantial changes in CD8 expression were observed for some of these patients. Hence, the correlation between CD8 expression and time to progression was explored. Among patients evaluable for a response, paired biopsy analyses showed the largest increase in CD8 gene expression occurred in the patient with NSCLC who had the longest duration of SD. This result was confirmed by the IHC analysis of tumorous CD8 expression.
Discussion
Treatment with PD-1/PD-L1 or CTLA-4 immune checkpoint inhibitors can result in long-term tumor responses in patients with advanced solid malignancies across a wide range of tumor types.30–32 However, primary and/or secondary resistance to these inhibitors is observed in a substantial proportion of patients,33 34 suggesting that novel therapies, including immunomodulatory approaches, are needed to improve on clinical outcomes. Combined agonistic engagement of immune co-stimulatory molecules expressed by T cells, such as OX40 and 4-1BB, may contribute to induce CD8+ and CD4+ T-cell effectors, cytokine secretion (ie, interferon-γ), enhanced antitumor immune responses, and CD8+ T-cell survival, as previously observed in preclinical studies, including tumor models in melanoma, hepatocellular carcinoma, and other solid tumor types.15–21
In this first-in-human study of a novel immunomodulatory combination of the OX40 and 4-1BB agonistic antibodies ivuxolimab and utomilumab, the combination was generally associated with a tolerable safety profile in patients with advanced solid tumors enrolled in the dose-escalation and expansion cohorts, with no DLTs and mostly grade 1–2 treatment-related AEs. The MTD was not reached at the highest dose levels evaluated (ivuxolimab 3 mg/kg Q2W plus utomilumab 100 mg Q4W). Few (7%) patients discontinued due to an AE. These safety and tolerability profiles are consistent with those observed in prior single-agent studies.10 14
In the dose-expansion portion of this study, tumor responses were observed in patients with malignant melanoma and advanced NSCLC who had received multiple lines of prior systemic anticancer therapy, including immune checkpoint inhibitors. Some anecdotal, though intriguing, responses were observed in some patients with uveal or mucosal melanoma. However, further evaluation in a larger number of patients is needed to better characterize antitumor activity of this OX-40 and 4-1BB agonistic antibody combination in advanced uveal and mucosal melanoma.
The serum exposure of ivuxolimab and the incidence of ADA+ and NAb+ against ivuxolimab were found to be in the same range with those observed in ivuxolimab monotherapy.14 The higher immunogenicity against ivuxolimab at lower dose groups is unlikely to be associated with drug interference with the assay, but more likely a biological effect, which has been observed from other monoclonal antibodies.35 The serum exposure of utomilumab was lower and more variable than that observed in utomilumab monotherapy,14 potentially due to higher immunogenicity in the combination therapy compared with utomilumab monotherapy (41.8% treatment-induced ADA and 12.7% Nab+).10 The higher incidence of immunogenicity against utomilumab has been observed in combination therapies of utomilumab with pembrolizumab or mogamulizumab.25 36 Among the three patients with PR, all of them were Nab– for ivuxolimab but Nab+ for utomilumab. The effect of ADA on safety was assessed by evaluating hypersensitivity or infusion reaction AEs. One (4%) ivuxolimab ADA+ patient and one (2%) ivuxolimab ADA– patient experienced infusion-related reaction; both patients were ADA+ for utomilumab. However, the effect of immunogenicity on efficacy and safety cannot be concluded due to the small sample size.
Other OX40-targeted, combined immunomodulatory strategies are in development for anticancer therapy, including a PD1-Fc-OX40 ligand construct and a CTLA-4 × OX40 bispecific antibody, which can induce enhanced immune responses in vivo.37–39 These agents have demonstrated antitumor activity in preclinical tumor models (ie, bladder, colon, and pancreatic cancers), thus providing further support for a potential benefit from agonistic engagement of T-cell co-stimulatory receptors such as OX40.
Combination of ivuxolimab or ivuxolimab/utomilumab with other immunomodulatory agents, with different mechanisms of action within the tumor immune microenvironment, can potentially further enhance antitumor activity in patients with cancer. Hence, a triple combination of ivuxolimab, utomilumab, and the anti-PD-L1 antibody avelumab or a double combination of ivuxolimab (or utomilumab) and avelumab are currently in phase I/II trials in patients with advanced, solid malignancies (NCT02554812) plus/minus radiation therapy (NCT03217747). A combination of ivuxolimab or utomilumab with avelumab is also currently in a randomized phase II trial in patients with metastatic triple-negative breast cancer (NCT03971409). Furthermore, as OX40 and 4-1BB co-stimulation by agonistic antibodies may facilitate immune responses to immunogenic cancer vaccines or Toll-like receptor (TLR) agonists,40–42 an ongoing phase II trial (NCT02554812) is evaluating ivuxolimab or utomilumab in combination with avelumab and the TLR9 agonist CMP-001.43
In conclusion, this first-in-human study of the combination of OX40 (ivuxolimab) plus 4-1BB (utomilumab) agonistic antibody in patients with advanced solid tumors demonstrated safety and preliminary antitumor activity in selected groups of patients. Pharmacodynamic results provide evidence supporting an active, immunomodulatory mechanism for ivuxolimab in combination with utomilumab. Based on these findings, further assessment of this regimen is currently being pursued in various combinational studies.
Acknowledgments
The authors thank the patients and their families/caregivers, the investigators, research nurses, study coordinators, and operations staff, who contributed to this study. The authors also thank B Fu, B Ganguly, C Fleener, C Taylor, C Bermingham, J O’Quin, C Konto, S Potluri, K Ching, H I Krupka, K K Liao, and V Bonato for their contributions. Medical writing was provided by S Mariani, MD, PhD; Elyse Smith, PhD; and David Sunter, PhD, of Engage Scientific Solutions, and funded by Pfizer.
Footnotes
Twitter: @DrElkhoueiry
Contributors: All authors contributed to this study, data analysis and interpretation, and manuscript development. All authors approved the final version. OH is the guarantor and accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This study was sponsored by Pfizer.
Competing interests: OH reports consulting fees from Aduro, Akeso, Amgen, Beigene, Bioatia, Bristol Myers Squibb, Roche Genentech, GlaxoSmithKline, Immunocore, Idera, Incyte, Janssen, Merck, Nextcure, Novartis, Pfizer, Sanofi Regeneron, SeaGen, Tempus, and Zelluna; honoraria for speaker bureaus from Bristol Myers Squibb, Novartis, Pfizer, and Sanofi Regeneron; and participation on a data safety monitoring board or advisory board for Aduro, Akeso, Amgen, Beigene, Bioatia, Bristol Myers Squibb, Roche Genentech, GlaxoSmithKline, Immunocore, Idera, Incyte, Janssen, Merck, Nextcure, Novartis, Pfizer, Sanofi Regeneron, SeaGen, Tempus, and Zelluna. AAC reports grants or contracts from AstraZeneca and Bristol Myers Squibb; consulting fees from Jazz, Janssen, and Pfizer; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Amgen, Blueprint, Genentech, Merck, Novartis, and Takeda; and participation on a data safety monitoring board or advisory board for AstraZeneca, Bristol Myers Squibb, Ipsen, and Novartis. JAT reports grants or contracts from Pfizer. TD reports grants or contracts to his institution from AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Daiichi Sankyo, Eisai, Eli Lilly, IQVIA, Janssen Pharma, Merck Serono, MSD, Novartis, Pfizer, Sumitomo Dainippon, and Taiho; consulting fees from AbbVie, Bayer, Chugai Pharma, Otuska Pharma, Rakuten Medical, Sumitomo Dainippon, Taiho, and Takeda; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Bristol Myers Squibb, Oncolys Bio Pharma, Ono Pharma, Rakuten Medical, and Taiho; and participation on a data safety monitoring board or advisory board for AbbVie, Amgen, Astellas Pharma, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Janssen Pharma, MSD, and Novartis. SH-L reports consulting fees from Amgen, Astellas, Bristol Myers Squibb, Genmab, Merck, Regeneron, and Xencor; and research grants from Astellas, Boehringer Ingelheim, Checkmate, Dragonfly, F Star, Kite Pharma, Merck, OncoC4, Vedanta, and Xencor. AD reports grants or contracts from Apexigen, Idera, and Nektar; and consulting fees from Idera and Nektar. J-PS reports consulting fees from AstraZeneca, Bristol Myers Squibb, Daiichi-Sakyo, Gilead, GlaxoSmithKline, LeoPharma, Eli Lilly, MSD, Mylan, Novartis, Pierre Fabre Oncology, Pfizer, Roche Genentech; and support for attending meetings and/or travel from Amgen, AstraZeneca, and Pfizer. NR reports research grants from Pfizer; personal fees from AbbVie, Apricity Therapeutics, AstraZeneca, Bellicum Pharmaceuticals, Boehringer Ingelheim, Brooklyn ImmunoTherapeutics, Calithera Biosciences, Dracen Pharmaceuticals, Editas Medicine, Eli Lilly and Company, EMD Serono Inc, G1 Therapeutics, Genentech, Gilead Sciences, GlaxoSmithKline, Gritstone Bio, Illumina, Merck, Neogenomics Laboratories, Novartis, Takeda Pharmaceutical Company, and Synthekine; and royalties related to a patent filed by Memorial Sloan Kettering Cancer Center: determinants of cancer response to immunotherapy, (PCT/US2015/062208) licensed to Personal Genome Diagnostics. EA reports consulting fees from Celgene Research, GlaxoSmithKline, MedImmune, and Merck Sharp & Dohme; and support for attending meetings and/or travel from AbbVie, MedImmune, Pfizer, Roche, and Sanofi. ABE-K reports personal fees from Agenus, ABL Bio, Bayer, BMS, Exelixis, Eisai, and AstraZeneca; grants and personal fees from Astex, Pieris, Cytomx, Gilead, EMD Serono, Roche/Genentech, and Merck; and grants from Fulgent outside the submitted work. PAO reports grants or contracts from Amgen, Armo BioSciences, Array, AstraZeneca/MedImmune, Bristol Myers Squibb, Celldex, CytomX, Merck, Neon Therapeutics, Novartis, Oncorus, Pfizer, Roche Genentech, and Xencor; consulting fees from Array, Merck, Bristol Myers Squibb, Evaxion, and Novartis; and participation on a data safety monitoring board or advisory board for Array, Merck, Bristol Myers Squibb and Novartis. FALME, WR, and JSW have nothing to disclose. JC and AF were employees of Pfizer at the time of the study and hold stock or stock options in Pfizer. CG and WY are employees of Pfizer and hold stock or stock options in Pfizer.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by France (Comite De Protection Des Personnes Ile De France III, study sites: #1010 and #1011), Japan (National Cancer Center IRB, study site: #1012), Netherlands (Medisch-Ethische Toetsingscommissie AVL, study sites: #1005 and #1006) and USA (University of Southern California (USC) Institutional Review Board, study site: #1001; Western Institutional Review Board, study sites: #1002 and #1003; U.T. MD Anderson Cancer Center, study site: #1004; UCLA Office of the Human Research Protection Program (OHRPP), study site: #1007; UConn Health Institutional Review Board (IRB), study site: #1008; Advarra IRB, study site: #1013; Dana-Farber Cancer Institute Institutional Review Board, study site: #1014; and Columbia University Medical Center Institutional Review Board, study site: #1015). Participants gave informed consent to participate in the study before taking part.
References
- 1.Sanmamed MF, Pastor F, Rodriguez A, et al. Agonists of co-stimulation in cancer immunotherapy directed against CD137, OX40, GITR, CD27, CD28, and ICOS. Semin Oncol 2015;42:640–55. 10.1053/j.seminoncol.2015.05.014 [DOI] [PubMed] [Google Scholar]
- 2.Bansal-Pakala P, Halteman BS, Cheng MH-Y, et al. Costimulation of CD8 T cell responses by OX40. J Immunol 2004;172:4821–5. 10.4049/jimmunol.172.8.4821 [DOI] [PubMed] [Google Scholar]
- 3.Chester C, Sanmamed MF, Wang J, et al. Immunotherapy targeting 4-1BB: mechanistic rationale, clinical results, and future strategies. Blood 2018;131:49–57. 10.1182/blood-2017-06-741041 [DOI] [PubMed] [Google Scholar]
- 4.Duhen RA, Ballesteros-Merino C, Bell RB. Neoadjuvant OX40 therapy in patients with head and neck cancer induces profound changes in tumor-infiltrating lymphocytes. J Immunol 2018;200 (1 Supplement):57.40. [Google Scholar]
- 5.Fisher TS, Kamperschroer C, Oliphant T, et al. Targeting of 4-1BB by monoclonal antibody PF-05082566 enhances T-cell function and promotes anti-tumor activity. Cancer Immunol Immunother 2012;61:1721–33. 10.1007/s00262-012-1237-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gough MJ, Crittenden MR, Sarff M, et al. Adjuvant therapy with agonistic antibodies to CD134 (OX40) increases local control after surgical or radiation therapy of cancer in mice. J Immunother 2010;33:798–809. 10.1097/CJI.0b013e3181ee7095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Long H, White AL, Jiang BB, et al. Targeting OX40 by monoclonal antibody PF-04518600 to enhance T cell functions and inhibit tumor growth. J Clin Oncol 2016;34:e14518. 10.1200/JCO.2016.34.15_suppl.e14518 [DOI] [Google Scholar]
- 8.Moran AE, Kovacsovics-Bankowski M, Weinberg AD. The TNFRs OX40, 4-1BB, and CD40 as targets for cancer immunotherapy. Curr Opin Immunol 2013;25:230–7. 10.1016/j.coi.2013.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sanchez-Paulete AR, Labiano S, Rodriguez-Ruiz ME, et al. Deciphering CD137 (4-1BB) signaling in T-cell costimulation for translation into successful cancer immunotherapy. Eur J Immunol 2016;46:513–22. 10.1002/eji.201445388 [DOI] [PubMed] [Google Scholar]
- 10.Segal NH, He AR, Doi T, et al. Phase I study of single-agent utomilumab (PF-05082566), a 4-1BB/CD137 agonist, in patients with advanced cancer. Clin Cancer Res 2018;24:1816–23. 10.1158/1078-0432.CCR-17-1922 [DOI] [PubMed] [Google Scholar]
- 11.Segal NH, Logan TF, Hodi FS, et al. Results from an integrated safety analysis of urelumab, an agonist anti-CD137 monoclonal antibody. Clin Cancer Res 2017;23:1929–36. 10.1158/1078-0432.CCR-16-1272 [DOI] [PubMed] [Google Scholar]
- 12.Wang R, Gao C, Raymond M, et al. An integrative approach to inform optimal administration of OX40 agonist antibodies in patients with advanced solid tumors. Clin Cancer Res 2019;25:6709–20. 10.1158/1078-0432.CCR-19-0526 [DOI] [PubMed] [Google Scholar]
- 13.Weinberg AD, Rivera MM, Prell R, et al. Engagement of the OX-40 receptor in vivo enhances antitumor immunity. J Immunol 2000;164:2160–9. 10.4049/jimmunol.164.4.2160 [DOI] [PubMed] [Google Scholar]
- 14.Diab A, Hamid O, Thompson JA, et al. A phase I, open-label, dose-escalation study of the OX40 agonist ivuxolimab in patients with locally advanced or metastatic cancers. Clin Cancer Res 2022;28:71–83. 10.1158/1078-0432.CCR-21-0845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gaspar M, Pravin J, Rodrigues L, et al. CD137/OX40 bispecific antibody induces potent antitumor activity that is dependent on target coengagement. Cancer Immunol Res 2020;8:781–93. 10.1158/2326-6066.CIR-19-0798 [DOI] [PubMed] [Google Scholar]
- 16.Konstorum A, Vella AT, Adler AJ, et al. A mathematical model of combined CD8 T cell costimulation by 4-1BB (CD137) and OX40 (CD134) receptors. Sci Rep 2019;9:10862. 10.1038/s41598-019-47333-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee S-J, Myers L, Muralimohan G, et al. 4-1BB and OX40 dual costimulation synergistically stimulate primary specific CD8 T cells for robust effector function. J Immunol 2004;173:3002–12. 10.4049/jimmunol.173.5.3002 [DOI] [PubMed] [Google Scholar]
- 18.Morales Del Valle C, Maxwell JR, Xu MM, et al. Costimulation induces CD4 T cell antitumor immunity via an innate-like mechanism. Cell Rep 2019;27:1434–45e3. 10.1016/j.celrep.2019.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morales-Kastresana A, Sanmamed MF, Rodriguez I, et al. Combined immunostimulatory monoclonal antibodies extend survival in an aggressive transgenic hepatocellular carcinoma mouse model. Clin Cancer Res 2013;19:6151–62. 10.1158/1078-0432.CCR-13-1189 [DOI] [PubMed] [Google Scholar]
- 20.Qui HZ, Hagymasi AT, Bandyopadhyay S, et al. CD134 plus CD137 dual costimulation induces eomesodermin in CD4 T cells to program cytotoxic Th1 differentiation. J Immunol 2011;187:3555–64. 10.4049/jimmunol.1101244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ryan JM, Mittal P, Menoret A, et al. A novel biologic platform elicits profound T cell costimulatory activity and antitumor immunity in mice. Cancer Immunol Immunother 2018;67:605–13. 10.1007/s00262-018-2116-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee S-J, Rossi RJ, Lee S-K, et al. CD134 costimulation couples the CD137 pathway to induce production of Supereffector CD8 T cells that become IL-7 dependent. J Immunol 2007;179:2203–14. 10.4049/jimmunol.179.4.2203 [DOI] [PubMed] [Google Scholar]
- 23.Mittal P, St Rose M-C, Wang X, et al. Tumor-unrelated CD4 T cell help augments CD134 plus CD137 dual costimulation tumor therapy. J Immunol 2015;195:5816–26. 10.4049/jimmunol.1502032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Braeckel-Budimir N, Dolina JS, Wei J, et al. Combinatorial immunotherapy induces tumor-infiltrating CD8+ T cells with distinct functional, migratory, and stem-like properties. J Immunother Cancer 2021;9:e003614. 10.1136/jitc-2021-003614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tolcher AW, Sznol M, Hu-Lieskovan S, et al. Phase Ib study of utomilumab (PF-05082566), a 4-1BB/CD137 agonist, in combination with pembrolizumab (MK-3475) in patients with advanced solid tumors. Clin Cancer Res 2017;23:5349–57. 10.1158/1078-0432.CCR-17-1243 [DOI] [PubMed] [Google Scholar]
- 26.Gopal AK, Levy R, Houot R, et al. first-in-human study of utomilumab, a 4-1BB/CD137 agonist, in combination with rituximab in patients with follicular and other CD20+ non-hodgkin lymphomas. Clin Cancer Res 2020;26:2524–34. 10.1158/1078-0432.CCR-19-2973 [DOI] [PubMed] [Google Scholar]
- 27.Chiou VL, Burotto M. Pseudoprogression and immune-related response in solid tumors. J Clin Oncol 2015;33:3541–3. 10.1200/JCO.2015.61.6870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 29.Lerner BA, Stewart LA, Horowitz DP, et al. Mucosal melanoma: new insights and therapeutic options for a unique and aggressive disease. Oncology 2017;31:e23–32. [PubMed] [Google Scholar]
- 30.Gong J, Chehrazi-Raffle A, Reddi S, et al. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: a comprehensive review of registration trials and future considerations. J Immunother Cancer 2018;6:8. 10.1186/s40425-018-0316-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carreau N, Pavlick A. Revolutionizing treatment of advanced melanoma with immunotherapy. Surg Oncol 2022;42:101180. 10.1016/j.suronc.2019.01.002 [DOI] [PubMed] [Google Scholar]
- 32.Nadal E, Massuti B, Dómine M, et al. Immunotherapy with checkpoint inhibitors in non-small cell lung cancer: insights from long-term survivors. Cancer Immunol Immunother 2019;68:341–52. 10.1007/s00262-019-02310-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nowicki TS, Hu-Lieskovan S, Ribas A. Mechanisms of resistance to PD-1 and PD-L1 blockade. Cancer J 2018;24:47–53. 10.1097/PPO.0000000000000303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shergold AL, Millar R, Nibbs RJB. Understanding and overcoming the resistance of cancer to PD-1/PD-L1 blockade. Pharmacol Res 2019;145:104258. 10.1016/j.phrs.2019.104258 [DOI] [PubMed] [Google Scholar]
- 35.Kuriakose A, Chirmule N, Nair P. Immunogenicity of biotherapeutics: causes and association with posttranslational modifications. J Immunol Res 2016;2016:1298473. 10.1155/2016/1298473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen EEW, Pishvaian MJ, Shepard DR, et al. A phase Ib study of utomilumab (PF-05082566) in combination with mogamulizumab in patients with advanced solid tumors. J Immunother Cancer 2019;7:342. 10.1186/s40425-019-0815-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Polesso F, Weinberg AD, Moran AE. Late-stage tumor regression after PD-L1 blockade plus a concurrent OX40 agonist. Cancer Immunol Res 2019;7:269–81. 10.1158/2326-6066.CIR-18-0222 [DOI] [PubMed] [Google Scholar]
- 38.Fromm G, de Silva S, Johannes K, et al. Agonist redirected checkpoint, PD1-Fc-OX40L, for cancer immunotherapy. J Immunother Cancer 2018;6:149. 10.1186/s40425-018-0454-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kvarnhammar AM, Veitonmäki N, Hägerbrand K, et al. The CTLA-4 x OX40 bispecific antibody ATOR-1015 induces anti-tumor effects through tumor-directed immune activation. J Immunother Cancer 2019;7:103. 10.1186/s40425-019-0570-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jensen SM, Maston LD, Gough MJ, et al. Signaling through OX40 enhances antitumor immunity. Semin Oncol 2010;37:524–32. 10.1053/j.seminoncol.2010.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sagiv Barfi I, Czerwinski DK, Shree T, et al. In situ vaccination with Cpg and anti-OX40 antibody: preclinical optimization for clinical translation. Blood 2018;132:2943. 10.1182/blood-2018-99-117872 [DOI] [Google Scholar]
- 42.Ito F, Li Q, Shreiner AB, et al. Anti-CD137 monoclonal antibody administration augments the antitumor efficacy of dendritic cell-based vaccines. Cancer Res 2004;64:8411–9. 10.1158/0008-5472.CAN-04-0590 [DOI] [PubMed] [Google Scholar]
- 43.Milhem M, Gonzales R, Medina T, et al. Abstract CT144: intratumoral Toll-like receptor 9 (TLR9) agonist, CMP-001, in combination with pembrolizumab can reverse resistance to PD-1 inhibition in a phase Ib trial in subjects with advanced melanoma. Cancer Res 2018;78:CT144. 10.1158/1538-7445.AM2018-CT144 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2022-005471supp001.pdf (4.5MB, pdf)
Data Availability Statement
Data are available upon reasonable request. Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.