Abstract
Background
Online consultations (OCs) allow patients to contact their care providers on the web. Worldwide, OCs have been rolled out in primary care rapidly owing to policy initiatives and COVID-19. There is a lack of evidence regarding how OC design and implementation influence care quality.
Objective
We aimed to synthesize research on the impacts of OCs on primary care quality, and how these are influenced by system design and implementation.
Methods
We searched databases from January 2010 to February 2022. We included quantitative and qualitative studies of real-world OC use in primary care. Quantitative data were transformed into qualitative themes. We used thematic synthesis informed by the Institute of Medicine domains of health care quality, and framework analysis informed by the nonadoption, abandonment, scale-up, spread, and sustainability framework. Strength of evidence was judged using the GRADE-CERQual approach.
Results
We synthesized 63 studies from 9 countries covering 31 OC systems, 14 (22%) of which used artificial intelligence; 41% (26/63) of studies were published from 2020 onward, and 17% (11/63) were published after the COVID-19 pandemic. There was no quantitative evidence for negative impacts of OCs on patient safety, and qualitative studies suggested varied perceptions of their safety. Some participants believed OCs improved safety, particularly when patients could describe their queries using free text. Staff workload decreased when sufficient resources were allocated to implement OCs and patients used them for simple problems or could describe their queries using free text. Staff workload increased when OCs were not integrated with other software or organizational workflows and patients used them for complex queries. OC systems that required patients to describe their queries using multiple-choice questionnaires increased workload for patients and staff. Health costs decreased when patients used OCs for simple queries and increased when patients used them for complex queries. Patients using OCs were more likely to be female, younger, and native speakers, with higher socioeconomic status. OCs increased primary care access for patients with mental health conditions, verbal communication difficulties, and barriers to attending in-person appointments. Access also increased by providing a timely response to patients’ queries. Patient satisfaction increased when using OCs owing to better primary care access, although it decreased when using multiple-choice questionnaire formats.
Conclusions
This is the first theoretically informed synthesis of research on OCs in primary care and includes studies conducted during the COVID-19 pandemic. It contributes new knowledge that, in addition to having positive impacts on care quality such as increased access, OCs also have negative impacts such as increased workload. Negative impacts can be mitigated through appropriate OC system design (eg, free text format), incorporation of advanced technologies (eg, artificial intelligence), and integration into technical infrastructure (eg, software) and organizational workflows (eg, timely responses).
Trial Registration
PROSPERO CRD42020191802; https://tinyurl.com/2p84ezjy
Keywords: general practice, systematic review, remote consultation, OC, triage, primary health care, care provider, health care professional, workforce, telemedicine, COVID-19, pandemic, primary care, health outcome, patient care
Introduction
Background
Online consultation (OC) systems allow patients to contact their health care provider over the internet to ask health-related questions and report symptoms [1]. Their query may then be resolved with a written response, telephone call, video consultation, or in-person visit. Many terms are used to describe this type of technology, including e-consultation, e-visit, and online triage (Multimedia Appendix 1 [2-28])—in this review, we refer to them all as online consultations. We distinguish OCs from “symptom checkers” [29] and other self-service systems that typically do not directly facilitate communication with a human health care provider and from patient portals [30], which may include generic email or secure messaging functionalities.
OCs are considered by policy makers in many countries as a way to address the increasing workload and decreasing workforce capacity in primary care [31-36] while still meeting patient expectations and improving access [37]. However, they have the potential to exacerbate health inequities [38,39] and increase inappropriate antibiotic prescriptions [40]. Furthermore, there are widely recognized challenges in initiating and sustaining the adoption of new technologies in primary care [41].
Although symptom checkers [29,42] and patient portals [30,43,44] have been well studied, only a small number of evidence syntheses directly relevant to OCs have been published: a systematic review of 57 articles on delivering “e-consultation” in primary care largely focused on generic stand-alone applications such as email and video (n=39/57, 68%) [45]; a scoping review of “online triage tools” included 13 papers, 4 of which (31%) were nonempirical (eg, opinion pieces) [46]; and a review of 17 studies of “intelligent online triage tools” focused only on those that used “artificial intelligence” (AI) [47].
Since these syntheses were conducted, OCs have gained wider traction in clinical practice worldwide—they have been indispensable in helping manage patients remotely to minimize the spread of COVID-19 [48,49], and English primary care providers have been mandated to offer OCs for all patients since April 2020 [50]. Moreover, OC system product design has progressed significantly to become more specialized and technologically advanced [51], with several more empirical research studies published on their use [2-11,52-64].
Given this rapid scale-up and increase in the diversity and complexity of OCs, further insight is needed into their impact on health care quality. Previous reviews have not reported the design or implementation details of the OCs they studied [45-47] despite their importance in understanding the causal mechanisms of how they affect care outcomes [65]. The aim of this study was to systematically review and synthesize the empirical quantitative and qualitative literature in a theoretically informed way to address this knowledge gap.
Objectives
Informed by existing theories, the aim of this study was to synthesize quantitative and qualitative research on (1) the impacts of OCs on primary care quality and (2) how these are influenced by OC system design and implementation.
Methods
Study Design
We consider OCs as complex interventions and, therefore, synthesized both quantitative and qualitative evidence to understand their impacts in specific contexts [66]. We did not perform a meta-analysis because of the heterogeneous and nonrandomized nature of the included studies [67]. We followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement [68].
Registration and Protocol
The study protocol was registered with PROSPERO (CRD42020191802) [69]. The original title was amended to be less general and more specific to the objectives of the review, and the objectives were amended to focus on care quality.
Inclusion Criteria
Papers that met the following criteria were included: empirical studies using quantitative or qualitative methods to examine the real-world use of OCs in primary care in any country, written in English, and published in 2010 or later. We excluded news articles, opinion pieces, literature reviews, non–English-language articles, and literature published before 2010.
We defined OCs as digital interventions that allow patients to contact their primary care provider by inputting “queries” into health care–specific web-based forms [1]. We included symptom checkers and similar self-service systems [54] if at least one of their outcomes directly facilitated contact with a primary care health professional. We included patient portals if they had a secure messaging functionality that used health care–specific forms [54]. We excluded stand-alone generic communication technologies such as email or videoconferencing software.
Search Strategy
We searched the Ovid MEDLINE, EMBASE, Web of Science, and Scopus databases during July 2020 (Multimedia Appendix 2 [12,53,56,58-60,63,70-73]). Our search strategy was developed from scoping searches of the literature and drew on search strategies used in related literature reviews [45,46]. We searched the National Technical Information Service, the Health Management Information Consortium, and Zetoc to find relevant gray literature, conference proceedings, and theses. We found further literature through citation mapping and in the reference lists of the included papers, searching during August 2020 and September 2020. SD and TC independently screened titles and abstracts and then full papers for eligibility, resolving differences through discussion at each stage. All literature searches were rerun by SD between November 2021 and February 2022.
Data Extraction and Quality Appraisal
We extracted data from the included papers as verbatim text, capturing study characteristics (eg, research design and study setting) and key findings relevant to our research objectives based on the nonadoption, abandonment, scale-up, spread, and sustainability (NASSS) framework [74] (Multimedia Appendix 3). We used the NASSS to capture “a rich, contextualised narrative of technology-supported change efforts and the numerous interacting influences that help explain its successes, failures, and unexpected events” [75]. The methodological quality of the studies was assessed using the Mixed Methods Appraisal Tool (MMAT), which is designed for qualitative, quantitative, and mixed methods studies [76]. We scored each paper using recommended quintile percentages as cutoffs and considered any paper scoring at least 60% as of “good” quality [77]. SD and TC extracted data from 10 papers independently, which confirmed high interrater agreement. Following this, SD extracted data from the remaining papers, which were checked by TC.
Data Synthesis
The data were imported into NVivo (version 12; QSR International) [78] for synthesis. To integrate both quantitative and qualitative data, during data synthesis, quantitative data were transformed into qualitative themes (“qualitising”) [79].
For objective 1, we considered “impacts of OCs on primary care quality” as consequences of using OCs that could relate to patients, primary care staff, or the wider system [65]. We used thematic synthesis [80], which involved SD and TC coding the text from the data extraction forms independently line by line, developing higher-level themes through regular discussion [80]. Impacts on care quality were synthesized inductively, with emerging themes mapped to the six Institute of Medicine domains of health care quality [81]: safe (avoiding harm to patients from care that is intended to help), effective (providing care based on scientific knowledge to produce better clinical outcomes), patient-centered (care that is respectful and responsive), timely (reducing waits and delays for those who receive and give care), efficient (avoiding waste), and equitable (care that does not vary in quality because of personal characteristics) [81]. Our emergent findings suggested that OCs had both positive and negative impacts and, therefore, theme descriptions were edited to be neutral (eg, safe→safety and efficient→efficiency).
For objective 2, we considered OC “design” as material properties of an OC, such as features and functionality [74], and “implementation” as the way an OC was introduced and used in a particular context [65]. As a design feature, we considered AI as the ability of machines to “mimic human intelligence as characterized by behaviors such as cognitive ability, memory, learning, and decision making” [82]. We synthesized the extracted data using framework analysis [83], which involved SD and TC reading and rereading each data extraction form and then coding them line by line independently—both deductively by using domains from the NASSS framework [74] for high-level themes and inductively by identifying additional subthemes. Through discussion, SD and TC summarized the findings into five high-level themes: condition complexity (health condition and the illness the OC is used for), technology (material properties of the OC and required knowledge for use), adopters (staff, patients, and carers expected to use the OC), organization (extent of work needed for implementation of the OC, capacity, and readiness), and wider system (policy context) [74]. Two NASSS domains—value proposition (value of the OC to the developer, patients, and health care system) and embedding and adaptation over time (learning and adaptation to changing contexts)—had limited applicability to our findings and were not included in the final synthesis. Informed by realistic evaluation [65], we considered our themes as contextual factors and identified patterns of explanations for how each led to the impacts on care quality from objective 1 (ie, “causal mechanisms”). Where appropriate, we considered the levels of OC adoption as a mechanism for how they affected care quality [65]. We used visual mapping to identify commonalities and discordances in causal mechanisms—first within individual papers and then across papers [83]. Where there were discordances, we explored potential explanations where possible (eg, related to the study setting).
The strength and quality of our findings for objectives 1 and 2 were assessed using the Grading of Recommendations Assessment, Development, and Evaluation-Confidence in Evidence from Reviews of Qualitative Research method [84]. This accounts for the methodological limitations of the contributing papers (according to MMAT assessments), relevance to the review question, coherence of the finding, and adequacy of its supporting data [84]. Confidence in each finding was designated as high, moderate, low, or very low. At each stage of the analysis, the findings were discussed and agreed upon with the wider study team. BCB reviewed all coded verbatim excerpts from the papers included in the final synthesis.
Results
Descriptive Summary
We synthesized 63 papers (Figure 1), including 52 (83%) journal papers [53], 7 (11%) evaluation reports [85], 3 (5%) conference papers [12], and 1 (2%) master’s degree thesis [13]. The studies were quantitative (33/63, 52%), qualitative (12/63, 19%), and mixed methods (18/63, 29%) and analyzed data from patients (16/63, 25% qualitative studies and 18/63, 29% quantitative studies), staff (22/63, 35% qualitative studies and 9/63, 14% quantitative studies), and clinical systems (33/63, 52% quantitative studies). All were set in one of 9 high-income countries, with most coming from the United States (21/63, 33%) and the United Kingdom (20/63, 32%; Multimedia Appendix 4 [2-27,52-64,70-73,77,85-104]). In all, 41% (26/63) of the studies were published in 2020 or later, and 17% (11/63) were conducted after the start of the COVID-19 pandemic. Examples of excluded studies are those that focused on stand-alone video consultations [105], involved communication between physicians and not patients [106], and were not based on primary care [107].
Figure 1.
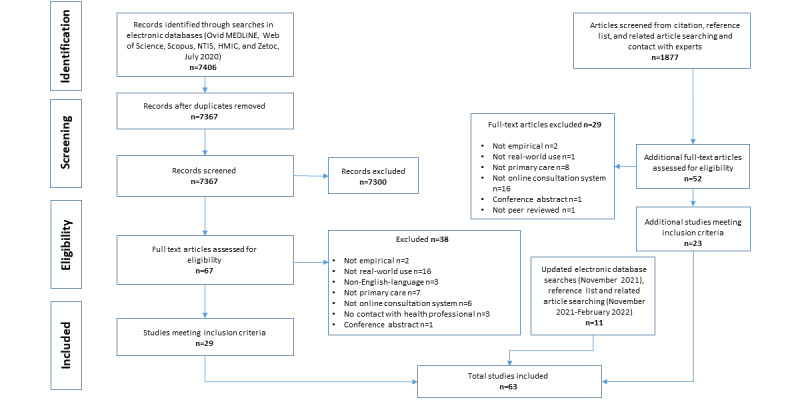
Flowchart of the study selection process. HMIC: Health Management Information Consortium; NTIS: National Technical Information Service.
In all, 83% (52/63) of the studies reported levels of OC adoption by patients and staff, of which 62% (32/52; 32/63, 51% of all studies) were described as “low” by the study authors [86]. OCs were adopted at a high rate in 63% (33/52; 33/63, 52% of all) of the studies [87], including high rates of adoption by certain patient groups even when overall OC adoption in the study was low [14].
The included papers described 31 OC systems summarized in Table 1 and detailed in Multimedia Appendix 5 [2-27,52-64,70-73,85-104]. In 25% (16/63) of the papers, the OC system was described sufficiently to meet our inclusion criteria but not in enough detail to determine specific design features. Of the 31 OCs described, most (23/31, 74%) offered two-way written communication between patients and staff [88], with a few (4/31, 13%) also offering communication by video [52]. In all, 13% (4/31) did not provide functionalities for staff to reply to patients via the system (ie, one-way communication only [14]). In total, 35% (11/31) required patients to describe their queries solely via multiple-choice questionnaires (MCQs) [89] compared with 13% (4/31) that solely required patients to describe their queries using unstructured free text [56]. In all, 42% (13/31) had a hybrid approach of primarily using MCQs with the option for patients to enter additional free text [90]. No free text OCs offered optional MCQs. In all, 26% (8/31) of the OC systems were integrated with the electronic health record (EHR) [58], and 3% (1/31) allowed patients to schedule telephone or in-person appointments with health care professionals themselves [54].
Table 1.
Online consultation (OC) system features (N=31).
| OC system feature and subcategory | Studies, n (%)a | ||
| Communication mode | |||
|
|
Two-way written communication between staff and patients | 23 (74) | |
|
|
One-way written communication (staff cannot reply to patients) | 4 (13) | |
|
|
Videoconferencing | 4 (13) | |
|
|
Unclear | 4 (13) | |
| Patient query format | |||
|
|
Multiple-choice questionnaires only | 11 (35) | |
|
|
Unstructured free text only | 4 (13) | |
|
|
Multiple-choice questionnaires with optional free text | 13 (42) | |
|
|
Unclear | 3 (10) | |
| Integration with other software | |||
|
|
Electronic health record | 8 (26) | |
|
|
Appointment scheduling | 1 (3) | |
|
|
No integration | 23 (74) | |
| Artificial intelligence function | |||
|
|
Adapting questions during query submission | 10 (32) | |
|
|
Prioritizing patient queries based on clinical urgency | 4 (13) | |
|
|
Signposting patients to the most appropriate care provider | 3 (10) | |
|
|
No artificial intelligence | 17 (55) | |
| Artificial intelligence method | |||
|
|
Preprogrammed logic and algorithms | 10 (32) | |
|
|
Unclear | 3 (10) | |
aCount of OC systems described in detail (n=31). Categories may add up to >31 as OC systems may have more than one feature in a category.
In total, 54% (13/24) of MCQ-based OC systems exhibited three types of AI: (1) adapting questions they asked patients as they submitted their query in response to previous answers given (10/31, 32%) [91]; (2) prioritizing patient queries based on clinical urgency (4/31, 13%) [54]; and (3) signposting patients to an appropriate care provider based on their query, such as self-care, primary care, or emergency department (3/31, 10%) [8]. These were mostly powered by preprogrammed logic and “algorithms” (10/31, 32%) [54], with the exact AI methodology unclear in the remainder (3/31, 10%) [15].
The methodological quality of most studies (42/63, 67%) was “good” (ie, ≥60% according to the MMAT [77]; Multimedia Appendix 6 [2-27,52-64,70-73,76,85-104]). Common limitations included a lack of detail on whether the OC was administered as intended [92] and small sample sizes [3].
Synthesis
Overview
To maintain readability, we present only moderate- and high-confidence findings and provide only 1 example reference per finding. Tables 2 and 3 provide all the references and specify whether the findings are qualitative or quantitative. Multimedia Appendix 7 [13,59,99] and Multimedia Appendix 8 [3, 5, 8-11, 13-17, 19-21, 25, 27, 54, 57, 59, 60, 63, 64, 71, 85, 90, 91, 95, 97, 100, 101] detail the low-confidence findings. Multimedia Appendix 9 [2-27,52,54-61,63,64,67,70-73,85-101] and Multimedia Appendix 10 [3-27, 52, 54-64, 70-73, 85-95, 97, 98, 100, 101] provide exemplar data.
Table 2.
Impacts of online consultations (OCs) on primary care quality.
| Theme | Subtheme |
| Safety (harm to patients) |
|
| Effective (providing care based on scientific knowledge to produce better clinical outcomes) | |
| Timeliness (reducing waits and delays) | |
| Efficiency (avoiding waste) |
|
| Equitable (variation because of personal characteristics) |
|
| Patient-centeredness (care that is respectful and responsive) |
|
aCERQual: Confidence in the Evidence from Reviews of Qualitative Research.
Table 3.
How the impacts of online consultations (OCs) on primary care quality are influenced by system design and implementation.
| Theme and OC design feature or implementation | Impact on care quality (from Table 2)a | CERQualb rating and references | |
| Condition complexity (illness the OC is used for) | |||
|
|
|
|
|
|
|
|
|
|
| Technology (material properties of the OC) | |||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Adopters (expected users of OCs) | |||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Organization (work needed to implement OCs) | |||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Wider system (policy context) | |||
|
|
|
|
|
|
|
|
|
|
aIncludes levels of OC adoption as a mechanism for how they affect care quality [65].
bCERQual: Confidence in the Evidence from Reviews of Qualitative Research.
cMCQ: multiple-choice questionnaire.
Objective 1: Impacts of OCs on Primary Care Quality
Safety
In 27% (17/63) of the studies, staff and patients expressed general concerns about the impact of OCs on patient safety, particularly regarding the potential loss of information from patients versus in-person or telephone consultations and how it could lead to misdiagnosis [55]. However, quantitative evidence from 17% (11/63) of the studies did not support these concerns in terms of emergency department attendance rates [92], hospitalizations [70], deaths [88], and other measures [59]. Furthermore, clinicians and patients in 22% (14/63) of the studies believed that OCs improved patient safety, for example, by producing a detailed shared written record of consultations [93] and helping reduce the spread of communicable diseases such as COVID-19 [63].
Effectiveness
In 6% (4/63) of the studies, antibiotics were prescribed to patients at a lower rate via OCs compared with in-person consultations [60].
Timeliness
In 46% (29/63) of the studies, OCs were perceived as increasing access to primary care services. It was easier and more convenient to make initial contact as patients could submit an OC query at any time without waiting on the phone or attending in person [14]. Once a query was submitted, patients also communicated with health professionals sooner as OCs tended to circumvent the traditional appointment-booking process [57].
Efficiency
In total, 52% (33/63) of the studies suggested that the workload decreased for both staff and patients when using OCs. Patient queries were written rather than spoken, incoming phone calls to receptionists were reduced [16], and patient histories did not need manual documentation [93]. Written queries were usually more detailed than when communicated verbally and were received by health care staff asynchronously, thus providing opportunities for more objective examination and more effective triage. Consequently, patient queries could more often be directed to other services or dealt with by other staff members rather than always by physicians [3]. Combined with their remote nature, OCs also gave staff more autonomy over how their work was organized, thus providing efficiency gains such as working from home and control over how to contact a patient rather than defaulting to an in-person consultation [13]. When telephone or in-person consultations were necessary, they were more focused and, therefore, quicker as the staff member could read the patient query before contact [17]. OCs reduced the workload for patients by avoiding the need to telephone their primary care provider to make an appointment, which often entailed long queues [18], and avoiding in-person consultations when possible, which typically involved travel, waiting rooms, and organizing time off work and childcare [15].
In contrast, 46% (29/63) of the studies suggested that OCs increased the workload for staff and patients. Staff described conducting OCs on top of their usual tasks [13] and dealing with them outside normal working hours [19]. They believed that, because OCs increased access to primary care, patients sought help more readily than they would have previously [17], thus creating “supply-induced demand” [108]. Processing OCs also created new administrative work such as filing them to EHRs and deciding whether they required input from a clinician [86]. Workload could also increase for patients if they perceived that entering their query into the OC system was more difficult than explaining it verbally [20].
OCs decreased costs for providers in 32% (20/63) of the studies largely by reducing in-person visits, which have associated expenditures related to staffing and utilities [21]. Patients reported that, owing to their convenience, having access to OCs stopped them from visiting other costly unscheduled care providers [92]. OCs decreased costs for patients in 6% (4/63) of the studies by avoiding in-person visits, which may entail expenses related to travel, unpaid work leave, and childcare [57].
In contrast, OCs increased costs for providers in 14% (9/63) of the studies owing to associated technology costs [63], time required for clinicians to triage patient queries [22], and insufficient reduction of in-person visits or telephone consultations [87].
Equitable
In all, 65% (41/63) of the studies suggested that OCs decreased equitable access to care services, as their use varied according to patient characteristics [63]. Conversely, 30% (19/63) of the studies suggested that OCs increased equitable access as they helped particular groups of patients who had previously struggled communicate with their primary care providers [14]. These characteristics are discussed in more detail in the Adopters section.
Patient-Centeredness
Although 21% (13/63) of the studies uncovered some patient dissatisfaction with OCs [90], 49% (31/63) found that most patients were at least as satisfied or more satisfied with OCs than with traditional in-person appointments [2]. Patients liked OCs for the aforementioned reasons: they improved access (timeliness), reduced their workload and costs (efficiency), and helped particular groups of patients communicate with their care providers (equitable).
Objective 2: How the Impacts of OCs on Primary Care Quality Are Influenced by System Design and Implementation
Condition Complexity
In all, 17% (11/63) of the studies suggested that OCs decreased staff workload when used for simple queries that were straightforward to resolve as they were more amenable to completion without needing to contact the patient directly via telephone or in person [5]. Simple queries included those related to administrative tasks, new and recurrent minor acute illnesses, prescriptions, tests, requests for advice, follow-up, and some chronic condition reviews [56]. These queries also decreased health costs as they saved clinicians time, for example, when administrative staff were able to relay messages and there was no direct contact between physician and patient [23]. In all, 11% (7/63) of the studies suggested that OCs increased staff workload and costs when used for complex queries such as those with multiple ill-defined symptoms [17]. These queries generally required verbal dialogue with and physical examination of the patient and were usually converted to telephone or in-person consultations to assess the patient further [23]. Staff felt that this duplicated the number of contacts with the patient for the same query.
Technology
In all, 21% (13/63) of the studies showed that, when patients had to use MCQs to input their OC query, it increased both patient and staff workload. Filling out long lists of questions shifted work from the clinician to the patient [20], and staff found them burdensome to read [86]. MCQs limited the amount of detail patients could enter, so staff could not always fully understand their request. This increased workload as they often had to contact the patient to obtain further information [23]. MCQs also asked questions about seemingly “irrelevant” symptoms, which staff were responsible for assessing and following up, diverting attention from the patient’s primary concern [10]. Owing to the restrictive nature of MCQs, patients regularly adapted their responses to obtain the outcome they wanted even when it was not the most appropriate use of resources. For example, reporting their symptoms differently to obtain an in-person consultation when self-care may have been more suitable (“gaming”) [17].
In all, 14% (9/63) of the studies suggested that MCQs could also decrease patient satisfaction. Reasons included the amount of work required to complete them [14], their inflexibility in obtaining the answers patients wanted from their primary care provider [9], and that they could be confusing to navigate [25].
In contrast, 11% (7/63) of the studies suggested that, when patients could primarily report their queries using unstructured free text, it decreased staff workload and increased patient safety. This was because patients were more able to fully describe their query in sufficient detail using their own words, and clinicians did not have to request further information as often [95].
In 10% (6/63) of the studies, two-way written communication within the OC decreased the workload for both staff and patients. The ability to reply to patients in writing meant queries could be answered and follow-up questions could be asked at times convenient to both staff and patients, avoiding lengthy telephone and in-person consultations when appropriate [55]. It was also easier to communicate complex information, for example, by sending educational materials or using preset message templates [95].
In all, 21% (13/63) of the studies highlighted that a lack of integration between the OC system and other core software used by providers increased staff workload. Nonintegration meant that the staff had to go through multiple steps to perform a task, such as when filing an OC to a patient’s EHR [21].
Adopters
Patients using OCs were more likely to be female (27/63, 43%) [70], younger (27/63, 43%) [91], and native speakers of the official language of the country they lived in (7/63, 11%) [25] and have a higher socioeconomic status (11/63, 17%) [57] than those not using OCs, thus decreasing equity. In contrast, both staff and patients felt that OCs increased access for particular groups of patients who struggled with traditional consultation methods, thus increasing equity and satisfaction with care. This included patients with mental health conditions who became anxious when speaking to health professionals on the telephone or in person (8/63, 13%) [20]; patients with verbal communication difficulties such as hearing loss who found it easier to communicate in writing (7/63, 11%) [90]; and patients with barriers to attending in-person appointments because of physical disabilities, geography, work commitments, or care responsibilities (8/63, 13%) [23]. In all, 13% (8/63) of the studies suggested that when staff and patients viewed traditional in-person methods as the gold standard, it could lead to resistance in adopting OCs [19].
Organization
In all, 8% (5/63) of the studies found that, when OCs were minimally advertised to patients, it understandably led to low rates of adoption [24]. In all, 11% (7/63) of the studies also showed that responding to a patient’s initial OC query quickly led to high patient satisfaction, as it provided an advantage over traditional methods of primary care contact [6]; by definition, this also increased primary care access.
In all, 21% (13/63) of the studies found that the staff workload increased when providers did not integrate OCs into their normal daily workflows. For example, not scheduling time for clinicians to deal with OCs meant that they were done in addition to their normal tasks [93], and not diverting all incoming patient demand via the OC meant that different communication routes were often used for the same issue, thereby duplicating work [5]. In all, 13% (8/63) of the studies suggested that provider workload decreased if sufficient resources were allocated to implementing OCs. This included their initial setup—for example, training to enable staff to more effectively handle OCs [15]—and their ongoing processing—for example, dedicated facilities such as quiet rooms to help staff respond to OCs without distraction [55].
In all, 8% (5/63) of the studies showed that a lack of continuity of care between patients and their known physician negatively affected patient satisfaction. This occurred when any physician could reply to an OC query and patients were not able to specify a physician to whom to address their query [64].
Wider System
In all, 10% (6/63) of the studies showed that government policies mandating OC use increased their adoption. Example policies aimed to increase digital modes of contact with primary care in general [87] and minimize in-person contact during the COVID-19 pandemic [63]. In all, 8% (5/63) of the studies demonstrated that a lack of long-term external financial support for OCs limited their sustainability as health care organizations could often not afford to pay their ongoing costs [23].
Discussion
Summary of Evidence
This review focused on how OCs affect primary care quality, as defined by Institute of Medicine domains, for patients, providers, and the wider system, as well as which factors, as specified through the NASSS framework, influence this quality. We synthesized qualitative and quantitative evidence from 63 studies conducted in 9 countries covering 31 OC systems described in detail, with wide-ranging functionalities including AI. In all, 41% (26/63) of the studies were published in 2020 onward, and 17% (11/63) were published after the COVID-19 pandemic. Our main findings were that OCs are safe and have positive impacts on care quality, including increased access to care and decreased patient costs. However, they can have conflicting impacts on provider costs, staff and patient workloads, patient satisfaction, and care equity. We found that the impacts OCs have on care quality are determined by the complexity of the patient queries they are used for, the design of the OC technology itself, the characteristics of staff and patient users, the way OCs are implemented by health care providers, and wider health policies.
Comparison of Findings With Other Reviews
Consistent with previous reviews relevant to OCs, we found a limited demographic of patients using OCs, leading to potential inequitable care [45,46]. We also found that the studies often did not sufficiently explore patients’ perspectives of OCs in depth [46]; only 14% (9/63) of the studies used interview-based methods with an average sample size of 24.5 (SD 10.14). This hampered efforts to understand how such inequities arose.
Contrary to previous reviews, we found that OC impacts on care quality are more complex and nuanced than previously reported [45-47]. For example, we identified mixed findings regarding their impact on workload, patient satisfaction, and equitable care. This contrasts with previous reviews, where OCs only increased [47] or had no impact [45] on workload, decreased patient safety [45,47], and increased inequity [45-47].
These new findings for OCs may be partly explained because 76% (48/63) of the included studies had not been covered by these previous reviews. Although there was some overlap of papers (7/57, 12% of papers [45]; 7/13, 54% of papers [46]; and 4/17, 24% of papers [47]), most did not meet our inclusion criteria as they were either nonempirical (4/57, 7% [45]; 4/13, 31% [46]; and 4/17, 24% [47]), published before 2010 (26/57, 46% [45] and 2/17, 12% [47]), not based on real-world primary care (16/57, 28% [45]; 1/13, 8% [46]; and 6/17, 35% [47]), or did not meet our functional definition of an OC (39/57, 68% [45]; 2/13, 15% [46]; and 6/17, 35% [47]; eg, symptom checkers with no link to a health professional [28]).
By focusing on design and implementation, we identified new ways in which OCs affect primary care quality. For example, we found that, by increasing access, OCs can increase staff workload by creating “supply-induced demand” [17,108] and that they can decrease workload by enabling more focused consultations [17]. Furthermore, as previous reviews often did not analyze the design or implementation of OCs [45-47], we identified influential factors that have not been previously described. For example, although some reviews identified increased workload when clinicians received insufficient patient information via an OC system [46], we found that this was particularly associated with MCQ-based OCs [23]. We identified that allowing patients to describe their queries using unstructured free text had the opposite effect [95] while also having a positive impact on patient safety [55]. Using unstructured free text means that patients can more fully describe their query in addition to allowing them to freely express their ideas, concerns, and expectations, as is common in patient-centered primary care consultations [109].
Strengths and Limitations
As evidenced by the range of examples in Multimedia Appendix 1, we adopted a fundamental functional definition of OCs rather than relying on the names given to them by the authors of the included studies. When combined with our comprehensive searches across multiple databases and inclusion of gray literature, we identified more empirical studies relevant to OCs than any previous evidence synthesis on the topic [45-47]. Combined with our focus on causal mechanisms, this helped us develop a new and theoretically informed understanding of OCs that has not been previously reported.
As in all systematic reviews, our synthesis is reliant on what the study authors reported. OC features were not always described in sufficient detail to understand how they affected care quality [62]. There was also a lack of patient perspective in the studies, particularly from OC nonusers [4]. We made our literature search strategy as inclusive as possible regarding the different terms used for OCs (Multimedia Appendix 1) but, owing to their wide-ranging nature, it is possible that some papers were missed. We updated our searches between November 2021 and February 2022 to capture more recently published studies but, owing to time constraints, only 1 author (SD) screened these newer papers. This enabled us to capture studies conducted in the context of COVID-19 (11/63, 17% of all included studies).
Implications for Practice and Research
Overview
Our findings show that the impacts of OCs on care quality are complex and can be influenced by the subtle ways in which OCs are designed and implemented. To maximize their benefit for patients and staff, we therefore provide recommendations for OC developers on how systems could be designed, health care organizations on how they can be implemented and used, and researchers on questions and areas for further investigation. They are discussed in the following sections under the high-level themes from objective 2 and summarized in Table 4.
Table 4.
Implications for online consultation (OC) research and practice.
| Theme | Implications | ||
|
|
OC designers | Health care providers | Researchers |
| Condition complexity |
|
|
|
| Technology |
|
|
|
| Adopters |
|
|
|
| Organization |
|
|
|
| Wider system | N/Ad |
|
|
aMCQ: multiple-choice questionnaire.
bAI: artificial intelligence.
cTIDieR: Template for Intervention Description and Replication.
dN/A: not applicable.
Condition Complexity
It is unclear whether OCs are unsuitable for complex patient queries or whether workflows and procedures can be better organized and OC systems can be better designed to deal with them. Therefore, we recommend that (1) complex conditions are routed through traditional consultation methods (eg, in person and telephone) and (2) further research is conducted on how these types of conditions could be better handled via OCs to ensure that they benefit all patients.
Technology
On the basis of existing evidence, we recommend that OC developers (1) allow patients to fully describe their queries using unstructured free text rather than MCQs, (2) support patients in providing sufficient detail in their queries for their primary care provider to respond quickly and safely, (3) allow for two-way written communication between staff and patients, and (4) integrate their solutions with existing core clinical software systems.
Technology design also plays a role in mitigating some of the undesirable outcomes we identified from using OCs, including increasing workload and costs. Increased workload is particularly important as it can lead to a mismatch between patient demand and health care resources, which can in turn threaten patient safety if providers are unable to deal with OCs in an appropriate time frame. A way this could happen is through increased demand—if there are too many OCs submitted by patients and not enough staff to deal with them [55]. Whether this additional demand is a supply-induced [108] or previously unmet (and now unmasked) need was unclear from the studies we included [15] and requires further research. Nevertheless, OC systems could help by (1) supporting patients to self-care or signposting them to other services when appropriate; (2) matching capacity to demand by limiting the number of OC queries that primary care providers can receive from patients; (3) supporting workflow, for example, by determining whether OCs require clinical input to relieve the workload of administrators [86]; (4) assisting in triaging patient queries to reduce the associated costs of solely relying on clinicians for triage [22]; and (5) highlighting when patients may require an in-person appointment to facilitate direct booking to avoid work duplication [23], which may relate to patient query complexity.
According to our definition [82], many of these functions may require AI to be most effective, which should be explored by OC designers (Figure 2). In all, 54% (13/24) of MCQ-based OC systems in our review used AI (Table 1) [54], although largely for other functions rather than the aforementioned ones. Furthermore, AI was usually not the focus of the studies, and we consequently found only low-confidence evidence regarding its use in OCs (Multimedia Appendix 8). Therefore, how AI could be used by OC systems in clinical practice requires further research.
Figure 2.
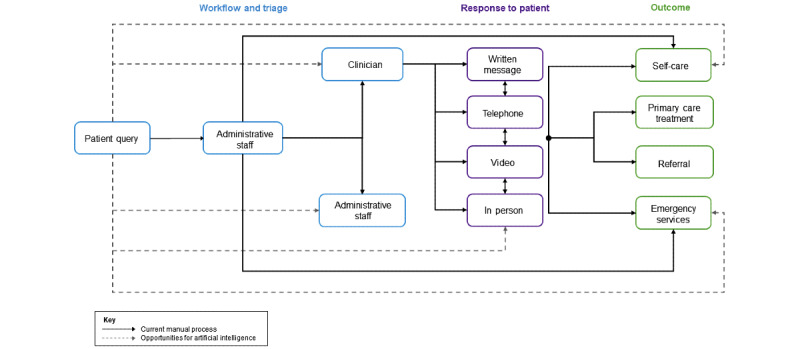
Artificial intelligence opportunities.
The included papers did not always adequately describe the OC systems studied, limiting our ability to determine how their specific features affected care quality. Future research should describe OC systems in detail so that evaluation findings can be usefully compared, for example, by using the Template for Intervention Description and Replication checklist [110].
Adopters
We found inadequate exploration of participant (especially patient) experiences to confidently explain how and why the impacts on care equity arose during OC use. Study authors and health care staff often speculated reasons [18], but this was insufficient to formulate evidence-based hypotheses. Future research should explore the perspectives of patients using (and not using) OCs from a wide range of backgrounds using in-depth qualitative techniques such as interview-based methods. Patients from a variety of backgrounds should be involved in how OC systems are designed and help plan how they are implemented in practice.
Staff and patients resisted adopting OCs when they viewed traditional in-person consultation methods as the gold standard. Although this was understandable for complex queries [17], it was unclear whether other factors also influenced this view. Future research should address this evidence gap, particularly as COVID-19 has made remote consultations more commonplace [49]. In the meantime, this perception could be challenged by explaining the benefits of OCs found in our review to prospective users [111].
Organization
For patients and staff to experience the benefits of OCs, they must be widely promoted to patients as a route for them to contact their primary care provider. This can happen through various channels, such as mail-out campaigns (eg, via SMS text message) or by verbally mentioning OCs when in contact with patients (eg, when receptionists speak to patients on the telephone).
To minimize workload associated with OCs, we recommend that organizations (1) allocate sufficient resources to both setting up and processing them, including the provision of training on how to use OCs, and to staff and facilities (eg, computers and rooms) to deal with them; (2) divert as much incoming patient demand as possible through the system to avoid duplication and increase the proportion of patient contacts that benefit from OCs; and (3) incorporate OCs into daily work patterns by scheduling protected time for staff to deal with them to ensure that they do not become additional tasks to complete on top of their normal work.
Our findings show that providers can increase access and patient satisfaction by responding quickly to OCs, although the definitions of what this involved were unclear. We recommend providing an initial response to patients’ OC queries as soon as possible on the same day—either through written message or telephone call. This does not mean that the entire query needs to be resolved at this point, only that initial contact has been made and the query has been acknowledged.
We included studies from 9 countries, all of which were high-income Western countries. Owing to their remote nature, OCs may play a role in middle-income countries where there are isolated communities and fewer health care staff per head of population. However, further research is required to understand how their technological and financial barriers could be overcome.
Wider System
Governmental policies to promote OCs are effective in increasing adoption, although centralized funding is needed to sustain their use. It is unclear what the long-term experience of such policies is from the papers we included, particularly in response to those relating to the COVID-19 pandemic.
Conclusions
This is the first theoretically informed synthesis of empirical research on OCs in primary care and uniquely includes studies conducted during the COVID-19 pandemic. It contributes new knowledge that OCs are safe and have positive impacts on care quality, including increased access to primary care and decreased patient costs. However, they are also complex and often produce conflicting impacts on provider costs, staff and patient workloads, patient satisfaction, and care equity. Some of these are unintended and conflict with the promotion of OCs by policy makers as a way to address already increasing workload and decreasing workforce capacity in primary care [31-36]. Unlike previous evidence syntheses on the topic, we have shown that negative impacts on care quality of OCs can be mitigated through appropriate system design (eg, free text formats and two-way written communication), incorporation of advanced technologies (eg, AI), and integration into technical infrastructure (eg, EHRs) and organizational workflows (eg, timely responses). Since the advent of COVID-19, OCs have become indispensable, although further engineering and implementation research is required to realize their full benefits.
Acknowledgments
This research was funded by Innovate UK (105178) and a Wellcome Trust Clinical Research Career Development Fellowship for BCB (209593/Z/17/Z). NP’s time was partially funded by the National Institute for Health and Care Research (NIHR) Greater Manchester Patient Safety Translational Research Centre. The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, or the Department of Health and Social Care. The NIHR had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data and the final responsibility to submit for publication.
Abbreviations
- AI
artificial intelligence
- EHR
electronic health record
- MCQ
multiple-choice questionnaire
- MMAT
Mixed Methods Appraisal Tool
- NASSS
nonadoption, abandonment, scale-up, spread, and sustainability framework
- OC
online consultation
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Terms used by the included studies for online consultations.
Search terms.
Data extraction form.
Descriptive summary of the included studies.
Description of the online consultation systems studied.
Quality appraisal of the included studies using the Mixed Methods Appraisal Tool.
Low-confidence findings for objective 1.
Low-confidence findings for objective 2.
Outcomes of online consultations in primary care (with exemplar data).
How outcomes of online consultations in primary care are influenced by system design and implementation (with exemplar data).
Footnotes
Authors' Contributions: SD, TC, and BCB refined the research question; developed the search strings; conducted screening, critical appraisal, data extraction, and data analysis; and wrote the first draft of the manuscript. NP contributed to the conception and design of the review. All authors contributed to the final analysis and approved the final submitted version of the manuscript.
Conflicts of Interest: BCB is clinical lead for a commercially available online consultation system.
References
- 1.Bakhai M, Atherton H. How to conduct written online consultations with patients in primary care. BMJ. 2021 Feb 24;372:n264. doi: 10.1136/bmj.n264. [DOI] [PubMed] [Google Scholar]
- 2.Johansson A, Larsson M, Ivarsson B. Patients' experiences with a digital primary health care concept using written dialogues: a pilot study. J Prim Care Community Health. 2020;11:2150132720910564. doi: 10.1177/2150132720910564. https://journals.sagepub.com/doi/10.1177/2150132720910564?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johansson A, Larsson M, Ivarsson B. General practitioners' experiences of digital written patient dialogues: a pilot study using a mixed method. J Prim Care Community Health. 2020;11:2150132720909656. doi: 10.1177/2150132720909656. https://journals.sagepub.com/doi/10.1177/2150132720909656?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, Lewis R, Iyer G, Macleod J, Horwood J. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract. 2021 Feb 25;71(704):e166–77. doi: 10.3399/BJGP.2020.0948. https://bjgp.org/cgi/pmidlookup?view=long&pmid=33558332 .BJGP.2020.0948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eldh AC, Sverker A, Bendtsen P, Nilsson E. Health care professionals' experience of a digital tool for patient exchange, anamnesis, and triage in primary care: qualitative study. JMIR Hum Factors. 2020 Dec 14;7(4):e21698. doi: 10.2196/21698. https://humanfactors.jmir.org/2020/4/e21698/ v7i4e21698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leung K, Qureshi S. Managing high frequency users of an electronic consultation system in primary care: a quality improvement project. BMJ Open Qual. 2021 Jun;10(2):e001310. doi: 10.1136/bmjoq-2020-001310. https://bmjopenquality.bmj.com/lookup/pmidlookup?view=long&pmid=34112657 .bmjoq-2020-001310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Landgren S, Cajander Å. Non-use of digital health consultations among Swedish elderly living in the countryside. Front Public Health. 2021 Sep 10;9:588583. doi: 10.3389/fpubh.2021.588583. doi: 10.3389/fpubh.2021.588583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nijhof D, Ingram A, Ochieng R, Roberts EJ, Poulton B, Ochieng B. Examining GP online consultation in a primary care setting in east midlands, UK. BMC Health Serv Res. 2021 Sep 30;21(1):1030. doi: 10.1186/s12913-021-07039-2. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-021-07039-2 .10.1186/s12913-021-07039-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nilsson E, Sverker A, Bendtsen P, Eldh AC. A human, organization, and technology perspective on patients' experiences of a chat-based and automated medical history-taking service in primary health care: interview study among primary care patients. J Med Internet Res. 2021 Oct 18;23(10):e29868. doi: 10.2196/29868. https://www.jmir.org/2021/10/e29868/ v23i10e29868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cajander Å, Larusdottir M, Hedström G. The effects of automation of a patient-centric service in primary care on the work engagement and exhaustion of nurses. Qual User Exp. 2020 Sep 19;5(1):9. doi: 10.1007/s41233-020-00038-x. [DOI] [Google Scholar]
- 11.Zanaboni P, Fagerlund AJ. Patients' use and experiences with e-consultation and other digital health services with their general practitioner in Norway: results from an online survey. BMJ Open. 2020 Jun 17;10(6):e034773. doi: 10.1136/bmjopen-2019-034773. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=32554721 .bmjopen-2019-034773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nijland N, van Gemert-Pijnen JE, Kelders SM, Brandenburg BJ, Seydel ER. Evaluation of the use of an ask-the-expert e-consultation service for support on health-related requests. Proceedings of the 2nd International Conference on eHealth, Telemedicine, and Social Medicine; eTELEMED '10; February 10-16, 2010; Saint Maarten, The Netherlands. 2010. pp. 72–6. [DOI] [PubMed] [Google Scholar]
- 13.Wästfelt E, Peber E. Impact of digi-physical healthcare. Lund University. 2020. [2020-09-01]. https://lup.lub.lu.se/student-papers/search/publication/9015211 .
- 14.Cowie J, Calveley E, Bowers G, Bowers J. Evaluation of a digital consultation and self-care advice tool in primary care: a multi-methods study. Int J Environ Res Public Health. 2018 May 02;15(5):896. doi: 10.3390/ijerph15050896. https://www.mdpi.com/resolver?pii=ijerph15050896 .ijerph15050896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evaluation of Babylon GP at Hand: final evaluation report. Ipsos MORI and York Health Economics Consortium. 2019. May, [2020-09-01]. http://allcatsrgrey.org.uk/wp/download/informatics/Evaluation-of-Babylon-GP-at-Hand-Final-Report.pdf .
- 16.Fagerlund AJ, Holm IM, Zanaboni P. General practitioners' perceptions towards the use of digital health services for citizens in primary care: a qualitative interview study. BMJ Open. 2019 May 05;9(5):e028251. doi: 10.1136/bmjopen-2018-028251. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=31061056 .bmjopen-2018-028251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Banks J, Farr M, Salisbury C, Bernard E, Northstone K, Edwards H, Horwood J. Use of an electronic consultation system in primary care: a qualitative interview study. Br J Gen Pract. 2018 Jan;68(666):e1–8. doi: 10.3399/bjgp17X693509. https://bjgp.org/cgi/pmidlookup?view=long&pmid=29109115 .bjgp17X693509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, McKinstry B, Porqueddu T, Salisbury C. The potential of alternatives to face-to-face consultation in general practice, and the impact on different patient groups: a mixed-methods case study. Health Serv Deliv Res. 2018 Jun;6(20):1–200. doi: 10.3310/hsdr06200. [DOI] [PubMed] [Google Scholar]
- 19.Atherton H, Brant H, Ziebland S, Bikker A, Campbell J, Gibson A, McKinstry B, Porqueddu T, Salisbury C. Alternatives to the face-to-face consultation in general practice: focused ethnographic case study. Br J Gen Pract. 2018 Apr;68(669):e293–300. doi: 10.3399/bjgp18X694853. https://bjgp.org/cgi/pmidlookup?view=long&pmid=29378697 .bjgp18X694853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carter M, Fletcher E, Sansom A, Warren FC, Campbell JL. Feasibility, acceptability and effectiveness of an online alternative to face-to-face consultation in general practice: a mixed-methods study of webGP in six Devon practices. BMJ Open. 2018 Feb 15;8(2):e018688. doi: 10.1136/bmjopen-2017-018688. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=29449293 .bmjopen-2017-018688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matheson C. University of Southampton. Southampton, UK: Centre of Implementation Science; 2016. Jun 15, [2020-09-01]. Implementation of WebGP and E-consultations in Wessex GP Practices: Interim Update Report. https://tinyurl.com/2h9s9pb5 . [Google Scholar]
- 22.Edwards HB, Marques E, Hollingworth W, Horwood J, Farr M, Bernard E, Salisbury C, Northstone K. Use of a primary care online consultation system, by whom, when and why: evaluation of a pilot observational study in 36 general practices in South West England. BMJ Open. 2017 Nov 22;7(11):e016901. doi: 10.1136/bmjopen-2017-016901. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=29167106 .bmjopen-2017-016901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farr M, Banks J, Edwards HB, Northstone K, Bernard E, Salisbury C, Horwood J. Implementing online consultations in primary care: a mixed-method evaluation extending normalisation process theory through service co-production. BMJ Open. 2018 Mar 19;8(3):e019966. doi: 10.1136/bmjopen-2017-019966. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=29555817 .bmjopen-2017-019966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greater Manchester digital primary care insight full report: Key findings from engagement June-July 2020. Health Innovation Manchester. 2020. [2021-10-01]. https://healthinnovationmanchester.com/wp-content/uploads/2020/12/PCIE-DPC-Full-report-FINAL-20.10.20-1.pdf .
- 25.GM Digital First Primary Care: Patient and public insights: Workshop results. Health Innovation Manchester. 2020. [2021-09-01]. https://healthinnovationmanchester.com/our-work/gm-digital-first-primary-care/
- 26.Bertelsen P, Petersen LS. Danish citizens and general practitioners' use of ICT for their mutual communication. Proceedings of the 15th World Congress on Health and Biomedical Informatics; MEDINFO '15; August 19-23, 2015; São Paulo, Brazil. 2015. pp. 367–9. [DOI] [PubMed] [Google Scholar]
- 27.Ekman B, Thulesius H, Wilkens J, Lindgren A, Cronberg O, Arvidsson E. Utilization of digital primary care in Sweden: descriptive analysis of claims data on demographics, socioeconomics, and diagnoses. Int J Med Inform. 2019 Jul;127:134–40. doi: 10.1016/j.ijmedinf.2019.04.016.S1386-5056(18)30740-8 [DOI] [PubMed] [Google Scholar]
- 28.Fraser H, Coiera E, Wong D. Safety of patient-facing digital symptom checkers. Lancet. 2018 Nov 24;392(10161):2263–4. doi: 10.1016/S0140-6736(18)32819-8.S0140-6736(18)32819-8 [DOI] [PubMed] [Google Scholar]
- 29.Chambers D, Cantrell AJ, Johnson M, Preston L, Baxter SK, Booth A, Turner J. Digital and online symptom checkers and health assessment/triage services for urgent health problems: systematic review. BMJ Open. 2019 Aug 01;9(8):e027743. doi: 10.1136/bmjopen-2018-027743. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=31375610 .bmjopen-2018-027743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Antonio MG, Petrovskaya O, Lau F. The state of evidence in patient portals: umbrella review. J Med Internet Res. 2020 Nov 11;22(11):e23851. doi: 10.2196/23851. https://www.jmir.org/2020/11/e23851/ v22i11e23851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The NHS Long Term Plan. National Health Service. 2019. Jan 7, [2021-03-01]. https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan/
- 32.Telehealth and technology-based health services in primary care. The Royal New Zealand College Of General Practitioners. 2017. Nov, [2021-03-01]. https://www.rnzcgp.org.nz/gpdocs/New-website/Advocacy/Position-Statements/Telehealth-and-technology-based-health-services-in-primary-care-updated-....pdf .
- 33.Gill M. A National Telehealth Strategy For Australia – For Discussion. Australian National Consultative Committee on Electronic Health. 2011. Nov, [2022-03-01]. https://globalaccesspartners.org/ancceh_telehealth_paper.pdf .
- 34.Daniel H, Sulmasy LS, Health and Public Policy Committee of the American College of Physicians Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Ann Intern Med. 2015 Nov 17;163(10):787–9. doi: 10.7326/M15-0498. https://www.acpjournals.org/doi/abs/10.7326/M15-0498?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .2434625 [DOI] [PubMed] [Google Scholar]
- 35.Hobbs FD, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, Salisbury C, National Institute for Health Research School for Primary Care Research Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007-14. Lancet. 2016 Jun 04;387(10035):2323–30. doi: 10.1016/S0140-6736(16)00620-6. https://linkinghub.elsevier.com/retrieve/pii/S0140-6736(16)00620-6 .S0140-6736(16)00620-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marchand C, Peckham S. Addressing the crisis of GP recruitment and retention: a systematic review. Br J Gen Pract. 2017 Apr;67(657):e227–37. doi: 10.3399/bjgp17X689929. https://bjgp.org/cgi/pmidlookup?view=long&pmid=28289014 .bjgp17X689929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beaney P, Odulaja A, Hadley A, Prince C, Obe RC. GP Online: turning expectations into reality with the new NHS app. Br J Gen Pract. 2019 Apr;69(681):172–3. doi: 10.3399/bjgp19X701333. https://bjgp.org/cgi/pmidlookup?view=long&pmid=30745356 .bjgp19X701333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parker RF, Figures EL, Paddison CA, Matheson JI, Blane DN, Ford JA. Inequalities in general practice remote consultations: a systematic review. BJGP Open. 2021 Jun;5(3):BJGPO.2021.0040. doi: 10.3399/BJGPO.2021.0040. http://bjgpopen.org/cgi/pmidlookup?view=long&pmid=33712502 .BJGPO.2021.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joy M, McGagh D, Jones N, Liyanage H, Sherlock J, Parimalanathan V, Akinyemi O, van Vlymen J, Howsam G, Marshall M, Hobbs FR, de Lusignan S. Reorganisation of primary care for older adults during COVID-19: a cross-sectional database study in the UK. Br J Gen Pract. 2020 Aug;70(697):e540–7. doi: 10.3399/bjgp20X710933. https://bjgp.org/cgi/pmidlookup?view=long&pmid=32661009 .bjgp20X710933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Han SM, Greenfield G, Majeed A, Hayhoe B. Impact of remote consultations on antibiotic prescribing in primary health care: systematic review. J Med Internet Res. 2020 Nov 09;22(11):e23482. doi: 10.2196/23482. https://www.jmir.org/2020/11/e23482/ v22i11e23482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cresswell K, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: an interpretative review. Int J Med Inform. 2013 May;82(5):e73–86. doi: 10.1016/j.ijmedinf.2012.10.007.S1386-5056(12)00199-2 [DOI] [PubMed] [Google Scholar]
- 42.Abd-Alrazaq AA, Rababeh A, Alajlani M, Bewick BM, Househ M. Effectiveness and safety of using chatbots to improve mental health: systematic review and meta-analysis. J Med Internet Res. 2020 Jul 13;22(7):e16021. doi: 10.2196/16021. https://www.jmir.org/2020/7/e16021/ v22i7e16021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015 Feb 10;17(2):e44. doi: 10.2196/jmir.3171. https://www.jmir.org/2015/2/e44/ v17i2e44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015 Jun 23;17(6):e148. doi: 10.2196/jmir.4255. https://www.jmir.org/2015/6/e148/ v17i6e148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mold F, Hendy J, Lai YL, de Lusignan S. Electronic consultation in primary care between providers and patients: systematic review. JMIR Med Inform. 2019 Dec 03;7(4):e13042. doi: 10.2196/13042. https://medinform.jmir.org/2019/4/e13042/ v7i4e13042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baines R, Tredinnick-Rowe J, Jones R, Chatterjee A. Barriers and enablers in implementing electronic consultations in primary care: scoping review. J Med Internet Res. 2020 Nov 12;22(11):e19375. doi: 10.2196/19375. https://www.jmir.org/2020/11/e19375/ v22i11e19375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gottliebsen K, Petersson G. Limited evidence of benefits of patient operated intelligent primary care triage tools: findings of a literature review. BMJ Health Care Inform. 2020 May;27(1):e100114. doi: 10.1136/bmjhci-2019-100114. https://informatics.bmj.com/lookup/pmidlookup?view=long&pmid=32385041 .bmjhci-2019-100114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fisk M, Livingstone A, Pit SW. Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res. 2020 Jun 09;22(6):e19264. doi: 10.2196/19264. https://www.jmir.org/2020/6/e19264/ v22i6e19264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Neves AL, Li E, Gupta PP, Fontana G, Darzi A. Virtual primary care in high-income countries during the COVID-19 pandemic: policy responses and lessons for the future. Eur J Gen Pract. 2021 Dec;27(1):241–7. doi: 10.1080/13814788.2021.1965120. https://europepmc.org/abstract/MED/34431426 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bakhai M, Croney L, Waller O, Henshall N, Felstead C. Using online consultations in primary care: implementation toolkit. National Health Service England. 2019. Sep 26, [2020-01-14]. https://www.england.nhs.uk/publication/using-online-consultations-in-primary-care-implementation-toolkit/
- 51.Marshall M, Shah R, Stokes-Lampard H. Online consulting in general practice: making the move from disruptive innovation to mainstream service. BMJ. 2018 Mar 26;360:k1195. doi: 10.1136/bmj.k1195. [DOI] [PubMed] [Google Scholar]
- 52.Stamenova V, Agarwal P, Kelley L, Fujioka J, Nguyen M, Phung M, Wong I, Onabajo N, Bhatia RS, Bhattacharyya O. Uptake and patient and provider communication modality preferences of virtual visits in primary care: a retrospective cohort study in Canada. BMJ Open. 2020 Jul 06;10(7):e037064. doi: 10.1136/bmjopen-2020-037064. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=32636284 .bmjopen-2020-037064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fernández OS, Seguí FL, Vidal-Alaball J, Bonet Simo JM, Vian OH, Cabo PR, Hernandez MC, Dominguez CO, Reig XA, Rodríguez YD, Peralta MM, Hermosilla E, León NM, Guimferrer N, González MA, Cuyàs FG, Sust PP. Primary care doctor characteristics that determine the use of teleconsultations in the Catalan public health system: retrospective descriptive cross-sectional study. JMIR Med Inform. 2020 Jan 31;8(1):e16484. doi: 10.2196/16484. https://medinform.jmir.org/2020/1/e16484/ v8i1e16484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Judson TJ, Odisho AY, Neinstein AB, Chao J, Williams A, Miller C, Moriarty T, Gleason N, Intinarelli G, Gonzales R. Rapid design and implementation of an integrated patient self-triage and self-scheduling tool for COVID-19. J Am Med Inform Assoc. 2020 Jun 01;27(6):860–6. doi: 10.1093/jamia/ocaa051. https://europepmc.org/abstract/MED/32267928 .5817825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Entezarjou A, Bolmsjö BB, Calling S, Midlöv P, Milos Nymberg V. Experiences of digital communication with automated patient interviews and asynchronous chat in Swedish primary care: a qualitative study. BMJ Open. 2020 Jul 23;10(7):e036585. doi: 10.1136/bmjopen-2019-036585. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=32709650 .bmjopen-2019-036585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.López Seguí F, Walsh S, Solans O, Adroher Mas C, Ferraro G, García-Altés A, García Cuyàs F, Salvador Carulla L, Sagarra Castro M, Vidal-Alaball J. Teleconsultation between patients and health care professionals in the Catalan primary care service: message annotation analysis in a retrospective cross-sectional study. J Med Internet Res. 2020 Sep 17;22(9):e19149. doi: 10.2196/19149. https://www.jmir.org/2020/9/e19149/ v22i9e19149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kelley LT, Phung M, Stamenova V, Fujioka J, Agarwal P, Onabajo N, Wong I, Nguyen M, Bhatia RS, Bhattacharyya O. Exploring how virtual primary care visits affect patient burden of treatment. Int J Med Inform. 2020 Sep;141:104228. doi: 10.1016/j.ijmedinf.2020.104228.S1386-5056(19)31064-0 [DOI] [PubMed] [Google Scholar]
- 58.López Seguí F, Vidal-Alaball J, Sagarra Castro M, García-Altés A, García Cuyàs F. General practitioners' perceptions of whether teleconsultations reduce the number of face-to-face visits in the Catalan public primary care system: retrospective cross-sectional study. J Med Internet Res. 2020 Mar 16;22(3):e14478. doi: 10.2196/14478. https://www.jmir.org/2020/3/e14478/ v22i3e14478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Murray MA, Penza KS, Myers JF, Furst JW, Pecina JL. Comparison of eVisit management of urinary symptoms and urinary tract infections with standard care. Telemed J E Health. 2020 May;26(5):639–44. doi: 10.1089/tmj.2019.0044. [DOI] [PubMed] [Google Scholar]
- 60.Penza KS, Murray MA, Myers JF, Furst JW, Pecina JL. Management of acute sinusitis via e-visit. Telemed J E Health. 2021 May;27(5):532–6. doi: 10.1089/tmj.2020.0047. [DOI] [PubMed] [Google Scholar]
- 61.Entezarjou A, Bonamy AK, Benjaminsson S, Herman P, Midlöv P. Human- versus machine learning-based triage using digitalized patient histories in primary care: comparative study. JMIR Med Inform. 2020 Sep 03;8(9):e18930. doi: 10.2196/18930. https://medinform.jmir.org/2020/9/e18930/ v8i9e18930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tarn DM, Hintz C, Mendez-Hernandez E, Sawlani SP, Bholat MA. Using virtual visits to care for primary care patients with COVID-19 symptoms. J Am Board Fam Med. 2021 Feb;34(Suppl):S147–51. doi: 10.3122/jabfm.2021.S1.200241. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=33622830 .34/Supplement/S147 [DOI] [PubMed] [Google Scholar]
- 63.Wilson G, Currie O, Bidwell S, Saeed B, Dowell A, Halim AA, Toop L, Richardson A, Savage R, Hudson B. Empty waiting rooms: the New Zealand general practice experience with telehealth during the COVID-19 pandemic. N Z Med J. 2021 Jul 09;134(1538):89–101. [PubMed] [Google Scholar]
- 64.Turner A, Morris R, Rakhra D, Stevenson F, McDonagh L, Hamilton F, Atherton H, Farr M, Blake S, Banks J, Lasseter G, Ziebland S, Hyde E, Powell J, Horwood J. Unintended consequences of online consultations: a qualitative study in UK primary care. Br J Gen Pract. 2022 Jan 27;72(715):e128–37. doi: 10.3399/BJGP.2021.0426. https://europepmc.org/abstract/MED/34903520 .BJGP.2021.0426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pawson R, Tilley N. Realistic Evaluation. Thousand Oaks, CA, USA: Sage Publications; 1997. [Google Scholar]
- 66.Noyes J, Booth A, Moore G, Flemming K, Tunçalp Ö, Shakibazadeh E. Synthesising quantitative and qualitative evidence to inform guidelines on complex interventions: clarifying the purposes, designs and outlining some methods. BMJ Glob Health. 2019 Jan 25;4(Suppl 1):e000893. doi: 10.1136/bmjgh-2018-000893. https://gh.bmj.com/lookup/pmidlookup?view=long&pmid=30775016 .bmjgh-2018-000893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Centre for Reviews and Dissemination. York, UK: University of York; 2009. Jan, [2021-01-03]. Systematic Reviews: CRD's guidance for undertaking reviews in health care. https://www.york.ac.uk/crd/SysRev/!SSL!/WebHelp/SysRev3.htm . [Google Scholar]
- 68.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71. http://www.bmj.com/lookup/pmidlookup?view=long&pmid=33782057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Darley S, Coulson T, Peek N, Vanderveer S, Wong D, Brown B. Online patient triage and consultation in primary care: a systematic review – CRD42020191802. PROSPERO. 2020. [2022-09-06]. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020191802 .
- 70.Penza KS, Murray MA, Pecina JL, Myers JF, Furst JW. Electronic visits for minor acute illnesses: analysis of patient demographics, prescription rates, and follow-up care within an asynchronous text-based online visit. Telemed J E Health. 2018 Mar;24(3):210–5. doi: 10.1089/tmj.2017.0091. [DOI] [PubMed] [Google Scholar]
- 71.Albert SM, Shevchik GJ, Paone S, Martich GD. Internet-based medical visit and diagnosis for common medical problems: experience of first user cohort. Telemed J E Health. 2011 May;17(4):304–8. doi: 10.1089/tmj.2010.0156. https://europepmc.org/abstract/MED/21457013 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.North F, Crane SJ, Chaudhry R, Ebbert JO, Ytterberg K, Tulledge-Scheitel SM, Stroebel RJ. Impact of patient portal secure messages and electronic visits on adult primary care office visits. Telemed J E Health. 2014 Mar;20(3):192–8. doi: 10.1089/tmj.2013.0097. https://europepmc.org/abstract/MED/24350803 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. Characteristics of patients who seek care via eVisits instead of office visits. Telemed J E Health. 2013 Jul;19(7):515–9. doi: 10.1089/tmj.2012.0221. https://europepmc.org/abstract/MED/23682589 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A'Court C, Hinder S, Fahy N, Procter R, Shaw S. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017 Nov 01;19(11):e367. doi: 10.2196/jmir.8775. https://www.jmir.org/2017/11/e367/ v19i11e367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Abimbola S, Patel B, Peiris D, Patel A, Harris M, Usherwood T, Greenhalgh T. The NASSS framework for ex post theorisation of technology-supported change in healthcare: worked example of the TORPEDO programme. BMC Med. 2019 Dec 30;17(1):233. doi: 10.1186/s12916-019-1463-x. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1463-x .10.1186/s12916-019-1463-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon MP, Griffiths F, Nicolau B, O’Cathain A, Rousseau MC, Vedel I, Pluye P. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018 Dec 18;34(4):285–91. doi: 10.3233/EFI-180221. [DOI] [Google Scholar]
- 77.Hong QN. Reporting the results of the MMAT (version 2018) Mixed Methods Appraisal Tool. 2020. Dec 9, [2021-03-01]. https://tinyurl.com/y9ebmcp8 .
- 78.NVivo: qualitative research data analysis software. QSR International. 2018. [2020-08-01]. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/try-nvivo .
- 79.Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, Apóstolo J, Kirkpatrick P, Loveday H. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. 2020 Oct;18(10):2108–18. doi: 10.11124/JBISRIR-D-19-00169.02174543-202010000-00003 [DOI] [PubMed] [Google Scholar]
- 80.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008 Jul 10;8:45. doi: 10.1186/1471-2288-8-45. https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-8-45 .1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Institute of Medicine (US) Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, USA: National Academies Press (US); 2001. [PubMed] [Google Scholar]
- 82.Chen L, Wong G. Transcriptome informatics. In: Ranganathan S, Gribskov M, Nakai K, Schönbach C, editors. Encyclopedia of Bioinformatics and Computational Biology. Oxford, UK: Academic Press; 2019. pp. 324–40. [Google Scholar]
- 83.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess B, editors. Analyzing Qualitative Data. London, UK: Routledge; 1994. pp. 173–94. [Google Scholar]
- 84.Lewin S, Glenton C, Munthe-Kaas H, Carlsen B, Colvin CJ, Gülmezoglu M, Noyes J, Booth A, Garside R, Rashidian A. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual) PLoS Med. 2015 Oct 27;12(10):e1001895. doi: 10.1371/journal.pmed.1001895. https://dx.plos.org/10.1371/journal.pmed.1001895 .PMEDICINE-D-15-00445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Online consultations research: Summary research findings. National Health Service England and National Health Service Improvement. 2019. Feb, [2020-09-01]. https://www.england.nhs.uk/wp-content/uploads/2019/09/online-consultations-reserach-summary-of-findings.pdf .
- 86.Casey M, Shaw S, Swinglehurst D. Experiences with online consultation systems in primary care: case study of one early adopter site. Br J Gen Pract. 2017 Nov;67(664):e736–43. doi: 10.3399/bjgp17X693137. https://bjgp.org/cgi/pmidlookup?view=long&pmid=28993306 .bjgp17X693137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Andersen KN, Nielsen JA, Kim S. Use, cost, and digital divide in online public health care: lessons from Denmark. Transform Gov People Process Policy. 2019 May 20;13(2):197–211. doi: 10.1108/tg-06-2018-0041. [DOI] [Google Scholar]
- 88.North F, Crane SJ, Stroebel RJ, Cha SS, Edell ES, Tulledge-Scheitel SM. Patient-generated secure messages and eVisits on a patient portal: are patients at risk? J Am Med Inform Assoc. 2013;20(6):1143–9. doi: 10.1136/amiajnl-2012-001208. https://europepmc.org/abstract/MED/23703826 .amiajnl-2012-001208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Player M, O'Bryan E, Sederstrom E, Pinckney J, Diaz V. Electronic visits for common acute conditions: evaluation of a recently established program. Health Aff (Millwood) 2018 Dec;37(12):2024–30. doi: 10.1377/hlthaff.2018.05122. [DOI] [PubMed] [Google Scholar]
- 90.Eccles A, Hopper M, Turk A, Atherton H. Patient use of an online triage platform: a mixed-methods retrospective exploration in UK primary care. Br J Gen Pract. 2019 May;69(682):e336–44. doi: 10.3399/bjgp19X702197. https://bjgp.org/cgi/pmidlookup?view=long&pmid=30910874 .bjgp19X702197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jung C, Padman R. Virtualized healthcare delivery: understanding users and their usage patterns of online medical consultations. Int J Med Inform. 2014 Dec;83(12):901–14. doi: 10.1016/j.ijmedinf.2014.08.004.S1386-5056(14)00147-6 [DOI] [PubMed] [Google Scholar]
- 92.McGrail KM, Ahuja MA, Leaver CA. Virtual visits and patient-centered care: results of a patient survey and observational study. J Med Internet Res. 2017 May 26;19(5):e177. doi: 10.2196/jmir.7374. https://www.jmir.org/2017/5/e177/ v19i5e177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bishop TF, Press MJ, Mendelsohn JL, Casalino LP. Electronic communication improves access, but barriers to its widespread adoption remain. Health Aff (Millwood) 2013 Aug;32(8):1361–7. doi: 10.1377/hlthaff.2012.1151. https://europepmc.org/abstract/MED/23918479 .32/8/1361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Padman R, Shevchik G, Paone S, Dolezal C, Cervenak J. eVisit: a pilot study of a new kind of healthcare delivery. Stud Health Technol Inform. 2010;160(Pt 1):262–6. [PubMed] [Google Scholar]
- 95.Adamson SC, Bachman JW. Pilot study of providing online care in a primary care setting. Mayo Clin Proc. 2010 Aug;85(8):704–10. doi: 10.4065/mcp.2010.0145. https://europepmc.org/abstract/MED/20516427 .S0025-6196(11)60183-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lawless M, Wright E, Davidson J. A collaborative approach to improving patient access in general practice: impact of three different pilot schemes in 12 general practices in Greenwich. London J Prim Care (Abingdon) 2016 Jun 10;8(4):56–65. doi: 10.1080/17571472.2016.1173946. https://europepmc.org/abstract/MED/28250835 .1173946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Johnson KM, Dumkow LE, Burns KW, Yee MA, Egwuatu NE. Comparison of diagnosis and prescribing practices between virtual visits and office visits for adults diagnosed with sinusitis within a primary care network. Open Forum Infect Dis. 2019 Oct 5;6(9):ofz393. doi: 10.1093/ofid/ofz393. https://europepmc.org/abstract/MED/31660415 .ofz393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bavafa H, Hitt LM, Terwiesch C. The impact of e-Visits on visit frequencies and patient health: evidence from primary care. Manage Sci. 2018 Dec;64(12):5461–80. doi: 10.1287/mnsc.2017.2900. https://europepmc.org/abstract/MED/33033417 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med. 2013 Jan 14;173(1):72–4. doi: 10.1001/2013.jamainternmed.305. https://europepmc.org/abstract/MED/23403816 .1392490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rohrer JE, Angstman KB, Adamson SC, Bernard ME, Bachman JW, Morgan ME. Impact of online primary care visits on standard costs: a pilot study. Popul Health Manag. 2010 Apr;13(2):59–63. doi: 10.1089/pop.2009.0018. [DOI] [PubMed] [Google Scholar]
- 101.Jung C, Padman R, Shevchik G, Paone S. Who are portal users vs. early e-Visit adopters? A preliminary analysis. AMIA Annu Symp Proc. 2011;2011:1070–9. https://europepmc.org/abstract/MED/22195168 . [PMC free article] [PubMed] [Google Scholar]
- 102.Prime Minister's Challenge Fund: Improving Access to General Practice. First Evaluation Report: October 2015. National Health Service England. 2015. Oct, [2020-09-01]. https://www.england.nhs.uk/wp-content/uploads/2015/10/pmcf-wv-one-eval-report.pdf .
- 103.Hertzog R, Johnson J, Smith J, McStay FW, da Graca B, Haneke T, Heavener T, Couchman GR. Diagnostic accuracy in primary care e-visits: evaluation of a large integrated health care delivery system's experience. Mayo Clin Proc. 2019 Jun;94(6):976–84. doi: 10.1016/j.mayocp.2019.02.011.S0025-6196(19)30202-2 [DOI] [PubMed] [Google Scholar]
- 104.Peabody MR, Dai M, Turner K, Peterson LE, Mainous 3rd AG. Prevalence and factors associated with family physicians providing e-Visits. J Am Board Fam Med. 2019;32(6):868–75. doi: 10.3122/jabfm.2019.06.190081. http://www.jabfm.org/cgi/pmidlookup?view=long&pmid=31704755 .32/6/868 [DOI] [PubMed] [Google Scholar]
- 105.Leng S, MacDougall M, McKinstry B. The acceptability to patients of video-consulting in general practice: semi-structured interviews in three diverse general practices. J Innov Health Inform. 2016 Jul 15;23(2):141. doi: 10.14236/jhi.v23i2.141. https://informatics.bmj.com/lookup/pmidlookup?view=long&pmid=27869579 . [DOI] [PubMed] [Google Scholar]
- 106.Ruas SS, Assunção AÁ. Teleconsultations by primary care physicians of Belo Horizonte: challenges in the diffusion of innovation. Telemed J E Health. 2013 May;19(5):409–14. doi: 10.1089/tmj.2012.0095. [DOI] [PubMed] [Google Scholar]
- 107.Jury SC, Kornberg AJ. Integrating telehealth in to 'business as usual': Is it really possible? J Telemed Telecare. 2016 Dec;22(8):499–503. doi: 10.1177/1357633X16675802.22/8/499 [DOI] [PubMed] [Google Scholar]
- 108.Rosen R. Meeting need or fueling demand? Improved access to primary care and supply-induced demand. Nuffield Trust and National Health Service England. 2014. Jun, [2020-09-01]. https://www.nuffieldtrust.org.uk/files/2017-01/meeting-need-or-fuelling-demand-web-final.pdf .
- 109.Larsen JH, Neighbour R. Five cards: a simple guide to beginning the consultation. Br J Gen Pract. 2014 Mar;64(620):150–1. doi: 10.3399/bjgp14X677662. https://bjgp.org/cgi/pmidlookup?view=long&pmid=24567647 .64/620/150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, Altman DG, Barbour V, Macdonald H, Johnston M, Lamb SE, Dixon-Woods M, McCulloch P, Wyatt JC, Chan A, Michie S. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014 Mar 07;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 111.Rogers EM. Diffusion of Innovations. New York, NY, USA: Free Press; 1962. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Terms used by the included studies for online consultations.
Search terms.
Data extraction form.
Descriptive summary of the included studies.
Description of the online consultation systems studied.
Quality appraisal of the included studies using the Mixed Methods Appraisal Tool.
Low-confidence findings for objective 1.
Low-confidence findings for objective 2.
Outcomes of online consultations in primary care (with exemplar data).
How outcomes of online consultations in primary care are influenced by system design and implementation (with exemplar data).


