Abstract
Prurigo pigmentosa (PP) is a rare skin disorder presenting as erythematous urticarial papules on the chest and leaving reticulated pigmentation. Although the etiology of PP is unknown, conditions associated with ketosis such as diabetes mellitus, ketogenic diet (KD), and anorexia nervosa are implicated. Herein, we report a 21-year-old woman who developed PP after adhering to a KD and responded to resuming a regular diet.
Keywords: Ketogenic diet, prurigo pigmentosa, treatment
Introduction
Prurigo pigmentosa (PP) is a rare pruritic inflammatory dermatosis characterized by erythematous urticarial papules. It was first reported in Japan by Nagashima et al. In 1971[1] PP was later coined in 1978.[2] It typically occurs in Asian women of childbearing age, although it has also been documented in other regions and ethnicities as well as in men.[3] The etiology of PP is largely unknown, however, various mechanical, inflammatory, and metabolic factors have been assigned to this condition. Importantly, PP has been strongly associated with conditions that commonly induce ketosis, such as restrictive diets, fasting, and uncontrolled diabetes mellitus. Resolution of PP after resuming a regular diet supported the causative role of the ketogenic state in this disease. In addition, certain systemic conditions including adult-onset Still's disease, atopy, Helicobacter pylori infection, and Sjogren's syndrome have also been reported in association with PP.[4]
The ketogenic diet (KD), a well-established treatment for childhood epilepsy has been increasingly used for the management of obesity and diabetes mellitus. KD is a very low carbohydrate, moderate protein, and high-fat diet that induces hepatic production of ketone bodies through activation of hepatic ketogenesis. During this process, fat is broken down into fatty acids and ketone bodies.[5]
PP goes through three stages; in the early stage, the disease presents as pruritic urticarial plaques or papules clinically and superficial perivascular neutrophilic infiltration in pathology. The next stage manifests as crusted erythematous papules and papulovesicles with spongiosis and necrotic keratinocytes. In the last stage, pigmented macules are seen with lymphocytic infiltrate and melanophages in the papillary dermis.[6]
In this report, we describe a 21-year-old woman who developed PP after adhering to a KD and responded to resuming a regular diet.
Case Report
An otherwise healthy 21-year-old woman presented with itchy skin lesions over the chest and neck evolving for 2 weeks. The rash occurred 1 week after starting a carbohydrate-restricted KD.
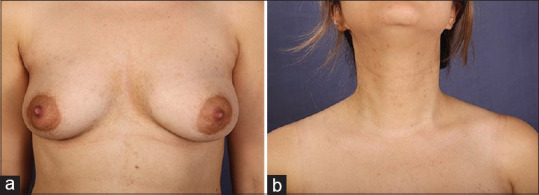
The skin examination showed symmetrically distributed erythematous papules interspersed with dark brown pigmentation in a reticulated pattern in the intermammary and submammary regions, and the neck [Figure 1a and b].
Figure 1.

(a) Prurigo pimentosa: Erythematous papules and plaques on the chest. (b) Prurigo pigmentosa: Erythematous papules on the neck
A punch biopsy was performed; histopathological examination of hematoxylin and eosin-stained tissue revealed acanthotic epidermis with prominent spongiotic vesicles containing lymphocytes and few neutrophils. Papillary dermis revealed superficial perivascular infiltrate of lymphocytes and scattered eosinophils [Figure 2a and b]. Dyskeratotic cells were noted in higher levels of epidermis and exocytosis of lymphocytes and red blood cells were evident.
Figure 2.
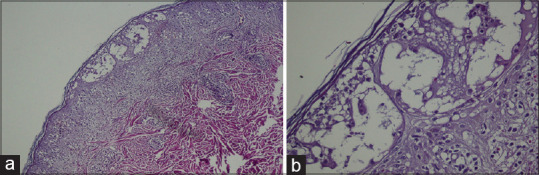
(a): ×10: Low power examination reveals an acanthotic epidermis with some spongiotic vesicles. Superficial dermis is infiltrated by lymphocytes and few eosnophils. (b) ×100: An acanthotic epidermis with prominent spongiotic vesicles containing lymphocytes and few neutrophils. Papillary dermis revesls superficial perivascular infiltrate of lymphocytes as well as few eosinophils
A diagnosis of PP was made based on clinical and pathological findings. The patient was advised to discontinue the KD and take minocycline.
However, she opted to resume a regular diet without taking the drug. She came to her follow-up appointment after 2 months while all of her lesions were resolved, leaving only light-brown postinflammatory pigmentation on her chest and neck [Figure 3a and b].
Figure 3.
(a) Her lesions resolved leaving only multiple post-inflammatory hyperpigmentation (PIH) on her chest. (b) Her lesions resolved leaving only multiple PIH on her neck
After 12 months of follow-up since she resumed a higher carbohydrate diet, there has been no recurrence.
Discussion
The term “PP” was first mentioned in the literature in 1978, 7 years after its first description by Nagashima et al.[1,2]
PP typically affects Japanese women aged 20–30, however, there are increasing reports of the disease in Middle Eastern and Western countries. Less than 300 cases of PP have been published so far.[7,8]
PP is characterized by erythematous pruritic coalescing papules arranged in a reticulate pattern resolving with postinflammatory hyperpigmentation. Pustular, vesicular, and bullous variants have been reported.[4,9,10]
Each stage of PP has distinct histopathological features. The early stage is characterized by a superficial and perivascular dermal neutrophilic infiltration along with papillary dermal edema and slight spongiosis. In the fully developed lesions, a heavier dermal infiltration of lymphocytes, neutrophils, and eosinophils in a lichenoid pattern, reticular degeneration of basal cell layer, and a variable degree of spongiosis and necrotic keratinocytes are seen. In the resolved lesions, a sparse lymphocytic dermal infiltration exists along with upper dermal melanophages.[11]
Although the pathogenesis is incompletely understood, several factors have been strongly associated with the condition, which may be grouped as metabolic (diabetes and ketosis), hormonal (pregnancy and menstruation), and physical factors (skin friction, trauma, and acupuncture).[4]
Ketosis has frequently been linked to PP development in various reports. This occurs with diabetes mellitus, fasting, dieting, anorexia nervosa, hyperemesis gravidarum of pregnancy, and following bariatric surgery, all of which are associated with PP.[7]
It has been hypothesized that ketone bodies play a role in inducing perivascular inflammation, primarily through neutrophils, thus explaining the positive response to medications suppressing neutrophil-mediated processes such as dapsone and tetracyclines. Furthermore, ketone bodies can directly affect cells by causing intracellular damage.[12] Reduced insulin levels, which have been reported to occur after bariatric surgery, may also contribute to the development of PP.[13]
KD is one of the main risk factors for PP. It consists of reducing the carbohydrate content in the diet usually to <50 g/d while increasing the fraction of fat and protein intake. The popularity of this dietary regimen is growing worldwide.[14] As a result, the reports of PP following KD, also known as “keto-rash” have increased on social media. KD is also used for epilepsy, Alzheimer's dementia, Parkinson's disease, brain, and other cancers, obesity, autism spectrum disorder, and endurance athletics.[5]
Bariatric surgeries have been linked to PP in some recent studies.[12,15] It is conceivable that underestimation or underdiagnosis in bariatric surgery could explain the low numbers of cases of PP. Since such procedures are becoming increasingly popular, physicians should be informed about this complication.
The treatment of PP following KD consists of the resumption of a balanced diet and the adjunction of antibiotics that inhibit neutrophil chemotaxis, such as minocycline, doxycycline, and dapsone.[4,5,12] Isotretinoin has also been used successfully in PP.[16]
This case report emphasizes the etiologic role of KD in PP and demonstrates that diet modification alone can be curative for KD-induced PP without the need for any other intervention as reported in a few other studies.
Conclusion
KD and bariatric surgery are currently growing in popularity. When dealing with patients who present with reticulated red papular lesions leaving hyperpigmentation compatible with PP, it is important to inquire about recent diet, bariatric surgery, or other conditions that may cause ketosis. Resuming a regular carbohydrate-rich diet may be recommended as the first step of treatment without an immediate antibiotic prescription. In other words, antibiotics should be kept as a second step or in noncompliant patients, and withdrawal of the KD is sufficient to resolve symptoms with no other intervention.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nagashima M, Ohshiro A, Schimuzu N. A peculiar pruriginous dermatosis with gross reticular pigmentation [in Japanese] Jpn J Dermatol. 1971;81:78–91. [Google Scholar]
- 2.Nagashima M. Prurigo pigmentosa: Clinical observations of our 14 cases. J Dermatol. 1978;5:61–7. doi: 10.1111/j.1346-8138.1978.tb01049.x. [DOI] [PubMed] [Google Scholar]
- 3.Michaels JD, Hoss E, Dicaudo DJ, Price H. Prurigo pigmentosa afer a strict ketogenic diet. Pediatr Dermatol. 2015;32:248–51. doi: 10.1111/pde.12275. [DOI] [PubMed] [Google Scholar]
- 4.Almaani N, Al-Tarawneh AH, Msallam H. Prurigo pigmentosa: A clinicopathological report of three middle eastern patients. Case Rep Dermatol Med. 2018;2018:9406797. doi: 10.1155/2018/9406797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maco MW, Lee E, Wu Y, Lee R. Treatment of prurigo pigmentosa with diet modification: A medical case study. Hawaii J Med Public Health. 2018;77:114–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Oh YJ, Lee MH. Prurigo pigmentosa: A clinicopathologic study of 16 cases. J Eur Acad Dermatol Venereol. 2012;26:1149–53. doi: 10.1111/j.1468-3083.2011.04263.x. [DOI] [PubMed] [Google Scholar]
- 7.Hartman M, Fuller B, Heaphy MR. Prurigo pigmentosa induced by ketosis: Resolution through dietary modification. Cutis. 2019;103:E10–3. [PubMed] [Google Scholar]
- 8.Asgari M, Daneshpazhooh M, Chams Davatchi C, Böer A. Prurigo pigmentosa: An underdiagnosed disease in patients of Iranian descent? J Am Acad Dermatol. 2006;55:131–6. doi: 10.1016/j.jaad.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 9.Kim TI, Choi JW, Jeong KH, Shin MK, Lee MH. Pustular prurigo pigmentosa treated with doxycycline. J Dermatol. 2016;43:965–6. doi: 10.1111/1346-8138.13307. [DOI] [PubMed] [Google Scholar]
- 10.Daneshpazhooh M, Safar F, Barikbin B, Safee-naraghi Z, Asgari M, Chams-Davatchi C. Vesicular prurigo pigmentosa in a 16-year-old girl. Nouv Dermatol. 2004;23:599–603. [Google Scholar]
- 11.Böer A, Misago N, Wolter M, Kiryu H, Wang XD, Ackerman AB. Prurigo pigmentosa: A distinctive inflammatory disease of the skin. Am J Dermatopathol. 2003;25:117–29. doi: 10.1097/00000372-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Alshaya MA, Turkmani MG, Alissa AM. Prurigo pigmentosa following ketogenic diet and bariatric surgery: A growing association. JAAD Case Rep. 2019;5:504–7. doi: 10.1016/j.jdcr.2019.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abbass M, Abiad F, Abbas O. Prurigo pigmentosa after bariatric surgery. JAMA Dermatol. 2015;151:796–7. doi: 10.1001/jamadermatol.2015.0247. [DOI] [PubMed] [Google Scholar]
- 14.Paoli A, Rubini A, Volek JS, Grimaldi KA. Beyond weight loss: A review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr. 2013;67:789–96. doi: 10.1038/ejcn.2013.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alsebayel MM, Ghobara YA, Al-Issa A. Facial prurigo pigmentosa after bariatric surgery. Cureus. 2020;12:e6909. doi: 10.7759/cureus.6909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akoglu G, Boztepe G, Karaduman A. Prurigo pigmentosa successfully treated with low-dose isotretinoin. Dermatology. 2006;213:331–3. doi: 10.1159/000096197. [DOI] [PubMed] [Google Scholar]


