1. INTRODUCTION
Syncope is a dramatic symptom, accounting for about 1.2% of all ED visits. 1 , 2 An electrocardiogram (ECG) is recommended in these patients. 3 , 4 Clinical risk stratification of patients with syncope includes interpretation of ECG findings. 1 , 5 , 6 , 7 , 8 , 9 In risk stratification studies an “abnormal” ECG is consistently the most important risk factor, especially when considering the risk of cardiac arrythmia and/or sudden death. The characteristics of an “abnormal” ECG are similar in these studies. Where differences exist, they are around numerical cut points and criteria requiring subjective interpretation. Furthermore, few studies have considered the knowledge, interpretation, and time needed to apply criteria at the bedside. 7 A consensus conference of experts determined 11 important characteristics of an “abnormal” ECG. 10 , 11 All these characteristics are automatically generated and reported by ECG machines.
In this study, we use natural language processing (NLP) to extract the 11 syncope‐specific criteria from a machine‐generated ECG report and use them to classify abnormal ECGs for syncope. We compare this classification to unstructured physician interpretation as well as the general summary classification of the machine report.
2. METHODS
Commonly used decision tools and expert guidelines were reviewed to come up with criteria for an “abnormal” syncope ECG. Table 1 summarizes the studies and guidelines. From this, we determined that any of the following 11 criteria as indicative of an “abnormal” ECG in a patient with syncope; QTc > 470, LBBB, QRS > 100, Q waves, ST segment changes, PR < 120 ms, any AV (Type I, II, III), left axis deviation, non‐sinus rhythm (including paced) multiple PVC's, sinus bradycardia <40.
Table 1.
Syncope high‐risk ECG criteria from risk stratification studies
| QTc > 470 |
| LBBB |
| QRS > 100 |
| PR < 120 ms |
| Any AV (Type I, II, III) |
| Left axis deviation |
| Non‐sinus rhythm (including paced) multiple PVC's |
| Sinus bradycardia < 40 |
| Q waves |
| ST segment changes |
An NLP algorithm was written in Python to extract the criteria from a typical ECG report (Figure 1). The report was extracted in XML format from the standard 12 lead ECG. The report was interpreted by the NLP algorithm and classified as abnormal if any “abnormal” characteristic was present.
Figure 1.
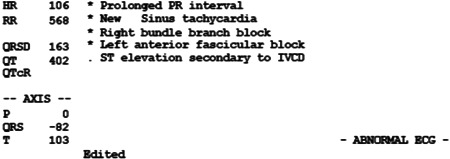
Example of ECG report processed with natural language processing. ECG, electrocardiogram.
To test and refine the algorithm it was applied to the first ECG from a random sample of 100 ED visits for syncope. These 100 ECGs also underwent precise manual application of the 1100 criteria. The manual application was considered the gold standard for accuracy and classification. The NLP algorithm was applied after refinement and used to classify ECGs as abnormal based on these criteria. The performance of the final refined NLP algorithm used to classify the ECG was assessed against the machine‐generated summary report and experienced physician interpretation. In the case of the machine‐generated summary report, it was classified as “normal/borderline” versus “other/abnormal.” The ECGs were also evaluated by two experienced board‐certified emergency medicine physicians. The physicians were aware that the ECG came from patients presenting to the emergency department with syncope but given no specific criteria to apply. They were asked to classify the ECGs as “normal” versus “abnormal” in the cases that they felt the ECG had a finding concerning for syncope. Accuracy, sensitivity, and specificity were calculated with 95% confidence intervals. All data were de‐identified by the institutions health information system before being provided to the researchers for analysis. The protocol was approved by researchers a t and the protocol was approved by the Stanford University Institutional Review Board with an exemption from informed consent.
3. RESULTS
The initial application and assessment of the NLP and script involved 1100 criteria from 100 ECGs of which 62% had at least one “abnormal” criterion. The initial algorithm application correctly classified 1090 of 1100 criteria resulting in 99% (95% CI: 98%–100%) accuracy. The 10 incorrect interpretations across seven ECGs resulted in one incorrectly classified ECG. Rescripting produced a refined algorithm with 100% accuracy and no incorrect categorizations. The refined NLP algorithm had 100% sensitivity (95% CI: 94%–100%) and 100% specificity (95% CI: 91%–100%) compared to the machine‐generated ECG report, 87% sensitivity (95% CI: 76%–94%) and 54% specificity (95% CI: 37%–69%) and physician determinations, sensitivities of 57% (95% CI: 43%–69%) and 85% (95% CI: 74%–93%), specificities of 76% (95% CI: 60%–89%) and 84% (95% CI: 70%–94%) (Table 2).
Table 2.
Comparison of high‐risk syncope ECG classification
| Method | Sensitivity (95% CI) | Specificity (95% CI) |
|---|---|---|
| NLP classification | 100% (94%–100%) | 100% (99%–100%) |
| ECG report | 87% (76%–94%) | 54% (37%–69%) |
| Physician 1 | 85% (74%–93%) | 84% (70%–94%) |
| Physician 2 | 57% (43%–69%) | 76% (60%–89%) |
Abbreviations: ECG, electrocardiogram; NLP, natural language processing.
4. DISCUSSION
In this study, we showed that NLP of a standard ECG report can accurately identify 11 predetermined ECG criteria for syncope. After identifying the criteria, they were utilized to correctly classify abnormal ECGs. The process does not require interpretation of the ECG waveforms and is faster and more accurate than experienced emergency physicians. The process may improve the bedside assessment of ECG criteria for syncope and the performance of clinical decision tools.
A standard 12 lead ECG comes with the waveforms and a machine‐generated report based on a computer algorithm used to interpret the raw ECG data. The use of computers to interpret ECG goes back to 1961 with automated reports becoming standard since the late 1970s. 12 , 13 , 14 Over the years, algorithm techniques and more data from more leads have improved the accuracy of the reports. 15 Current machine‐generated reports are very accurate with small variations between different manufacturers. These differences usually involve interval measurements and interpretation. 16 Traditionally machine‐generated reports are usually overread by physicians for accuracy and there are guidelines for their use. More recently the machine‐generated reports have been found useful for triage decisions in Emergency Departments. 17 , 18
In this study, we performed NLP techniques on the automated report and used manual interpretation of the variables as the gold standard. The initial scripting had 10 incorrect interpretations. Four of these were interval measurement discrepancies. Specifically, the automated report did not note first‐degree AVB as detailed on the ECG with a PR interval greater than 200 ms. These were easily rescripted using the numerical output and not the written report for this criterion. Other misses were due to spelling the entire word “premature ventricular contractions” versus PVC and one miss had both atrial fibrillation and sinus rhythm in the report. The features missed although recurrent were rare and easily rescripted to improve accuracy.
The preliminary development of the NLP algorithm involved the assessment of 1100 manually checked criteria but was limited to 100 ECGs and only one type of machine‐generated report. Further testing and interpretation of other machine‐generated reports are warranted. However, with the standardization of machines and reports, we would expect little or no differences in our findings. For the purposes of NLP scripting, any automated report that could be converted to XML format could be interpreted and classified. If these automated report and format could be imported into a bedside clinical application widespread validation and implementation could be undertaken.
5. CONCLUSION
We report the preliminary findings of a simple NLP algorithm that can be applied to an ECG machine automated report to allow near‐perfect classification of abnormal syncope ECGs. This NLP algorithm may be a valuable tool to help accurately interpret ECGs in patients with syncope and improve their risk stratification.
AUTHOR CONTRIBUTIONS
James Quinn: Conceptualization; Formal analysis; Methodology; Supervision; Writing – original draft. David Kim: Data curation; Formal analysis; Methodology; Writing – review & editing. Brian Travis Rice: Writing – review & editing. Wei David Hao: Investigation; Writing – review & editing.
ETHICS STATEMENT
The Stanford University Institutional Review Board with an exemption from informed consent under the policies of the US Federal Policy for the Protection of Human Subjects Research.
TRANSPARENCY STATEMENT
The lead author James Quinn affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Abstract presented at the Annual Meeting of the Society of Academic Emergency Medicine, New Orleans, LA USA, May 2022.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short‐term serious outcomes. Ann Emerg Med. 2004;43(2):224‐232. [DOI] [PubMed] [Google Scholar]
- 2. Quinn J, Chung S, Murchland A, et al. Association between US physician malpractice claims rates and hospital admission rates among patients with lower‐risk syncope. JAMA Netw Open. 2020;3(12):e2025860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shen WK, Sheldon RS, Benditt DG, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Rhythm Society. Circulation. 2017;136(5):e60‐e122. [DOI] [PubMed] [Google Scholar]
- 4. Costantino G, Furlan R. Syncope risk stratification in the emergency department. Cardiol Clin. 2013;31(1):27‐38. [DOI] [PubMed] [Google Scholar]
- 5. Costantino G, Perego F, Dipaola F, et al. Short‐ and long‐term prognosis of syncope, risk factors, and role of hospital admission: results from the STePS (Short‐Term Prognosis of Syncope) study. J Am Coll Cardiol. 2008;51(3):276‐283. [DOI] [PubMed] [Google Scholar]
- 6. Colivicchi F, Ammirati F, Melina D, Guido V, Imperoli G, Santini M. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J. 2003;24(9):811‐819. [DOI] [PubMed] [Google Scholar]
- 7. Probst MA, Gibson T, Weiss RE, et al. Risk stratification of older adults who present to the Emergency Department with syncope: the FAINT score. Ann Emerg Med. 2020;75(2):147‐158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reed MJ, Newby DE, Coull AJ, Jacques KG, Prescott RJ, Gray AJ. The Risk stratification Of Syncope in the Emergency department (ROSE) pilot study: a comparison of existing syncope guidelines. Emerg Med J. 2007;24(4):270‐275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thiruganasambandamoorthy V, Stiell IG, Sivilotti MLA, et al. Predicting short‐term risk of arrhythmia among patients with syncope: the Canadian syncope arrhythmia risk score. Acad Emerg Med. 2017;24(11):1315‐1326. [DOI] [PubMed] [Google Scholar]
- 10. Sun B, Costantino G. Syncope risk stratification in the ED: directions for future research. Acad Emerg Med. 2013;20(5):503‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sun BC, Thiruganasambandamoorthy V, Cruz JD. Standardized reporting guidelines for emergency department syncope risk‐stratification research. Acad Emerg Med. 2012;19(6):694‐702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Milliken JA, Wartak J, Orme W, Skoulikidis AP, Lywood DW. Use of computers in the interpretation of electrocardiograms. Can Med Assoc J. 1969;101(7):39‐43. [PMC free article] [PubMed] [Google Scholar]
- 13. Bailey JJ, Berson AS, Garson A, et al. Recommendations for standardization and specifications in automated electrocardiography: bandwidth and digital signal processing. A report for health professionals by an ad hoc writing group of the Committee on Electrocardiography and Cardiac Electrophysiology of the Council on Clinical Cardiology, American Heart Association. Circulation. 1990;81(2):730‐739. [DOI] [PubMed] [Google Scholar]
- 14. Kligfield P, Gettes LS, Bailey JJ, et al. Recommendations for the standardization and interpretation of the electrocardiogram. Part I: the electrocardiogram and its technology. A scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Heart Rhythm. 2007;4(3):394‐412. [DOI] [PubMed] [Google Scholar]
- 15. Chang KC, Hsieh PH, Wu MY, et al. Usefulness of machine learning‐based detection and classification of cardiac arrhythmias with 12‐lead electrocardiograms. Can J Cardiol. 2020;37:94‐104. [DOI] [PubMed] [Google Scholar]
- 16. Kligfield P, Badilini F, Denjoy I, et al. Comparison of automated interval measurements by widely used algorithms in digital electrocardiographs. Am Heart J. 2018;200:1‐10. [DOI] [PubMed] [Google Scholar]
- 17. Hughes KE, Lewis SM, Katz L, Jones J. Safety of computer interpretation of normal triage electrocardiograms. Acad Emerg Med. 2017;24(1):120‐124. [DOI] [PubMed] [Google Scholar]
- 18. Winters LJ, Dhillon RK, Pannu GK, Terrassa P, Holmes JF, Bing ML. Emergent cardiac outcomes in patients with normal electrocardiograms in the emergency department. Am J Emerg Med. 2022;51:384‐387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


