Abstract
We analyzed the effect of COVID-19 on healthcare demand and invasive pneumococcal disease in children in Catalonia, Spain. Compared with 2018–2019, we noted large reductions in healthcare activities and incidence of invasive pneumococcal disease in 2020. These changes likely resulted from nonpharmaceutical measures implemented during the COVID-19 pandemic.
Keywords: invasive pneumococcal disease, serotype, 13-valent pneumococcal conjugate vaccine, nonpharmaceutical measures, COVID-19, SARS-CoV-2, coronavirus disease, severe acute respiratory syndrome coronavirus 2, bacteria, viruses, respiratory infections, zoonoses, Catalonia, Spain
SARS-CoV-2 was identified in 2019, and the World Health Organization declared COVID-19 a pandemic on March 11, 2020. As of July 11, 2021, >186 million cases and >4 million deaths had been recorded (1).
The first imported case of COVID-19 in Catalonia, Spain, was reported on February 26, 2020. Endemic transmission was declared on March 14, when the government of Spain introduced a strict lockdown until May 11. Other mandates followed, such as mask use, physical distancing, and reducing frequency of social contacts to reduce disease transmission (2). The peak number of cases was recorded in April 2020; cases subsequently declined and then occurred in epidemic waves. In 2020, a total of 356,724 cases and 8,723 deaths were reported in Catalonia (3).
Measures to reduce COVID-19 transmission have been associated with a reduction in diseases caused by respiratory pathogens, such as invasive pneumococcal disease (IPD) (4). IPD caused by Streptococcus pneumoniae has high rates of severe illness and death, especially in the very old and very young. In Catalonia, IPD incidence in children <5 years of age was 29.1/100,000 population in 2018, and 74.4% of cases were caused by serotypes not included in the 13-valent pneumococcal conjugate vaccine (PCV13) (5). Vaccine coverage in children was 92.9% in 2019. We assessed the effect of COVID-19 on the demand for care of IPD in children in 2020 compared with 2018–2019.
The Study
We investigated IPD cases identified during 2018–2020 in 3 pediatric hospitals, Sant Joan de Déu, Vall d’Hebron, and HM Nens, which serve 521,463 children <18 years of age, 32% of pediatric patients in Catalonia. A confirmed case of IPD was defined as isolation or detection of S. pneumoniae DNA by PCR from a normally sterile site. Data collected were number of emergency department (ED) visits and admissions; requests for sterile cultures as blood, cerebrospinal fluid, and pleural fluid; requests for PCR for pneumococcus; confirmed cases of IPD; and serotype distribution.
We calculated mean incidence rates per 100,000 person-years by using population served by the 3 hospitals each year. We compared incidence rates in 2018–2019 with 2020 rates by calculating incidence rate ratio (IRR) and 95% CI annually, by quarters and age groups (0–4 and 5–17 years). We expressed percentage change in IRR according to the formula (1–IRR) × 100. We performed analysis by using R version 3.5.0 (The R Project for Statistical Computing, https://www.r-project.org).
Total numbers of visits to EDs were 225,031 in 2018, 229,256 in 2019, and 148,637 in 2020; total numbers of hospital admissions were 11,421 in 2018, 11,206 in 2019, and 8,423 in 2020. Compared with mean incidence in 2018–2019, ED visits declined by 35% in 2020, and hospital admissions declined by 26% (Table 1). The number of cultures was reduced in 2020 by 6%, and the number of requested PCR tests specific for S. pneumoniae declined by 23%, predominantly in children 0–4 years of age (23%).
Table 1. Healthcare activity and IPD incidence by age group, Catalonia, Spain, 2018–2019 and 2020*.
| Variable | No. cases (incidence, cases/100,000 population) |
IRR (95% CI) | p value | |
|---|---|---|---|---|
| Mean 2018–19 | 2020 | |||
| All ages | ||||
| Emergency department visits | 227,148 (43,661.3) | 148,637 (28,437.6) | 0.65 (0.64–0.66) | <0.0001 |
| Hospital admissions | 11,313 (2,174.5) | 8,423 (1,611.5) | 0.74 (0.72–0.76) | <0.0001 |
| Samples for culture, HSJD | 7,489 (1,439.5) | 7,106 (1,359.5) | 0.94 (0.91–0.98) | 0.001 |
| Samples for PCR, HSJD and HVH | 641 (123.2) | 497 (95.1) | 0.77 (0.69–0.87) | <0.0001 |
| IPD cases | 57 (11.0) | 20 (3.8) | 0.35 (0.21–0.57) | <0.0001 |
| PCV13 serotypes | 25 (4.8) | 10 (1.9) | 0.40 (0.18–0.82) | 0.01 |
| Serotype 3 | 17 (3.3) | 9 (1.7) | 0.53 (0.22–1.17) | 0.07 |
| Non-PCV13 serotypes |
29 (5.6) |
10 (1.9) |
0.34 (0.17–0.70) |
0.003 |
| 0–4 y | ||||
| Emergency department visits | 108,757 (93,016.7) | 68,684 (60,617.9) | 0.65 (0.64–0.66) | <0.0001 |
| Hospital admissions | 6,519 (5,575.5) | 4,256 (3,756.2) | 0.67 (0.65–0.70) | <0.0001 |
| Samples for culture, HSJD | ND | ND | NA | NA |
| Samples for PCR, HSJD and HVH | 459 (392.6) | 342 (301.8) | 0.77 (0.67–0.88) | 0.0002 |
| IPD cases | 44 (37.6) | 15 (13.2) | 0.35 (0.19–0.62) | 0.0001 |
| PCV13 serotypes | 18 (15.4) | 8 (7.1) | 0.46 (0.19–1.04) | 0.06 |
| Serotype 3 | 12 (10.3) | 8 (7.1) | 0.69 (0.27–1.69) | 0.42 |
| Non-PCV13 serotypes |
25 (21.4) |
7 (6.2) |
0.29 (0.12–0.67) |
0.002 |
| 5–17 y | ||||
| Emergency department visits | 118,391 (29,353.5) | 79,953 (19,530.7) | 0.66 (0.65–0.67) | <0.0001 |
| Hospital admissions | 4,794 (1,188.6) | 4,167 (1,017.9) | 0.86 (0.82–0.89) | <0.0001 |
| Samples for culture. (HSJD | ND | ND | NA | NA |
| Samples for PCR. HSJD and HVH | 182 (45.1) | 155 (37.9) | 0.84 (0.68–1.04) | 0.11 |
| IPD cases | 13 (3.2) | 5 (1.2) | 0.38 (0.13–1.06) | 0.06 |
| PCV13 serotypes | 7 (1.7) | 2 (0.5) | 0.28 (0.06–1.36) | 0.17 |
| Serotype 3 | 5 (1.2) | 1 (0.2) | 0.20 (0.02–1.69) | 0.21 |
| Non-PCV13 serotypes | 4 (1.0) | 3 (0.7) | 0.74 (0.16–3.30) | 0.71 |
*HSJD, Hospital Sant Joan de Dèu; HVH, Hospital Vall Hebron; IPD, invasive pneumococcal disease; IRR, incidence rate ratio; NA, not applicable; ND, not done; PCV13, 13-valent pneumococcal conjugate vaccine.
IPD incidence per 100,000 person-years was 11 in 2018–2019 and 3.8 in 2020, a reduction of 65%; this same reduction was observed in the 0–4-year age group in 2020 (Table 2). Reduction of IPD incidence in 2020 was greater in the second and fourth quarter; no IPD cases were reported in the second quarter of 2020. Incidence per 100,000 person-years of IPD caused by PCV13 serotypes was 4.8 in 2018–2019 and 1.9 in 2020; IPD caused by non-PCV13 serotypes was 5.6 in 2018–2019 and 1.9 in 2020 (Table 1; Figure 1). Serotype 3 was the most frequent serotype in 2018–2019 (30.6%) and 2020 (45%) (Figure 2).
Table 2. Healthcare activity and IPD incidence by quarter, Catalonia, Spain, 2018–19 and 2020*.
| Variable | No. cases (incidence, cases/100,000 population) |
IRR (95% CI) | p value | |
|---|---|---|---|---|
| Mean 2018–2019 | 2020 | |||
| 1st quarter | ||||
| Emergency department visits | 61,590 (11,838.5) | 54,430 (10,413.7) | 0.88 (0.87–0.89) | <0.0001 |
| Hospital admissions | 3,049 (586.1) | 2,785 (532.8) | 0.91 (0.86–0.96) | 0.0003 |
| Samples for culture, HSJD | 1,968 (378.3) | 2,192 (419.4) | 1.11 (1.04–1.18) | 0.0009 |
| Samples for PCR, HSJD and VH | 185 (35.6) | 182 (34.8) | 0.98 (0.80–1.20) | 0.84 |
| IPD cases | 17 (3.3) | 15 (2.9) | 0.88 (0.43–1.77) | 0.72 |
| PCV13 serotypes | 7 (1.3) | 9 (1.7) | 1.28 (0.47–3.62) | 0.64 |
| Serotype 3 | 5 (1.0) | 8 (1.5) | 1.59 (0.51–5.35) | 0.43 |
| Non-PCV13 serotypes |
10 (1.9) |
6 (1.1) |
0.60 (0.20–1.65) |
0.33 |
| 2nd quarter | ||||
| Emergency department visits | 55,519 (10,671.6) | 23,025 (4,405.2) | 0.41 (0.40–0.42) | <0.0001 |
| Hospital admissions | 2,772 (532.8) | 1,670 (319.5) | 0.60 (0.56–0.64) | <0.0001 |
| Samples for culture, HSJD | 1,891 (363.5) | 1,633 (312.4) | 0.86 (0.80–0.92) | <0.0001 |
| Samples for PCR, HSJD and VH | 141 (27.1) | 107 (20.5) | 0.76 (0.59–0.97) | 0.03 |
| IPD cases | 15 (2.9) | 0 | NA | <0.0001 |
| PCV13 serotypes | 8 (1.5) | 0 | NA | 0.008 |
| Serotype 3 | 6 (1.2) | 0 | NA | 0.03 |
| Non-PCV13 serotypes |
6 (1.2) |
0 |
NA |
0.03 |
| 3rd quarter | ||||
| Emergency department visits | 44,594 (8,571.6) | 34,933 (6,683.5) | 0.78 (0.77–0.79) | <0.0001 |
| Hospital admissions | 2,171 (417.3) | 1,810 (346.3) | 0.83 (0.78–0.88) | <0.0001 |
| Samples for culture, HSJD | 1,789 (343.9) | 1,618 (309.6) | 0.90 (0.84–0.96) | 0.002 |
| Samples for PCR, HSJD and VH | 112 (21.5) | 86 (16.5) | 0.76 (0.58–1.01) | 0.06 |
| IPD cases | 6 (1.2) | 2 (0.4) | 0.33 (0.05–1.57) | 0.18 |
| PCV13 serotypes | 2 (0.4) | 0 | – | 0.25 |
| Serotype 3 | 1 (0.2) | 0 | – | 0.50 |
| Non-PCV13 serotypes |
3 (0.6) |
2 (0.4) |
0.66 (0.11–3.97) |
0.65 |
| 4th quarter | ||||
| Emergency department visits | 65,445 (12,579.5) | 36,249 (6,935.3) | 0.55 (0.54–0.56) | <0.0001 |
| Hospital admissions | 3,321 (638.4) | 2,158 (412.9) | 0.65 (0.61–0.68) | <0.0001 |
| Samples for culture, HSJD | 1,841 (353.9) | 1,663 (318.2) | 0.90 (0.84–0.96) | 0.002 |
| Samples for PCR, HSJD and VH | 203 (39.0) | 122 (23.3) | 0.60 (0.48–0.75) | <0.0001 |
| IPD cases | 19 (3.7) | 3 (0.6) | 0.16 (0.04–0.49) | 0.001 |
| PCV13 serotypes | 8 (1.5) | 1 (0.2) | 0.12 (0.01–0.78) | 0.02 |
| Serotype 3 | 5 (1.0) | 1 (0.2) | 0.20 (0.01–1.44) | 0.22 |
| Non-PCV13 serotypes | 10 (1.9) | 2 (0.4) | 0.20 (0.03–0.82) | 0.02 |
*HSJD, Hospital Sant Joan de Dèu; HVH, Hospital Vall Hebron; IPD, invasive pneumococcal disease; IRR, incidence rate ratio; NA, not applicable; PCV13, 13-valent pneumococcal conjugate vaccine.
Figure 1.
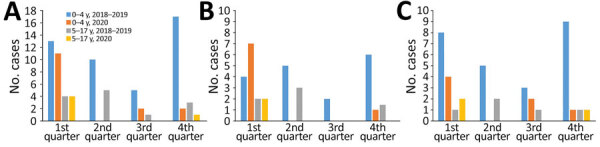
Invasive pneumococcal disease cases by quarter, age group, and year, Catalonia, Spain. A) Global cases; B) 13-valent pneumococcal conjugate vaccine serotypes; C) non–13-valent pneumococcal conjugate vaccine serotypes.
Figure 2.
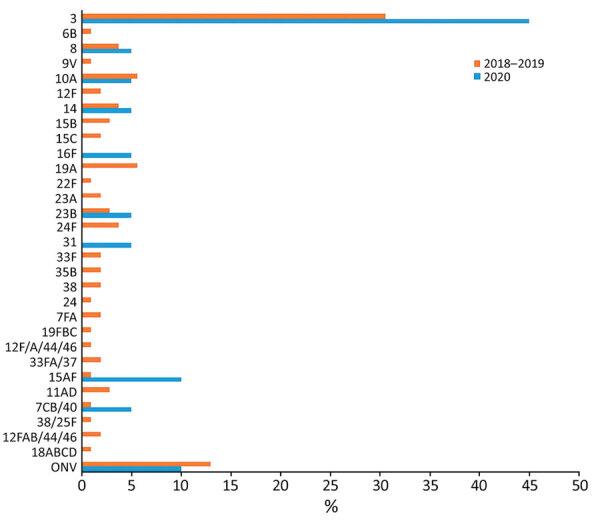
Distribution of invasive pneumococcal disease serotypes, Catalonia, Spain, 2018–2019 and 2020
Conclusions
The lockdown during the first months of the COVID-19 pandemic in 2020, together with social distancing measures, reduced mobility, and limits on the number of persons at social gatherings, had a positive effect on preventing IPD transmission in children and on indicators of healthcare activity. Overall reduction in IPD incidence was observed throughout 2020 compared with incidence for 2018–2019. No IPD cases were detected in the second quarter of 2020, coinciding with the lockdown, and a reduction of 84% was observed in the fourth quarter, coinciding with intensifying containment measures after the second wave of COVID-19 (6).
The percentage reduction in IPD cases in 2020 was similar in children <5 years of age (65%) and those 5–17 years of age (62%), although in the older group the reduction was not statistically significant because very few cases occurred in 2020. Other authors have described reductions in IPD during the COVID-19 pandemic. A prospective analysis from 26 countries found reductions of IPD of 68% at 4 weeks and of 82% at 8 weeks (7). In Hong Kong, observed IPD cases declined by 74.7% in 2020 compared with 2015–2019 (8). Some authors have stated that during 2020 no campaign occurred to increase pneumococcal vaccination and no other changes in practice affecting diagnosis or notification requirements for IPD were enacted that would explain reductions in incidence (9).
Serotype 3 was the most frequent serotype in the 2 periods (30.6% in 2018–2019 and 45% in 2020), and no significant reduction was detected. Similar results were observed by Teng et al. (8): 52.9% of cases in 2015–2019 and 45.7% in 2020 were serotype 3. We observed reduction in IPD incidence in 2020 compared with 2018–2019 in PCV13 (60%) and non-PCV13 (66%) serotypes.
A systematic review of 15 studies (10) concluded that nonpharmaceutical interventions could delay the introduction of influenza virus and are therefore effective in controlling influenza epidemics. In Catalonia, the active surveillance system for influenza and other acute respiratory infections found that influenza epidemic activity in the 2019–20 season had a short duration of 8 weeks (weeks 3–11) (11). Other authors recorded a similar situation; influenza and respiratory syncytial virus incidence declined sharply, and the season in 2020 was brief and ended rapidly compared with previous years (12). Viral infections might create favorable conditions in nasopharyngeal mucosa for invasive, colonizing pneumococcus causing IPD, so reduced influenza transmission during the pandemic might also have contributed to the reduction in IPD (8).
We found a reduction in ED visits (35%) and hospital admissions (26%) for IPD in 2020 compared with 2018–2019. Declines were greatest in the second quarter (59% for ED visits, 40% for hospital admissions), followed by the fourth quarter (45% for ED visits, 35% for hospital admissions), coinciding with the total lockdown and more stringent public health measures adopted because of the second epidemic wave in this setting (6). The number of cultures and specific requests for S. pneumoniae PCR declined less than the number of ED visits, hospital admissions, and IPD incidence in 2020. Increased public awareness of adequate individual use of nonpharmaceutical protective measures and social distancing measures had an effect on reducing incidence of IPD and other respiratory infections (13).
One limitation of our study is that the data analyzed came from just 32% of pediatric patients in Catalonia treated in 3 pediatric reference hospitals. However, the hospitals were reference hospitals; therefore, we believe these data are representative of the pediatric population in Catalonia. In addition, not all patients were tested during the first wave, so the exact incidence of SARS-CoV-2 infection in the first months of the pandemic is unknown. A strength of the study is that data were collected in a similar way throughout the study.
In summary, the reduction in ED visits and hospital admissions in 2020 compared to 2018–2019 in Catalonia was greater than the reduction in requests for culture and PCR specific for S. pneumoniae. The reduction in IPD incidence was more marked during the second quarter of 2020, coinciding with COVID-19 lockdowns.
Acknowledgments
We thank all the participants of this study. We are grateful to Lorena Coronas for her support in data management and manuscript submission.
CIBER of Epidemiology and Public Health (CIBERESP), Carlos III Health Institute, Madrid (PI17/00337) and the Catalan Agency for the Management of Grants for University Research (AGAUR Grant number 2017/SGR 1342 and 2017/SGR00742) supported this study.
C.M.-A. received a grant from Pfizer laboratories to Sant Joan de Déu Foundation. J.J.G.-G. received travel grants and fees from Pfizer.
Biography
Dr. Ciruela is the head of the Emerging Diseases service in the General Subdirectorate for Surveillance and Response to Public Health Emergencies of the Public Health Agency of Catalonia, Spain. Her main research interest is the epidemiology and control of infectious diseases, focusing on emerging and reemerging infections.
Footnotes
Suggested citation for this article: Ciruela P, Soldevila N, García-Garcia JJ, González-Peris S, Díaz-Conradi A, Redin A, et al. Effect of COVID-19 pandemic on invasive pneumococcal disease in children, Catalonia, Spain. Emerg Infect Dis. 2022 Nov [date cited]. https://doi.org/10.3201/eid2811.211741
References
- 1.World Health Organization. Weekly epidemiological update on COVID-19 [cited 2021 Jul 28]. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19–13-july-2021
- 2.Ministry of the President. Spain. Royal Decree 463/2020, of March 14, declaring the state of alarm for the management of the situation of the health crisis caused by COVID-19 [cited 2021 Jun 15]. https://www.boe.es/eli/es/rd/2020/03/14/463
- 3.Coordination Center for Health Alerts and Emergencies. Update No. 282. Coronavirus disease (COVID-19) [cited 2021 Jun 15]. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_282_COVID-19.pdf
- 4.Mutnal MB, Arroliga AC, Walker K, Mohammad A, Brigmon MM, Beaver RM, et al. Early trends for SARS-CoV-2 infection in central and north Texas and impact on other circulating respiratory viruses. J Med Virol. 2020;92:2130–8. 10.1002/jmv.26010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ciruela P, Jané M. Epidemiology of invasive pneumococcal disease in Catalonia, report 2017–2018. 2020. Nov 25 [cited 2021 Jun 22]. https://canalsalut.gencat.cat/web/.content/_Professionals/Vigilancia_epidemiologica/documents/arxius/malaltia-pneumoccocica-invasiva-informe-2017-2018_final-en.pdf
- 6.Deputy director of public health surveillance and response to emergencies. Department of Health. Technical summary report of COVID-19 cases in Catalonia, number 39 [in Spanish]. 2021. Jan 5 [cited 2021 Jun 15]. https://salutpublica.gencat.cat/web/.content/minisite/aspcat/vigilancia_salut_publica/vigilancia_covid19/informes_tecnics_covid19/39-informe-tecnic-covid-19-es.pdf
- 7.Brueggemann AB, Jansen van Rensburg MJ, Shaw D, McCarthy ND, Jolley KA, Maiden MCJ, et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021;3:e360–70. 10.1016/S2589-7500(21)00077-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teng JLL, Fok KMN, Lin KPK, Chan E, Ma Y, Lau SKP, et al. Substantial decline in invasive pneumococcal disease (IPD) during COVID-19 pandemic in Hong Kong. Clin Infect Dis. 2022;74:335–8. 10.1093/cid/ciab382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim RH, Chow A, Ho HJ. Decline in pneumococcal disease incidence in the time of COVID-19 in Singapore. J Infect. 2020;81:e19–21. 10.1016/j.jinf.2020.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ryu S, Gao H, Wong JY, Shiu EYC, Xiao J, Fong MW, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—international travel-related measures. Emerg Infect Dis. 2020;26:961–6. 10.3201/eid2605.190993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deputy director of public health surveillance and response to emergencies, Department of Health. Information Plan on acute respiratory diseases in Catalonia (PIDIRAC) 2019–2020 [in Spanish] [cited 2021 Jun 15]. https://canalsalut.gencat.cat/web/.content/_Professionals/Vigilancia_epidemiologica/documents/arxius/balanc-temporada-gripal-2019-20.pdf
- 12.Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children - A nationwide register study in Finland. EClinicalMedicine. 2021;34:100807. 10.1016/j.eclinm.2021.100807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yun HE, Ryu BY, Choe YJ. Impact of social distancing on incidence of vaccine-preventable diseases, South Korea. J Med Virol. 2021;93:1814–6. 10.1002/jmv.26614 [DOI] [PubMed] [Google Scholar]


