Background:
To evaluate the clinical efficacy of acupuncture and moxibustion therapy compared to non-acupuncture therapy in the treatment of simple obesity in adult.
Methods:
Randomized clinical trials concerning acupuncture and moxibustion therapy as a treatment of simple adult obesity were searched in the following Chinese and English databases: Chinese National Knowledge Infrastructure, China Science and Technology Journal Database, WanFang Database, Chinese Biomedical Literature Database, PubMed, Web of Science, Embase, Medline and Cochrane Library. Two researchers independently screened suitable literature according to inclusion and exclusion criteria, extracted data, and evaluated the quality of included studies using the Jadad score scale. After that, data analysis was performed using RevMan 5.4.1 software, Stata 17.0 software and SPSS 25.0 software.
Results:
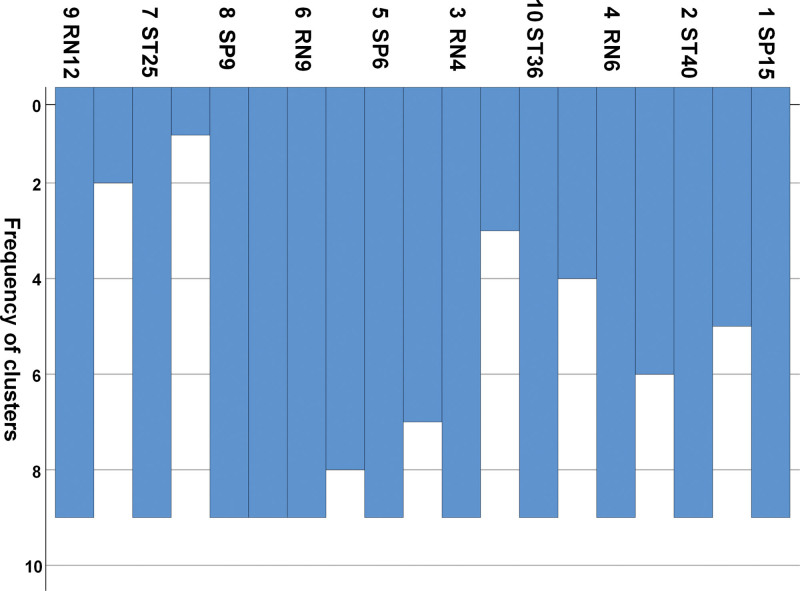
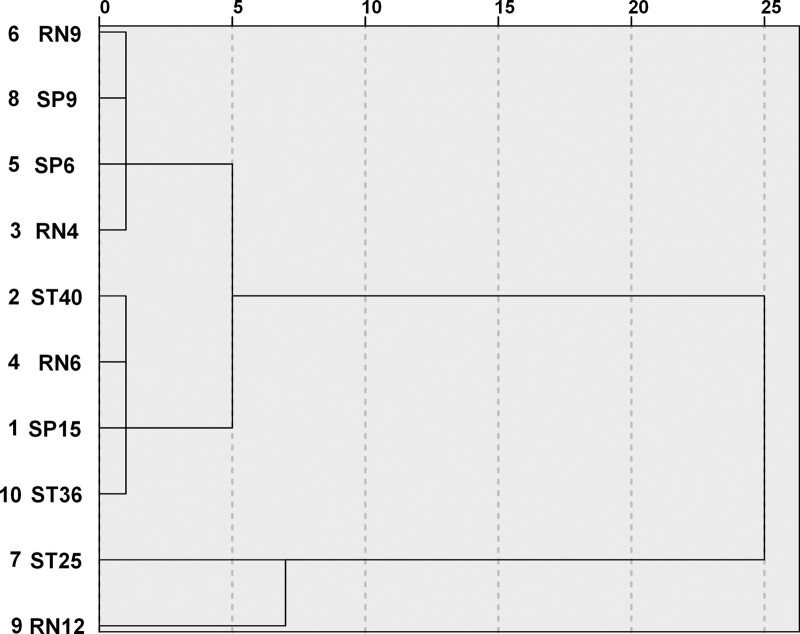
A total of 14 studies involving 1116 adults with simple obesity were included in the meta-analysis. Results revealed that BMI, body weight, waist circumference, total effective rate, triglyceride in the acupuncture group were superior to those in the non-acupuncture group, while there was no statistical difference in improving low density lipoprotein, high density lipoprotein and total cholesterol. As to the selection of acupoints, the acupoints of the stomach meridian of Foot Yangming have the highest frequency of use, with a frequency of 30 times, accounting for 35%. The acupoints can be divided into three clusters: the first category: RN9-SP9-SP6-RN4; the second category: ST40-RN6-SP15-ST36; the third category: ST25-RN12.
Conclusion:
Acupuncture and moxibustion is effective in treating adult simple obesity; however, due to the low score of the included studies, we still expect the results of higher-quality literature to provide a higher-level evidence-based basis for clinical decision-making. Furthermore, for the treatment of adult simple obesity, acupoints analysis revealed that Tianshu (ST25), Zhongwan (RN12), Zusanli (ST36), Fenglong (ST40) and Qihai (RN6) can form the basis for the treatment of simple obesity in adult.
Keywords: acupuncture therapy, cluster analysis, meta-analysis, simple obesity, systematic review
1. Introduction
Simple obesity refers to a disease with abnormal body mass caused by excessive intake of calories than consumption and excessive accumulation of fat in the body.[1] Obesity is a major risk factor for metabolic diseases (cardiovascular diseases, cancer and diabetes), which can significantly increase the risk of metabolic diseases (such as type 2 diabetes and fatty liver), cardiovascular diseases (hypertension, myocardial infarction, and stroke), musculoskeletal diseases (osteoarthritis) and premature death.[2] Weight gain is strongly related to the increased mortality of all cancers and cancers at multiple specific sites.[3] According to the survey of China chronic disease and nutrition monitoring from 2015 to 2019, the overweight rate of adults in China is 34.3%, and the obesity rate is 16.4%, which has become an urgent public health problem to be solved.[4]
The common methods of modern medical treatment for simple obesity mainly include intensive lifestyle intervention drug therapy and surgical treatment, but it is not suitable for long-term use because of its poor effect, high cost, high risk, more side effects and other reasons.[5,6] The external treatment of simple obesity has attracted more and more attention, and acupuncture and moxibustion is one of the commonly used external treatment methods.[7] Acupuncture and moxibustion therapy generally refers to a kind of therapy that uses special metal needles to stimulate acupoints with lifting, thrusting, and rotating, or uses Moxa as raw material to warm the skin surface of acupoints, and prevent and treat diseases by dredging the meridians, regulating functions of the viscera, or warming the meridians, supporting yang and dispersing cold.[8] As an important part of traditional Chinese medicine, it is widely used in the clinical treatment of simple obesity and has the advantages of safety, effectiveness, simplicity and green economy.[9] We compared the clinical efficacy of acupuncture and non-acupuncture in the treatment of adult simple obesity through meta-analysis, to provide evidence for clinical practice and related research.
2. Data and Methods
2.1. Patient and public involvement
There was no patient and public involvement in present meta-analysis. An ethical approval is not necessary for a meta-analysis.
2.2. Inclusion criteria for the literature
(1) Type of study: randomized controlled trial (RCT) of acupuncture and moxibustion in the treatment of simple obesity in adults.
(2) Participants: age ≥ 18 years old, unlimited gender, race, course of disease and source of cases, which meet the diagnostic criteria of simple obesity.
(3) Intervention measures: acupuncture and moxibustion therapy was used in the experimental group, and non-acupuncture therapy was used in the control group.
2.3. Exclusion criteria for the literature
(1) Both the experimental group and the control group were treated with acupuncture and moxibustion;
(2) The basic treatment was different between the groups: the experimental group had some kind of non-acupuncture intervention, but the control group did not carry out this intervention;
(3) The experimental group or control group used traditional Chinese medicine or proprietary Chinese medicine;
(4) Study on acupuncture and moxibustion treatment of other basic diseases accompanied by obesity.
2.4. Retrieval strategy
The Chinese National Knowledge Infrastructure, China biomedical literature database, Chongqing VIP full-text database, WanFang database, PubMed, Web of Science, Embase, Medline, the Cochrane Library were used to collect and sort out RCT related literature on acupuncture treatment of simple obesity published by various data platforms. The retrieval time was designed from the beginning of database construction to 2021-10-26.
Chinese search words and strategy (肥胖OR超重OR营养过剩) AND (针OR灸OR穴) AND (试验OR研究OR临床). English equivalents: (“Obesity” OR “Overnutrition” OR “Overweight” OR “Fat” OR “Obese”) AND (“Acupuncture” OR “moxibustion” OR “electroacupuncture” OR “needl*” OR “acupoint*”) AND (“random*” OR “RCT” OR “study*” OR “Trial”) Table 1.
Table 1.
PubMed: session results.
| Search number | Query | Results |
|---|---|---|
| #1 | Overnutrition OR Overweight OR Obesity OR Fat OR Obese | 656,743 |
| #2 | Acupuncture OR electroacupuncture OR needl* OR acupoint* OR moxibustion | 206,101 |
| #3 | random* OR RCT OR study* OR Trial | 11,518,096 |
| #4 | #1 AND #2 AND #3 | 1894 |
2.5. Outcome assessment indicators
Main outcome measure: BMI.
Secondary outcome measures: total effective rate, weight, waist circumference (WC), triglyceride (TG), low density lipoprotein (LDL), high density lipoprotein (HDL), cholesterol, total cholesterol (TC).
2.6. Literature screening and data extraction
Two researchers (Yin and Li) independently read the title and abstract, and read the full text of the literature that may meet the criteria to determine whether it really meets the inclusion criteria. In the event of disagreement, it shall be discussed or decided by a third researcher (Zhang and Zhao).
The two researchers conducted independent data extraction for the final included research, including: the author, year, research location, inclusive and exclusive criteria, diagnosis criteria, experimental period, course, age, gender, sample size, intervention, course of treatment, randomized method, allocation concealment, blinding, withdrawal and loss of follow-up, clinical indicators and adverse reaction, etc. Use Microsoft Excel 2019 to make data sheets and record relevant information.
2.7. Quality evaluation
The modified Jadad scale[10] was used to evaluate the quality of the included RCT. The low quality research was 1 to 2 points, and the high quality research was 3 to 5 points. Use the software Review Manager 5.4.1 to evaluate the quality and bias risk of the included literature and draw the bias risk assessment form. Both evaluations were conducted independently by two researchers. In the event of disagreement, it shall be discussed or decided by a third researcher.
2.8. Statistical analysis
Meta-analysis was performed using Review Manager 5.4.1 software. χ2 test was used to test the heterogeneity of the included studies, and the degree of heterogeneity was observed according to I2 value. Significance index I2 50% was set for the quantitative analysis of heterogeneity, where I2 < 50% indicates that the heterogeneity of all included clinical studies is small, the fixed-effects model was used for analysis. Otherwise, the REM (random-effects model) was used for analysis, and the possible reasons for the heterogeneity are discussed. If necessary, a subgroup analysis is performed. At the same time, the statistical analysis quantity of dichotomous data was evaluated using the odd ratio, the estimation of the 95% confidence interval (CI) interval estimation was used as the statistical analysis quantity of continuous data, the test level α = 0.05, and P < .05 indicates a statistical difference between the two groups.[11] The funnel chart was drawn with Stata 17 and the publication bias was detected using Begg’s test.[12] If P > .05, there was no publication bias. On the contrary, there is publication bias exists.
SPSS 25 was used to perform frequency analysis and cluster analysis of the acupuncture points used in the included literature. The cluster analysis used systematic clustering to generate icicle figure, and clustering used the method of average connection between groups to generate pedigree chart.
3. Results
3.1. Retrieval
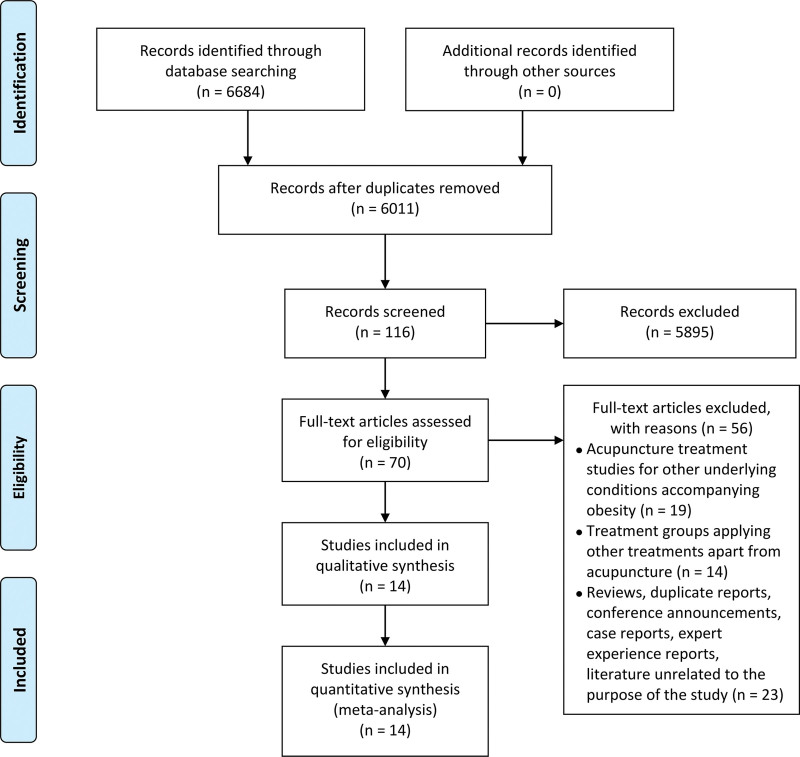
A total of 8864 related literature were retrieved. 8748 articles were excluded after reading the title and abstract in the initial screening, 46 were excluded through preliminary browsing, 56 were excluded according to the inclusion and exclusion criteria in the second screening, and 14 studies were finally included[13–26] (see Table, Supplemental Digital Content, which shows the excluded studies, http://links.lww.com/MD/H689). There are 6 dissertations (2 doctoral dissertations and 4 master dissertations) and 8 journal papers, including 13 literature in Chinese and 1 in English. A total of 1116 patients with simple obesity were included. Literature screening process and results are shown in Figure 1.
Figure 1.
Literature screening flow chart.
3.2. Included research characteristics
(1) Study type: all 14 studies were single-center randomized controlled studies.
(2) Participants: patients from inpatients, outpatients, TCM treatment centers or clinics.
(3) Number of cases: the number of cases in the experimental group and the control group varied from 23 to 143.
(4) Course of treatment: the course of treatment ranges from 1 month to 1 year.
(5) Interventions:
The acupuncture and moxibustion therapies included in this study include body acupuncture, ear acupuncture, ear pressure, intradermal needle(acupoint embedding), pulse current acupuncture, warm acupuncture, moxa moxibustion and other therapies,[8] the types of acupuncture and moxibustion therapy, acupoint selection and needle manipulation are not distinguished; non-acupuncture therapy includes diet control, exercise intervention, weight-loss drug (western medicine) intervention, massage, cupping, scrapping, physical therapy, etc.
Acupuncture and moxibustion were used in all 14 of the experimental groups, and the control groups of 5 studies[13,16,17,21,23] did not have targeted treatment in addition to basic treatment, the control group of 4 studies[14,19,20,25] was primarily treated with drugs, the control group of 2 studies[24,26] was primarily treated with abdominal massage, the control group of 2 studies[18,22] mainly used diet, exercise and other treatments, and the control group of 1 study[15] was treated with comfort needle.
Inclusion and exclusion criteria: 14 studies included inclusion and exclusion criteria
Diagnostic and efficacy evaluation Criteria:
1. Diagnostic criteria adopted mainly in Asia and Australia:
a. Refer to the World Health Organization (WHO) diagnostic criteria for obesity in the Asia-Pacific region, and the Chinese Criteria for Diagnosis and Efficacy Evaluation of Simple Obesity:
(1) Body mass index (BMI): Classified according to adult obesity indicators formulated by WHO in 2000: Pre-obesity: BMI of 22.0 to 24.99 kg/m2; Degree I obesity: BMI of 25.0 to 29.99 kg/ m2; Degree II obesity: BMI ≥ 30 kg/m2. (2) Degree of obesity: (measured body mass − standard body mass)/standard body mass; Standard body weight = [height (CM) − 100] × 0.9. Mild obesity: 20% to 30%; Moderate obesity: 30% to 50%; Severe obesity: >50%. (3) WC: measure the midpoint level of the line between the anterior superior iliac spine and the lower edge of the 12th rib. Male WC ≥85 cm; Female WC ≥80 cm. Simple obesity can be diagnosed if the above three items meet more than two items and exclude secondary obesity, such as thalamic disease, pituitary disease and pancreatic obesity.
b. The standard of obesity for Chinese adults in the Guidelines for The Prevention and Control of Overweight and Obesity in China is: BMI index ≥ 28; WC ≥ 80 cm; Waist to hip ratio ≥ 0.85, those who meet the above two items can be diagnosed as simple obesity.
2. Main diagnostic criteria adopted in Europe:
The diagnostic criteria for obesity of Caucasians formulated with reference to WHO 2000 are as follows: the diagnostic criteria for obesity of Caucasians: BMI (kg/m2) obesity grade: 25 to 29.9 is overweight, >30 is obesity (critical), 30 to 34.9 is 1 degree obesity, 35 to 39.9 is 2 degree obesity, and >40 is 3 degree obesity.
3. Efficacy evaluation Criteria
Six studies[13,14,19,20,22,23] adopted the criteria issued by the World Health Organization (WHO) in 2000, one study[15] adopted the standards formulated in Chinese adult obesity prevention expert consensus, and one study[17] adopted the Diagnostic standards of Obesity and Hyperlipidemia, one study[18] adopted the Criteria formulated in the Guidelines for The Management of Overweight and Obesity in Adults, two studies[16,21,25] adopted the Criteria for the Diagnosis and Efficacy Evaluation of Simple Obesity in 1997, and one study[24] adopted the Chinese Adult Body Mass Index Classification Standard, One study[26] used the Internationally Recognized Obesity Assessment Method (Table 2).
Table 2.
Basic characteristics of included literature.
| Included research | Region | Diagnostic and efficacy evaluation criteria | Gender | Age | Number | Interventions | Basic treatment | Duration of intervention (wk) | Efficacy indicators | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | T | C | T | C | T | C | ||||||
| Chen, 2019 | Guangdong, China | I | 34.43 ± 7.63 | 34.60 ± 5.21 | 28 | 23 | Acupuncture | No treatment | Diet and exercise | 10 | ①②③④ | ||
| Du, 2019 | Guangxi, China | I | 14 | 46 | 40.07 ± 9.04 | 41.1 ± 9.51 | 30 | 30 | Acupuncture | Metformin | Diet and exercise | 13 | ①②③④ |
| Zhang, 2019 | Shanghai, China | II | 33 | 51 | 33.05 ± 6.60 | 36.17 ± 9.71 | 42 | 42 | Acupuncture | Comfort Pins | Diet and exercise | 26 | ①②③④ ⑤⑥⑦⑧ |
| Li, 2019 | New South Wales, Australia | V | 23 | 37 | 35.92 ± 3.36 | 37.84 ± 3.90 | 30 | 30 | Acupuncture | No treatment | Exercise | 6 | ①③④ |
| Chen, 2018 | Guangdong, China | III | 53 | 31 | 36.25 ± 13.68 | 38.85 ± 15.64 | 42 | 42 | Acupuncture | No treatment | Diet and exercise | 52 | ③④⑤⑧ |
| Li, 2018 | Tianjin, China | IV | 27 | 33 | 30.3 ± 0.9 | 32.0 ± 11.6 | 30 | 30 | Acupuncture | Diet control | Diet | 8 | ①②⑤ ⑥⑦⑧ |
| Tang, 2018 | Guangdong, China | I | 28 | 38 | 33.36 ± 9.63 | 34.79 ± 9.67 | 33 | 33 | Acupuncture | Orlistat | Diet and exercise | 8 | ①②③ |
| JENS 2017 | Germany | I | 33 | 27 | 42.27 ± 11.79 | 50.77 ± 10.79 | 30 | 30 | Acupuncture | CM3 drugs | Diet and exercise | 26 | ①②⑤⑥ |
| Huang, 2015 | Perak, Malaysia | V | 11 | 43 | 28.107 ± 10.73 | 28 ± 10.54 | 28 | 26 | Acupuncture | No treatment | Diet and exercise | 13 | ②③④⑤ ⑥⑦⑧⑩ |
| Chen, 2012 | Sichuan, China | I | 46 | 34 | 42.48 ± 4.20 | 41.32 ± 3.74 | 40 | 40 | Acupuncture | Diet and exercise | No treatment | 5 | ①②④ |
| Zhang, 2012 | Sichuan, China | I | 21 | 36 | 27.613 ± 7.854 | 28.486 ± 8.651 | 29 | 28 | Acupuncture | No treatment | Diet | 8 | ①③④ |
| Zeng, 2006 | Guangdong, China | VI | 12 | 38 | 25 | 25 | Acupuncture | Abdominal massage | Diet | 4 | ②⑤⑥⑦⑧ | ||
| Ma, 2006 | Shandong, China | V | 34 | 116 | 33.76 ± 1.30 | 34.01 ± 0.92 | 100 | 50 | Acupuncture | Sibutramine | No treatment | 13 | ②⑤⑥⑨ |
| Yu, 2005 | Shaanxi, China | VII | 12 | 191 | 143 | 60 | Acupuncture | Abdominal massage | Diet and exercise | 8 | ⑤⑥⑦⑧ | ||
I = World Health Organization (WHO) Diagnostic Criteria for Obesity, II = Expert Consensus on the Prevention and Treatment of Obesity in Chinese Adults, III = Diagnostic Criteria for Obesity and Hyperlipidemia, IV = Recommendations on the Boundaries of Overweight and Obesity in Chinese Adults, V = Diagnostic and Efficacy Assessment Criteria for Simple Obesity Diseases, VI = Classification Standards for Body Mass Index of Chinese Adults, VII = The world-recognized method for assessing obesity. ①Total effective rate ②BMI ③Waist circumference ④Weight ⑤TC ⑥TG ⑦HDL-C ⑧LDL-C ⑨Leptin ⑩Insulin sensitivity index (ISI).
Main evaluation indicators
BMI, total effective rate, weight, WC, TC, TG, HDL-C, LDL-C, adverse reactions (Table 2 for details).
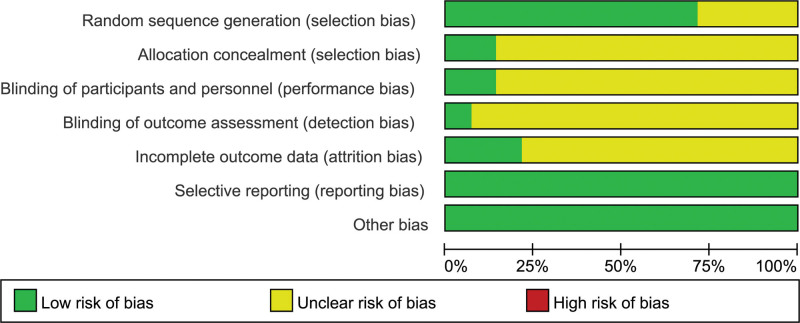
3.3. Methodological quality evaluation of included studies
According to the Jadad literature quality scoring standard, all 14 literature were scored from the aspects of the generation of random sequence, the realization of randomization concealment, the implementation of blind method, the records of withdrawal and loss of follow-up, etc. Three studies[15,21,23] had a Jadad score of 4 to 7, which were high-quality studies. Randomization was used in all studies. Among them, 11 studies[13–23] adopted randomization concealment; only 2 studies[15,21] adopted the blind method; five studies[13–15,21,23] described withdrawal and loss of follow-up (Table 3).
Table 3.
Quality of included literature Jadad rating scale.
| Included research | Generation of random sequences | Randomization hidden | Blind method | Withdrawal and lost visits | Total score |
|---|---|---|---|---|---|
| Su, 2020 | 0 | 1 | 0 | 0 | 1 |
| Chen, 2019 | 1 | 1 | 0 | 1 | 3 |
| Du, 2019 | 1 | 1 | 0 | 1 | 3 |
| Zhang, 2019 | 2 | 2 | 1 | 1 | 6 |
| Li, 2019 | 2 | 1 | 0 | 0 | 3 |
| Chen, 2018 | 1 | 1 | 0 | 0 | 2 |
| Li, 2018 | 1 | 1 | 0 | 0 | 2 |
| Tang, 2018 | 1 | 1 | 0 | 0 | 2 |
| JENS 2017 | 2 | 1 | 0 | 0 | 3 |
| Zhang, 2016 | 1 | 1 | 0 | 0 | 2 |
| Huang, 2015 | 1 | 1 | 1 | 1 | 4 |
| Chen, 2012 | 1 | 1 | 0 | 0 | 2 |
| Zhang, 2012 | 2 | 2 | 0 | 1 | 5 |
| Zeng, 2006 | 1 | 0 | 0 | 0 | 1 |
| Ma, 2006 | 1 | 0 | 0 | 0 | 1 |
| Wu, 2006 | 1 | 0 | 0 | 0 | 1 |
| Yu, 2005 | 1 | 0 | 0 | 0 | 1 |
The 14 studies finally included in our analysis were all RCT trials. Among them, 9 studies[13–20,23] used a random number table to determine the low risk of bias; 1 study[24] determined the low risk of bias by using a random method with no return lottery; 4 studies[21,22,25,26] that described randomization methods were identified as having an unclear risk of bias; 2 studies[15,23] with sealed envelopes for allocation concealment were identified as having a low risk of bias, and the remaining 12 studies that did not describe the concealment of allocation were considered to have an unclear risk; 2 studies[15,21] clearly reported participants with a low risk of perceived bias for blindness (single blindness); other studies that did not mention blinding methods were considered to be at risk of ambiguity; only one study[23] reported blind analysis and evaluation of observation records and was determined as a low risk of bias; the remaining studies that did not mention such measures were considered to be at risk of ambiguity. Five studies[13–15,21,23] reported shedding and loss of follow-up, which were identified as low risk of bias; others did not report these situations and were identified as unclear risks. Reporting bias: All 14 studies reported preset results that were identified as low-risk bias (Figs. 2 and 3).
Figure 2.
Bias risk table for included studies.
Figure 3.
Risk assessment tables for each study included in the study.
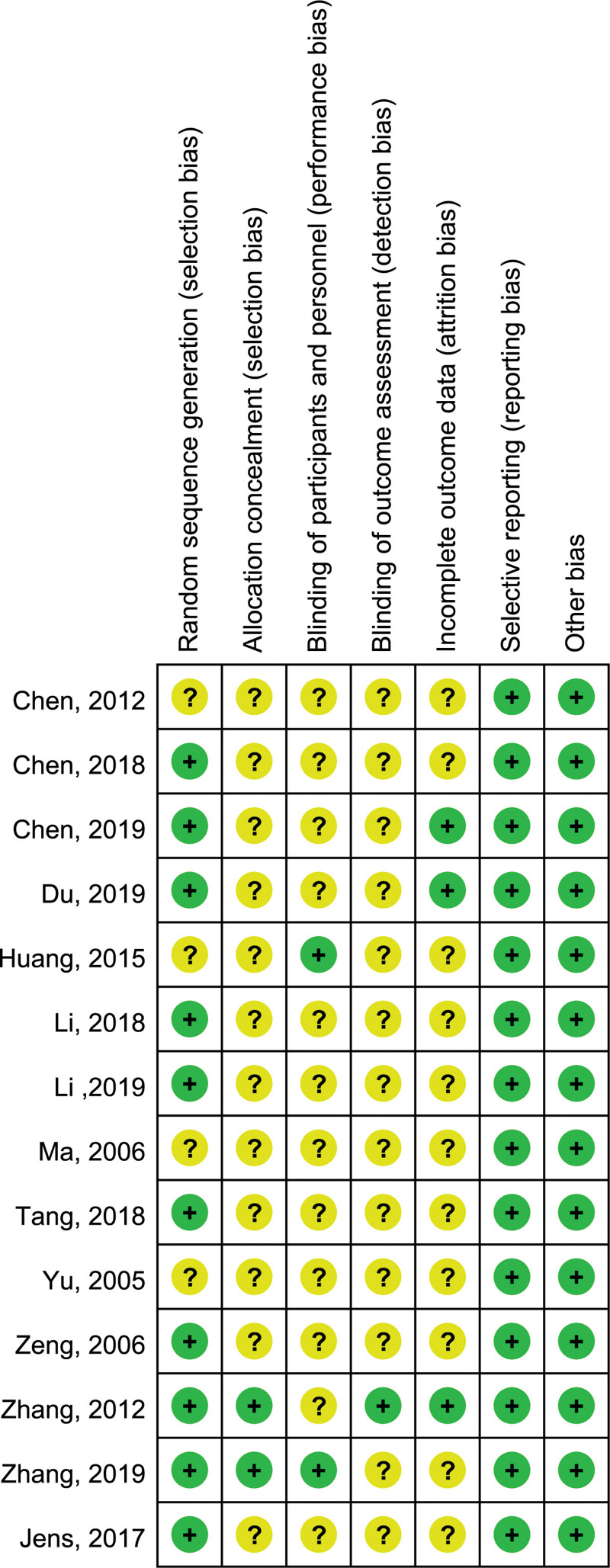
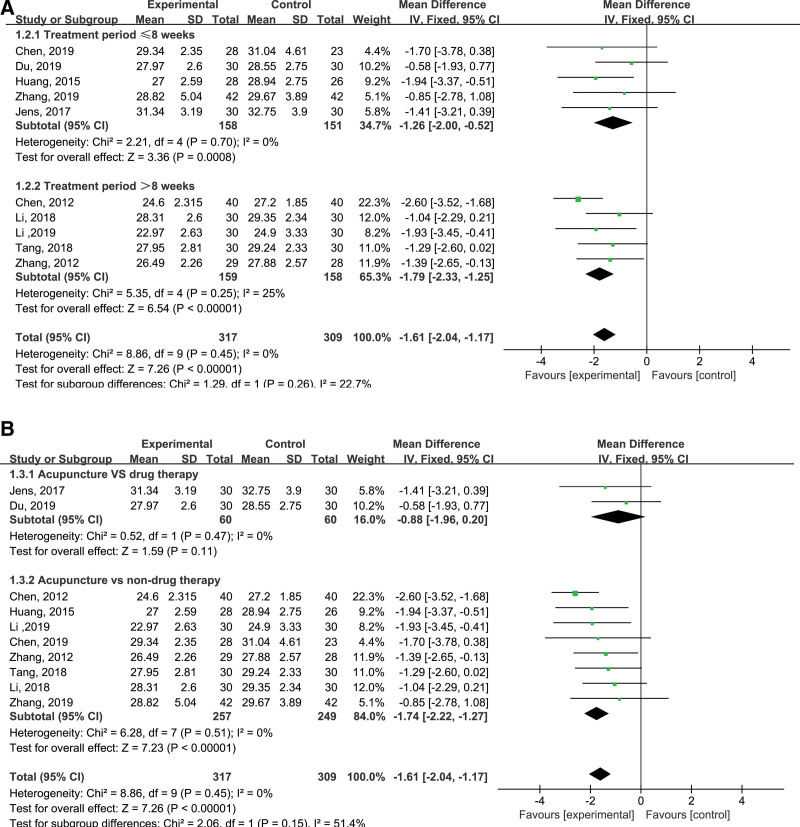
3.4. Meta-analysis of the efficacy of acupuncture therapy in the treatment of simple obesity
3.4.1. Body mass index.
Among the 14 studies, 10[13–16,18–23] reported BMI, and the results of meta-analysis on the efficacy of acupuncture and moxibustion in the treatment of simple obesity are shown in Figure 4. The results of the heterogeneity test showed that the heterogeneity of the included studies was small (I2 = 0%, P = .45), so the fixed-effect model was used for the analysis, and the combined MD value was −1.61, 95%CI was (−2.04, −1.17). There was significant difference between the experimental group and the control group (P < .001), suggesting that acupuncture was more effective than other intervention measures in reducing BMI.
Figure 4.
Forest map of body mass index.
In addition, it can be seen in Figure 4A that the MD value of the 8-week treatment period was −1.26, and that of the treatment period >8 weeks was −1.79, indicating that BMI decreased more obviously with the increase of acupuncture and moxibustion treatment period.
As can be seen from Figure 4B, the MD value of acupuncture and moxibustion therapy VS drug therapy was −0.88, and that of acupuncture and moxibustion therapy versus non-drug therapy was −1.74. There was a moderate degree of heterogeneity between the two subgroups (I2 = 51.4%, P = .15), indicating that there was a certain difference in the effect of healthy lifestyle and drug use on BMI decline.
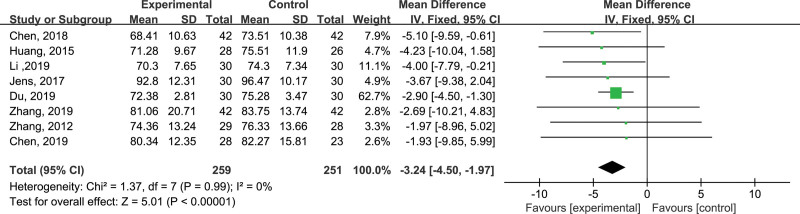
3.4.2. Weight.
Among the 14 studies, 8[13–17,20,21,23] reported body weight. The results of meta-analysis on the efficacy of acupuncture in the treatment of simple obesity were shown in Figure 5. The results of the heterogeneity test results showed that the heterogeneity of the included studies was small (P = .99, I2 = 0%), so the fixed-effect model was used for the analysis. The combined MD value was −3.24, and the 95% CI was (−4.50, −1.97). There was statistical difference between experimental group and control group (P < .001), suggesting that acupuncture and moxibustion therapy is more effective than other interventions in reducing body weight.
Figure 5.
Forest plot of body weight.
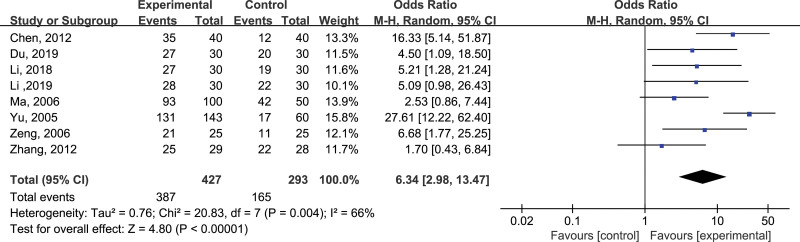
3.4.3. Total effective rate.
Among the 14 studies, 8 papers[14,16,18,22–26] reported the total effective rate. The results of the meta-analysis of the total effective rate of acupuncture and moxibustion in the treatment of simple obesity are shown in Figure 6. The results of the heterogeneity test results showed that the included studies had high heterogeneity (P = .004, I2 = 66%). After analysis, it was found that the most likely source of heterogeneity lies in the large difference between the acupoints described in Yu aoshuang 2005[26] and other 13 literature. This article did not directly elaborate on specific acupuncture points, but replaced them with unfixed meridian points, so the random effect model was used for analysis. The combined odd ratio value was 6.24, 95% CI was (2.98, 13.47). There was a statistical difference between the experimental group and the control group (P < .001), suggesting that the total effective rate of acupuncture and moxibustion therapy in treating simple obesity is higher than other interventions.
Figure 6.
Forest plot of total effective rate.
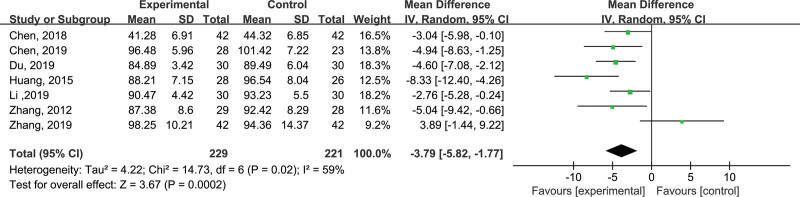
3.4.4. Waist circumference.
Among the 14 studies, 7 studies[13–17,21,23] reported WC. The results of meta-analysis of WC on the efficacy of acupuncture and moxibustion in treating simple obesity are shown in Figure 7. The results of heterogeneity test showed that the included studies had heterogeneity (P = .02, I2 = 59%), using a random effect model for analysis, the combined MD value was −3.79, 95% CI was (−5.82, −1.77), there was a statistical difference between the experimental group and the control group (P < .001), suggesting that acupuncture and moxibustion therapy can reduce WC, and it is more effective than other interventions.
Figure 7.
Waist circumference forest map.
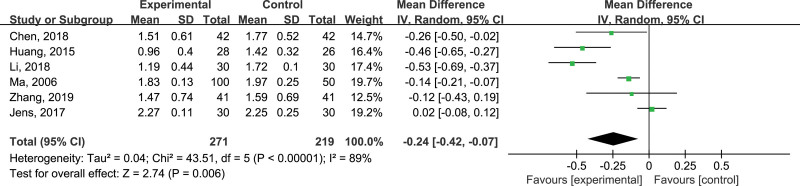
3.4.5. Triglycerides.
Among the 14 studies, 6 studies[15,18,20–22,25] reported TG. The results of meta-analysis of the TG on the efficacy of acupuncture and moxibustion in the treatment of simple obesity are shown in Figure 8. The REM was used for meta-analysis, the results of the heterogeneity test showed that the included studies were highly heterogeneous (P < .001, I2 = 89%), and the source of the heterogeneity was still not identified after analysis. The combined MD value was −0.24, and the 95% CI was (−0.42, −0.07), there was a statistical difference between the experimental group and the control group (P = .006 < .05), suggesting that acupuncture and moxibustion therapy can reduce TG more effectively than non-acupuncture therapy.
Figure 8.
Forest map of triglyceride.
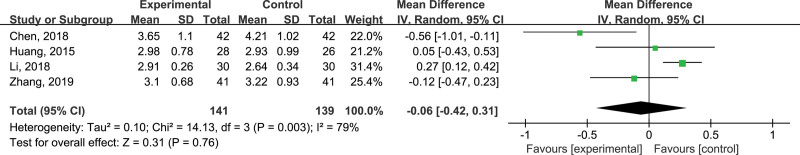
3.4.6. Low-density lipoprotein.
Among the 14 studies, 4 studies[15,17,18,21] reported LDLs, and the results of the LDL meta-analysis on the efficacy of acupuncture and moxibustion therapy in treating simple obesity are shown in Figure 9. The random -effects model was used for analysis. The results of the heterogeneity test showed that the included studies had a high degree of heterogeneity (P = .003, I2 = 79%), and the source of the heterogeneity was still not identified after the analysis. The combined MD value was −0.06, and the 95% CI was (−0.42, 0.31), there was no statistical difference between the experimental group and the control group (P = .76 > .05), suggesting that acupuncture and moxibustion therapy compared to other therapies are equally effective in reducing LDL.
Figure 9.
Forest map of low density lipoprotein.
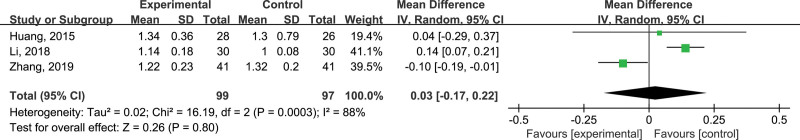
3.4.7. High density lipoprotein.
Among the 14 studies, 3 studies[15,18,21] reported HDL, and the meta-analysis results of HDL on the efficacy of acupuncture and moxibustion in the treatment of simple obesity are shown in Figure 10. The heterogeneity test results show that there is a high degree of heterogeneity (P < .001, I2 = 88%) in the included studies, and the source of heterogeneity has not been identified after analysis. The REM was used for analysis. The combined MD value was 0.03, and the 95% CI was (−0.17, 0.22), there was no statistical difference between the experimental group and the control group (P = .80 > .05), suggesting that acupuncture and moxibustion therapy compared with other therapies may be equally effective in increasing HDL.
Figure 10.
High-density lipoprotein forest map.
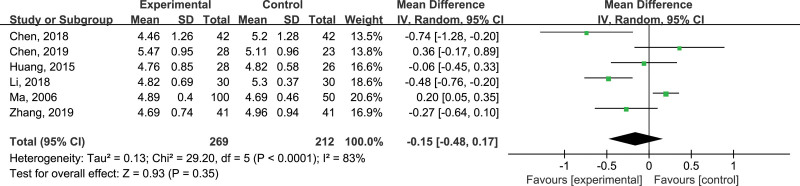
3.4.8. Total cholesterol.
Among the 14 studies, 6 studies[13,15,17,18,21,25] reported TC. Figure 11 shows the results of a meta-analysis of TC in the treatment of simple obesity with acupuncture and moxibustion. There is high heterogeneity in the study (P < .001, I2 = 83%), and the source of heterogeneity has not been determined after the analysis. The random effects model was used for analysis. The combined MD value was −0.15, and the 95% CI was (−0.48, 0.17), there was no statistical difference between the experimental group and the control group (P = .35 > .05), suggesting that acupuncture and moxibustion therapy and other therapies have similar effects in reducing TC.
Figure 11.
Forest map of total cholesterol.
3.4.9. Adverse reactions.
Among the 14 studies, 3 studies[14,15,23] clearly reported adverse reactions such as skin discomfort and subcutaneous hematoma in the treatment group, and the rest did not report adverse reactions.
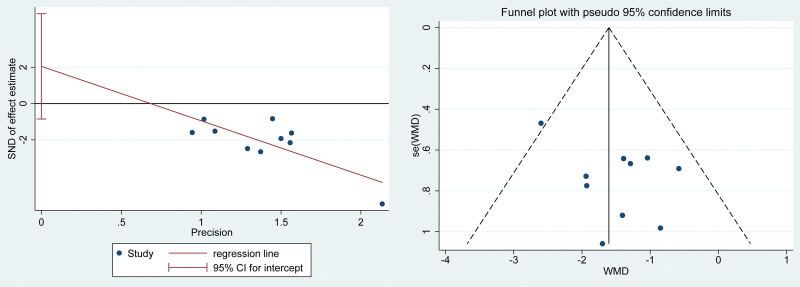
3.5. Analysis of publication bias
Meta-analysis of the effect of acupuncture and moxibustion therapy on the reduction of the BMI of simple obesity, egg test showed P = .142 > .05, according to the results of the egg test, it is not considered that there is publication bias. The funnel plot and egg test are shown in Figure 12.
Figure 12.
Publication bias funnel plot and Egger test plot.
3.6. Analysis of the use of acupuncture and moxibustion points
The frequency of acupoints used in the 14 literature mentioned above was counted and the acupoints with a frequency of 1 were excluded. The main points of the 14 acupuncture prescriptions involved 21 acupoints, and the total frequency of use was 88; the most frequently used acupoint was ST25, Followed by RN12, ST36, ST40, RN6, etc. (see Table 4 for details).
Table 4.
Frequency of the acupoints.
| Acupoints | Frequency | Proportion | Acupoints | Frequency | Proportion |
|---|---|---|---|---|---|
| ST25 | 12 | 13.6 | ST27 | 2 | 2.3 |
| RN12 | 9 | 10.2 | GB26 | 2 | 2.3 |
| ST36 | 7 | 8 | C018 | 2 | 2.3 |
| SP15 | 6 | 6.8 | KI16 | 2 | 2.3 |
| ST40 | 6 | 6.8 | LI11 | 2 | 2.3 |
| RN6 | 6 | 6.8 | RN5 | 2 | 2.3 |
| RN4 | 4 | 4.5 | BL21 | 2 | 2.3 |
| SP6 | 4 | 4.5 | Total | 88 | 100.0 |
| RN9 | 4 | 4.5 | |||
| SP9 | 4 | 4.5 | |||
| SP14 | 3 | 3.4 | |||
| ST24 | 3 | 3.4 | |||
| BL20 | 3 | 3.4 | |||
| ST28 | 3 | 3.4 |
The 21 acupoints are mainly in 6 meridians. Among them, the acupoints of the stomach meridian of Foot Yangming have the highest frequency of use, with a frequency of 30 times, accounting for 35%, and the number of commonly selected acupoints is 5. The second highest frequency is Renmai, the frequency of use is 25, and the number of selected acupoints is 5, accounting for 29%. The proportion is 20%. Table 5 for details.
Table 5.
Statistics of meridians associated with acupoints for simple obesity treated with acupuncture therapy.
| Meridian | Frequency | Proportion | Acupoints | ||||
|---|---|---|---|---|---|---|---|
| ST | 30 | 0.35 | ST27 | ST40 | ST24 | ST25 | ST36 |
| RN | 25 | 0.29 | RN4 | RN6 | RN5 | RN9 | RN12 |
| SP | 20 | 0.23 | SP15 | SP14 | SP6 | ST28 | SP9 |
| BL | 5 | 0.06 | BL20 | BL21 | |||
| LI | 2 | 0.02 | LI11 | ||||
| KI | 2 | 0.02 | KI16 | ||||
| Ear | 2 | 0.02 | Ear acupoints | ||||
Cluster analysis was performed on acupoints with a frequency of more than 4 in 14 literature, and an icicle diagram (Fig. 13) and a pedigree diagram (Fig. 14) were obtained. From Figures 13 and 14, the acupoints can be divided into three clusters: the first category: RN9-SP9-SP6-RN4; the second category: ST40-RN6-SP15-ST36; the third category: ST25-RN12.
Figure 13.
Icicle map of acupoints.
Figure 14.
Genealogy of acupoints.
4. Discussion
In 2019, the number of deaths caused by chronic diseases in China accounted for 88.5% of the total number of deaths, and 80.7% of the deaths from central and cerebrovascular diseases, tumors, and chronic respiratory diseases. Obesity is closely related to these diseases. Obesity is also very harmful to acute infectious diseases, it is an independent risk factor for adverse outcomes (including death) of COVID-19, higher BMI is directly proportional to worse outcomes of COVID-19.[27] Obesity is even a new type of disease.
A large body of scientific evidence shows that body weight is the result of adjustment by the body, while obesity is a disorder of the regulatory system.[28] Some patients cannot achieve the desired effect by simply changing their lifestyle, and usually require drug adjuvant therapy.[29] Drugs for the treatment of obesity are traditionally divided into two categories: appetite suppressants and gastrointestinal lipase Blockers.
Appetite suppressants can be roughly divided into the following categories: First, norepinephrine transporter inhibitors, such as phentermine, are the first sympathomimetic amines approved for short-term weight loss, and it is common that adverse reactions include increased blood pressure, nervousness, headache, dry mouth, etc. Second, serotonin receptor agonists, such as locarcillin, are the second weight loss drugs that can be used for a long time. Its common adverse reactions include: Headache, dizziness, nausea, etc. Third, GABA receptor agonists, such as phentermine topiramate, are the most effective antiobesity drugs among the approved drugs. Its common adverse reactions are paresthesia, dysgeusia, constipation, dry mouth, etc.; fourth, opioid receptor antagonists combined with dopamine and norepinephrine reuptake inhibitors, such as naltrexone/bupropion compound preparation, its common adverse reactions are nausea, constipation, dizziness, mouth Dry, etc.; fifth, glucagon-like peptide-1 receptor agonists, such as liraglutide, its common adverse reactions are nausea, vomiting, diarrhea, pancreatitis, gallbladder disease, etc.
Gastrointestinal lipase resistance antibiotics, such as orlistat, have common adverse reactions such as diarrhea, oily stools, etc.[28,30,31] Some researchers believe that during the 1-year obesity treatment process, compared to the placebo group, the reduction of weight loss drugs as an adjunct to lifestyle intervention can achieve a better weight loss effect. However, for patients whose weight loss does not reach 5% of their original body weight, drug withdrawal can be considered to avoid possible adverse reactions caused by drugs.[32]
Therefore, it is necessary to find a safer and more effective method for the treatment of simple obesity, while the efficient and safety of acupuncture and moxibustion therapy has been already reported in the treatment of obesity.[33] It can reduce energy intake and increase energy consumption by regulating the body’s energy metabolism.[34] It has been clear that abnormal leptin blood-brain transport and defective expression of the leptin receptor gene are important causes of obesity, leptin levels have a benign regulatory effect and can promote the expression of the hypothalamic leptin receptor gene.[35] Studies have also shown that acupuncture can regulate appetite through the hypothalamus, adipose tissue, and gastrointestinal tract, and can activate brown adipose tissue. BAT produces heat to achieve the effect of weight loss.[36]
To form a scientific and reliable basis for clinical guidelines, this study used BMI, total effective rate, body weight, WC, and blood lipids as efficacy evaluation indicators, and a total of 14 literature were included for meta-analysis. BMI is the main indicator of our study, because it is not only objective indicators of overweight and obesity in the general population, but also strong associations to varying degrees with the causes of death from cancer, cardiovascular diseases, respiratory diseases, blood and endocrine diseases, digestive system diseases, musculoskeletal diseases and genitourinary diseases.[37]
In order to guide the acupuncture and moxibustion clinical operation, the acupoints used in the included studies were also analyzed. First, the most frequently used meridians were the ST, RN and PL. “Su Wen Tiao Jing Lun Chapter 62”says: “If there is excess in shape, then abdominal distention and phlegm will be unfavorable. If it is insufficient, the four branches will not be used... If there is excess in shape, then purge its yang meridian. If it is insufficient, replenished its yang meridian.” Excessive shape means obesity, and the spleen controls the meat in Traditional Chinese Medicine Theory, and the spleen is responsible for obesity; purging its yang meridian is the ST, because the ST and PL belong to each other, and the spleen and stomach are external and internal to each other, which is in charge of the digestion and absorption of food, so purging the ST can be used as one of the main principles of obesity treatment.[38,39] The RN is the “sea of Yin Meridians,” which can regulate the Qi of all Yin Meridians in the whole body; the Ren Meridian runs through the chest. On the midline of the abdomen, acupoints on the RN can regulate the Five Zang Organs, activate Qi and Blood, and play an important role in the mechanism of acupuncture for weight loss.[40]
Second, the most frequently used acupoints are ST25, followed by RN12, ST36, ST40, RN6, etc. ST25 is the acupoint of the large intestine meridian of Hand Yangming, which can regulate the intestines, regulate the Qi and strengthen the function of spleen; RN12 is the acupoint of the stomach meridian of Foot Yangming, the meeting point of the Six Fu Organs, which can promote clearing and lowering turbidity, tune up the three burners; ST36 is the combined point of the stomach meridian of Foot Yangming, and the combined point under the stomach, can strengthen the function of spleen and stomach, strengthen the body and eliminate pathogenic factors; ST40 is the collateral point of the stomach meridian of Foot Yangming, the key point for treating phlegm, which can dispel phlegm. Phlegm and dampness, dredging the meridians; RN6 is the original acupoint, which can clear San Jiao, move Qi and disperse stagnation.[15,23]
Third, we studied the clustering relationship between the main acupoints selected for clinical treatment: RN9-SP9-SP6-RN4 has the highest clustering, combining the functions of strengthening function of the Spleen and removing dampness, diuresis and eliminating fat; the second is ST40-RN6-SP15-ST36, which has the effects of regulating qi and stomach, resolving phlegm and removing fat; followed by ST25-RN12, Tongda is used for removing phlegm and accumulation, and strengthening the function of stomach and spleen. Acupuncture and moxibustion have been called green therapy for weight loss, because it has no specific damage to the body.
In addition to these, we should emphasize the prevention and treatment of related complications through weight loss. Thereby improving the patient’s health status is the main goal of obesity treatment, not weight loss itself. A healthy lifestyle should never be ignored: studies have shown[41] that for overweight or obese patients, lifestyle changes are the basis for treatment of obesity, and the diet should be high-quality and the patients can stick to it; In terms of exercise, patients are required to do at least 150 minutes of moderate-intensity exercise per week, and identify frequency, intensity, type, and timing. In addition, self-monitoring in daily life, such as self-weighing, daily steps, high-intensity exercise, and continuous food logging, increases patients’ weight loss success. Weighing three or more times a week, at least 60 minutes of high-intensity exercise every week, and recording the diet for three or more days a week.[42] It can be seen that a healthy lifestyle has an irreplaceable effect on weight loss.
Finally, we want to explain the problems of the included studies. First, among the 14 studies included in this paper, only 3[15,21,23] are high-quality studies, and most of the studies have unclear randomization methods, Second, most studies did not use safety records, only two[13,19] conducted safety-related observations; and most studies were limited to the observation of short-term efficacy, lack of long-term follow-up of patients. There is a lack of relevant evaluation on the long-term efficacy of acupuncture in the treatment of simple obesity. Third, the duration of acupuncture intervention varies, how long does acupuncture intervention achieve the best effect, and when is the bottleneck period of acupuncture treatment? The relationship between efficacy and dose-effect is also worthy of further discussion. Fourth, the diagnosis and efficacy evaluation criteria of simple obesity are not unified, which leads to different definitions of the total clinical efficacy in each literature, which has certain influence on the combined results. Moreover, although there was no a priori protocol at present, our review also provides a detailed analysis of the primary and secondary outcomes of numerous randomized controlled trials, which makes our paper convincing and referential.
In future acupuncture research, strict research design should be carried out, including the application of the gold standard, the realization of randomization concealment, the implementation of the blind method, the recording of withdrawal and loss to follow-up, the treatment of adverse reactions, and the observation of safety, etc. Carry out better quality randomized controlled trials to provide reliable evidence-based evidence for the clinical treatment of simple obesity.
5. Conclusions
Acupuncture and moxibustion therapy is effective in treating simple obesity. However, due to the low score of the included studies, we still expect the results of higher-quality literature to provide higher-level evidence-based basis for clinical decision-making. Furthermore, for the treatment of simple obesity, acupoint analysis revealed that Tianshu (ST25), Zhongwan (RN12), Zusanli (ST36), Fenglong (ST40) and Qihai (RN6) can form the basis for the treatment of simple obesity.
Author contributions
Conceptualization: Yu Yin, Qi Zhao.
Data curation: Yu Yin, Shuying Li, Hao Chen.
Formal analysis: Yu Yin, Hailun Jiang.
Funding acquisition: Qi Zhao.
Investigation: Hailun Jiang, Chunsheng Yin.
Methodology: Yu Yin, Hailun Jiang.
Software: Yu Yin, Hailun Jiang, Hao Chen.
Validation: Yu Yin, Yi Zhang.
Writing – original draft: Yu Yin.
Writing – review & editing: Hailun Jiang, Qi Zhao, Yi Zhang.
Supplementary Material
Abbreviations:
- BMI =
- body mass index
- CI =
- confidence interval
- HDL =
- high density lipoprotein
- LDL =
- low density lipoprotein
- RCT =
- randomized controlled trial
- REM =
- random-effects model
- TC =
- total cholesterol
- TG =
- triglycerides
- WC =
- waist circumference
China’s Key National Research and Development Program (nos. 2018YFC1704102 and 2019YFC0840709) and Tianjin Science and Technology Project (no. 18PTLCSY00060).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Supplemental Digital Content is available for this article.
How to cite this article: Yin Y, Zhao Q, Li S, Jiang H, Yin C, Chen H, Zhang Y. Efficacy of acupuncture and moxibustion therapy for simple obesity in adults: A meta-analysis of randomized controlled trials. Medicine 2022;101:43(e31148).
Contributor Information
Yu Yin, Email: 1960590509@qq.com.
Shuying Li, Email: 2790235985@qq.com.
Hailun Jiang, Email: jhl1996@qq.com.
Chunsheng Yin, Email: 1960590509@qq.com.
Hao Chen, Email: how7302@163.com.
Yi Zhang, Email: zhangyi790707@163.com.
References
- [1].Wei BH, Jia BP. Standard for the diagnosis and curative effect evaluation of simple obesity. Chin J Int Trad Western Med. 1998;317–9. (article in Chinese) [Google Scholar]
- [2].Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98. [DOI] [PubMed] [Google Scholar]
- [3].Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–38. [DOI] [PubMed] [Google Scholar]
- [4].Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9:373–92. [DOI] [PubMed] [Google Scholar]
- [5].Gao Y, Wang Y, Zhou J, Hu Z, Shi Y. Effectiveness of electroacupuncture for simple obesity: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2020;2020:2367610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Nimptsch K, Konigorski S, Pischon T. Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism. 2019;92:61–70. [DOI] [PubMed] [Google Scholar]
- [7].Jin YT, Chen X, Zhuo Y, et al. Clinical research progress of external TCM treatment for simple obesity of spleen deficiency and dampness stagnation. J Clin Acup Moxib. 2018;34:79–83. (article in Chinese) [Google Scholar]
- [8].State Bureau of Technical Supervision. People’s Republic of China National Standard TCM Clinical Diagnosis and Treatment Terminology: Treatment Method Part. China Standards Press. 1997. (article in Chinese) [Google Scholar]
- [9].Fan XL, Yu ML, Fu SP, Zhuang Y, Lu SF. Effectiveness of acupuncture in treatment of simple obesity in animal models: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2019;2019:5459326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. [DOI] [PubMed] [Google Scholar]
- [11].Chen LS, Li YY, Chen H, Liu BW, Wang DW, Zhao YH. Polyglycolic acid sutures embedded in abdominal acupoints for treatment of simple obesity in adults: a randomized control trial. Chin Med. 2019;14:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Du HZ. Clinical observation on the treatment of simple obesity by conditioning the three-point acupoint embedding Chinese. Guangxi University of Traditional Chinese Medicine, Nanning, China. [Thesis] 2019. (article in Chinese) [Google Scholar]
- [13].Zhang KP. Clinical study of acupoints catgut embedding for simple obesity. Shanghai University of Traditional Chinese Medicine, Shanghai, China. [Thesis]. 2019. (article in Chinese) [Google Scholar]
- [14].Li ZX, Xu NG, Zhang HH, et al. Effect of acupuncture combined with kinesitherapy in treatment of simple obesity. Chin Gen Pract. 2019;22:161–3. (article in Chinese) [Google Scholar]
- [15].Chen XY, Mo SJ, Hu ZH. Treating obesity syndrome based on the TCM prevention of disease theory. Clin J Chin Med. 2018;10:106–8. (article in Chinese) [Google Scholar]
- [16].Li WZ, Jiang W, Liu J. Treatment of simple obesity patients with phlegm dampness stagnation syndrome with warming needle moxibustion. Acup Res. 2018;43:522–5. (article in Chinese) [DOI] [PubMed] [Google Scholar]
- [17].Tang FH. The clinical study of acupuncture combined with fine moxibustion for the treatment of obesity with spleen deficiency and obesity. Guangzhou University of Traditional Chinese Medicine, Guangzhou, China. [Thesis] 2018. (article in Chinese) [Google Scholar]
- [18].Mittelbach J. Clinical study of acupuncture treatment of obesity with CM3. Shandong University of Traditional Chinese Medicine. [Thesis] 2017. (article in Chinese) [Google Scholar]
- [19].Huang FL. Clinical study on the treatment of simple obesity with eight acupoints around the navel, Acupuncture and massage College. Nanjing University of Chinese Medicine, Nanjing, China. [Thesis] 2015. (article in Chinese) [Google Scholar]
- [20].Chen Y, Zhou J, Tang B. Efficacy of electroacupuncture in patients with simple obesity and the effect of serum Chemerin. Jiangsu J Trad Chin Med. 2012;44:50–2. (article in Chinese) [Google Scholar]
- [21].Zhang JS. Clinical observation of acupoints catgut embedding combined with dietary guidance and aerobic exercise in the treatment of simple obesity. Chengdu University of Traditional Chinese Medicine, Chengdu, China. [Thesis] 2012. (article in Chinese) [Google Scholar]
- [22].Zeng HW, Nie B. The clinical observation on electric acupuncture catgut implantation at acupoints and auricular point sticking for treatment of simple obesity. J Clin Acup Moxib. 2006;22:13–4. (article in Chinese) [Google Scholar]
- [23].Ma QJ, Bi XY, Ma JH. Clinical study on 100 cases of simple obesity treated by acupuncture. Shandong J Trad Chin Med. 2006:464–5. (article in Chinese) [Google Scholar]
- [24].Yu AS, Yang JS, Wei LX, Xie YY. Observation on therapeutic effect of simple obesity treated with acupuncture, auricular point sticking and TDP. Chin Acup Moxib. 2005:80–2. (article in Chinese) [PubMed] [Google Scholar]
- [25].Guidelines for medical nutrition treatment of overweight/obesity in China (2021). Chin J Front Med Sci. 2021;13:1–55. (article in Chinese) [Google Scholar]
- [26].Bessesen DH, Van Gaal LF. Progress and challenges in anti-obesity pharmacotherapy. Lancet Diabetes Endocrinol. 2018;6:237–48. [DOI] [PubMed] [Google Scholar]
- [27].Cui JY, Xie XH. The development of pharmacotherapy for obesity. Chin J New Drugs. 2016;25:163–9. (article in Chinese) [Google Scholar]
- [28].Jiang L, Tang XL, Guan CH, Fu SB. Advances in drug therapy for obesity. Chin J Clin Pharmacol. 2021;37:1923–7. (article in Chinese) [Google Scholar]
- [29].Kushner RF. Weight loss strategies for treatment of obesity: lifestyle management and pharmacotherapy. Prog Cardiovasc Dis. 2018;61:246–52. [DOI] [PubMed] [Google Scholar]
- [30].Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311:74–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Firouzjaei A, Li GC, Wang N, Liu WX, Zhu BM. Comparative evaluation of the therapeutic effect of metformin monotherapy with metformin and acupuncture combined therapy on weight loss and insulin sensitivity in diabetic patients. Nutr Diabetes. 2016;6:e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Liang F, Koya D. Acupuncture: is it effective for treatment of insulin resistance? Diabetes Obes Metab. 2010;12:555–69. [DOI] [PubMed] [Google Scholar]
- [33].Shen Q, Wang GD. Acupuncture weight loss mechanism of simple obesity. Chin J Rehabil Med. 2005:638–40. (article in Chinese) [Google Scholar]
- [34].Du HY, Zhang YB. The effect and molecular mechanism of acupuncture in the treatment of obesity. Shanghai J Acup Moxib. 2013;32:691–4. (article in Chinese) [Google Scholar]
- [35].Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 192 million participants. Lancet. 2016;387:1377–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Hyunjoo, Li XZ. The application law research of the stomach meridian of foot-yangming and its acupoints according to the modern literature. Shandong University of Traditional Chinese Medicine, Jinan, China. [Thesis] 2017. (article in Chinese) [Google Scholar]
- [37].Bai QJ. The evaluate the clinical efficacy of curing the abdomen type of the simple obesity is treated with the elongated needle along the stomach meridian of foot Yangming penetrating acupuncture. Chengdu University of Traditional Chinese Medicine, Chengdu, China. [Thesis] 2012. (article in Chinese) [Google Scholar]
- [38].Rong S. Analysis of the selection of obesity by acupuncture and moxibustion based on data mining technology. Changchun University of Traditional Chinese Medicine, Changchun, China. [Thesis] 2017. (article in Chinese) [Google Scholar]
- [39].Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387:1947–56. [DOI] [PubMed] [Google Scholar]
- [40].Painter SL, Ahmed R, Hill JO, et al. What matters in weight loss? An in-depth analysis of self-monitoring. J Med Internet Res. 2017;19:e160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.