Abstract
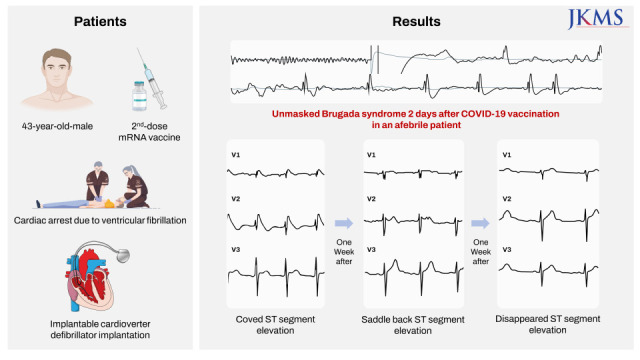
A 43-year-old man presented with cardiac arrest 2 days after the second coronavirus disease 2019 (COVID-19) vaccination with an mRNA vaccine. Electrocardiograms showed ventricular fibrillation and type 1 Brugada pattern ST segment elevation. The patient reported having no symptoms, including febrile sensation. There were no known underlying cardiac diseases to explain such electrocardiographic abnormalities. ST segment elevation completely disappeared in two weeks. Although there were no genetic mutations or personal or family history typical of Brugada syndrome, flecainide administration induced type 1 Brugada pattern ST segment elevation. This case suggests that COVID-19 vaccination may induce cardiac ion channel dysfunction and cause life threatening ventricular arrhythmias in specific patients with Brugada syndrome.
Keywords: Brugada Syndrome, Ventricular Fibrillation, COVID-19 Vaccines
Graphical Abstract
INTRODUCTION
Arrhythmogenic complications of coronavirus disease 2019 (COVID-19) infection are being increasingly reported in the pandemic era. Direct viral invasion, myocardial inflammation, cytokine storm, autonomic dysfunction, and ion channel dysfunction have been suggested as the causes of COVID-19 infection-related cardiac arrhythmias.1,2 Cases of COVID-19 vaccination-induced cardiac arrhythmia have also been reported.2 Although the exact pathophysiologic mechanisms responsible for COVID-19 vaccination-induced cardiac arrhythmias are remain unknown, immunologic reactions may play a key role to produce or enhance arrhythmogenicity as with those in COVID-19 viral infection. Several case studies have reported that COVID-19 infection or vaccination can transiently induce type 1 Brugada pattern ST segment elevation with or without fever.3,4,5 There has been a concern that uncontrolled fever after COVID-19 infection or vaccination may induce life-threatening ventricular arrhythmias in patients with Brugada syndrome.2,6 However, it was not clear whether COVID-19 vaccination can actually induce cardiac arrest in those patients. The authors report a case of Brugada syndrome with documented ventricular fibrillation which occurred 2 days after COVID-19 vaccination.
CASE DESCRIPTION
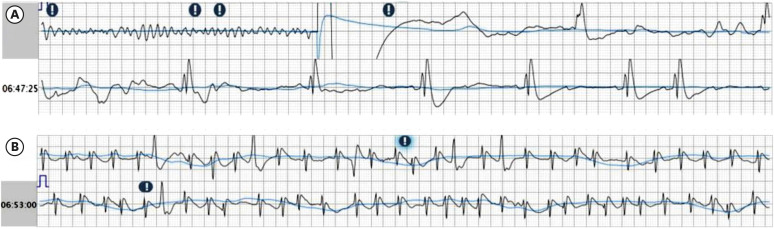
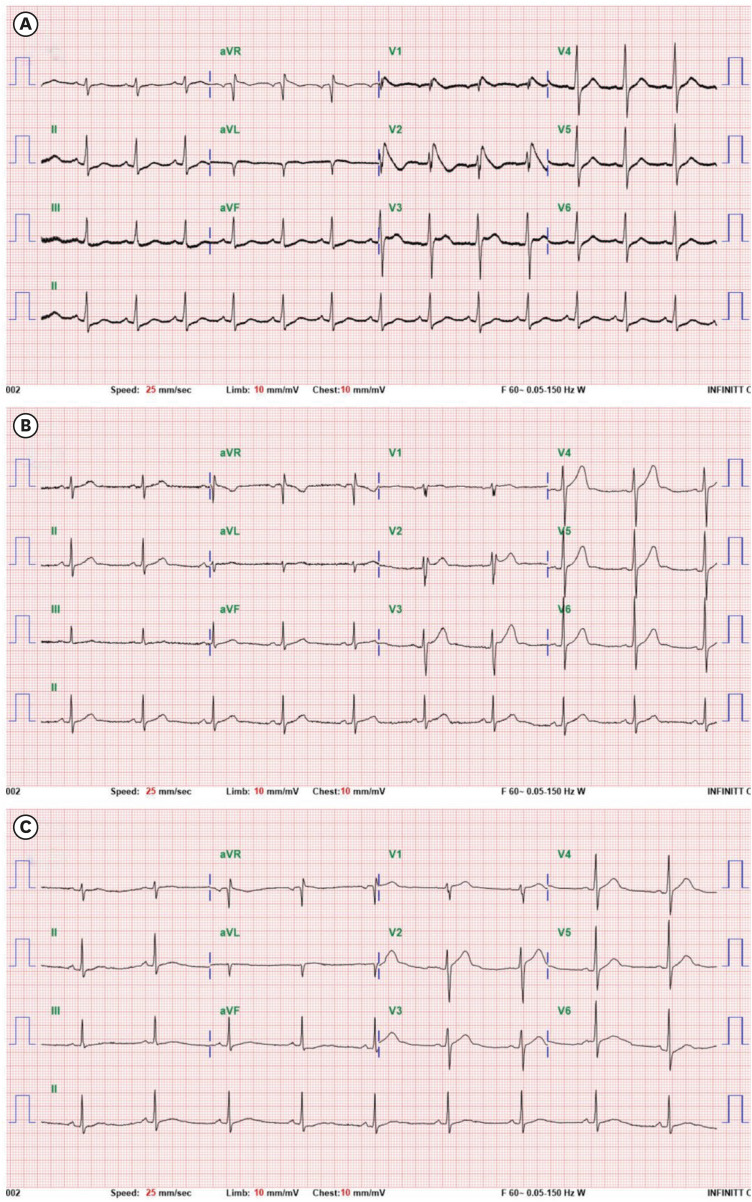
A 43-year-old man presented with out-of-hospital cardiac arrest 2 days after receiving a second COVID-19 vaccination (Comirnaty™ Injection, Pfizer-BioNTech), collapsing suddenly while having breakfast early in the morning (AM 6:30). Initial electrocardiogram (ECG) recorded by the automated external defibrillator showed ventricular fibrillation (Fig. 1A) and coved-type ST segment elevation after the return of sinus rhythm (Fig. 1B). Standard 12-lead ECG also showed coved-type ST segment elevations compatible with type 1 Brugada pattern electrocardiographic abnormalities (Fig. 2A). The patient’s body temperature upon arrival at the emergency department was 36.4ºC. Sodium, potassium, and magnesium concentrations were 137 mmol/L (reference range, 136–146 mmol/L), 3.5 mmol/L (reference range, 3.5–5.1 mmol/L), and 2.7 mg/dL (reference range, 1.8–2.6 mg/dL). Cardiac troponin-I and NT-proBNP concentrations were 0.0024 ng/mL (reference range, 0–0.0342 ng/mL) and 88.8 pg/mL (reference range, < 85.8 pg/mL). Highly sensitive C-reactive protein concentrations were 1.21 mg/dL (range 0–0.5 mg/dL). There were no structural abnormalities observed on echocardiographic examinations. Diagnostic coronary angiography with ergonovine provocation test showed normal coronary arteries.
Fig. 1. Electrocardiogram recorded by the automated external defibrillator. (A) Initially-recorded rhythm showed ventricular fibrillation which was terminated by defibrillator shock therapy. (B) Rhythm strip acquired 5 minutes after the return of sinus rhythm showed coved-type ST segment elevation.
Fig. 2. Serial ST segment changes recorded by the standard 12-lead ECGs. (A) ECG acquired 2 hours after the cardiac arrest at the emergency department showed coved-type (type 1 Brugada pattern) ST segment elevations in the V1–V2 precordial leads. (B) ECG acquired 8 days after the cardiac arrest showed saddleback-type (type 2 Brugada pattern) ST segment elevations. (C) ECG acquired 14 days after the cardiac arrest showed complete disappearance of ST segment elevations.
ECG = electrocardiogram.
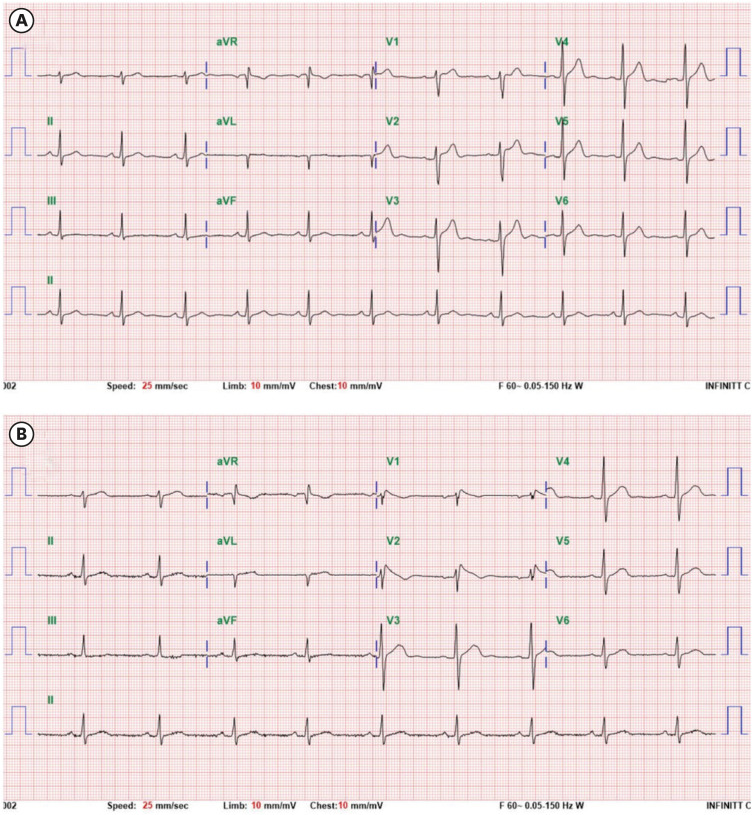
After the recovery of consciousness, the patient reported having no symptoms including febrile sensation between the second COVID-19 vaccination and the cardiac arrest event. The patient also reported taking no medications or having any comorbid diseases. Although the patient had an 8-year-history of alcohol drinking, he had allegedly not consumed any alcohol for over one week before the second vaccination. There was no personal or family history of sudden arrhythmic death or unexplained syncope. Type 1 or 2 Brugada pattern ST segment elevations were not observed in his father or two younger brothers. There was no fever or recurrent ventricular fibrillation during the admission period. ST segment elevations of coved-type changed to saddle back-type one week after the cardiac arrest event (Fig. 2B). ST segment elevations disappeared completely 2 weeks after the cardiac arrest event (Fig. 2C). Despite typical electrocardiographic manifestations, gene studies using a cardiac arrhythmia next generation sequencing multi-gene panel did not reveal any pathogenic mutations in the SCN5A gene. The patient underwent an implantable cardioverter-defibrillator implantation and was discharged without neurologic sequalae. Six months after discharge, oral flecainide provocation test was performed to more clearly differentiate Brugada syndrome from Brugada phenocopy (Fig. 3). One hour after administration of oral flecainide 400 mg, type1 Brugada pattern ST segment elevation appeared on ECG, supporting the diagnosis of congenital Brugada syndrome according to the algorithmic approach proposed by Obeyesekere et al.7
Fig. 3. Serial ST segment changes recorded by the standard 12-lead ECGs using Brugada leads. (A) ECG acquired at baseline showed no significant ST segment elevation. (B) ECG acquired 1 hours after oral flecainide 400 mg single dose administration showed appearance of coved-type (type 1 Brugada pattern) ST segment elevations in the V1–V2 Brugada leads, which were located in the third intercostal space.
ECG = electrocardiogram.
Ethics statement
The case study’s purpose and methods were reviewed and publication was approved by the Institutional Review Board of Dong-A University Hospital (Approval No. DAUHIRB-22-001). Written informed consent for publication of the clinical findings including images was obtained from the patient.
DISCUSSION
Several studies have reported on the incidence of out-of-hospital cardiac arrest increased during the COVID-19 pandemic.8 Other studies have reported that various cardiac arrhythmias complicate COVID-19 vaccination, although the incidence of cardiac arrest is very low.9 Myocardial inflammation, cytokine storm, autonomic dysfunction, and ion channel dysfunction appear to be associated with the occurrence of COVID-19 vaccination-induced cardiac arrhythmias,1,9,10 however, the exact pathophysiologic mechanisms responsible remain unknown. It is well known that patients with Brugada syndrome are susceptible to fever, which can exacerbate sodium channel dysfunction thereby enhancing arrhythmogenicity.11 However, there is limited clinical evidence showing that COVID-19 vaccination itself may cause transient dysfunction in myocardial ion channels. A case study reported that COVID-19 vaccination induced transient Brugada type 1 ST segment elevations and premature ventricular extrasystoles without fever in an asymptomatic individual.4 Another case study reported that COVID-19 vaccination induced ventricular fibrillation storm in a patient with congenital long QT syndrome although the fever status was not described.12
In this case, a middle-aged man suddenly collapsed due to ventricular fibrillation early in the morning and type 1 Brugada pattern ST segment elevation was documented, as with typical manifestations of congenital Brugada syndrome. Although the patient did not have a prior or family history of sudden arrhythmic death, unexplained syncope or SCN5A gene mutations, flecainide provocation test revealed type 1 Brugada pattern ST segment elevation compatible with a diagnosis of congenital Brugada syndrome.7 Because there were no other conditions or diseases which could explain the appearance of type 1 Brugada pattern ECG abnormalities during cardiac arrest and flecainide provocation test, after exclusion of Brugada phenocopy,13 we could presume a diagnosis of congenital Brugada syndrome unmasked by COVID-19 vaccination. These findings may suggest that COVID-19 vaccination itself causes transient cardiac ion channel dysfunction even without fever, and this effect is sufficient to cause life-threatening ventricular arrhythmias in specific patients with Brugada syndrome. There were no provocation studies to directly demonstrate that COVID-19 vaccination itself induces ion channel dysfunctions. Because serial ECGs after the first or second vaccination were not obtained, it is still uncertain whether COVID-19 vaccination directly induced ion channel dysfunction to cause ventricular fibrillation. We postulation that COVID-19 vaccination can induce potent ion channel dysfunction and ventricular arrhythmia, which can be proven only when type 1 Brugada pattern ST segment elevation reappears or fetal ventricular arrhythmia recurs after subsequent COVID-19 vaccination or COVID-19 infection.
The reason why cardiac arrest occurred following the second vaccination may be explained by an enhanced immunologic response following booster vaccination.14,15 Prior studies reported that the incidence of cardiac arrhythmias complicating COVID-19 vaccination with an mRNA vaccine peaks within one month after the second vaccination,2 which supports the role of the immunologic response in arrhythmogenicity.
We presented a case of sudden cardiac arrest induced after COVID-19 vaccinations in an afebrile patient with unmasked Brugada syndrome. More studies are necessary to prove exact pathophysiological mechanisms responsible for COVID-19 vaccination-induced cardiac arrhythmia.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Park JS.
- Data curation: Park JS, Lim KH.
- Formal analysis: Park JS, Lim KH.
- Funding acquisition: Park JS.
- Investigation: Park JS, Lim KH.
- Methodology: Park JS, Lim KH.
- Software: Park JS, Lim KH.
- Validation: Park JS, Lim KH.
- Visualization: Park JS, Lim KH.
- Writing - original draft: Park JS, Lim KH.
- Writing - review & editing: Park JS, Lim KH.
References
- 1.Saha SA, Russo AM, Chung MK, Deering TF, Lakkireddy D, Gopinathannair R. COVID-19 and cardiac arrhythmias: a contemporary review. Curr Treat Options Cardiovasc Med. 2022;24(6):87–107. doi: 10.1007/s11936-022-00964-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022;28(2):410–422. doi: 10.1038/s41591-021-01630-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang D, Saleh M, Garcia-Bengo Y, Choi E, Epstein L, Willner J. COVID-19 Infection unmasking Brugada syndrome. HeartRhythm Case Rep. 2020;6(5):237–240. doi: 10.1016/j.hrcr.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okawa K, Kan T. Unmasked type 1 Brugada ECG pattern without a fever after a COVID-19 vaccination. HeartRhythm Case Rep. 2022;8(4):267–269. doi: 10.1016/j.hrcr.2022.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adedeji OM, Falk Z, Tracy CM, Batarseh A. Brugada pattern in an afebrile patient with acute COVID-19. BMJ Case Rep. 2021;14(7):e242632. doi: 10.1136/bcr-2021-242632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sorgente A, Capulzini L, Brugada P. The known into the unknown: Brugada syndrome and COVID-19. JACC Case Rep. 2020;2(9):1250–1251. doi: 10.1016/j.jaccas.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Obeyesekere MN, Klein GJ, Modi S, Leong-Sit P, Gula LJ, Yee R, et al. How to perform and interpret provocative testing for the diagnosis of Brugada syndrome, long-QT syndrome, and catecholaminergic polymorphic ventricular tachycardia. Circ Arrhythm Electrophysiol. 2011;4(6):958–964. doi: 10.1161/CIRCEP.111.965947. [DOI] [PubMed] [Google Scholar]
- 8.Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5(8):e437–e443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fazlollahi A, Zahmatyar M, Noori M, Nejadghaderi SA, Sullman MJ, Shekarriz-Foumani R, et al. Cardiac complications following mRNA COVID-19 vaccines: a systematic review of case reports and case series. Rev Med Virol. 2022;32(4):e2318. doi: 10.1002/rmv.2318. [DOI] [PubMed] [Google Scholar]
- 10.Choi S, Lee S, Seo JW, Kim MJ, Jeon YH, Park JH, et al. Myocarditis-induced sudden death after BNT162b2 mRNA COVID-19 vaccination in Korea: case report focusing on histopathological findings. J Korean Med Sci. 2021;36(40):e286. doi: 10.3346/jkms.2021.36.e286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Battrawy I, Lang S, Zhao Z, Akin I, Yücel G, Meister S, et al. Hyperthermia influences the effects of sodium channel blocking drugs in human-induced pluripotent stem cell-derived cardiomyocytes. PLoS One. 2016;11(11):e0166143. doi: 10.1371/journal.pone.0166143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Slater NR, Murphy KR, Sikkel MB. VT storm in long QT resulting from COVID-19 vaccine allergy treated with epinephrine. Eur Heart J. 2022;43(11):1176. doi: 10.1093/eurheartj/ehab748. [DOI] [PubMed] [Google Scholar]
- 13.Baranchuk A, Nguyen T, Ryu MH, Femenía F, Zareba W, Wilde AA, et al. Brugada phenocopy: new terminology and proposed classification. Ann Noninvasive Electrocardiol. 2012;17(4):299–314. doi: 10.1111/j.1542-474X.2012.00525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mulligan MJ, Lyke KE, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature. 2020;586(7830):589–593. doi: 10.1038/s41586-020-2639-4. [DOI] [PubMed] [Google Scholar]
- 15.Kim IC, Kim H, Lee HJ, Kim JY, Kim JY. Cardiac imaging of acute myocarditis following COVID-19 mRNA vaccination. J Korean Med Sci. 2021;36(32):e229. doi: 10.3346/jkms.2021.36.e229. [DOI] [PMC free article] [PubMed] [Google Scholar]