Dear Editor,
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic is not over yet. It continues to cause concern worldwide with its emerging new variants. The immunopathogenesis mechanism and relationship with the disease severity in individuals are still not clearly understood. Coronavirus disease 2019 (COVID-19) severity is thought to depend on the host, virus, and environmental factors. Therefore, evidence that will enable us to detect new biomarkers to target COVID-19 severity may be more helpful in this battle. It is known that gut microbiota is associated with disease severity in SARS-CoV-2-positive patients.1 Faecalibacterium prausnitzii is an important bacterium with anti-inflammatory properties capable of producing short-chain fatty acids (SCFAs), such as butyrate, and is considered a new probiotic in the gut microbiota.2
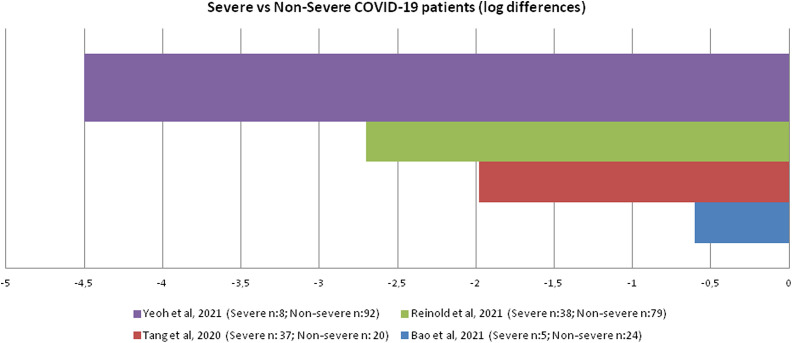
When searched Pubmed and Pubmed Central on January 25, 2022, with the keywords “Faecalibacterium” and “COVID-19,” 480 articles were found, but only 4 of them investigated F. prausnitzii amounts in the gut microbiota between severe and non-severe COVID-19 patients. In these 4 articles, 215 non-severe and 88 severe (severe/critical) COVID-19 patients were analyzed for F. prausnitzii amounts in the gut microbiota.1,3-5 Regardless of age differences, F. prausnitzii was reported to have decreased in the gut microbiota of severe COVID-19 patients compared to non-severe COVID-19 patients.1,3-5 Figure 1 shows a comparison of F. prausnitzii in the gut microbiota reported in severe COVID-19 patients with those in non-severe COVID-19 patients. Reinold et al3 reported that proinflammatory cytokines such as interleukin-6 were high and the anti-inflammatory response was suppressed in severe COVID-19 patients compared to non-severe COVID-19 patients. This was correlated with a decrease in F. prausnitzii amounts in the gut microbiota. The “lung–gut axis” indicates bidirectional communication, and it appears that SCFAs-producing bacteria in the gut microbiota play an important role in the inflammatory response in the lungs. We obtained data supporting the lung–gut axis effect of F. prausnitzii in the gut microbiota of children with asthma2
Figure 1.
Comparison of Faecalibacterium prausnitzii in the gut microbiota reported in severe COVID-19 patients with those in non-severe COVID-19 patients. COVID-19, coronavirus disease 2019.
To conclude, F. prausnitzii might be declining in the gut microbiota of severe and critical COVID-19 patients. The monitoring of the F. prausnitzii amount in the gut microbiota using the quantitative polymerase chain reaction method can be evaluated to follow-up disease severity. In addition, the follow-up of this bacterium in donor stools and the standardized use of this bacterium in fecal microbiota transplantation could be considered in the treatment of severe and critical COVID-19 patients. On the other hand, due to both limited studies and difficulties in comparing results, definite conclusions cannot be drawn. The decline of F. prausnitzii abundance in the gut microbiota may be innocent. Prospective follow-up is required. In addition, some clinical trials investigating the safety of F. prausnitzii in case of therapeutic use are ongoing; it should be approached carefully until its safety is confirmed.
Footnotes
Peer-review: Externally peer-reviewed.
Declaration of Interests: The author declare that he has no competing interest.
References
- 1. . Yeoh YK, Zuo T, Lui GC.et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut. 2021;70(4):698 706. 10.1136/gutjnl-2020-323020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. . Demirci M, Tokman HB, Uysal HK.et al. Reduced Akkermansia muciniphila and Faecalibacterium prausnitzii levels in the gut microbiota of children with allergic asthma. Allergol Immunopathol (Madr). 2019;47(4):365 371. 10.1016/j.aller.2018.12.009) [DOI] [PubMed] [Google Scholar]
- 3. . Reinold J, Farahpour F, Fehring C.et al. A pro-inflammatory gut microbiome characterizes SARS-CoV-2 infected patients and a reduction in the connectivity of an anti-inflammatory bacterial network associates With severe COVID-19. Front Cell Infect Microbiol. 2021;11:747816. 10.3389/fcimb.2021.747816) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. . Bao L, Zhang C, Lyu J.et al. Beware of pharyngeal Fusobacterium nucleatum in COVID-19. BMC Microbiol. 2021;21(1):277. 10.1186/s12866-021-02336-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. . Tang L, Gu S, Gong Y.et al. Clinical significance of the correlation between changes in the major intestinal bacteria species and COVID-19 severity. Engineering (Beijing). 2020;6(10):1178 1184. 10.1016/j.eng.2020.05.013) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a