Abstract
Significance
Using mHealth apps alone at home without the support of healthcare experts could mean that older adults might not fully utilize the functions of the apps, recognize their benefits, and sustain their use. Incorporating an integrated health-social partnership model to support the app usage when further help is needed by the older adults might maximize the apps' benefits in the long term.
Objectives
This study aimed to examine the benefits of adding nursing interaction supported by a health-social partnership model in the use of mHealth, and the sustained beneficial effects on psychological outcomes, including quality of life, self-efficacy, and depression, among older adults after the completion of the program.
Methods
A three-arm, randomized controlled trial design was adopted. Community-dwelling older adults with chronic pain, hypertension, or diabetes, were randomly assigned to either the mHealth, mHealth with interactivity, or control group. Subjects in both the mHealth and the mHealth with interactivity groups received the mHealth application. In addition, the mHealth with interactivity group received support from a nurse case manager, who was supported by a health-social partnership team. mHealth apps and services from a nurse case manager were not provided to the control group. The primary outcome measure was quality of life, and secondary outcomes were self-efficacy and depression. Data were collected at pre-intervention (T1), post-intervention (T2), and at 3 months post-intervention to measure the sustained effect of the program.
Results
There were 74 mHealth+I, 71 mHealth, and 76 control group subjects enrolled in the program. No statistically significant between-group, within-group, and interaction effects between group and time in both physical component summary (PCS) and mental component summary (MCS) scores were found among the three groups. The mHealth group showed an improvement in PCS and depression scores from T1 to T2, sustained at T3; while the mHealth+I group demonstrated improved self-efficacy from T1 to T2, with a decrease at T3.
Conclusion
Adding nurse-directed telephone calls may be of little to no benefit at all in the long term. Future studies may consider a longer intervention period to build and sustain quality of life and self-efficacy levels among community-dwelling older adults.
Clinical trial registration
www.ClinicalTrials.gov, identifier: NCT03878212.
Keywords: apps, health-social partnership, interactivity, mobile health, elderly, aged
Introduction
In the past few years, mHealth applications (mHealth apps) have become a popular channel for older adults to acquire health knowledge and monitor their health conditions (1, 2). Statistics showed that up to the year 2022, more than 350,000 mHealth apps were available in the market, many of them promoting chronic disease self-management among community-dwelling older adults (3). Although the features of these apps vary, in general, they include, but are not limited to, the monitoring of vital signs, health notifications, self-health assessments, multimedia educational materials, and medical appointment reminders (4, 5). Multiple systematic reviews have confirmed that the apps have beneficial effects for older adults, leading to improved blood pressure (6), glycemic control (7), quality of life (8), and treatment adherence (9), and to reductions in hospital admissions (10).
During the COVID-19 pandemic, mental illnesses and the demand for psychological services reached an all-time high among older adults. This has shifted the attention of researchers and healthcare professionals from developing mHealth apps focused only on physical health to those concerned with both the physical and psychological health of users (11, 12). For example, an mHealth app targeting older adults with chronic obstructive pulmonary disease was developed to monitor not only their vital signs, but also to measure the impact of disease on their moods and emotions (13). However, since the users did not receive support from healthcare professionals even though they reported borderline vital signs and unstable emotional states in the app, more than half of participants stopped using the app and reported no relief in depression and anxiety after the program (13). Another study adopted an mHealth app with the aim of maintaining the physical and psychological health of patients with cardiovascular diseases by providing health information and installing a chat function for cardiac patients to contact healthcare professionals when they had urgent enquires (14). Similar to the previous study, approximately half of the participants showed very low usage of the app, as there was no active support from healthcare professionals. The negative results found in blood pressure, activation, and depression levels among the participants in this study also indicated that the app itself was no replacement for the physical presence of healthcare professionals (14, 15). The evidence also suggests that using an mHealth app alone without interaction with healthcare experts may induce a feeling of loneliness, which may lead to depression, lower self-efficacy, and a higher risk of developing a mental disorder (16–18).
In order to improve the psychological health of older adults, previous studies suggested that it is critical to have support from interdisciplinary health and social care professionals including nurses, social workers, and general practitioners (19–21). Commonly appointed as case managers and health educators, nurses are able to provide individualized comprehensive health assessments and care, assist with self-care activities, and offer basic counseling, such as general guidance and interpersonal communication. Social workers can also connect older adults with important psychosocial and financial resources, and general practitioners can prescribe and monitor psychobiological treatment regimes. In terms of mHealth programs, having these health and social experts provide continuous psychological health monitoring, assist and motivate older adults to make daily use of the app, and meet their individual needs, can subsequently lead to better psychological health and quality of life. However, to the best of our understanding, there is no study evaluating the effects of an mHealth program with the support of a health-social partnership team on the psychological outcomes of community-dwelling older adults. The current manuscript will present the methodology, interventions, results of the program, discussion of the benefits of adding nursing interaction supported by a health-social partnership model in the use of mHealth, as well as the sustained beneficial effects on psychological outcomes among older adults after the completion of the program. The findings of the study will provide evidence to inform policy makers and health providers of the importance of human interaction in the use of technology.
Methods
Study design and settings
This was a single-blinded, three-armed randomized controlled trial. The data collectors were blinded, while the interventionists and the participants were not. The participants were recruited through five community centers run under the auspices of a non-governmental organization. The study was conducted based on the Declaration of Helsinki principles and was registered at ClinicalTrials.gov (NCT03878212).
Subjects, recruitment strategy, and randomization
Our app targeted the three most common health problems among community-dwelling older adults, as identified in the latest survey: pain, hypertension, and diabetes mellitus (22). Older adults with at least one of these problems were recruited to the program if they (1) were aged 60 or above and (2) had a smartphone. Excluded were those who (1) had already been involved in other mHealth programs, (2) had been recently hospitalized with a known psychiatric problem within the last 6 months, (3) were bedbound, or (4) who did not have Internet coverage at home.
Simple random sampling was employed to select the participants since it only involves a single random selection and requires little advance knowledge about the participants. Eligible participants were approached in the community centers by a designated staff member. Those who agreed to participate were asked to sign a consent form and were assigned to one of the three groups in this study (i.e., mHealth+I, mHealth, and control) through a computer software program, Research Randomizer. The group assignments were placed in sealed envelopes and opened sequentially at the time of randomization.
Sample size
Sample size was calculated using the GPower 3.1.9.7 software. The software supports a priori sample size calculation by imputing the effect size, desired alpha level, and power level (23). The sample size required for an effect size of 0.2 from a previous similar study (22) and for a margin of error of 0.05 was estimated as being a minimum of 60 participants for each group, assuming a power of 80%. Considering 20% as the likely drop-out rate during the study, the total sample size needed was 72 participants per group, i.e., a total of 216 participants.
Interventions
This was a three-month program. There were three groups in the study: the mHealth group, the mHealth with interactivity group (mHealth+I), and the control group. Details of the intervention are found in our published protocol (24).
mHealth group
Trained staff from the community center helped the participants in the mHealth group download and use an mHealth app developed by the research team and a telecommunication company. The app has several features, including the monitoring of vital signs, scheduling of appointments, notification of medications, and the dissemination of updated health education. A nurse monitored the vital signs of the participants daily in the app database and when abnormalities were found, she would call and assess the participants within 24 h via smartphone and follow the working protocol to either educate the participants in self-care techniques and knowledge or refer the participants to a hospital. The working protocol was developed based on the Omaha System (25) and guidelines from the National Institute for Health and Care Excellence (26). There was also one button that was installed in the app for participants to call the nurse when they considered it to be necessary. The main purpose of the app was to empower the participants to self-manage the three common problems (i.e., pain, hypertension, and diabetes) encountered in late life. The participants were told to use the app daily during the 3-month intervention period. When they had not used it for more than 1 week, a reminder message would pop up on the smartphone screen.
mHealth with interactivity group (mHealth+I)
In addition to the use of the mHealth app, participants in the mHealth+I group received eight proactive calls from a nurse over the 3-month program period (i.e., First month: weekly calls; Second and third months: biweekly calls). In these eight telephone calls, the nurse not only assessed the physical health of the participants, but also their psychological health by using a holistic assessment tool, the Omaha System. The Omaha system was adopted to identify the needs and chief complaints of an individual in four domains: environmental, psychosocial, physiological, and health-related behavior (25). It was found to be applicable for older adults in the community and proven valid for local use (20). Following an assessment, the nurse engaged and empowered the participants to set self-help goals and realistic action plans, and provided psychological support by giving positive verbal encouragement during the conversation. When deemed necessary, the nurse would refer the participants to our health-social partnership team, which included social workers and a general practitioner, according to a team-decided referral protocol. The social workers provided home and meal delivery services, counseling, and financial support, while the general practitioner provided medical consultations, and treatment and procedures to the participants. A biweekly case conference was held between the nurse, the social workers, and the general practitioners to discuss the progress and updated conditions of the subjects, suggest revising or modifying the contract goals, and address the concerns of the subjects.
Control group
The participants in the control group did not receive the mHealth app or proactive calls from nurses.
Data collection
Data were collected at three time-points: pre-intervention (T1), 3 months post-intervention (T2), and 3 months after the completion of the program (T3) to measure the sustained effect of the program. The research assistants, who were trained and blinded to the group assignments, were responsible for collecting the data in the five community centers.
Outcome measures
Quality of life was measured using the 12-item Short Form Health Survey version 2—Chinese (HK) version (SF12v2) (27). The 12 items in the questionnaire were rated on Likert-type scales and summed to provide easily interpretable scales for physical component summary (PCS) and mental component summary (MCS). PCS includes physical functioning, bodily pain, and role-physical, whereas MCS encompasses social functioning, role-emotional, and mental health (28). Higher scores in both components indicated better quality of life. The validity and reliability of the scale have been confirmed in numerous studies (29–31). Higher scores indicate a better quality of life.
Self-efficacy was measured using the General Self-efficacy scale (GCSE) (32). The scores for this 10-item Likert scale ranged from 10 to 40, with higher scores indicating better self-efficacy. The scale showed excellent reliability for Chinese older adults (32).
Depression was assessed using the Geriatric Depression Scale (GDS). This 15-item questionnaire was used to explore the participants' feelings with dichotomous answers. Scores from each item were added for a total possible score of 15, with higher scores representing a higher severity of depressive symptoms. Good reliability, validity, and factor structure were demonstrated (33).
Demographic data were collected at baseline, including information on gender, age, marital status, living conditions, caregiver, and frequency of care.
Data analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 26 software. Baseline demographic data were presented using count numbers and percentages. The outcomes for each group were presented in terms of mean, standard deviation, and 25th and 75th percentiles. The Generalized Estimating Equation was adopted to evaluate the between-group, within-group, and interaction effects between time and group for each outcome since it does not require the outcome variable to have a normal distribution (34). This feature could be highly beneficial to this study as we anticipated that outcomes such as self-efficacy and depression for community-dwelling older adults would be heavily skewed. Intention-to-treat was used as the primary analysis in this study. P < 0.05 were regarded as significant for a two-tailed test.
Ethical considerations
Ethical approval for the study was obtained from the Ethics Sub-committee of the Hong Kong Polytechnic University (HSEARS20190312002). Written consent was received from all participants. Participants were assured that they could withdraw from the study at any time without any adverse consequences. The data collected were encrypted in a password-protected database.
Results
Participant flow
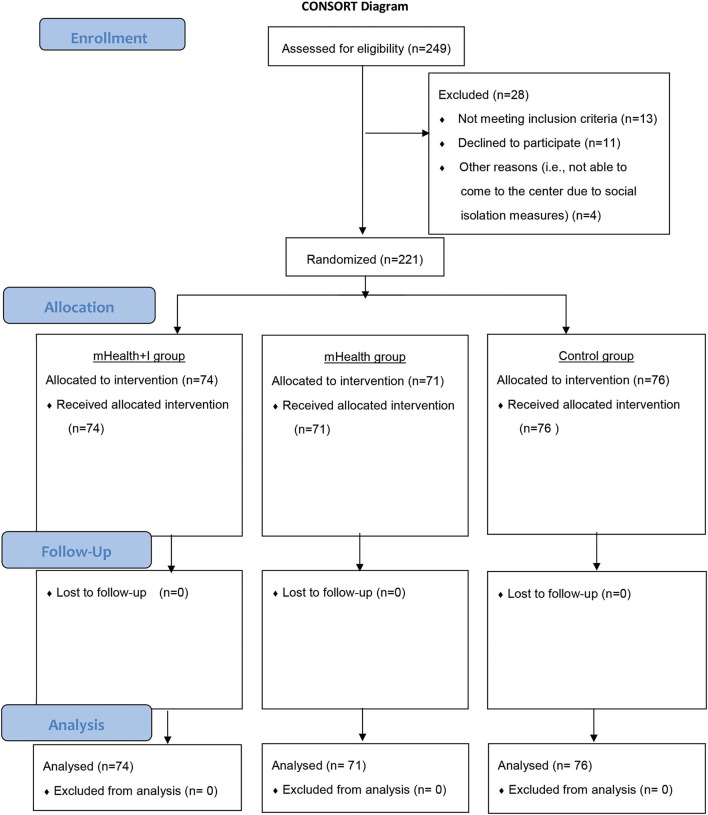
Of the 249 potential community-dwelling older adults who were assessed for eligibility, 221 agreed to join the program and were randomized into the mHealth+I (n = 74), mHealth (n = 71), or control groups (n = 76). No participant dropped out from the program. Figure 1 shows the CONSORT diagram.
Figure 1.
CONSORT table.
Sample description
There were no statistically significant differences in demographic characteristics among the three groups at baseline. Regarding marital status, most participants were married (45.7%) or widowed (47.1%). The majority lived in a flat (98.2%) with either family members (43.0%) or their spouse (26.2%), while 30.8% lived alone. Many reported that they took care of themselves (70.1%). Some were taken care of by their children (41.6%), their spouse (24.4%), or siblings (10.4%). More than half claimed that they always received care from others when needed (65.6%). The baseline demographic characteristics of each group are reported in Table 1.
Table 1.
Demographic characteristics of the participants.
| Total | mHealth + I group | mHealth group | Control group |
p-value Chi-square test/ Kruskal-Wallis Test |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n = 221) | (n = 74) | (n = 71) | (n = 76) | |||||||
| Count |
Table valid N % |
Count |
Column valid N % |
Count |
Column valid N % |
Count |
Column valid N % |
|||
| Gender | Male | 36 | 16.3% | 14 | 18.9% | 9 | 12.7% | 13 | 17.1% | 0.579 |
| Female | 185 | 83.7% | 60 | 81.1% | 62 | 87.3% | 63 | 82.9% | ||
| Age | Mean (SD) | 76.56 | (7.96) | 74.69 | (7.57) | 77.63 | (7.84) | 77.38 | (8.21) | 0.083 |
| Median (range) | 76 | (60–98) | 73.50 | (60–98) | 78.0 | (60–91) | 77.50 | (63–95) | ||
| Marital status | Single | 5 | 2.30% | 2 | 2.70% | 1 | 1.40% | 2 | 2.60% | 0.308 |
| Married | 101 | 45.7% | 39 | 52.7% | 24 | 33.8% | 38 | 50.0% | ||
| Divorced | 11 | 5.00% | 3 | 4.10% | 5 | 7.00% | 3 | 3.90% | ||
| Widowed | 104 | 47.1% | 30 | 40.5% | 41 | 57.7% | 33 | 43.4% | ||
| Living conditions | Flat | 217 | 98.2% | 72 | 97.3% | 70 | 98.6% | 75 | 98.7% | 0.735 |
| Subdivided flat | 2 | 0.90% | 1 | 1.40% | 1 | 1.40% | 43 | 0.00% | ||
| Cage home | 2 | 0.90% | 1 | 1.40% | 0 | 0.00% | 71 | 1.30% | ||
| Others | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | 5 | 0.00% | ||
| Living | Alone | 68 | 30.8% | 21 | 28.4% | 31 | 43.7% | 16 | 21.1% | 0.065 |
| With spouse | 58 | 26.2% | 19 | 25.7% | 13 | 18.3% | 26 | 34.2% | ||
| With family | 95 | 43.0% | 34 | 45.9% | 27 | 38.0% | 34 | 44.7% | ||
| Caregiver: self | Yes | 155 | 70.1% | 55 | 74.3% | 47 | 66.2% | 53 | 69.7% | 0.562 |
| No | 66 | 29.9% | 19 | 25.7% | 24 | 33.8% | 23 | 30.3% | ||
| Caregiver: spouse | Yes | 54 | 24.4% | 18 | 24.3% | 16 | 22.5% | 20 | 26.3% | 0.867 |
| No | 167 | 75.6% | 56 | 75.7% | 55 | 77.5% | 56 | 73.7% | ||
| Caregiver: | Yes | 23 | 10.4% | 7 | 9.50% | 8 | 11.3% | 8 | 10.5% | 0.938 |
| siblings | No | 198 | 89.6% | 67 | 90.5% | 63 | 88.7% | 68 | 89.5% | |
| Caregiver: | Yes | 92 | 41.6% | 34 | 45.9% | 27 | 38.0% | 31 | 40.8% | 0.616 |
| children | No | 129 | 58.4% | 40 | 54.1% | 44 | 62.0% | 45 | 59.2% | |
| Caregiver: | Yes | 5 | 2.30% | 2 | 2.70% | 1 | 1.40% | 2 | 2.60% | 0.841 |
| Children-in-law | No | 216 | 97.7% | 72 | 97.3% | 70 | 98.6% | 74 | 97.4% | |
| Caregiver: | Yes | 3 | 1.40% | 1 | 1.40% | 1 | 1.40% | 1 | 1.30% | 0.999 |
| Friends | No | 218 | 98.6% | 73 | 98.6% | 70 | 98.6% | 75 | 98.7% | |
| Caregiver: | Yes | 7 | 3.20% | 1 | 1.40% | 3 | 4.20% | 3 | 3.90% | 0.547 |
| Neighbors | No | 214 | 96.8% | 73 | 98.6% | 68 | 95.8% | 73 | 96.1% | |
| Caregiver: | Yes | 8 | 3.60% | 4 | 5.40% | 2 | 2.80% | 2 | 2.60% | 0.600 |
| Volunteers | No | 213 | 96.4% | 70 | 94.6% | 69 | 97.2% | 74 | 97.4% | |
| Caregiver: | Yes | 19 | 8.60% | 7 | 9.50% | 5 | 7.00% | 7 | 9.20% | 0.850 |
| Domestic helpers | No | 202 | 91.4% | 67 | 90.5% | 66 | 93.0% | 69 | 90.8% | |
| Frequency of care | Always | 145 | 65.6% | 49 | 66.2% | 41 | 57.7% | 55 | 72.4% | 0.510 |
| Sometimes | 37 | 16.7% | 14 | 18.9% | 13 | 18.3% | 10 | 13.2% | ||
| Only at night | 11 | 5.00% | 2 | 2.70% | 6 | 8.50% | 3 | 3.90% | ||
| No help from others | 28 | 12.7% | 9 | 12.2% | 11 | 15.5% | 8 | 10.5% | ||
SD, standard deviation.
Effectiveness of the interventions on outcomes
Quality of life
The Physical Component Summary (PCS) and Mental Component Summary (MCS) scores were derived from the SF-12v2. As seen in Table 3, there were no statistically significant between-group, within-group, and interaction effects between group and time in both the PCS and MCS scores in the three groups. Only the mHealth group exhibited an improvement in mean PCS scores from T1 to T3 (Figures 2, 3).
Figure 2.
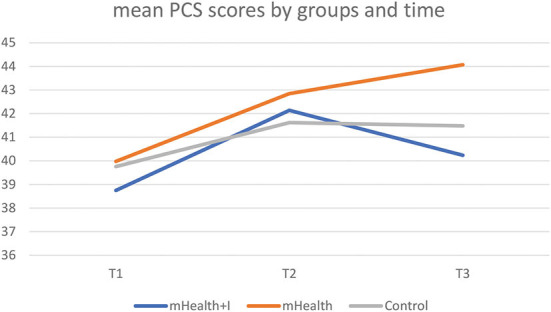
Mean PCS scores by three groups and time.
Figure 3.
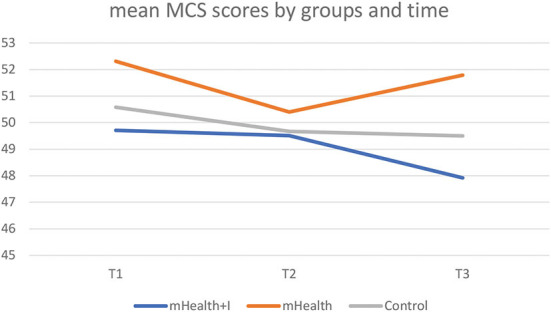
Mean MCS scores by three groups and time.
Self-efficacy
Table 3 shows that there was statistically significant improvement in GCSE scores within the mHealth+I group [β = −2.31 (95%CI of β, −4.26 to −0.36), p = 0.020]. The GEE analysis revealed that there was also an interaction effect between the mHealth+I group in T2 and the control group in T1 [β = 2.81 (95%CI of β, 0.74–4.89), p = 0.008]. However, Table 2 and Figure 4 showed that the GCSE scores of the mHealth+I group dropped from T2 to T3 after an improvement from T1 to T2, which indicated that the intervention effect was not maintained 3 months after the completion of the program.
Table 2.
The mean differences of the outcomes between T1 and T2 for each group.
| Outcomes | Groups | Mean | Standard deviation | Percentile | ||
|---|---|---|---|---|---|---|
| 25 | 75 | |||||
| Quality of life—PCS | Control group | T3 | 41.48 | 9.32 | 35.66 | 48.81 |
| T2 | 41.62 | 8.17 | 35.14 | 48.35 | ||
| T1 | 39.76 | 10.27 | 32.99 | 47.84 | ||
| mHealth group | T3 | 44.07 | 8.52 | 38.72 | 49.67 | |
| T2 | 42.85 | 10.57 | 36.31 | 49.87 | ||
| T1 | 39.98 | 10.20 | 33.12 | 48.35 | ||
| mHealth+I group | T3 | 40.24 | 9.82 | 31.82 | 47.76 | |
| T2 | 42.14 | 8.99 | 34.66 | 50.01 | ||
| T1 | 38.75 | 9.33 | 33.36 | 44.52 | ||
| Quality of life—MCS | Control group | T3 | 49.50 | 12.67 | 42.68 | 59.64 |
| T2 | 49.67 | 11.01 | 44.60 | 57.30 | ||
| T1 | 50.58 | 11.56 | 44.40 | 59.52 | ||
| mHealth group | T3 | 51.79 | 10.69 | 44.00 | 59.94 | |
| T2 | 50.40 | 10.15 | 44.00 | 59.30 | ||
| T1 | 52.31 | 10.94 | 44.50 | 60.53 | ||
| mHealth+I group | T3 | 47.92 | 10.39 | 40.13 | 52.97 | |
| T2 | 49.51 | 9.43 | 45 | 56.29 | ||
| T1 | 49.71 | 10.80 | 42.18 | 59.19 | ||
| Self-efficacy | Control group | T3 | 26.55 | 6.53 | 24.68 | 30.24 |
| T2 | 26.28 | 5.33 | 23.50 | 29.50 | ||
| T1 | 26.70 | 6.36 | 22.50 | 30.00 | ||
| mHealth group | T3 | 26.89 | 5.84 | 24.00 | 30.00 | |
| T2 | 27.73 | 5.22 | 24.00 | 30.00 | ||
| T1 | 26.15 | 6.88 | 22.00 | 31.00 | ||
| mHealth+I group | T3 | 25.62 | 7.13 | 21.00 | 30.00 | |
| T2 | 26.78 | 6.39 | 22.00 | 30.00 | ||
| T1 | 24.39 | 5.90 | 21.00 | 29.00 | ||
| Depression | Control group | T3 | 3.92 | 3.38 | 1.05 | 6.02 |
| T2 | 3.75 | 3.08 | 1.00 | 6.00 | ||
| T1 | 3.63 | 3.26 | 1.00 | 6.00 | ||
| mHealth group | T3 | 3.24 | 3.33 | 1.05 | 6.05 | |
| T2 | 3.54 | 3.14 | 1.00 | 5.00 | ||
| T1 | 4.08 | 3.77 | 1.00 | 7.00 | ||
| mHealth+I group | T3 | 4.41 | 3.46 | 2.05 | 6.11 | |
| T2 | 3.81 | 2.84 | 2.00 | 5.00 | ||
| T1 | 4.47 | 3.59 | 2.00 | 7.00 | ||
PCS, physical component summary; MCS, mental component summary.
Figure 4.
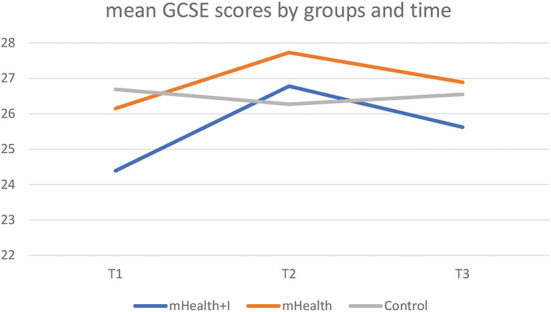
Mean GCSE scores by three groups and time.
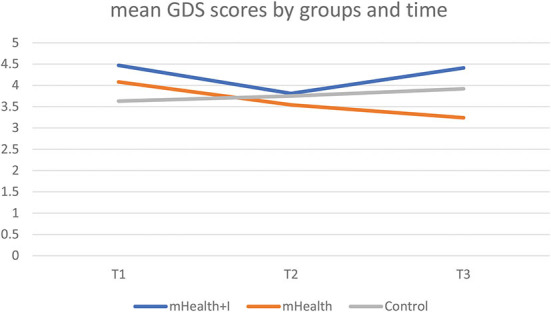
Depression
The baseline mean scores for all three groups were below the cut-off point of 5 (35). Table 2 showed that the mHealth group experienced an improvement in mean GDS scores from T1 to T3. There was a statistically significant interaction effect between the mHealth group in T3 and the control group in T1 [β = −1.14 (95%CI of β, −2.20 to −0.07), p = 0.04] (Table 3). Figure 5 illustrates the mean GDS scores by group and time.
Table 3.
Parameter estimates of outcomes.
| B | SE | 95% CI | Wald χ2 | Sig. | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Quality of life—PCS | ||||||
| (Intercept) | 39.76 | 1.17 | 37.47 | 42.06 | 1,153.62 | < 0.001* |
| mHealth+I group | −1.01 | 1.59 | −4.13 | 2.11 | 0.40 | 0.53 |
| mHealth group | 0.22 | 1.68 | −3.07 | 3.50 | 0.02 | 0.90 |
| Time = 3 | 1.72 | 1.28 | −0.78 | 4.23 | 1.82 | 0.18 |
| Time = 2 | 1.86 | 0.99 | −0.08 | 3.80 | 3.52 | 0.06 |
| mHealth + I group* Time = 3 | −0.23 | 1.78 | −3.73 | 3.26 | 0.02 | 0.90 |
| mHealth + I group * Time = 2 | 1.53 | 1.52 | −1.45 | 4.52 | 1.01 | 0.31 |
| mHealth group* Time = 3 | 2.37 | 1.80 | −1.16 | 5.89 | 1.73 | 0.19 |
| mHealth group * Time = 2 | 1.02 | 1.76 | −2.44 | 4.48 | 0.33 | 0.56 |
| Quality of life—MCS | ||||||
| (Intercept) | 50.58 | 1.32 | 48.00 | 53.16 | 1,473.94 | < 0.001* |
| mHealth+I group | −0.87 | 1.81 | −4.42 | 2.69 | 0.23 | 0.63 |
| mHealth group | 1.73 | 1.84 | −1.89 | 5.34 | 0.88 | 0.35 |
| Time = 3 | −1.08 | 1.47 | −3.96 | 1.80 | 0.55 | 0.46 |
| Time = 2 | −0.91 | 1.03 | −2.92 | 1.10 | 0.79 | 0.37 |
| mHealth+I group* Time = 3 | −0.71 | 2.00 | −4.63 | 3.20 | 0.13 | 0.72 |
| mHealth+I group * Time = 2 | 0.71 | 1.63 | −2.48 | 3.90 | 0.19 | 0.66 |
| mHealth group* Time = 3 | 0.57 | 2.06 | −3.47 | 4.60 | 0.08 | 0.78 |
| mHealth group * Time = 2 | −0.99 | 1.62 | −4.17 | 2.19 | 0.37 | 0.54 |
| Self-efficacy | ||||||
| (Intercept) | 26.70 | 0.73 | 25.28 | 28.12 | 1,355.10 | < 0.001* |
| mHealth + I group | −2.31 | 0.99 | −4.26 | -0.36 | 5.37 | 0.02 |
| mHealth group | −0.54 | 1.09 | −2.68 | 1.59 | 0.25 | 0.62 |
| Time = 3 | −0.15 | 0.78 | −1.67 | 1.38 | 0.03 | 0.85 |
| Time = 2 | −0.42 | 0.81 | −2.02 | 1.17 | 0.27 | 0.61 |
| mHealth + I group* Time = 3 | 1.37 | 1.02 | −0.63 | 3.38 | 1.81 | 0.18 |
| mHealth+I group * Time = 2 | 2.81 | 1.06 | 0.74 | 4.89 | 7.07 | 0.008 |
| mHealth group* Time = 3 | 0.88 | 1.07 | −1.22 | 2.98 | 0.67 | 0.41 |
| mHealth group * Time = 2 | 2.00 | 1.09 | −0.14 | 4.13 | 3.37 | 0.07 |
| Depression | ||||||
| (Intercept) | 3.63 | 0.72 | 2.90 | 4.36 | 95.73 | < 0.001* |
| mHealth + I group | 0.84 | 0.56 | −0.25 | 1.93 | 2.29 | 0.13 |
| mHealth group | 0.45 | 0.58 | −0.68 | 1.59 | 0.61 | 0.43 |
| Time = 3 | 0.29 | 0.40 | −0.49 | 1.07 | 0.53 | 0.47 |
| Time = 2 | 0.12 | 0.35 | −0.57 | 0.81 | 0.11 | 0.74 |
| mHealth + I group* Time = 3 | −0.36 | 0.52 | −1.38 | 0.67 | 0.47 | 0.49 |
| mHealth + I group * Time = 2 | −0.78 | 0.47 | −1.71 | 0.15 | 2.72 | 0.10 |
| mHealth group* Time = 3 | −1.14 | 0.54 | −2.20 | -0.07 | 4.39 | 0.04 |
| mHealth group * Time = 2 | −0.67 | 0.54 | −1.72 | 0.38 | 1.56 | 0.21 |
SE, standard error; *p < 0.05.
Figure 5.
Mean GDS scores by three groups and time.
Discussion
The increasing emergence of mHealth applications warrants an evaluation of their impact not only on physical health, but also on psychological outcomes. The current study examined the added benefit of including nurse-directed telephone follow-up calls supported by a health-social partnership approach in the use of mHealth, as well as the sustained effects on psychological outcomes among community-dwelling older adults. The findings of the study highlight the point that whereas the mHealth group showed improved PCS and depression scores from T1 to T2, which were sustained at T3, the mHealth+I group demonstrated improved self-efficacy from T1 to T2 with a decrease at T3. Overall, the study's findings may offer evidence regarding the positive impact of the mHealth app on some psychological outcomes. However, adding the nurse-directed telephone calls may be of little to no benefit in the long term.
The sustained beneficial effects on PCS and depression levels in the mHealth group participants indicated that the impact of the mHealth application lasted beyond the immediate post-intervention phase. The mHealth application employed in this study offered a one-stop shop for community-dwelling older adults to monitor their vital parameters and facilitated exchanges with a healthcare provider. These active, ongoing interactive processes may have helped to ease the distress associated with not knowing what one's symptoms meant and offering access to professional support if required [Hernandez (36)]. Besides, the interactive platform offered a convenient mode of delivery for health interventions and facilitating self-management, which may have put the minds of these older adults at ease to actively participate in their care during the intervention period (37).
The study also observed improved self-efficacy within the mHealth+I group from T1 to T2. However, the self-efficacy scores dropped at T3, demonstrating that the improvement in self-efficacy that was observed could not be sustained after the completion of the program. Self-efficacy refers to the perceived capability or belief that one can perform a targeted behavior (38). It remains a robust predictor of various health behaviors (39). An increase in the level of self-efficacy is often associated with the perception of a lowering of barriers to engaging in health behaviors, which in turn translates into an increased level of motivation to participate in the required activity (40). It is possible that the gradual increase in the self-efficacy of the older adults as observed at T2 was due to the consistent engagement and support from the health-social partnership team during the intervention period. When the support ended at T2, their levels of self-efficacy dropped. This finding may imply that a longer period may be required to build and sustain self-efficacy levels among community-dwelling older adults. This is particularly important as community-dwelling older adults are a heterogeneous group with diverse chronic illnesses. Considering that the impact of these chronic illnesses may differ, different durations of support may be required for different individuals if self-efficacy levels are to be sustained. In future studies aimed at improving and sustaining improved levels of self-efficacy over longer periods, it may therefore be necessary to consider this factor in the design and implementation of interventions. Also, a gradual approach to weaning older adults off formal support should be considered if such support is included in an intervention.
Related works
Although no study was identified regarding the sustained effects of mHealth applications on psychological outcomes for older adults, some studies have reported positive sustained effects following the utilization of mHealth apps. For instance, in a recent systematic review and meta-analysis of seven studies, the authors observed that the mHealth app had a sustained positive effect on anxiety and depression during the follow-up at 11 weeks (41). In another systematic review and meta-analysis of 28 studies, it was observed that mHealth interventions improved the mental health outcomes of employees and that the effects were sustained across varying time-points (42). A possible reason for this result could be that frequent use of the mHealth app over the study period may have helped the participants to acquire and apply self-care skills and knowledge and to note the positive changes in their health, which might have given them the motivation to continue using the app after the program. There was also another systematic review of eight studies showing that the benefits of app usage such as reducing depression, stress, and substance use among people with all ages can be maximized with the support of mental health professionals (37). However, the small number of studies and participants included in each of the studies, the high risk of bias, and unknown efficacy of long-term follow-up warrant the need for more scientific evidence.
Similar to the finding observed regarding improved self-efficacy in the mHealth+I group, other studies have also reported improved self-efficacy among community-dwelling older adults. For instance, Müller et al. (43) reported an improvement in self-efficacy following the implementation of a mHealth app which comprised of SMS text-messaging and follow-up reminders for older adults over a 12-week period. Physical activity self-efficacy was also reported to have improved among older adults following the implementation of a physical activity mHealth app (44). Despite the improvement in self-efficacy, Fanning et al. (44) did not observe any meaningful improvement in the quality of life of the older adults despite the comprehensive mHealth app that was implemented. Conversely, Christiansen et al. (45) observed improved quality of life following the implementation of a mHealth app for older adults with mild cognitive impairment noting that having moderately or high technical skills in using mHealth technology and using the internet via mHealth technology on a daily or weekly basis was associated with good to excellent QoL. Despite the mixed findings, these studies did not examine the sustained effects of the mHealth apps beyond the intervention duration which makes it rather difficult to draw stronger conclusions in relation to the current study. While more work may be needed to understand this phenomenon, the emerging evidence seems to suggest that mHealth applications may have a positive impact on psychological outcomes in both the short and medium term.
Limitations
Some limitations were noted in this study. First, the study was not able to capture the long-term effect of the intervention (i.e., longer than 6 months) due to the limited time and budget involved. Second, the results are not generalizable to older adults who have no smartphone or Internet coverage at home. Third, the nurse in the study did not provide immediate help because she worked only during office hours. Fourth, the study did not collect objective data. The subjective data collected via self-reported questionnaires in this study may create bias to the result. Regardless of these limitations, the findings of the present study are likely to have a meaningful impact on bringing psychological relief to community-dwelling older adults.
Conclusion
The results of the present study suggest that the therapeutic effects of an mHealth app on community-dwelling older adults can be improved or maintained with regard to psychological outcomes, which include quality of life, self-efficacy, and depression. Future research should focus on ways to motivate older adults to use the mHealth app, in order to maximize its benefits.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Committee of the Hong Kong Polytechnic University. The participants provided their written informed consent to participate in this study.
Author contributions
AW and FW designed the study. AW, JB, and AL drafted the article, which was critically revised by all of the authors. KC and SW coordinated the data collection and supervised the quality of the program. AW conducted the statistical analysis. AW, FW, JB, KC, SW, and AL had full access to interim reports on statistics, analyses, and tables. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by a grant from the Nethersole Institute of Continuing Holistic Health Education (NICHE) (Ref No. ZH4B). The funding organization had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or the decision to publish the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the Hong Kong Lutheran Social Service and Smartone for supporting this study.
References
- 1.Census Statistics Department. Thematic Household Survey Report No.75. (2022). Available online at: https://www.ogcio.gov.hk/en/about_us/facts/doc/THS_Report_No_75.pdf (accessed February 26, 2022).
- 2.Pews Research Center (2021). Mobile fact sheet. https://www.pewresearch.org/internet/fact-sheet/mobile/
- 3.IQVIA Institute,. Digital Health Trends 2021: Innovation, Evidence, Regulation, Adoption. (2021). Available online at: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/digital-health-trends-2021/iqvia-institute-digital-health-trends-2021.pdf?and_=1654618540252 (accessed May 5, 2022).
- 4.Debon R, Coleone JD, Bellei EA, De Marchi ACB. Mobile health applications for chronic diseases: a systematic review of features for lifestyle improvement. Diab Metab Synd Clin Res Rev. (2019) 13:2507–12. 10.1016/j.dsx.2019.07.016 [DOI] [PubMed] [Google Scholar]
- 5.Matthew-Maich N, Harris L, Ploeg J, Markle-Reid M, Valaitis R, Ibrahim S, et al. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR mHealth uHealth. (2016) 4:e5127. 10.2196/mhealth.5127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li R, Liang N, Bu F, Hesketh T. The effectiveness of self-management of hypertension in adults using mobile health: systematic review and meta-analysis. JMIR mHealth uHealth. (2020) 8:e17776. 10.2196/17776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonoto BC, de Araújo VE, Godói IP, de Lemos LLP, Godman B, Bennie M, et al. Efficacy of mobile apps to support the care of patients with diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. JMIR mHealth uHealth. (2017) 5:e4. 10.2196/mhealth.6309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coorey GM, Neubeck L, Mulley J, Redfern J. Effectiveness, acceptability and usefulness of mobile applications for cardiovascular disease self-management: systematic review with meta-synthesis of quantitative and qualitative data. Eur J Prev Cardiol. (2018) 25:505–21. 10.1177/2047487317750913 [DOI] [PubMed] [Google Scholar]
- 9.Gandhi S, Chen S, Hong L, Sun K, Gong E, Li C, et al. Effect of mobile health interventions on the secondary prevention of cardiovascular disease: Systematic review and meta-analysis. Can J Cardiol. (2017) 33:219–31. 10.1016/j.cjca.2016.08.017 [DOI] [PubMed] [Google Scholar]
- 10.Yang F, Wang Y, Yang C, Hu H, Xiong Z. Mobile health applications in self-management of patients with chronic obstructive pulmonary disease: A systematic review and meta-analysis of their efficacy. BMC Pulm Med. (2018) 18:1–9. 10.1186/s12890-018-0671-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Figueroa CA, Aguilera A. The need for a mental health technology revolution in the COVID-19 pandemic. Front Psychiatry. (2020) 11:523. 10.3389/fpsyt.2020.00523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaninotto P, Iob E, Demakakos P, Steptoe A. Immediate and longer-term changes in the mental health and well-being of older adults in England during the COVID-19 pandemic. JAMA Psychiatry. (2022) 79:151–9. 10.1001/jamapsychiatry.2021.3749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whelan ME, Velardo C, Rutter H, Tarassenko L, Farmer AJ. Mood monitoring over one year for people with chronic obstructive pulmonary disease using a mobile health system: retrospective analysis of a randomized controlled trial. JMIR mHealth uHealth. (2019) 7:e14946. 10.2196/14946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang SH, Baek H, Cho J, Kim S, Hwang H, Lee W, et al. Management of cardiovascular disease using an mHealth tool: a randomized clinical trial. NPJ Dig Med. (2021) 4:1–7. 10.1038/s41746-021-00535-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klaver NS, van de Klundert J, Askari M. Relationship between perceived risks of using mHealth applications and the intention to use them among older adults in the Netherlands: cross-sectional study. JMIR mHealth uHealth. (2021) 9:e26845. 10.2196/26845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bakker D, Kazantzis N, Rickwood D, Rickard N. Mental health smartphone apps: review and evidence-based recommendations for future developments. JMIR Mental Health. (2016) 3:e7. 10.2196/mental.4984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen YRR, Schulz P. The effect of information communication technology interventions on reducing social isolation in the elderly: a systematic review. J Med Internet Res. (2016) 18:e18–e18. 10.2196/jmir.4596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mushtag R, Shoib S, Shah T, Mushtag S. Relationship between loneliness, psychiatric disorders and physical health? A review on the psychological aspects of loneliness. J Clin Diagn Res. (2014) 8:WE01–4. 10.7860/JCDR/2014/10077.4828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong AKC, Wong FKY. The psychological impact of a nurse-led proactive self-care program on independent, non-frail community-dwelling older adults: a randomized controlled trial. Int J Nurs Stud. (2020) 110:103724. 10.1016/j.ijnurstu.2020.103724 [DOI] [PubMed] [Google Scholar]
- 20.Wong AKC, Wong FKY, Chow KKS, Wong SM, Lee PH. Effects of a telecare case management program for homebound older adults during the COVID-19 pandemic: a pilot randomized clinical trial. JAMA Netw Open. (2021) 4:e2123453. 10.1001/jamanetworkopen.2021.23453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong AKC, Wong FKY, Ngai JSC, Hung SYK, Li WC. Effectiveness of a health-social partnership program for discharged non-frail older adults: a pilot study. BMC Geriatr. (2020) 20:1–9. 10.1186/s12877-020-01722-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong AKC, Wong FKY, Chang K. Effectiveness of a community-based self-care promoting program for community-dwelling older adults: a randomized controlled trial. Age Ageing. (2019) 48:852–8. 10.1093/ageing/afz095 [DOI] [PubMed] [Google Scholar]
- 23.Kang H. Sample size determination and power analysis using the G*Power software. J Educ Eval Health Prof. (2021) 18:17. 10.3352/jeehp.2021.18.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong AKC, Wong FKY, Chang KK. A proactive mobile health application program for promoting self-care health management among older adults in the community: study protocol of a three-arm randomized controlled trial. Gerontology. (2020) 66:506–13. 10.1159/000509129 [DOI] [PubMed] [Google Scholar]
- 25.Martin KS. The Omaha System: A Key to Practice, Documentation, and Information Management (2nd ed.). Omaha, NE: Health Connections Press; (2005). [Google Scholar]
- 26.National Institute for Health Care Excellence. Home Care: Delivering Personal Care and Practical Support to Older People Living in Their Own Homes. NICE Guideline. (2015). Available online at: https://www.nice.org.uk/guidance/ng21/resources/home-care-delivering-personal-care-and-practical-support-to-older-people-living-in-their-own-homes-pdf-1837326858181 (accessed September 21, 2020).
- 27.Lam ETP, Lam CLK, Fong DYT, Huang WW. Is the SF-12 version 2 health survey a valid and equivalent substitute for the SF-36 version 2 health survey for the Chinese? J Eval Clin Pract. (2013) 19:200–208. 10.1111/j.1365-2753.2011.01800.x [DOI] [PubMed] [Google Scholar]
- 28.Ware JJ, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34:220–33. 10.1097/00005650-199603000-00003 [DOI] [PubMed] [Google Scholar]
- 29.Lam ETP, Lam CLK, Fong DYT, Huang WW. Is the SF-12 version 2 health survey a valid and equivalent substitute for the SF-36 version 2 health survey for the Chinese? J Eval Clin Pract. (2013) 19:200–8. [DOI] [PubMed] [Google Scholar]
- 30.Mak KK, Ho SY, Fong DYT, Lo WS, Lai YK, Lam TH. Norms and demographic differences of the short form-12 health survey version 2 in Chinese adolescents. J Pediatr Child Health. (2011) 47:173–82. 10.1111/j.1440-1754.2010.01939.x [DOI] [PubMed] [Google Scholar]
- 31.Wong WS, Chen PP, Chow YF, Wong S, Fielding R. A study of the reliability and concurrent validity of the Chinese version of the Pain Medication Attitude Questionnaire (ChPMAQ) in a sample of Chinese patients with chronic pain. Pain Med. (2016) 17:1137–44. 10.1093/pm/pnv086 [DOI] [PubMed] [Google Scholar]
- 32.Leung DYP, Leung AYM. Factor structure and gender invariance of the Chinese General Self-Efficacy Scale among soon-to-be-aged adults. J Adv Nurs. (2011) 67:1383–92. 10.1111/j.1365-2648.2010.05529.x [DOI] [PubMed] [Google Scholar]
- 33.Chiu HF, Lee HC, Wing YK, Kwong PK, Leung CM, Chung DW. Reliability, validity and structure of the Chinese Geriatric Depression Scale in a Hong Kong Context: a preliminary report. Singapore Med J. (1994) 35:477–80. [PubMed] [Google Scholar]
- 34.Salazar A, Ojeda B, Duenas M, Fernandez F, Failde I. Simple generalized estimating equations (GEEs) and weighted generalized estimating equations (WGEEs) in longitudinal studies with dropouts: guidelines and implementation in R. Stat Med. (2016) 35:3424–48. 10.1002/sim.6947 [DOI] [PubMed] [Google Scholar]
- 35.Pocklington C, Gilbody S, Manea L, McMillan D. The diagnostic accuracy of brief versions of the Geriatric Depression Scale: a systematic review and meta-analysis. Int J Geriatr Psychiatry. (2016) 31:837–57. 10.1002/gps.4407 [DOI] [PubMed] [Google Scholar]
- 36.Silva E, Lawler S, Langbecker D. The effectiveness of mHealth for self-management in improving pain, psychological distress, fatigue, and sleep in cancer survivors: a systematic review. J Cancer Surviv. (2019) 13:97–107. 10.1007/s11764-018-0730-8 [DOI] [PubMed] [Google Scholar]
- 37.Donker T, Petrie K, Proudfoot J, Clarke J, Birch MR, Christensen H. Smartphones for smarter delivery of mental health programs: a systematic review. J Med Internet Res. (2013) 15:e2791. 10.2196/jmir.2791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bandura A. Health promotion by social cognitive means. Health Educ Behav. (2004) 31:143–64. 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 39.Baumann H, Fiedler J, Wunsch K, Woll A, Wollesen B. mHealth interventions to reduce physical inactivity and sedentary behavior in children and adolescents: systematic review and meta-analysis of randomized controlled trials. JMIR mHealth uHealth. (2022) 10:e35920. 10.2196/35920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Motl RW, McAuley E. Physical activity, disability, and quality of life in older adults. Phys Med Rehabil Clin. (2010) 21:299–308. 10.1016/j.pmr.2009.12.006 [DOI] [PubMed] [Google Scholar]
- 41.Lecomte T, Potvin S, Corbière M, Guay S, Samson C, Cloutier B, et al. Mobile apps for mental health issues: meta-review of meta-analyses. JMIR mHealth uHealth. (2020) 8:e17458. 10.2196/17458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stratton E, Jones N, Peters SE, Torous J, Glozier N. Digital mHealth interventions for employees: systematic review and meta-analysis of their effects on workplace outcomes. J Occup Environ Med. (2021) 63:e512–25. 10.1097/JOM.0000000000002267 [DOI] [PubMed] [Google Scholar]
- 43.Müller AM, Khoo S, Morris T. Text messaging for exercise promotion in older adults from an upper-middle-income country: randomized controlled trial. J Med Internet Res. (2016) 18:e5235. 10.2196/jmir.5235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fanning J, Brooks AK, Hsieh KL, Kershner K, Furlipa J, Nicklas BJ, et al. The effects of a pain management-focused mobile health behavior intervention on older adults' self-efficacy, satisfaction with functioning, and quality of life: a randomized pilot trial. Int J Behav Med. (2022) 29:240–6. 10.1007/s12529-021-10003-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Christiansen L, Sanmartin Berglund J, Anderberg P, Cellek S, Zhang J, Lemmens E, et al. Associations between mobile health technology use and self-rated quality of life: a cross-sectional study on older adults with cognitive impairment. Gerontol Geriatr Med. (2021) 7:23337214211018924. 10.1177/23337214211018924 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.