Abstract
Prior to the COVID-19 pandemic, virtual care (VC) was not routinely offered for assessment of low back pain (LBP), a highly prevalent, disabling condition. COVID-19 related healthcare closures resulted in a rapid backlog of patients referred to a provincial interprofessional LBP program. Without management, these patients were at high risk of experiencing untoward outcomes. Virtual care became a logical option. However, many clinicians lacked experience and confidence with LBP virtual care (LBP-VC); and either were unfamiliar with, or did not have access to, requisite technology. Multi-stakeholder engagement was utilized to understand barriers, identify enablers, and ultimately promote VC for LBP. As a result of the multi-stakeholder engagement, the concept of a toolkit for LBP-VC, including clinical resources and guidelines, emerged. The toolkit contains preparatory steps for VC and a standardized approach to virtual LBP assessment. Key steps in the toolkit have potential applicability to other musculoskeletal populations.
Keywords: access to care, COVID, primary care, quality improvement, community health, spine, low back pain, virtual care
Introduction/Objectives
Virtual care for assessment of low back pain (LBP) was not routinely offered to patients prior to the COVID-19 pandemic. LBP is a highly prevalent, disabling, and costly condition, seen in primary care settings. It is the most common problem among the working population in high-income countries.1-6 If left untreated, LBP can lead to significant burden on patients and the health system, including unnecessary healthcare utilization,6,7 increased opioid use and dependence,8 chronic disability,9 and other untoward outcomes.10,11
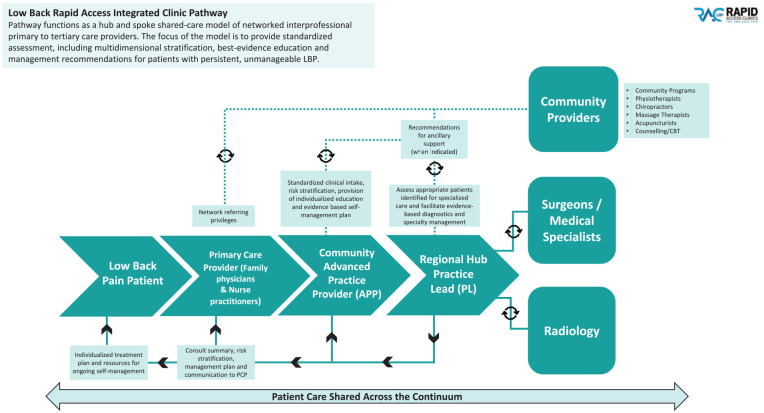
Due to patient and system-level burden of LBP, the Interprofessional Spine Assessment and Education Clinics (ISAEC) was developed and successfully piloted in 3 distinct regions of Ontario, Canada, between 2012 and 2018.12 In 2018, the ISAEC program was expanded province-wide and renamed Rapid Access Clinic—Low Back Pain (RAC-LBP).13-15 The program functions as a hub-and-spoke shared-care model of networked interprofessional primary to tertiary care providers. The model is a primary care initiative that provides standardized in-person assessment, including multidimensional stratification16 for both medical and psychological prognostic risk, and best-evidence education and management recommendations for patients with persistent, unmanageable LBP. Primary care providers include family physicians, nurse practitioners, community-based advanced practice practitioners (APPs) (physiotherapists and chiropractors), regional practice leads (PLs) (physiotherapists and chiropractors), and spine surgeons. The APPs and PLs have advanced musculoskeletal training for assessment and management of LBP. This includes best evidence reviews as well as digital and hands-on training for examination of low back assessment, prognostic risk stratification, and management. The integrated clinical pathway is summarized in Figure 1.
Figure 1.
Ontario RAC-LBP integrated clinical pathway.
In March 2020, a province-wide state of emergency in response to COVID-19 resulted in closure of all non-essential businesses and ambulatory healthcare services, as well as self-management resources. However, primary care physicians and nurse practitioners continued to refer patients. Within 2 weeks there were more than 1000 pending RAC-LBP referrals from primary care physicians and nurse practitioners. Individuals with LBP were at significant risk for physical and mental health deterioration, due to the lack of clinical and self-management resources and pandemic-related stressors.17-19 A large proportion of patients with LBP can be managed conservatively,13 do not require imaging,13,20 will have a normal neurological exam,21,22 and benefit from a personalized home exercise program with education, guidance, and strategies for self-management.22,23 This evidence supported the potential to utilize virtual care (VC) to assess and manage this patient population, when in-person assessment and management was very limited.
However, most RAC-LBP chiropractors and physiotherapists identified a lack of confidence and experience with low back pain–virtual care (LBP-VC) including ability to reliably identify abnormal physical examination findings. In addition, many clinicians either lacked familiarity with, or did not have knowledge of, requisite technology. We, therefore, realized an in-depth multi-stakeholder engagement process was necessary to address clinicians’ concerns and promote confident adoption of VC.
Our objectives are:
To outline the process utilized to successfully develop and implement standardized LBP-VC, across a large provincial geographical region; and
To describe the Toolkit contents for LBP-VC, including a reproducible standardized virtual physical examination.
Methods
An extensive province-wide multi-stakeholder engagement consultation was undertaken. Although we describe 4 phases below, an overlapping iterative approach was undertaken, due to the urgency posed by the COVID-19 pandemic.
The initial phase involved 12 weekly focus groups on LBP-VC, moderated by the provincial clinical leadership team. Focus groups included RAC-LBP APPs and PLs, who worked in publicly-funded hospitals and privately-owned clinics, across rural and urban geographical regions. Inclusion of clinicians brought regional and practical perspectives to discussions; and understanding of nuances related to delivering VC in their respective environments. In addition, since RAC-LBP APPs are the first point of contact for patients after primary care provider referral and are responsible for co-managing conservative care for LBP, it was important to ascertain perspectives on regional barriers and enablers to LBP-VC. One of the 12 focus groups also involved a Ministry of Health representative, who was included to obtain support and endorsement of LBP-VC as the initial funding agreement was for in-person care. In addition, we needed to demonstrate the versatility of the original in-person model of care, and demonstrate, with committed leadership, that provincial standardized LBP-VC was achievable.
Focus groups were conducted through virtual technology utilizing brainstorming methodology. Brainstorming aims to generate as many fresh and creative ideas as possible.24,25 Video recordings and written notes were subsequently reviewed for emergent themes. The concept of a toolkit for LBP-VC emerged with the goal of a standardized approach to virtual low back assessments.
Phase 2 involved individual and group consultations with physiotherapy and chiropractic provincial regulatory colleges and professional associations. The purpose of the individual consultations was to share background information about the RAC-LBP and the emergent need for LBP-VC due to COVID-19; and to gain a preliminary understanding of regulatory or professional concerns about implementation of LBP-VC. The purpose of the group discussions was to inform and seek feedback on development of a toolkit for a standardized approach to LBP-VC; and to seek support to enable overcoming barriers to achieve LBP-VC delivery.
Phase 3 involved consultation with spine surgeons; and synthesis of information from Phases 1 and 2 to develop written materials for inclusion in RAC-LBP-Toolkit. One of the key written components was an in-depth guide to performing a virtual functional physical examination of the spine. In addition, real life experiences from clinicians who were piloting the virtual examination processes and procedures were incorporated. Feedback, from clinicians and patients, was included in RAC-LBP-Toolkit in the form of quotes and practical instructions. In addition, senior healthcare administrators provided input on feasibility of the RAC-LBP-Toolkit.
Phase 4 involved a consensus process with 5 main stakeholder groups: clinicians; regional hospital administrative leads; Ministry of Health representative; regulatory colleges; and professional associations. The draft RAC-LBP-Toolkit was shared for feedback, critique, and endorsement. All feedback was incorporated into a final version, agreed upon by all stakeholder groups.
Following distribution of the RAC-LBP Toolkit, a provincial webinar was conducted with administrative and clinical leadership to promote implementation; and share experiences with VC delivery.
Results
Overall, VC was implemented across all 16 regional hubs, including 29 communities in the Province of Ontario. For example, during April and May 2020, 34/63 (54%) of patients who were offered VC accepted it. In July and August 2020, as VC became more commonly used amongst the general populace, 64/102 (63%) of patients offered VC, accepted.
There was agreement amongst all stakeholders that need for standardized LBP-VC was paramount and immediate. To develop a standardized process, we needed to address identified barriers and enablers to LBP-VC. The barriers and enablers are presented in Table 1.
Table 1.
LBP-VC Barriers and Enablers.
| Barriers | Enablers |
|---|---|
| Lack of awareness of, and access to, secure online platforms that meet regulatory requirements | One of the Regulatory Colleges provided examples of secure online platforms that met regulatory requirements. |
| Ontario Telemedicine Network (OTN) increased its’ user capacity to include clinicians not based in hospitals. | |
| The College of Physiotherapists of Ontario and The Ontario Physiotherapy Association concurrently conducted webinars for members on how to start a VC practice. | |
| Existing experience and expertise with VC among Northern Ontario clinicians with VC was leveraged. | |
| Lack of requisite technology infrastructure amongst clinicians | Consultation with digital health experts. |
| Hospital administrators purchased equipment to enable LBP-VC (webcams, laptops, speakers). | |
| Lack of criteria defining appropriateness of patients for LBP-VC from both safety and quality perspectives | Stakeholders contributed to criteria definition recognizing not all patients are appropriate for LBP-VC; inclusion and exclusion criteria were developed. |
| Signed informed consent was not established for email communication or VC | Input from hospitals and community-based institutions informed development of signed online informed consent process and forms (e.g., scripts describing LBP-VC and fillable informed consent forms). |
| Limitations of performing clinical examination virtually (e.g., assessment of neurological status) | The provincial clinical leadership team, in consultation with clinicians, developed standardized clinical resources and guidelines for virtual assessment of LBP, including neurological tests, that are typically performed with a hands-on approach. |
| Lack of defined process for escalation to spine surgeon with VC | All clinicians agreed on standardized process, including a lower threshold and criteria, for escalation of care. |
In summary, the needs and requirements identified through the multi-stakeholder engagement, were considered and addressed, and informed the contents of “Rapid Access Clinic—Low Back Pain: Virtual Assessment and Education Toolkit,”26 hereafter referred to as “RAC-LBP-Toolkit,” (found at https://www.lowbackrac.ca/for-providers.html).
This section summarizes the contents of the RAC-LBP-Toolkit,26 which provides standardized processes for virtual assessment and management of LBP. The processes outlined in the resources and guidelines have been adopted provincially with excellent face-validity, based on high scores for patient satisfaction with virtual care; and uptake as well as feedback from clinicians. Specifics related to these unique resources are described in Table 2. For each step, online written resources and videos were developed, to optimize patient and provider experience. Professional requirements were incorporated, according to regulatory guidelines and practice standards, with special attention to privacy of information and informed consent, in a virtual context.
Table 2.
Key Steps and Components for LBP-VC.
| Key steps | Components |
|---|---|
| Preparatory | |
| Preparing your practice | Establish infrastructure to support LBP-VC that includes: |
| • A secure platform that meets privacy standards | |
| • A computer, laptop, or tablet that has a camera or webcam that can be repositioned, speakers, microphone, and internet connection | |
| • Compliance with professional regulatory college requirements | |
| • A clinical pathway for escalation of care to surgeon | |
| Selecting your appropriate patient | Patients requiring initial assessment or follow-up appointment may be appropriate for LBP-VC if: |
| • Clinically appropriate/medically stable | |
| • Agreeable to videoconference | |
| • Have a basic understanding of technology | |
| • Have access to technology that supports VC (computer/laptop/tablet, webcam, microphone, internet access, email address) | |
| Patients with any of the following may need review to determine if safe/appropriate for LBP-VC: | |
| • Significant medical history | |
| • Visual or auditory impairments | |
| • Severe neurological impairment | |
| • Severe mobility restriction | |
| • Language barrier | |
| Preparing your patient | Introduce LBP-VC using standardized script |
| Discuss risks and benefits of LBP-VC | |
| Obtain consent to email correspondence | |
| Obtain address of assessment, telephone contact, and alternative contact in case of emergency | |
| Patient clinical intake form completed by patient | |
| Arranging your virtual appointment | Schedule appointment and send link to virtual platform |
| Send patient the following: | |
| • Virtual connection instructions, including troubleshooting | |
| • Instructions on how to prepare your environment for virtual appointment | |
| • Patient education video on how to prepare for the physical/functional assessment | |
| Standardized approach to LBP-VC assessment | |
| Starting your virtual appointment | Clinician ensures private space with appropriate equipment and lighting |
| Obtain consent for virtual assessment as per protocols | |
| Performing “The Virtual RAC-LBP Spine Assessment” | Conduct comprehensive subjective assessment as per usual, including risk of inflammatory back pain, risk of chronicity, risk of opioid dependency, yellow flags, urgent and emergent red flags |
| Performing “The Virtual RAC-LBP Spine Assessment” | Conduct a standardized virtual LBP objective assessment including observation, gait, functional strength testing for lumbar spine myotomes*, range of motion (lumbar spine and lower extremities), modified straight leg raise test, and additional tests modified to virtual setting as described in RAC-LBP-Toolkit24 |
| *LBP-VC functional strength tests for lumbar spine myotomes include method of assessment, grading definitions, and tips on determining grade when ambiguity exists. | |
| Screening (routine) for potential upper motor neuron signs in a virtual setting | Administer DOWN (Dropping/Off-balance/Weakness/Numbness) questionnaire for cervical myelopathy27 |
| Conduct the following special tests—finger escape sign, rapid alternating movements | |
| Assessing cervical range of motion and upper extremity myotomes as needed | Conduct cervical spine range of motion as per usual |
| LBP-VC functional strength tests for cervical spine myotomes include method of assessment, grading definitions, and tips on determining grade when ambiguity exists | |
RAC-LBP-Toolkit also highlights limitations to LBP-VC such as: inability to provide hands-on assessment or treatment; risk to safety within the context of the home (eg, tripping while executing a movement); risk that health information may be intercepted or unintentionally disclosed; and possibility of technical difficulties. Processes to minimize risk and optimize the virtual assessment are outlined, including correspondence via electronic mail should be to an address that is password protected and only accessible by the patient, having an alternative communication plan should there be technical difficulties, and always confirming patient address and alternative contact person in case of an emergency. Lastly, RAC-LBP Toolkit recommends if the patient does not have the appropriate requirements to participate in LBP-VC, or the provider does not feel they can perform an effective or safe assessment, the referral should be on hold until an onsite assessment can be arranged. Alternatively, a screening telephone assessment can rule out any concerning features and if indicated (as would occur during a LBP-VC assessment) escalate for urgent in-person assessment.
For non-urgent presentations, in order to enable trust and confidence in the process and providers, patients were always provided a choice for follow-up method, appropriate to the pandemic criteria at the time. Those who had unclear or concerning presentations were always recommended to have an in-person follow-up. Additionally, our shared-care model mandates a follow-up with the referring primary care provider to review management recommendations. Furthermore, patients who were considered potential surgical candidates at the time of virtual consult by the PL were subsequently assessed in-person by the surgeon. This allowed for further in-person physical examination to determine and discuss appropriateness for surgery, prognosis, surgical risks/benefits review, address patient/family questions/concerns, and when applicable, undertake informed consent for surgery.
Conclusions
High rates of adoption by clinicians, for a standardized LBP-VC assessment across a large geographical region were enabled through multi-stakeholder engagement which resulted in development of the RAC-LBP-Toolkit. Extensive multi-stakeholder consultation provided pragmatic information related to privacy; informed consent; professional standards; regional variations in use of, and access to, technology; and clinical and patient barriers and enablers, ultimately informing development of RAC-LBP-Toolkit content.26 The RAC-LBP-Toolkit26 enabled clinicians to confidently provide a province-wide standardized approach to LBP-VC. In addition, clinicians felt confident in the VC processes for identifying situations when escalation of care was necessary.
Some of the identified LBP-VC barriers have been reported28 including some patients may not have equipment to support LBP-VC; confidentiality risks; and inability to perform adequate physical examination. Australian authors identified the need to develop and test a clinically robust standardized virtual low back physical examination.29 In keeping with this recommendation, one of the key strengths of our RAC-LBP Toolkit was the development of a reproducible alternative functional assessment for LBP diagnosis and identification of clinically significant findings requiring escalation to urgent on-site evaluation.
Future directions include validating LBP-VC physical examination findings compared to hands-on assessment. There is also a need to explore cost-effectiveness of LBP-VC at scale; patient-related factors including demographics, satisfaction, preference, and acceptance with LBP-VC; treatment outcomes, including surgical; safety considerations such as security of online platforms, physical patient safety during the assessment; and comparing rate of escalation to surgeon with in-person and virtual assessment. These areas for future study are supported by Liddy et al30 who also recommend further research on patient safety, morbidity, mortality, and cost-effectiveness metrics.
RAC-LBP-Toolkit processes for VC are comparable with those described by McIntyre et al28 who broadly implemented VC at one institution. With implementation of RAC-LBP-Toolkit, our process for LBP-VC has been operationalized at a multi-institutional level. While RAC-LBP-Toolkit was developed in urgency to care for a growing backlog of patients with LBP, potential applications exist in non-pandemic times. Increasing VC is supported by a publication that reports despite only 6% of Canadians participating in VC, 41% of Canadians would like to have video visits with their healthcare providers.31 Other authors in a physical medicine and rehabilitation practice concur that VC may be the preferred method for spine assessment, citing 64.5% preferred VC over in-person spine appointments during COVID-19.32
In conclusion, although we did not assess if VC would be the patient-preferred method during normal and non-emergency circumstances, our data suggest that factors such as individual circumstances, prior experiences, relationships with health care providers, current symptoms/clinical presentation, climate/weather, and geography may play a role in patient preference for care delivery method. In addition, key steps (informed by multi-stakeholder engagement) within the RAC-LBP-Toolkit have potential applicability to other musculoskeletal populations.
Acknowledgments
The authors acknowledge the RAC-LBP Operations team for their leadership: Silvi Groe, Clinical Director; Samra Mian-Valiante, Director, Strategy; and Kelly Lane, Project Director. We also acknowledge the UHN Foundation for ongoing support. In addition, we thank all key stakeholders who contributed to Toolkit development with special mention to the 16 regional practice leads: Jennifer Nugent, Windsor Regional Hospital; Andrew Bigness, St. Michael’s Hospital; Ravi Rastogi, London Health Sciences Centre; Sheri Robertson, Thunder Bay Regional Health; Mark Kubert, Grand River Hospital; Michael Duffy, Couchiching Family Health Team; David Dos Santos, Hamilton Health Sciences; Ihab El-Sawaf, Scarborough Health Network; Karen Tsui, William Osler Health System; Savvas Frantzeskos, Kingston Health Sciences Centre; Henry Candelaria, Trillium Health Partners; Kirsten Henderson, The Ottawa Hospital; Wesley Wong, Markham Stouffville Hospital; Rhonda Matthews, Sault Area Hospital; Maria Rachevitz, Sunnybrook Health Sciences Centre; Renée-Ann Wilson, Health Sciences North.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Leslie Jayne Soever  https://orcid.org/0000-0002-2095-4050
https://orcid.org/0000-0002-2095-4050
References
- 1. Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39:619-626. [DOI] [PubMed] [Google Scholar]
- 2. Wu A, March L, Zheng X, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6):299-313. doi: 10.21037/atm.2020.02.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Geurts JW, Willems PC, Kallewaard J-W, van Kleef M, Dirksen C. The impact of chronic discogenic low back pain: costs and patients’ burden. Pain Res Manag. 2018;2018:1-8. doi: 10.1155/2018/4696180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buchbinder R, Blyth FM, March LM, Brooks P, Woolf AD, Hoy DG. Placing the global burden of low back pain in context. Best Pract Res Clin Rheumatol. 2013;27:575-589. doi: 10.1016/j.berh.2013.10.007 [DOI] [PubMed] [Google Scholar]
- 5. Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996-2016. JAMA. 2020;323(9):863-884. doi: 10.1001/jama.2020.0734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367. [DOI] [PubMed] [Google Scholar]
- 7. Edwards J, Hayden J, Asbridge M, Gregoire B, Magee K. Prevalence of low back pain in emergency settings: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2017;18:143. doi: 10.1186/s12891-017-1511-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Frogner BK, Harwood K, Andrilla CHA, Schwartz M, Pines JM. Physical therapy as the first point of care to treat low back pain: an instrumental variables approach to estimate impact on opioid prescription, health care utilization, and costs. Health Serv Res. 2018;53(6):4629-4646. doi: 10.1111/1475-6773.12984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010;303(13):1295-1302. doi: 10.1001/jama.2010.344 [DOI] [PubMed] [Google Scholar]
- 10. Williamson V, Greenberg N, Bowden G, Rothenfluh D, Nnadi C, Reynolds J. The mental health impact of providing spine care during COVID-19. Spine J. 2020;20:1363-1366. doi: 10.1016/j.spinee.2020.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Walston Z, McLester C, McLester J. Effect of low back pain chronicity on patient outcomes treated in outpatient physical therapy: a retrospective observational study. Arch Phys Med Rehabil. 2020;101:861-869. doi: 10.1016/j.apmr.2019.11.009 [DOI] [PubMed] [Google Scholar]
- 12. Zarrabian M, Bidos A, Fanti C, et al. Improving spine surgical access, appropriateness and efficiency in metropolitan, urban and rural settings. Can J Surg. 2017;60(5):342-348. doi: 10.1503/cjs.016116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rapid Access Clinics for Low Back Pain. About the RAC low back pain program. Published 2015. Accessed July 12, 2022. www.isaec.org
- 14. Ontario. Ontario making treatment faster for hip, knee and lower back pain. Published December 18, 2017. Accessed July 12, 2022. https://news.ontario.ca/en/release/47597/ontario-making-treatment-faster-for-hip-knee-and-lower-back-pain
- 15. Ontario. Investments in rapid access clinics for muscle and bone disorder assessment. Published December 18, 2017. Accessed July 12, 2022. https://news.ontario.ca/en/backgrounder/47592/investments-in-rapid-access-clinics-for-muscle-and-bone-disorder-assessment
- 16. Rampersaud YR, Bidos A, Fanti C, Perruccio AV. The need for multidimensional stratification of chronic low back pain (LBP). Spine. 2017;42(22):E1318-E1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Martin S, Tallian K, Nguyen VT, van Dyke J, Sikand H. Does early physical therapy intervention reduce opioid burden and improve functionality in the management of chronic lower back pain? Ment Health Clin. 2020;10(4):215-221. doi: 10.9740/mhc.2020.07.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Traeger A, Buchbinder R, Harris I, Maher C. Diagnosis and management of low-back pain in primary care. CMAJ. 2017;189(45):E1386-E1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368-2383. [DOI] [PubMed] [Google Scholar]
- 20. Patel ND, Broderick DF, Burns J, et al. ACR appropriateness criteria low back pain. J Am Coll Radiol. 2016;13:1069-1078. doi: 10.1016/j.jacr.2016.06.008 [DOI] [PubMed] [Google Scholar]
- 21. Hall H. Effective spine triage: patterns of pain. Ochsner J. 2014;14:88-95. [PMC free article] [PubMed] [Google Scholar]
- 22. Clinically Organized Relevant Exam (CORE) Back Tool and Toolkit. Published 2016. Accessed July 12, 2022. https://cep.health/clinical-products/low-back-pain/
- 23. Lim YZ, Chou L, Au RT, et al. People with low back pain want clear, consistent and personalised information on prognosis, treatment options and self-management strategies: a systematic review. J Physiother. 2019;65:124-135. doi: 10.1016/j.jphys.2019.05.010 [DOI] [PubMed] [Google Scholar]
- 24. Besant H. The journey of brainstorming. J Trans Innov. 2016;2:1-7. [Google Scholar]
- 25. History and use of brainstorming. Published 1997-2012. Accessed July 12, 2022. http://www.brainstorming.co.uk/tutorials/historyofbrainstorming.html
- 26. Rapid Access Clinic for Low Back Pain. Virtual assessment and education toolkit. Published 2020. Accessed July 12, 2022. https://www.lowbackrac.ca/for-providers.html
- 27. Barkoh K, Ohiorhenuan IE, Lee L, et al. The DOWN Questionnaire: a novel screening tool for cervical spondylotic myelopathy. Glob Spine J. 2019;9:607-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McIntyre M, Robinson LR, Mayo A. Practical considerations for implementing virtual care in physical medicine and rehabilitation: for the pandemic and beyond. Am J Phys Med Rehabil. 2020;99:464-467. doi: 10.1097/phm.0000000000001453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Truter P, Russell T, Fary R. The validity of physical therapy assessment of low back pain via telerehabilitation in a clinical setting. Telemed J E Health. 2014;20(2):161-167. [DOI] [PubMed] [Google Scholar]
- 30. Liddy C, Moroz I, Mihan A, Nawar N, Keely E. A systematic review of asynchronous, provider-to-provider, electronic consultation services to improve access to specialty care available worldwide. Telemed J E Health. 2019;25(3):184-198. doi: 10.1089/tmj.2018.0005 [DOI] [PubMed] [Google Scholar]
- 31. Auditor General of Ontario. Value for Money Audit. Virtual care: use of communication technologies for patient care. Published December 2020. Accessed July 12, 2022. www.auditor.on.ca
- 32. Bhuva S, Lankford C, Patel N, Haddas R. Implementation and patient satisfaction of telemedicine in spine physical medicine and rehabilitation patients during the COVID-19 shutdown. Am J Phys Med Rehabil. 2020;99(12):1079-1085. [DOI] [PubMed] [Google Scholar]