Abstract
Objective
Tracheostomy is a common procedure that requires management by a multidisciplinary team of health care providers across a range of surgical and nonsurgical specialties. Nonsurgical health care providers have demonstrated a lack of knowledge and confidence in tracheostomy care, which improve with tracheostomy education programs. However, tracheostomy care is rarely included in preresidency medical education. The purpose of this study is to evaluate the effectiveness of a tracheostomy care video on third-year medical students’ knowledge of and confidence in performing tracheostomy care.
Methods
Prior to beginning clinical rotations, third-year medical students completed a 10-question tracheostomy care knowledge test (100 points total) and 11-question confidence survey (110 points total). After watching an 18-minute teaching video on tracheostomy care, students repeated the knowledge test and confidence survey.
Results
An overall 147 medical students completed the educational module. After they watched the tracheostomy education video, their average score on the knowledge test improved from 57.8 to 88.9 out of 100 (P < .0001), and their average rating in confidence improved from 12.7 to 49.1 out of 110 (P < .0001). Students rated the helpfulness of the video a 7.4 out of 10.
Discussion
Medical students’ knowledge of tracheostomy care and confidence in caring for patients with tracheostomies improved after watching the video. Tracheostomy education should be included in early medical education so that future physicians of various specialties can better care for this patient population.
Implications for Practice
Internet-published videos are an accessible educational resource with great potential application to various topics within otolaryngology, including tracheostomy care.
Keywords: PS/QI, medical education, resident education, tracheostomy, video education
Tracheostomy is among the most commonly performed procedures in those who are critically ill.1 The number of patients living with tracheostomy has increased over the last 20 years,2 with >100,000 tracheostomy procedures performed per year in the United States.3 During the SARS-CoV-2 pandemic beginning in 2019, the number of intensive care unit admissions has risen significantly, with many patients requiring mechanical ventilation because of respiratory failure.4,5 Tracheostomy can help wean patients from ventilatory support and prevent complications of long-term mechanical ventilation.6,7 In the setting of COVID-19, some studies have reported that early tracheostomy to shorten duration of mechanical ventilation has shown favorable outcomes in terms of morbidity and mortality, 30-day survival, and shorter duration of intensive care unit stay.8,9
Tracheostomy is associated with a 40%-50% rate of complications, the majority of which are nonemergent (only about 1% are catastrophic, with possibility of death or permanent disability).10,11 Emergent complications, such as tube decannulation, tube obstruction, and hemorrhage, will require care from emergency providers, while nonemergent complications, such as plugged or dislodged tube, desaturation, speaking valve complications, and tube changes, can involve primary care providers and pediatricians.2,12-14 To best care for patients with tracheostomies, all health care providers should be well versed in tracheostomy care at a basic level. Despite this, previous studies have shown low confidence and knowledge levels with tracheostomy care in nonotolaryngologic providers.2,14-17
The clinical consensus statement by the American academy of otolaryngology head and neck surgery (AAO-HNS) in 2013 recognizes the paucity of standardized tracheostomy care and calls for physicians, nurses, and other caretakers for patients with a tracheostomy to minimize complications and reduce variations in practice.18 One way to introduce the standards laid out in the consensus statement is through medical education. An educational curriculum can improve knowledge of tracheostomy care as well as confidence and self-efficacy.16
Previous studies have focused their tracheostomy education programs on residents, first responders, and nonsurgical physicians. Undergraduate medical students (prior to beginning clinical rotations) have not been targeted as a primary group of investigation. Introducing complicated topics such as tracheostomy care at a preclinical stage is important to improve medical students’ confidence and knowledge for when they do encounter patients with tracheostomies in the clinical setting. Formal training curriculums are an important primer to interactions with patients with tracheostomies, because exposure to patients in clinical settings alone is insufficient for gaining competency in managing airway emergencies.17 Primary care physicians classified otolaryngology as one of the most highly relevant surgical disciplines and identified it as a surgical area in which they would benefit from additional exposure and training.19 Some of the key deficits in primary care provider knowledge of otolaryngologic topics are indications for tracheostomy and airway obstruction,19 emphasizing the importance of a standardized tracheostomy curriculum. The goal of a tracheostomy education curriculum is to improve medical students’ confidence and knowledge in tracheostomy care. By teaching future providers, patients with tracheostomies will receive better care and better teaching from their health care providers as well.
Previous studies have shown that videos are an effective method of delivering educational programs to patients.20,21 Videos have been integrated into other tracheostomy care teaching curriculums but not as the primary educational component. By using pre- and posteducation tests, this study assesses the effectiveness of a short educational video paired with a short quiz on level of comfort and overall knowledge of tracheostomy care in third-year medical students prior to clinical rotations.
Materials and Methods
The primary educational resource was an 18-minute video created to address the basics of tracheostomy care from a patient care perspective. It was created by the Eastern Virginia Medical School’s Department of Otolaryngology. The original purpose of the video was for patient education after patients and caretakers requested an updated tracheostomy care video. For this project, the video was paired with a quiz to be applied as an educational tool under the assumption that undergraduate medical students could benefit equally from the video as patients and caretakers. The content of the video is based on objectives identified in the AAO-HNS’s clinical consensus statement and the T-CARES curriculum by Loerzel et al,18,21 as well as clinician-identified relevant information and knowledge gaps. The video uses accessible language and layman’s terms to address common questions and complications. An online format was used so that patients can easily access it at their leisure. It is posted on YouTube and is available for public viewing (https://www.youtube.com/watch?v=Q29gKYH4_jg).
The effectiveness of the video was evaluated via 2 questionnaires: a knowledge test about the contents of the video and a confidence survey relating to the contents of the video. The questionnaires were administered before and after watching the video. The tracheostomy care curriculum, consisting of prevideo questionnaires, the video, and postvideo questionnaires, was administered entirely online.
The prevideo questionnaires allowed for collection of baseline knowledge for each student. The baseline scores for confidence and knowledge could then be compared directly with the postvideo scores for evaluation of changes of each individual’s performance. Because no score was reported to the students or their course instructor at any point, there was more incentive to complete the knowledge and confidence surveys honestly.
Topics of the video include indications for tracheostomy, types of tracheostomy tubes and variations, parts of a tracheostomy tube, tracheostomy care basics, humidification and suctioning, stoma care, how to change a tracheostomy tube, changes to expect with a new tracheostomy, and common problems and emergencies.
Because no standardized assessment of tracheostomy management exists,22 we chose to create a new instrument specific to our teaching tool. The goal of the knowledge assessment instrument was to evaluate whether medical students grasped the main topics of the video. Therefore, we developed the questions for knowledge assessment based on consensus among 5 tracheostomy experts (including otolaryngology faculty and nurses) to identify topics that are clinically relevant and/or common gaps in knowledge that were covered within the video. The format was a 10-question multiple-choice questionnaire, with 2 true-false questions and 8 four-choice questions. The students did not receive feedback about their answers or scores. This allowed a more accurate collection of knowledge and confidence gained from watching the video without extrinsic feedback about their performance.
The confidence survey contained 11 items intended to assess confidence with the topics covered in the video and the questions on the knowledge assessment. Students assigned a rating from 1 to 10, with 10 being the most knowledgeable/comfortable with the named skill. The confidence survey always followed the knowledge assessment, and the questions about confidence directly correlated with the questions on the knowledge assessment. Because students did not receive a score on the knowledge assessment, the external influence of quiz score did not play a role in confidence ratings. The change in confidence ratings were thus more representative of subjective gains in confidence on each question. At the end of the module, students were asked to provide a rating of video helpfulness by using a slider out of 10 points, with 10 signifying most helpful. The full questionnaire as administered to students is attached as supplemental material (available online).
Participants in the curriculum were third-year medical students at Eastern Virginia Medical School. The short curriculum was administered as part of third-year curricular requirements, during the preclerkship phase between June 21 and 25, 2021. Students were permitted to complete the curriculum at any point during that date range. All responses were collected, but those who did not complete the curriculum to the last question of the confidence survey were counted as “incomplete” and therefore excluded. Students were required to complete the online curriculum as part of their preclerkship course and were provided the link to the REDCap survey (Research Electronic Data Capture) through their course website. Responses were kept anonymous, and there was no record kept of individuals who participated in the study. All components of the curriculum were approved by the Eastern Virginia Medical School’s Institutional Review Board (21-03-XX-0054).
Paired 2-sample t tests were performed for means to compare pre- and postvideo scores on the knowledge test and confidence survey. The P value of the 2-tailed t test was reported. The average scores at the pre- and postvideo stages were reported with a pass/fail rate on the knowledge test. The pass rate was set to 70 points based on the pass benchmark of >68 for preclinical medical student didactic courses set by the home institution. Comparisons of change in score on the knowledge test and confidence survey of each individual were also recorded.
Results
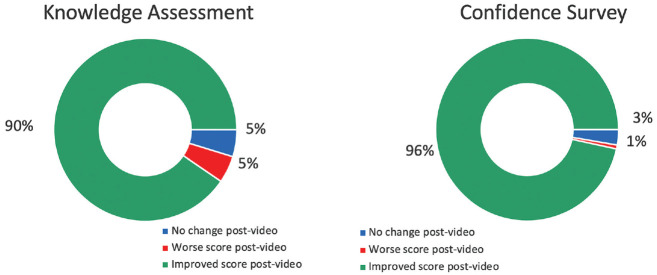
An overall 147 third-year medical students participated in the module over the course of 5 days. For the knowledge assessment, the benchmark for a passing score was set at 70 points (7 correct answers out of 10). The pre- and postvideo knowledge assessments showed a sizable difference in passing rates (Figure 1). Of the prevideo responses, 64.6% of students (n = 95) failed the prevideo knowledge test by scoring <70. Only 1 student scored 100% on the knowledge test prevideo. After they watched the video, the pass rate improved to 93.2% (n = 110), with 79 students receiving a score of 100% on the knowledge assessment. When individuals’ pre- and postvideo scores were compared (Figure 2), most students improved, with just 5% (n = 7) failing to improve and 5% (n = 7) performing worse.
Figure 1.
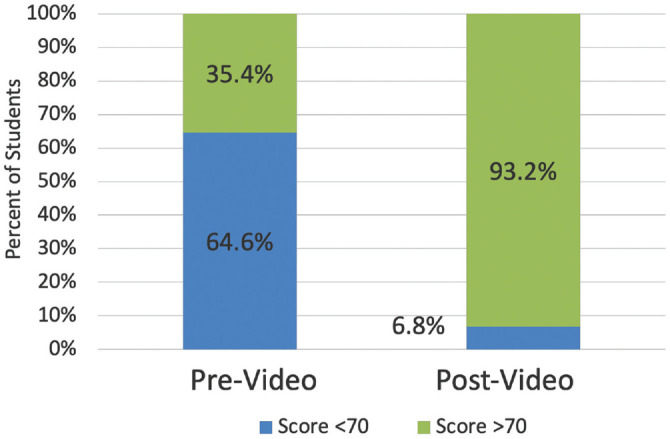
Percentage of students achieving a passing score of 70: pre- and postvideo.
Figure 2.
Individuals’ pre- and postvideo scores and confidence rankings stratified by change in postvideo score.
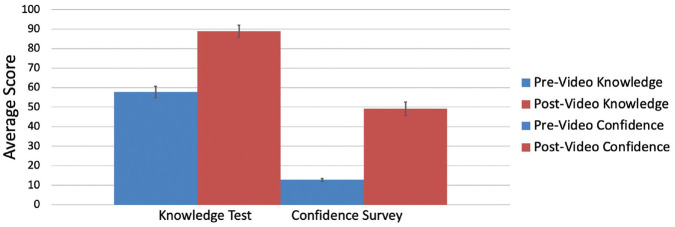
The average scores on the knowledge assessment and confidence survey at the postvideo timepoint increased (Figure 3). When pre- and postvideo scores on the knowledge assessment were compared, the average prevideo score was 57.8 (SD, 2.88). The average postvideo score was 88.9 (SD, 2.98), showing an average increase in score of 31.1 points (95% CI, 27.8-34.5). The P value for average scores was P < .0001. With regard to the confidence survey, the average confidence rating prevideo was 12.7 (SD, 0.68) out of 110 possible points. The minimum possible rating was 11 points total. The prevideo confidence survey indicates a very low level of confidence. After students watched the video, the confidence rating rose to 49.1 (SD, 3.39), indicating a moderate level of confidence with tracheostomy care. The average increase in confidence was 36.4 points (95% CI, 33.0-39.8). The P value for the average score was P < .0001.
Figure 3.
Pre- and postvideo average scores on the knowledge test and confidence survey with 95% CI brackets.
Students were not able to see their scores on the knowledge test at any point, so the confidence level was not influenced by students’ knowledge of their performance on the test. When individuals’ pre- and postvideo self-ratings on the confidence survey were compared (Figure 2), 96% of students (142 students) rated their confidence higher. Four students declared no difference in confidence (3%), while only 1 (<1%) rated the confidence lower after watching the teaching video.
Overall, 95% of the responses included a helpfulness rating of the video (n = 139). On average, helpfulness was rated a 7.4 out of 10 on a sliding scale. Students who performed worse on measures of either confidence or knowledge (n = 5 students) still rated the video as helpful, with an average score of 6.2 out of 10.
Discussion
The tracheostomy video curriculum was effective in improving student confidence and knowledge of tracheostomy care, as evidenced by the significant increases in pre- and postvideo measures. The pass rate on the tracheostomy knowledge quiz increased 28.6%, while the average score improved by 31 points (3 more questions answered correctly). The confidence rating improved by 36 points, indicating that students increased their confidence rating on each question by at least 3 points after watching the video. The average improvement in knowledge and confidence ratings in medical students mirrors results from prior studies in different caretaker populations that used longer, more complicated simulation models.2,12-14,16,23,24
As expected, undergraduate medical student knowledge of and confidence with tracheostomy care are low. Otolaryngology is rarely included as a preclerkship module, and it is a poorly visualized specialty within early medical education.18,25 As a result, very few students performed well. The confidence rating prior to watching the video was uniformly low as compared with knowledge assessment scores, 13 out of 110 on average, with a range between 11 and 35. An average score of 13 indicates that most students rated their confidence at the lowest rating for most questions. The educational intervention was effective likely because most students started from a low level at baseline and were given a focused and simple primer on the topic.
Tokarz et al demonstrated that, among internal medicine and emergency medicine residents who have cared for patients with tracheostomy or laryngectomy, less than half were able to correctly address basic airway emergencies.17 When primed with formal tracheostomy education, residents performed better following clinical rotations than their peers who attended rotations without a tracheostomy training course.16 Therefore, formal education on airways and tracheostomy is a necessity in early medical education. As tracheostomy care is increasingly becoming a multidisciplinary practice, all future health care providers can benefit from training.16,18
Internet-published video is a medium with a range of applications that can be valuable in patient, provider, and student education. Because the video has been published to YouTube, it is widely accessible and does not suffer from the same barriers as in-person teaching modules.
Previous studies in tracheostomy education have relied on simulation, lecture, or both. While valuable and effective, the logistical arrangements require much greater oversight, time, and resources for the organizers and the participants. In contrast, an Internet-published video can be easily incorporated into educational programs and provide a similar benefit to learners. Michel et al demonstrated the success of using a computer-based learning module for teaching high-yield otolaryngology topics in third- and fourth-year medical students.25 The same format of a short teaching video based on clinical guidelines paired with a pre- and postvideo knowledge assessment is generalizable and can increase exposure to less-visualized medical specialties or high-risk skills that would benefit from formal teaching curriculum. In addition, it can increase exposure and interest in specialties such as otolaryngology.25,26 However, the virtual format of our educational module limits actual hands-on experience of tracheostomy care. The video curriculum is intended as a primer to clinical experience or as an adjunct to other clinical training.
Limitations include a lack of standardized educational curriculum for tracheostomy. The 10 questions on our quiz cannot encompass all that is important in tracheostomy care and represents only what we felt were important topics in the preclinical setting. While standardization of a tracheostomy care curriculum is challenging without a set of clinical practice guidelines, our video touches on many of the clinical consensus statements and allows health care practitioners who view the video to start with a baseline level of knowledge.18 Administering the same curriculum to all members at an institution will allow care team members to work more efficiently and benefit more from anecdotal exchanges of knowledge. An additional limitation is that our postvideo assessments capture only short-term gains in knowledge and confidence. Collecting additional data at the postrotation point in the same population could provide valuable information about the longevity of the knowledge and confidence gained. It would also be an opportunity to evaluate subjective comfort with tracheostomy care during rotations. A limitation with regard to student education is that the video was created and intended for patient education and does not include certain topics that are more relevant for student trainees, such as the difference between laryngectomy and tracheostomy.
Implications for Practice
For medical student or resident education, the tracheostomy care video is easy to implement as it requires just 18 minutes to watch and is easily paired with a quiz to incentivize active learning. Computer-assisted instruction has shown to be beneficial in terms of availability, repetition, efficiency, and ability for use in self-assessment.27 It is becoming increasingly popular to include videos as a component of remote learning or as a virtual modality of a multimodal curriculum.28 Because students have access to the video at any time, it can serve as a reference tool or a refresher when they do encounter patients with tracheostomy.
For patients, the video is a valuable supplement to the necessary hands-on teaching that patients receive when preparing for tracheostomy surgery and can improve quality of life postoperatively. In the setting of percutaneous coronary intervention, adjunct discharge education through videos shown on iPads improved patient knowledge, confidence, and satisfaction.20 Given the results of the video in medical students, the video will likely be similarly effective for patients. Providing a supplemental resource can benefit only the patients. Following tracheostomy and discharge home, access to video resources led to increased quality of life scores.29 Internet-published video is easy to reference when patients have nonemergent questions or concerns, and it can improve patients’ senses of agency over their health. Previous research has shown that implementing tracheostomy education programs for caregivers is effective as well.13
With regard to patient application, our study was limited to medical students entering clinical clerkships. We have collected data from further cohorts of third-year preclerkship students and plan to collect data from the original cohort of students in this study at the conclusion of their clerkship rotations 2 years after they first watched the video. We plan to compare data from cohorts of fourth-year medical students who were and were not exposed to this tracheostomy video before clinical rotations. We would like to repeat the project in patients and caretakers of patients with tracheostomy to assess for effectiveness of the video and any differences in reception and effects of the video.
Conclusion
Preclinical medical students lack knowledge of and confidence with tracheostomy care. A video-based short educational curriculum for tracheostomy care resulted in significant improvements in knowledge and confidence measures. The short video paired with a knowledge assessment curriculum provides instrumental background information for procedures and topics that will be encountered during clinical rotations and is particularly helpful in less-visualized medical specialties. This virtual educational tool can be easily administered to a variety of populations, including patients, caretakers, and other health care professionals.
Author Contributions
Serena F. Pu, concept and design, final approval of project, data analysis, critical revisions, wrote manuscript; John V. Boyle, concept and design, critical revisions, data interpretation, final approval of project, wrote manuscript; Benjamin J. Rubinstein, concept and design, critical revisions, final approval of project; Matthew J. Bak, concept and design, critical revisions, final approval of project; A. Brooke Hooper, concept and design, data acquisition, critical revisions, final approval of project; Jonathan R. Mark, concept and design, critical revisions, data interpretation, final approval of project, supervision of project, wrote manuscript
Disclosures
Competing interests: None.
Sponsorships: This work was supported by the EVMS/CHKD Summer Scholars Research Program.
Funding source: None.
Supplemental Material
Supplemental material, sj-docx-1-opn-10.1177_2473974X221134267 for Video-Based Tracheostomy Care Education for Medical Students by Serena F. Pu, John V. Boyle, Benjamin J. Rubinstein, Matthew J. Bak, A. Brooke Hooper and Jonathan R. Mark in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Acknowledgments
We acknowledge Brian Main for his assistance with preparation of the REDCap survey. We also acknowledge Laura Stone, BSN, for her assistance in preparing the Institutional Review Board application.
Footnotes
This article was presented at the Virginia Society of Otolaryngology 2022 Annual Meeting; Williamsburg, Virginia; April 8-9, 2022.
ORCID iD: Serena F. Pu  https://orcid.org/0000-0002-4627-6403
https://orcid.org/0000-0002-4627-6403
Supplemental Material: Additional supporting information is available at http://journals.sagepub.com/doi/suppl/10.1177/2473974X221134267
References
- 1. Casserly P, Lang E, Fenton JE, Walsh M. Assessment of healthcare professionals’ knowledge of managing emergency complications in patients with a tracheostomy. Br J Anaesth. 2007;99(3):380-383. doi: 10.1093/bja/aem167 [DOI] [PubMed] [Google Scholar]
- 2. Mehta K, Schwartz M, Falcone TE, Kavanagh KR. Tracheostomy care education for the nonsurgical first responder: a needs-based assessment and quality improvement initiative. OTO Open. 2019;3(2):2473974X19844993. doi: 10.1177/2473974X19844993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shah RK, Lander L, Berry JG, Nussenbaum B, Merati A, Roberson DW. Tracheotomy outcomes and complications: a national perspective. Laryngoscope. 2012;122(1):25-29. doi: 10.1002/lary.21907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225-1228. doi: 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Michetti CP, Burlew CC, Bulger EM, Davis KA, Spain DA; Critical Care and Acute Care Surgery Committees of the American Association for the Surgery of Trauma. Performing tracheostomy during the COVID-19 pandemic: guidance and recommendations from the Critical Care and Acute Care Surgery Committees of the American Association for the Surgery of Trauma. Trauma Surg Acute Care Open. 2020;5(1):e000482. doi: 10.1136/tsaco-2020-000482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shiba T, Ghazizadeh S, Chhetri D, St John M, Long J. Tracheostomy considerations during the COVID-19 pandemic. OTO Open. 2020;4(2):2473974X20922528. doi: 10.1177/2473974X20922528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Glibbery N, Karamali K, Walker C, Fitzgerald O’Connor I, Fish B, Irune E. Tracheostomy in the coronavirus disease 2019 patient: evaluating feasibility, challenges and early outcomes of the 14-day guidance. J Laryngol Otol. 2020;134(8):688-695. doi: 10.1017/S0022215120001759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Queen Elizabeth Hospital Birmingham COVID-19 Airway Team. Safety and 30-day outcomes of tracheostomy for COVID-19: a prospective observational cohort study. Br J Anaesth. 2020;125(6):872-879. doi: 10.1016/j.bja.2020.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bontempo LJ, Manning SL. Tracheostomy emergencies. Emerg Med Clin North Am. 2019;37(1):109-119. doi: 10.1016/j.emc.2018.09.010 [DOI] [PubMed] [Google Scholar]
- 11. Lee ST, Kim MG, Jeon JH, et al. Analysis of morbidity, mortality, and risk factors of tracheostomy-related complications in patients with oral and maxillofacial cancer. Maxillofac Plast Reconstr Surg. 2016;38(1):32. doi: 10.1186/s40902-016-0078-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Agarwal A, Marks N, Wessel V, et al. Improving knowledge, technical skills, and confidence among pediatric health care providers in the management of chronic tracheostomy using a simulation model. Pediatr Pulmonol. 2016;51(7):696-704. doi: 10.1002/ppul.23355 [DOI] [PubMed] [Google Scholar]
- 13. Prickett K, Deshpande A, Paschal H, Simon D, Hebbar KB. Simulation-based education to improve emergency management skills in caregivers of tracheostomy patients. Int J Pediatr Otorhinolaryngol. 2019;120:157-161. doi: 10.1016/j.ijporl.2019.01.020 [DOI] [PubMed] [Google Scholar]
- 14. Dorton LH, Lintzenich CR, Evans AK. Simulation model for tracheotomy education for primary health-care providers. Ann Otol Rhinol Laryngol. 2014;123(1):11-18. doi: 10.1177/0003489414521144 [DOI] [PubMed] [Google Scholar]
- 15. Yelverton JC, Nguyen JH, Wan W, Kenerson MC, Schuman TA. Effectiveness of a standardized education process for tracheostomy care. Laryngoscope. 2015;125(2):342-347. doi: 10.1002/lary.24821 [DOI] [PubMed] [Google Scholar]
- 16. Benjamin J, Roy K, Paul G, et al. Improving resident self-efficacy in tracheostomy management using a novel curriculum. MedEdPORTAL. 2020;16:11010. doi: 10.15766/mep_2374-8265.11010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tokarz E, Szymanowski AR, Loree JT, Muscarella J. Gaps in training: misunderstandings of airway management in medical students and internal medicine residents. Otolaryngol Head Neck Surg. 2021;164(5):938-943. doi: 10.1177/0194599820949528 [DOI] [PubMed] [Google Scholar]
- 18. Mitchell RB, Hussey HM, Setzen G, et al. Clinical consensus statement: tracheostomy care. Otolaryngol Head Neck Surg. 2013;148(1):6-20. doi: 10.1177/0194599812460376 [DOI] [PubMed] [Google Scholar]
- 19. Ishman SL, Stewart CM, Senser E, et al. Qualitative synthesis and systematic review of otolaryngology in undergraduate medical education. Laryngoscope. 2015;125(12):2695-2708. doi: 10.1002/lary.25350 [DOI] [PubMed] [Google Scholar]
- 20. Wischer JL, Oermann MH, Zadvinskis IM, Kinney KC. Effects of iPad video education on patient knowledge, satisfaction, and cardiac rehabilitation attendance. Qual Manag Health Care. 2018;27(4):204-208. doi: 10.1097/QMH.0000000000000185 [DOI] [PubMed] [Google Scholar]
- 21. Loerzel VW, Crosby WW, Reising E, Sole ML. Developing the Tracheostomy Care Anxiety Relief Through Education and Support (T-CARES) program. Clin J Oncol Nurs. 2014;18(5):522-527. doi: 10.1188/14.CJON.522-527 [DOI] [PubMed] [Google Scholar]
- 22. Roof SA, Gray M, Meyer A, et al. An interactive workshop to increase comfort and knowledge regarding adult tracheostomy management: a pilot study. Journal of Scientific Innovation in Medicine. 2020;3(3):22. doi: 10.29024/jsim.51 [DOI] [Google Scholar]
- 23. Keilin CA, Farlow JL, Malloy KM, Bohm LA. Otolaryngology curriculum during residency preparation course improves preparedness for internship. Laryngoscope. 2021;131(7):E2143-E2148. doi: 10.1002/lary.29443 [DOI] [PubMed] [Google Scholar]
- 24. Miles A, Greig L, Jackson B, Keesing M. Evaluation of a tracheostomy education programme for speech-language therapists. Int J Lang Commun Disord. 2020;55(1):70-84. doi: 10.1111/1460-6984.12504 [DOI] [PubMed] [Google Scholar]
- 25. Michel MC, Thal A, Sparks AD, Zapanta PE. Using computer-assisted instruction to increase otolaryngology education during medical school. MedEdPORTAL. 2021;17:11065. doi: 10.15766/mep_2374-8265.11065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Spiers H, Enayati H, Moussa R, et al. Augmenting ENT surgery outside the medical school curriculum: the role of a 1-day otolaryngology course. J Laryngol Otol. 2019;133(4):269-274. doi: 10.1017/S0022215119000331 [DOI] [PubMed] [Google Scholar]
- 27. Fung K. Otolaryngology–head and neck surgery in undergraduate medical education: advances and innovations. Laryngoscope. 2015;125(suppl 2):S1-S14. doi: 10.1002/lary.24875 [DOI] [PubMed] [Google Scholar]
- 28. Ruthberg JS, Quereshy HA, Ahmadmehrabi S, et al. A multimodal multi-institutional solution to remote medical student education for otolaryngology during COVID-19. Otolaryngol Head Neck Surg. 2020;163(4):707-709. doi: 10.1177/0194599820933599 [DOI] [PubMed] [Google Scholar]
- 29. Mohammadi N, Farahani M, Vatandost S. Effect of videotape for home instruction on the quality of life of tracheostomy patients: a randomized clinical trial. J Med Life. 2015;8(spec iss 4):287-294. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-opn-10.1177_2473974X221134267 for Video-Based Tracheostomy Care Education for Medical Students by Serena F. Pu, John V. Boyle, Benjamin J. Rubinstein, Matthew J. Bak, A. Brooke Hooper and Jonathan R. Mark in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation