Abstract
Objectives
Home visiting is a popular approach to improving the health and well-being of families with infants and young children in the United States; but, to date, no home visiting program has achieved population impact for families in rural communities. The current report includes evaluation results from the dissemination of a brief, universal postpartum home visiting program to four high-poverty rural counties.
Methods
The study utilized a quasi-experimental design. From Sept. 1, 2014–Dec. 31, 2015, families of all 994 resident births in four rural eastern North Carolina counties were assigned to receive Family Connects (FC; intervention group). A representative subsample of families participated in impact evaluation when the infants were 6 months old: 392 intervention group families and 126 families with infants born between Feb. 1, 2014–July 31, 2014 (natural comparison group). Data were analyzed preliminarily for reporting to funders in 2016 and, more comprehensively, using propensity score matching in 2020.
Results
Of FC-eligible families, 78% initiated participation; 83% of participating families completed the program (net completion = 65%). At age 6 months, intervention parents reported more community connections, more frequent use of community services, greater social support, and greater success with infants sleeping on their backs. Intervention infants had fewer total emergency department and urgent care visits. Intervention parents had more total emergency department and urgent care visits and (marginally) fewer overnights in the hospital.
Conclusions for practice
FC can be implemented successfully in high-poverty rural communities with broad reach and positive benefits for infants and families.
Keywords: Home visiting, Population health, Rural health, Prevention, System of care
Introduction
Compared to urban counterparts, rural families with infants and young children in the United States have been shown to experience poorer outcomes across a wide range of population health indicators, including greater postpartum depression (Mollard et al., 2016), greater maternal morbidity and mortality (Kozhimannil et al., 2019), more child accidents and injuries, lower breastfeeding rates, and less participation in well-child care (Probst et al., 2018; US Department of Health and Human Services, 2015). These disparities are partially attributed to challenges in service availability and delivery. Although 75% of US counties are rural, only 10% of healthcare providers operate in rural communities (Matthews et al., 2017); hospital closures rates are higher (Rubin, 2018); and health departments are typically less well-funded and understaffed (Harris et al., 2016). Although the past decade has seen new approaches to rural health promotion, including telehealth, integration of primary and mental health care, and utilization of community health workers, substantial barriers related to lack of available services remain (for a review, see Warren & Smalley, 2014). Additional innovative approaches are needed to support population health and well-being for rural families with infants and young children.
Home visiting is a popular public-health intervention for improving family health in United States. Federal support for home visiting has increased over the past decade, with over $2.5 billion allocated through the Maternal, Infant, and Early Childhood Home Visiting (MIECHV) program between 2010 and 2017 (Congressional Research Service, 2018). Although multiple meta-analytic studies link home visiting to a variety of positive maternal and child outcomes (e.g., Kendrick et al., 2000), few programs implement universal screening and referral processes as part of enrollment (for exceptions, see Green et al., 2016; Whiteside-Mansell et al., 2007). To date, no home visiting program has demonstrated population impact for children and families in rural communities.
FC is a short-term nurse home visiting approach designed to deliver brief education and intervention, assess family needs, and connect families to community resources for ongoing support. FC achieves population reach by combining top–down engagement of community agencies with bottom-up engagement of individual families. FC is delivered universally, tailoring intervention to family-specific needs. FC does not replace more intensive services, including long-term home visiting; rather, FC assesses families to match them with the community services they need and choose. Findings from two randomized-controlled trials (RCT) demonstrated high-quality implementation and positive impact on family health and well-being, including increased community connections, better maternal mental health, and reduced infant emergency medical care utilization (Dodge et al., 2014, 2019; Goodman et al., 2021).
While promising, FC impact has not yet been evaluated outside of Durham, NC, the urban community in which the model was developed. Both implementation quality and impact might decrease as the model is disseminated (e.g., Duggan et al., 2018). FC is designed to achieve positive impact by connecting families to community services; it is unknown whether broad reach and positive outcomes can be achieved in high-poverty, rural communities characterized by more limited resources.
The current study evaluated the implementation and impact of FC in four high-poverty, rural counties in eastern North Carolina (Beaufort, Bertie, Chowan, and Hyde). Given the limited availability of resources and services in these communities, it was hypothesized that (1) the program could be implemented with broad reach and high quality and (2) the magnitude of positive effects would be smaller compared to previous RCTs conducted in a well-resourced urban community.
Methods
Evaluation Design
The study utilized a quasi-experimental, natural comparison design because an RCT was inconsistent with the local mandate to deliver services to all families. FC implementation occurred from Sept. 1, 2014–Dec. 31, 2015 (described in detail below); and all resident county births were eligible for FC. Impact evaluation compared outcomes for families of infants born in the months immediately prior to program launch (comparison group n = 360; Feb. 1, 2014–July 31, 2014) to families of infants born during the FC implementation period (intervention group n = 1068; Sept. 1, 2014-Dec. 31, 2015). Outcomes were assessed for both groups via a 30-min telephone interview when the infants were 6 months old. Families of August 2014 births were omitted a priori because FC training and piloting occurred during this transition month.
To reduce potential bias, all families assigned to FC were recruited for impact evaluation without regard to their actual FC participation; further, participating families were “blind” to the primary goal of evaluating FC. Interviews were completed by research aides unaffiliated with FC and were not informed which families received FC. All families provided consent prior to completing the interview and were compensated for their participation. All study procedures were approved by the Duke University Campus IRB.
Intervention Population and Procedures
From Sept. 1, 2014–Dec. 31, 2015, FC was implemented by a team of nurses and staff employed at a rural public health department. The eligible population included 994 resident births identified through infant hearing screen records provided weekly by the North Carolina Department of Health and Human Services. Records for 74 resident births were not identified through this process; these families were excluded from implementation analyses. In-person scheduling was conducted at one community hospital in the largest county; all other families were scheduled via telephone.
Implementation followed a manualized protocol comprising three core components. First was direct intervention, including (a) a two hour integrated home visit (IHV) conducted by a registered public health nurse, including birthing parent and infant health assessments, brief education (e.g., safe sleep), assessment of family-specific needs and, for families with significant need, referrals to community resources for longer-term support; (b) 1–2 in-home or telephone follow-up encounters, as clinically necessary, to conduct additional assessment or to facilitate connections to services; and (c) a telephone follow-up one month after case closure to assess community connection outcomes. Families provided consent prior to the IHV and received a small gift for participation (e.g., diapers, book).
During the IHV, nurses utilized the Family Support Matrix (Dodge et al., in press) to assess family health and psychosocial risk for 12 empirically-derived factors across four domains (Healthcare: parent health, infant health, health care plans; Parenting/childcare: childcare plans, parent-infant relationship, management of infant crying; Family safety/resources: material supports, family violence, maltreatment history; and Parent well-being: depression/anxiety, substance abuse, social/emotional support). The assessment emphasizes a family–friendly discussion drawing on nurses’ clinical judgment and parents’/caregivers’ views of family needs. The interview incorporates validated screening instruments for depression (Cox et al., 1987), substance use (Brown & Rounds, 1995), and family violence (Straus & Douglas, 2004). Each of the 12 factors was rated on a four-point scale: “1” (low risk) no subsequent intervention; “2” (moderate risk) short-term, nurse-delivered intervention; “3” (significant risk) referral (with parent consent) to matched community services; and “4” (imminent risk) emergency intervention (< 1% of cases).
The second model component comprised engagement of community agencies, identifying services mapped onto the 12 assessment factors to result in an FC-specific electronic agency directory utilized by nurses to identify the “best” fit for a family’s needs. The work with agencies also promotes feedback loops between FC and service providers regarding family needs and community capacity. The third component was an electronic database exclusive to FC staff that houses the community agency directory and serves as the FC service record.
Impact Evaluation Population and Procedures
Research aides utilized short-form birth records to identify families eligible for the impact evaluation when infants were 6 months old. Records were obtained for 1428 families (see Fig. 1); 185 families were ineligible to participate: 177 families could not be confirmed as living in a study county; 6 families experienced a birthing parent or infant death prior to the interview; and 2 families did not speak English or Spanish and could not provide consent. Of the 1243 families eligible to participate, 518 (41.6%) successfully completed the survey (comparison group n = 126; intervention group n = 392), with a marginally higher participation rate among intervention group families (43.1% vs. 37.6%, X2(1) = 3.04, p = 0.08). For the 11 families with twins, one member of the pair was randomly excluded from all analyses.
Fig. 1.
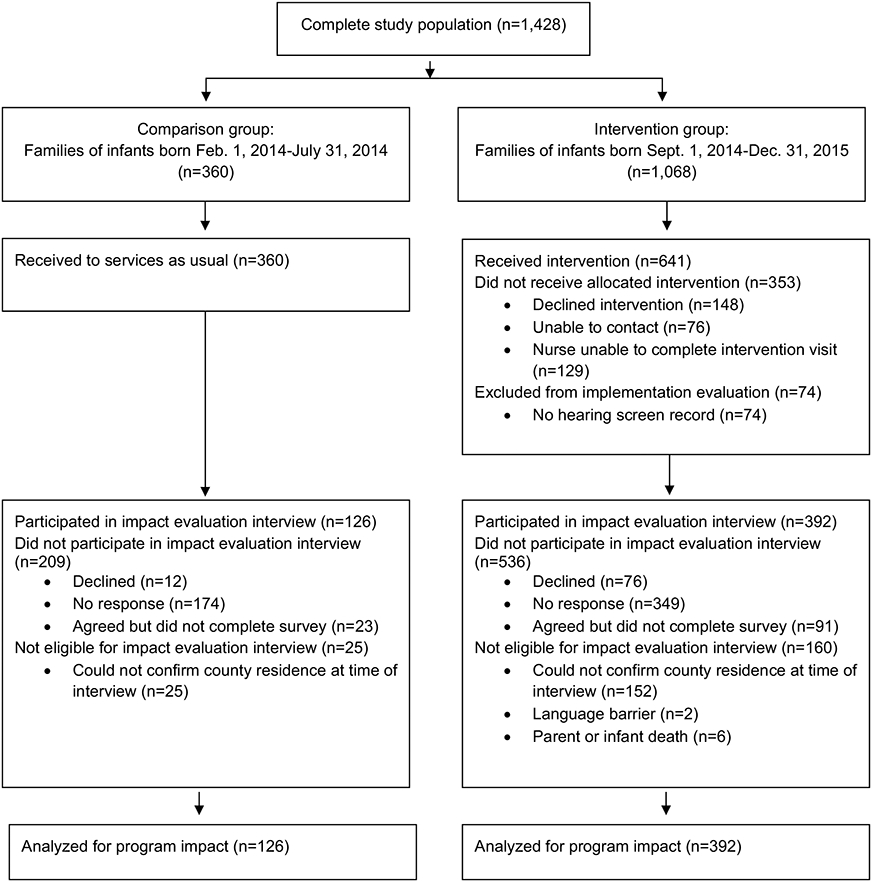
Flow diagram for Family Connects quasi-experimental study
Measures of Program Implementation
Scheduling and IHV completion rates were used to assess program reach. The nursing supervisor accompanied each home visiting nurse once per quarter to assess FC protocol fidelity across 62 required items and nurse-rater reliability in the rating of family risk. The supervisor and nurse independently rated the Family Support Matrix; reliability was calculated using Cohen’s Kappa (κ; Cohen, 1988), which accounts for chance agreement. Successful connections to community resources were measured through telephone contacts with the family four weeks after case closure.
Measures of Program Impact
Birth records provided baseline information on family demographics and infant medical risk at birth. A telephone survey when infants were 6 months old, completed by the birthing parent, collected information on family utilization of community resources, parenting and childcare, and parent and infant health and well-being.
Baseline Variables
Child characteristics included number of infant birth risks (range 0–3; birthweight < 2500 g, gestational age < 37 weeks, other birth complications, not specified), infant gender (0 = male, 1 = female), and infant age in months. Birthing parent and family characteristics included teen parent (age < 20; 0 = no, 1 = yes), minority race/ethnicity (0 = no, 1 = yes), parent Medicaid insurance at birth (0 = no, 1 = yes), parent education (range 1–8), multiple birth (0 = no, 1 = yes), and marital status (0 = single, 1 = married).
Community Services Utilization
Parents reported the total number of community resources utilized since birth (total community connections). Parents also reported on frequency of service use, total services currently used, and the helpfulness of the services (Durham Family Initiative, 2008).
Parenting and Childcare
Parents reported on use of non-parental childcare (0 = no, 1 = yes), and their positive parenting behaviors (7 items, e.g., “read books with infant”) and negative parenting behaviors (10 items, e.g., “shouted at infant”; Lounds et al., 2004; Straus et al., 1995), and beliefs about infant negative intentionality (e.g., “Can your baby do things on purpose to annoy you?”; Feldman & Reznick, 1996).
If the biological father was involved, birthing parents also reported on father-child relationship quality (10 items, e.g., “Hugs or shows physical affection toward child”), help with family work (4 items, e.g., “How often does he look after child?”), and financial support (6 items, e.g., father buys “child care items, such as diapers and baby wipes”; Center for Research on Child Wellbeing, 2008).
Infant Health and Well-being
Parents reported on current breastfeeding (0 = no, 1 = yes) and whether their infant most often slept on his/her back (0 = no, 1 = yes). Parents also reported on infant total emergency department (ED) visits, urgent care visits, and total overnights spent in hospital since their post-birth hospital discharge. These items were summed to measure infant total emergency care episodes.
Birthing Parent Health and Well-being
Parents reported on completion of their 6-week postpartum health check-up (0 = no, 1 = yes) and total emergency care episodes since their post-birth hospital discharge.
Parents completed the Edinburgh Postnatal Depression Scale (cut point > 10; Cox et al., 1987) and the Generalized Anxiety Scale (cut point > 5; Spitzer, et al., 2006) to screen for symptoms of depression and anxiety (0 = no, 1 = yes), respectively. Parents also completed a 12-item version of the Social Provisions Scale (Cutrona, 1984), measuring perceived social support.
Statistical Analysis Plan
Missing Data
All analyses were conducted in 2020 using STATA 14.2 (StataCorp, 2015). Twenty percent of participants had one or more missing values in baseline variables and outcomes. Results from Little’s test (Little & Rubin, 2014) suggest values were not missing completely at random (MCAR; X2(398) = 457.81, p < 0.05). Ten multiply imputed (MI) datasets were created, with missing values imputed from other baseline characteristics. Imputed data files were subjected to statistical tests, and estimates were merged (Garson, 2015; Little & Rubin, 2014).
Baseline Tests of Sample Equivalence
No differences in baseline characteristics were observed between the full birth population ( n = 1428) and full evaluation-eligible sample ( n = 1243) or between the full birth population ( n = 1428) and evaluation-participating sample ( n = 518) (Table 1). Within the evaluation-participating sample, intervention group families were more likely to be married (61.1% vs. 48.3%; p = 0.01).
Table 1.
Baseline sample characteristics for population and selected evaluation subsample groups
| Birth population vs. eligible & interviewed evaluation subsamples | Interviewed comparison vs. intervention subsamples |
||||
|---|---|---|---|---|---|
|
|
|
||||
| Birth population (n = 1428) Mean |
Eligible sample (n = 1243) Mean (p-value) |
Participating sample (n = 518) Mean (p-value) |
Comparison participating sample (n = 126) Mean |
Intervention participating sample (n = 392) Mean (p-value) |
|
| Infant birth characteristics | |||||
| Number of birth risks | 0.32 | 0.31 (0.78) | 0.31(0.80) | 0.33 | 0.30 (0.77) |
| Low birth weight, (%) | 10.71 | 10.14 (0.63) | 9.65 (0.50) | 10.32 | 9.44 (0.77) |
| Premature birth, (%) | 11.20 | 10.86 (0.78) | 10.81 (0.81) | 12.70 | 10.20 (0.43) |
| Any birth complications, (%) | 9.96 | 10.07 (0.92) | 10.44 (0.75) | 9.52 | 10.74 (0.70) |
| Infant female, (%) | 50.56 | 50.20 (0.85) | 51.74 (0.65) | 57.94 | 49.74 (0.11) |
| Infant age in months (M, SD) | – | – | – | 5.76, 1.12 | 5.86, 0.99 (0.33) |
| Birthing parent characteristics | |||||
| Multiple birth, (%) | 1.89 | 1.77 (0.82) | 2.12 (0.74) | 3.97 | 1.53 (0.10) |
| Mother medicaid at birth (%) | 62.41 | 60.35 (0.28) | 60.35 (0.41) | 67.46 | 58.06 (0.06) |
| Teen parent, (%) | 8.89 | 8.69 (0.85) | 9.27 (0.80) | 9.52 | 9.18 (0.91) |
| Mother education | 3.84 | 3.91 (0.23) | 4.02 (0.23) | 3.80 | 4.09 (0.07) |
| Mother is married, (%) | 44.74 | 46.82 (0.28) | 48.55 (0.14) | 38.89 | 51.66 (0.01) |
| Birthing parent race/ethnicity | |||||
| White, (%) | 47.20 | 49.48 (0.24) | 48.84 (0.52) | 46.03 | 49.74 (0.47) |
| Black, (%) | 39.99 | 38.54 (0.44) | 40.54 (0.83) | 42.06 | 40.05 (0.69) |
| Hispanic/Latinx, (%) | 9.87 | 9.25 (0.59) | 8.88 (0.51) | 9.52 | 8.67 (0.77) |
| Other, (%) | 2.94 | 2.74 (0.75) | 1.74 (0.14) | 2.38 | 1.53 (0.53) |
Column 2 is contrasted with column 1, with significance level in parentheses. Column 3 is contrasted with column 1, with significance level in parentheses. Column 5 is contrasted with column 4, with significance level in parentheses
Propensity Score Matching Analyses
Observed baseline differences were accounted for using propensity score matching (PSM) and estimating average treatment effects (ATE; d’Agostino, 1988). The propensity score, defined as the conditional probability of being treated given observed baseline characteristics, reduces multidimensional covariates to a one-dimensional score. This score balances baseline characteristics between groups, reducing bias in estimating treatment effects (Austin, 2011; d’Agostinao, 1988; Guo & Fraser, 2014). Propensity scores were calculated using a logistic model with treatment status as the dependent variable; covariates included the eight baseline characteristics noted above. A diagnostic test checked for covariate balance after observations between the two groups; PSM was successful in eliminating all baseline differences between groups. Next, PSM imputed the missing potential outcome for each subject from a similar subject that received the other treatment level. Finally, treatment effects were estimated for each outcome. Intervention effect sizes were calculated as (MeanIntervention–MeanComparison)/Average standard deviation.
Results
Family Connects Implementation
Recruitment and Participation
Overall, 994 FC-eligible birthing families were identified through hearing screen records in the four counties. Of these, 770 (77.5%) scheduled an IHV; among scheduled families, 641 (83.2%) completed the program (net completion = 64.5%). Among families completing the program, 33.2% were white, 35.7% were Black, 10.0% were Hispanic/Latinx, and 21.1% were other/multiracial; 69% received Medicaid, and 41% percent were married. The father or partner resided in home for 61.5% of families; 33.8% of resident fathers/partners were present for the IHV.
Fidelity
The nursing director accompanied the nurse on a home visit for 22 of 641 families (3.4%). Director-rated nurse adherence to the manualized protocol was 87.0% (range = 68.9%-95.1%), which was judged to be high. Inter-rater agreement on scoring of risk across all nurses was κ = 0.78, which is considered substantial (Cohen, 1988).
Assessment of Family Risk/Needs
Five of 641 families (0.8%) reported an emergency need requiring immediate intervention (rated as “4”). An additional 633 families (98.8%) reported at least one need requiring local services: 348 families (54.3%) had at least one rating of “3”, indicating significant risk best addressed by referral to community services; 285 (44.5%) had at least one “2” (but not “3” or “4”), indicating mild-to-moderate risk best addressed by brief nurse supportive guidance in-home. Only 3 (0.5%) families received lowest-need score (“1”) across all 12 factors.
Referrals to Community Resources
Follow-up contacts four weeks after case closure were completed with 262 families; these families reported outcomes on a total of 326 referrals to community services (representing 48.9% of all 667 nurse-family referrals made across all 641 participating families). Families reported that a successful connection was established for 85.9% (280/326) of referrals, and services had been received for 81.0% (264/326).
Impact Evaluation
Community Service Utilization
As shown in Table 2, families assigned to intervention group (herein called FC families) reported more total community connections since birth (95% Confidence Interval (CI) = 0.22, 0.80; effect size = 0.20), and reported using those services more frequently (95% CI = 0.53, 3.05; effect size = 0.16) than families assigned to the control group. No group differences were observed in total services being used at the time of the interview or the perceived helpfulness of services utilized.
Table 2.
Propensity score matching analyses to test impact of family connects on community resources and supports, parenting, and child care: intervention-eligible vs. comparison families (n = 518 children)
| Intervention (n = 392) |
Comparison (n = 126) |
Average Treatment Effects | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Variable | Mean | SD | Mean | SD | Difference | s.e | p-value | 95% CI | |
| Community resources & supports | |||||||||
| Total number of community connections | 5.66 | 2.69 | 5.15 | 2.50 | 0.51 | 0.15 | < 0.01 | 0.22 | 0.80 |
| Frequency of community service use | 23.03 | 11.59 | 21.24 | 10.39 | 1.79 | 0.64 | 0.01 | 0.53 | 3.05 |
| Total services used now | 4.55 | 2.42 | 4.53 | 2.29 | 0.02 | 0.13 | 0.88 | −0.24 | 0.28 |
| Helpfulness of community services | 3.72 | 0.41 | 3.74 | 0.38 | −0.02 | 0.02 | 0.33 | −0.07 | 0.02 |
| Mother parenting beliefs & behaviors | |||||||||
| Mother positive parenting behaviors | 4.56 | 0.52 | 4.53 | 0.48 | 0.02 | 0.03 | 0.42 | −0.04 | 0.08 |
| Mother negative parenting behaviors | 0.07 | 0.17 | 0.07 | 0.11 | 0.00 | 0.01 | 0.71 | −0.01 | 0.02 |
| Mother negative intentionality beliefs | 0.18 | 0.36 | 0.18 | 0.32 | 0.00 | 0.02 | 0.96 | −0.04 | 0.04 |
| Father involvement | |||||||||
| Father—infant relationship quality (n = 347) | 2.36 | 0.45 | 2.26 | 0.44 | 0.11 | 0.03 | < 0.01 | 0.05 | 0.16 |
| Father help with family work (n = 347) | 2.50 | 0.52 | 2.34 | 0.54 | 0.15 | 0.03 | < 0.01 | 0.09 | 0.22 |
| Father financial support for infant (n = 347) | 2.10 | 0.87 | 2.06 | 0.83 | 0.04 | 0.05 | 0.46 | −0.06 | 0.14 |
| Child care | |||||||||
| Proportion using non-parental childcare | 55.32% | 0.50 | 61.78% | 0.49 | −6.46% | 0.03 | 0.03 | −0.12 | 0.00 |
Multiple imputation was applied to address missing data (n = 10). Infant birth risk score (0–3), Infant age in months, infant gender (1 = Girl), twin (1 = Yes), parent medicaid status at birth (1 = Yes), teenage parent (1 = Yes), family minority race/ethnicity (1 = Yes), parent education (1–8), and marital status (1 = Yes). Difference intervention-eligible—comparison
Parenting and Childcare
Birthing parents did not differ by group in their self-reported positive or negative parenting behaviors or in their beliefs regarding infant negative intentionality. FC parents, however, did report greater father-infant relationship quality (95% CI = 0.05, 0.16; effect size = 0.22) and father help with family work (95% CI = 0.09, 0.22; effect size = 0.30). No differences were observed in paternal financial support for the infant. FC families were less likely to report using non-parent childcare relative to comparison groups families (55.32% vs. 61.78%, p = 0.03) (see Table 2). FC families were 11% more likely to report that the infant slept on his/her back relative to comparison group families (72.99% vs. 65.81%, p = 0.01). No group differences were observed for current breastfeeding (see Table 3).
Table 3.
Propensity score matching analyses to test impact of Family Connects on parent and infant health and well-being: intervention vs. comparison families (n = 518 children)
| Intervention (n = 392) |
Comparison (n = 126) |
Average treatment effects | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Variable | Mean | SD | Mean | SD | Difference | s.e | p-value | 95% CI | |
| Infant emergency healthcare | |||||||||
| Total number of emergency care episodes | 1.30 | 2.10 | 1.90 | 3.13 | −0.61 | 0.17 | < 0.01 | −0.93 | −0.28 |
| Number of ED and urgent care visits | 1.20 | 1.95 | 1.74 | 2.94 | −0.55 | 0.16 | < 0.01 | −0.85 | −0.24 |
| Number of overnights in hospital | 0.10 | 0.54 | 0.16 | 0.77 | −0.06 | 0.04 | 0.16 | −0.14 | 0.02 |
| Infant health & well-being | |||||||||
| Infant sleeps on back | 72.99% | 0.44 | 65.81% | 0.47 | 0.07% | 0.03 | 0.01 | 0.02 | 0.13 |
| Infant currently breastfeeding | 31.01% | 0.46 | 28.59% | 0.45 | 0.02% | 0.03 | 0.37 | −0.03 | 0.08 |
| Birthing parent emergency healthcare | |||||||||
| Total number of emergency care episodes | 1.02 | 2.25 | 0.79 | 1.86 | 0.23 | 0.13 | 0.08 | −0.03 | 0.49 |
| Number of ED and urgent care visits | 0.98 | 2.16 | 0.71 | 1.58 | 0.28 | 0.12 | 0.02 | 0.04 | 0.51 |
| Number of overnights in hospital | 0.04 | 0.24 | 0.08 | 0.55 | −0.05 | 0.03 | 0.07 | −0.10 | 0.00 |
| Birthing parent health & well-being | |||||||||
| Parent received 6-week postpartum check-up | 93.13% | 0.25 | 95.29% | 0.21 | −0.02% | 0.01 | 0.14 | −0.05 | 0.01 |
| Parent clinical depression or anxiety | 25.17% | 0.43 | 29.40% | 0.46 | −4.23% | 0.03 | 0.13 | −0.10 | 0.01 |
| Parent social support | 3.41 | 0.53 | 3.34 | 0.51 | 0.07 | 0.03 | 0.02 | 0.01 | 0.14 |
Multiple imputation was applied to address missing data (n = 10). Infant birth risk score (0–3), infant age in months, infant gender (1 = Girl), twin (1 = Yes), parent medicaid status at birth (1 = Yes), teenage parent (1 = Yes), family minority race/ethnicity (1 = Yes), parent education (1–8), and marital status (1 = Yes). Difference intervention-eligible—comparison
Infant Health and Well-being
Relative to comparison group families, FC families reported less total infant emergency medical care (95% CI = −0.93, −0.28; effect size = 0.23; see Table 3). FC families had fewer infant ED and urgent care visits (95% CI = −0.85, −0.24; effect size = 0.22) but not fewer total infant overnights in the hospital.
Birthing Parent Health and Well-being
No group differences were found in total emergency care utilization for birthing parents (see Table 3). FC parents reported making more ED and urgent care visits for themselves than did comparison group parents (95% CI = 0.04, 0.51; effect size = 0.14) and (non-significantly) fewer hospital overnight stays. FC parents reported greater perceived social support relative to comparison group parents (95% CI = 0.01, 0.14; effect size = 0.13). No differences were observed for maternal 6-week postpartum health-check completion or endorsed symptoms of depression or anxiety.
Conclusions for Practice
Results from this quasi-experimental field trial indicate that FC effectively engages families living in high-poverty rural counties during the postpartum period with broad reach and high program fidelity, leading to positive population impacts on family health and well-being. Implementation findings indicate FC had broad community reach, high nurse reliability and fidelity to the manualized protocol, and nurse-family referral connection rates that exceeded rates observed in prior trials (Dodge et al., 2014, 2019). The findings provide compelling evidence that FC can be disseminated through rural public health departments with high quality. The high completion rate (65% of all eligible families) suggests that the FC is well suited for rural contexts. Considering that limited access to services and rural families’ preference for services that are well integrated with existing networks can be barriers to service uptake (e.g., Warren & Smalley, 2014), multiple program design elements may support high uptake, including (1) delivering in-home services at a time where families have near universal needs for support; (2) staffing by local community members; (3) working collaboratively to connect families with matched community resources and services that are both needed and desired; and (4) maintaining local advisory boards to support an ongoing community voice in program implementation.
Impact findings indicate 10 (45%) significant effects across 22 outcomes examined. FC was effective in the proximal goal of improving family connections to community resources and resource utilization. FC eligibility also predicted less infant utilization of emergency medical care, greater use of “back to sleep” techniques, greater paternal involvement with their children and in family work, and greater parent overall social support.
Effect sizes are modest but comparable to previously reported results from RCTs in Durham, NC (author citations). Importantly, multiple observed effects are consistent with prior FC RCTs, including increased community connections, increased father-infant relationship quality, and reduced infant emergency medical care use. The current findings expand existing evidence on model efficacy and suggest FC can be disseminated without decrements in overall efficacy and impact in rural settings. Positive impact suggests that public investments in care systems combing identification and alignment of sources and services with universal screening and family-centered referrals is a promising and affordable approach to promoting population health in rural communities.
Limitations
Although the investigators sought to maximize scientific rigor by incorporating a “blinded” impact evaluation and by including families based on “intent-to-treat” without regard to FC participation, the evaluation was a quasi-experiment and not an RCT. Although baseline comparisons indicate that the evaluation sample was representative of the broader population and that participation was not biased between comparison and intervention groups, it is possible that observed intervention effects were a result of unmeasured differences in third variables. Population-level healthcare delivery patterns may have changed over the study period; however, no policy, macroeconomic, or healthcare changes were reported during this time. Finally, all outcomes examined are based on parent self-report. While there is no reason to suspect systematic bias in responses across study groups, accuracy of self-report can be affected by factors such as recall bias or social desirability.
A strength of the current study is the replication of multiple effects observed in prior FC RCTs. However, some effects were not replicated for these rural communities. Most of these non-replications clustered around parent postpartum health and healthcare, including postpartum depression and anxiety and 6-week postpartum health check completion. Unexpectedly, FC birthing parents also reported greater utilization of ED and urgent care and services. As a part of the protocol, FC nurses educated parents about the importance of seeking healthcare for themselves and their infants and attempted to connect parents with mental and physical health needs to appropriate community services. Perhaps a scarcity of mental health services and primary care providers in these communities resulted in FC parents increasing their use of urgent care and ED services. This finding highlights a potential limitation of a systems approach in the context of low-resourced communities and may suggest the need for further refinement of the FC protocol, innovation in the delivery of mental health and primary care services to rural communities (e.g., telehealth), and more comprehensive evaluation of links between FC and maternal health in future evaluations.
Conclusion
The findings demonstrate that a community-wide, postnatal home visiting program can be implemented in rural communities characterized by chronic economic disadvantage with broad population reach, high quality, and population impact on infant and family health and well-being. For rural populations in which community resources are often limited and geographically dispersed, universal postpartum screening and referral approaches, like Family Connects, can successfully engage and connect families to matched sources of support during a time when many families experience needs for support, making such programs an efficient and worthy investment.
Significance.
What is already known on this subject?
Findings from two randomized-controlled trials (RCT) in Durham, NC demonstrated that Family Connects, a community-wide postpartum nurse home visiting program, can be accomplished with high-quality implementation and positive impact on family health and well-being.
What this study adds?
Family Connects can be implemented with high quality and broad reach in high-poverty rural communities with evidence of greater community connections and social support, greater infant safe sleep, and less infant emergency medical care through age 6 months. Family Connects represents a promising approach to promoting community-wide postpartum family well-being in rural communities.
Acknowledgements
The authors acknowledge the contributions of many staff members in implementing Family Connects and its evaluation. The authors thank Dr. Nissa Towe-Goodman and three anonymous reviewers for their helpful comments on previous versions of this manuscript. Funding for the evaluation was provided by The North Carolina Department of Health and Human Services, The Duke Endowment, and grant R01HD069981 from the Eunice Kennedy Shiver National Institute for Child Health and Human Development. The design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; and decision to submit the manuscript for publication are the responsibility of the authors with no influence by any funder. The views expressed are those of the authors and do not necessarily reflect the views of funders. The first author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Conflict of interest The authors acknowledge that they are disseminating the Family Connects program and report no other conflict of interest in the study reported here.
Disclosures The authors acknowledge they have no financial interest in the findings reported in this manuscript. They occasionally give lectures about the research for a modest stipend.
References
- Austin PC (2011). An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research, 46(3), 399–424. 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman Benjamin, W., Dodge KA, Bai Y Murphy RA, & O’Donnell K. (2021). Effect of a universal postpartum nurse home visiting program on child maltreatment and emergency medical care at 5 years of age. JAMA Network Open 4(7), e2116024. 10.1001/jamanetworkopen.2021.16024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RL, & Rounds L (1995). Conjoint screening questionnaires for alcohol and drug abuse: Criterion validity in a primary care practice. Wisconsin Medical Journal, 94(3), 135–140. [PubMed] [Google Scholar]
- Center for Research on Child Wellbeing (2008). The fragile families and child wellbeing study (survey of new parents): Mothers' baseline survey public use version. Retrieved June 4, 2009, from: http://www.fragilefamilies.princeton.edu/documentation.asp
- Cohen J (1988). Statistical power for the behavioral sciences (2nd ed.). Lawrence Erlbaum. [Google Scholar]
- Congressional Research Service (2018). Maternal, infant, and early childhood home visiting (MIECHV) program: Background and funding. Retrieved February 9, 2020, from: https://fas.org/sgp/crs/misc/R43930.pdf
- Cox JL, Holden JM, & Sagovsky R (1987). Detection of postnatal depression: Development of the 10-item Edinburgh postnatal depression scale. British Journal of Psychiatry, 150(6), 782–786. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Cutrona C (1984). Social support and stress in the transition to parenthood. Journal of Abnormal Psychology, 93(4), 378–390. 10.1037/0021-843X.93.4.378 [DOI] [PubMed] [Google Scholar]
- d’Agostino RB (1988). Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine, 17(19), 2265–2281. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Goodman WB, Bai Y, Murphy RA, & O’Donnell K (in press). Maximizing the return on investment in early childhood home visiting through enhanced eligibility screening. Child Abuse & Neglect. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Goodman WB, Murphy RA, O’Donnell K, Sato J, & Guptill S (2014). Implementation and randomized controlled trial evaluation of universal postnatal nurse home visiting. American Journal of Public Health, 104(S1), S136–S143. 10.2105/AJPH.2013.301361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Goodman WB, Bai Y, O’Donnell K, & Murphy RA (2019). Effect of a community agency–administered nurse home visitation program on program use and maternal and infant health outcomes. JAMA Network Open, 2(11), e1914522. 10.1001/jamanetworkopen.2019.14522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan A, Portilla XA, Filene JH, Crowne SS, Hill CJ, Lee H, & Knox V (2018). Implementation of evidence-based early childhood home visiting: Results from the mother and infant home visiting program evaluation. OPRE Report 2018–76A. Retrieved May 10, 2019, from: https://www.acf.hhs.gov/sites/default/files/opre/mihope_implementation_report_2018_10_26_508b.pdf [Google Scholar]
- Durham Family Initiative. (2008). DFI cross-site interview. Center for Child and Family Policy, Duke University. [Google Scholar]
- Feldman R, & Reznick JS (1996). Maternal perception of infant intentionality at 4 and 8 months. Infant Behavior and Development, 19(4), 483–496. 10.1016/S0163-6383(96)90008-9 [DOI] [Google Scholar]
- Garson GD (2015). Missing values analysis and data imputation. Statistical Associates Publishers. [Google Scholar]
- Green BL, Tarte JM, Sanders MB, & Waller MS (2016). Testing the effectiveness of health families America in an accredited statewide system: Outcomes and cost-benefits of the health families Oregon program—final project report. Portland State University and NPC Research. [Google Scholar]
- Guo S, & Fraser MW (2014). Propensity score analysis: Statistical methods and applications (Vol. 11). SAGE Publications. [Google Scholar]
- Harris JK, Beatty K, Leider JP, Knudson A, Anderson BL, & Meit M (2016). The double disparity facing rural local health departments. Annual Review of Public Health, 37, 167–184. 10.1146/annurev-publhealth-031914-122755 [DOI] [PubMed] [Google Scholar]
- Kendrick D, Elkan R, Hewitt M, Dewey M, Blair M, Robinson J, Williams D, & Brummell K (2000). Does home visiting improve parenting and the quality of the home environment? A systematic review and meta-analysis. Archives of Disease in Childhood, 82(6), 443–451. 10.1136/adc.82.6.443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozhimannil KB, Interrante JD, Henning-Smith C, & Admon LK (2019). Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health Affairs, 38(12), 2077–2085. 10.1377/hlthaff.2019.00805 [DOI] [PubMed] [Google Scholar]
- Little RJ, & Rubin DB (2014). Statistical analysis with missing data (Vol. 333). Wiley. [Google Scholar]
- Lounds JJ, Borkowski JG, & Whitman TL (2004). Reliability and validity of the mother-child neglect scale. Child Maltreatment, 9(4), 371–381. 10.1177/1077559504269536 [DOI] [PubMed] [Google Scholar]
- Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, Cunningham TJ, Khan LK, Caraballo RS, Holt JB, Eke PI, & Giles WH (2017). Health-related behaviors by urban-rural county classification—United States, 2013. MMWR Surveillance Summaries, 66(5), 1–8. 10.15585/mmwr.ss6605a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollard E, Hudson DB, & Pullen C (2016). An integrative review of postpartum depression in rural US communities. Archives of Psychiatric Nursing, 30(3), 418–426. 10.1016/j.apnu.2015.12.003 [DOI] [PubMed] [Google Scholar]
- Probst JC, Barker JC, Enders A, & Gardiner P (2018). Current state of child health in rural America: How context shapes children’s health. Journal of Rural Health, 34(suppl 1), s3–s12. 10.1111/jrh.12222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin R (2018). Declining numbers of rural U.S. hospitals. JAMA, 320(20), 2067. 10.1001/jama.2018.18506 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata statistical software: Release 14. StataCorp LP. [Google Scholar]
- Straus M, & Douglas E (2004). A short form of the revised conflict tactics scale, and typologies for severity and mutuality. Violence and Victims, 19(5), 507–520. 10.1891/vivi.19.5.507.63686 [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, & Runyan D (1995). The parent-child conflict tactics scales (PCCTS), form A. Family Research Laboratory, University of New Hampshire. [Google Scholar]
- U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau (2015). The health and well-being of children in rural areas: A portrait of the nation, 2011–2012. Retrieved February 9, 2020, from: https://mchb.hrsa.gov/nsch/2011-12/rural-health/pdf/rh_2015_book.pdf
- Warren JC, & Smalley KB (Eds.). (2014). Rural public health: Best practices and preventive models. Springer. [Google Scholar]
- Whiteside-Mansell L, Bradley R, Conners N, & Bokony P (2007). The family map: Structured family interview to identify risks and strengths in head start families. NHSA Dialog, 10(3–4), 189–209. 10.1080/15240750701742239 [DOI] [Google Scholar]


