Abstract
During the immediate period following psychiatric hospitalization, adolescents are at increased risk for suicide attempts and re-hospitalization. Because most adolescents return to school during this time, school-related experiences are important considerations during the transition from inpatient hospitalization. This study sought to understand how adolescent perceptions of school may change following hospitalization, and how these changes may predict recovery from a suicide-related crisis. Participants included 155 adolescents (Mage=15.2 years; 68.6% female, 65.4% White; 14.7% Hispanic/Latinx; grades 7–12) hospitalized for a suicide-related crisis assessed 3-weeks and 6-months following discharge. Results from Latent Change Score models indicated a worsening of perceptions of teacher relationships (mean change [Δ]=1.52), connectedness to learning (Δ=1.55), parent involvement (Δ=1.82), and academic satisfaction (Δ=1.34), as well as higher frequency of perceived bullying victimization (Δ=0.71) following hospitalization. Poorer perceptions of teacher relationships and higher frequency of perceived bullying victimization during hospitalization (β = 0.31 and 0.34), as well as worsening changes of teacher relationships and increased frequency of perceived bullying victimization following hospitalization (β = 0.48 and 0.41) were associated with higher levels of suicidal ideation severity 3-weeks following discharge. Poorer and worsening perceptions of teacher relationships were associated with higher levels of suicidal ideation intensity at 3-weeks (β = 0.37 and 0.54). Poorer perceptions of connectedness to learning during hospitalization emerged as a significant predictor of higher levels of suicidal ideation intensity 6-months following hospitalization (β = 0.20). Results reinforce the importance of fostering positive adult relationships and preventing bullying both prior to and immediately following psychiatric hospitalization.
Keywords: Suicide-Related Behaviors, Academic Satisfaction, Parent Involvement, Teacher Relationships, Connectedness to Learning
Introduction
Formulations about suicide-related risk and ongoing treatment provided to individuals with suicide-related thoughts and behaviors (STB) are considered to be among the most stressful aspects of clinical practice, wrought with ethical challenges and taking a heavy toll on clinicians’ emotions (Jobes et al., 2008; Rothes et al., 2014). School psychologists, who are often expected to provide tertiary interventions to students experiencing a suicide-related crisis, are among the professionals facing these challenges (Brown et al., 2018; Erps et al., 2020). In addition to their role in the risk formulation process, school psychologists may also face decisions about how best to support adolescents as they return to school following hospitalization for a suicide-related crisis (Marraccini et al., 2019).
Although some hospitalized youth have described feeling a sense of safety and relief upon hospitalization, they have also expressed strong negative emotional reactions to psychiatric care, such as fear, anxiety, and shock (Haynes et al 2011; Moses, 2011; Salamone-Violi et al., 2015). Following hospital discharge, these youth must then return to their homes and schools, where they are expected to reacclimate to typical routines and also engage in intensive treatment (Prinstein et al., 2008; Savina et al., 2014). Returning students must manage their mental health symptoms in school, while also addressing work remediation, navigating ongoing social stressors, and facing perceived stigma related to their mental health (Marraccini & Pittleman, 2021; Preyde et al., 2018; Tougas et al., 2019; White et al., 2017). During this period, youth are also at high risk of making a suicide attempt or for being rehospitalized for a mental health crisis (Chung et al., 2017).
Thus, the referral process for intensive care of adolescents with suicide-related crises, which commonly occurs in school settings (Crepeau-Hobson, 2013; Soto et al., 2009), marks only the beginning of the ongoing school-related supports and services that may be needed by adolescents experiencing suicide-related crises. Unfortunately, limited research has addressed how schools can play a role in recovery from suicide-related crises (Marraccini et al., 2019). The present study aimed to contribute to the gap in this literature by (a) exploring adolescent perceptions of school during hospitalization and 3-weeks following hospital discharge and (b) examining how these perceptions and changes in perceptions predicted subsequent suicidal ideation. Findings could inform school-wide and individual interventions aimed at supporting recovery from suicide-related crises, helping to make the transition from hospitals to schools a little bit less stressful for these youth.
Suicide-Related Risk and Recovery
Suicide is the second leading cause of death among non-Hispanic White, Asian American, and American Indian adolescents, and the third leading cause of death in Hispanic and non-Hispanic Black adolescents (ages 13–18; Centers of Disease Control and Prevention [CDC], 2019a; 2019b). Each year, approximately 7–8% of high school students attempt suicide (CDC, 2013) and 1.8% are hospitalized due to suicide-related thoughts and behaviors (STB; Plemmons et al., 2018). Schools are a common referral source for intensive care for adolescents with a suicide-related crisis (Crepeau-Hobson, 2013; Soto et al., 2009) and also a primary environment adolescents return to following hospital discharge (Savina et al., 2014).
During the immediate period following psychiatric hospitalization for STB, adolescents are at increased risk for making a suicide attempt (Chung et al., 2017; Goldston et al., 2001; Wolff et al., 2018). Although adolescents discharged from inpatient settings would likely benefit from immediate, intensive interventions that focus on relapse prevention and allow for close monitoring (Goldston et al., 1999; 2001; Prinstein et al., 2008), post-hospital treatment utilization remains low (James et al., 2010; Spirito et al., 2011). Therefore, adolescents return to school at high-risk for suicide, with or without ongoing supports outside of schools.
Adolescents also face myriad of issues related to their return to school, such as ongoing academic problems, social difficulties, missed course work, and extensive absences. Returning adolescents have expressed concerns about managing symptoms at school and reacclimating to school routines (Preyde et al., 2018). More recent work (Marraccini & Pittleman, 2021) illustrates adolescents’ desire to strengthen school adult relationships following hospital discharge, and the importance of improving the school’s psychosocial climate. School and mental health providers have shared similar concerns, emphasizing the need to reduce stigma around mental health problems and concerns about in-school behaviors upon return (Clemens et al., 2010, 2011; Simon & Savina, 2010).
With exception (King et al., 2019; Luukkonen et al., 2009; Tossone et al., 2014), few studies have explored school-related predictors of STB in clinical samples. In an exploration of children and adolescents seen in a psychiatric intake response center, youth with a history of peer victimization and learning difficulties (e.g., motivation problems, having a learning disability) were found to be between 4–5 times as likely to return to a pediatric psychiatric center within two-years compared to youth without such histories (Tossone et al., 2014). Specific school factors, such as receiving special education services, difficulty with attention, concentration, or motivation, and bullying experiences, were linked to increased risk for re-hospitalization (Tossone et al., 2014). In another study (King et al., 2019) that surveyed over 2,000 adolescents seen in the emergency department, school connectedness emerged as a key predictor of suicide attempts three-months post-hospitalization, even after accounting for more common predictors (e.g., history of STB). Findings from univariate analysis also supported bullying as a significant predictor of STB; however, effects of bullying did not remain significant after accounting for other predictors (King et al., 2019). Finally, the only study to explore a clinical sample of youth hospitalized in an acute psychiatric hospital was conducted in Finland by Luukkonen and colleagues (2009). Among a sample of 508 Finish adolescents, history of bullying experiences was associated with increased odds for lifetime history of having made a suicide attempt in girls (but not boys). Findings were based on retrospective self-report and did not explore outcomes longitudinally.
Negative school experiences can serve as a trigger or vulnerability for STB among adolescents. The cognitive-behavioral model of adolescent suicide posits that maladaptive cognition, behavior, and affective responses to stressors interact to trigger suicidal behavior among youth with predisposed vulnerabilities (Spirito et al., 2012), inclusive of school problems. The interpersonal theory of suicide proposes that the most dangerous form of suicidal behavior stems from an experienced state of thwarted belongingness (i.e., loneliness, social isolation) and perceived burdensomeness to others, with hopelessness about these interpersonal experiences intensifying the desire for suicidal behavior (Van Orden et al., 2010). Here, school can serve as a protective factor, increasing students’ sense of belonging when feeling a connection to school members (King et al., 2019), but can also exacerbate risk when students feel unwelcome or face difficult school experiences, such as academic failure (Walsh & Eggert, 2007) or bullying (Luukkonen et al., 2009).
Research conducted with general school populations suggests a significant association between suicide and school-related experiences (e.g., academics, bullying, school connectedness; Marraccini & Brier, 2017; Walsh & Eggert, 2007; van Geel et al., 2021), but few studies have explored the potential for school risk and protective factors to influence recovery from a suicide-related crisis. Individuals with a history of self-injury, attempts, or exposure to suicidal behavior are significantly more likely to make a suicide attempt (Van Orden et al., 2010), underscoring the importance of considering these school-related factors in recovery following psychiatric hospitalization for STB. To our knowledge, no studies have addressed changes in perceptions of school during and following hospitalization as predictors of adolescent recovery from STB.
School-Related Predictors of Suicide-Related Thoughts and Behaviors
Following an ecological systems theory, the potential for schools to influence recovery from STB is extensive. Bronfenbrenner’s (1979) ecological model proposes a transactional relationship between environment and development, making schools an important context for understanding adolescent social-emotional growth. For example, both school connectedness and positive school relationships have long been advocated as important influencers of health and development (Blum & Libbey, 2004; Whitlock et al., 2014). Multiple studies highlight the potential for school connectedness to play a protective role against STB (Marraccini & Brier, 2017), with teacher relationships measured alone (McNeely & Falci, 2004) and also as a component within school connectedness (Cornell & Huang, 2016; Young et al., 2011) linked to reductions in STB. For example, using the National Longitudinal Study of Adolescent Health data set, McNeely and Falci (2004) found that adolescents endorsing items related to teacher caring were less likely to report STB over a one-year period.
Parent involvement in education has also been found to relate to lower rates of STB in racially and ethnically diverse middle school students (Wang et al., 2019), and has been shown to negatively correlate with depression (Wang & Sheikh-Khalil, 2014). More broadly, parent involvement in school may help foster positive social, emotional, and academic outcomes across childhood and adolescence (Reinke et al., 2019) and appears to promote healthy student-teacher relationships (Cheuang, 2019). Because parent-adolescent connectedness has been widely supported as a protective factor against suicide attempts (Kuramoto-Crawford et al., 2017), parent involvement in schools could serve as another protective factor against suicide during recovery from hospitalization. Preliminary support for the importance of parent involvement in the school re-entry process following psychiatric hospitalization has been supported in qualitative work focused on adolescent perceptions (Marraccini & Pittleman, 2021), but we are unaware of studies that have addressed its influence on recovery.
The potential for academic difficulties to exacerbate risk, and conversely, academic successes to serve as a protective factor against STB, has been explored in numerous community samples of adolescents (Hall et al., 2018; Whaley & Noel, 2013). Lower levels of academic motivation are also significantly related to reporting having made a suicide attempt (Flouri & Buchanan, 2002). Difficulties with academics have been identified by school and mental health providers as a primary stressor for adolescents reintegrating into schools (Clemens et al., 2010); however, no research has explored satisfaction of academics or connectedness to learning as a facilitator for recovery in adolescents struggling with suicidal urges.
Finally, a vast literature supports the negative relationship between bullying victimization experiences and STB in general school-aged populations (e.g., van Geel et al., 2014; Holt et al., 2015), with a recent meta-analysis supporting a significant association between victimization and suicidal ideation over time (van Geel et al., 2021). Bullying victimization also appears to serve as a risk factor for STB across diverse student groups, including racial and ethnic minoritized and lesbian, gay, bisexual, transgender, queer or questioning students (Hatchel et al., 2019; Marraccini et al., 2021). Although a few studies have explored how bullying may predict STB in clinical samples (Luukkonen et al., 2009; Tossone et al., 2014), none have exclusively focused on youth hospitalized for a suicide-related crisis.
The Present Study
Considering the potential for school-related factors to influence recovery from STB and the minimal research focused on school perceptions during and following hospitalization, the current study aimed to fill a significant gap in the literature to inform school-based suicide prevention targeting this critical high-risk period for youth. First, we aimed to uncover if perceptions of teacher relationships, connectedness to learning, parent involvement, academic satisfaction, and bullying victimization changed from hospitalization to 3-weeks following hospital discharge. We hypothesized that there would be significant changes in perceptions of each school construct across timepoints. Second, we explored the relationship between changes in perceptions of teacher relationships, connectedness to learning, parent involvement, academic satisfaction, and bullying victimization collected retrospectively following hospitalization with subsequent severity (e.g., presence of specific plans, intent to act on them) and intensity (e.g., how frequently thoughts occur, how long thoughts last) of suicidal ideation assessed at 3-weeks and 6-months post-discharge. We hypothesized that changes reflecting deterioration of perceptions of each school construct would significantly relate to higher severity and intensity of self-reported suicidal ideation at each time-point. Finally, for our third aim, we conducted a joint analysis of the most salient school-related predictors of severity and intensity of suicidal ideation at 3-weeks and 6-months following discharge after accounting for depressive symptoms. By examining how adolescent perceptions of teacher relationships, connectedness to learning, parent involvement, academic satisfaction, and bullying victimization change during this critically high-risk time, findings can inform the development of practical in-school supports and interventions to prevent suicide.
Method
Adolescents hospitalized for STB were recruited as part of a larger study examining affect dysregulation and social context to predict recovery from suicidal crises (Nugent et al., under review). Because school-related measures addressing school climate and bullying experiences were added partway into recruitment, only data collected from a subsample of participants are presented here. Participants were recruited following admission to a psychiatric inpatient hospital located in the northeast of the US. Following informed consent and assent procedures, adolescents completed a battery of self-report measures related to affect, health, and environment. Adolescents also participated in clinical interviews to assess presence, frequency, and severity of STB at three time-points: during hospitalization (baseline), and 3-weeks and 6-months post-hospital discharge. Although not the focus of the current study, daily assessments measuring affect and health risk behaviors deployed on a smartphone were collected over the 3-weeks following discharge. Adolescents and parents received payment to reimburse their time. Study procedures were approved by hospital Institutional Review Boards.
Participants
Participants for this study consisted of 155 adolescents hospitalized for STB completing school-related measures added to the larger study (n=194) partway through study implementation. Of these, 152 and 155 completed procedures at 3-weeks and 6-months, respectively. Eligibility criteria for the larger study included (1) past-month STB verified by interview; (2) aged 13–18; (3) ability to speak, read and understand English; and (4) comfort with the use of smartphone technology related to aims of the larger study. Adolescents with current psychotic symptoms, developmental delay or pervasive development disorder, or substance use interfering with participation were excluded.
Measures
Adolescents completed a battery of self-report measures and interviews at three time-points: hospitalization, and 3-weeks and 6-months following hospital discharge.
Demographic Characteristics
Demographic variables obtained during hospitalization included sex assigned at birth (female, male), gender identity recoded to identify gender diversity (cisgender, gender minoritized), race (White, Black/African American, American Indian/Alaska Native, Asian, Native Hawaiian/Other Pacific Islander, multiple races), ethnicity (Hispanic, not Hispanic), grade in school (7th-12th), and age at enrollment (13–18).
Depression
Self-reported depressive symptoms were measured with the 20-item Center for Epidemiological Studies Depression Scale for Children (CES-DC; Radloff, 1977) during hospitalization. Participants rate how frequently each item applied to them on a 4-point scale ranging from 0 (not at all) to 3 (a lot of the time) over the past two weeks. The CES-DC has been demonstrated to have adequate internal reliability for clinical and nonclinical children and adolescent samples (Stockings et al., 2015). A mean summary score was calculated and used to control for baseline depressive symptoms in final models and demonstrated adequate internal reliability (ω=.92).
Suicidal Ideation
The Columbia-Suicide Severity Rating Scale (C-SSRS; Posner et al., 2011) was administered to assess STB during the follow-up visits, representing (1) the time period between hospital discharge and approximately 3-weeks following discharge; and (b) the month prior to the 6-month follow-up visit. The psychometric properties of the C-SSRS for measuring presence, severity, and intensity of STB are well established (Posner et al., 2011). For this study, we used two suicidal ideation summary scores: severity (ranging from 0–5), which reflects different types of ideation and intention to act; and intensity (ranging from 0–25), indicating length, frequency, and difficulty of controlling suicidal ideation (see Supplementary materials for details about each score). We selected measures of both severity and intensity to account for the complexity of suicidal ideation, rather than calculating presence of suicidal ideation alone, and because each are considered significant risk factors for suicide attempts (Horwitz et al., 2015).
School-Related Variables
School-related measures included the Adolescent Peer Relations Instrument (APRI; Parada et al., 2005) and the School Climate Measure (SCM; Zullig et al., 2015). Participants completed school-related measures during hospitalization (reporting retrospectively on school experiences before hospitalization) and 3-weeks following discharge. The APRI measures verbal, physical, and social forms of bullying. The APRI has demonstrated discriminant validity over time (Marsh et al., 2011) and strong internal consistency (Parada et al., 2005). For the present study, only verbal and social forms of bullying were included, and we calculated a total bullying victimization score with all of the victimization items.
The SCM is a comprehensive self-report measure of school climate that has been validated for use with middle and high school students. The SCM yields up to 10 factors or subscales, with previous research supporting adequate internal consistency across individual components (Zullig et al., 2015). Specific subscales were selected for the current study based on previous work (presented in the literature review) that suggests school relationships, parent involvement, and academics may relate to suicide-risk (see Supplementary Materials for details about included subscales).
We conducted Confirmatory Factor Analyses (CFAs) separately for each of the included school-related constructs to ensure that items loaded consistently on common factors representing each school-related domain at each assessment (in hospital and post-discharge). Results from CFA yielded adequate model fit at both time-points, with all factor loadings above .50 (see Supplementary Table S1). Estimates for internal reliability were also adequate (ω= .74 to .97). We calculated mean scores of items for each domain for use in subsequent analyses.
Analyses
Latent Change Score models (LCSMs) were conducted to examine change scores of perceptions of teacher relationships, connectedness to learning, parent involvement, academic satisfaction, and bullying victimization captured during hospitalization and 3-weeks following hospital discharge. LCSMs are a class of Structural Equation Modeling that can be flexibly used to model change over time. We employed an approach similar to Kievit and colleagues (2018), beginning with the simplest model, then expanding the model to examine change scores as predictors of suicidal ideation, then accounting for covariates. As shown in Figure 1, we constructed the model to fit observed variables at two time-points (“baseline” school perceptions during hospitalization and 3-weeks following hospitalization, shown in squares) to estimate the reliable average change in school perceptions between assessments as a latent variable (ΔSC, shown as a circle). We fixed the autoregressive parameter between each timepoint to 1 and included a regression parameter (β) between school perceptions measured during hospitalization and the latent change score to represent the extent to which change is dependent on school perceptions at baseline. Mean structure is estimated using a constant (shown in the triangle) to obtain the average levels of school perceptions at baseline and the average change in school perceptions at 3-week follow-up.
Figure 1.
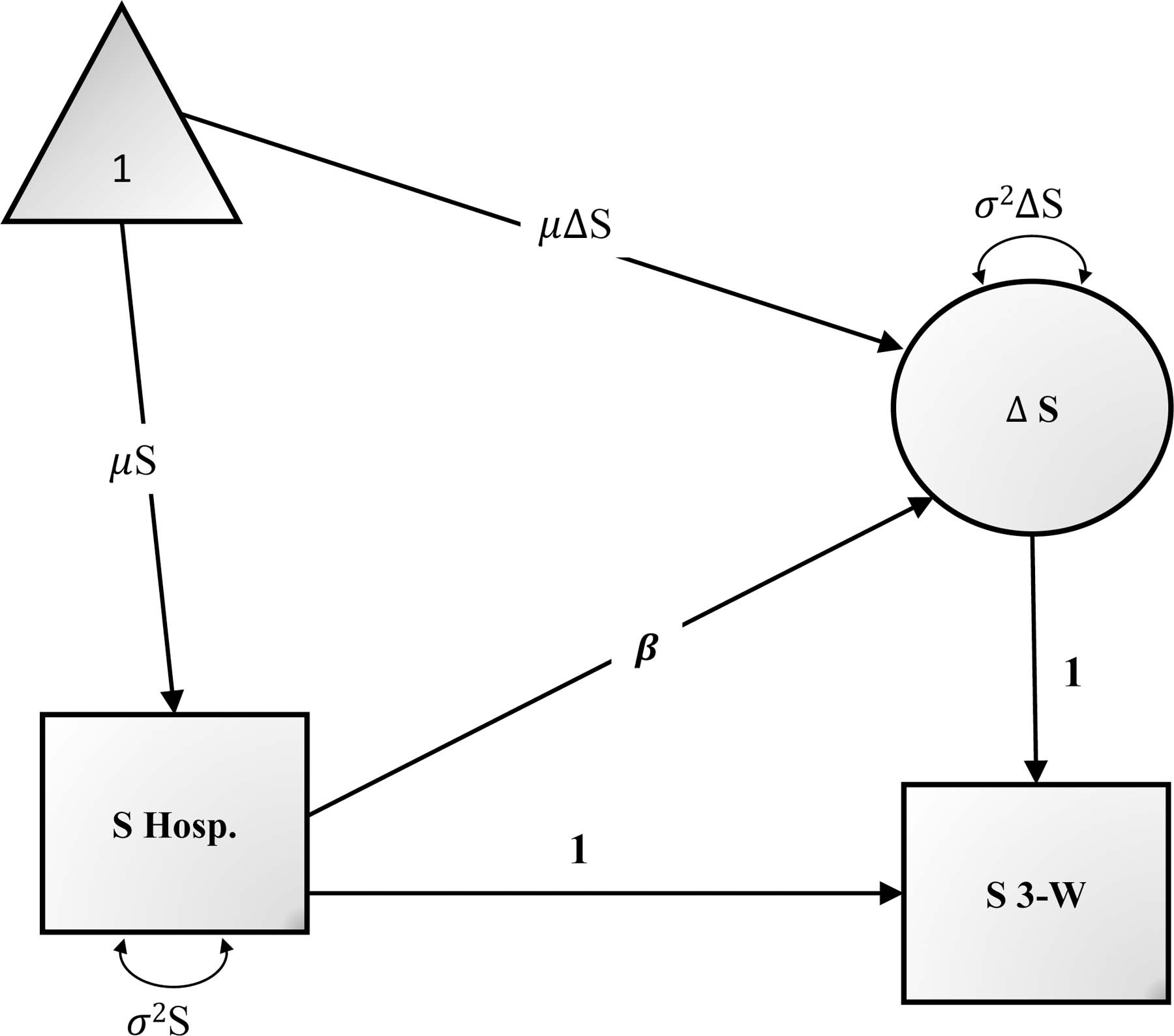
Latent change score model for exploring perceptions of school experiences following hospitalization for a suicide-related crisis.
Notes. S=school experience; β=regression estimate; µ=constant; Δ=latent change score; σ2=variance.
Next, we followed a stepwise approach for our analyses. To address our first aim, to explore if perceptions of each of the school factors significantly changed during hospitalization to 3-weeks following hospitalization, we ran separate LCSMs for each domain. To explore our second aim, to determine if baseline perceptions and significant changes in perceptions predicted suicidal ideation over 3-weeks and 6-months following hospitalization, we tested two models. First, we examined whether baseline level of school perceptions (i.e., during hospitalization) and change in school perceptions were associated with greater suicidal ideation severity and intensity. If significant, we next tested additional models controlling for depressive symptoms to determine whether these effects were robust above effects of depressive symptoms. To address our third aim, to identify the most salient predictors of suicidal ideation, we built a final model that included the joint effects of all significant change scores, baseline scores, and covariates from each model tested in our second aim as predictors of suicidal ideation and severity. The goal for this analysis was to examine the effects of multiple, school-related variables (controlling for depression) on suicidal ideation together in a single model.
Model fit was evaluated using the comparative fit index (CFI; >.9 indicating good fit), root mean square error of approximation (RMSEA; <.08 indicating good fit) and corresponding confidence interval (Brown & Cudeck, 1992; Kline, 2016). LCSMs were conducted in MPlus Version 7 using maximum likelihood estimation (Muthén & Muthén, 1998–2020), which provides standard errors and test statistics that are robust to non-normality. Missing data were handled with Full Information Maximum Likelihood (FIML).
Results
Sample Characteristics and Descriptive Statistics
Adolescents in the current study (n=155) were between ages 13–18 (Mage=15.2 years, standard deviation [SD]=1.41). Adolescents reported their sex (as recorded on their birth certificate) as female (68.6%) or male (28.2%) and their gender as girl/woman (59.6%), boy/man (30.8%), identifying in some other way (4.5%), or unsure (0.6%). A total of 13.5% indicated that their gender did not match the sex described on their birth certificates. Adolescents described their race as American Indian/Alaskan Native (1.9%), Asian (1.3%), Black/African American (7.7%), White (65.4%), or more than one race (14.1%). They reported their ethnicity as Hispanic (14.7%) or non-Hispanic (78.2%). Adolescents were in grades 7 (4.5%), 8 (10.3%), 9 (9.6%), 10 (16.7%), 11 (12.8%), or 12 (10.3%).1
Adolescents reported a lifetime history of between 0 and 17 suicide attempts (mean attempts=1.9). Average hospital stay was 8.7 days (median=8.0 days), with majority of adolescents recommended for intensive outpatient care (47.4%) or outpatient psychotherapy (39.1%) upon hospital discharge. A total of 23.1% of adolescents were identified as having an Individualized Education Plan based on data extracted from medical records. The majority of adolescents were also identified as having a depressive disorder (85.2%) and/or anxiety disorder (58.7%). Additional details regarding participant characteristics, descriptive statistics, and bivariate correlations of each of the variables of interest are shown in Supplementary Materials (see Tables S2, S3, and S4).
Changes in Perceptions of School following Hospital Discharge
To explore our first aim, to examine if perceptions of positive teacher relationships, connectedness to learning, parent involvement, academic satisfaction, and bullying victimization changed from hospitalization to 3-weeks following hospital discharge, we conducted a series of LCSMs. Parameter estimates of results from the LCSMs are shown in Table 1. The mean levels of the change scores from before hospitalization and 3-weeks following hospitalization for all school-related variables were significant, indicating an overall increase (worsening) of perceptions of each school domain over time. There was also significant variance in change scores for all variables of interest (p<.001), demonstrating that not all participants changed at the same rate or to the same degree. Perceptions during hospitalization significantly predicted change scores for all variables, such that students reporting higher (worse) perceptions of school tended to change at a slower rate compared to those reporting more positive perceptions at p<.001.
Table 1.
Latent Change Score Models (n=139)
| Parameter | Standardized Estimate (SE) | Unstandardized Estimate (SE) | p-value |
|---|---|---|---|
| Positive Teacher Relationships | |||
| Mean level at baseline | 3.02(0.18) | 2.99(0.09) | <.001 |
| Mean level of Δ | 1.52(0.19) | 1.51 (0.31) | <.001 |
| Variance of Δ | 0.60(0.08) | 0.59(0.12) | <.001 |
| Effect of mean level of baseline on Δ(β) | −0.63(0.06) | −0.63(0.10) | <.001 |
| Connectedness to Learning | |||
| Mean level at baseline | 3.80(0.26) | 3.57(0.09) | <.001 |
| Mean level of Δ | 1.55(0.28) | 1.30(0.37) | <.001 |
| Variance of Δ | 0.77(0.06) | 0.55(0.10) | <.001 |
| Effect of mean level of baseline on Δ(β) | −0.48(0.07) | −0.43(0.10) | <.001 |
| Parent Involvement | |||
| Mean level at baseline | 3.46(0.21) | 3.43(0.09) | <.001 |
| Mean level of Δ | 1.82(0.24) | 1.91(0.42) | <.001 |
| Variance of Δ | 0.66(0.08) | 0.74(0.11) | <.001 |
| Effect of mean level of baseline on Δ(β) | −0.58(0.07) | −0.62(0.12) | <.001 |
| Academic Satisfaction | |||
| Mean level at baseline | 2.94(0.19) | 3.39(0.11) | <.001 |
| Mean level of Δ | 1.34(0.18) | 1.71(0.35) | <.001 |
| Variance of Δ | 0.654(0.07) | 1.07(0.14) | <.001 |
| Effect of mean level of baseline on Δ(β) | −0.59(0.06) | −0.65(0.10) | <.001 |
| Bullying Victimization | |||
| Mean level at baseline | 1.55(0.07) | 2.31(0.14) | <.001 |
| Mean level of Δ | 0.71(0.10) | 1.07(0.25) | <.001 |
| Variance of Δ | 0.60(0.09) | 1.38(0.32) | <.001 |
| Effect of mean level of baseline on Δ(β) | −0.63(0.07) | −0.64(0.11) | <.001 |
Notes. p-values were calculated from unstandardized results. Δ=change score; SE=standard error.
Perceptions of School as Predictors of Suicidal Ideation
Results of LCSM models addressing our second aim, which assessed baseline perceptions of school and latent change scores of perceptions of school as predictors of severity and intensity of suicidal ideation occurring over the 3-week and 6-month time periods following discharge, are shown in Tables 2–3 and elaborated on in the following sections.
Table 2.
Predictors of Suicidal Ideation During 3-Weeks Post-Hospitalization
| Severity | Intensity | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 (n=152) | Model 2 (n=136) | Model 1 (n=152) | Model 2 (n=136) | |||||||||
| Parameter | β(SE) | B(SE) | p | β (SE) | B(SE) | p | β (SE) | B(SE) | p | β (SE) | B(SE) | p |
| Positive Teacher Relationships | ||||||||||||
| CES-DC | 0.33(0.07) | 0.91(0.22) | <.001 | 0.41(0.07) | 5.22(0.98) | <.001 | ||||||
| Baseline Teacher Relationships | 0.49(0.10) | 0.83(0.18) | <.001 | 0.40(0.10) | 0.70(0.17) | <.001 | 0.49(0.10) | 3.78(0.83) | <.001 | 0.37(0.09) | 2.94(0.71) | <.001 |
| Change in Teacher Relationships | 0.53(0.09) | 0.89(0.17) | <.001 | 0.54(0.08) | 0.94(0.16) | <.001 | 0.54(0.09) | 4.12(0.76) | <.001 | 0.54(0.08) | 4.28(0.62) | <.001 |
| Connectedness to Learning | ||||||||||||
| CES-DC | 0.28(0.09) | 0.78(0.24) | .001 | 0.37(0.08) | 4.63(1.05) | <.001 | ||||||
| Baseline Connectedness | 0.25(0.09) | 0.44(0.17) | .011 | 0.17(0.10) | 0.31(0.19) | .097 | 0.28(0.09) | 2.24(0.79) | .005 | 0.16(0.10) | 1.31(0.79) | .099 |
| Change in Connectedness | 0.20(0.10) | 0.40(0.18) | .025 | 0.22(0.09) | 0.44(0.17) | .009 | 0.25(0.09) | 2.30(0.80) | .004 | 0.26(0.09) | 2.40(0.72) | .001 |
| Parent Involvement | ||||||||||||
| CES-DC | ||||||||||||
| Baseline Parent Involvement | 0.21(0.11) | 0.36(0.19) | .066 | 0.19(0.11) | 1.49(0.84) | .075 | ||||||
| Change in Parent Involvement | 0.16(0.10) | 0.25(0.16) | .107 | 0.16(0.11) | 1.14(0.77) | .139 | ||||||
| Academic Satisfaction | ||||||||||||
| CES-DC | 0.31(.09) | 0.85(0.26) | .001 | 0.39(0.08) | 4.91(1.08) | <.001 | ||||||
| Baseline Academic Satisfaction | 0.25(0.11) | 0.36(0.16) | .028 | 0.02(.11) | 0.03(0.17) | .871 | 0.28(0.11) | 1.89(0.76) | .012 | 0.14(0.12) | 0.92(0.82) | .262 |
| Change in Academic Satisfaction | 0.19(0.10) | 0.25(0.13) | .064 | 0.24(0.11) | 1.46(0.66) | .027 | 0.24(0.11) | 1.48(0.65) | .024 | |||
| Bullying Victimization | ||||||||||||
| CES-DC | 0.24(0.08) | 0.65(0.23) | .005 | 0.34(0.08) | 4.20(1.02) | <.001 | ||||||
| Baseline Bullying Victimization | 0.45(0.13) | 0.51(0.14) | <.001 | 0.44(0.15) | 0.50(0.16) | .002 | 0.38(0.12) | 1.96(0.61) | .001 | 0.30(0.13) | 1.53(0.64) | .017 |
| Change in Bullying Victimization | 0.45(0.14) | 0.50(0.15) | .001 | 0.50(0.13) | 0.56(0.14) | <.001 | 0.29(0.14) | 1.50(0.67) | .026 | 0.29(0.13) | 1.49(0.61) | .014 |
Notes. p-values were calculated from unstandardized results. β=standardized regression estimate; B = unstandardized regression estimate; SE=standard error; CES-DC = Center for Epidemiological Studies Depression Scale for Children.
Table 3.
Predictors of Suicidal Ideation During 6-Months Post-Hospitalization
| Severity | Intensity | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 (n=155) | Model 2 (n=137) | Model 1 (n=155) | Model 2 (n=137) | |||||||||
| Parameter | β(SE) | B(SE) | p | β (SE) | B(SE) | p | β (SE) | B(SE) | p | β (SE) | B(SE) | p |
| Positive Teacher Relationships | ||||||||||||
| CES-DC | ||||||||||||
| Baseline Teacher Relationships | 0.19(0.14) | 0.27(0.19) | .166 | 0.26(0.13) | 1.84(0.97) | .058 | ||||||
| Change in Teacher Relationships | 0.10(0.11) | 0.15(0.16) | .349 | 0.16(0.12) | 1.16(0.90) | .194 | ||||||
| Connectedness to Learning | ||||||||||||
| CES-DC | 0.17(0.10) | 0.38(0.21) | .078 | 0.22(0.09) | 2.40(1.02) | .019 | ||||||
| Baseline Connectedness | 0.25(0.11) | 0.37(0.16) | .021 | 0.18(0.09) | 0.27(0.14) | .056 | 0.34(0.10) | 2.53(0.76) | .001 | 0.20(0.10) | 1.46(0.70) | .039 |
| Change in Connectedness | 0.05(0.10) | 0.09(0.17) | .599 | 0.15(0.10) | 1.20(0.81) | .136 | ||||||
| Parent Involvement | ||||||||||||
| CES-DC | ||||||||||||
| Baseline Parent Involvement | 0.11(0.10) | 0.15(0.14) | .284 | 0.09(0.10) | 0.64(0.74) | .385 | ||||||
| Change in Parent Involvement | −0.10(0.11) | −0.13(0.15) | .368 | −0.09(0.12) | −0.58(0.77) | .447 | ||||||
| Academic Satisfaction | ||||||||||||
| CES-DC | ||||||||||||
| Baseline Academic Satisfaction | 0.12(0.12) | 0.14(0.14) | .323 | 0.20(0.12) | 1.21(0.70) | .083 | ||||||
| Change in Academic Satisfaction | −0.04(0.10) | −0.05(0.11) | .662 | 0.10(0.11) | 0.52(0.62) | .4399 | ||||||
| Bullying Victimization | ||||||||||||
| CES-DC | ||||||||||||
| Baseline Bullying Victimization | 0.24(0.17) | 0.22(0.16) | .168 | .23(.15) | 1.06(0.71) | .134 | ||||||
| Change in Bullying Victimization | 0.19(0.13) | 0.17(0.12) | .157 | .15(.12) | 0.68(0.57) | .235 | ||||||
Notes. p-values were calculated from unstandardized results. β=standardized regression estimate; B = unstandardized regression estimate; SE=standard error; CES-DC = Center for Epidemiological Studies Depression Scale for Children.
Suicidal Ideation (Severity) at 3-Weeks Post-Discharge
The first model for each school variable included baseline levels and change scores of school climate variables as predictors of suicidal ideation severity at 3-weeks post-discharge (see Table 2). Neither baseline nor change in perceptions of parent involvement were significant predictors of suicidal ideation severity at 3-weeks. Baseline perceptions of positive teacher relationships, connectedness to learning, academic satisfaction, and bullying victimization, as well as change in perceptions of teacher relationships, connectedness to learning, and bullying victimization (but not academic satisfaction) significantly predicted higher suicidal ideation severity in each model. For the second set of models, we included self-reported depressive symptoms collected at baseline as an additional predictor of suicidal ideation severity to better understand how robust effects were for school variables above the effect of depression. For all models, depressive symptoms significantly predicted suicidal ideation; however, only positive teacher relationships and bulling victimization (both baseline perceptions and change in perceptions), as well as worsening changes in perceptions of school connectedness remained significant predictors of higher suicidal ideation after accounting for depressive symptoms.
Suicidal Ideation (Intensity) at 3-Weeks Post-Discharge
Models exploring school variables as predictors of intensity of suicidal ideation are shown in Table 2. With the exception of perceptions of parent involvement, both changes and baseline perceptions of all school variables significantly predicted higher levels of suicidal ideation intensity at 3-weeks. After accounting for self-reported depressive symptoms collected at baseline, positive teacher relationships and bullying victimization (both baseline perceptions and change in perceptions), as well as worsening changes in perceptions of connectedness to learning and academic satisfaction remained significant predictors of higher levels of suicidal ideation intensity.
Suicidal Ideation (Severity) at 6-Months Post-Discharge
We next examined perceptions of school as predictors of suicidal ideation severity over a one month period prior to a 6-month follow-up assessment (see Table 3). The only significant school predictor of 6-month suicidal ideation severity included baseline perceptions of connectedness to learning, which only approached significance (p=.056) after accounting for depressive symptoms. Accordingly, no additional models were explored.
Suicidal Ideation (Intensity) at 6-Months Post-Discharge
Finally, we explored school variables as predictors of suicidal ideation intensity over the one month period prior to a 6-month follow-up assessment (see Table 3). Only baseline perceptions of connectedness to learning was significantly related to higher levels of suicidal ideation intensity. After accounting for depressive symptoms at 6-months, baseline perceptions of connectedness to learning remained a significant predictor of higher levels of suicidal ideation intensity at 6-months.
Joint Models of School Predictors of Suicidal Ideation
To explore our third aim, we conducted a joint analysis of the most salient school-related predictors of severity and intensity of suicidal ideation following hospital discharge after accounting for depressive symptoms. Because only one significant school variable (connectedness to learning) emerged for suicidal ideation at 6-months, optimized models were only explored for suicidal ideation severity and intensity at 3-weeks (see Supplementary Table S4).
Suicidal Ideation (Severity) at 3-Weeks
The final model including the most salient predictors of severity of suicidal ideation identified in Aim 2 explored the following predictor variables: baseline depressive symptoms, perceptions of positive teacher relationships, connectedness to learning, and bullying victimization; and changes in perceptions of positive teacher relationships and bullying victimization. Students reporting higher levels of depressive symptoms, worse perceptions of teacher relationships and bully victimization, and worsening changes in perceptions of teacher relationships and bully victimization were significantly more likely to have higher severity of suicidal ideation over the 3-week period following hospitalization. Changes in perceptions of connectedness to learning were no longer significantly related to suicidal ideation severity at 3-weeks in the final model. The optimized model yielded adequate fit (CFI=0.828, RMSEA=0.107, 90% CI 0.041, 0.175).
Suicidal Ideation (Intensity) at 3-Weeks
The final model exploring significant predictors of suicidal ideation intensity at 3-weeks based on findings from Aim 2 included baseline perceptions of depressive symptoms, positive teacher relationships, and bullying victimization; and change in perceptions of positive teacher relationships, connectedness to learning, academic satisfaction, and bullying victimization. Only depressive symptoms, baseline perceptions of positive teacher relationships, and change in perceptions of positive teacher relationships remained significant predictors of suicidal ideation intensity. The final model yielded adequate fit (CFI=0.928, RMSEA=0.112, 90% CI 0.000, 0.230). Thus, students reporting higher levels of depression and worse perceptions of teacher relationships at baseline, as well as worsening changes in perceptions of teacher relationships from baseline to 3-weeks, were significantly more likely to report higher intensity of suicidal ideation 3-weeks following hospital discharge.
Discussion
As deaths by suicide and rates of psychiatric hospitalizations for suicide-related crises continue to rise, it is increasingly important to consider how adolescents’ perceptions of school-related experiences may influence recovery from STB. Because the immediate time-period following hospitalization for a suicide-related crisis is known to be particularly high-risk for suicide attempts and hospitalizations (Chung et al., 2017), and majority of adolescents return to schools during this period, identifying salient risk and protective factors can inform strategies for schools in supporting adolescent recovery from STB. Previous research has largely focused on school-related influences of suicide in non-clinical samples; however, findings from a small number of studies suggest the potential for school connectedness, bullying, and learning problems to influence recovery from STB (King et al., 2019; Tossone et al., 2014).
Expanding on this foundational work, we aimed to understand how adolescent perceptions of positive teacher relationships, connectedness to learning, parent involvement in school, academic satisfaction, and bullying victimization may change following hospitalization and also how these perceptions (both during hospitalization and changes following hospitalization) may predict severity and intensity of suicidal ideation. Although findings from separate models intimate the importance of fostering positive perceptions of majority of these domains for youth recovering from STB, after accounting for depressive symptoms, adolescent perceptions of positive teacher relationships and bullying victimization emerged as key predictors of suicidal ideation during the immediate period following discharge. Findings are consistent with those reported by previous researchers (King et al., 2019; Luukkonen et al., 2009; Tossone et al., 2014), which highlight the importance of targeting school connectedness for risk assessments and prevention interventions for recovering youth and the potential for bullying to serve as a risk factor for rehospitalization. Although perceptions of school-related domains did not emerge as the most robust predictors for longer term recovery from STB (6-months following hospitalization) in the current study, their potential to influence the immediate period following hospital discharge holds practical implications for school reintegration procedures following psychiatric hospitalization aimed at preventing suicide during this high risk period.
Changes in Perceptions of School
Results supported significant changes in adolescent perceptions of positive teacher relationships, connectedness to learning, parent involvement in school, academic satisfaction, and bullying victimization from hospitalization to 3-weeks following hospital discharge. On average, changes reflected a worsening of perceptions across time. Change scores did appear to vary by individuals, however, with results suggesting that worse perceptions of school prior to hospitalization were less likely to change than more positive perceptions. Although we are not aware of other studies exploring changes in perceptions of school following hospital discharge, some research has sought to understand how adolescent relationships may change during this transitional period. Czyz and colleagues (2012) examined social connectedness following psychiatric hospitalization and found a significant increase in connectedness to non-family adults (but not family or peers) 3-months post-discharge, as well as increased connectedness to family in female participants only (Czyz et al., 2012). Thus, previous research supports improved connectedness 3-months post-discharge; however, findings presented here suggest a decline in adolescent perceptions of school relationships and experiences 3-weeks post-discharge. This discrepancy likely reflects differences in timing of assessments, with the initial period following hospitalization expected to be particularly difficult compared to several months later when youth may have acclimated to community settings and typical routines.
Irrespective of risk for suicide, findings suggest that adolescents returning to school following hospitalization may feel less connected to teachers and learning, less satisfied academically, and that they perceive their parents as less involved in school than prior to their hospitalization. They may also perceive increased experiences of bullying victimization when they return to school. These changes may in part reflect the difficult transition adolescents experience as they return to schools following hospitalization (Tougas et al., 2019), and also provide partial evidence for the discrepancy described by school and hospital professionals regarding readiness for hospital discharge compared to readiness to return to school (Clemens et al., 2010). Previous work indicates that adolescents do report struggling with academics upon school return (Marraccini & Pittleman, 2021; Preyde et al., 2018) and also express a desire for teachers to connect with them emotionally, moving beyond a sole focus on academics (Marraccini & Pittleman, 2021; Preyde et al., 2018). Given that, on average, most adolescents demonstrated a worsening in perceptions over time, in addition to considering academic accommodations for returning students, re-entry plans should also address student relationships and bullying, as well as school engagement.
Predictors of 3-Week Suicidal Ideation
Analyses that did not adjust for covariates indicated that worse perceptions of teacher relationships, connectedness to learning, academic satisfaction, and bullying victimization during hospitalization, and worsening changes in perceptions of teacher relationships, connectedness to learning, and bullying victimization following hospital discharge were significantly related to higher levels of both severity and intensity of suicidal ideation over the 3-week period following hospitalization. Worsening perceptions of academic satisfaction were significantly related to intensity of suicidal ideation, but not severity of ideation; and parent involvement in school did not significantly relate to severity or intensity of suicidal ideation. These findings support the importance of fostering positive perceptions of each of these domains, but because most effects did not remain significant after accounting for depression, they should be considered in combination with other salient predictors of recovery (i.e., psychological functioning, family relationships). Although positive school experiences may serve as a less potent protective factor against STB compared to other factors, school-related experiences may still contribute overall protective effects, reinforcing the importance of improving perceptions of school for these high-risk youth (Marraccini & Brier, 2017).
In the final models accounting for depressive symptoms, perceptions of teacher relationships and bullying victimization during hospitalization and changes in perceptions of teacher relationships and bullying victimization following hospitalization remained important contributors to severity of suicidal ideation, with only positive perceptions of teacher relationships (during hospitalization and changes following hospitalization) contributing effects for intensity of suicidal ideation. These findings underscore the importance of fostering positive student-teacher relationships and preventing bullying experiences, with the potential for these efforts to enhance recovery from suicide-related crises.
These findings also highlight how changes in perceptions of student-teacher relationships during the immediate period following psychiatric hospitalization for a suicide-related crisis may impact recovery. Because worsening perceptions in teacher-student relationships demonstrated the greatest effects on suicidal ideation during the immediate period following hospitalization – even when accounting for depressive symptoms and perceptions of teacher relationships during hospitalization – a focus on improved relationships between school professionals and returning students may be a critical component to successful school re-entry and contribute to mitigation of severity and intensity of suicidal ideation.
Predictors of 6-Month Suicidal Ideation
When exploring longer term recovery from a suicide-related crisis, only baseline perceptions of connectedness to learning emerged as a significant predictor of severity and intensity of suicidal ideation. After accounting for depressive symptoms, however, connectedness to learning only approached significance as a predictor of suicidal ideation severity. Of note, effect sizes for both depressive symptoms and self-reported connectedness to learning were relatively small for severity of ideation (β=0.17, β=0.18, respectively) and intensity (β=.23, β=.20, respectively). Still, considering how connectedness to learning may have longer term implications for recovery, with previous work reporting lower levels of academic motivation as a risk factor for suicide attempt (Flouri & Buchanan, 2002), the findings reported here point to a link between perceptions of connectedness to learning overall (i.e., occurring prior to suicide-related crises) and suicide risk over time. That is, feeling connected to learning – related to excitement about school work, the ability to make suggestions about courses that are offered, feeling enthusiastic about learning, and being rewarded and praised for following school rules – appears important not only for academic outcomes, but also for mental health.
Implications
While early changes in perceptions following hospitalization are salient for recovery during the initial high-risk weeks following hospitalization, perceptions of school during hospitalization, that is a sense of students’ connectedness to learning prior to a suicide-related crisis, may have lasting effects on recovery from STB. Accordingly, approaches for improving school re-entry experiences should focus on both universal prevention (i.e., improving perceptions of school climate for all students, prior to crises) and targeted interventions for adolescents returning to school following hospitalization for a suicide-related crisis.
In particular, findings underscore the importance of embracing school-wide approaches that emphasize strong interpersonal relationships, which appear to have a protective effect against suicide (Cornell & Huang, 2016; McNeely & Falci, 2004; Young et al., 2011) and promote learning and academic achievement (Valiente et al., 2008) in nonclinical samples. Universal programs that jointly prevent against suicide and bullying (Holt et al.,2020) may also play a critical role in cultivating a school environment that supports recovery from a suicide-related crisis. By adopting upstream approaches, such as transformative social-emotional learning (TSEL) curriculums, teachers and school professionals can learn culturally grounded skills to facilitate student learning, connectedness, engagement, and growth (Jagers et al., 2019). As consultants, school psychologists can help reinforce known approaches for improving student-teacher relationships, including sensitivity and responsiveness to individual student needs, positive regard, and appreciation for student perspectives and experiences (Pianta et al., 2012).
Students returning to school from psychiatric hospitalization for STB have also described how strong teacher-relationships were instrumental for specific aspects of a successful school re-entry (Marraccini & Pittleman, 2021), with the findings reported here supporting the potential for a focused effort on improving student-teacher relationships to protect against severity and intensity of suicidal ideation. Such an approach might include action steps for teachers and school psychologists to engage in regular check-ins with returning students that allow time for reviewing missed lessons and coursework, as well as unstructured conversations and activities that are student-led or guided by student interests. School re-entry plans, developed in collaboration with students, parents, and community health providers, can also outline both a point-person supporting reintegration and a trusted adult for returning youth to seek support from (Marraccini et al., 2019; Tougas et al., 2019). Because findings suggested increased frequency of bullying experiences following hospitalization that were linked to severity of suicidal ideation, re-entry plans should also address and mitigate any ongoing bullying experiences. By disseminating knowledge about the complexity of recovery from suicide-related crises, school psychologists can also help improve the psychosocial climate of schools for students returning following psychiatric hospitalization (Marraccini & Pittleman, 2021).
Limitations and Future Directions
There are several limitations to the current study to consider. Both predictor and outcome variables were measured using self-report surveys and thus are limited by self-reporting biases and limited to perceptions, captured in the moment. Baseline perceptions of school climate and bullying were measured during hospitalization, which can be a particularly stressful experience for adolescents. Accordingly, perceptions of school may have been different if they were captured prior to hospitalization.
Similar limitations related to the validity of perceptions of school at the 3-week time-point should be noted. Although we added a question addressing whether or not adolescents had recently attended school to data collection procedures mid-way in the study, for the first 54 participants completing school-related surveys, we did not measure whether or not they had returned to school. Although we excluded data from participants indicating they had not returned to school for subsequent participants, it is possible that findings collected at either time-point reflect perceptions of school by both adolescents who had returned to school and adolescents who had not returned to school.
The limitations of assessing suicidal ideation using self-report methods, as well as the limited predictive validity of suicidal ideation for suicide attempts (Silverman & Berman, 2014), are also noteworthy. Although we aimed to capture both severity and intensity of ideation to move beyond simply the presence of ideation, because we did not examine school-related predictors of suicide attempts, findings cannot be generalized beyond suicidal ideation. Still, the school-related implications of reducing severity and intensity of suicidal ideation for improved attendance and participation in academics and social activities are clear, as findings help inform improved school experiences during recovery from STB. Finally, because this study was observational – that is we did not attempt to alter any naturally occurring experiences – causality cannot be inferred, and these findings should be considered preliminary. Future work that explores samples longitudinally, following adolescents prior to hospitalization and after hospitalization, is merited to better understand the distinction between universal approaches to suicide prevention and the most important approaches for schools to consider to prevent subsequent STB following a suicide-related crisis. Moreover, longitudinal studies could help elucidate how school-based experiences may interact with depression to predict recovery and inform tailored school-based interventions.
Finally, there is a critical need for studies that focus on the recovery experiences of ethnic, racial, and sexual minoritized students following a suicide-related crisis. Unfortunately, the present study contributes to a large body of suicide prevention research that is largely based on white, heteronormative culture (Marraccini et al., 2021). Although a notable number of participants in this study’s sample identified as gender diverse, limitations in power prevented subgroup analysis by gender, ethnicity, and racial identity (note that descriptive statistics for key variables in each group are presented in Supplementary Table S4). Because ethnic-racial and sexual minoritized students are less likely to feel connected to their school and may perceive their school climate as less warm and caring compared to their white, heterosexual peers (Bonny et al., 2000; Hong et al., 2011; Joyce, 2015), future studies exploring mechanisms for positive school relationships among minoritized youth could help further our understanding of suicide prevention across identities.
Conclusion
By focusing on a clinical sample of adolescents hospitalized for a suicide-related crisis, and following them over a 6-month period, findings contribute new information regarding school-related risk and protective factors for recovery from STB. Findings support the importance of student-teacher relationships and bullying victimization experiences prior to hospitalization and the potential for worsening relationships and increased bullying experiences following hospitalization to serve as risk factors for severity and intensity of suicidal ideation during the immediate time-period following discharge. Perceptions of connectedness to learning during hospitalization may also contribute longer-term effects for recovery from STB. Because it is well known that there are multiple pathways to risk for suicide, findings should be considered in conjunction with other known risk and protective factors of suicide. School professionals supporting the return of adolescents hospitalized for a suicide-related crisis should tailor re-entry plans according to the specific drivers described by individual adolescents and also build in approaches to foster school adult-student relationships and address bullying experiences for returning youth.
Supplementary Material
Public Significance Statement:
Findings from the current study identified the importance of fostering student-teacher relationships and preventing bullying experiences for students returning to school following psychiatric hospitalization for a suicide-related crisis. Whole-school approaches promoting positive relationships for all youth, as well as targeted approaches for youth recovering from a suicide-related crisis, may play a protective role against severity and intensity of suicidal ideation in the early period following hospitalization.
Acknowledgements:
The researchers would like to acknowledge the families who donated their time to this project.
The project described was supported by the National Institutes of Health, through Grant Award Number R01MH105379 (Nugent). Marisa Marraccini’s effort was supported by the National Institutes of Health, through Grant Award Numbers K23MH122775 (Marraccini) and L30MH117655 (Marraccini), as well as internal funding from the University of North Carolina (UNC) at Chapel Hill (Marraccini). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or UNC.
Footnotes
Cumulative frequencies may not add to 100% since not all adolescents elected to answer all questions.
References
- Blum RW, & Libbey HP (2004). School connectedness (executive summary). Journal of School Health, 74(7), 231–232. [Google Scholar]
- Bonny AE, Britto MT, Klostermann BK, Hornung RW, & Slap GB (2000). School disconnectedness: Identifying adolescents at risk. Pediatrics, 106(5), 1017–1021. 10.1542/peds.106.5.1017 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U (1979). The Ecology of Human Development: Experiments by Nature and Design Harvard University Press. [Google Scholar]
- Browne MW, & Cudeck R (1992). Alternative ways of assessing model fit. Sociological Methods & Research, 21(2), 230–258. [Google Scholar]
- Brown JA, Goforth AN, & Machek G (2018). School psychologists’ experiences with and training in suicide assessment: Challenges in a rural state. Contemporary School Psychology, 22(2), 195–206. doi: 10.1007/s40688-017-0147-9 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention (2013). 10 leading causes of death by age group, United States – 2013 Retrieved from http://www.cdc.gov/injury/wisqars/pdf/leading_causes_of_death_by_age_group_2013-a.pdf
- Centers for Disease Control and Prevention (2019a). Leading casues of death in males, United States Retrieved from https://www.cdc.gov/men/lcod/index.htm
- Centers for Disease Control and Prevention. (2019b). Leading casues of death in females, United States Retrieved from https://www.cdc.gov/women/lcod/index.htm
- Cheuang C (2019). Parents’ involvement and adolescents’ school adjustment: Teacher-student relationshipts as a mechanism of change. School Psychology, 34, 350–362. 10.1037/spq0000288 [DOI] [PubMed] [Google Scholar]
- Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, & Large MM (2017). Suicide rates after discharge from psychiatric facilities: A systematic review and meta-analysis. JAMA Psychiatry, 74(7), 694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemens EV, Welfare LE, & Williams AM (2010). Tough transitions: mental health care professionals’ perception of the psychiatric hospital to school transition. Residential Treatment For Children & Youth, 27(4), 243–263. 10.1080/0886571x.2010.520631 [DOI] [Google Scholar]
- Clemens EV, Welfare LE, & Williams AM (2011). Elements of Successful School Reentry After Psychiatric Hospitalization. Preventing School Failure: Alternative Education for Children and Youth, 55(4), 202–213. 10.1080/1045988x.2010.532521 [DOI] [Google Scholar]
- Cornell D & Huang F (2016) Authoritative school climate and high school student risk behavior: A cross-sectional multi-level analysis of student self-reports. Journal of Youth and Adolescence 45(11):2246–2259. 10.1007/s10964-016-0424-3 [DOI] [PubMed] [Google Scholar]
- Crepeau-Hobson F (2013). An Exploratory Study of Suicide Risk Assessment Practices in the School Setting. Psychology in the Schools, 50(8), 810–822. [Google Scholar]
- Czyz EK, Zhuquing L, King CA (2012). Social connectedness and one-year trajectories among suicidal adolescents following psychiatric hospitalization. Journal of Clinical Child & Adolescent Psychology, 41(2), 214–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erps KH, Ochs S, & Myers CL (2020). School psychologists and suicide risk assessment: Role perception and competency. Psychology in the Schools, 57(6), 884–900. [Google Scholar]
- Flouri E, & Buchanan A (2002). The protective role of parental involvement in adolescent suicide. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 23(1), 17–22. 10.1027/0227-5910.23.1.17 [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Reboussin BA, Reboussin DM, Frazier PH, Harris AE (2001). Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study. Journal of American Academy of Child and Adolescent Psychiatry, 40(1), 91–99. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Reboussin DM, Reboussin BA, Frazier PH, Kelley AE (1999). Suicide attempts among formerly hospitalized adolescents: a prospective naturalistic study of risk during the first 5 years after discharge. Journal of American Academy of Child and Adolescent Psychiatry, 38(6), 660–671 [DOI] [PubMed] [Google Scholar]
- Hall M, Fullerton L, FitzGerald C, & Green D (2018). Suicide risk and resiliency factors among Hispanic teens in New Mexico: Schools can make a difference. Journal of School Health, 88(3), 227–236. 10.1111/josh.12599 [DOI] [PubMed] [Google Scholar]
- Hatchel T, Polanin JR, & Espelage DL (2019a). Suicidal thoughts and behaviors among LGBTQ youth: meta-analyses and a systematic review. Archives of Suicide Research, 13, 1–37. [DOI] [PubMed] [Google Scholar]
- Haynes C, Eivors A, & Crossley J (2011). ‘Living in an alternative reality’: adolescents’ experiences of psychiatric inpatient care. Child and adolescent mental health, 16(3), 150–157. [DOI] [PubMed] [Google Scholar]
- Holt MK, Bowman C, Alexis A, & Murphy A (2020). Bullying, suicide, and suicide prevention in education. In Shapiro H (Ed.), The Wiley Handbook on Violence [Google Scholar]
- Holt MK, Vivolo-Kantor AM, Polanin JR, Holland KM, DeGue S, Matjasko JL, … & Reid G. (2015). Bullying and suicidal ideation and behaviors: a meta-analysis. Pediatrics, 135(2), e496–e509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong JS, Espelage DL, & Kral MJ (2011). Understanding suicide among sexual minority youth in America: An ecological systems analysis. Journal of Adolescence, 34(5), 885–894. 10.1016/j.adolescence.2011.01.002 [DOI] [PubMed] [Google Scholar]
- Horwitz AG, Czyz EK, King CA (2015). Predicting Future Suicide Attempts Among Adolescent and Emerging Adult Psychiatric Emergency Patients. Journal of Clinical Child and Adolescent Psycholology, 44(5), 751–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagers RJ, Rivas-Drake D, & Williams B (2019). Transformative Social and Emotional Learning (SEL): Toward SEL in service of educational equity and excellence. Educational Psychologist, 54, 162–184. 10.1080/00461520.2019.1623032 [DOI] [Google Scholar]
- James S, Charlemagne SJ, Gilman AB, Alemi Q, Smith RL, Tharayil PR, & Freeman K (2010). Post-discharge services and psychiatric rehospitalization among children and youth. Administration and Policy in Mental Health and Mental Health Services Research, 37(5), 433–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jobes DA, Rudd MD, Overholser JC, & Joiner TE Jr (2008). Ethical and competent care of suicidal patients: Contemporary challenges, new developments, and considerations for clinical practice. Professional Psychology: Research and Practice, 39(4), 405. [Google Scholar]
- Joyce HD (2015). School connectedness and student–teacher relationships: A comparison of sexual minority youths and their peers. Children & Schools, 37(3), 185–192. [Google Scholar]
- Kievit RA, Brandmaier AM, Ziegler G, Van Harmelen AL, de Mooij SM, Moutoussis M, Goodyer IM Bullmore EM, Jones PB, Fonagy P, NSPN Consortium., Lindenberger U, & Dolan RJ (2019). Developmental cognitive neuroscience using latent change score models: A tutorial and applications. Developmental Cognitive Neuroscience, 33, 99–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Grupp-Phelan J, Brent D, Dean JM, Webb M, Bridge JA, Spirito A, Chernick LS, Mahabee-Gittens EM, Mistry RD, Rea M, Keller A, Rogers A, Shenoi R, Cwik M, Busby DR, Casper TC & the Pediatric Emergency Care Applied Research Network. (2019). Predicting 3-month risk for adolescent suicide attempts among pediatric emergency department patients. Journal of Child Psychology and Psychiatry 60,1055–1064. 10.1111/jcpp.13087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2016). Principles and Practice of Structural Equation Modeling, fourth ed. The Guilford Press, New York. [Google Scholar]
- Kuramoto-Crawford SJ, Ali MM, & Wilcox HC (2017). Parent-child connectedness and long-term risk for suicidal ideation in a nationally representative sample of US adolescents. Crisis, 38, 309–318. [DOI] [PubMed] [Google Scholar]
- Luukkonen AH, Räsänen P, Hakko H, & Riala K (2009). Bullying behavior is related to suicide attempts but not to self-mutilation among psychiatric inpatient adolescents. Psychopathology, 42(2), 131–138. [DOI] [PubMed] [Google Scholar]
- Marsh HW, Nagengast B, Morin AJS, Parada RH, Craven RG, Hamilton LR (2011). Construct validity of the multidimensional structure of bullying and victimization: An application of exploratory structural equation modeling. Journal of Educational Psychology, 103(3),701–732. [Google Scholar]
- Marraccini ME, & Brier ZM (2017). School connectedness and suicidal thoughts and behaviors: A systematic meta-analysis. School Psychology Quarterly, 32(1), 5–21. 10.1037/spq0000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, Lee S, & Chin AJ (2019). School reintegration post-Ppychiatric hospitalization: Protocols and procedures across the nation. School Mental Health, 1–14. [Google Scholar]
- Marraccini ME, Pittleman C (2021). Returning to School Following Hospitalization for Suicide-Related Thoughts and Behaviors: Recognizing Student Voices for Improving Practice. School Psychology Review 10.1080/2372966X.2020.1862628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, Griffin D, O’Neill C, Martinez R, Chin A, Toole E, Grapin SL, Naser SC (2022). School risk and protective factors of suicide: A cultural model of suicide risk and protective factors in school. School Psychology Review, 51(3), 266–289. 10.1080/2372966X.2020.1871305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely C & Falci C (2004). School connectedness and the transition into and out of health-risk behavior among adolescents: A comparison of social belonging and teacher support. Journal of School Health, 74(7) 284–292. [DOI] [PubMed] [Google Scholar]
- Moses T (2011). Adolescents’ perspectives about brief psychiatric hospitalization: What is helpful and what is not?. Psychiatric Quarterly, 82(2), 121–137. [DOI] [PubMed] [Google Scholar]
- Muthén & Muthén, 1998–2020. Mplus (Version 8)[computer software] (1998–2017) Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Parada RH, Marsh HW, & Craven RG (2005). There and back again from bully to victim and victim to bully: A reciprocal effects model of bullying behaviours in schools Sydney, Australia: SELF Research Centre, University of Western Sydney. [Google Scholar]
- Pianta RC, Hamre BK, & Allen JP (2012). Teacher-student relationships and engagement: Conceptualizing, measuring, and improving the capacity of classroom interactions. In Christenson SL, Reschly AL & Wiley C (Eds.), Handbook of Research on Student Engagement (pp. 365–386). Springer, Boston, MA. [Google Scholar]
- Plemmons G, Hall M, Doupnik S, Gay J, Brown C, Browning W, Casey R, Freundlich K, Johnson DP, Lind C, Rehm K, Thoman S, & Williams D (2018). Hospitalization for Suicide Ideation or Attempt: 2008–2015. Pediatrics, 141(6). 10.1542/peds.2017-2426 [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Nock MK, Simon V, Aikins JW, Cheah CS, Spirito A (2008). Longitudinal trajectories and predictors of adolescent suicidal ideation and attempts following inpatient hospitalization. Journal of Consultation and Clinical Psycholology, 76(1), 92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhil L, Shen S, & Mann J (2011). The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry, 168(12), 1266–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preyde M, Parekh S, & Heintzman J (2018). Youths’ experiences of school re-integration following psychiatric hospitalization. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 27(1), 1. [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Reinke WM, Smith TE, Herman KC (2019). Family-school engagement across child and adolescent development. School Psychology, 34(4), 346–349. [DOI] [PubMed] [Google Scholar]
- Rothes IA, Henriques MR, Leal JB, & Lemos MS (2014). Facing a patient who seeks help after a suicide attempt. Crisis [DOI] [PubMed] [Google Scholar]
- Salamone-Violi GM, Chur-Hansen A, & Winefield HR (2015). ‘I don’t want to be here but I feel safe’: Referral and admission to a child and adolescent psychiatric inpatient unit: The young person’s perspective. International journal of mental health nursing, 24(6), 569–576. [DOI] [PubMed] [Google Scholar]
- Savina E, Simon J, & Lester M (2014). School reintegration following psychiatric hospitalization: An ecological perspective. Child & Youth Care Forum, 43(6), 729–746. 10.1007/s10566-014-9263-0 [DOI] [Google Scholar]
- Silverman MM, & Berman AL (2014). Suicide risk assessment and risk formulation part I: A focus on suicide ideation in assessing suicide risk. Suicide and Life-Threatening Behavior, 44(4), 420–431. [DOI] [PubMed] [Google Scholar]
- Simon JB, & Savina EA (2010). Transitioning children from psychiatric hospitals to schools: The role of the special educator. Residential Treatment For Children & Youth, 27(1), 41–54. 10.1080/08865710903508084 [DOI] [Google Scholar]
- Soto EC, Frederickson AM, Trivedi H, et al. (2009). Frequency and correlates of inappropriate pediatric psychiatric emergency room visits. Journal of Clinical Psychiatry, 70(8), 1164–1177. [DOI] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C, Weismoore J, & Miller A (2012). Adolescent suicidal behavior. In Kendall BC (Ed), Child and adolescent therapy: Cognitive-behavioral procedures, 234–256. [Google Scholar]
- Spirito A, Simon V, Cancilliere MK, Stein R, Norcott C, Loranger K, & Prinstein MJ (2011). Outpatient psychotherapy practice with adolescents following psychiatric hospitalization for suicide ideation or a suicide attempt. Clinical child psychology and psychiatry, 16(1), 53–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockings E, Degenhardt L, Lee YY, Mihalopoulos C, Liu A, Hobbs M, & Patton G (2015). Symptom screening scales for detecting major depressive disorder in children and adolescents: a systematic review and meta-analysis of reliability, validity and diagnostic utility. Journal of affective disorders, 174, 447–463. [DOI] [PubMed] [Google Scholar]
- Tossone K, Jefferis E, Bhatta MP, Bilge-Johnson S, & Seifert P (2014). Risk factors for rehospitalization and inpatient care among pediatric psychiatric intake response center patients. Child Adolescent Psychiatry Mental Health, 8(1), 27. 10.1186/1753-2000-8-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tougas A, Rassy J, Frenette-Bergeron É, & Marcil K (2019). “Lost in Transition”: A systematic mixed studies review of problems and needs associated with school reintegration after psychiatric hospitalization. School Mental Health 11, 629–649. 10.1007/s12310-019-09323-3 [DOI] [Google Scholar]
- Valiente C, Lemery-Chalfant K, Swanson J, & Reiser M (2008). Prediction of children’s academic competence from their effortful control, relationships, and classroom participation. Journal of Educational Psychology, 100, 67–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Geel M, Goemans A, Zwaanswijk W, & Vedder P (2021). Does peer victimization predict future suicidal ideation? A meta-analysis on longitudinal studies. Aggression and Violent Behavior, 101577. [Google Scholar]
- Van Geel M, Vedder P, & Tanilon J (2014). Relationship between peer victimization, cyberbullying, and suicide in children and adolescents: a meta-analysis. JAMA pediatrics, 168(5), 435–442. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE Jr (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh E, & Eggert LL (2007). Suicide risk and protective factors among youth experiencing school difficulties. International Journal of Mental Health Nursing, 16(5), 349–359. 10.1111/j.1447-0349.2007.00483.x [DOI] [PubMed] [Google Scholar]
- Wang MT, & Sheilkh-Khalil S (2014). Does parental involvement matter for student achievement and mental health in high school? Child Development, 85(2), 610–625 [DOI] [PubMed] [Google Scholar]
- Wang C, La Salle TP, Do KA, Wu C, & Sullivan KE (2019). Does parental involvement matter for students’ mental health in middle school? School Psychology, 34(2), 222–232. 10.1037/spq0000300 [DOI] [PubMed] [Google Scholar]
- Whaley AL, & Noel L (2013). Academic achievement and behavioral health among Asian American and African American adolescents: testing the model minority and inferior minority assumptions. Social Psycholology of Education 16(1) 23–43. 10.1007/s11218-012-9206-2 [DOI] [Google Scholar]
- White H, LaFleur J, Houle K, Hyry-Dermith P, Blake SM (2017). Evaluation of a school-based transition program designed to facilitate school reentry following a mental health crisis or psychiatric hospitalization. Psychology in the Schools, 54(8), 868–82. [Google Scholar]
- Whitlock J, Wyman PA, & Moore SR (2014). Connectedness and suicide prevention in adolescents: Pathways and implications. Suicide and Life-Threatening Behavior, 44(3), 246–272. [DOI] [PubMed] [Google Scholar]
- Wolff JC, Davis S, Liu RT, et al. (2018). Trajectories of Suicidal Ideation among Adolescents Following Psychiatric Hospitalization. Journal of Abnormal Child Psychology, 46(2), 355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young R, Sweeting H, & Ellaway A (2011). Doschools differ in suicide risk? The influence of school and neighbourhood on attempted suicide, suicidal ideation and self-harm among secondary school pupils. BMC Public Health, 11, 874. 10.1186/1471-2458-11-874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zullig KJ, Collins R, Ghani N, Hunter AA, Patton JM, Huebner ES, & Zhang J (2015). Preliminary development of a revised version of the School Climate Measure. Psychological Assessment, 27(3), 1072–1081. 10.1037/pas0000070 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


