This cohort study examines the association of diverse cerebrovascular pathologies (globally and regionally) with scam susceptibility in older adults.
Key Points
Question
Are cerebrovascular pathologies associated with scam susceptibility in older adults?
Findings
In this cohort study, older persons from the community with cerebral infarcts pathologically were found to have a higher susceptibility to scams during life, even after adjusting for common neurodegenerative pathologies and other cerebrovascular pathologies, vascular risk factors, and cognitive function.
Meaning
Vascular brain health may play an important role in scam susceptibility.
Abstract
Importance
Scam susceptibility is associated with adverse financial and health outcomes, including an increased risk of cognitive decline and dementia. Very little is known about the role of cerebrovascular pathologies with scam susceptibility.
Objective
To examine the association of diverse cerebrovascular pathologies (globally and regionally) with scam susceptibility.
Design, setting, and Participants
This clinical-pathological cohort study included participants from 2 ongoing studies of aging that began enrollment in 1994 and 1997. In 2010, participants were enrolled in the decision-making and behavioral economics substudy and were followed up for a mean (SD) of 3.4 (2.6) years prior to death. From 1365 older persons with clinical evaluations, 69 were excluded for having dementia at baseline. From 538 older persons who died, 408 had annual assessments for scam susceptibility, cardiovascular risk burden, and cognitive function and consented to brain donation for detailed neuropathologic examination. Data were analyzed from June 2021 through September 2022.
Exposures
Neuropathologic examination identified the presence of macroscopic and microscopic infarcts, atherosclerosis, arteriolosclerosis, cerebral amyloid angiopathy, and common neurodegenerative pathologies (Alzheimer disease, limbic-predominant age-related transactive response DNA-binding protein 43 encephalopathy, and Lewy bodies).
Results
There was a total of 408 participants. The mean (SD) age at death was 91 (6.1) years, the mean (SD) amount of education was 15.6 (3.1) years, and 297 (73%) were women. Participants included 4 Latino individuals (1%), 7 non-Latino Black individuals (2%), and 397 non-Latino White individuals (97%). The frequency of participants with macroscopic infarcts was 38% (n = 154), microinfarcts was 40% (n = 163), and moderate to severe vessel disease; specifically, atherosclerosis was 20% (n = 83), arteriolosclerosis was 25% (n = 100), and cerebral amyloid angiopathy was 35% (n = 143). In linear regression models adjusted for demographics and neurodegenerative pathologies, macroscopic infarcts were associated with greater scam susceptibility (estimate [SE], 0.18 [0.07]; P = .009). This association persisted after adjusting for cardiovascular risk burden and global cognition. Regionally, infarcts localized to the frontal, temporal, and occipital lobes and thalamus were associated with greater scam susceptibility. Neither arteriosclerosis, atherosclerosis, cerebral amyloid angiopathy, nor microinfarcts were associated with scam susceptibility.
Conclusions and Relevance
Cerebrovascular pathologies, specifically cerebral infarcts, is linked with greater scam susceptibility in older adults, independent of common neurodegenerative diseases such as Alzheimer disease. Future studies examining in vivo magnetic resonance imaging markers of cerebrovascular pathologies with scam susceptibility and related decision-making outcomes will be important.
Introduction
Each year, millions of individuals in the US devastatingly experience financial exploitations and fraud, with elderly individuals being at a disproportionate risk. Financial exploitation has a direct negative impact on an individual’s financial independence, mental and physical well-being, self-esteem, and relationship with others.1,2,3,4 For the older population, recovery from such financial losses can be almost impossible. The enormity of this public health crisis has been further exposed during the COVID-19 pandemic and economic fallout, with a dramatic rise in fraud attempts targeted toward vulnerable at-risk older individuals.5 In 2020, the US Federal Trade Commission estimated that older adults lost $100 million to COVID-19–related fraud alone.6 To raise public awareness, the US Senate Special Committee on Aging publishes an annual report on fighting fraud.6 Further, to combat this problem, the US Department of Justice coordinates efforts to provide support to older individuals who experience fraud and enhance state and local justice efforts.7
From a public health perspective, understanding the factors and mechanisms associated with the risk of financial exploitation is of particular interest. Prior studies from our group have shown that susceptibility to scams and in general decision-making are complex behaviors that require multiple resources and that age-associated factors, including cognition,8,9,10 psychosocial and contextual factors,11,12 and personality,13,14 are important correlates. Further, we show that even among individuals who are cognitively intact, subtle changes in cognition can increase susceptibility to scams.10 There are very few studies, especially autopsy studies, examining the biological basis for susceptibility to financial exploitation in elderly individuals; however, despite increased awareness that aging increases our vulnerability to financial exploitation3,15 and now widespread recognition that the aging brain is particularly vulnerable to accumulating Alzheimer disease (AD) pathologic changes and other neurodegenerative processes, such as transactive response DNA-binding protein 43 (TDP-43) and α-synuclein proteinopathies.16,17,18
In recent work, we showed that the accumulation of neurodegenerative pathology, specifically β-amyloid pathology, was associated with greater scam susceptibility, including among persons without dementia.19 These findings support the notion that age-related changes in the aging brain may be associated with early behavioral changes. Strikingly, almost 90% of postmortem brains from persons older than 65 years harbor cerebrovascular pathologies, with more than 70% having mixed AD with cerebrovascular pathologies17; however, the role of vascular pathologies with scam susceptibility has yet to be studied.
In this study, we build on our prior work by examining the association of diverse cerebrovascular pathologies, including macroinfarcts and microinfarcts, atherosclerosis, arteriolosclerosis, and cerebral amyloid angiopathy (CAA) with scam susceptibility among older adults who underwent brain autopsy. Additionally, we further explored regional associations between cerebrovascular pathologies in cortical, subcortical, and watershed-specific brain regions.
Methods
Participants
Participants were from 1 of 2 ongoing clinical-pathologic studies of aging, the Religions Orders Study or the Rush Memory and Aging Project. Upon enrollment, which began in 1994 and 1997, participants consented to annual clinical evaluations and brain donation at the time of death. Data on race and ethnicity were collected by self-report. A decision-making substudy, which includes annual assessments scam susceptibility, was added to the Religions Orders Study and Rush Memory and Aging Project in 2010. Studies were approved by the Institutional Review Board of Rush University Medical Center. All participants signed an informed consent and an Anatomical Gift Act for brain donation.20 Details of studies and inclusion of participants is included in eMethods 1 in the Supplement. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline was followed.
Scam Susceptibility
Participants rated statements that were carefully designed to assess behaviors associated with vulnerability to fraud and scams along a 7-point Likert-type scale ranging from strongly agree (1) to strongly disagree (7). Statements were developed based on findings from the AARP4 and the Financial Industry Regulatory Authority risk meter,21 regarding the behaviors commonly associated with exploitation. For example, one item asks participants if they feel like they need to answer the telephone even if they do not know who is calling, and another item asks participants if they usually listen when a telemarketer calls. Participants rated their level of agreement with each item and scam susceptibility was quantified as the mean rating across the 5 items, with higher scores indicating greater susceptibility. For analyses, the mean score for scam susceptibility was derived from all assessments over time (the mean number of visits was 4). Details of scam susceptibility validity is included in eMethods 2 and the eFigure in the Supplement.
Psychosocial Factors
Psychosocial factors include measures of psychological well-being,14 depressive symptoms,22 neuroticism, purpose in life,23 anxiety, and extraversion.24 Details included in eMethods 3 in the Supplement.
Global Cognitive Assessment
Scores from a battery of 19 neuropsychological tests were used to create summary indices of global cognitive function, which included assessment in 5 specific cognitive domains: episodic memory, semantic memory, working memory, perceptual speed, and visuospatial ability. Scores were z-transformed and averaged to obtain the summary scores for global cognitive function (all 19 tests) and for each individual domain, as previously described.25,26 For analyses, last valid annual visit scores were used.
Cerebrovascular Pathology
Cerebral Infarcts
Location, age, and size of macroscopic infarcts27,28,29 visible on gross examination were documented (Figure 1). Subsequently, the age of infarct was confirmed by microscopy and documented as acute, subacute, or chronic. Macroscopic infarcts were categorized into the following regional locations (regions are not mutually exclusive): frontal, temporal, parietal, occipital, basal ganglia, and thalamus. Cortical infarcts included those located in the cortical gray and typically the underlying white matter. Basal ganglia included infarcts in the caudate, putamen, globus pallidus, and internal capsule. Subcortical infarcts (present in subcortical gray or deep white matter) were further categorized into lacunes (defined as ≤10 mm in size) and nonlacunes (defined as ≥11 mm in size). Microscopic infarcts were not visible to the naked eye and identified by microscopy. Microscopic infarcts were further categorized into watershed microinfarcts if present in watershed brain regions (midfrontal gyrus, anterior watershed, and posterior watershed). For analyses, only chronic infarcts were considered, and all infarct variables categorized into absent vs present.
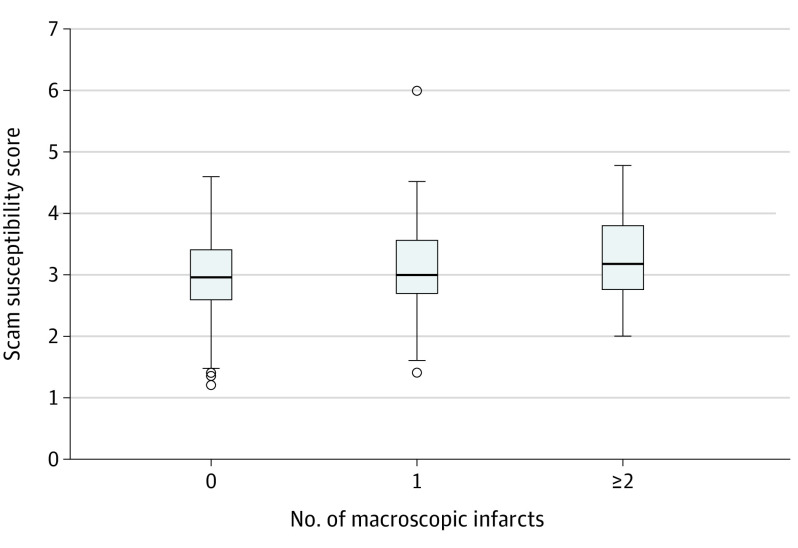
Figure 1. Cerebrovascular Pathologies.
Representative images showing a macroscopic infarct involving the frontal lobe (A), a lacunar infarct in the subcortical frontal white matter (B), a lacunar infarct in the caudate (C), atherosclerosis plaques in the basilar and associated cerebral arteries (D), a chronic microscopic infarct (E), severe arteriolosclerosis pathology (F), and cerebral amyloid angiopathy (G). Scale bar represents 200 μm (E), 50 μm (F), and 500 μm (G).
Arteriolosclerosis
Small vessels in the basal ganglia, anterior watershed, and posterior watershed regions were evaluated on hematoxylin and eosin-stained sections.30 For analyses, grading used a semiquantitative 4-level rating system (0 = none, 1 = mild, 2 = moderate, and 3 = severe) based on the histological changes of the small arterioles, including intimal deterioration, smooth muscle degeneration, and hyaline concentric thickening with narrowing of the vascular lumen.
CAA
Meningeal and parenchymal vessels from 4 neocortical regions (midfrontal, midtemporal, inferior parietal, and calcarine cortices) were semiquantitatively evaluated on sections immunostained with monoclonal antibodies against β-amyloid.31
Atherosclerosis
Large vessel atherosclerosis was semiquantitatively evaluated at the circle of Willis at the base of the brain and included evaluation of the vertebral, basilar, posterior, middle, and anterior cerebral arteries, and their proximal branches.32 Visual examination included the number of atherosclerotic plaques, extent of vessel involvement, and the degree of vessel occlusion.
Neurodegenerative Pathologies
We quantified 4 neurodegenerative pathologies28,33,34,35,36, including pathologic diagnostic assessment for AD, LATE-NC, dementia with Lewy body disease, and Parkinson disease (eMethods 4 in the Supplement).
Statistical Analyses
We first examined bivariate correlations of demographics, cognitive function, psychosocial factors, vascular risk burden, and neuropathologic characteristics with scam susceptibility. Primary analyses included a single multivariable linear regression model with terms for demographics (age at death, sex, and education) and common age-related neuropathologies (8 neuropathologic indices in total including AD pathology, Lewy bodies, limbic-predominant age-related TDP-43 encephalopathy [LATE-NC], macroscopic and microscopic infarcts, arteriolosclerosis, atherosclerosis, and CAA) to examine vascular pathologic associations with scam susceptibility. Sensitivity analyses included terms for the presence of vascular risk burden (which includes history of smoking, diabetes, and hypertension), global cognition, each individual cognitive domain, well-being, and neuroticism. In secondary analyses, linear regression models examined regional associations of macroscopic infarcts with scam susceptibility that included terms for demographics and AD pathology, as well as watershed microvascular pathology (ie, watershed arteriolosclerosis, watershed microinfarcts, and nonwatershed microinfarcts) with scam susceptibility that included terms for demographics, AD pathology, and macroscopic infarcts. Statistical significance for all analyses was determined at α level of 0.05. Analysis took place between June 2021 and September 2022.
Results
Characteristics of 408 participants are presented in Table 1. The mean (SD) age at death was 91 (6.1) years (range, 69.3-104.6 years), the mean (SD) level of education was 15.5 (3.1) years, and 297 (73%) were women. Participants included 4 Latino individuals (1%), 7 non-Latino Black individuals (2%), and 397 non-Latino White individuals (97%). Vascular risk factors were common, with 92 (23%) reporting a history of diabetes, 285 (70%) reporting hypertension, and 162 (40%) reporting being past or current smokers. Presence of cerebrovascular pathologies were common, with the most common vascular pathology being macroscopic and microscopic infarcts. Participants with macroscopic infarcts were more likely to have arteriolosclerosis (odds ratio [OR], 2.3; 95% CI, 1.6-3.4), microinfarcts (OR, 2.2; 95% CI, 1.5-3.4), and atherosclerosis pathology (OR, 3.4; 95% CI, 2.3-5.1).
Table 1. Demographics, Clinical, Psychosocial, and Neuropathologic Characteristics and Correlations With Scam Susceptibility.
| Factor | Mean (SD) | Correlation with scam susceptibilitya | P value |
|---|---|---|---|
| Demographics | |||
| Age at death, y | 91.3 (6.1) | 0.28 | <.001 |
| Men, No. (%) | 111 (27) | –0.29 | .77 |
| Women, No. (%) | 297 (73) | ||
| Education | 15.6 (3.1) | 0.05 | .27 |
| Cognition | |||
| Global cognition | –0.7 (1.0) | –0.35 | <.001 |
| Episodic memory | –0.6 (1.2) | –0.34 | <.001 |
| Semantic memory | –0.5 (1.1) | –0.35 | <.001 |
| Working memory | –0.5 (1.0) | –0.25 | <.001 |
| Visuospatial ability | –0.2 (1.0) | –0.28 | <.001 |
| Perceptual speed | –1.0 (0.9) | –0.37 | <.001 |
| Psychosocial factors | |||
| Depression | 1.6 (1.9) | –0.01 | .78 |
| Neuroticism | 15.0 (6.5) | 0.13 | .01 |
| Well-being | 5.2 (0.6) | –0.25 | <.001 |
| Purpose | 3.4 (0.5) | –0.06 | .21 |
| Anxiety | 1.3 (1.5) | 0.04 | .42 |
| Extraversion | 15.7 (3.1) | 0.01 | .87 |
| Vascular risk burden, No. (%) | |||
| Diabetes | 92 (23) | 1.39 | .17 |
| Hypertension | 285 (70) | –0.33 | .74 |
| Smoking | 162 (40) | 3.00 | .003 |
| Neuropathology, No. (%) | |||
| Macroscopic infarcts | 154 (38) | –2.79 | .006 |
| Microinfarcts | 163 (40) | –2.03 | .04 |
| Arteriolosclerosis (basal ganglia) | 100 (25) | –2.97 | .003 |
| CAA | 143 (35) | –0.79 | .43 |
| Atherosclerosis | 83 (20) | –2.41 | .02 |
| AD pathologic diagnosis | 256 (63) | –3.65 | .0003 |
| LATE-NC (stage 2/3) | 135 (33) | –3.05 | .002 |
| Lewy bodies | 104 (25) | –1.82 | .07 |
Abbreviations: AD, Alzheimer disease; CAA, cerebral amyloid angiopathy; LATE-NC, limbic-predominant age-related transactive response DNA-binding protein 43 encephalopathy.
Correlations derived from Spearman or t tests.
Scam Susceptibility
Bivariate analyses revealed that older age but not education was correlated with greater scam susceptibility. Men and women did not differ in scam susceptibility. Lower cognitive scores in global cognition and in all 5 cognitive domains, as well as poorer well-being and higher neuroticism, was associated with greater scam susceptibility. Among the vascular risk burden, only smoking was correlated with higher scam. Presence of multiple neuropathologies, including macroscopic and microscopic infarcts, arteriolosclerosis, atherosclerosis, a pathologic diagnosis of AD, and LATE-NC (stage 2 or higher) was correlated with higher scam susceptibility (Table 1).
Cerebrovascular Pathologies With Scam Susceptibility
Linear regression models were used to examine whether cerebrovascular pathologies were associated with scam susceptibility; all models adjusted for demographics and common neurodegenerative pathologies, including AD, TDP-43, and Lewy body pathology. We found that macroscopic infarcts were associated with greater scam susceptibility. There was a positive association between arteriolosclerosis pathology and scam susceptibility, but it was not significant (Table 2, model 1). By contrast, we did not find an association of scam susceptibility with other cerebrovascular pathologies, including microscopic infarcts, CAA, or atherosclerosis. In these analyses, AD pathology was associated with scam susceptibility (as previously reported; eTables 3 and 4 in the Supplement). To assess the robustness of the association, sensitivity analyses adjusted for overall vascular risk burden, global cognition (Table 2, models 2 and 3), and specific cognitive domains, as well as well-being and neuroticism (eTable 2 in the Supplement). Notably, the associations between macroscopic infarcts with scam susceptibility remained unchanged.
Table 2. Association of Cerebrovascular Pathologies With Scam Susceptibility.
| Variable | Scam susceptibility | |||||
|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | ||||
| Estimate (SE) | P value | Estimate (SE) | P value | Estimate (SE) | P value | |
| Macroscopic infarcts | 0.18 (0.07) | .009 | 0.21 (0.07) | .004 | 0.16 (0.07) | .02 |
| Arteriolosclerosis (basal ganglia) | 0.07 (0.04) | .06 | 0.08 (0.04) | .05 | 0.07 (0.03) | .05 |
| CAA | –0.04 (0.03) | .25 | –0.05 (0.03) | .15 | –0.04 (0.03) | .20 |
| Microinfarcts | 0.04 (0.07) | .52 | 0.04 (0.07) | .58 | 0.04 (0.06) | .52 |
| Atherosclerosis | –0.003 (0.05) | .96 | –0.002 (0.05) | .96 | –0.03 (0.04) | .50 |
| AD pathology | 0.24 (0.06) | <.001 | 0.24 (0.06) | <.001 | 0.12 (0.06) | .06 |
| TDP-43 | 0.04 (0.03) | .15 | 0.04 (0.03) | 15 | 0.02 (0.02) | .52 |
| Lewy bodies | 0.10 (0.07) | .18 | 0.11 (0.07) | .15 | 0.04 (0.07) | .56 |
Abbreviations: AD, Alzheimer disease; CAA, cerebral amyloid angiopathy; TDP-43, transactive response DNA-binding protein 43.
β Co-efficient estimates in each cell were obtained from a single linear regression model adjusted for age at death, sex, education, and all neuropathologic indices (11 terms in total).
Regression model further adjusted for vascular risk factor burden (12 terms in total).
Regression model further adjusted for global cognition (13 terms in total).
Regional Macroinfarcts With Scam Susceptibility and Cognition
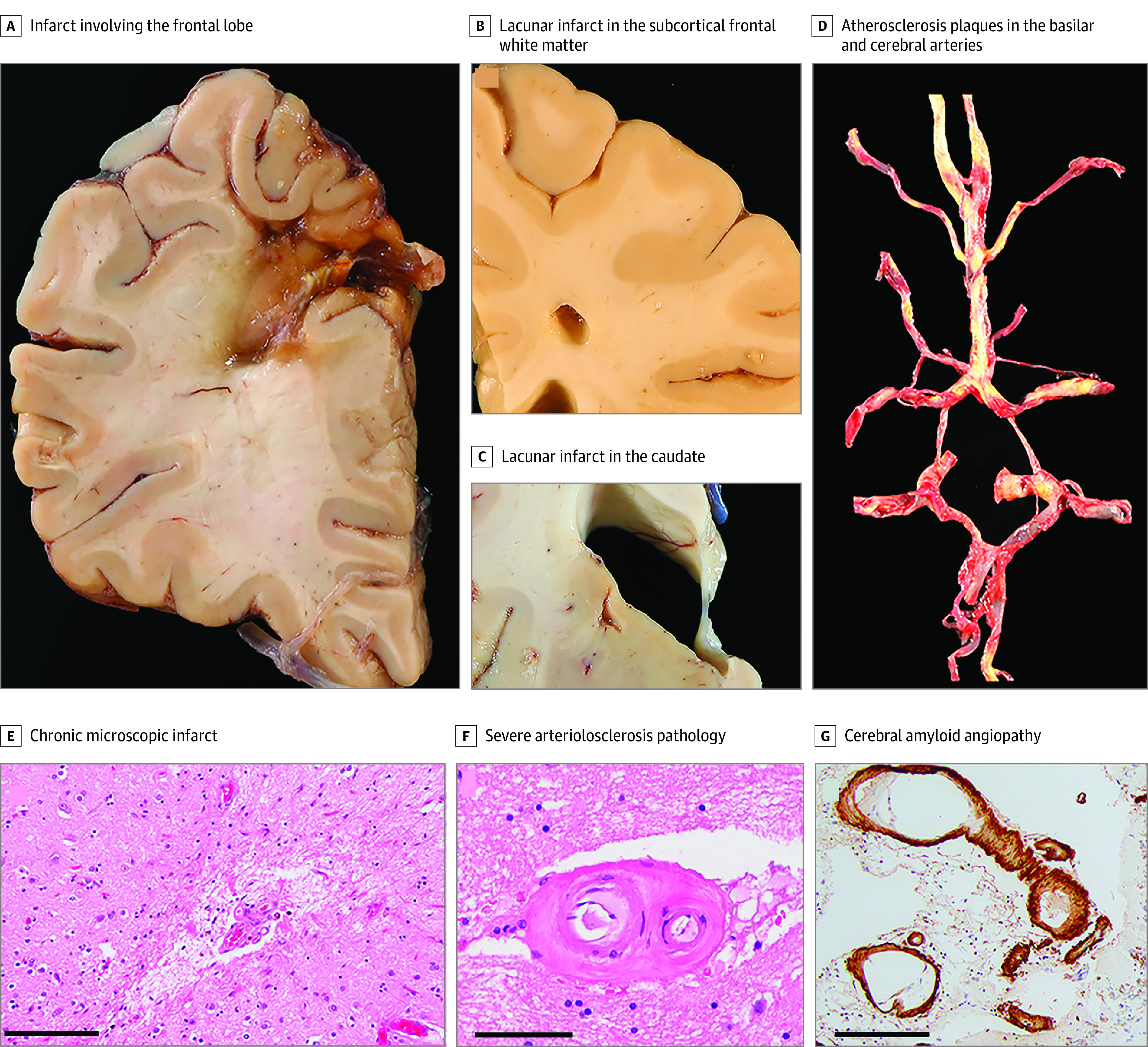
Among those that had macroscopic infarcts, 21% had a single infarct and 17% had multiple (≥2 infarcts). Those who had 2 or more infarcts had a higher scam susceptibility score (Figure 2). Macroinfarcts were more frequent in the frontal lobe followed by the basal ganglia, parietal lobe, and thalamus (Table 3). Among those with subcortical infarcts (either in subcortical gray or white matter), 119 (82%) had lacunes defined as 10 mm or smaller in size.
Figure 2. Scam Susceptibility Across None, Single, and Multiple Macroscropic Infarcts.
Table 3. Regional Macroscopic Infarcts With Scam Susceptibility and Global Cognitiona.
| Brain regionb | No. (%) | Scam susceptibility | Global cognition | ||
|---|---|---|---|---|---|
| β (SE) | P value | β (SE) | P value | ||
| Frontal lobe | 65 (16) | 0.24 (0.09) | .006 | –0.09 (0.12) | .43 |
| Parietal lobe | 31 (7.6) | –0.004 (0.12) | .97 | –0.39 (0.16) | .02 |
| Temporal lobe | 26 (6.4) | 0.36 (0.13) | .006 | –0.29 (0.18) | .17 |
| Occipital lobe | 19 (4.6) | 0.47 (0.15) | .002 | –0.28 (0.21) | .17 |
| Basal ganglia | 61 (15) | 0.15 (0.09) | .10 | –0.14 (0.12) | .25 |
| Thalamus | 30 (7.4) | 0.36 (0.12) | .003 | –0.33 (0.17) | .04 |
| Lacunar | 97 (24) | 0.24 (0.07) | .001 | –0.25 (0.10) | .02 |
| Nonlacunar | 22 (5) | 0.04 (0.10) | .67 | –0.07 (0.13) | .57 |
The estimates are derived from linear regression models with scam susceptibility or global cognition as separate outcomes and each individual brain region as the predictor. All models adjusted for age at death, sex, education, and Alzheimer disease pathology.
Brain region(s) are not mutually exclusive.
Secondary analyses examined the association of regional macroscopic infarcts with scam susceptibility and separately with global cognition. In linear regression models adjusted for demographics and AD pathology, we found that infarcts localized to the frontal, temporal, and occipital lobes and thalamus were related to scam susceptibility. Specifically, infarcts in the thalamus were associated with both scam susceptibility and global cognition, while infarcts in the frontal and occipital lobes were associated with greater scam susceptibility, but not with global cognition nor to any cognitive domain (Table 3 and eTable 1 in the Supplement). Next, we examined whether the association of infarcts differed by size, ie, total lacunes vs nonlacunes. We found that lacunes (<10 mm in size), but not nonlacunes, were associated with both greater scam susceptibility and global cognition (Table 3).
Watershed Microvascular Pathology With Scam Susceptibility
Prior work from our group has shown that watershed brain regions, which lie at the arterial border zones, are more vulnerable to microvascular pathologies.29,30 In linear regression models adjusted for demographics, macroscopic infarcts, and AD pathology, we found a positive association between arteriolosclerosis pathology in the anterior watershed region and scam susceptibility, but it was not significant. We did not find an association between arteriolosclerosis in the posterior watershed region or between watershed microinfarcts or nonwatershed microinfarcts with scam susceptibility (eTable 5 in the Supplement).
Discussion
To our knowledge, this is the first study examining multiple cerebrovascular pathologies with scam susceptibility in older persons. We found that cerebral infarcts are associated with greater scam susceptibility above and beyond accumulating AD and other neurodegenerative pathologies. Importantly, this association persists after adjusting for vascular risk burden and cognition. Together, our findings suggest that vascular brain health may play an important role in scam susceptibility.
Scam susceptibility is associated with adverse financial and health outcomes, including cognitive decline and dementia.10,14,37 Understanding brain health in the context of scam susceptibility is a novel area. There are extremely limited data that offer insight into the neurobiological basis underlying scam susceptibility, and in general decision-making processes, in older persons. In a recent study, we showed that accumulating neurodegenerative pathology, specifically β-amyloid, is associated with scam susceptibility, highlighting a specific neurodegenerative-biological footprint with scam susceptibility.19 Our current study extends these findings in several important ways. First, we examined the association of diverse cerebrovascular pathologies that are commonly found in the aging brain with scam susceptibility, expanding an extremely limited literature regarding vascular brain health as it is associated with scam susceptibility. Second, we found that the association between cerebrovascular pathologies, particularly macroscopic infarcts, is independent of accumulating AD and non-AD proteinopathies. Third, regional vascular changes, including frontal brain regions, may be important for scam susceptibility. Lastly, we observed an association between cerebrovascular pathologies with scam susceptibility independent of cognition, fostering the notion that neural factors may be involved relatively independent of cognition.
The reasons why scam susceptibility (and in general decision-making) are sensitive to specific neuropathologies are unclear. Previous work from our group and others have shown that different neuropathologies in the aging brain can have varying impacts on related behaviors such as cognition.38,39,40 Moreover, we have shown that the functional impact of various pathologies depends on combination, severity, and pattern of accumulation of brain pathologies.41 Decision-making, in particular scam susceptibility, are complex behaviors that involve integration and coordination of diverse cognitive, affective, and socioemotional resources that rely on distributed neural networks.5,14,42,43 We conceptualize that the presence of macroscopic infarcts (as well as AD pathology) impacts these brain networks and degrades specific abilities that may heighten vulnerability to scams. Neuroimaging studies have identified several interacting brain regions within, or highly connected to the frontal lobe, a brain region particularly vulnerable to infarcts (strokes) and β-amyloid pathology in early stages of AD, are likely involved in economic decision-making and socioemotional abilities.44,45 Findings from the current study also provides support for a frontal lobe involvement toward decision-making. Accumulating evidence indicates that vascular brain injury is common in older individuals without overt cognitive impairment,17,46,47 which may impact socio-cognitive and -emotional abilities in early stages of the disease process. Additionally, we and others have shown multiple pathologies coexist in the aging brain. Our prior work shows that mixed pathologies are common and that the combinations/profiles of mixed pathologies,41 including the combinations of cerebrovascular pathologies, are complex.48 In the current study, individuals with macroscopic infarcts were more likely to have arteriolosclerosis pathology, microinfarcts, and large vessel disease, and it may be the case that certain combinations of pathologies have stronger impact on scam susceptibility. While we do not have sufficient power to address this now, future studies will examine associations between the specific groups of mixed pathologies with scam susceptibility and decision-making.
Regarding biological and mechanistic pathways, cerebrovascular stress may induce damage to a myriad of white matter networks,49 disrupt white matter integrity,50 and initiate inflammatory pathways,51,52 which in turn can result in brain structural alterations53,54 and numerous long-term behavioral/decision-making deficits. A robust factor associated with vascular brain injury is inflammation, with evidence to suggest that systemic inflammation triggers a neuroinflammatory response in the brain.55,56 Chronic inflammation may play a negative role in health outcomes, especially in those with increased vulnerability to vascular brain injuries and has been linked with psychosocial factors and personality traits,57,58 critical factors that contribute to an individual’s decision-making processes. Our current study complements and extends our prior work showing an association between white matter integrity59 and gray matter volume,45 detected with in vivo magnetic resonance imaging, with scam susceptibility in the same cohort. Together, these findings pave the way to develop a framework for future longitudinal studies that include in vivo cerebrovascular markers and inflammatory biomarkers with scam susceptibility.
These findings have important clinical implications and suggest that individuals with poor vascular brain health (or numerous strokes) may have a heightened vulnerability to scams. Further, these findings suggest that cerebrovascular disease, specifically cerebral infarcts, impact a broader spectrum of behavior that extends beyond cognition, including decision-making. While the scam susceptibility measure used in this study was developed for an epidemiologic study and is not suitable to predict those individuals with macroscopic infarcts, an appropriately validated measures to assess scam susceptibility in clinical settings may offer very important diagnostic tools. This is the first study, to our knowledge, to link vascular brain injuries with scam susceptibility. Data came from a group of well-characterized, community-based, older persons. We used a well-validated measure of scam susceptibility derived from statements that are widely used in finance studies regarding the behaviors that make individuals more susceptible to scams. Further, we examined a diverse portfolio of cerebrovascular pathologies, including both cerebral infarcts and small- and large-vessel diseases, as well as regional pathologies, revealing nuanced vascular pathologic associations with scam susceptibility.
Limitations
There are some limitations to this work. First, the study cohort consisted of a highly selective group of older adults who were primarily well educated and non-Hispanic White. For the study results to be generalized, the findings should be replicated in a more diverse sample. Second, pathologies are evaluated on small, sampled brain regions; thus, we may be underestimating the burden of specific pathologies. Third, findings from this study are observational and therefore does not infer causality.
Conclusions
Future work exploring mechanistic factors associated vascular brain injury in the context of decision-making will be important to unravel pathways that contribute to decision-making and scams in older persons.
eMethods 1. Inclusion of Participants
eMethods 2. Scam Susceptibility
eMethods 3. Assessment of Psychosocial Factors
eMethods 4. Assessment of Postmortem Indices of Neurodegenerative Pathologies
eFigure. Histogram of Scam Susceptibility
eTable 1. Association of Regional Macroscopic Infarcts with Cognitive Domains
eTable 2. Association of Macroscopic Infarcts with Scam Susceptibility is Independent of Cognitive Domains and Psychosocial Factors
eTable 3. Association of β-amyloid Pathology with Scam Susceptibility
eTable 4. Association of Pathologic Diagnoses with Scam Susceptibility
eTable 5. Association of Watershed Microvascular Pathologies with Scam Susceptibility
References
- 1.True Link. The True Link report on elder financial abuse 2015. Published January 2015. Accessed March 2018. http://documents.truelinkfinancial.com/True-Link-Report-On-Elder-Financial-Abuse-012815.pdf
- 2.Peterson JC, Burnes DP, Caccamise PL, et al. Financial exploitation of older adults: a population-based prevalence study. J Gen Intern Med. 2014;29(12):1615-1623. doi: 10.1007/s11606-014-2946-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burnes D, Henderson CR Jr, Sheppard C, Zhao R, Pillemer K, Lachs MS. Prevalence of financial fraud and scams among older adults in the United States: a systematic review and meta-analysis. Am J Public Health. 2017;107(8):e13-e21. doi: 10.2105/AJPH.2017.303821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AARP Foundation . AARP Foundation national fraud victim study. Published March 2011. Accessed September 27, 2022. https://assets.aarp.org/rgcenter/econ/fraud-victims-11.pdf
- 5.Nolte J, Hanoch Y, Wood S, Hengerer D. Susceptibility to COVID-19 scams: the roles of age, individual difference measures, and scam-related perceptions. Front Psychol. 2021;12:789883. doi: 10.3389/fpsyg.2021.789883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United States Senate Special Committee on Aging . Fighting fraud: Senate Aging Committee identifies top 5 scams targeting our nation’s seniors since 2015. Accessed September 27, 2022. https://www.aging.senate.gov/imo/media/doc/Fraud%20Book%202021.pdf
- 7.U.S. Department of Health and Human Services . Fraud alert: COVID-19 scams. Updated February 2, 2022. Accessed September 27, 2022 https://oig.hhs.gov/fraud/consumer-alerts/fraud-alert-covid-19-scams
- 8.Boyle PA, Yu L, Wilson RS, Segawa E, Buchman AS, Bennett DA. Cognitive decline impairs financial and health literacy among community-based older persons without dementia. Psychol Aging. 2013;28(3):614-624. doi: 10.1037/a0033103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boyle PA, Yu L, Wilson RS, Gamble K, Buchman AS, Bennett DA. Poor decision making is a consequence of cognitive decline among older persons without Alzheimer’s disease or mild cognitive impairment. PLoS One. 2012;7(8):e43647. doi: 10.1371/journal.pone.0043647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boyle PA, Yu L, Schneider JA, Wilson RS, Bennett DA. Scam awareness related to incident Alzheimer dementia and mild cognitive impairment: a prospective cohort study. Ann Intern Med. 2019;170(10):702-709. doi: 10.7326/M18-2711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han SD, Barnes LL, Leurgans S, Yu L, Bennett DA, Boyle PA. Literacy mediates racial differences in financial and healthcare decision making in older adults. J Am Geriatr Soc. 2020;68(6):1279-1285. doi: 10.1111/jgs.16381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weissberger GH, Han SD, Yu L, et al. Impact of early life socioeconomic status on decision making in older adults without dementia. Arch Gerontol Geriatr. 2021;95:104432. doi: 10.1016/j.archger.2021.104432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.James BD, Boyle PA, Bennett DA. Correlates of susceptibility to scams in older adults without dementia. J Elder Abuse Negl. 2014;26(2):107-122. doi: 10.1080/08946566.2013.821809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yu L, Mottola G, Barnes LL, et al. Correlates of susceptibility To Scams In Community-Dwelling Older Black adults. Gerontology. 2021;67(6):729-739. doi: 10.1159/000515326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shao J, Zhang Q, Ren Y, Li X, Lin T. Why are older adults victims of fraud? current knowledge and prospects regarding older adults’ vulnerability to fraud. J Elder Abuse Negl. 2019;31(3):225-243. doi: 10.1080/08946566.2019.1625842 [DOI] [PubMed] [Google Scholar]
- 16.Jellinger KA, Attems J. Challenges of multimorbidity of the aging brain: a critical update. J Neural Transm (Vienna). 2015;122(4):505-521. doi: 10.1007/s00702-014-1288-x [DOI] [PubMed] [Google Scholar]
- 17.Kapasi A, DeCarli C, Schneider JA. Impact of multiple pathologies on the threshold for clinically overt dementia. Acta Neuropathol. 2017;134(2):171-186. doi: 10.1007/s00401-017-1717-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahimi J, Kovacs GG. Prevalence of mixed pathologies in the aging brain. Alzheimers Res Ther. 2014;6(9):82. doi: 10.1186/s13195-014-0082-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kapasi A, Yu L, Stewart C, Schneider JA, Bennett DA, Boyle PA. Association of amyloid-β pathology with decision making and scam susceptibility. J Alzheimers Dis. 2021;83(2):879-887. doi: 10.3233/JAD-210356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bennett DA, Buchman AS, Boyle PA, Barnes LL, Wilson RS, Schneider JA. Religious Orders Study and Rush Memory and Aging Project. J Alzheimers Dis. 2018;64(s1):S161-S189. doi: 10.3233/JAD-179939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Financial Industry Regulatory Authority . Financial Industry Regulatory Authority risk meter. Accessed March, 2020. https://tools.finra.org/risk_meter/
- 22.Wilson RS, Nag S, Boyle PA, et al. Brainstem aminergic nuclei and late-life depressive symptoms. JAMA Psychiatry. 2013;70(12):1320-1328. doi: 10.1001/jamapsychiatry.2013.2224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu L, Boyle PA, Wilson RS, Levine SR, Schneider JA, Bennett DA. Purpose in life and cerebral infarcts in community-dwelling older people. Stroke. 2015;46(4):1071-1076. doi: 10.1161/STROKEAHA.114.008010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buchman AS, Boyle PA, Wilson RS, Leurgans SE, Arnold SE, Bennett DA. Neuroticism, extraversion, and motor function in community-dwelling older persons. Am J Geriatr Psychiatry. 2013;21(2):145-154. doi: 10.1016/j.jagp.2012.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson RS, Barnes LL, Mendes de Leon CF, et al. Depressive symptoms, cognitive decline, and risk of AD in older persons. Neurology. 2002;59(3):364-370. doi: 10.1212/WNL.59.3.364 [DOI] [PubMed] [Google Scholar]
- 26.Bennett DA, Schneider JA, Arvanitakis Z, et al. Neuropathology of older persons without cognitive impairment from two community-based studies. Neurology. 2006;66(12):1837-1844. doi: 10.1212/01.wnl.0000219668.47116.e6 [DOI] [PubMed] [Google Scholar]
- 27.Schneider JA, Boyle PA, Arvanitakis Z, Bienias JL, Bennett DA. Subcortical infarcts, Alzheimer’s disease pathology, and memory function in older persons. Ann Neurol. 2007;62(1):59-66. doi: 10.1002/ana.21142 [DOI] [PubMed] [Google Scholar]
- 28.Schneider JA, Wilson RS, Bienias JL, Evans DA, Bennett DA. Cerebral infarctions and the likelihood of dementia from Alzheimer disease pathology. Neurology. 2004;62(7):1148-1155. doi: 10.1212/01.WNL.0000118211.78503.F5 [DOI] [PubMed] [Google Scholar]
- 29.Kapasi A, Leurgans SE, James BD, et al. Watershed microinfarct pathology and cognition in older persons. Neurobiol Aging. 2018;70:10-17. doi: 10.1016/j.neurobiolaging.2018.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kapasi A, Yu L, Petyuk V, Arfanakis K, Bennett DA, Schneider JA. Association of small vessel disease with tau pathology. Acta Neuropathol. 2022;143(3):349-362. doi: 10.1007/s00401-021-02397-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boyle PA, Yu L, Nag S, et al. Cerebral amyloid angiopathy and cognitive outcomes in community-based older persons. Neurology. 2015;85(22):1930-1936. doi: 10.1212/WNL.0000000000002175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arvanitakis Z, Capuano AW, Leurgans SE, Bennett DA, Schneider JA. Relation of cerebral vessel disease to Alzheimer’s disease dementia and cognitive function in elderly people: a cross-sectional study. Lancet Neurol. 2016;15(9):934-943. doi: 10.1016/S1474-4422(16)30029-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bennett DA, Wilson RS, Schneider JA, et al. Apolipoprotein E epsilon4 allele, AD pathology, and the clinical expression of Alzheimer’s disease. Neurology. 2003;60(2):246-252. doi: 10.1212/01.WNL.0000042478.08543.F7 [DOI] [PubMed] [Google Scholar]
- 34.Schneider JA, Arvanitakis Z, Yu L, Boyle PA, Leurgans SE, Bennett DA. Cognitive impairment, decline and fluctuations in older community-dwelling subjects with Lewy bodies. Brain. 2012;135(Pt 10):3005-3014. doi: 10.1093/brain/aws234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nelson PT, Dickson DW, Trojanowski JQ, et al. Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report. Brain. 2019;142(6):1503-1527. doi: 10.1093/brain/awz099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nag S, Yu L, Boyle PA, Leurgans SE, Bennett DA, Schneider JA. TDP-43 pathology in anterior temporal pole cortex in aging and Alzheimer's disease. Acta Neuropathol Commun. 2018;6(1). doi: 10.1186/s40478-018-0531-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ueno D, Daiku Y, Eguchi Y, et al. Mild Cognitive Decline Is a Risk Factor for Scam Vulnerability in Older Adults. Front Psychiatry. 2021;12:685451. doi: 10.3389/fpsyt.2021.685451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yu L, Boyle PA, Leurgans S, et al. Effect of common neuropathologies on progression of late life cognitive impairment. Neurobiol Aging. 2015;36(7):2225-2231. doi: 10.1016/j.neurobiolaging.2015.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boyle PA, Wilson RS, Yu L, et al. Much of late life cognitive decline is not due to common neurodegenerative pathologies. Ann Neurol. 2013;74(3):478-489. doi: 10.1002/ana.23964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boyle PA, Wang T, Yu L, et al. To what degree is late life cognitive decline driven by age-related neuropathologies? Brain. 2021;144(7):2166-2175. doi: 10.1093/brain/awab092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyle PA, Yu L, Wilson RS, Leurgans SE, Schneider JA, Bennett DA. Person-specific contribution of neuropathologies to cognitive loss in old age. Ann Neurol. 2018;83(1):74-83. doi: 10.1002/ana.25123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burton A, Cooper C, Dar A, Mathews L, Tripathi K. Exploring how, why and in what contexts older adults are at risk of financial cybercrime victimisation: a realist review. Exp Gerontol. 2022;159:111678. doi: 10.1016/j.exger.2021.111678 [DOI] [PubMed] [Google Scholar]
- 43.Wen J, Yang H, Zhang Q, Shao J. Understanding the mechanisms underlying the effects of loneliness on vulnerability to fraud among older adults. J Elder Abuse Negl. 2022;34(1):1-19. doi: 10.1080/08946566.2021.2024105 [DOI] [PubMed] [Google Scholar]
- 44.Zha R, Li P, Liu Y, Alarefi A, Zhang X, Li J. The orbitofrontal cortex represents advantageous choice in the Iowa gambling task. Hum Brain Mapp. 2022;43(12):3840-3856. doi: 10.1002/hbm.25887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Duke Han S, Boyle PA, Yu L, et al. Grey matter correlates of susceptibility to scams in community-dwelling older adults. Brain Imaging Behav. 2016;10(2):524-532. doi: 10.1007/s11682-015-9422-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Debette S, Beiser A, DeCarli C, et al. Association of MRI markers of vascular brain injury with incident stroke, mild cognitive impairment, dementia, and mortality: the Framingham Offspring Study. Stroke. 2010;41(4):600-606. doi: 10.1161/STROKEAHA.109.570044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.DeCarli C. Clinically asymptomatic vascular brain injury: a potent cause of cognitive impairment among older individuals. J Alzheimers Dis. 2013;33(suppl 1):S417-S426. doi: 10.3233/JAD-2012-129004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lamar M, Leurgans S, Kapasi A, et al. Complex profiles of cerebrovascular disease pathologies in the aging brain and their relationship with cognitive decline. Stroke. 2022;53(1):218-227. doi: 10.1161/STROKEAHA.121.034814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Petersen M, Frey BM, Schlemm E, et al. Network localisation of white matter damage in cerebral small vessel disease. Sci Rep. 2020;10(1):9210. doi: 10.1038/s41598-020-66013-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sam K, Peltenburg B, Conklin J, et al. Cerebrovascular reactivity and white matter integrity. Neurology. 2016;87(22):2333-2339. doi: 10.1212/WNL.0000000000003373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wiseman SJ, Doubal FN, Chappell FM, et al. Plasma biomarkers of inflammation, endothelial function and hemostasis in cerebral small vessel disease. Cerebrovasc Dis. 2015;40(3-4):157-164. doi: 10.1159/000438494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wright P, Veronese M, Mazibuko N, et al. Patterns of mitochondrial TSPO binding in cerebral small vessel disease: an in vivo PET study with neuropathological comparison. Front Neurol. 2020;11:541377. doi: 10.3389/fneur.2020.541377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.De Guio F, Duering M, Fazekas F, et al. Brain atrophy in cerebral small vessel diseases: extent, consequences, technical limitations and perspectives: the HARNESS initiative. J Cereb Blood Flow Metab. 2020;40(2):231-245. doi: 10.1177/0271678X19888967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith EE, O’Donnell M, Dagenais G, et al. ; PURE Investigators . Early cerebral small vessel disease and brain volume, cognition, and gait. Ann Neurol. 2015;77(2):251-261. doi: 10.1002/ana.24320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Naveed M, Zhou QG, Han F. Cerebrovascular inflammation: a critical trigger for neurovascular injury? Neurochem Int. 2019;126:165-177. doi: 10.1016/j.neuint.2019.03.011 [DOI] [PubMed] [Google Scholar]
- 56.Mun KT, Hinman JD. Inflammation and the link to vascular brain health: timing is brain. Stroke. 2022;53(2):427-436. doi: 10.1161/STROKEAHA.121.032613 [DOI] [PubMed] [Google Scholar]
- 57.Ranjit N, Diez-Roux AV, Shea S, et al. Psychosocial factors and inflammation in the multi-ethnic study of atherosclerosis. Arch Intern Med. 2007;167(2):174-181. doi: 10.1001/archinte.167.2.174 [DOI] [PubMed] [Google Scholar]
- 58.Wagner EN, Ajdacic-Gross V, Strippoli MF, et al. Associations of personality traits with chronic low-grade inflammation in a Swiss community sample. Front Psychiatry. 2019;10:819. doi: 10.3389/fpsyt.2019.00819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lamar M, Arfanakis K, Yu L, et al. White matter correlates of scam susceptibility in community-dwelling older adults. Brain Imaging Behav. 2020;14(5):1521-1530. doi: 10.1007/s11682-019-00079-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Inclusion of Participants
eMethods 2. Scam Susceptibility
eMethods 3. Assessment of Psychosocial Factors
eMethods 4. Assessment of Postmortem Indices of Neurodegenerative Pathologies
eFigure. Histogram of Scam Susceptibility
eTable 1. Association of Regional Macroscopic Infarcts with Cognitive Domains
eTable 2. Association of Macroscopic Infarcts with Scam Susceptibility is Independent of Cognitive Domains and Psychosocial Factors
eTable 3. Association of β-amyloid Pathology with Scam Susceptibility
eTable 4. Association of Pathologic Diagnoses with Scam Susceptibility
eTable 5. Association of Watershed Microvascular Pathologies with Scam Susceptibility