Abstract
Eating disorders are severe mental illnesses with the second highest mortality rate of all psychiatric illnesses. Eating disorders are exceedingly deadly because of their complexity. Specifically, eating disorders are highly comorbid with other psychiatric illnesses (up to 95% of individuals with an eating disorder have at least one additional psychiatric illness), have extremely heterogeneous presentations, and individuals often migrate from one specific eating disorder diagnosis to another. In this Perspective, we propose that understanding eating disorder comorbidity and heterogeneity via a network theory approach offers substantial benefits for both conceptualization and treatment. Such a conceptualization, strongly based on theory, can identify specific pathways that maintain psychiatric comorbidity, how diagnoses vary across individuals, and how specific symptoms and comorbidities maintain illness for one individual, thereby paving the way for personalized treatment.
ToC Blurb
Eating disorders are especially deadly because of high psychiatric comorbidity, heterogeneity within and between diagnoses, and diagnostic migration. In this Perspective, Levinson et al. propose that a network theory approach to eating disorders addresses this complexity, with substantial benefits for conceptualization and treatment.
Introduction
Eating disorders consist of several diagnoses. These diagnoses include anorexia nervosa (failure to maintain a healthy weight accompanied by significant fears of weight gain), bulimia nervosa (extreme overeating followed by compensatory behaviors to avoid weight-gain), binge-eating disorder (frequently consuming large amounts of food in one sitting with a concurrent sense of loss of control), and other specified feeding and eating disorder (OSFED; any other eating disorder that does not fall neatly into one of the other three categories). Regardless of diagnosis, all eating disorders involve an over-focus on weight and shape and corresponding eating disorder behaviors (for example, binge eating, restriction, and purging). Individuals with anorexia nervosa have a 5–7% standardized mortality rate, individuals with bulimia nervosa have a 2% morality rate, and individuals with binge-eating disorder have a 1.77–2.9% mortality rate1–4.
In addition to high mortality rates, individuals with eating disorders experience poor life outcomes which influence their physical and psychological wellbeing. These poor life outcomes include cognitive impairments (such as executive functioning deficits)5, emotional impairments (such as disinhibited emotional responses)6, difficulties making decisions7, interference with interpersonal relationships (such as social withdrawal)8, low quality of life9, and increased risk of suicidality10. Eating disorders also have one of the highest rates of medical complications compared to other psychiatric illnesses. Medical complications of eating disorders include hair loss11, dental enamel erosion12, osteoporosis13, low blood pressure14, bradycardia (slow heart rate, < 60 beats/minute)15, tachycardia (fast heart rate, >100 beats/minute)16, gastrointestinal bleeding17, growth impediments18, and cardiac arrest. Many of these complications persist even after eating disorder symptoms improve, such as increased risk for cardiovascular disease19, infertility20, and gastrointestinal issues21.
The psychological and physical effects of eating disorders are profound, yet treatment-seeking rates are low. Lifetime treatment-seeking estimates for individuals with anorexia nervosa, bulimia nervosa, and binge-eating disorder range from 34.5%−63.5%22. Even when treatment is sought, the efficacy of evidence-based treatments for eating disorders (for example, cognitive-behavioral therapy; CBT) is low (~50%)23 and relapse rates are high (~35–50%)24. The costs of eating disorders extend beyond the physical and psychological effects on individuals; eating disorders are a costly burden to the health system. In 2018–2019 alone, the total economic cost of eating disorders in the US was 64.7 billion dollars25.
The severity and complexity of eating disorders is further impacted by high rates of psychiatric comorbidity, high levels of heterogeneity both within and between diagnoses, and the likelihood of diagnostic migration (crossing from one eating disorder diagnosis to another) during the course of illness. These factors influence the severity of eating disorders because comorbid symptomatology might reinforce and strengthen eating disorder symptoms. For example, compulsive checking behaviors (a symptom of obsessive-compulsive disorder) could lead to increased body checking (the habit of seeking information about body weight, shape, size, or appearance through behaviors such as pinching the stomach or continually looking in the mirror), which might perpetuate overvaluation of shape. Furthermore, both heterogeneity and diagnostic migration within and between diagnoses can impact treatment efficacy (for example, most treatments only focus on the eating disorder, rather than comorbid illness symptoms), which can lead to prolonged illness and difficulty in treatment (patients might not respond to standard treatments that do not address the comorbidities).
In this Perspective, we describe the impact of eating disorder comorbidity and heterogeneity, and consider the importance of theory building for conceptualizations of comorbidity26. Next, we discuss how applying network theory and analysis at both group and idiographic levels can enhance understanding of eating disorder comorbidity, and lead to personalized treatments. Although we use eating disorders as the psychiatric illness of example, a network perspective to psychiatric comorbidity and heterogeneity can be expanded across all forms of psychopathology to improve understanding of how psychiatric illnesses develop and persist.
Eating disorder complexity
The complexity of eating disorders is evidenced by the high rates of comorbidity, heterogeneity, and fluidity of diagnoses. Eating disorders are highly comorbid with other psychiatric illnesses; indeed, up to 95% of individuals with an eating disorder have at least one additional psychiatric illness27. Across eating disorder diagnoses, comorbid psychiatric diagnoses include anxiety disorders28–30, obsessive-compulsive disorder31, body dysmorphic disorder32, post-traumatic stress disorder (PTSD)33, depressive disorders (major depressive disorder and dysthymia)27,34, bipolar disorder27,35,36, attention-deficit/hyperactivity disorder37,38, substance use disorders27,39, and borderline personality disorder40,41 (Table 1).
Table 1.
Eating Disorder Comorbidity
| Comorbid disorder | Anorexia nervosa | Bulimia nervosa | Binge-eating disorder | Overall |
|---|---|---|---|---|
| % | % | % | % | |
| Anxiety disorders | 33% – 72%28,157 | 41–75%28,157 | 65%27 | -- |
| Generalized anxiety disorder | 24% – 31%28 | 10% – 55%28,158 | 12%27 | -- |
| Social anxiety disorder | 16% – 88%159 | 17% – 68%159 | 32%27 | -- |
| Panic disorder | 13% – 24%157 | 4% – 21%157,158 | 13%27 | -- |
| Agoraphobia | 20% – 27%157 | 16% – 34%157,158 | 7%27 | -- |
| Obsessive-compulsive disorder | 44%31 | 19%31 | 8%27 | 21% – 41%29,159 |
| Post-traumatic stress disorder | 12%27 | 45%27 | 26%27 | 4% – 62%27,96,159 |
| Mood disorders | 42%27 | 70%27 | 46%27 | >50%*34 |
| Major depressive disorder | 39%27 | 50%27 | 32%27 | -- |
| Bipolar disorder | 3%27,36 | 5% –18%27,36 | 9% – 13%27,36 | 14.3%36 |
| Borderline personality disorder | 0% – 29%*40,160 | 3% – 31 %*40,160 | -- | 14% – 53%*160 |
| Attention-deficit hyperactivity disorder | 16%27 | 35%27 | 20%27 | 21%38 |
| Substance use disorders | 27%27 | 37%27 | 23%27 | 25%39 |
Note: All rates are lifetime prevalence except for those with an *.
Point prevalence (prevalence measured at a specific point in time)
There is conflicting evidence about whether a psychiatric diagnosis increases the risk of developing an eating disorder or vice versa, or whether eating disorders and other psychiatric illness develop simultaneously42. There is likely a combination of these illness pathways. For example, if an individual has social anxiety disorder, their increased sensitivity to social rejection might lead them to criticize their own body harshly. This harsh criticism could lead to restricting food to maintain a body shape they believe is socially desirable. Thus, anxiety disorders might lead to eating disorders. By contrast, an individual with an eating disorder who has disturbances in body image might worry about what to wear when they leave their house to minimize judgment from others. This worry over what to wear could lead the individual to fear social situations where they perceive there will be people judging their body and other social aspects, such as how they behave in social situations. Thus, an eating disorder could lead to an anxiety disorder. Finally, if an individual has heightened intolerance to uncertainty, they might fear social situations where they do not know who will be present and be afraid to try new food for fear of how their body will react. Thus, underlying vulnerabilities might lead to both eating disorders and anxiety disorders.
Most evidence-based treatments for eating disorders specifically aim to address eating disorder psychopathology43,44. However, because eating disorders have high rates of comorbidity with other psychiatric diagnoses, treatments that can simultaneously address eating disorders and comorbid psychopathology are urgently needed. Only treating eating disorders leaves patients with unremitted comorbid psychopathology which increases risk for relapse, and makes eating disorder treatments less effective because they do not address the complex interrelationships among eating disorders symptoms and co-occurring conditions45.
Symptom presentation is also highly heterogeneous within46–48 and between49,50 eating disorder diagnoses. This heterogeneity is perhaps most clearly evidenced by the fact that OSFED is the most prevalent eating disorder diagnosis51 (and yet is less studied than anorexia nervosa, bulimia nervosa, and binge-eating disorder). OSFED includes combinations of eating disorder symptoms that do not fall under a diagnosis of anorexia nervosa, bulimia nervosa, or binge-eating disorder52,53. Notably, there are no significant differences in impairment or risk factors between anorexia nervosa, bulimia nervosa, binge-eating disorder, and OSFED49 (with the caveat that there are some neurobiological differences54,55), suggesting there might not be clinically meaningful difference between diagnostic categories. Thus, a symptom-level approach to eating disorder presentation and diagnosis could be more appropriate than semi-arbitrary categories. This between-diagnosis heterogeneity is important because it makes accurate diagnosis and—therefore treatment—difficult. For example, a person with an eating disorder’s illness could be maintained by symptoms such as shame, rather than traditional eating disorder symptoms (such as overvaluation of weight). However, this type of non-traditional symptom would not be addressed in treatment leaving treatment ineffective at targeting the most important aspects of their eating disorder.
Furthermore, symptom heterogeneity is high even within individuals with the same diagnosis56,57. For example, an individual with anorexia nervosa might fear weight gain and engage in food restriction to lose or maintain weight, whereas another individual with anorexia nervosa might fear judgment of their body and therefore engage in compulsive exercise. This symptom heterogeneity might explain why standardized treatments with a ‘one size fits all’ approach do not work for treating many eating disorders58 and the low recovery rates even after receipt of evidence-based treatment59–61. As mentioned above, the high heterogeneity means that most standard treatments are not tailored to specific symptoms that are problematic on an individual-level. Thus, a treatment approach that considers each individuals’ complex symptom presentation might be needed to address person-specific symptoms.
The propensity for diagnostic migration further complicates high heterogeneity within eating disorders. Diagnostic migration (also known as diagnostic crossover) occurs when eating disorder symptoms transition within eating disorder subtypes (for example, from anorexia nervosa-restriction to anorexia nervosa-binge purge62) or between eating disorder diagnoses63 (for example, from anorexia nervosa to bulimia nervosa62,64,65, bulimia nervosa to anorexia nervosa64,65, bulimia nervosa to binge-eating disorder1,2, or binge-eating disorder to bulimia nervosa64,66). The trajectory of diagnostic migration is not uniform; some literature suggests that migration is most likely to occur in the first five years of illness65, while other evidence suggests that migration happens during relapse (that is, an individual can develop a different diagnosis during relapse)64. There are many predictors of diagnostic migration including the presence of comorbid diagnoses (such as depression, anxiety, or panic disorder)64,67, substance abuse64,67, early age of disorder onset64, and parental characteristics (for example, perceived parental criticism and low levels of perceived parental empathy)65,68. Diagnostic migration can also occur multiple times over the course of an eating disorder (for example, an individual with anorexia nervosa could develop bulimia nervosa and later OSFED, or relapse to anorexia nervosa)64.
Diagnostic migration in eating disorders is common: an estimated ~50% of individuals transition within or between eating disorders over time64,69,70. There is also evidence for diagnostic progression, or transitioning from subthreshold to threshold diagnoses66. This high level of diagnostic migration causes problems for research because it is difficult to make broad inferences about a group of individuals with a specific eating disorder without contextualizing if they have had prior eating disorder diagnoses. High rates of diagnostic migration also influence treatment efficacy and a therapist’s ability to target the correct symptoms in treatment. For example, if an individual is being treated for anorexia nervosa and then develops bulimia nervosa, the treatment would need to shift to focus on the new behaviors and cognitions that developed. Alternatively, this migration might reflect that common core symptoms (for example, social fears) were never addressed.
In sum, eating disorders are characterized by high comorbidity, heterogeneity, and diagnostic migration within and between eating disorder diagnoses. These features suggest that a symptom level approach, which focuses on variations in levels of symptomatology, might be more appropriate for conceptualizing and treating eating disorders than categorical diagnoses.
Network theory and eating disorders
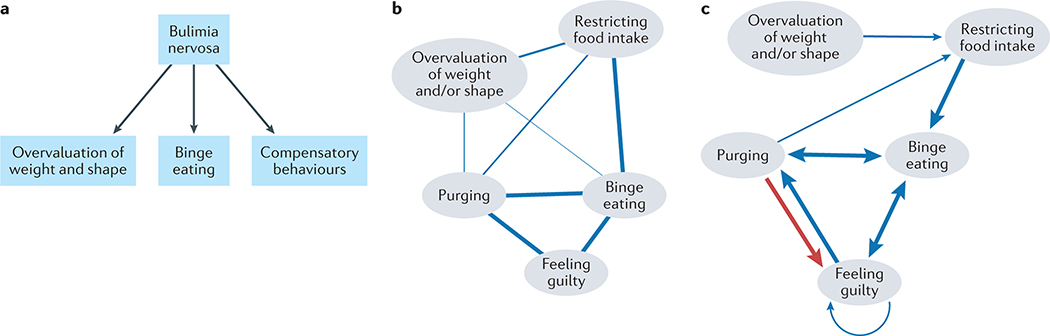
The structure of the Diagnostic and Statistical Manual Version 571 (DSM-5) is based on a medical model of disease, which groups symptoms into clusters of categories that are used to diagnose mental disorders. Eating disorders were initially conceptualized in this framework, leading to distinct diagnoses (anorexia nervosa, bulimia nervosa, binge-eating disorder, and OSFED). The latent variable model mirrors disease models in medicine, and conceptualizes mental disorders as latent variables giving rise to symptoms72. For example, according to a latent variable model, bulimia nervosa is an underlying syndrome that causes observable symptoms characterizing the syndrome, overvaluation of weight and shape, binge eating, and compensatory behaviors73 (Figure 1A). Associations among observable symptoms are attributed to shared variance of the latent construct. For example, overvaluation of weight and shape, binge eating, and compensatory behaviors might relate to each other because they stem from the same common cause of bulimia nervosa (Figure 1A).
Figure 1. Latent and network models of bulimia nervosa.
A) A conceptual figure of a latent variable model of bulimia nervosa. B) A conceptual figure of a network model of bulimia nervosa. C) A conceptual figure of an idiographic temporal network of bulimia nervosa. Blue edges denote positive relations, and red lines denote negative relations between symptoms. Nodes: overval wt/sh = overvaluation of weight and/or shape. restrict = restricting food intake. purge = purging. binge eat = binge eating. guilt = feeling guilty.
However, this traditional framework does not adequately reflect the complexity of symptom relations within one disorder, or co-occurring mental disorders. First, it is unlikely that a single latent construct causes all symptoms. That is, it is unlikely that an eating disorder per se is the cause of all eating disorder symptoms. Instead, symptoms of eating disorders dynamically impact other symptoms (see74 for a discussion). Second, it is not possible to view symptoms independent of their cause72 For example, in a latent variable framework a clinician would have no guidance on which specific symptoms are causally relevant for treatment, and instead would be given blanket guidance to target an ‘eating disorder’. Third, symptoms of co-occurring disorders are unlikely to exist because of covariation in latent constructs72. For example, if a clinician was working from a latent variable framework they would focus on an overall ‘eating disorder’ rather than symptoms such as ‘fear of weight gain’. Clinical reality more closely mirrors focusing on symptoms such as fear of weight gain, rather than broad diagnoses.
By contrast, network theory conceptualizes mental disorders as complex systems in which symptom dynamics constitute a mental disorder73,74. In other words, instead of a latent entity causing symptoms, network theory proposes that symptoms interact to form causal, sustaining relationships72,75. For example, overvaluation of weight and shape, binge eating, and compensatory behaviors are related because symptoms influence other symptoms. That is, the overvaluation of weight and shape leads to restricting food intake, which leads to binge eating, which leads to compensatory behaviors, thereby producing the symptom cluster that comprises bulimia nervosa (Figure 1B). Network analysis is the analytic extension of network theory that uses advanced quantitative methods to test network theory with data72,76. See Box 1 for an overview of network analysis components. Throughout the manuscript we refer to aspects of theory when emphasizing the theoretical framework and network analysis when discussing the corresponding statistical techniques.
Box 1: Overview of Network Components.
Network analysis refers to statistical methodologies designed to test network theory. Although network analysis stems from network theory, the two should not be misconstrued as the same26. For instance, network theory posits that symptoms maintain causal interactions rather than symptoms stemming from a single latent construct74, whereas network analysis involves mathematical estimation of symptom interactions accounting for all other symptom interactions (for example, a Gaussian Graphical Model114). Within models formed through network analysis, symptoms are nodes (depicted by circles), and relations between symptoms are edges (depicted by lines connecting nodes). Most network analyses use cross-sectional data to estimate partial correlation networks accounting for all other symptom relations within the network126. Edges may be weighted, where thicker lines indicate more highly correlated nodes than nodes with thinner edges (which denote weaker correlations). Nodes with high edge weights are theorized to reflect self-sustaining relations among symptoms, agnostic of causality or directionality74,161.
Symptoms are quantified by centrality metrics. Potential treatment targets or symptoms that are more important relative to other symptoms in a network are identified by high centrality values72,116,162. Although there are several centrality metrics148, strength centrality (the sum of the absolute value of correlation coefficients between a node and all connected nodes) has the most support for use in cross-sectional networks120. Under the centrality hypothesis83, central symptoms activate other symptoms within the network. Thus, intervening upon central symptoms is theorized to disrupt the network’s structure (that is, reduce symptoms comprising the disorder)74,82,120,130. Research with prospective data has demonstrated that cross-sectional network analysis can provide insights on symptom dynamics163, symptom severity164, and prognosis. Further, central symptoms predict outcomes and are highly heritable162,165.
Finally, the term ‘symptom’ implies a latent variable, such that behaviors, cognitions, affect, and physiological arousal are indicative of (or a symptom of) an underlying disorder. To avoid this connotation of latent cause, scholars within the network literature often refer to behaviors, cognitions, affect, physiological arousal as ‘elements’74,130,166. Although ‘element’ may better reflect the network approach, we use ‘symptom’ to increase readability for a wide audience, who may not be as familiar with the language used within the network literature.
Network and latent variable models have been contrasted at length within the psychological literature (see 26,77–80). The distinction between network and latent variable models is ultimately conceptual, and reflects how the presence of symptoms characterizing mental disorders are explained73. One could conceptualize psychopathology as an unobservable underlying cause giving rise to symptoms (latent variable model) or as symptoms forming predictable, causal relations that are maintained over time (network model). However, network and latent variable theory are not necessarily mutually exclusive; rather, the two frameworks differ in focus. A latent variable approach focuses on static entities, or syndromes. A network approach focuses on symptom interactions. Although the distinction between network and latent variable models is theoretical, there are clinical implications. Latent variable models are statistical models that are often misinterpreted as theoretical models (which might not explain psychological phenomena26). Thus, directly identifying treatment targets (symptoms) via network models might be more useful to clinical practice than focusing on an underlying entity, which might be difficult to explicitly target with treatments72,74,75,81,82.
Comorbidity, heterogeneity, and diagnostic migration in eating disorders have been conceptualized primarily through a latent variable approach83. In the following sections, we suggest that network theory can better address comorbidity and diagnostic migration because it ‘zooms in’ on specific symptom relations to identify dynamical symptom change and how some symptoms might lead to additional symptoms of the same or different disorders. This type of conceptualization can better address the high levels of heterogeneity seen in the eating disorders.
Comorbidity and diagnostic migration through a network lens
Comorbid mental disorders are associated with several adverse outcomes, including poorer prognosis84, greater impairment85, and a greater likelihood of suicide86 relative to one mental disorder diagnosis. Given the high comorbidity among mental disorders87, modeling how symptoms characterizing one mental disorder relate to another might inform clinical decisions aimed at treating symptom dynamics that reinforce comorbidities. The latent variable model attributes comorbid symptom relations to the covariance in latent syndromes74,83. This understanding of comorbidity has been examined through psychometric methodology consistent with factor analysis26. For example, for an individual who presents with anorexia nervosa and social anxiety disorder, one would assume that this comorbidity exists because the latent entities anorexia nervosa and social anxiety disorder have bidirectional associations.
By contrast, a network approach understands comorbid mental disorders by bridge symptoms, or elements that are not exclusive to one disorder. Instead, bridge symptoms are mechanisms that sustain direct, causal relations between diagnostic clusters (for example, lack of appetite might bridge between eating disorders and depression symptoms)83. Bridge symptoms are often quantified by bridge strength. In contrast to strength centrality (symptoms that are considered core or ‘trigger’ symptoms for all other symptoms in the network), bridge strength only accounts for node connections in different diagnostic clusters88. Therapeutic intervention aimed at bridge symptoms is theorized to disrupt symptom pathways between disorders83,88 and has the potential to sever feedback loops that reinforce psychopathology.
Network theory delineates how symptoms of one disorder interact and maintain themselves. Importantly, network theory also delineates how symptoms of multiple disorders interact83, which is advantageous because most mental disorders do not occur in isolation89–91. For example, eating disorders are highly comorbid with anxiety disorders92,93. Many models have been proposed to understand this overlap. For example, models of shared etiology suggest that underlying latent variables (such as cognitive avoidance) are shared between anxiety and eating disorders92; models of shared vulnerabilities suggest that social appearance anxiety is a shared vulnerability between anxiety and eating disorders94; and models of shared cognitive vulnerabilities suggest that cognitive-affective factors such as intolerance of uncertainty underlie generalized anxiety disorder and eating disorders95. However, these models are based on latent variable theory, which does not allow for specific tests of how one illness progresses to the other via symptoms as mechanisms.
By contrast, network theory suggests that comorbidity across multiple illnesses is maintained and spread through specific symptom relationships72,74, and network analysis offers a way to quantify these relationships. For example, from a network theory perspective one could hypothesize that cognitions focused on body shape disturbance (observable symptom characteristic of anorexia nervosa) might lead to fear of judgment (observable symptom characteristic of social anxiety disorder), which then leads to behavioral restriction and avoiding situations in which one might be scrutinized. From this perspective, it is easy to imagine how symptoms of one illness could spread to another (see ref74 for additional examples).
Research has begun to examine how symptoms of comorbid internalizing and externalizing disorders relate to eating disorder symptoms. There have been investigations of the relationships between symptoms of eating disorders and post-traumatic stress disorder96, social anxiety disorder97, obsessive-compulsive disorder98,99, trait anxiety100,101, worry102, depression101,103, and alcohol use symptoms104. This research can pinpoint specific bridge symptoms (or illness pathways according to network theory) that are theorized to spread from one cluster of symptoms to another. Pinpointing these symptoms has high clinical utility as they can be conceptualized as potential treatment targets that can disrupt the spread of one illness to another.
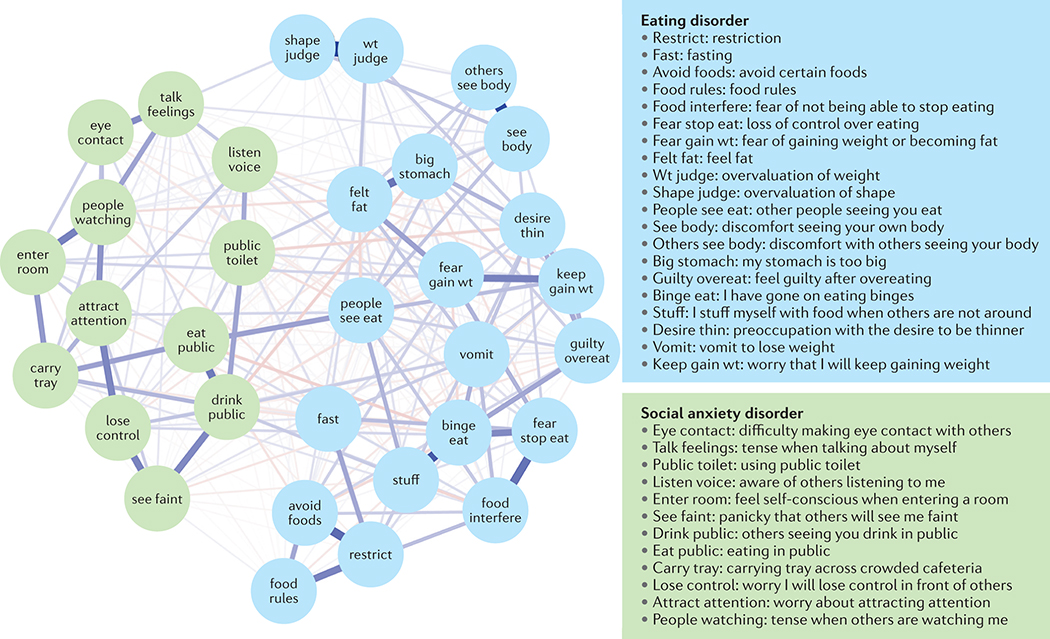
For example, difficulty eating and drinking in public were identified as bridge symptoms between social anxiety disorder and eating disorder symptoms (see Figure 2)97. Thus, according to network theory interventions that address difficulty eating and drinking in public (such as exposure therapy105) should weaken symptom relations among social anxiety disorder and eating disorders. In other words, intervention upon eating and drinking in public should be the ‘best bet’ treatment target to maximally disrupt both social anxiety and eating disorder symptoms. This type of treatment avenue that targets shared symptoms is exciting, given that traditionally therapists would need to target one illness at a time. By contrast, intervention on shared symptom targets should treat both disorders simultaneously, which could lead to more effective treatment, lower rates of relapse, and less time in treatment. However, no work to date has conclusively shown that intervention on central or bridge symptoms will be more effective than intervention on non-central symptoms. It might be necessary to work on more proximal symptoms either first or in addition to central symptoms.
Figure 2. A network of eating disorder and social anxiety disorder symptoms.
This network shows symptoms of eating disorder (20 symptoms) and social anxiety disorder (12 symptoms) based on data from clinical (n = 508) and non-clinical (n = 1707) individuals. Red lines indicate negative associations between symptoms; blue lines indicate positive associations between symptoms; thicker lines indicate stronger associations. Adapted from ref97 with permission, PUBLISHER
Similarly, network theory mitigates issues related to diagnostic migration. Instead of understanding eating disorders as diagnostic categories where an individual may or may not meet criteria for a specific disorder, conceptualizing illness at the level of symptoms (or mechanisms) allows for a more precise understanding of how symptoms within and across eating disorder categories change or stay stable. For example, relying on latent variable theory a clinician might notice that a patient who previously had a diagnosis of anorexia nervosa (symptoms of restriction, fear of weight gain, and low weight) now has a diagnosis of bulimia nervosa (restriction, fear of weight gain, binge eating, and purging). By contrast, network theory and analysis capture how symptoms of restriction and fear of weight gain might lead directly to binge eating and purging and how these dynamics might change over time. Instead of clinicians deciding if they should treat anorexia nervosa or bulimia nervosa, there can be explicit guidance on which symptoms, regardless of diagnosis, should be targeted in treatment.
Heterogeneity in idiographic networks
Perhaps the most exciting application of network theory is the extension of network analysis from cross-sectional to idiographic networks. Heterogeneity in eating disorders is high46,56,106. Even within similar diagnoses, symptom profiles are drastically different57,107. Practically, this means that when a patient presents for treatment, a categorical diagnosis does little to provide the clinician with guidance on what to target in treatment. Instead, clinicians are left to use their judgment to personalize treatment and/or modify existing evidence-based treatments to fit their specific patient, despite data showing that clinician judgment is biased (that is, clinicians do not select the best treatment targets and generally use similar treatments regardless of patient presentation or needs)108–110. An idiographic (within-one person) approach to conceptualizing and treating patients has the potential to overcome these barriers, promote understanding of heterogeneity and treat symptoms relevant for the individual111.
Idiographic networks estimate symptom dynamics within a unit of time (contemporaneous networks; symptom relations not attributed to temporal effects) and across time (temporal networks; symptom relations predicted from one time point to another; see Figure 1C) by applying vector autoregressive models to individual time-series data112,113. In other words, idiographic networks move from a static point in time (as in cross-sectional networks) and from a group-based or average level to an individual level. Strength centrality is used to measure central symptoms within contemporaneous networks, and out-strength (the degree a symptom predicts other symptoms) and in-strength (the degree a symptom is influenced by other nodes) measure central symptoms in temporal networks114,115.
For example, Figure 1c depicts a conceptual model of temporal associations among symptoms that might present in bulimia nervosa. Although conclusions cannot be made based on visual inspection alone, it appears that guilt might have the highest in-strength because it has the most edges pointing toward it. Binge eating and purging might have the highest out-strength because the most edges extend outward from these nodes. These relations may indicate that binge eating and purging are exerting the most influence on other symptoms, whereas the feeling of guilt might be the most sensitive to eating disorder behaviors. This interpretation differs from the model displayed in Figure 1b primarily because the edges are directed, possibly indicating causal relations among nodes. Thus, Figure 1c shows how symptoms might relate to each other across time, in contrast to Figure 1b which shows the general strength of symptom relations agnostic to temporality.
Multilevel vector autoregressive models combine idiographic and nomothetic approaches by estimating within person networks and a group network, where node connections represent the standard deviation of individual effects116. Stronger connections between nodes indicate increased person-specific variability relative to the group (average) network116. This type of shift is important because it means that clinical researchers can build person-specific treatments instead of relying on data based on group averages. Idiographic networks are especially promising for addressing diagnostic heterogeneity with personalized medicine, such that therapeutic interventions could be tailored to an individual’s symptom dynamics81,82,113. For example, we can identify if fear of weight gain predicts increased engagement in purging for a patient with an eating disorder presentation that includes purging, whereas we can identify if social fears predicts restriction for this type of eating disorder presentation.
Idiographic network analyses turn one individual’s data into its own dataset (rather than combining multiple individuals’ data into one dataset) by drawing on intensive longitudinal data collection methods (ecological momentary assessment or multiple assessments usually within one day for several weeks)113,115,117,118. Thus, idiographic network analysis can identify symptoms that maintain the illness within one person which might be causal factors for developing or worsening additional symptoms. Idiographic network analysis can also identify co-occurring symptoms (for example, anxiety and depression) and underlying mechanisms or core beliefs (for example, fear of losing control or fear of weight gain) both within seconds (contemporaneous models) and over time (temporal models). Both of these models are important because we can identify how cognitions, behavior, affect, and co-occurring conditions occur across seconds (contemporaneous) and longer time periods, such as hours (temporal). Heterogeneous behaviors operate on different time scales119,120 and therefore the ability to model multiple time scales is needed.
Idiographic networks can address problems caused by the high comorbidity between eating disorders and other types of psychopathology and diagnostic migration. Instead of focusing on one categorical disorder or the other (for example, should a clinician target social anxiety disorder or an eating disorder first?), eating disorder psychopathology is translated to the symptom level, where categories are no longer needed. This use is similar to that of bridge symptoms in cross-sectional networks, except that it can be applied on the individual-level to make inferences about individuals, rather than groups. Idiographic networks can include any symptoms of relevance (selected by the researcher, clinician, and/or patient; see ref121 for a discussion of how to combine clinician and patient report into networks) and identify precisely which symptoms should be targeted, regardless of whether the symptom falls into a specific category of illness. This type of thinking is not new for clinicians. However, it is a huge shift for clinical researchers who generally develop treatments based on group averages and insurance companies who traditionally rely on diagnostic categories to determine if a patient should receive coverage.
Implications for clinical practice
Next, we discuss direct clinical implications stemming from the use of network theory for eating disorders, and how network theory ‘fits’ with current evidence-based practices. Although we focus on CBT and its extensions, we think that network theory can also be extended to many other symptom-based treatments, such as interpersonal treatments and the Unified Protocol.
Most practicing clinicians are familiar with cognitive behavior theory and the model extending from this theory122. Cognitive behavior theory forms the basis for CBT, and third wave therapies such as dialectical behavior therapy (DBT)123 and acceptance and commitment therapy (ACT)124. In the cognitive behavior model, a reinforcing cycle of behaviors, affect, cognitions, and physiology drives pathology125,126. Each of these model components are reinforced and maintained by core beliefs126. For example, in the case of an eating disorder the cognition ‘I am fat’ might cause the behavior ‘restriction’, which then leads to the emotion ‘anxiety,’ which changes physiology (for example, increased gastric sensations), ultimately feeding back into the perception of being fat. Importantly, all of these behaviors, cognitions, affect, and physiology are theorized to stem from core beliefs (deeply rooted schemas one holds about themselves, others, and the world126,127). According to cognitive-behavioral theory, modification of cognitions and behaviors is possible128,129. For example, it is possible to change behaviors and cognitions to disrupt the reinforcing cycle. Crucially, it is theorized that intervention on core beliefs, which is the ultimate target of treatment, should disrupt the entire negative reinforcement cycle more than intervention on more proximal symptoms (such as automatic thoughts or cognitions, and behaviors)126,127.
The basic tenets of the cognitive behavior model map onto network theory. Network theory also hypothesizes that pathology symptoms (cognitions, behavior, affect, and physiology) dynamically interact with each other to strengthen and ultimately maintain pathology72. However, the terminology differs (Figure 3). For example, in network theory a symptom is a node, whereas in cognitive behavior theory a symptom is categorized as a cognition, behavior, emotion, or physiological symptom. In network theory pathways among symptoms are partial correlation values, which are represented by double arrows in a cognitive behavior theory model. Importantly, in network theory central symptoms are hypothesized to maintain all other symptoms73,83,130. Practically, this means that identifying central symptoms, and intervention on such symptoms, should maximize the impact of the intervention on all other symptoms because it directly causes the rest of the symptoms in the network. This definition is entirely consistent with core beliefs (which correspond to central symptoms) in cognitive behavior theory126,127. By extension, network theory can also be used to evaluate how symptoms interact as conceptualized through the lens of other treatment approaches, such as DBT and ACT. Thus, networks theory allows empirical evaluation of case conceptualizations derived from CBT, DBT, or ACT modalities.
Figure 3. Cognitive behavior and network models of eating disorders.
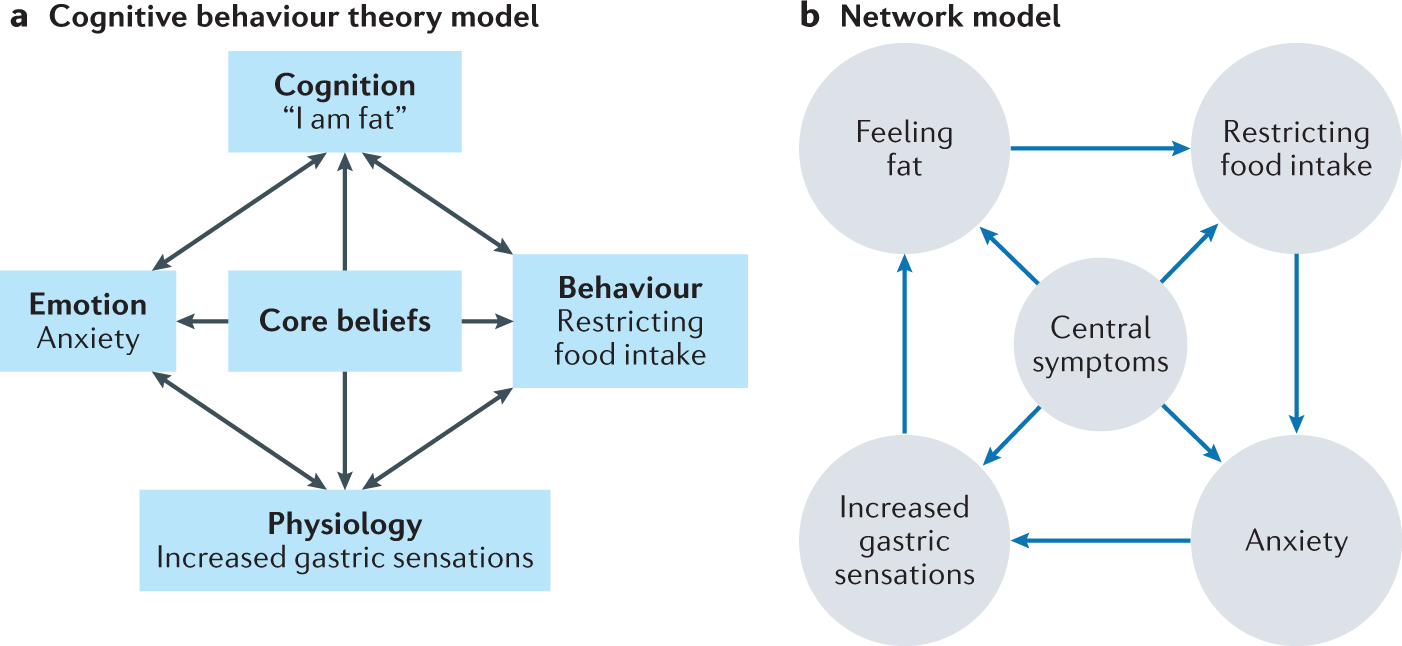
A) A conceptual model of an eating disorder using cognitive behavior theory. Eating disorder symptoms (cognitions, behaviors, emotions, and physiology) are represented in rectangles. B) A conceptual model of an eating disorder using network theory. Within a network model, symptoms are represented by nodes (circles). The directed lines connecting nodes represent partial correlations between nodes in the network model.
Finally, one of the most difficult parts of a clinician’s job is deciding on their own (in private practice) or as part of an interdisciplinary treatment team (generally used in more intensive outpatient, inpatient and residential eating disorder treatments 131,132) which eating disorder symptoms should be addressed, and when (for example, after how many sessions) to make adjustments to maximize and hasten change for a patient. Research on this issue shows that clinicians generally believe they have above average clinical skills133. However, when clinical decision-making via a team-based strategy involving expert clinicians is compared to data-driven approaches, data-driven approaches outperform clinician judgment134. These data are reinforced by a large literature showing that clinician judgment is flawed108,135,136 and research showing that an artificial intelligence approach to matching therapists to patients outperforms selection via a team of clinicians with substantial clinical expertise137,138. Together, this research suggests that a clinician-guidance system that uses idiographic data to bolster decision making on what symptoms to target and when could significantly improve clinical practice and outcomes.
A clinician-guidance system along these lines is clearly needed for eating disorders. Only 50% of patients respond to evidence based treatments23,139, there are no evidence-based treatments for adult anorexia nervosa139–141, and up to 60% of patients relapse after treatment24. Moreover, most eating disorders are treated through team-based eating disorder specialty care (a team generally compromising therapist, dietitian, physician, and prescriber who meet to decide on treatment goals and interventions)131 Instead of spending treatment team time deciding what to target, this could be decided using idiographic models, which would free-up significant clinician time. Thus, using idiographic network analysis as an algorithm to guide such decision-making has the potential to make a large impact on treatment effectiveness and efficiency by matching symptom targets to evidence-based treatments. Instead of relying on guess-work, clinicians would have a data-driven way to decide what to target in treatment.
For example, instead of using the CBT model to guide which symptoms should be targeted, idiographic network analysis can quantify symptom connections using data collected at the beginning of treatment to show how symptoms relate to each other. Then, treatment targets can be selected based on centrality indices that show how targeting particular symptoms will impact the entire symptom cycle. These targets can then be matched to personalized evidence-based interventions.
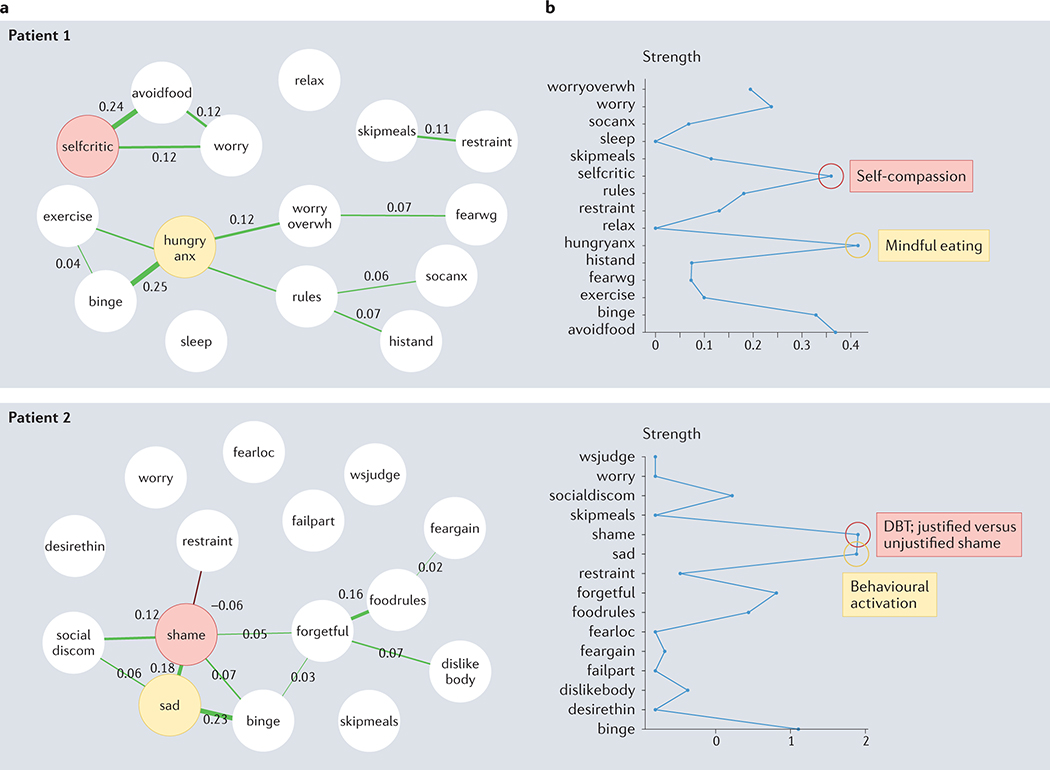
Figure 4a shows network data from two patients with a diagnosis of bulimia nervosa. The first participant’s network identified shame and sadness as the most central symptoms (Figure 4b). Therefore, corresponding interventions of DBT-justified vs unjustified shame (identifying if shame is rationale or irrational) and behavioral activation (engaging in pleasurable daily activities) were delivered. The second participant had drastically different central symptoms: hunger anxiety and self-criticism (Figure 4b). As such, mindful eating (purposefully attending to the food one is eating) and self-compassion (approaching oneself in a non-judgmental and kind manner) interventions were delivered. Thus, the selection of treatment modules varies considerably depending on symptom presentation. By contrast, a CBT model would treat these patients in a standardized manner, starting with teaching regular eating, then moving to challenging thoughts; this would not address the most crucial aspects of the individuals’ disorder.
Figure 4. Example idiographic networks of an eating disorder and comorbid symptoms.
a) Symptom networks for two white, female patients in their late 30s diagnosed with bulimia nervosa. b) Plots of symptom strength centrality. The two most central symptoms for each patient and the corresponding evidence-based treatment are shown in red and yellow. selfcritic = self-criticism; hungry anx = hunger anxiety; shame = feeling of shame; sad = feeling sadness; DBT = dialectical behavioural therapy.
To implement such methods in ‘real life’ clinical practice, data can be collected via ecological momentary assessment through a smart phone application. Any questions deemed relevant by the clinician can be assessed (we use a standard set of questions in our research142). These data can then be run through a network algorithm that provides information on which central symptoms to target in treatment. Advanced technologies, such as mobile apps combined with software that can integrate advanced algorithms into user-friendly formats, can transform network analyses into an easy to use system for clinicians that does not require any knowledge of network statistics. We envision (and are working on developing) a system that automatically collects data via a smart-phone application and outputs central symptoms and treatment recommendations. Outputted networks and central symptoms can be used with patients for case conceptualization and psychoeducation about their illness. Future research is needed on how to develop and effectively deliver such a system. Importantly, clinician input is needed to ensure that this system bridges the research-practice gap. For example, recent research found that clinicians were hesitant to apply a network model in clinical care81,143; therefore including clinician input is needed to increase uptake.
Conclusions
Eating disorders are highly comorbid with additional psychiatric disorders27, diagnostic migration is common, and there is high heterogeneity of symptom presentation. The field has been stymied by addressing these issues solely from a latent variable and categorical approach. Network theory provides a new theoretical conceptualization of each of these issues, and network analysis provides a corresponding analytic framework to address questions about comorbidity, migration, and heterogeneity from a symptom perspective. Understanding and treating eating disorders lag behind many other psychiatric illnesses. Thus, these are welcome and exciting approaches to help build better and more personalized treatments for those with eating disorders.
The eating disorder field is not alone in its ability to benefit from network theory and analysis. Comorbidity is high across all psychiatric illnesses, patients change from one illness presentation to another, and heterogeneity of mental disorders is both a historic and present issue in psychopathology91. For instance, there are currently 636,120 ways an individual can meet the DSM-571 criteria for PTSD144, which means that any two individuals with PTSD will likely have different symptom dynamics. Many voices have echoed the limitations of a categorical approach to psychiatric illness56,145,146. Network theory and analysis offers an opportunity to turn toward a new way of thinking that coincides with cognitive behavior theory and is familiar to practicing clinicians. We hope that researchers and clinicians alike will embrace such a shift in thinking to improve mental health care for all.
Although we are enthusiastic about the promise of network analysis, most of the ideas presented here are tentative and need to be corroborated by future research. There is research showing how cross-sectional network analysis can be used to conceptualize eating disorders82 and comorbid disorders97,100 and how idiographic networks can be used to personalize treatment142. However, there has been no research testing if targeting bridge symptoms can disrupt the flow of symptoms from one illness to another, or testing which symptoms and/or relationships in a network model should be targeted to produce the most effective outcomes. For example, fears of social eating and drinking bridge between social anxiety and eating disorder symptoms97. The next step in this research is to test whether interventions that target fears of social eating have a stronger impact on overall eating disorder and social anxiety symptoms than interventions that target eating and social anxiety disorder symptoms more generally or one at a time (for example, first treating eating disorder symptoms and then treating social anxiety disorder symptoms). Similarly, we are unaware of any research using network analysis to understand diagnostic migrations for eating disorders, despite the strong rationale to do so.
Research using idiographic network analysis to personalize treatment is similarly in its infancy. We are only aware of one published study147 and one ongoing clinical trial from our team using these methods to personalize treatment. Many questions remain unanswered, such as how to best use idiographic methods to personalize treatment (for example, which type of centrality should be used or should centrality be used at all?), whether personalized treatments outperform standardized evidence based treatments such as CBT, and whether receiving personalized feedback on its own (regardless of intervention) outperforms treatment as usual. Future research should address these important questions within eating disorders and other areas of clinical psychology.
Finally, there are limitations to network analytic methods, many of which been described elsewhere119,148. Three caveats are especially relevant here. First, there has been a lot of discussion on the limits of network analysis because it is new (see ref120 for a review), but all statistical methodologies have inherent limitations. Having experienced the growth in the use of network analysis and the expansion of tools available to answer theoretical questions, we are excited by the prospect of what future methodological advances hold. Ideally those developing these methods will work closely with clinical researchers so that these methods are suited for and can be readily applied to important clinical questions.
Second, many studies using network methods have been cross-sectional and so cannot provide insights on causality. Nevertheless, these ‘snapshots’ of time can provide important data on the structure of pathology stemming from a symptom-based approach, and can guide which symptoms are assessed in prospective and experimental research. For example, our first use of network theory and analysis showed that ‘fear of weight gain’ was a central symptom in a cross-sectional network149; those data have since sparked an important line of research showing that fear of weight gain can be targeted successfully in exposure treatment for eating disorders105.
Third, there is no evidence that centrality will translate to modifiable and important treatment targets, as suggested by network theory119,148,150. However, there is growing evidence that network-identified central symptoms predict eating disorder (and other psychiatric illness) outcomes151. It is notoriously difficult to predict eating disorder outcomes and the fact that network analysis can do so suggests that centrality has strong construct validity. Future experimental and treatment research that investigates the role of centrality is needed.
Ideally, knowledge gained from network models should be complemented by intervention, experimental, simulation, and causal relations approaches to derive the ideal treatment targets152–155. Additionally, other models, such as hierarchical taxonomy of psychopathology (HITOP)156, could be considered along with network theory. However, HITOP does not rely on a symptom-based approach, which separates network theory from many other existing dimensional theories and models. Most importantly, researchers must use a method that answers their theoretically-based questions, many of which are well suited to network analysis.
Acknowledgements
The authors thank all of our participants and patients who have helped us formulate these ideas. The authors also thank the EAT lab for providing support, collaboration, and an environment focused on positive change.
Footnotes
Competing interests
The authors declare no competing interests.
References
- 1.Arcelus J, Mitchell AJ, Wales J & Nielsen S Mortality Rates in Patients With Anorexia Nervosa and Other Eating Disorders: A Meta-analysis of 36 Studies. Arch. Gen. Psychiatry 68, 724–731 (2011). [DOI] [PubMed] [Google Scholar]
- 2.Smink FRE, van Hoeken D & Hoek HW Epidemiology of Eating Disorders: Incidence, Prevalence and Mortality Rates. Curr. Psychiatry Rep. 14, 406–414 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fichter MM, Quadflieg N & Hedlund S Long-term course of binge eating disorder and bulimia nervosa: relevance for nosology and diagnostic criteria. Int. J. Eat. Disord. 41, 577–586 (2008). [DOI] [PubMed] [Google Scholar]
- 4.Suokas JT et al. Mortality in eating disorders: a follow-up study of adult eating disorder patients treated in tertiary care, 1995–2010. Psychiatry Res. 210, 1101–1106 (2013). [DOI] [PubMed] [Google Scholar]
- 5.Roberts ME, Tchanturia K, Stahl D, Southgate L & Treasure J A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol. Med. 37, 1075–1084 (2007). [DOI] [PubMed] [Google Scholar]
- 6.Rosval L et al. Impulsivity in women with eating disorders: problem of response inhibition, planning, or attention? Int. J. Eat. Disord. 39, 590–593 (2006). [DOI] [PubMed] [Google Scholar]
- 7.Tchanturia K et al. An investigation of decision making in anorexia nervosa using the Iowa Gambling Task and skin conductance measurements. J. Int. Neuropsychol. Soc. JINS 13, 635–641 (2007). [DOI] [PubMed] [Google Scholar]
- 8.Keel PK, Mitchell JE, Miller KB, Davis TL & Crow SJ Social adjustment over 10 years following diagnosis with bulimia nervosa. Int. J. Eat. Disord. 27, 21–28 (2000). [DOI] [PubMed] [Google Scholar]
- 9.de la Rie S, Noordenbos G, Donker M & van Furth E The patient’s view on quality of life and eating disorders. Int. J. Eat. Disord. 40, 13–20 (2007). [DOI] [PubMed] [Google Scholar]
- 10.Klump KL, Bulik CM, Kaye WH, Treasure J & Tyson E Academy for eating disorders position paper: Eating disorders are serious mental illnesses. Int. J. Eat. Disord. 42, 97–103 (2009). [DOI] [PubMed] [Google Scholar]
- 11.Tyler I, Wiseman MC, Crawford RI & Birmingham CL Cutaneous manifestations of eating disorders. J. Cutan. Med. Surg. 6, 345–353 (2002). [DOI] [PubMed] [Google Scholar]
- 12.Lifante-Oliva C, López-Jornet P, Camacho-Alonso F & Esteve-Salinas J Study of oral changes in patients with eating disorders. Int. J. Dent. Hyg. 6, 119–122 (2008). [DOI] [PubMed] [Google Scholar]
- 13.Powers PS Osteoporosis and eating disorders. J. Pediatr. Adolesc. Gynecol. 12, 51–57 (1999). [DOI] [PubMed] [Google Scholar]
- 14.Awazu M, Matsuoka S, Kamimaki T, Watanabe H & Matsuo N Absent circadian variation of blood pressure in patients with anorexia nervosa. J. Pediatr. 136, 524–527 (2000). [DOI] [PubMed] [Google Scholar]
- 15.Muuss RE Adolescent eating disorder: Anorexia nervosa. Adolescence 20, 525–536 (1985). [PubMed] [Google Scholar]
- 16.Braude MR et al. Acute medical stabilisation of adults with anorexia nervosa: experience of a defined interdisciplinary model of care. Intern. Med. J. 50, 77–85 (2020). [DOI] [PubMed] [Google Scholar]
- 17.Mitchell JE, Pomeroy C & Huber M A clinician’s guide to the eating disorders medicine cabinet. Int. J. Eat. Disord. 7, 211–223 (1988). [Google Scholar]
- 18.Swenne I Poor catch-up growth in late adolescent boys with eating disorders, weight loss and stunting of growth. Eur. Eat. Disord. Rev. 21, 395–398 (2013). [DOI] [PubMed] [Google Scholar]
- 19.Tith RM et al. Association of Bulimia Nervosa With Long-term Risk of Cardiovascular Disease and Mortality Among Women. JAMA Psychiatry 77, 44–51 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tabler J, Utz RL, Smith KR, Hanson HA & Geist C Variation in reproductive outcomes of women with histories of bulimia nervosa, anorexia nervosa, or eating disorder not otherwise specified relative to the general population and closest-aged sisters. Int. J. Eat. Disord. 51, 102–111 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Porcelli P, Leandro G & De Carne M Functional Gastrointestinal Disorders and Eating Disorders: Relevance of the Association in Clinical Management. Scand. J. Gastroenterol. 33, 577–582 (1998). [DOI] [PubMed] [Google Scholar]
- 22.Coffino JA, Udo T & Grilo CM Rates of Help-Seeking in US Adults With Lifetime DSM-5 Eating Disorders: Prevalence Across Diagnoses and Differences by Sex and Ethnicity/Race. Mayo Clin. Proc. 94, 1415–1426 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van den Berg E et al. Meta-analysis on the efficacy of psychological treatments for anorexia nervosa. Eur. Eat. Disord. Rev. 27, 331–351 (2019). [DOI] [PubMed] [Google Scholar]
- 24.McFarlane T, Olmsted MP & Trottier K Timing and prediction of relapse in a transdiagnostic eating disorder sample. Int. J. Eat. Disord. 41, 587–593 (2008). [DOI] [PubMed] [Google Scholar]
- 25.Streatfeild J et al. Social and economic cost of eating disorders in the United States: Evidence to inform policy action. Int. J. Eat. Disord. 54, 851–868 (2021). [DOI] [PubMed] [Google Scholar]
- 26.Fried EI Lack of Theory Building and Testing Impedes Progress in The Factor and Network Literature. Psychol. Inq. 31, 271–288 (2020). [Google Scholar]
- 27.Hudson JI, Hiripi E, Pope HG & Kessler RC The Prevalence and Correlates of Eating Disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 61, 348–358 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Godart NT, Flament MF, Perdereau F & Jeammet P Comorbidity between eating disorders and anxiety disorders: A review. Int. J. Eat. Disord. 32, 253–270 (2002). [DOI] [PubMed] [Google Scholar]
- 29.Kaye WH, Bulik CM, Thornton L, Barbarich N & Masters K Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am. J. Psychiatry 161, 2215–2221 (2004). [DOI] [PubMed] [Google Scholar]
- 30.Kerr-Gaffney J, Harrison A & Tchanturia K Social anxiety in the eating disorders: a systematic review and meta-analysis. Psychol. Med. 48, 2477–2491 (2018). [DOI] [PubMed] [Google Scholar]
- 31.Mandelli L, Draghetti S, Albert U, De Ronchi D & Atti A-R Rates of comorbid obsessive-compulsive disorder in eating disorders: A meta-analysis of the literature. J. Affect. Disord. 277, 927–939 (2020). [DOI] [PubMed] [Google Scholar]
- 32.Ruffolo JS, Phillips KA, Menard W, Fay C & Weisberg RB Comorbidity of body dysmorphic disorder and eating disorders: Severity of psychopathology and body image disturbance. Int. J. Eat. Disord. 39, 11–19 (2006). [DOI] [PubMed] [Google Scholar]
- 33.Mitchell KS, Mazzeo SE, Schlesinger MR, Brewerton TD & Smith BN Comorbidity of partial and subthreshold ptsd among men and women with eating disorders in the national comorbidity survey-replication study: PTSD and Eating Disorders in Men and Women. Int. J. Eat. Disord. 45, 307–315 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeSocio JE Challenges in diagnosis and treatment of comorbid eating disorders and mood disorders. Perspect. Psychiatr. Care 55, 494–500 (2019). [DOI] [PubMed] [Google Scholar]
- 35.McElroy SL, Kotwal R, Keck PE & Akiskal HS Comorbidity of bipolar and eating disorders: distinct or related disorders with shared dysregulations? J. Affect. Disord. 86, 107–127 (2005). [DOI] [PubMed] [Google Scholar]
- 36.McElroy SL et al. Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. J. Affect. Disord. 128, 191–198 (2011). [DOI] [PubMed] [Google Scholar]
- 37.Bleck JR, DeBate RD & Olivardia R The Comorbidity of ADHD and Eating Disorders in a Nationally Representative Sample. J. Behav. Health Serv. Res. 42, 437–451 (2015). [DOI] [PubMed] [Google Scholar]
- 38.Brewerton TD & Duncan AE Associations between Attention Deficit Hyperactivity Disorder and Eating Disorders by Gender: Results from the National Comorbidity Survey Replication: ADHD and Eating Disorders by Gender. Eur. Eat. Disord. Rev. 24, 536–540 (2016). [DOI] [PubMed] [Google Scholar]
- 39.Bahji A et al. Prevalence of substance use disorder comorbidity among individuals with eating disorders: A systematic review and meta-analysis. Psychiatry Res. 273, 58–66 (2019). [DOI] [PubMed] [Google Scholar]
- 40.Cassin S & Vonranson K Personality and eating disorders: A decade in review. Clin. Psychol. Rev. 25, 895–916 (2005). [DOI] [PubMed] [Google Scholar]
- 41.Sansone RA, Levitt JL & Sansone LA The Prevalence of Personality Disorders Among Those with Eating Disorders. Eat. Disord. 13, 7–21 (2004). [DOI] [PubMed] [Google Scholar]
- 42.O’Brien KM & Vincent NK Psychiatric comorbidity in anorexia and bulimia nervosa: nature, prevalence, and causal relationships. Clin. Psychol. Rev. 23, 57–74 (2003). [DOI] [PubMed] [Google Scholar]
- 43.Fairburn CG, Cooper Z & Shafran R Cognitive behaviour therapy for eating disorders: a ‘transdiagnostic’ theory and treatment. Behav. Res. Ther. 41, 509–528 (2003). [DOI] [PubMed] [Google Scholar]
- 44.Lock J & le Grange D Family-based treatment of eating disorders. Int. J. Eat. Disord. 37, S64–S67 (2005). [DOI] [PubMed] [Google Scholar]
- 45.Herzog DB, Nussbaum KM & Marmor AK Comorbidity and outcome in eating disorders. Psychiatr. Clin. North Am. 19, 843–859 (1996). [DOI] [PubMed] [Google Scholar]
- 46.Carr MM & Grilo CM Examining heterogeneity of binge-eating disorder using latent class analysis. J. Psychiatr. Res. 130, 194–200 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Riesco N et al. Other Specified Feeding or Eating Disorders (OSFED): Clinical heterogeneity and cognitive-behavioral therapy outcome. Eur. Psychiatry 54, 109–116 (2018). [DOI] [PubMed] [Google Scholar]
- 48.Sysko R, Hildebrandt T, Wilson GT, Wilfley DE & Agras WS Heterogeneity moderates treatment response among patients with binge eating disorder. J. Consult. Clin. Psychol. 78, 681–690 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fairweather-Schmidt AK & Wade TD DSM-5 eating disorders and other specified eating and feeding disorders: Is there a meaningful differentiation?: Dsm-5 Eating Disorders and Osfed. Int. J. Eat. Disord. 47, 524–533 (2014). [DOI] [PubMed] [Google Scholar]
- 50.Thomas JJ, Vartanian LR & Brownell KD The relationship between eating disorder not otherwise specified (EDNOS) and officially recognized eating disorders: Meta-analysis and implications for DSM. Psychol. Bull 135, 407–433 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Galmiche M, Déchelotte P, Lambert G & Tavolacci MP Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am. J. Clin. Nutr. 109, 1402–1413 (2019). [DOI] [PubMed] [Google Scholar]
- 52.Fairburn CG & Cooper Z Eating disorders, DSM–5 and clinical reality. Br. J. Psychiatry 198, 8–10 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keel PK, Brown TA, Holm-Denoma J & Bodell LP Comparison of DSM-IV versus proposed DSM-5 diagnostic criteria for eating disorders: Reduction of eating disorder not otherwise specified and validity. Int. J. Eat. Disord. 44, 553–560 (2011). [DOI] [PubMed] [Google Scholar]
- 54.Frank GKW, Shott ME & DeGuzman MC The neurobiology of eating disorders. Child Adolesc. Psychiatr. Clin. N. Am. 28, 629–640 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brooks SJ, Rask-Andersen M, Benedict C & Schiöth HB A debate on current eating disorder diagnoses in light of neurobiological findings: is it time for a spectrum model? BMC Psychiatry 12, 76 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Forbush KT et al. Understanding eating disorders within internalizing psychopathology: A novel transdiagnostic, hierarchical-dimensional model. Compr. Psychiatry 79, 40–52 (2017). [DOI] [PubMed] [Google Scholar]
- 57.Levinson CA, Vanzhula I & Brosof LC Longitudinal and personalized networks of eating disorder cognitions and behaviors: Targets for precision intervention a proof of concept study. Int. J. Eat. Disord. 51, 1233–1243 (2018). [DOI] [PubMed] [Google Scholar]
- 58.Wilson GT, Grilo CM & Vitousek KM Psychological treatment of eating disorders. Am. Psychol. 62, 199–216 (2007). [DOI] [PubMed] [Google Scholar]
- 59.Keel PK & Mitchell JE Outcome in bulimia nervosa. Am. J. Psychiatry 154, 313–321 (1997). [DOI] [PubMed] [Google Scholar]
- 60.Keel PK, Dorer DJ, Franko DL, Jackson SC & Herzog DB Postremission predictors of relapse in women with eating disorders. Am. J. Psychiatry 162, 2263–2268 (2005). [DOI] [PubMed] [Google Scholar]
- 61.Carter JC et al. A prospective study of predictors of relapse in anorexia nervosa: implications for relapse prevention. Psychiatry Res. 200, 518–523 (2012). [DOI] [PubMed] [Google Scholar]
- 62.Eddy KT et al. Diagnostic Crossover in Anorexia Nervosa and Bulimia Nervosa: Implications for DSM-V. Am. J. Psychiatry 165, 245–250 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Plessow F & Eddy KT Diagnostic Crossover. in Encyclopedia of Feeding and Eating Disorders (ed. Wade T) 1–5 (Springer Singapore, 2016). doi: 10.1007/978-981-287-087-2_122-1. [DOI] [Google Scholar]
- 64.Castellini G et al. Diagnostic Crossover and Outcome Predictors in Eating Disorders According to DSM-IV and DSM-V Proposed Criteria: A 6-Year Follow-Up Study. Psychosom. Med. 73, 270–279 (2011). [DOI] [PubMed] [Google Scholar]
- 65.Tozzi F et al. Symptom Fluctuation in Eating Disorders: Correlates of Diagnostic Crossover. Am. J. Psychiatry 162, 732–740 (2005). [DOI] [PubMed] [Google Scholar]
- 66.Stice E, Marti CN, Shaw H & Jaconis M An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J. Abnorm. Psychol. 118, 587–597 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bulik CM, Sullivan PF, Fear J & Pickering A Predictors of the Development of Bulimia Nervosa in Women with Anorexia Nervosa: J. Nerv. Ment. Dis. 185, 704–707 (1997). [DOI] [PubMed] [Google Scholar]
- 68.Strober M, Freeman R & Morrell W The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int. J. Eat. Disord. 22, 339–360 (1997). [DOI] [PubMed] [Google Scholar]
- 69.Forbush KT et al. A new approach to eating-disorder classification: Using empirical methods to delineate diagnostic dimensions and inform care. Int. J. Eat. Disord. 51, 710–721 (2018). [DOI] [PubMed] [Google Scholar]
- 70.Milos G, Spindler A, Schnyder U & Fairburn CG Instability of eating disorder diagnoses: prospective study. Br. J. Psychiatry 187, 573–578 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. (American Psychiatric Association, 2013). [Google Scholar]
- 72.Borsboom D & Cramer AOJ Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annu. Rev. Clin. Psychol. 9, 91–121 (2013). [DOI] [PubMed] [Google Scholar]
- 73.Bringmann LF & Eronen MI Don’t blame the model: Reconsidering the network approach to psychopathology. Psychol. Rev. 125, 606–615 (2018). [DOI] [PubMed] [Google Scholar]
- 74.Borsboom D A network theory of mental disorders. World Psychiatry 16, 5–13 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jones PJ & Robinaugh DR An Answer to “So What?” Implications of Network Theory for Research and Practice. FOCUS 19, 204–210 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Epskamp S, Borsboom D & Fried EI Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 50, 195–212 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Guyon H, Falissard B & Kop J-L Modeling Psychological Attributes in Psychology – An Epistemological Discussion: Network Analysis vs. Latent Variables. Front. Psychol. 8, 798 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Costantini G et al. State of the aRt personality research: A tutorial on network analysis of personality data in R. J. Res. Personal. 54, 13–29 (2015). [Google Scholar]
- 79.Cramer AOJ et al. Dimensions of Normal Personality as Networks in Search of Equilibrium: You Can’t like Parties if you Don’t like People. Eur. J. Personal. 26, 414–431 (2012). [Google Scholar]
- 80.van Bork R et al. Latent Variable Models and Networks: Statistical Equivalence and Testability. Multivar. Behav. Res. 56, 175–198 (2021). [DOI] [PubMed] [Google Scholar]
- 81.Burger J et al. Bridging the gap between complexity science and clinical practice by formalizing idiographic theories: a computational model of functional analysis. BMC Med. 18, 99 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Levinson CA, Vanzhula IA, Brosof LC & Forbush K Network analysis as an alternative approach to conceptualizing eating disorders: Implications for research and treatment. Curr. Psychiatry Rep. 20, 67 (2018). [DOI] [PubMed] [Google Scholar]
- 83.Cramer AOJ, Waldorp LJ, van der Maas HLJ & Borsboom D Comorbidity: a network perspective. Behav. Brain Sci. 33, 137–150; discussion 150–193 (2010). [DOI] [PubMed] [Google Scholar]
- 84.Keel PK & Brown TA Update on course and outcome in eating disorders. Int. J. Eat. Disord. 43, 195–204 (2010). [DOI] [PubMed] [Google Scholar]
- 85.Roy-Byrne PP et al. Lifetime panic–depression comorbidity in the National Comorbidity Survey: Association with symptoms, impairment, course and help-seeking. Br. J. Psychiatry 176, 229–235 (2000). [DOI] [PubMed] [Google Scholar]
- 86.Nock MK, Hwang I, Sampson NA & Kessler RC Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Mol. Psychiatry 15, 868–876 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kessler RC et al. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62, 593–602 (2005). [DOI] [PubMed] [Google Scholar]
- 88.Jones PJ, Ma R & McNally RJ Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivar. Behav. Res. 56, 353–367 (2021). [DOI] [PubMed] [Google Scholar]
- 89.Plana-Ripoll O et al. Exploring Comorbidity Within Mental Disorders Among a Danish National Population. JAMA Psychiatry 76, 259–270 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.van Loo HM, Romeijn J-W, de Jonge P & Schoevers RA Psychiatric comorbidity and causal disease models. Prev. Med. 57, 748–752 (2013). [DOI] [PubMed] [Google Scholar]
- 91.Lilienfeld SO The Research Domain Criteria (RDoC): an analysis of methodological and conceptual challenges. Behav. Res. Ther. 62, 129–139 (2014). [DOI] [PubMed] [Google Scholar]
- 92.Pallister E & Waller G Anxiety in the eating disorders: Understanding the overlap. Clin. Psychol. Rev. 28, 366–386 (2008). [DOI] [PubMed] [Google Scholar]
- 93.Bulik CM, Sullivan PF, Fear JL & Joyce PR Eating disorders and antecedent anxiety disorders: A controlled study. Acta Psychiatr. Scand. 96, 101–107 (1997). [DOI] [PubMed] [Google Scholar]
- 94.Levinson CA & Rodebaugh TL Social anxiety and eating disorder comorbidity: The role of negative social evaluation fears. Eat. Behav. 13, 27–35 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Konstantellou A, Campbell M, Eisler I, Simic M & Treasure J Testing a cognitive model of generalized anxiety disorder in the eating disorders. J. Anxiety Disord. 25, 864–869 (2011). [DOI] [PubMed] [Google Scholar]
- 96.Vanzhula IA, Calebs B, Fewell L & Levinson CA Illness pathways between eating disorder and post-traumatic stress disorder symptoms: Understanding comorbidity with network analysis. Eur. Eat. Disord. Rev. 27, 147–160 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Levinson CA et al. Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. Int. J. Eat. Disord. 51, 693–709 (2018). [DOI] [PubMed] [Google Scholar]
- 98.Meier M et al. Obsessive–compulsive symptoms in eating disorders: A network investigation. Int. J. Eat. Disord. 53, 362–371 (2020). [DOI] [PubMed] [Google Scholar]
- 99.Vanzhula IA, Kinkel-Ram SS & Levinson CA Perfectionism and Difficulty Controlling Thoughts Bridge Eating Disorder and Obsessive-Compulsive Disorder Symptoms: A Network Analysis. J. Affect. Disord. 283, 302–309 (2021). [DOI] [PubMed] [Google Scholar]
- 100.Forrest LN, Sarfan LD, Ortiz SN, Brown TA & Smith AR Bridging eating disorder symptoms and trait anxiety in patients with eating disorders: A network approach. Int. J. Eat. Disord. 52, 701–711 (2019). [DOI] [PubMed] [Google Scholar]
- 101.Levinson CA et al. The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. J. Abnorm. Psychol. 126, 340–354 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ralph-Nearman C, Williams BM, Ortiz AML, Smith AR & Levinson CA Pinpointing core and pathway symptoms among sleep disturbance, anxiety, worry, and eating disorder symptoms in anorexia nervosa and atypical anorexia nervosa. J. Affect. Disord. 294, 24–32 (2021). [DOI] [PubMed] [Google Scholar]
- 103.Sahlan RN et al. Disordered eating, self-esteem, and depression symptoms in Iranian adolescents and young adults: A network analysis. Int. J. Eat. Disord. 54, 132–147 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cusack CE, Christian C, Drake JE & Levinson CA A network analysis of eating disorder symptoms and co-occurring alcohol misuse among heterosexual and sexual minority college women. Addict. Behav. 118, 106867 (2021). [DOI] [PubMed] [Google Scholar]
- 105.Levinson CA et al. Eating disorder symptoms and core eating disorder fears decrease during online imaginal exposure therapy for eating disorders. J. Affect. Disord. 276, 585–591 (2020). [DOI] [PubMed] [Google Scholar]
- 106.Beltz AM, Moser JS, Zhu DC, Burt SA & Klump KL Using person-specific neural networks to characterize heterogeneity in eating disorders: Illustrative links between emotional eating and ovarian hormones. Int. J. Eat. Disord. 51, 730–740 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Levinson CA, Vanzhula IA, Smith TW & Stice E Group and longitudinal intra-individual networks of eating disorder symptoms in adolescents and young adults at-risk for an eating disorder. Behav. Res. Ther. 135, 103731 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fichter MM & Quadflieg N How precisely can psychotherapists predict the long-term outcome of anorexia nervosa and bulimia nervosa at the end of inpatient treatment? Int. J. Eat. Disord. 54, 535–544 (2021). [DOI] [PubMed] [Google Scholar]
- 109.Nakash O & Saguy T Social Identities of Clients and Therapists During the Mental Health Intake Predict Diagnostic Accuracy. Soc. Psychol. Personal. Sci. 6, 710–717 (2015). [Google Scholar]
- 110.Featherston R, Downie LE, Vogel AP & Galvin KL Decision making biases in the allied health professions: A systematic scoping review. PloS One 15, e0240716 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Molenaar PCMA Manifesto on Psychology as Idiographic Science: Bringing the Person Back Into Scientific Psychology, This Time Forever. Meas. Interdiscip. Res. Perspect. 2, 201–218 (2004). [Google Scholar]
- 112.Fried EI & Cramer AOJ Moving forward: challenges and directions for psychopathological network theory and methodology. Perspect. Psychol. Sci. J. Assoc. Psychol. Sci. 12, 999–1020 (2017). [DOI] [PubMed] [Google Scholar]
- 113.Epskamp S et al. Personalized Network Modeling in Psychopathology: The Importance of Contemporaneous and Temporal Connections. Clin. Psychol. Sci. J. Assoc. Psychol. Sci. 6, 416–427 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Epskamp S, Waldorp LJ, Mõttus R & Borsboom D The Gaussian Graphical Model in Cross-Sectional and Time-Series Data. Multivar. Behav. Res. 53, 453–480 (2018). [DOI] [PubMed] [Google Scholar]
- 115.Fisher AJ et al. Exploring the idiographic dynamics of mood and anxiety via network analysis. J. Abnorm. Psychol. 126, 1044–1056 (2017). [DOI] [PubMed] [Google Scholar]
- 116.Bringmann LF et al. A network approach to psychopathology: New insights into clinical longitudinal data. PLOS ONE 8, e60188 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Piccirillo ML & Rodebaugh TL Foundations of idiographic methods in psychology and applications for psychotherapy. Clin. Psychol. Rev. 71, 90–100 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Piccirillo ML, Beck ED & Rodebaugh TL A Clinician’s Primer for Idiographic Research: Considerations and Recommendations. Behav. Ther. 50, 938–951 (2019). [DOI] [PubMed] [Google Scholar]
- 119.Bringmann LF Person-specific networks in psychopathology: Past, present, and future. Curr. Opin. Psychol. 41, 59–64 (2021). [DOI] [PubMed] [Google Scholar]
- 120.Robinaugh DJ, Hoekstra RHA, Toner ER & Borsboom D The network approach to psychopathology: a review of the literature 2008–2018 and an agenda for future research. Psychol. Med. 50, 353–366 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Burger J et al. A clinical PREMISE for personalized models: Towards a formal integration of case formulations and statistical networks. (2021) doi: 10.31234/osf.io/bdrs7. [DOI] [PubMed] [Google Scholar]
- 122.Beck AT Cognitive Therapy: Past, Present, and Future. J. Consult. Clin. Psychol. 61, 194–98 (1993). [DOI] [PubMed] [Google Scholar]
- 123.Linehan MM Cognitive-behavioral treatment of borderline personality disorder. xvii, 558 (Guilford Press, 1993). [Google Scholar]
- 124.Hayes SC, Strosahl KD, Bunting K, Twohig M & Wilson KG What is acceptance and commitment therapy? in A practical guide to acceptance and commitment therapy (eds. Hayes SC & Strosahl KD) 3–29 (Springer, 2004). [Google Scholar]
- 125.Wright JH Cognitive Behavior Therapy: Basic Principles and Recent Advances. FOCUS 4, 173–178 (2006). [Google Scholar]
- 126.Beck JS & Beck JS Cognitive behavior therapy: Basics and beyond. (The Guilford Press, 2011). [Google Scholar]
- 127.Wenzel A Modification of Core Beliefs in Cognitive Therapy. in Standard and Innovative Strategies in Cognitive Behavior Therapy (ed. de Oliveira IR) 17–34 (InTech, 2012). [Google Scholar]
- 128.Beck AT The Current State of Cognitive Therapy: A 40-Year Retrospective. ARCH GEN PSYCHIATRY 62, 953–959 (2005). [DOI] [PubMed] [Google Scholar]
- 129.Hopko DR, Lejuez CW, Ruggiero KJ & Eifert GH Contemporary behavioral activation treatments for depression: Procedures, principles, and progress. Clin. Psychol. Rev. 23, 699–717 (2003). [DOI] [PubMed] [Google Scholar]
- 130.Fried EI et al. Mental disorders as networks of problems: a review of recent insights. Soc. Psychiatry Psychiatr. Epidemiol. 52, 1–10 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Halmi KA Salient components of a comprehensive service for eating disorders. World Psychiatry Off. J. World Psychiatr. Assoc. WPA 8, 150–155 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Anderson LK et al. Treating Eating Disorders at Higher Levels of Care: Overview and Challenges. Curr. Psychiatry Rep. 19, 48 (2017). [DOI] [PubMed] [Google Scholar]
- 133.Walfish S, McAlister B, O’Donnell P & Lambert MJ An Investigation of Self-Assessment Bias in Mental Health Providers. Psychol. Rep. 110, 639–644 (2012). [DOI] [PubMed] [Google Scholar]
- 134.Fernandez KC, Fisher AJ & Chi C Development and initial implementation of the Dynamic Assessment Treatment Algorithm (DATA). PloS One 12, e0178806 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Garb HN Clinical Judgment and Decision Making. Annu. Rev. Clin. Psychol. 1, 67–89 (2005). [DOI] [PubMed] [Google Scholar]
- 136.Dawes RM, Faust D & Meehl PE Clinical Versus Actuarial Judgment. 8 (2021). [DOI] [PubMed] [Google Scholar]
- 137.Kraus DR et al. Predicting therapist effectiveness from their own practice-based evidence. J. Consult. Clin. Psychol. 84, 473–483 (2016). [DOI] [PubMed] [Google Scholar]
- 138.Constantino MJ, Boswell JF, Coyne AE, Swales TP & Kraus DR Effect of Matching Therapists to Patients vs Assignment as Usual on Adult Psychotherapy Outcomes: A Randomized Clinical Trial. JAMA Psychiatry 78, 960–969 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Bulik CM, Berkman ND, Brownley KA, Sedway JA & Lohr KN Anorexia nervosa treatment: A systematic review of randomized controlled trials. Int. J. Eat. Disord. 40, 310–320 (2007). [DOI] [PubMed] [Google Scholar]
- 140.Kaye WH & Bulik CM Treatment of Patients With Anorexia Nervosa in the US—A Crisis in Care. JAMA Psychiatry 78, 591 (2021). [DOI] [PubMed] [Google Scholar]
- 141.Fairburn CG Evidence-based treatment of anorexia nervosa. Int. J. Eat. Disord. 37, S26–S30 (2005). [DOI] [PubMed] [Google Scholar]
- 142.Levinson CA et al. Using individual networks to identify treatment targets for eating disorder treatment: a proof-of-concept study and initial data. J. Eat. Disord. 9, 147 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Frumkin MR, Piccirillo ML, Beck ED, Grossman JT & Rodebaugh TL Feasibility and utility of idiographic models in the clinic: A pilot study. Psychother. Res. J. Soc. Psychother. Res. 31, 520–534 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Galatzer-Levy IR & Bryant RA 636,120 Ways to Have Posttraumatic Stress Disorder. Perspect. Psychol. Sci. 8, 651–662 (2013). [DOI] [PubMed] [Google Scholar]
- 145.Kotov R et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J. Abnorm. Psychol. 126, 454–477 (2017). [DOI] [PubMed] [Google Scholar]
- 146.Conway CC & Krueger RF Rethinking the Diagnosis of Mental Disorders: Data-Driven Psychological Dimensions, Not Categories, as a Framework for Mental-Health Research, Treatment, and Training. Curr. Dir. Psychol. Sci. 30, 151–158 (2021). [Google Scholar]
- 147.Rubel JA, Fisher AJ, Husen K & Lutz W Translating Person-Specific Network Models into Personalized Treatments: Development and Demonstration of the Dynamic Assessment Treatment Algorithm for Individual Networks (DATA-IN). Psychother. Psychosom. 87, 249–251 (2018). [DOI] [PubMed] [Google Scholar]
- 148.Bringmann LF et al. What do centrality measures measure in psychological networks? J. Abnorm. Psychol. 128, 892–903 (2019). [DOI] [PubMed] [Google Scholar]
- 149.Levinson CA et al. Longitudinal group and individual networks of eating disorder symptoms in individuals diagnosed with an eating disorder. J. Abnorm. Psychol. (In Press). [DOI] [PubMed] [Google Scholar]
- 150.Spiller TR et al. On the validity of the centrality hypothesis in cross-sectional between-subject networks of psychopathology. BMC Med. 18, 297 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Levinson CA et al. Personalized networks of eating disorder symptoms predicting eating disorder outcomes and remission. Int. J. Eat. Disord. 53, 2086–2094 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Klintwall L, Bellander M & Cervin M Perceived causal problem networks: Reliability, central problems, and clinical utility for depression. Assessment 10731911211039280 (2021) doi: 10.1177/10731911211039281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Lunansky G et al. Intervening on psychopathology networks: Evaluating intervention targets through simulations. Methods (2021) doi: 10.1016/j.ymeth.2021.11.006. [DOI] [PubMed] [Google Scholar]
- 154.Mansueto AC, Wiers RW, van Weert JCM, Schouten BC & Epskamp S Investigating the feasibility of idiographic network models. Psychol. Methods (2022) doi: 10.1037/met0000466. [DOI] [PubMed] [Google Scholar]
- 155.Quax R, Apolloni A & Sloot PMA The diminishing role of hubs in dynamical processes on complex networks. J. R. Soc. Interface 10, 20130568 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wright AGC et al. The hierarchical structure of DSM-5 pathological personality traits. J. Abnorm. Psychol. 121, 951–957 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Godart NT et al. Anxiety disorders in subjects seeking treatment for eating disorders: a DSM-IV controlled study. Psychiatry Res. 117, 245–258 (2003). [DOI] [PubMed] [Google Scholar]
- 158.Godart NT, Flament MF, Lecrubier Y & Jeammet P Anxiety disorders in anorexia nervosa and bulimia nervosa: co-morbidity and chronology of appearance. Eur. Psychiatry J. Assoc. Eur. Psychiatr. 15, 38–45 (2000). [DOI] [PubMed] [Google Scholar]
- 159.Swinbourne JM & Touyz SW The co-morbidity of eating disorders and anxiety disorders: a review. Eur. Eat. Disord. Rev. 15, 253–274 (2007). [DOI] [PubMed] [Google Scholar]
- 160.Shah R & Zanarini MC Comorbidity of Borderline Personality Disorder. Psychiatr. Clin. North Am. 41, 583–593 (2018). [DOI] [PubMed] [Google Scholar]
- 161.McNally RJ Can network analysis transform psychopathology? Behav. Res. Ther. 86, 95–104 (2016). [DOI] [PubMed] [Google Scholar]
- 162.Contreras A, Nieto I, Valiente C, Espinosa R & Vazquez C The Study of Psychopathology from the Network Analysis Perspective: A Systematic Review. Psychother. Psychosom. 88, 71–83 (2019). [DOI] [PubMed] [Google Scholar]
- 163.von Klipstein L, Borsboom D & Arntz A The exploratory value of cross-sectional partial correlation networks: Predicting relationships between change trajectories in borderline personality disorder. PLoS ONE 16, e0254496 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Boschloo L, van Borkulo CD, Borsboom D & Schoevers RA A Prospective Study on How Symptoms in a Network Predict the Onset of Depression. Psychother. Psychosom. 85, 183–184 (2016). [DOI] [PubMed] [Google Scholar]
- 165.van Borkulo C et al. Association of Symptom Network Structure With the Course of Depression. JAMA Psychiatry 72, 1219–1226 (2015). [DOI] [PubMed] [Google Scholar]
- 166.Fried EI Moving forward: how depression heterogeneity hinders progress in treatment and research. Expert Rev. Neurother. 17, 423–425 (2017). [DOI] [PubMed] [Google Scholar]