Abstract
Background:
Home visits are an important part of Geriatrics education for medical and dental students (MS), and the lessons learned by students from these experiences inform further curriculum development. A mixed methods analysis of students’ lessons learned from a single Geriatrics home visit shapes the future focus and impact of similar educational programs to ultimately improve the care of older adults.
Methods:
Over a 3-year period at Harvard Medical School, approximately 495 first year MS participated in an educational Geriatrics home visit to learn about the geriatric assessment. Three hundred and forty-eight students completed voluntary anonymous evaluation forms, rating whether their interest in geriatrics increased after the home visit and describing two lessons learned. We analyzed the student responses and conducted a qualitative content analysis of the lessons learned, identifying major themes within the Geriatrics 5Ms Framework (Mobility, Mind, Medications, Multicomplexity, and Matters Most).
Results:
Most students (70.7%) reported their interest in Geriatrics somewhat or greatly increased after the home visit. Three hundred and ten students (89% of participants) reported 605 lessons learned; 174 students’ lesson learned related to Multicomplexity (56.1%), and 158 students reported a lesson related to Mobility (51%).
Discussion:
After a Geriatrics home visit, a majority of students report an increase interest in Geriatrics. The most common lessons learned relate to Mobility and Multicomplexity, essential areas of focus in a Geriatrics curriculum. Educational home visits are an important opportunity to increase student interest in geriatrics and build their skills to improve the care of older adults using the Geriatrics 5Ms Framework.
Keywords: geriatric medical education, home visit, medical student, older adults, undergraduate medical education
INTRODUCTION
All medical students need training to care for older adults; COVID-19 has highlighted the urgent need for robust preparation in Geriatrics for all doctors.1 Home visits are a uniquely effective and impactful way to teach principles of caring for older adult, aligned with the medical student competencies in Geriatrics.2–4 These visits provide medical students the opportunity to learn about the social determinants of health, functional status and person-centered goals and values.3 This home-based learning can then inform students’ approach to caring for older adults in the clinic and hospital where the majority of medical training occurs.5
Though the best ways to leverage the educational impact of a Geriatrics home visit still need to be determined, there are many potential areas of relevant content that could be emphasized, such as getting to know older adults as people and learning about home safety. Home visits have been shown to positively influence medical students’ perceptions of older adults and the field of Geriatrics.2,6,7 While studies have examined medical student satisfaction from home visits, few studies focus on the content learned from these home visits, and clinicians have ambitious expectations about the teaching that could occur during a visit.8
The aim of our study is to describe lessons learned by first year medical and dental students from a Geriatrics home visit experience and a didactic on sites of care. Through a mixed methods analysis of student evaluations, we explore the specific aspects of the home visit that are most impactful for students, which can guide Geriatrics curriculum development, address learning gaps and engage students in learning to care for older adults.
METHODS
To identify aspects of the home visit that students found most impactful, we reviewed evaluations from first year medical and dental students participating in a required Geriatrics session at Harvard Medical School between 2016 and 2018. As part of the Geriatrics curriculum at Harvard Medical School, later formally defined as The Aging and End of Life Care curricular theme,9 students participated in educational small group Geriatrics home visits. Students visited with older adult volunteers in an independent living facility affiliated with the medical school. The visit and subsequent debriefing session occurred in groups of 2 or 3 students with a preceptor, who was a geriatrician or geriatrics fellow. Prior to the visit, students participated in an interactive didactic session to understand various sites of care for older adults, which has been evaluated separately.10 Beginning in 2017, the students also received a pocket card based on the Geriatrics 5Ms framework (Mobility, Mind, Medications, Multicomplexity and Matters Most)11,12 which aligns with the Age-Friendly Health Systems initiative.11–13 In subsequent years of the curriculum, first year students also completed an online Aquifer Geriatrics clinical case on home safety and functional assessment prior to the visit.14,15
During the home visit, students got a glimpse into older adults’ home environments and were taught how to approach the Geriatrics interview and physical examination using a worksheet, which in 2017 was re-aligned with the Geriatrics 5Ms (Supplement Text S1). Following the visit, the students debriefed with their preceptor and were then asked to fill out a brief, voluntary, anonymous evaluation (Supplement Text S2). Faculty did not know which students submitted evaluations. The evaluation form was collected as part of ongoing educational quality improvement efforts, and subsequently used for this manuscript as a secondary analysis. Students were asked to rate to what extent this session had (1) increased their interest in the field of geriatrics and (2) impacted their comfort assessing common geriatric principles, using a 5-point Likert scale (1-strongly disagree to 5-strongly agree). Students were then asked in an open-ended question to describe two lessons they learned from the home visit. This project was deemed by the Harvard Medical School Academy for Medical Education to be an educational quality improvement project and exempt from further Institutional Review Board review.
The approach used was a convergent mixed methods secondary analysis of closed-ended and open-ended data. Descriptive statistics were used to analyze responses related to confidence and interest in geriatrics. All quantitative data were analyzed using Microsoft Excel (Version 16.52) and JMP statistical software (JMP®, Version 14. SAS Institute Inc., Cary, NC, 1989–2019). Open-ended responses of students’ lessons learned were analyzed using the Framework Method for content analysis,16 as it allows for both deductive (in this case, the Geriatrics 5Ms) and inductive (themes arising from the data) approaches to content analysis. Two coders (KG and CB, a geriatrician and an education researcher, respectively) independently reviewed the lessons learned and generated potential codes/themes. Having both a clinician and non-clinician code the data helped with ensuring data were coded objectively. The two coders met regularly to discuss their interpretations of and reflections on the data (“reflexivity”) and to compare potential codes, in order to develop a working codebook. This codebook was then used to jointly code students’ lessons learned. In the case of any disagreements between the two coders in the coding process, a third clinician author not involved in the initial coding process helped to resolved discrepancies (AWS). Codes were subsequently organized into the Geriatrics 5Ms framework to understand what broad areas of Geriatric medicine were of particular interest to students. This coding structure was then reviewed by the larger research group to identify major themes. All qualitative data were organized and analyzed using Dedoose, version 8.0.35; Socio-Cultural Research Consultants, Los Angeles, CA.
RESULTS
Between the years 2016 and 2018, approximately 495 first year HMS students participated in a one-time, half-day Geriatrics home visit educational experience. 348 voluntary anonymous evaluation forms were collected from the students, for a 70.3% response rate. Characteristics of the students are described in Table 1.
TABLE 1.
Characteristics of first year students participating in geriatric home visits, 2016–2018 (n = 348)
| Characteristic | N (% of total) |
|---|---|
| Student group | |
| Medical | 279 (80.2) |
| Dental | 67 (19.3) |
| Not identified | 2 (0.6) |
| Gender | |
| Female | 169 (48.6) |
| Male | 162 (46.6) |
| Other or not identified | 17 (4.9) |
Quantitative analysis: Confidence and interest in geriatrics
Overall, medical and dental students reported an increase in both interest in the field of geriatrics and comfort with assessing specific geriatric topics after a single home visit experience. Of the 348 students, 70.7% agreed or strongly agreed that the experience increased their interest in the field of geriatrics (51.7% agreed, 19.0% strongly agreed).
Similarly, students were asked to rate the extent to which they agreed that their comfort level with assessing various Geriatrics domains increased as a result of the home visit. The percentage of students who reported increased comfort assessing functional status was 91.7%, for cognitive function was 91.1%, home safety was 90.2%, for fall risk was 88.8% and for asking about advance directives was 81.0%.
Qualitative analysis: Focus on the geriatrics 5Ms framework
A total of 310 students (89% of respondents) reported 605 lessons learned, and the lessons were analyzed for themes. After organizing the lessons learned in the Geriatrics 5Ms framework, the most common themes, as detailed in Table 2, fell under the umbrella themes of Multicomplexity (174 total excerpts, 56.1% of students) followed by Mobility (158 total excerpts, 51.0% of students). The percentage of students is equal to the number of students that commented on a theme divided by 310.
TABLE 2.
Lessons learned by medical and dental students from a Geriatrics home visit
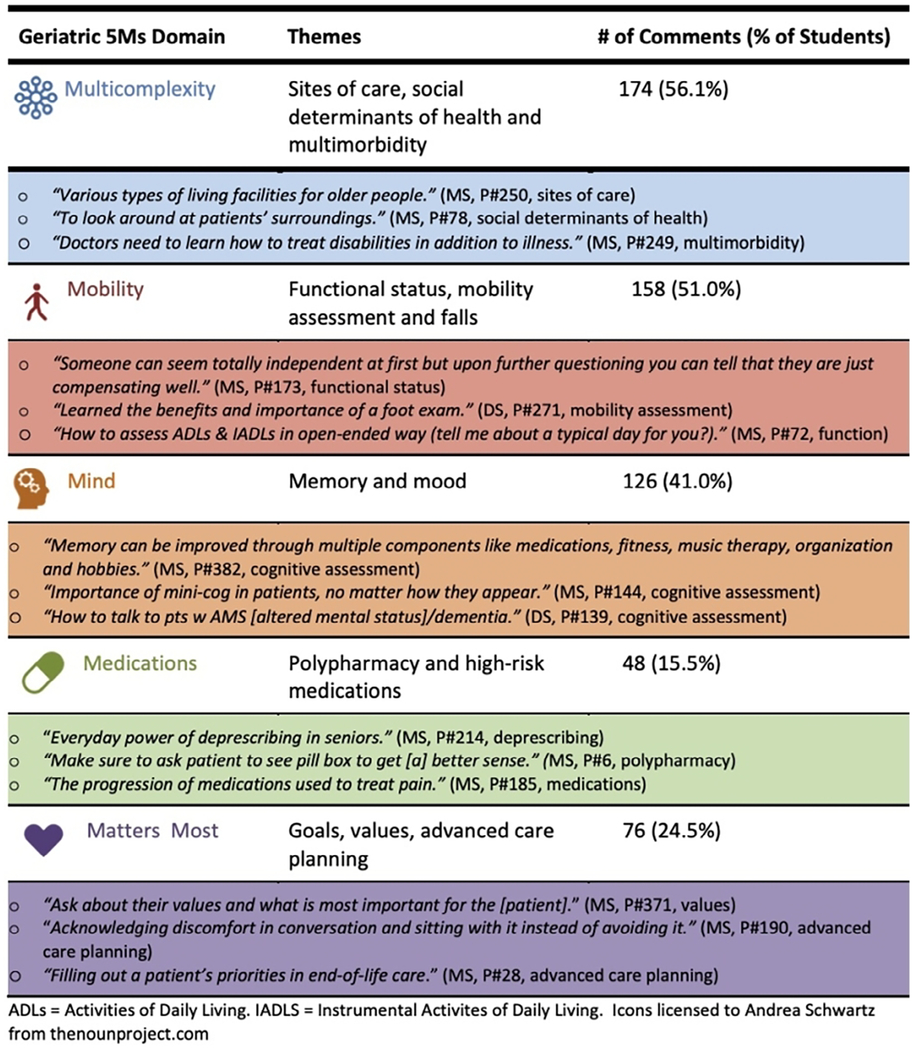
|
Note: Representative quotations of lessons learned by medical and dental students from a Geriatrics home visit experience. Total number of lessons learned (n = 605) reported by medical students (MS) and dental students (DS) who completed evaluation forms (n = 310), coded by the Geriatric 5Ms,11 in order of frequency. Twenty-four evaluations had no comments (7.7%). (P = participant). Icons licensed to Andrea Schwartz from https://thenounproject.com.
Abbreviations: ADLs, activities of daily living; IADLS, instrumental activities of daily living.
Multicomplexity
A total of 77 (44.3%) students among the 174 students that commented on Multicomplexity noted the different types of living facilities for older adults as a lesson learned, which may also reflect the impact of the didactic session prior to the home visit. Many commented on the differences between independent living and skilled nursing facilities. Others commented on the value of a home visit itself and observing the home environment. Students also recognized the value of services in the home including physical and occupational therapy. One student discussed “[the] spectrum of different facilities for the elderly and [how] it is important to find out which one the patient lives in” (Medical Student, Participant #401).
Mobility
Many of the 158 students who commented on Mobility identified the importance of functional assessment (146 excerpts, 92.5%). One student wrote, “older adults are a delight to work with and have a broad and more dynamic spectrum of functionality” (Medical Student, Participant #164). Another wrote, “aging is not synonymous with deterioration of function” (Medical Student, Participant #429). Many students also commented specifically on the clinical tests geriatricians use to assess function, falls and mobility such as foot evaluations (35 excerpts, 22.2%), Timed Up and Go Test (24 excerpts, 15.2%), activities of daily living (17 excerpts, 10.8%) and instrumental activities of daily living (15 excerpts, 9.5%).
Mind, Medication, and Matters Most
Lessons learned for the other 3M domains (Mind, Medications, and Matters Most) in the Geriatrics 5Ms framework included several common themes. Many of the 126 students that commented on Mind, focused on the mini-cog (68 excerpts, 53.5%) and dementia (29 excerpts, 22.8%), while a few commented on screening for depression (10 excerpts, 7.9%). One student wrote, “I learned how difficult it is to evaluate cognitive function and how nuanced it is” (Dental Student, Participant #184).
First year medical and dental students are eager to understand different medications and classes. A total of 48 students commented on the Medication domain and most focused on certain medications to treat different illnesses such as blood pressure and pain (37 excerpts, 77.0%). A few students noted the concept of polypharmacy (14 excerpts, 29.2%) and the value of deprescribing (5 excerpts, 10.4%). One student commented on learning about the “Everyday power of deprescribing in seniors” (Medical Student, Participant #214).
A total of 76 students listed lessons learned with respect to the domain of Matters Most. In this domain, many students noted documentation and discussion of advance care planning directives (18 excerpts, 23.7%). Some students commented on how to address and communicate difficult topics with patients (12 excerpts, 15.8%). One student noted, an “important teaching point: ask about their values and what is most important for the [patient]” (Medical Student, Participant #371).
DISCUSSION: HOME VISITS HELP STUDENTS LEARN ABOUT THE GERIATRICS 5Ms
The results from our analysis indicate that most students report an increased interest in the field of geriatrics and an increased comfort in assessing geriatric domains following a single Geriatrics home visit and didactics session that included an emphasis on the Geriatrics 5Ms framework. The majority of students’ lessons learned focus on the domains of Mobility and Multicomplexity. More specifically, our results show that most students took away lessons related to functional assessment and the different living facilities for older adults.
A Geriatrics home visit has a positive impact on medical students’ attitudes toward and knowledge of older adults.2,6,17,18 Our study aligns with prior results and deepens our understanding of specific content areas that medical students learn from home visits. Specifically, a home visit can teach about any aspect of Geriatric care, as it provides a unique learning environment outside of the classroom or hospital.19 The didactic session offered prior to the home visit also helped students understand and appreciate different sites of care available for older adults and help students appreciate the difference between, for instance, assisted living and independent living facilities, compared to skilled nursing facilities.19
We hypothesize that Mobility and Multicomplexity are mentioned more frequently because first year medical students can apply skills already learned to these areas. They were provided with guidance on how to assess gait and taught about different sites of care in the preceding didactics about Multicomplexity. The students may feel more comfortable addressing these 2Ms with their level of training and lack of clinical skills as compared to later years in medical training. The other domains—Mind, Medications and Matters Most—may require more advanced interpersonal and clinical skills that medical students will likely feel more comfortable with later in their training. Geriatric educators should emphasize that the Geriatric 5Ms should be considered parts of a whole, and that home visits provide a unique environment to learn about how each of the M domains inform one another. Although the majority of student comments focused on Mobility and Multicomplexity, educators should draw explicit connections between all the 5M domains. For example, an educator could highlight the impact of Mentation and/or Medications on Mobility, exploring how a person living with dementia and/or polypharmacy has different considerations for risk factors for falls. Another example is an educator aligning Multicomplexity with What Matters Most to an older adult, asking if the patient’s care preferences align with their current living situation and supports. All the M domains can be uniquely taught in the home setting. Educators should carefully plan the learning goals for a home visit session and emphasize different M domains but also the connection between all the 5M domains.
Students in our study report an appreciation of the opportunity to learn about all aspects of Geriatric care, and specifically mention the new information about Mobility and Multicomplexity that may not be covered in other aspects of the traditional medical school curriculum, whereas Mind, Medications and Matters Most may be more likely to have their own focus within the classroom. Future iterations of this curriculum could include a longitudinal home visit experience which could enable educators to emphasize 1M domain during each visit, to allow deeper engagement with each important content area. For example, to understand the M for Medications, home visits could focus on medication administration, and students could spend time observing how medications are organized and understood by the older adult.
Our results highlight the interest in Multicomplexity by medical students, though Multicomplexity is not included in the 4Ms of the Age-Friendly Health Systems (AFHS) initiative.20,21 The 4Ms included in the AFHS initiative allow health systems to have a shared language about caring for older adults in any clinical setting. The 5th M of Multicomplexity may be unique to the individual patient rather than the health system at large, and is a major focus of medical student competencies in Geriatrics.3 Multicomplexity encompasses many topics and reminds learners to consider social determinants of health, health equity, transitions and sites of care as well as caregiver burden when caring for an older adult.13
Another point to note is that this article is a retrospective secondary data analysis that evaluates previously collected student evaluations to learn about the impact of a Geriatrics home visit. A randomized study may better evaluate the impact of the individual home visit session, for instance dividing the students into groups to assess the impact of the pre-session didactic.
Limitations of our study include that it was a single site study at one urban medical school; results may not be generalizable to other academic settings or to a different population of older adult volunteers. Students had already participated in a didactics session on Geriatrics in which they were introduced to the Geriatric 5Ms. This prior exposure may have influenced the way they responded to the survey. Because of the subjective nature of qualitative research, the two coders organized the take-away points within the Geriatrics 5Ms framework using their own understanding of the students’ comments, which may have been subject to interpretation bias. Additionally, the Geriatrics 5Ms framework was introduced in 2017 in the middle year of our data collection,11 so although similar content was covered before and after the change, the 5Ms were not explicitly named and emphasized in the first year of data collection, which may have impacted the students’ learning in subsequent years.
CONCLUSION
Our findings suggest that specific, targeted learning objectives focused on the Geriatrics 5Ms may focus and optimize the learning potential of home visits for medical and dental students. Most students learned lessons related to the importance of Mobility and Multicomplexity when caring for older adults. Knowing that Mobility and Multicomplexity are most impactful and enjoyable for medical students can guide Geriatrics home visit educators to focus their curriculum and optimally engage students when caring for older adults in their home. Since most medical students will care for older adults in their careers, capitalizing on students’ interest in the home care curriculum may impart lasting lessons in Geriatrics that can help improve care for older adults as part of an Age Friendly Health System.13
Supplementary Material
Supplemental Text S2. Geriatrics home visit evaluation provided to students following the home visit and debriefing session with their preceptor. The evaluations were submitted anonymously.
Supplemental Text S1. Geriatrics home visit student worksheet with instructions on the Geriatrics interview and physical examination using the Geriatrics 5Ms. Each student used this worksheet to organize questions and answers during their home visit.
Key Points.
Geriatrics home visits provide a unique educational setting for medical and dental students; limited time means educators must focus their teaching goals.
Students participating in a Geriatrics home visit describe lessons learned, which were analyzed and coded using the Geriatrics 5Ms Framework.
The most frequent lessons learned centered on the themes of Multicomplexity and Mobility for older adults, which can be taught in an impactful way in a home visit setting.
Why does this paper matter?
Geriatrics educators conducting home visits should emphasize themes of the Geriatrics 5Ms, with particular attention to the domains of Multicomplexity and Mobility. This focus will provide impactful educational experiences unique to the home setting.
ACKNOWLEDGMENTS
The authors wish to thank the staff and residents at Hebrew Senior Life’s Center Communities of Brookline for hosting the Geriatric clinical immersion, including Melissa Greeley, Alexandra Mayville and Tabetha Fine-berg; Kelly Doherty, Sarah Aguierre, Xavian Morales; The Mount Auburn Hospital Fellowship in Health Professional Education, including Dr. Mab Butterfield Dr. Alexandra Chabrerie and Dr. Cherie Noe, and the HMS Academy Medical Education Fellowship, including Dr. David Hirsch and Dean Edward Hundert; The faculty, students and leadership in the HMS Practice of Medicine Course, as well as Dr. Anne Fabiny, Dr. Lewis Lipsitz and the Reynolds Foundation who led and supported the development of an earlier version of this home visit program. The authors wish to acknowledge the support of the Harvard Medical School Dean’s Innovation Award (AWS). Some of this material is the result of work supported with resources and the use of facilities at the Veterans Affairs Boston Healthcare System and the New England Geriatric Research Education and Clinical Center. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
CONFLICT OF INTEREST
No potential competing interest was reported by the authors.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- 1.Callahan KE, Tumosa N, Leipzig RM. Big ‘G’ and little ‘g’ geriatrics education for physicians. J Am Geriatr Soc. 2017;65(10): 2313–2317. doi: 10.1111/jgs.14996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagle BJ, Berry A, Gorman L, Dangiolo MA. Preliminary qualitative evaluation of an in-home geriatric care elective experience for third-year medical students. Cureus. 2018;10(4): 1–15. doi: 10.7759/cureus.2415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AGS Publishes Updated AGS Minimum Geriatrics Competencies for Graduating Medical Students. www.americangeriatrics.org. Published June 21, 2021. Accessed 3/1/2022. https://www.americangeriatrics.org/media-center/news/ags-publishes-updated-ags-minimum-geriatrics-competencies-graduating-medical
- 4.Leipzig RM, Granville L, Simpson D, Anderson MB, Sauvigné K, Soriano RP. Keeping granny safe on July 1: a consensus on minimum geriatrics competencies for graduating medical students. Acad Med. 2009;84(5):604–610. [DOI] [PubMed] [Google Scholar]
- 5.Roane DM, Tucker J, Eisenstadt E, Gomez M, Kennedy GJ. Assessing the benefits of a geropsychiatric home-visit program for medical students. Acad Psychiatry. 2012;36(3):216–218. [DOI] [PubMed] [Google Scholar]
- 6.Abbey L, Willett R, Selby-Penczak R, McKnight R. Social learning: medical student perceptions of geriatric house calls. Gerontol Geriatr Educ. 2010;31(2):149–162. [DOI] [PubMed] [Google Scholar]
- 7.O’Donnell L, Carson L, Forciea MA, et al. What students experienced: a narrative analysis of essays written by first-year medical students participating in a Geriatrics home visit. J Am Geriatr Soc. 2013;61(9):1592–1597. [DOI] [PubMed] [Google Scholar]
- 8.Solomon P, Risdon C. Promoting interprofessional learning with medical students in home care settings. Med Teach. 2011; 33(5):e236–e241. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz A, Schaefer K. A longitudinal aging and end-of-life care curriculum for medical students using the geriatric 5Ms framework. Innov Aging. 2020;4(Suppl_1):9. [Google Scholar]
- 10.Goreshnik A, Corey MT, Rhodes Kropf J, Schwartz AW. Learning about sites of care for older adults: a jigsaw educational session for medical students. Age Ageing. 2022;51(3):1–5. doi: 10.1093/ageing/afac032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tinetti M, Huang A, Molnar F. The geriatrics 5M’s: a new way of communicating what we do. J Am Geriatr Soc. 2017;65(9): 2115. [DOI] [PubMed] [Google Scholar]
- 12.Holliday AM, Hawley CE, Schwartz AW. Geriatrics 5Ms pocket card for medical and dental students. J Am Geriatr Soc. 2019; 67(12):E7–E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating age-friendly health systems—a vision for better care of older adults. Healthcare (Amst). 2018;6(1):4–6. [DOI] [PubMed] [Google Scholar]
- 14.Sehgal M, Syed Q, Callahan KE, et al. Introducing aquifer geriatrics, the American Geriatrics Society National Online Curriculum. J Am Geriatr Soc. 2019;67(4):811–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramaswamy R, Shah AA, Denson KM, et al. Teaching geriatrics during the COVID-19 pandemic: aquifer geriatrics to the rescue. J Am Geriatr Soc. 2021;69(7):1740–1742. doi: 10.1111/jgs.17169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ritchie J, Ormston R, Lewis J, Nicholls CM, eds. Qualitative Research Practice. 2nd ed. SAGE Publications; 2014. [Google Scholar]
- 17.Robertson ML, Schuchman M, Cudjoe TKM, Colburn J. Innovative educational approaches to house calls in the time of COVID-19. J Am Geriatr Soc. 2021;69(8):E20–E22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cetrone E, Young M, Demers L. No place like home: student and faculty perspectives on the value of house calls in medical education. J Am Geriatr Soc. 2021;7(1):E1–E4. doi: 10.1111/jgs.17505 [DOI] [PubMed] [Google Scholar]
- 19.Moo LR. Home video visits: two-dimensional view of the geriatric 5 M’s. J Am Geriatr Soc. 2020;68(11):2425–2427. [DOI] [PubMed] [Google Scholar]
- 20.Fulmer T, Mate KS, Berman A. The age-friendly health system imperative. J Am Geriatr Soc. 2018;66(1):22–24. [DOI] [PubMed] [Google Scholar]
- 21.Morgan E, De Lima B, Pleet A, Eckstrom E. Health equity in an age-friendly health system: identifying potential care gaps. J Gerontol A Biol Sci Med Sci. 2022. 1–5. doi: 10.1093/gerona/glac060 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Text S2. Geriatrics home visit evaluation provided to students following the home visit and debriefing session with their preceptor. The evaluations were submitted anonymously.
Supplemental Text S1. Geriatrics home visit student worksheet with instructions on the Geriatrics interview and physical examination using the Geriatrics 5Ms. Each student used this worksheet to organize questions and answers during their home visit.


