Abstract
Objective
To examine whether racial disparities in access to pediatric mental health care were affected during the COVID-19 telemedicine transition at both The Children’s Hospital of Philadelphia (CHOP) and Boston Children’s Hospital (BCH).
Method
Electronic health records were queried for all unique outpatient visits from a pre-pandemic period in 2019 and a within-pandemic period in 2020. Changes in the proportion of patients were compared based on insurance status, clinic location, and racial identification. Hypotheses were tested via logistic regression analyses.
Results
At CHOP, from 2019 to 2020, the proportion of racially minoritized patients significantly declined within a 1-month period from 62% to 51%, whereas the proportion of White-identifying patients increased from 38% to 49% (β = 0.47; z = 3.60; p =.0003), after controlling for insurance status and clinic location. At BCH, the proportion of racially minoritized patients significantly declined within a longer 6-month period between 2019 and 2020, from 62% to 59%, whereas the proportion of White-identifying patients increased from 38% to 41% (β = 0.13; z = 2.8; p = .006), after controlling for insurance status.
Conclusion
At CHOP and BCH, the COVID-19 telemedicine transition exacerbated pre-existing racial disparities in pediatric mental health services. Our findings suggest that racially minoritized patients receiving services in urban areas may be particularly at risk for losing access when telemedicine is implemented. Although there are limitations to this racial dichotomization, examining differences between White and racially minoritized patients can highlight ways in which White-identifying individuals have disproportionately received enhanced access to healthcare resources.
Key words: psychiatry, pediatrics, telehealth, pandemic, racial disparities
In the prior 2 decades, racial disparities in mental health care have been extensively documented and shown to be greater than disparities in almost all other areas of medical care.1 A robust literature demonstrates that compared to White patients, racially and ethnically minoritized groups have reduced access to mental health services and are less likely to receive evidence-based care2 , 3; unfortunately, these disparities have only widened in the last decade,4 , 5 leaving many questions about how these disparities have been affected by the COVID-19 pandemic.
Beginning in March 2020, in the midst of the pandemic-related emergency disaster announcements and stay-at-home orders, hospitals across the country scrambled to transition from in-person services to exclusively telemedicine service delivery for patients and their families. Emerging evidence from the broader academic community demonstrates that these rapid transitions to telemedicine have both exposed and, in many instances, exacerbated the degree of racial disparities in access to healthcare. For example, one study in a primary care department within a large academic health system investigated racial disparities in visits during the transition to telemedicine, demonstrating an increase in the proportion of non-Hispanic White patients receiving services and a decrease in racially minoritized groups (eg, Black or African American, Latinx, Asian/Pacific Islander).6 One large health care system in New York found that Black patients had a 40% lower chance of receiving telemedicine compared to White patients during the months of March and April 2020.7
In pediatrics specifically, racial disparities in telemedicine use have been elucidated during the COVID-19 pandemic. One adolescent medicine department found that during their COVID-19 transition, patients coded as non-White (African American, Asian, and other) had lower telemedicine visit completion rates when compared to White patients.8 Another study determined that in pediatric primary care, significant racial disparities existed in telemedicine services—among emergency and chronic visits—following the transition to telemedicine.9 A recent study from a pediatric integrative primary care practice that included mental health services found that Black children were 35% less likely to be scheduled for telemedicine appointments than their White counterparts.10
Although data from pediatric specialties is rapidly emerging, one significant gap is the dearth of literature on racial disparities specifically in pediatric mental health specialty departments during the transition to telemedicine. The current study sought to examine how racial disparities in access to pediatric mental health care were affected during the COVID-19 transition to telemedicine at 2 major academic pediatric medical centers: The Children’s Hospital of Philadelphia (CHOP), located in the Philadelphia metropolitan region of Pennsylvania; and Boston Children’s Hospital (BCH), located in Boston, Massachusetts.
Our primary objective was to evaluate whether a significant difference existed in the relative proportion of racially minoritized patients seen before and after each hospital’s transition to telemedicine services (initiated on March 6, 2020, at CHOP and March 10, 2020, at BCH) and whether this transition altered pre-existing racial disparities in mental health services for children. In light of the aforementioned literature, we hypothesized that the transition to telemedicine would exacerbate disparities in service use for racially minoritized patients when compared to their White counterparts. Secondarily, we aimed to evaluate the contributions to racial disparities in access to care to the changes in the proportion of insurance types [commercial insurance (ie, private) vs noncommercial insurance (ie, public or state-funded, self-pay, or charity care)] and changes in the proportion of patients seen in urban vs non-urban settings.
These secondary aims were included becaues broader social science literature has suggested that racially minoritized populations are overrepresented in urban environments11 and face more systemic barriers to mental health care, including differential access to insurance coverage.12 In summary, issues of racial inequalities are entangled with broader issues of geographic residence and insurance coverage.13 In addition, patients with commercial insurance coverage are commonly beneficiaries of employer-sponsored health plans. Thus, populations with commercial insurance largely overrepresent employed individuals,14 connecting insurance type to broader issues of poverty, unemployment, and underemployment. Regarding our secondary aims, we hypothesized that changes in the proportion of insurers and geographic residence would help to explain changes in the relative proportion of racial groups engaged in services. To our knowledge, this study is the first to date to examine telemedicine-related racial disparities specifically within pediatric mental health specialty departments in the context of COVID-19.
Method
Both outpatient divisions included in this study, namely, the Department of Child and Adolescent Psychiatry and Behavioral Sciences (DCAPBS) at CHOP and the Department of Behavioral and Psychiatric Services (DBPS) at Boston Children’s Hospital, have psychiatric and behavioral health centers that provide care for patients with a wide range of psychiatric conditions and deliver care in multiple subspecialties within medicine. In addition, both of these programs provide care for a diverse patient population through their respective main hospitals as well as through several satellite locations in their greater metropolitan regions. To descriptively determine whether similar trends could be found within comparable psychiatric departments in 2 different children’s hospitals, the same methods of data collection and analyses were used for both the CHOP and BCH datasets. The patient visits in the datasets represented a range of services, including individual psychotherapy, family therapy, medication management, and others. Furthermore, many patient visits represented mental health services delivered within ambulatory medical specialty settings (eg, cardiology, gastroenterology, nephrology).
The first dataset consists of the Children’s Hospital of Philadelphia’s Department of Child and Adolescent Psychiatry and Behavioral Services, in which CHOP’s research team requested administrative reports (Microsoft Excel spreadsheets) that queried billing data from electronic health records (EHR) for all unique outpatient in-person visits during a 1-month period, from March 15, 2019, to April 15, 2019 (T1, 1 year before COVID-19 transition), as well as all unique telemedicine visits during the same month in the following year, from March 15, 2020, to April 15, 2020 (T2, the COVID-19 response). Telemedicine visits were formally coded in the dataset as being synchronous audio-visual communications between clinician and families. We were not able to specifically examine telephone visits separately, as heterogeneity in clinician coding behaviors rendered these data difficult to collect (phone visits may have been coded as telemedicine visits and vice versa); plus, many clinicians do not bill for telephone encounters, so these data would not be included in a billing dataset. Because of patient-safety and system-based concerns, CHOP’s DCAPBS limited new patient evaluations during the initial telemedicine transition, which left almost exclusively established patients eligible to continue services for a brief time. As a result, a secondary analysis was conducted on the CHOP dataset to include only established patients in the 2019 and 2020 time periods.
The second dataset consists of Boston Children’s Hospital’s Department of Behavioral and Psychiatric Services, in which the BCH research team requested administrative reports that queried billing data from electronic health records (EHR) for all unique outpatient in-person visits during the same 1-month period as CHOP, March 15, 2019, to April 15, 2019, and all unique telemedicine visits from March 15, 2020, to April 15, 2020. This study began as a single-site investigation at CHOP (to assess the 1-month time period) and later developed into a collaborative effort with BCH, at which time it was decided to include an expanded dataset with a 6-month period, comparing March 15, 2019, to September 15, 2019 (T1) and March 15, 2020, to September 15, 2020 (T2).
Both hospitals’ datasets contained patients’ self-identified race and/or ethnicity (White, Black or African American, Asian, American Indian and Alaska Native, Native Hawaiian or other Pacific Islander, multi-racial, or other), location of service, insurance provider, type of service used, and date of service. Self-identified race and/or ethnicity is typically captured during the administrative registration process when patients initially enroll for services (see Table 1 for racial identities). All non-White identities, including “other,” were categorized as racially minoritized patients to maintain adequate statistical power. We acknowledge the limitations of this racial dichotomization, which represents a collapsing of myriad social identities into 1 category and renders “White” as the reference; however, examining such differences between White and racially minoritized patients can help to examine ways that White-identifying patients receive greater access to resources within the healthcare system.4 , 5 Patients who had an “unknown” designation or “refused” to self-identify were removed from both datasets, which represented a negligible number of patients.
Table 1.
Summary of Demographics
| 1-Month time period |
6-Month time period |
|||||||
|---|---|---|---|---|---|---|---|---|
| BCH (2019) |
BCH (2020) |
BCH (2019) |
BCH (2020) |
|||||
| N 3,500 |
% 100 |
N 3,959 |
% 100 |
N 19,071 |
% 100 |
N 18,585 |
% 100 |
|
| Self-identified race: | ||||||||
| Black or African American | 344 | 9.83 | 426 | 10.76 | 1,907 | 9.99 | 1,809 | 9.73 |
| White | 2,373 | 67.80 | 2,627 | 66.36 | 13,076 | 68.56 | 13,006 | 69.98 |
| American Indian or Alaska Native | 23 | 0.66 | 15 | 0.37 | 95 | 0.50 | 79 | 0.43 |
| Asian | 157 | 44.86 | 198 | 5.00 | 910 | 4.77 | 743 | 3.99 |
| Native Hawaiian or Other Pacific Islander | 11 | 0.31 | 6 | 0.15 | 45 | 0.24 | 16 | 0.09 |
| Other | 592 | 16.91 | 686 | 17.33 | 3,038 | 15.93 | 2,932 | 15.78 |
| CHOP (2019) | CHOP (2020) | |||||||
|---|---|---|---|---|---|---|---|---|
| N 2,580 |
% 100 |
N 1,488 |
% 100 |
|||||
| Self-identified race: | ||||||||
| Black or African American | 464 | 17.98 | 224 | 15.05 | ||||
| White | 1,667 | 64.61 | 1,007 | 67.67 | ||||
| American Indian or Alaska Native | 3 | 0.12 | 1 | 0.07 | ||||
| Asian | 67 | 2.60 | 37 | 2.49 | ||||
| Native Hawaiian or Other Pacific Islander | 1 | 0.04 | 1 | 0.07 | ||||
| Other | 316 | 12.25 | 169 | 11.36 | ||||
| Multi-racial | 62 | 2.40 | 49 | 3.29 | ||||
| Indian | 22 | 0.85 | 6 | 0.40 | ||||
Note: All unique telemedicine visits at CHOP and BCH for 1-month period refer specifically to March 15 to April 15, 2019, and from March 15 to April 15, 2020. The 6-month time period at BCH refers specifically to March 15 to September 15, 2019, and March 15 to September 15, 2020. BCH = Boston Children’s Hospital. CHOP = Children’s Hospital of Philadelphia.
Within each dataset, insurance status was dichotomized as either commercial insurance (ie, private insurance) or noncommercial insurance (ie, state-sponsored or public insurance, charity care, and self-pay). Of note, it may be possible for some commercial insurance carriers to actually have state-funded plans, as some private insurers provide Medicaid coverage, and international insurers were deleted from the BCH dataset (international insurers were not collected in the CHOP dataset). We dichotomized location of service (urban vs non-urban clinic sites) as a rough proxy for residence, that is, inferring that urban residents are likely to receive services within the urban clinical sites and vice versa.
Logistic regression analyses were conducted to discern whether there was a significant difference in the proportion of racially minoritized patients seen between the 2 time periods and whether there existed an effect of insurance status, location of service (urban vs non-urban clinical sites), or racial identity (White vs racially minoritized status) on the number of unique patients seen between 2019 and 2020. Significance testing was conducted on the relative proportions of visits (number of visits determines the degrees of freedom and significance). Only de-identified aggregate data were shared between institutions, so no protected health information was shared. The study was reviewed and received an Institutional Review Board exemption at both CHOP and BCH.
Results
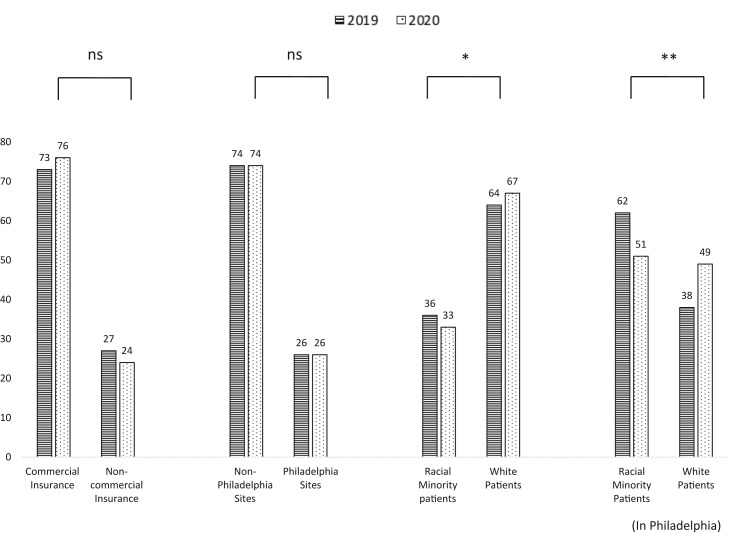
Total Study Samples at CHOP
During the 2019 T1 study period at CHOP, there were 2622 unique patient visits, which declined to 673 in the 2020 T2 study period. The proportion of patients seen at Philadelphia sites vs non-Philadelphia sites within the cohort did not change. Non-Philadelphia clinical site patients made up 74% of CHOP service users, whereas Philadelphia site patients comprised the other 26%, in both 2019 and 2020 (β = 0.01; z = 0.12; p = .901). When controlling for insurance type, the change remained nonsignificant (β = 0.04; z = 0.48; p = .630).
Insurance Status in the CHOP Cohort
The proportion of patients based on insurance status within the CHOP cohort did not significantly change in the telemedicine transition. In 2019, commercial insurance carriers made up 73% of CHOP patients whereas noncommercial insurance users represented 27%. In 2020, commercial insurance users constituted 76% of the overall cohort, whereas noncommercial carriers represented 24%, a statistically nonsignificant difference (β = −0.12; z = −1.56; p = .119).
Racial Disparities in the CHOP Cohort: 1-Month Time Period
There were significant changes in the racial composition of the CHOP patient pool following the transition to telemedicine. In 2019, White-identifying patients comprised 64% of DCAPBS patients, whereas racially minoritized patients represented 36% of the cohort. In 2020, White-identifying patients made up 67%, whereas racially minoritized patients comprised 33%, leading to a significant change within the overall cohort between 2019 and 2020, all clinical sites included (β = 0.15; z = 2.19; p = .029). When controlling for both insurance and within-city clinical sites, the change in racial composition remained significant (β = 0.15; z = 1.99; p = .047). The difference in racial composition between time periods was exacerbated when considering only the patients seen at Philadelphia-based clinical sites. From 2019 to 2020, the proportion of racially minoritized patients declined from 62% to 51%, whereas the proportion of White-identifying patients increased from 38% to 49% (β = 0.47; z = 3.60; p = .0003).
Secondary Analysis: Established Patient Visits Only
In a secondary analysis, CHOP researchers investigated the possibility that the observed differences in racial composition between 2019 and 2020 since DCAPBS’ transition to telemedicine services were accompanied by temporary limitations in new patient visits. This limitation resulted in an increase in the proportion of follow-up visits from 78% in 2019 to 97% in 2020 (β = 2.5539; z = 13.40; p <2e-16), with an accompanying reduction in new patient visits from 22% to 3%. Notably, minoritized racial groups comprised a greater percentage of new patient visits (42%) compared to follow-up visits (34%) in 2019 (β = 0.28028, z = 2.836, p = .00456), suggesting the possibility that our finding of racial disparities in telemedicine could be due to the increase in the relative proportion of follow-up visits compared to new patient visits.
The secondary analysis (limited to established patient visits only) revealed that in both 2019 and 2020 for patients being seen at Philadelphia-based sites, the change in racial composition was still significant. From 2019 to 2020, the proportion of racially minoritized patients seen for follow-up visits declined from 61% to 51%, whereas the proportion of White-identifying patients increased from 39% to 49% (β = 0.39947, z = 2.971, p = .00297). Figure 1 depicts changes in patient demographic proportions at CHOP from 2019 to 2020.
Figure 1.
Observed Changes in Proportion (%) of Patient Demographics at Children’s Hospital of Philadelphia During the One-Month Time Frame From 2019 to 2020
Note:This figure shows demographic changes in insurance status, Philadelphia clinical sites, and racial minority status between T1 (March-April 2019) and T2 (March-April 2020), during the telehealth transition to address the COVID-19 pandemic. Each demographic category is shown in terms of the proportion (%) relative to the total number of unique patient visits during T1 (stripes) and T2 (dots). There was a significant difference in racial composition from T1 to T2 both inside and outside of Philadelphia sites. Significance was assessed with logistical regression analyses. ns = Not significant.
∗p < .05; ∗∗p < .01.
Total Study Samples at BCH
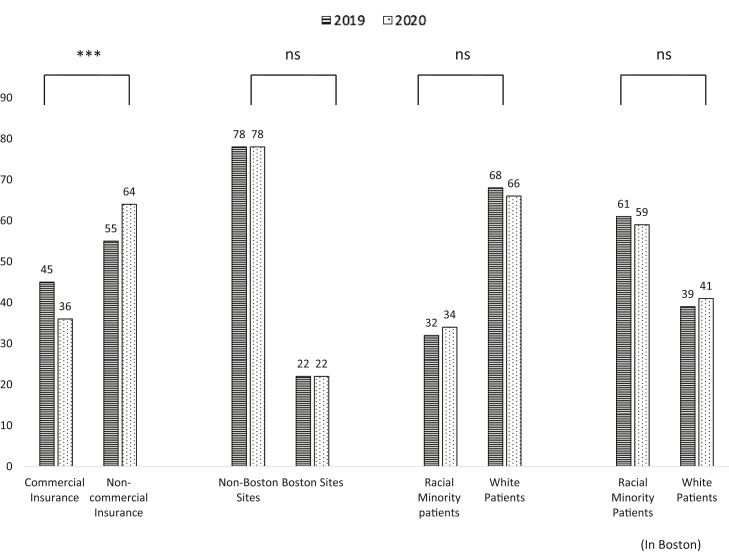
At BCH, there were 3500 unique patient visits in T1, which increased to 3958 unique patient visits in T2. Similar to CHOP, BCH did not find a significant difference in the relative proportion of patients seen within the city clinical sites vs outside the city in the 1-month time frame. At BCH, both in 2019 and in 2020, non−Boston site patients made up 78% of the DPBS patients, and Boston site patients comprised 22% of patients (β = −0.04; z = −0.63; p = .526). When controlling for insurance type, this nonsignificance was maintained (β = −0.01; z = −0.16; p = .871).
Racial Disparities in the BCH Cohort: 1-Month Time Period
There were no significant changes in the racial composition of patients seen at BCH within this same 1-month comparison between 2019 and 2020. In 2019, White-identifying patients made up 68% of patients within DPBS, and racially minoritized patients made up 32%. In 2020, the proportion of White-identifying patients seen within DPBS decreased to 66%, whereas racially minoritized patients increased to 34%, which was a statistically nonsignificant change (β = −0.06; z = −1.31; p = .190). When the logistic regression was conducted again, comparing the racial composition of patients during the 1-month period in 2019 vs 2020, and controlling for insurance type and whether the patient was seen at within-city sites, the significance was further attenuated (β = 0.003; z = 0.05; p = 0.961). This statistically nonsignificant change remained when considering only those patients who were seen within the Boston city sites. From 2019 to 2020, the relative proportion of racially minoritized patients being seen at Boston sites declined from 61% to 59%, whereas the proportion of White patients increased from 39% to 41% but was not statistically significant (β = 0.07; z = 0.73; p = .468). When controlling for insurance type, the change remained nonsignificant (β = 0.19; z =1.76; p = .079). Figure 2 depicts the observed changes in proportion of patient demographics at BCH during the 1-month time frame.
Figure 2.
Observed Changes in Proportion (%) of Patient Demographics at Boston Children’s Hospital During the One-Month Time Frame From 2019 to 2020
Note:This figure shows demographic changes in insurance status, Boston residence, and racial minority status between T1 (March to April 2019) and T2 (March to April 2020), when the telehealth transition began to address the COVID-19 pandemic. Each demographic category is shown in terms of the proportion (%) relative to the total number of unique patient visits during T1 (stripes) and T2 (dots). There was a significant difference in the distribution of patient insurance status from T1 to T2. Significance was assessed with logistical regression analyses. ns = Not significant.
∗∗∗p < .001.
Insurance Status in the BCH Cohort
Within the 1-month time frame, BCH did see a significant difference in the distribution of patient insurance status. In 2019, commercial insurance users made up 45% of DPBS patients, and noncommercial users made up 55%. In 2020, commercial insurance users decreased to 36%, and noncommercial users increased to 64% (β = 0.38; z = 7.96; p = 1.77e-15).
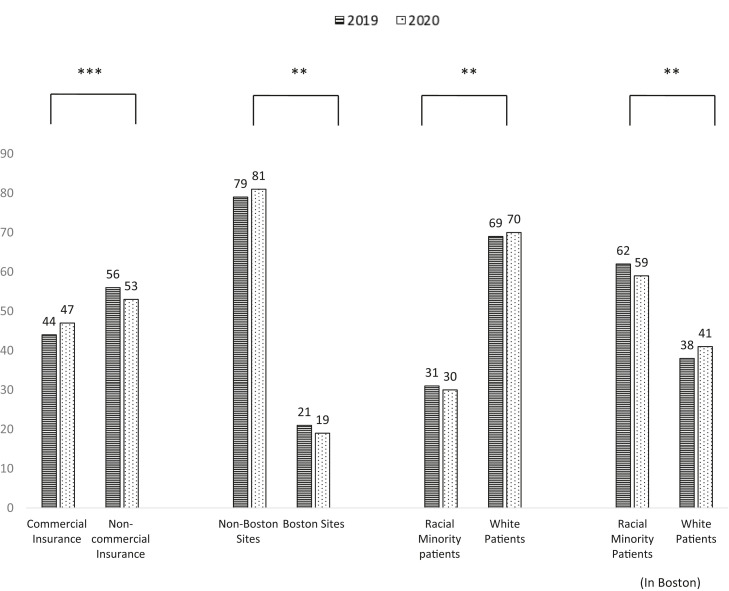
Secondary Analysis: 6-Month Time Period at BCH
A secondary analysis was conducted to assess for change over a longer, 6-month time period during the transition to telemedicine at BCH. When the timeline at BCH was expanded to include 6 months of unique patient visits, there were 19,071 in T1, which fell to 18,585 in T2. Using this expanded dataset, which included total patient visits in the DPBS from March to September in both 2019 and 2020, the same analyses as for the 1-month time frame were conducted.
There was a significant change to relative proportions of commercial insurance carriers in the secondary analysis, demonstrating an increase in the proportion of commercial insurers from 2019 to 2020. In 2019, commercial insurance users made up 44% of total DPBS patients, and noncommercial users made up 56%. In 2020, commercial insurance users increased to 47%, and noncommercial users decreased to 53% (β = −0.10; z = −4.93; p = 8.45e-07).
In contrast to the 1-month analyses, BCH saw a significant difference in the distribution of patients seen at within-city clinical sites vs outside of Boston in the 6-month timeframe. At BCH, non−Boston site patients made up 79% of the total DPBS patients, whereas Boston residents comprised 21% of patients in 2019, which increased significantly to 81% non-Boston residents and decreased significantly to 19% Boston residents in 2020 (β = 0.07; z = 2.76; p = .006). After controlling for insurance as a covariate, significance was maintained (β = −0.09; z = −4.79; p = 1.65e-06).
In the 6-month timeframe, the racial composition of patients changed significantly at BCH. In 2019, White-identifying patients made up 69% of patients within DPBS, and racially minoritized patients made up 31%. In 2020, the proportion of White-identifying patients seen within the DPBS increased to 70%, whereas the proportion of racial minoritized patients decreased to 30% (β = 0.07; z = 2.978; p = .003). A significant change in racial composition was maintained when considering only Boston-based clinical sites. From 2019 to 2020, the relative proportion of racially minoritized patients seen at Boston sites decreased from 62% to 59%, whereas the proportion of White-identifying patients increased from 38% to 41% (β = 0.13; z = 2.8; p = .006). When controlling for insurance type, the statistical significance remained (β = 0.11; z = 2.18; p =.028). When the logistic regression controlled for both insurance type and within-Boston sites, the significance was attenuated (β = 0.04; z =1.49; p = .136). However, significance in racial composition was maintained when the regression controlled only for either insurance status (β = 0.05; z = 2.22; p = .026) or only for within-city clinical sites (β = 0.05; z = 2.19; p = .028). Figure 3 depicts the observed changes in proportion of patient demographics at BCH during the 6-month time frame.
Figure 3.
Observed Changes in Proportion (%) of Patient Demographics at Boston Children’s Hospital During theSix-Month Time Frame From 2019 to 2020
Note:This figure shows demographic changes in insurance status, Boston residence, and racial minority status between T1 (March to September 2019) and T2 (March to September 2020), when the telehealth transition to address the COVID-19 pandemic was complete. Each demographic category is shown in terms of the proportion (%) relative to the total number of unique patient visits during T1 (stripes) and T2 (dots). There were significant declines in the number of racial minority patients being seen from 2019 to 2020, and significant increases in the number of White patients being seen from 2019 to 2020. In addition, there was a significant difference in the distribution of patient insurance status from T1 to T2. Significance was assessed with logistical regression analyses.
∗∗p < .01; ∗∗∗p < .001.
Discussion
Although implementation of telemedicine holds much promise for greater accessibility of mental health services, our findings demonstrate that the transition to telemedicine in 2020 at both CHOP and BCH reflects what many other academic centers6, 7, 8, 9, 10 have found: an exacerbation of racial disparities in overall service use. In 2020, clinicians at both CHOP and BCH appears to have seen fewer racially minoritized patients and more White-identifying patients compared to the same period in 2019, although the findings emerged at different time points (CHOP within 1 month and BCH within 6 months, also acknowledging that findings may have been apparent at 1 month but that this study may not have been adequately powered to detect earlier differences). This racial disparity became more pronounced when analyzing a subset of city-based patients only, which revealed a significant decrease in racially minoritized patients being seen for services during the telemedicine transition in both Philadelphia and Boston. At CHOP, these differences were not explained by changes in insurance carriers or changes in the total proportion of urban-based clinical sites vs non−urban based sites. At BCH, there was a significant decrease in the proportion of noncommercial insurance carriers in 2020, which did have an impact on the racial disparities seen. When controlling for insurance type at BCH, the change in racial composition was nonsignificant.
Although this study’s aim was to elucidate descriptive trends rather than the underlying causal mechanisms, the findings from both children’s hospitals may suggest that racially minoritized populations receiving services in urban areas were among the most vulnerable to being lost to follow-up in the transition to telemedicine services. The findings at BCH, in particular, may suggest the notion that racial disparities in access to telemedicine (and other health services) are tied to geographic location and insurance access. Broader public health literature has demonstrated that suburban regions demonstrate higher rates of health insurance when compared to urban regions.11 Findings at CHOP, where racial disparities were found without significant differences in insurance carriers or geographic location of sites, may suggest that race, in some cases, operates independently of insurance and geographic location to affect a person’s access to mental health care.
The current study’s design and analyses have several limitations. First, the collection and description of patients’ racial and ethnic identities, derived from EHR, is inherently constrained. Patients (more specifically, their parents or guardians) are provided only a limited number of options for how they can self-identify during the registration process. Although only a negligible portion declined to self-identify, the self-identification process is in itself a limitation, especially as patients who select “other” or “multi-racial” could potentially have myriad racial identities not captured. Furthermore, we dichotomized the racial categories into White vs racially minoritized for reasons of statistical power, and this limited our ability to examine specific racial groups. Second, the cross-sectional nature of our methods and dataset (billing data) constrained our ability to infer why certain patients did not have follow-up visits and limited our ability to assess longitudinal changes, as patients may have followed-up past the point of data collection. Overall, these limitations restricted the ability to clarify any underlying clinical factors (eg, age, sex, provider type, diagnosis, or type of service) or administrative contributions to the racial disparities in telemedicine use.
In addition, the billing datasets disallowed a specific examination of telephone appointments (audio-only) as a separate variable due to the heterogeneity in clinician billing behaviors (some clinicians bill for telephone encounters and others do not). In addition, based on our experience, many of the video visits were switched to telephone because of technical difficulties but were still billed as telemedicine, thereby rendering a conflation of audio-only and telehealth visits within the same dataset. There may also have been institutionally specific policies and practices (at each hospital and within each different integrated care settings) that help to explain these results, which we did not specifically assess. For example, CHOP paused new patient visits initially, resulting in fewer unique patients being seen during the transition to telemedicine, leading to a much smaller sample size at CHOP compared to BCH. Moreover, patients may have experienced more delays in care for system-specific reasons that we were unable to investigate.
Despite these limitations, our study had several strengths: researchers included data from the same time period in 2019 and 2020 for comparison, controlling for seasonal oscillations in referrals and visits. In addition, each unique patient was counted only once for the analyses of these time periods, so that high-using patients (ie, those seen multiple times per week) were not overrepresented in the sample. Most notably, the collaborative method of including datasets from 2 separate large institutions strengthens the findings. These findings suggest that current systems of telemedicine service delivery in academic children’s hospitals may not adequately support racially minoritized communities in accessing telemedicine services and maintaining engagement over time, proposing that other academic centers located in urban districts may be vulnerable to perpetuating the same inequities, which warrants further investigation. In addition, racially minoritized populations living in large cities are more likely to be marginalized within other social determinants of health (eg, education, employment, transportation, wealth) that increase barriers to healthcare12 and were disproportionately impacted by the COVID-19 pandemic in terms of morbidity, mortality, and socioeconomic consequences.17 So, it remains unclear whether the switch to telemedicine was a causal driver of a loss of access or is confounding within pre-existing barriers; or whether the loss of access was simply a consequence of the disproportionate impacts of COVID19 on racially minoritized communities.
Although it is a common conception that implementation of telemedicine services expands access to care and reduces barriers (eg, transportation to appointments), our results may suggest that expansion of access is not guaranteed for all populations, and pre-existing racial and ethnic disparities in care may be exacerbated by telemedicine implementation. Similar to the disproportionate rates of COVID-19 infections in racially minoritized communities,13 disparate access to telemedicine is likely a multifactorial socioeconomic issue that connects to disparities in various social determinants of health and historical legacies of structural racism. Future studies should screen for and examine social determinants of health and other barriers to care prospectively to examine potential mechanisms and reasons for demographic changes in patient populations. Researchers and clinicians have begun to make recommendations for overcoming these barriers, including minimizing linguistic barriers with the use of remote interpreters and providing technology education for patients with lower levels of digital literacy. Policy makers have explored providing financial incentives for insurance plans to cover telemedicine visits, establishing national metrics of quality care for telemedicine, and instating programs to ensure adequate access to the Internet for low-income consumers.15 , 16
In summary, our study demonstrates that telemedicine services do not necessarily guarantee increased access to care for all populations. Instead, telemedicine may exacerbate extant disparities. Mental health service providers, at pediatric hospitals and academic centers broadly, must develop systems to track racial and ethnic disparities and to monitor the progress of initiatives aiming to improve equity and access. Systemic barriers to care reduce the odds of racially minoritized patients maintaining consistent care, and given these results, may play a disproportionate role in those communities receiving care in urban centers. Expansion of equitable and culturally responsive services will continue to be a source of national grievance if proactive steps are not taken to address racial disparities in child mental health care.
Footnotes
Molly Ball, BA, Nora Roscoe, BA, and David Glahn, PhD, are supported by The Tommy Fuss Center for Neuropsychiatric Disease Research. Aaron Alexander-Bloch, MD, PhD is supported by grant K08MH120564-04 from the National Institute of Mental Health.
This article is part of a special series devoted to addressing bias, bigotry, racism, and mental health disparities through research, practice, and policy. The series is edited by Assistant Editor Eraka Bath, MD, Deputy Editor Wanjikũ F.M. Njoroge, Associate Editor Robert R. Althoff, MD, PhD, and Editor-in-Chief Douglas K. Novins, MD.
The research was performed with permission from the Children's Hospital of Philadelphia and Boston Children's Hospital Institutional Review Board.
Dr. Alexander-Bloch served as the statistical expert for this research.
Author Contributions
Conceptualization: Williams, Seltzer, Alexander-Bloch, Glahn, Morrow
Data curation: Ball, Roscoe, Seltzer, Vo, Cagande
Formal analysis: Ball, Roscoe, Alexander-Bloch
Methodology: Williams, Hobbs, Raman
Project administration: Williams, Ball, Roscoe, Alexander-Bloch
Software: Ball, Roscoe
Supervision: Morrow
Visualization: Ball, Roscoe, Alexander-Bloch
Writing – original draft: Williams, Ball, Roscoe, Harowitz, Alexander-Bloch, Morrow
Writing – review and editing: Williams, Ball, Roscoe, Harowitz, Hobbs, Seltzer, Vo, Cagande, Alexander-Bloch, Morrow
Disclosure: Drs. Williams, Seltzer, Vo, Cagande, Alexander-Bloch, Glahn, and Morrow and Mss. Ball, Roscoe, Harowitz, Hobbs, and Raman have reported no biomedical financial interests or potential conflicts of interest.
References
- 1.Dankwa-Mullan I., Rhee K.B., Williams K., et al. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. Am J Public Health. 2010;100(S1):S12–S18. doi: 10.2105/AJPH.2010.191619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang P.S., Berglund P., Kessler R.C. Recent care of common mental disorders in the United States : prevalence and conformance with evidence-based recommendations. J Gen Intern Med. 2000;15(5):284–292. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young A.S., Klap R., Sherbourne C.D., Wells K.B. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58(1):55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
- 4.Blanco C., Patel S.R., Liu L., et al. National trends in ethnic disparities in mental health care. Med Care. 2007:1012–1019. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- 5.Cook B.L., Trinh N.-H., Li Z., Hou S.S.-Y., Progovac A.M. Trends in racial-ethnic disparities in access to mental health care, 2004-2012. Psychiatr Serv. 2017;68(1):9–16. doi: 10.1176/appi.ps.201500453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nouri S., Khoong E.C., Lyles C.R., Karliner L. Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. N Engl J Med Catal. 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123 Published online.
- 7.Chunara R., Zhao Y., Chen J., et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Informatics Assoc. 2021;28(1):33–41. doi: 10.1093/jamia/ocaa217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wood S.M., White K., Peebles R., et al. Outcomes of a rapid adolescent telehealth scale-up during the COVID-19 pandemic. J Adolesc Health. 2020;67(2):172–178. doi: 10.1016/j.jadohealth.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walters J., Johnson T., DeBlasio D., et al. Integration and impact of telemedicine in underserved pediatric primary care. Clin Pediatr (Phila) 2021;60(11-12):452–458. doi: 10.1177/00099228211039621. [DOI] [PubMed] [Google Scholar]
- 10.Chakawa A., Belzer L.T., Perez-Crawford T., Yeh H.W. COVID-19, Telehealth, and pediatric integrated primary care: disparities in service use [published online ahead of print, August 3, 2021] J Pediatr Psychol. 2021:jsab077. doi: 10.1093/jpepsy/jsab077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schnake-Mahl A.S., Sommers B.D. Health care in the suburbs: an analysis of suburban poverty and health care access. Health Aff. 2017;36(10):1777–1785. doi: 10.1377/hlthaff.2017.0545. [DOI] [PubMed] [Google Scholar]
- 12.Holmes N., Berube A. City and metropolitan inequality on the rise, driven by declining incomes. 2016. https://www.brookings.edu/research/city-and-metropolitan-inequality-on-the-rise-driven-by-declining-incomes/ Published online January 14, 2016. Brookings Institution.
- 13.Tai D.B., Shah A., Doubeni C.A., Sia I.G., Wieland M.L. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72(4):703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bureau of United States Census. Health insurance coverage in the United States. https://www.census.gov/library/publications/2020/demo/p60-271.html
- 15.Barney A., Buckelew S., Mesheriakova V., Raymond-Flesch M. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health. 2020;67(2):164–171. doi: 10.1016/j.jadohealth.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Curfman A.L., Hackell J.M., Herendeen N.E., et al. Telehealth: improving access to and quality of pediatric health care. Pediatrics. 2021;148(3) doi: 10.1542/peds.2021-053129. [DOI] [PMC free article] [PubMed] [Google Scholar]