Abstract
The coronavirus disease 2019 (COVID-19) global public health emergency, has exposed the fragility of health systems. Access to healthcare became a scarce commodity as healthcare providers and resource-poor populations became victims of the novel corona virus. Therefore, this study focuses on Africa's readiness to integrate telemedicine into the weak health systems and its adoption may help alleviate poor healthcare and poverty after COVID-19. We conducted a narrative review through different search strategies in Scopus on January 20, 2021, to identify available literature reporting implementation of various telemedicine modes in Africa from January 1, 2011 to December 31, 2020. We summarized 54 studies according to geographies, field, and implementation methods. The results show a willingness to adopt telemedicine in the resource-poor settings and hard-to-reach populations, which will bring relief to the inadequate healthcare systems and alleviate poverty of those who feel the burden of healthcare cost the most. With adequate government financing, telemedicine promises to enhance the treating of communicable and non-communicable diseases as well as support health infrastructure. It can also alleviate poverty among vulnerable groups and hard-to-reach communities in Africa with adequate government financing. However, given the lack of funding in Africa, the challenges in implementing telemedicine require global and national strategies before it can yield promising results. This is especially true in regards to alleviating the multidimensionality of poverty in post-COVID-19 Africa.
Keywords: Telemedicine, Resource-poor, Health issues, Poverty alleviation, Coronavirus disease 2019 (COVID-19), Post-COVID-19 reformation, Africa
1. Introduction
The exponential impacts of the coronavirus disease 2019 (COVID-19) pandemic on African health systems and health-related issues are undeniable. The World Health Organization (WHO) declared a pandemic and alerted the public, healthcare workers, governments, and countries on controversies and issues surrounding the risk factors, prevention, and treatments of COVID-19. The global response was swift but neglected vital concerns about healthcare workers’ safety, facilities, and healthcare delivery to resource-poor regions. The pandemic triggered redirecting of already-strained health workers and state budget resources from fighting existing diseases—such as HIV, tuberculosis, and malaria—to the front lines of the new global health emergency. The result of this underscored health financing gaps that are heightened by poverty.1
Poverty has been a complex concept to define or conceptualize. Global policies have targeted resolving the 1 USD per day threshold set in 1990, the absolute line, national poverty line, personal consumption, purchasing power parity, and newly suggested added societal poverty line to reflect realities in both higher income and low-income countries.2, 3 However, existing literature agreed about poverty being multidimensional.4 Access to capital and income influence the kind of healthcare and other services accessed and consumed by households and families in rural villages, towns, and megacities.5 The cycle of poverty in Africa is not a new topic. However, it has been aggravated by the public health emergencies stemming from the COVID-19 global pandemic. First, poverty has consistently bred diseases in Africa pre-COVID-19, and the prevalence of diseases has been attributed to low standards of living and lack of access to healthcare services.6, 7 Thus, the advancement in healthcare service delivery through telemedicine and the willingness of Africans to adopt it may foster development in impoverished regions where healthcare services are already in short supply. The COVID-19 pandemic has exposed poverty and health vulnerabilities in hard-to-reach communities globally.8 The peculiarities of the hard-to-reach communities in Africa are characterized by multidimensionality of poverty, including health poverty;4 hence, adopting telemedicine is a promising prospect for improving the quality of life on the continent.
Telemedicine in global health has been considered ideal by health stakeholders, including the World Bank and WHO. According to the WHO, telemedicine can reduce the impacts of limited healthcare workers and long hours spent on routine health cases in clinics, which promotes efficiency and reduces stress on healthcare workers.9 The innovation ensures scheduling flexibility, speed, timeliness, and easy delivery of health services through mobile applications and other technological devices shared by clinicians and patients, limiting regular physical contact that could otherwise increase health risks. However, despite observable prospects for vulnerable healthcare workers, and resource-poor populations, the innovation has not yet enjoyed a wider adoption during the COVID-19 pandemic.
The global public health emergency exposed the fragility of Africa's healthcare capacity as well as health worker's vulnerabilities, but the worldwide surge in the use of technology during the pandemic highlighted a possible solution for overcoming poverty and meeting health assistance needs in Africa's developing countries—specifically, the broader adoption of telemedicine. Central questions crucial to the current study include how the prominence of and efforts to use telemedicine help provide solutions toward poverty and its role in healthcare treatment in poor African countries. However, there are multiple barriers to adopting and scaling telemedicine in Africa, especially where policy and program implementation include a broad range of stakeholders.
The present study first explored and summarized the literature on telemedicine applications in different African countries to investigate popular applications, barriers, and scaling-up of telemedicine to combat public health issues such as inadequate healthcare facilities, health worker overload, information sharing, testing, and delivery of results. Secondly, we explored how advancements in telemedicine may be harnessed to alleviate poverty among resource-poor and hard-to-reach populations. The evidence from these studies can increase the adoption of telemedicine in Africa and provided laudable solutions towards overcoming the global multidimensionality of poverty.
2. Materials and methodology
2.1. Search approach
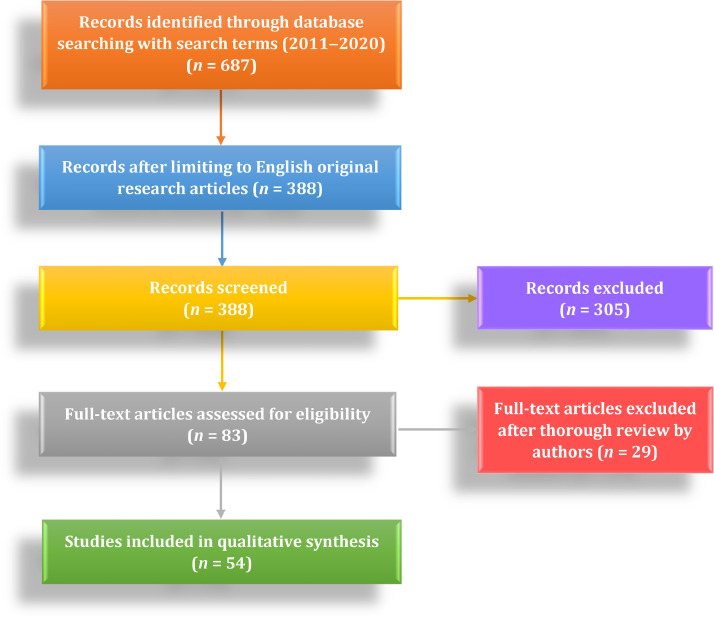
On January 20, 2021, the Scopus database was searched to identify literature reporting evidence in Africa on implementing various telemedicine modes from January 1, 2011 to December 31, 2020. Searching was limited to studies in English (see Fig. 1 ). Mesh terms “telemedicine” OR “mHealth” OR “telehealth” OR “eHealth” AND “Africa” were used to search under TITLE-ABS-KEYWORD in the database to retrieve articles screened for the review. The study adopted the search, appraisal, synthetic and analytical framework to review data sources and recorded results on a Microsoft Excel sheet. The authors appraised titles and abstracts of all search results, and finally, the full texts of the selected publications were obtained to determine inclusion. An in-depth discussion with co-authors resolved disagreements on fulfillment of the inclusion criteria until a consensus was reached. We had to report quantitatively on the process of implementation, use, and evaluation of telemedicine. We considered published literature focusing on Africa, especially Sub-Saharan Africa and those with the inclusion of Africa among low- and middle-income countries. Thus, non-African-centered articles were excluded.
Fig. 1.
Flow chart of document retrieval from Scopus database.
2.2. Data extraction
The included studies were reviewed independently by four different authors. The studies were also examined in full text, and data was collected regarding types of publication, type of study, countries, telemedicine mode implemented/evaluated, type of health issues, number of studies and challenges/barriers, and efforts to scale them. As part of the analysis, we sought to describe and highlight telemedicine's prominence through the nature of studies, different fields, and modalities of their implementation. Subsequently, we analyzed telemedicine's interests, the difficulties and limitations, and the scaling efforts described across the identified studies.
3. Results
This study initially had 687 articles screened to 83 papers at the review's commencement. A careful examination of all literature and elimination of studies that didn't focus on or only faintly mentioned Africa was done. After applying the selection criteria, 54 articles were included in this review.
A total of 13 (24.07%) of the articles were cross-sectional studies with the collection and retrospective analysis, and concurrently, 26 (48.15%) of the studies were qualitative studies based on interviews and ethnographic reports of experts in the field. In the final analysis, 9 (16.67%), 5 (9.26%), and 1 (1.85%) of the rest of the articles were survey, mixed, and cohort studies, respectively.
3.1. Geographies and fields of implementation
The geographies of articles included South Africa 22 (40.74%), Nigeria 5 (9.26%), Ghana 6 (11.11%), and Malawi 2 (3.70%). About 18.52% was broadly categorized as Sub-Saharan Africa/middle-low-income region. Sudan, Sierra Leone, Rwanda and other African countries in specifics cumulatively account for 16.67% of regions included in the study. To understand telemedicine and its role in meeting global health needs in Africa's countries, the study categorized selected studies into those that focused on communicable diseases, non-communicable diseases and those focusing on healthcare facilities and healthcare workers’ conditions and readiness to embrace telemedicine. The analysis exposed the adoption of telemedicine in supporting solutions towards the goal of overcoming poverty globally.
The published studies spanned communicable diseases, non-communicable diseases, and the readiness or application of telemedicine and frameworks to improve Africa's healthcare services and facilities, as shown in Table 1 .
Table 1.
The characteristics of the selected articles (n = 54).
| Study area | Reference | Field of implementation | Type of telemedicine | Country/Region covered |
|---|---|---|---|---|
| Communicable diseases | 10–15 | HIV & AIDS /Reproductive health | Smartphone | South Africa10, 11, 12, 13, 14, 15 |
| 16–19 | Maternal/Child healthcare | Smartphone apps/SMS | South Africa,16 Ghana,17,19 Rwanda18 | |
| 20–21 | Ebola | Smartphone/Tablet | Sierra Leone,20 Nigeria21 | |
| 22 | Tuberculosis | Cellular phone | South Africa22 | |
| Non-communicable diseases | 23–24 | Hypertension | Smartphone/SMS | Nigeria,23 South Africa24 |
| 25–31 | Cancer | Phone, Telegraphic text, screening | Ghana,25, 26 Sub-Saharan Africa,27, 28,31 South Africa,29 Nigeria30 | |
| 32 | Stroke | Smartphone | Ghana32 | |
| 33 | Chronic headache | Mobile phone | Sub-Saharan Africa33 | |
| 34–38 | Hearing loss & Screening | Smartphone | Malawi,34 South Africa35, 36, 37, 38 | |
| 39 | Mental health | Smartphone/Video | Ghana39 | |
| 40 | Diabetes | GPS/Laptop | Sub-Saharan Africa40 | |
| 41 | Burn | Smartphone | South Africa41 | |
| 42–61 | Workers/Facilities | Smartphone/Tablet/ Video | Sub-Saharan Africa,42,46,51,55,59 South Africa,43,53, 54,56,60 Nigeria,44,57 Senegal,45 Ethiopia,47 Sudan,48 Kenya,49 Uganda,50 Swaziland,52 Seychelles,58 Malawi61 | |
| 62–63 | Scaling use frameworks | Teledermatology | South Africa62, 63 |
SMS: short message service.
3.2. Telemedicine in the treatment of communicable diseases
The study explored telemedicine's application to infectious diseases such as HIV and AIDS, sexual and reproductive health (SRH) treatments, Ebola, and tuberculosis in Africa, especially among hard-to-reach populations. In specific terms, publications on mHealth technologies like smartphones and tutorial applications being used to reinforce Ebola contact tracing, monitor existing HIV and AIDS prevention programs, HIV home-based testing and counseling, and SRH among youth and adults.10, 11 , 20, 21 These studies clearly showed that between 2011‒2020, smartphones and mobile apps enabled medical healthcare. In addition, these studies observed that in countries such as Malawi and South Africa, mHealth technologies including smartphones, short message service (SMS), and mobile apps provided innovative ways to offer young adults access to reproductive health treatment and information. Studies on HIV/AIDS and SRH related issues explored usage and preference, candidacy, and effectiveness of mobile phones, applications, and web portals to support access to HIV/AIDS prevention and care as well as SRH treatments among youth and adults.
Therefore, telemedicine that included HIV/AIDS home-based testing and counseling offered a one-stop-shop to alleviate poverty by targeting rural poor hindered by shortages of funds and great distances to access healthcare. Health staff in telemedicine also perceived their role as a special mission that empowers people. Some patients understood and utilized this mindset to bond socially and get answers to significant problems. The technological assets provided timely and accurate patient data. Health officials used aggregated data to direct resources and address shortages of supplies like drugs.10 , 12, 13 In treating tuberculosis, telephone triage provided an effective management style of after-hours patient loads at primary healthcare centers to reduce overloads.22
MHealth biometrics and mobile phone apps have been carefully adapted to provide patient identification, information, and learning experience during an emergency. Despite the difficulties of achieving high-quality contact tracing in Africa's low-resource environments, the use of contact tracing apps Dimagi Comms Care Platform in Sierra Leone was an indication of mHealth progress. Public adherence to its use showed a general preference for intelligent solutions for treating such health emergencies as Ebola.20
South Africa has the highest number of mobile phone users in Africa. MHealth projects such as Young Africa Live has 2 million registered youth. Young Africa Live has a partnership with Vodacom and development agencies such as the U.S. Agency for International Development (USAID). The platform facilitates educational and health content that empowers youth to learn, share ideas, and make informed decisions on sexual matters. Significantly, the users not only change their own lives but subsequently act as agents of social change that address issues at a societal level.
Despite the aforementioned gains, challenges to the full adoption of telemedicine are still prevalent. mHealth projects in most countries, particularly South Africa, progressed without dealing with contentious issues such as low-skilled health expertise, and social actors’ role in sexual health policies and implementation. Several initiatives neglected sexual rights and stigmatization.15 Other complaints are related to issues about privacy in the willingness to use mobile apps, SMS, and interactive voice messages such as those on South Africa's MomConnect and Rwanda's RapidSMS for maternal and child healthcare.16, 17, 18, 19
3.3. Non-communicable diseases and implementation of telemedicine
One of telemedicine's standard applications in this study focused on non-communicable diseases including hypertension, hearing loss, cervical and breast cancer, and chronic headache. The studies captured the application of several innovative uses of smartphones, personalized text, SMS, and videos by healthcare workers to treat hypertension, cancer, and chronic headache There were popular views about the effective use of smartphones and short messages to improve hypertensive patients’ health knowledge and behavioral change. Patients’ ability to access health information via mHealth helped build trust and confidence in the expertise of health workers.23
Furthermore, smartphones and personalized texts were used to implement and reinforce post-healthcare treatment and services, particularly task shifting and clients’ follow-up. For example, these technologies were deployed in task shifting and allocation of clinicians in charge of post-stroke patients.32 , 40 Studies showed that healthcare workers adapted well to the treatment of cervical and breast cancers. Smartphone, SMS, and teleradiotherapy text and network immensely helped management and follow-up with clients receiving cancer screening programs.25, 26, 27, 28, 29, 30
Telehealth adapted well to direct expertise and skills learned towards treating other diseases and conditions as well. A typical case cited was the mHealth program DREAM which, as argued, can help fight against chronic headache, which continues to affect millions of individuals in Sub-Saharan Africa, where resources are limited.33 Audiovisual usage was implemented, assessed, and considered a prospect in treating people with a mental health condition in Ghana.39
Multiple publications included the use of smartphones for consultation, referral, and screenings for hearing conditions. Recent studies testing the accuracy and reliability of self-test audiometry in adults are comparative, focused on smartphone self-test in non-sound treated environments, and reference audiometry in community clinics in limited-resource settings.35 Others concentrated on the accuracy and reliability of smartphone and audio teleology for self-test audiometry in addition to screening services for diabetes in adults in low-income and vulnerable communities.35, 36 Additional studies found that telehealth can enhance the treatment of burn conditions and hearing loss in Africa's limited-resource communities among both adults and children.34 , 37, 38 , 41
3.4. Implementation and readiness of healthcare workers and facilities
This section investigated healthcare workers, other stakeholders, and healthcare facilities favoring a systematic adoption of telemedicine in public health. In this category, some studies investigated healthcare workers’ readiness and facilities to adopt, integrate, and implement telemedicine. Adopting and applying user-friendly mHealth technologies to Africa's health system and healthcare delivery is crucial.42 However, the implementation can only be strategic when readiness toward the objective is investigated and recreated. Among the reviewed studies was a reflective argument that purported that implementing telemedicine in African countries failed proper needs assessment. This oversight in technological-push countries, including South Africa, leads to a large amount of dormant equipment.43
A similar trend of neglect by clinicians was traced to Nigeria's government hospitals. Telemedicine was regarded as a dual responsibility in which reinforcement factors could be used to motivate clinicians.44 However, in district hospitals and health centers, Senegalese physicians would accept and use telemedicine if they had sufficient time and it were easy to use.45 For years, RAFT's (Réseau en Afrique Francophone pour la Télémédecine) educational and clinical experience built the capacity of some francophone and anglophone health professionals, technicians and scientific associations, and societies via telemedicine to combat numerous diseases, including tuberculosis. However, lessons that must be learned include aligning eHealth and telemedicine activities with local needs and national health strategies.46 In Sudan, the universities’ roles in evolving and scaling the Gezira Family Medicine Projects using video conferencing and the virtual lecture was phenomenal. However, broader investigations are required on family medicine, primary care doctors, and the negative impact of flooding and logistics.48
Studies observed that strategy, technology, users, and organization are crucial influencers of telemedicine acceptance in Africa. Embracing and integrating telemedicine required the substantial need to improve health centers in many countries, such as Ethiopia and Sudan.47, 48 In Kenyan hospitals, patient and community-centered approaches are essential in adopting and driving required mHealth infrastructure and investment before significant progress can be made.49 However, this review found that readiness to integrate telemedicine varies according to stakeholder types, job title, and roles in the health field, as well as health situations. In Uganda, more physicians and health administrators were positive about adoption than nurses, allied workers, and the public.50 Divergent views from the stakeholder's perspective cannot override the success of Malawi's SL eCCM App and Swaziland's use of SMS to deliver blood test results to clinics in remote areas. However, further studies are needed on how national wealth and community leaders’ interests can influence consensus and conflicting priorities.51, 52
Limited studies investigated and provided evidence on the impact of external and global bodies in the adoption of and failed attempts at telemedicine in Africa. A dual approach encompasses technological and educational support, and international collaboration is needed. Only few studies focused on the use of technologies by health practitioners, patient data security concerns, and approaches toward addressing them, with the exception of South Africa. South Africa demonstrated the viability of mHealth for large-scale national health surveillance at reduced time and cost. The required time, financial resources, and full-time technicians for system set-up, design, testing, and management queries may reduce prominence in many countries. The outdatedness of paper-tracing had been highlighted as feedback, and follow-up gaps limited reporting in health systems. mHealth facilities required for referrals and recall are crucial, but few studies focused on adaptation, supports, and feedback loops. Three basic technical requirements (bandwidth, network coverage, and stable power supply) were identifiable challenges to Nigeria's palliative care. Further studies are required on how age, gender, and social status influenced the adoption of mHealth for health surveillance and what technologies and variables favor acceptance. Consequently, studies focused on scaling efforts. A survey of image-based diagnostic support in clinical and public settings identified strategies to overcome technical and organizational barriers by inviting frontline health workers, experts, and stakeholders from African countries and Sweden. More articles included in the study were on teledermatology, benefits realization management, a roadmap for sustainable scaling, and a review, but these were mainly in South Africa.
4. Discussion
This study explored the prominence of telemedicine in providing access to healthcare with a view of surveying its potential expansion given the lessons learned during the COVID-19 pandemic and its promising role in poverty alleviation in under-resourced settings of Africa. The study investigated different geographies where telemedicine was introduced, modalities adopted, and fields or diseases these health innovations were implemented in addressing. As a result, the review uncovered Africa's readiness to fully embrace telemedicine during public health emergencies such as COVID-19 in a sustainable manner without jeopardizing the concerns of stakeholders during implementation. We found mobile usage in Africa tremendously ubiquitous as a means of electronic information and telecommunication. To a significant extent, telemedicine can provide solutions to poverty alleviation, improve quality of life, and ensure universal healthcare access during public health emergencies.
The prominence of telemedicine in Africa has been evidenced by the adoption and integration of the technologies to provide essential healthcare services in remote and impoverished communities initially without primary assets to healthcare treatments. However, observed efforts were disproportional, with South Africa, Nigeria, Ghana, Malawi, Senegal in the lead and primary recipients of adoption in multiple health fields. Other countries were Uganda, Ethiopia, Sierra Leone, Swaziland, Sudan, Seychelles, Rwanda, and Kenya. Reviewed articles also included those on Sub-Saharan African and low- and middle-income countries, citing more than one African country.
Their studies acknowledged mixed perceptions, preferences, and efforts to take advantage of evolving technologies through Smartphones, tablets, Mobile Apps, Web portals, and GPS to facilitate healthcare treatment, especially in rural and low-resource communities. SMS, interactive voice (audio), and telegraphic text make it easy to send, collect, and share vital health information between healthcare practitioners and end-users. Remarkably, there was the implementation of consultation, counseling, and care in the treatment of HIV/AIDS, SRH, and maternal-child health (MCH). The reconciliation of health policy and mobile technology integration was scantly mentioned in literature. The imbalance and incompatibility of skills and digital knowledge of health experts were left unaddressed due to the absence of strategic government policies and initiatives toward a systemic use of mHealth in hospitals.15 The social integration of mHealth into the broader society has been overlooked. Data handling and privacy concerns are endemic, particularly when they involved such sensitive issues as stigmatization.
One of the implementation fields was teleconsultation, counseling, and care for treating communicable diseases like HIV/AIDS, SRH, and MCH. HIV-positive women receiving antiretroviral therapy, pregnant women, and youth had no trouble accepting the mHealth technologies MomConnect, mAssist, and Young Africa Live. These applications helped ease access to pregnancy information, sex education, and other healthcare data; they make treatments available, accessible, and convenient.16 The incomplete and late arrival of paper-based contact tracing during the Ebola control in Sierra Leone provided evidence of inherent dangers during global public health emergencies. The studies, including that of Nigeria's mobile tutorial application, is evidence that Africa is ripe for the mHealth revolution to a certain extent. If challenges observed such as those in mHealth technology Ebola contact tracing apps are strategically addressed, the emerging data revolution can improve public health accessibility and data on drugs, patients’ health conditions, diseases, and control measures in Africa.20, 21
Optimistically speaking, global funding and growing commitment to Sustainable Development Goals 3 and 17 related to health issues show that efforts toward universal healthcare delivery are well under way.64, 65 Health financing, or healthcare funding, has a significant correlation and contribution to the vitality of the healthcare system, which later improves the health and wellbeing of children, youth, and the elderly.66 As such, Africa's changing economic structure had created healthy financial outlooks in the decade before the COVID-19 pandemic.67 Thus, increased national wealth should generate health funding that improves the healthcare system, health status, and the quality of life of resource-poor populations. Government funding has been the primary source of healthcare provision in Africa. However, a WHO report in 2018 showed that government spending has often fluctuated since 2002 and remained low as of 2018.68 In Kenya, Nigeria, and South Africa, the governments attempted to mobilize domestic funding for healthcare by increasing tax revenue collection, which led to absolute increases in public health spending but not in real per capita terms.69
Telemedicine, through the years, has gradually become a vital force driving social change and poverty alleviation in African communities. Innovative technologies provide fast and easy ways to reach millions of African youths in South Africa, Tanzania, and Kenya. In the result analysis, our study identified the role played by the platform Young Africa Live created by Praekelt Foundation with USAID partnership. The platform aided in generating educational and health content that helped millions to discuss related matters that inform decisions about their health, education, and social networks. Furthermore, telemedicine was also used to empower medical personnel and scale up family medicine. Family medicine is a relatively new field in African nations compared to the United States and other developed countries. Therefore, the investment in state health capacity has been hailed as the right path.
With Africa's readiness to adopt various forms of telemedicine, the remoteness of hard-to-reach populations (primarily due to low economic status), can be tackled with robust government financing. Although it has been postulated that financing healthcare can be challenging,70 systematic planning may yield laudable results in improving telemedicine coverage in resource-poor regions. Evidenced in countries like China, where a five-phase poverty alleviation program has produced admirable results in resource-poor communities over the last four decades,71 implementing a similar approach to scaling up telemedicine in Africa will likely alleviate poverty and improve healthcare coverage and delivery. Phased-in implementation may be adopted by the joint task force of the WHO and national governments by providing funding to increase awareness of currently available telemedicine options. In parallel, expansion of resources should include the installation of health posts and centers equipped with diagnostic, treatment, and preventive care tools that are supported by technologies, such as teleconsultation equipment and software. Thusly, healthcare quality can be raised while reducing the burden of cost and need for health financing in resource-poor communities.
There are a few limitations to be considered when adopting this study's findings. First, the study's methodological approach in search and appraisal was solely based on the authors’ discretions and, therefore, may be subject to bias in selecting articles included in the review. Secondly, telemedicine is a complex domain that is gaining massive global coverage; consequently, it is impossible to cover all of its application forms in a single study. Lastly, the multidimensionality of poverty creates a scope dilemma, and thus future studies addressing telemedicine and health should more closely focus their discourse.
5. Implications for future research and direction
Telemedicine has enormous potential and technological toolkits that can deliver cutting-edge solutions to global poverty and healthcare delivery during any global public health emergency. We demonstrated in this study that apart from being embraced by healthcare workers and growing technologically-inclined young Africans, telemedicine to a significant extent offered assistance in healthcare delivery and overcoming the burdens of poverty in Africa. It can be adapted well to Africa's remote communities that are without access to health facilities and workers while facilitating social change and mobility. Nevertheless, there are particular challenges for which we have proffered solutions. We hope that future studies will incorporate other disciplines, like economics and finance, to appropriate the financial funds for large-scale adoption of telemedicine in healthcare centers across Africa. In addition, future studies can focus on digital supply chains, value chains, and the prevention of technology redundancy.
Furthermore, linking tele-financing, investment ecosystems, and private investors to telemedicine is essential. Most African governments are still new to telemedicine. Its absence from the priority list on the national health framework indicates poor access to funds and mHealth innovation. Studies can focus on global telemedicine investment, national telemedicine investment, their drivers, and how they integrate and innovate to address health and poverty globally. Future studies should investigate how policies emerge, the role of norms in telehealth policies, and how they become institutionalized. These studies can focus on mechanisms to reconcile different priorities and conflicts in mHealth technologies and the roles of social networks.
Additionally, future studies can investigate the governance of mHealth technologies. Privacy, abortion, and women's rights are issues that the mHealth platform alone cannot solve. Questions remain including whether value co-creation could solve this problem, and how innovation emerges. Future studies can also explore the technology architectures to see how simple, easy-to-use, and socio-cultural-specific telehealth technologies can be manufactured, marketed, and accessed in developing countries. Finally, future studies can focus on digital gaps and how such gaps can be bridged, possibly through universities or national and international collaborations.
6. Conclusion
Telemedicine is still relatively new in Africa, considering geographies of implementation out of fifty-four countries. Africa's low-resource societies face several problems, including great travel distances for frequent health treatments to under-staffed hospitals, which are concentrated mainly in big cities. In emergencies, mHealth technologies on smartphones, mobile apps and web portals have the unique advantages of data availability, real-time sharing of health status, tutorials and a more-affordable way of securing treatments.
Health systems are faced with an unprecedented opportunity to learn and synergize from the recent experiences in Africa and the rest of the world triggered by the global COVID-19 health crisis. The lessons learned should be used to chart a safer path towards poverty alleviation. Sub-Saharan African countries need national health policies that incorporate eHealth technologies and telemedicine strategies to tackle emerging infectious and viral diseases like Ebola and COVID-19. The national eHealth strategies should consider stakeholders’ contributions to health and information in addition to input from medical researchers, eHealth experts, social advocates, mobile service providers, doctors, nurses, and other medical professionals. These measures will enable stakeholders to provide reliable information on the cost and resources needed for low-cost but efficient eHealth technologies across the board. Data availability, sharing, and privacy concerns should be treated with fairness and respect for the owners' security and wishes. Through legislation and public awareness, governments can address sensitive issues, which may include stigmatization, sexual abuse, and rights, and the inequities that fuel them.
CRediT author statement
Tosin Yinka Akintunde: Conceptualization, Methodology, Validation, Formal analysis, Data curation, Writing—Original draft, Writing—Review & Editing, Visualization, Supervision. Oluseye David Akintunde: Methodology, Validation, Data curation, Writing—Review & Editing. Taha Hussein Musa: Methodology, Data curation, Writing—Review & Editing. Muhideen Sayibu: Data curation, Writing—Review & Editing. Angwi Enow Tassang: Methodology, Validation, Resources, Writing—Review & Editing. Linda M. Reed: Writing—Review & Editing. Shaojun Chen: Supervision, Writing—Review & Editing.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Edited by Yanjie Zhang
References
- 1.Oladele TT, Olakunde BO, Oladele EA, Ogbuoji O, Yamey G. The impact of COVID-19 on HIV financing in Nigeria: a call for proactive measures. BMJ Glob Health. 2020;5(5):e002718. doi: 10.1136/bmjgh-2020-002718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ravallion M, Chen S, Sangraula P. Dollar a day revisited. World Bank Econ Rev. 2009;23(2):163–184. doi: 10.1093/wber/lhp007. [DOI] [Google Scholar]
- 3.Jolliffe D, Prydz EB. Societal poverty: a relative and relevant measure. World Bank Econ Rev. 2021;35(1):180–206. doi: 10.1093/wber/lhz018. [DOI] [Google Scholar]
- 4.Clarke P, Erreygers G. Defining and measuring health poverty. Soc Sci Med. 2020;244:112633. doi: 10.1016/j.socscimed.2019.112633. [DOI] [PubMed] [Google Scholar]
- 5.De Vreyer P, Lambert S. Inequality, poverty, and the intra-household allocation of consumption in Senegal. World Bank Econ Rev. 2021;35(2):414–435. doi: 10.1093/wber/lhz052. [DOI] [Google Scholar]
- 6.Beegle K, Christiaensen L, Dabalen A, Gaddis I. The World Bank; Washington, DC: 2016. Poverty in a rising Africa. [DOI] [Google Scholar]
- 7.Mars M. Telehealth in the developing world. International Development Research Centre. CRC Press; Canada: 2011. [Google Scholar]
- 8.Kronenfeld JP, Penedo FJ. Novel Coronavirus COVID-19: telemedicine and remote care delivery in a time of medical crisis, implementation, and challenges. Transl Behav Med. 2021;11(2):659–663. doi: 10.1093/tbm/ibaa105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO Global Observatory for eHealth. Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. https://apps.who.int/iris/handle/10665/44497. Accessed February 5, 2021.
- 10.Adeagbo O, Herbst C, Blandford A, et al. Exploring people's candidacy for mobile health-supported HIV testing and care services in rural kwaZulu-natal, South Africa: qualitative study. J Med Internet Res. 2019;21(11):1–13. doi: 10.2196/15681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Comulada WS, Wynn A, van Rooyen H, Barnabas RV, Eashwari R, van Heerden A. Using mHealth to deliver a home-based testing and counseling program to improve linkage to care and ART adherence in rural South Africa. Prev Sci. 2019;20(1):126–136. doi: 10.1007/s11121-018-0950-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mogoba P, Phillips TK, Myer L, Ndlovu L, Were MC, Clouse K. Smartphone usage and preferences among postpartum HIV-positive women in South Africa. AIDS Care. 2019;31(6):723–729. doi: 10.1080/09540121.2018.1563283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Heerden A, Harris DM, van Rooyen H, et al. Perceived mHealth barriers and benefits for home-based HIV testing and counseling and other care: Qualitative findings from health officials, community health workers, and persons living with HIV in South Africa. Soc Sci Med. 2017;183:97–105. doi: 10.1016/j.socscimed.2017.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Visser M, Kotze M, van Rensburg MJ. An mHealth HIV prevention programme for youth: lessons learned from the iloveLife.mobi programme in South Africa. AIDS Care. 2020;32(sup2):148–154. doi: 10.1080/09540121.2020.1742866. [DOI] [PubMed] [Google Scholar]
- 15.Waldman L, Stevens M. Sexual and reproductive health and rights and mHealth in policy and practice in South Africa. Reprod Health Matters. 2015;23(45):93–102. doi: 10.1016/j.rhm.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Barron P, Pillay Y, Fernandes A, Sebidi J, Allen R. The MomConnect mHealth initiative in South Africa: early impact on the supply side of MCH services. J Public Health Policy. 2016;37(2):S201–S212. doi: 10.1057/s41271-016-0015-2. [DOI] [PubMed] [Google Scholar]
- 17.Brinkel J, Dako-Gyeke P, Krämer A, May J, Fobil JN. An investigation of users’ attitudes, requirements and willingness to use mobile phone-based interactive voice response systems for seeking healthcare in Ghana: a qualitative study. Public Health. 2017;144:125–133. doi: 10.1016/j.puhe.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 18.Ruton H, Musabyimana A, Gaju E, et al. The impact of an mHealth monitoring system on health care utilization by mothers and children: an evaluation using routine health information in Rwanda. Health Policy Plan. 2018;33(8):920–927. doi: 10.1093/heapol/czy066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brinkel J, May J, Krumkamp R, et al. Mobile phone-based interactive voice response as a tool for improving access to healthcare in remote areas in Ghana – an evaluation of user experiences. Trop Med Int Health. 2017;22(5):622–630. doi: 10.1111/tmi.12864. [DOI] [PubMed] [Google Scholar]
- 20.Danquah LO, Hasham N, MacFarlane M, et al. Use of a mobile application for Ebola contact tracing and monitoring in northern Sierra Leone: a proof-of-concept study. BMC Infect Dis. 2019;19(1):1–12. doi: 10.1186/s12879-019-4354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Otu A, Ebenso B, Okuzu O, Osifo-Dawodu E. Using a mHealth tutorial application to change knowledge and attitude of frontline health workers to Ebola virus disease in Nigeria: a before-and-after study. Hum Resour Health. 2016;14(1):1–9. doi: 10.1186/s12960-016-0100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adeniji AA, Mabuza LH. ‘Telephone Triage’: a possible means of managing the after-hours patient load at primary health care facilities in South Africa. South African Fam Pract. 2018;60(6):219-224. doi:10.1080/20786190.2018.1504863.
- 23.Cremers AL, Alege A, Nelissen HE, et al. Patients’ and healthcare providers’ perceptions and practices regarding hypertension, pharmacy-based care, and mHealth in Lagos, Nigeria: a mixed methods study. J Hypertens. 2019;37(2):389–397. doi: 10.1097/HJH.0000000000001877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hacking D, Haricharan HJ, Brittain K, Lau YK, Cassidy T, Heap M. Hypertension health promotion via text messaging at a community health center in South Africa: A mixed methods study. JMIR mHealth uHealth. 2016;4(1):1–9. doi: 10.2196/mhealth.4569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asgary R, Adongo PB, Nwameme A, et al. MHealth to train community health nurses in visual inspection with acetic acid for cervical cancer screening in Ghana. J Low Genit Tract Dis. 2016;20(3):239–242. doi: 10.1097/LGT.0000000000000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Asgary R, Cole H, Adongo P, et al. Acceptability and implementation challenges of smartphone-based training of community health nurses for visual inspection with acetic acid in Ghana: mHealth and cervical cancer screening. BMJ Open. 2019;9(7):e030528. doi: 10.1136/bmjopen-2019-030528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Datta NR, Heuser M, Bodis S. A roadmap and cost implications of establishing comprehensive cancer care using a teleradiotherapy network in a group of sub-saharan african countries with no access to radiation therapy. Int J Radiat Oncol Biol Phys. 2016;95(5):1334–1343. doi: 10.1016/j.ijrobp.2016.03.030. [DOI] [PubMed] [Google Scholar]
- 28.Foerster M, Anele A, Adisa C, et al. Few losses to follow-up in a Sub-Saharan African cancer cohort via active mhealth follow-up: the prospective ABC-DO breast cancer cohort. Am J Epidemiol. 2020;189(10):1185–1196. doi: 10.1093/aje/kwaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moodley J, Constant D, Botha MH, van der Merwe FH, Edwards A, Momberg M. Exploring the feasibility of using mobile phones to improve the management of clients with cervical cancer precursor lesions. BMC Womens Health. 2019;19(1):1–10. doi: 10.1186/s12905-018-0702-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Odigie VI, Yusufu LMD, Dawotola DA, et al. The mobile phone as a tool in improving cancer care in Nigeria. Psychooncology. 2012;21(3):332–335. doi: 10.1002/pon.1894. [DOI] [PubMed] [Google Scholar]
- 31.Okunade K, Bashan Nkhoma K, Salako O, et al. Understanding data and information needs for palliative cancer care to inform digital health intervention development in Nigeria, Uganda and Zimbabwe: protocol for a multicountry qualitative study. BMJ Open. 2019;9(10):1–9. doi: 10.1136/bmjopen-2019-032166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nichols M, Sarfo FS, Singh A, et al. Assessing mobile health capacity and task shifting strategies to improve hypertension among ghanaian stroke survivors. Am J Med Sci. 2017;354(6):573–580. doi: 10.1016/j.amjms.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leone M, Palombi L, Guidotti G, et al. What headache services in sub-Saharan Africa? The DREAM program as possible model. Cephalalgia. 2019;39(10):1339–1340. doi: 10.1177/0333102419849014. [DOI] [PubMed] [Google Scholar]
- 34.Pimmer C, Mbvundula F. One message, many voices: mobile audio counselling in health education. J Health Care Poor Underser. 2018;29(1):463–480. doi: 10.1353/hpu.2018.0031. [DOI] [PubMed] [Google Scholar]
- 35.Sandström J, Swanepoel DW, Laurent C, Umefjord G, Lundberg T. Accuracy and reliability of smartphone self-test audiometry in community clinics in low income settings: a comparative study. Ann Otol Rhinol Laryngol. 2020;129(6):578–584. doi: 10.1177/0003489420902162. [DOI] [PubMed] [Google Scholar]
- 36.Thornton J. Remotest working. Nurs Stand. 2014;28(27):19. doi: 10.7748/ns2014.03.28.27.19.s26. [DOI] [PubMed] [Google Scholar]
- 37.van Wyk T, Mahomed-Asmail F, Swanepoel DW. Supporting hearing health in vulnerable populations through community care workers using mHealth technologies. Int J Audiol. 2019;58(11):790–797. doi: 10.1080/14992027.2019.1649478. [DOI] [PubMed] [Google Scholar]
- 38.Yousuf Hussein S, Swanepoel DW, Mahomed F, Biagio de Jager L. Community-based hearing screening for young children using an mHealth service-delivery model. Glob Health Action. 2018;11(1):1467077. doi: 10.1080/16549716.2018.1467077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ben-Zeev D. Mobile health for mental health in West Africa: the case for Ghana. Psychiatr Serv. 2018;69(7):741–743. doi: 10.1176/appi.ps.201700555. [DOI] [PubMed] [Google Scholar]
- 40.Ovbiagele B. Tackling the growing diabetes burden in Sub-Saharan Africa: a framework for enhancing outcomes in stroke patients. J Neurol Sci. 2015;348(1-2):136–141. doi: 10.1016/j.jns.2014.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.den Hollander D, Mars M. Smart phones make smart referrals: the use of mobile phone technology in burn care—a retrospective case series. Burns. 2017;43(1):190–194. doi: 10.1016/j.burns.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 42.Folaranmi T. MHealth in Africa: challenges and opportunities. Perspect Public Health. 2014;134(1):14–15. doi: 10.1177/1757913913514703. [DOI] [PubMed] [Google Scholar]
- 43.Treurnicht MJ, Van Dyk L. A decision support system for equipment allocation in a telemedicine referral network. S Afr J Ind Eng. 2014;25(1):29–38. doi: 10.7166/25-1-641. [DOI] [Google Scholar]
- 44.Adenuga KI, Iahad NA, Miskon S. Towards reinforcing telemedicine adoption amongst clinicians in Nigeria. Int J Med Inform. 2017;104:84–96. doi: 10.1016/j.ijmedinf.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 45.Ly BA, Labonté R, Bourgeault IL. The beliefs of senegal's physicians toward the use of telemedicine. Pan Afr Med J. 2019;34:1–12. doi: 10.11604/pamj.2019.34.97.20216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bediang G, Perrin C, de Castañeda RR, et al. The RAFT telemedicine network: Lessons learnt and perspectives from a decade of educational and clinical services in low- and middle-incomes countries. Front Public Health. 2014;2:180. doi: 10.3389/fpubh.2014.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abera Amare A, Mengesha GH, Musa PF. Assessment of Ethiopian health facilities readiness for implementation of telemedicine. Commun Assoc Inf Syst. 2014;34(1):1247–1268. doi: 10.17705/1cais.03465. [DOI] [Google Scholar]
- 48.Mohamed KG, Hunskaar S, Abdelrahman SH, Malik EM. Scaling up family medicine training in Gezira, Sudan - a 2-year in-service master programme using modern information and communication technology: a survey study. Hum Resour Health. 2014;12(1):1–9. doi: 10.1186/1478-4491-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ngongo BP, Ochola P, Ndegwa J, Katuse P. The moderating role of top executives’ sex, level of education and knowledge on adoption of mobile health applications by hospitals in Kenya. J Healthc Leadersh. 2019;11:115–126. doi: 10.2147/JHL.S226341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kiberu VM, Scott RE, Mars M. Assessment of health provider readiness for telemedicine services in Uganda. Health Inf Manag J. 2019;48(1):33–41. doi: 10.1177/1833358317749369. [DOI] [PubMed] [Google Scholar]
- 51.Dharmayat KI, Tran T, Hardy V, et al. Sustainability of ‘mhealth’ interventions in sub-Saharan Africa: a stakeholder analysis of an electronic community case management project in Malawi. Malawi Med J. 2019;31(3):177–183. doi: 10.4314/mmj.v31i3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hao WR, Hsu YH, Chen KC, et al. LabPush: A pilot study of providing remote clinics with laboratory results via short message service (SMS) in Swaziland, Africa—A qualitative study. Comput Methods Programs Biomed. 2015;118(1):77–83. doi: 10.1016/j.cmpb.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 53.Wallis L, Hasselberg M, Barkman C, et al. A roadmap for the implementation of mHealth innovations for image-based diagnostic support in clinical and public-health settings: a focus on front-line health workers and health-system organizations. Glob Health Action. 2017;10(sup 3):1340254. doi: 10.1080/16549716.2017.1340254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Singh Y, Jackson D, Bhardwaj S, Titus N, Goga A. National surveillance using mobile systems for health monitoring: complexity, functionality and feasibility. BMC Infect Dis. 2019;19(Suppl 1):786. doi: 10.1186/s12879-019-4338-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mechael P, Nemser B, Cosmaciuc R, et al. Capitalizing on the characteristics of mhealth to evaluate its impact. J Health Commun. 2012;17(suppl 1):62–66. doi: 10.1080/10810730.2012.679847. [DOI] [PubMed] [Google Scholar]
- 56.Odendaal W, Lewin S, McKinstry B, et al. Using a mHealth system to recall and refer existing clients and refer community members with health concerns to primary healthcare facilities in South Africa: a feasibility study. Glob Health Action. 2020;13(1):1717410. doi: 10.1080/16549716.2020.1717410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Van Gurp J, Soyannwo O, Odebunmi K, et al. Telemedicine’s potential to support good dying in Nigeria: a qualitative study. PLoS One. 2015;10(6):e0126820. doi: 10.1371/journal.pone.0126820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yepes M, Maurer J, Viswanathan B, Gedeon J, Bovet P. Potential reach of mhealth versus traditional mass media for prevention of chronic diseases: Evidence from a nationally representative survey in a middle-income country in Africa. J Med Internet Res. 2016;18(5):e114. doi: 10.2196/jmir.5592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee S, Begley CE, Morgan R, Chan W, Kim SY. M-Health policy readiness and enabling factors: comparisons of Sub-Saharan Africa and organization for economic cooperation and development countries. Telemed eHealth. 2018;24(11):908–921. doi: 10.1089/tmj.2017.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jack C, Singh Y, Mars M. Pitfalls in computer housekeeping by doctors and nurses in KwaZulu-Natal: no malicious intent. BMC Med Ethics. 2013;14(suppl 1):S8. doi: 10.1186/1472-6939-14-S1-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mastellos N, Tran T, Dharmayat K, et al. Training community healthcare workers on the use of information and communication technologies: a randomised controlled trial of traditional versus blended learning in Malawi, Africa. BMC Med Educ. 2018;18(1):1–13. doi: 10.1186/s12909-018-1175-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Walters LEM, Scott RE, Mars M. Exploration of benefits realisation management for teledermatology scale-up framework development and sustainable scaling. Informatics Med Unlocked. 2019;15:100160. doi: 10.1016/j.imu.2019.02.004. [DOI] [Google Scholar]
- 63.Walters LEM, Scott RE, Mars M. A teledermatology scale-up framework and roadmap for sustainable scaling: evidence-based development. J Med Internet Res. 2018;20(6):e224. doi: 10.2196/jmir.9940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization, The World Bank. Tracking Universal Health Coverage: 2017 Global Monitoring Report. https://www.worldbank.org/en/topic/universalhealthcoverage/publication/tracking-universal-health-coverage-2017-global-monitoring-report. Accessed February 5, 2021.
- 65.Head MG, Goss S, Gelister Y, et al. Global funding trends for malaria research in sub-Saharan Africa: a systematic analysis. Lancet Glob Health. 2017;5(8):e772–e781. doi: 10.1016/S2214-109X(17)30245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nathaniel S, Khan S. Public health financing, environmental quality, and the quality of life in Nigeria. J Public Aff. 2020;20(3):e2103. doi: 10.1002/pa.2103. [DOI] [Google Scholar]
- 67.Diao X, Harttgen K, McMillan M. The changing structure of Africa's economies. World Bank Econ Rev.2017;31(2):412-433. doi:10.1093/wber/lhw070.
- 68.Current health expenditure (% of GDP)—Sub-Saharan Africa. The World Bank Group website. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?end=2018&locations=ZG&start=2000. Accessed July 5, 2021.
- 69.Doherty J, Kirigia D, Okoli C, et al. Does expanding fiscal space lead to improved funding of the health sector in developing countries?: lessons from Kenya, Lagos State (Nigeria) and South Africa. Glob Health Action. 2018;11(1):1461338. doi: 10.1080/16549716.2018.1461338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Siciliani L, Hurst J. Tackling excessive waiting times for elective surgery: a comparative analysis of policies in 12 OECD countries. Health Policy (New York) 2005;72(2):201–215. doi: 10.1016/j.healthpol.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 71.Sun Z, Zhao L, Wang S, Zhang H, Wang X, Wan Z. Targeted poverty alleviation and households’ livelihood strategy in a relation-based society: Evidence from northeast China. Int J Environ Res Public Health. 2021;18(4):1–18. doi: 10.3390/ijerph18041747. [DOI] [PMC free article] [PubMed] [Google Scholar]