Abstract
Despite documented effectiveness of pre-exposure prophylaxis (PrEP), PrEP uptake remains low among at-risk populations. The 2015 CDC report estimates that about 1.2 million people in the US have indications for PrEP. However, only 49,158 or 4% of the targeted population are currently using PrEP. Efforts to optimize uptake of PrEP may be facilitated by the development of a comprehensive theoretical framework which can be used to understand reasons for poor uptake and to develop interventions to maximize PrEP uptake and adherence. This article reviews research on correlates of PrEP uptake and presents findings organized within an Information-Motivation-Behavioral Skills (IMB) model framework. In the context of PrEP uptake, the IMB model asserts that to the extent that at-risk groups are well-informed about PrEP, motivated to act on their knowledge, and have necessary behavioral skills to seek out and initiate PrEP regimen, they will successfully overcome obstacles to initiate and adhere to PrEP. The article proposes an adaptation the IMB model for PrEP uptake, provides empirical support for the adapted IMB model extracted from related research, and discusses its application in PrEP uptake interventions.
Keywords: Pre-exposure prophylaxis, Information–motivation–behavioral skills model, PrEP uptake, Correlates of PrEP initiation
Introduction
Pre-exposure prophylaxis (PrEP) is a form of HIV prevention that uses medication to protect HIV-negative people from acquiring HIV. The combination of emtricitabine/tenofovir (marketed as Truvada) was approved by the Food and Drug Administration (FDA) in 2012 for prevention of HIV based on compelling data from several major studies [1–4] and confirmed in a systematic review [5] demonstrating that PrEP reduces the risk of HIV infection by as much as 92% [6]. The World Health Organization [7] and Centers for Disease Control (CDC) [8] have issued public health guidance on PrEP prescription.
While initial demand for PrEP following FDA approval was low, a sharp increase (as high as 332% by some estimates) has since been observed in some settings [9], with levels of interest in PrEP being especially high in metropolitan areas like New York [10] and San Francisco [11, 12]. Despite the increase in patient demand for this novel method of HIV prevention, the availability of PrEP has not been sufficiently scaled to meet demand. According to the CDC, more that 1.25 million Americans are candidates for PrEP [13]. An estimated 25% of sexually active adult men who have sex with men (N = 492,000), 18.5% of people who inject drugs (N = 115,000), and 0.4% of heterosexually active adults (N = 624,000), are at high enough risk for HIV to warrant consideration of PrEP. However, a recent study estimates that only 49,158 people are taking PrEP for prevention. It means that only about 4% of targeted population are using this prevention method [14].
Despite evidence that PrEP is effective, especially with higher adherence, a review of the recent HIV prevention intervention advances [15] demonstrated a number of issues that significantly restrict the impact of PrEP programs. Most interventions are designed intuitively and they fail to engage conceptual frameworks for HIV risk behavior change (such as the adaption of IMB model proposed here). In addition, few interventions have systematically assessed subjects’ pre-existing HIV knowledge, HIV risk reduction motivation, and their behavioral skills with respect to HIV prevention, in order to design the program according to their actual pre-existing or future needs. Furthermore, these programs often fail to motivate their clients to modify their risky behaviors or help them to acquire and retain the knowledge and skills necessary for that change. Finally, most of these interventions have not been rigorously evaluated. The limitations described above can be addressed by grounding interventions in a theoretical approach to individual-level behavioral change. This research project attempts to ground future PrEP programs using the adaptation of information–motivation–behavioral skills (IMB) model.
A comprehensive framework, such as IMB model, differs from the ‘single issue’ approach adopted in many studies in that it includes the breadth of factors, as well as the relationships among the factors that may influence PrEP uptake. There is a significant body of literature demonstrating that theoretical frameworks can be successful in predicting and promoting HIV preventive behavior [16–18]. Additionally, a number of PrEP randomized controlled trials such as CAPRISA [19], Fem-PrEP [20], iPrex [21], and Voice [22] have used information-motivation-behavioral skills model (IMB) to guide their adherence efforts. One recent publication has provided evidence for the utility of the IMB model to increase willingness to use PrEP among high-risk drug users in treatment [23].
This paper will (1) propose a comprehensive theoretical framework of factors that are likely to influence PrEP uptake, (2) provide a review of current literature on PrEP uptake, and (3) integrate findings from this literature review into the existing theoretical model (IMB) adapted for understanding and promoting PrEP uptake. Since most of the existing literature on PrEP uptake focuses on men who have sex with men, this study will adapt the same focus. Future research is needed to determine whether the same constructs proposed in this model will apply to other populations (cis-gender women, transgender people, heterosexual men).
An Information–Motivation–Behavioral Skills Model of PrEP Uptake
The present study applies the information–motivation–behavioral skills (IMB) model, a validated theoretical framework for understanding and promoting health behaviors [24], to conceptualize factors that influence PrEP uptake among men who have sex with men. Our adaptation of the IMB model for PrEP uptake describes the information, motivation, and behavioral skills that are conceptually and empirically linked to engaging in PrEP regimen, but usually described separately in the existing PrEP literature. This situated IMB model of PrEP uptake outlines interrelationships between the constructs and suggests potential mechanisms that may be used to translate this framework into comprehensive PrEP promotion interventions.
In the context of PrEP uptake, the adapted IMB model asserts that PrEP information, PrEP motivation, and PrEP behavioral skills are fundamental determinants of PrEP uptake. The situated model asserts that to the extent that men who have sex with men are well-informed about PrEP [25], motivated to act on their knowledge [26], and have necessary behavioral skills (such as negotiating PrEP with a provider [27] and a partner [28], securing funding [29], going through eligibility screening [30], and considering potential side-effects [31]) to seek out and initiate PrEP regimen, they will successfully overcome obstacles to initiate PrEP (Fig. 1).
Fig. 1.
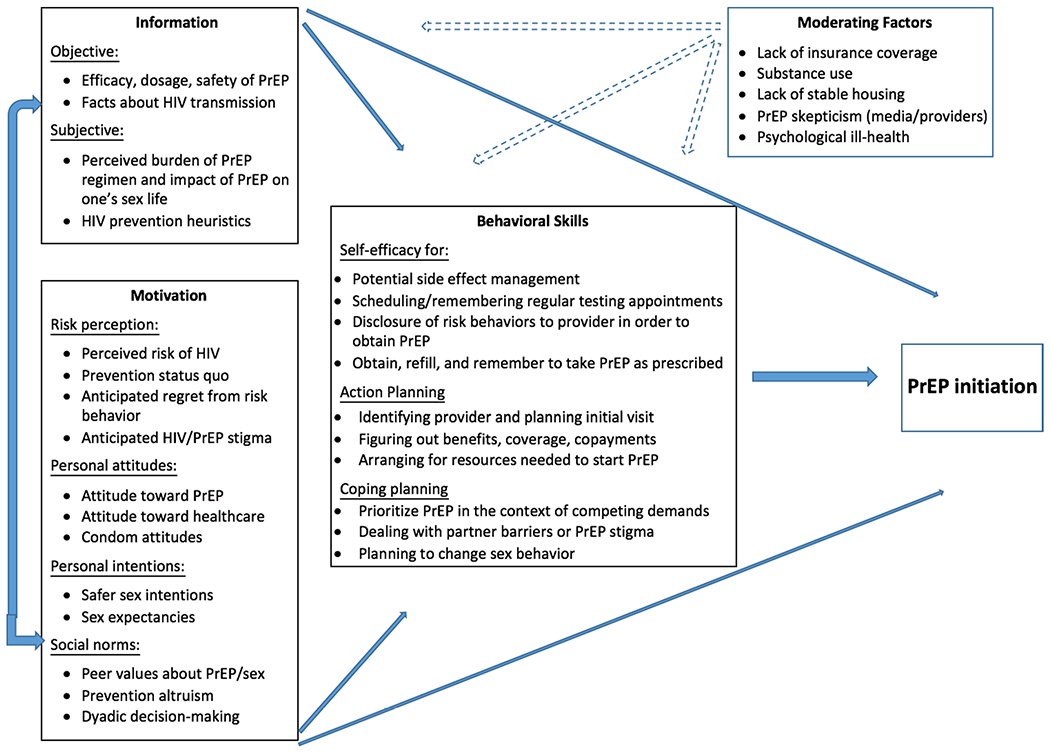
Information–motivation–behavioral skills model of PrEP uptake
Legend: dotted arrows show a potential influence
This situated IMB model of PrEP uptake is a mediational model and follows previous IMB models [32] where PrEP information and motivation work through, and are generally limited by, an individual’s level of PrEP related behavioral skills to influence individual willingness to start PrEP regimen. In other words, a well-informed or highly motivated gay man may still have issues with starting PrEP regimen if he lacks the skills needed to acquire PrEP. The IMB model also specifies that in certain cases prevention information and motivation may have direct effect on preventive behavior in cases when development of novel skills is not necessary (for instance, a frequent post-exposure prophylaxis PEP user switching to PrEP). Given the fact that the skills needed for PrEP uptake are novel and complex (e.g. finding a provider, figuring out insurance benefits), it is likely to assume that behavioral skills will mediate the relations between information and motivation and PrEP uptake, and the direct paths from information and motivation to PrEP uptake will be negligible.
The literature on barriers to PrEP uptake and PrEP disengagement may provide some support for mediation effect of behavioral skills on the relationships between model constructs (information and motivation) and PrEP uptake. Aside from changes in perceived sexual risk (motivational construct), many studies [33–35] point out to lack of behavioral skills as the main reason why men refuse to start or quit PrEP regimen. One major barrier to PrEP uptake is cost related to health insurance [36], prescription copay [37], and costs of quarterly STI and HIV testing [38]. Inability to navigate cost-related issues prevents patients who are interested in PrEP from taking it [39, 40]. Inability to manage side effects (lack of behavioral skills) may deter informed and motivated men from engaging in PrEP [41–43]. Finally, perceived inability to take a pill daily (lack of behavioral skills) will result in low uptake of PrEP among informed and motivated patients [44, 45].
In addition to describing effects of PrEP related information, motivation, and behavioral skills on PrEP uptake, the adapted IMB model recognizes that certain factors may moderate the relationships between constructs of this model. We are only beginning to learn about these moderating factors from PrEP demonstration projects describing real-world uptake [26]. Most of what was previously known about PrEP uptake comes from randomized controlled studies where PrEP is offered in a supportive setting by a sensitive provider at no cost, regardless of an individual’s insurance coverage. This setting is void of many environmental factors that may directly or indirectly affect PrEP uptake such as lack of insurance coverage [46], substance use [47], lack of stable housing [48], PrEP skepticism in media or among providers [49], and depression [50].
The following sections describe the three major constructs of the IMB model adapted for PrEP uptake, a number of subdomains related to each construct, and moderating factors. The paper will describe ways in which this adapted IMB model may assist in understanding of PrEP uptake by highlighting determinants of PrEP uptake, as well as their interconnectedness, and the potential it has to inform future PrEP implementation studies and interventions.
PrEP Information and PrEP Uptake
According to reports from the first PrEP demonstration projects, sufficient knowledge about PrEP is critical to enable successful PrEP implementation [51]. However, the research consistently shows that populations most at risk are usually the least likely to be aware of or to access new innovations in healthcare, be they diagnostic, preventative, or therapeutic [52]. Therefore, it is important to identify the optimal methods for providing PrEP information and adequately reaching at-risk population who could benefit from PrEP. The mere provision of information about PrEP efficacy and ways of accessing it may not be enough to influence PrEP uptake [53]. Janis [54] has argued that a major limitation of many theoretical frameworks of preventive behavior is the assumption that health-relevant information is appraised and acted on in a rational manner. From this perspective, when an individual is appraising a situation in a heuristic/subjective/irrational manner, conventional definitions of rational health beliefs and information are not likely to predict preventive behavior. Christensen et al. [55] have developed Irrational Health Belief scale that included a number of items that can be applied in the context of PrEP. Therefore, we believe that successful PrEP outreach should include provision of not only objective information (i.e. efficacy, dosage, side effects, safety of PrEP), but also assessment of subjective information (perceived burden of PrEP regimen, efficacy, toxicity and impact of PrEP on one’s sex life), and HIV prevention information (objective facts about HIV transmission and subjective HIV prevention heuristics).
PrEP is a novel biomedical HIV prevention method. It is still in early stages of implementation and public knowledge about it is inadequate. Accurate information about PrEP is essential to promote uptake. Factual or objective information includes knowledge about PrEP, its effectiveness, potential side effects, role of adherence in achieving effectiveness, where to find a PrEP-friendly provider, what to expect from the initial PrEP visit to a provider, and how to fund PrEP regimen. The adapted IMB model implies that while accurate information about PrEP may facilitate uptake, PrEP misinformation may represent a significant barrier to PrEP uptake. Examples of being misinformed include having beliefs that other forms of prevention will no longer be needed, misinformation about severity and frequency of occurrence of side effects, or the belief that use of PrEP is not warranted for monogamous couples (Table 1).
Table 1.
Information, motivation, behavioral skills correlates of PrEP uptake
| Study | Sample | Findings |
|---|---|---|
| PrEP information and PrEP Uptake | ||
| Objective information | ||
| Borges et al. [92] | Patients at two NYC public STD clinics (N = 389) | Limited prior knowledge of PrEP, indicating an opportunity to provide information to those at high risk of HIV |
| Dolezal et al. [36] | MSM recruited in Boston, Pittsburgh, and San Juan (N = 228) | Very limited awareness of PrEP, public education is needed to raise awareness |
| Hood et al. [23] | MSM who reside in Washington State (N = 2168) | PrEP awareness is high among high risk MSM due to implementation of a state wide PrEP program |
| Mantell et al. [93] | MSM participating in Gay Pride events in NYC (N = 480) | Limited awareness and knowledge of PrEP |
| Bauermeister et al. [52] | Convenience online sample of young MSM (18–24 years old) (N = 1507) | Very low knowledge of PrEP among respondents |
| Mayer et al. [94] | two groups MSM members of a sexual networking site (N = 6683 and 4759) | Very low levels of knowledge about PrEP among both groups |
| Eaton et al. [41] | African American MSM in Atlanta (N = 436) | PrEP awareness and intention correlates with HIV awareness |
| Garnett et al. [95] | 1673 substance-using black men who have sex with men and transgender women in NYC | Awareness of PrEP was reported among 18.2% of participants, need for targeted dissemination of PrEP information to key populations to increase awareness and ultimately improve uptake of PrEP |
| Subjective information | ||
| Galindo et al. [24] | MSM and trans women in three CA metropolitan areas (N = 30) | Lack of trust in one’s own abilities to fit PrEP into medical routine and anticipating changes in one’s sexual behavior as potential deterrents for PrEP use |
| Saberi et al. [26] | San Francisco bay area MSM (164 couples) (N = 328) | Expectation that PrEP will affect sex decision-making by reducing worries about HIV infection, complacency in talking to partners about HIV risks, less condom use |
| Gamarel and Golub [39] | MSM recruited in NYC (N = 164) | Desire for more intimacy in sex is a motivator to use PrEP |
| PrEP motivation and PrEP uptake | ||
| Perceived risk of HIV | ||
| Parsons et al. [96] | National US sample of 1071 MSM (N = 1071) | Willingness to take PrEP is highest among men who perceive themselves being at risk for HIV |
| Cohen et al. [21] | 557 MSM enrolled in open label PrEP study in Miami, San Francisco, Washington DC (N = 557) | PrEP uptake by study participants correlates with self-perceived risk of HIV |
| Krakower et al. [97] | 398 MSM surveyed before iPrEX results were published and 4558 MSM surveyed post iPrEX recruited online (N = 4956) | PrEP interest was associated with perceiving oneself at increased risk for HIV acquisition |
| Zarwell et al. [98] | 564 MSM in New Orleans (N = 564) | The most commonly cited reason for not taking PrEP was not feeling at risk for HIV |
| Uthappa et al. [99] | 400 MSM and TGs (N = 400) | Having a high self-perceived risk of HIV was one of the strongest facilitators of PrEP acceptance |
| Anticipated regret | ||
| Elsesser et al. [48] | Members of an internet-based MSM sexual networking site (N = 7305) | Intent to take PrEP correlates with periods of anticipated increased risk/anticipated regret |
| Status quo | ||
| Kwakwa et al. [47] | 5606 patients undergoing HIV rapid testing in Philadelphia (N = 5606) | The main reason for openness to PrEP among respondents was their desire to increase the level of personal protection from HIV (change status quo) |
| Anticipated HIV/PrEP stigma | ||
| Oldenburg et al. [49] | 4098 HIV-uninfected MSM members of sexual networking site (N = 4098) | MSM living in more stigmatizing environments had decreased use of antiretroviral-based HIV-prevention strategies |
| Liu et al. [11] | 261 patients in San Francisco City Clinic, 123 patients enrolled in Kaiser Permanente Health Plan, and 15 patients from Bay Area Perinatal AIDS Center (N = 399) | PrEP stigma can pose a barrier to uptake and retention in PrEP programs |
| Biello et al. [57] | 237 HIV-uninfected, PrEP-naive MSM reporting concurrent substance dependence and sexual risk (N = 237) | Anticipated stigma from primary and casual partners represent barriers to PrEP use |
| Oldenburg et al. [67] | 254 MSM respondents who reported recent condomless sex in the context of concurrent stimulant use (N = 254) | HIV stigma is a barrier to PrEP uptake |
| Golub et al. [100] | A New York City sample of 160 MSM (N = 160) | Negative stereotypes about PrEP users were identified by 80% of participants. PrEP-related stereotypes might impact willingness to discuss PrEP. |
| Attitudes toward PrEP | ||
| Bauermeister et al. [52] | Young MSM (18-24 years old) (N = 1507) | Perceived difficulties in accessing PrEP and managing side-effects as the reason to decline PrEP |
| Stein et al. [65] | Opiate injectors entering detoxification treatment (N = 351) | Perceived burden of PrEP regimen is a deterrent for PrEP uptake |
| King et al. [29] | High risk MSM (N = 451) | Concerns about taking a daily medication and potential long-term side effects as reasons for declining PrEP |
| Attitudes towards healthcare | ||
| Underhill et all [25] | 31 MSM sex workers, 25 MSM who were not (N = 56) | PrEP requires individuals to disclose risk behavior to clinicians, but medical mistrust may limit disclosure |
| Taylor et al. [63] | PrEP focus groups with MSM (N = 39) | Barrier for PrEP: apprehension discussing risky sexual behaviors and PrEP use with health care providers |
| Kwakwa et al. [47] | 5606 patients undergoing HIV rapid testing in Philadelphia (N = 5606) | Mistrust in healthcare establishment (especially among African American respondents) as the reason for declining PrEP |
| Holloway et al. [101] | 687 YMSM recruited via social networks in California (N = 687) | Medical mistrust together with concerns about drug effects and adherence significantly decrease PrEP willingness among YMSM |
| Condom attitudes | ||
| Hoff et al. 54] | San Francisco bay and New York city couples (N = 458) | Condom fatigue is the predictor of intention to use PrEP |
| Brooks et al. [28] | 25 serodiscordant MSM couples in LA area (N = 50) | PrEP is likely to be adopted when viewed as the opportunity to engage in sex using a noncondom HIV prevention method. Negative condom attitudes correlate with intention to use PrEP |
| Grov et al. [102] | 158 highly sexually active HIV-negative GBM in New York City (N = 156) | Men who engaged in condomless anal intercourse were interested in PrEP |
| Sex expectancies | ||
| Gamarel and Golub [39] | MSM recruited in NYC (N = 164) | Intimacy motivations, expectations of more closeness during sex may play a central role in PrEP adoption |
| Oldenburg et al. [67] | 254 MSM respondents in Boston who reported recent condomless sex in the context of concurrent stimulant use (N = 254) | Expectations of a worry-free sex as a motivator to start PrEP |
| Social norms | ||
| Zarwell et al. [70] | 564 MSM in New Orleans (N = 564) | Few participants knew anyone in their social or sexual network who took PrEP, citing this as the reason for unwillingness to consider PrEP |
| Mantell et al. [74] | MSM participating in Gay Pride events in NYC (N = 480) | Men who believed that some of their friends would use PrEP were interested in using it themselves |
| Kuhns et al. [103] | 394 YMSM recruited in Chicago and Houston (N = 394) | YMSM peer network size is related to PrEP uptake, suggesting that having a larger number of YMSM within one’s social network is associated with PrEP use |
| Young et al. [104] | 423 young black MSM recruited in Chicago (N = 423) | Interventions that leverage peer influence processes to facilitate PrEP uptake are promising strategies to improve sexual health engagement and overcome disparities in outcomes among this at-risk population |
| Dyadic decision-making | ||
| Saberi et al. [26] | 164 MSM couples in San Francisco (N = 328) | Importance of negotiation of sexual safety among partners |
| Brooks [28] | 25 serodiscordant MSM couples in LA area (N = 50) | Relationship dynamics may influence PrEP use and adherence |
| Mitchell et al. [105] | 29 MSM couples in Atlanta and Detroit (N = 58) | Importance of sexual agreement and negotiation of PrEP use with the partner |
| Prevention ALTRUISM | ||
| Hoff et al. [54] | San Francisco bay and New York city couples (N = 458) | Desire to protect their partners as motivator to engage in PrEP |
| Gamarel [66] | 60 NYC MSM in romantic relationships (N = 60) | Top sex goals were to protect themselves and their partners and to have responsible sex |
| Behavioral skills | ||
| Taylor et al. [63] | PrEP focus groups with MSM (N = 39) | Participants described strategies that will help them adhere to PrEP regimen – anticipating changes in schedule, daily rituals, external reminders, and anticipating changes in sexual decision-making |
| Golub et al. [40] | MSM and transgender women in NYC (N = 184) | Self-efficacy for navigating condom use in the context of PrEP, for ability to discuss PrEP with a provider, and for taking daily pill/managing potential side effects are predictors of PrEP use |
| Brooks et al. [44] | low socioeconomic status BMSM residing in LA (N = 224) | PrEP adoption intention correlates with self-efficacy for obtaining/filling prescription and managing potential side effects |
| Stack et al. [106] | MSM recruited online (N = 3217) | Preferences for different PrEP regimens are associated with the sexual frequency and planning behaviors of potential users |
| Galindo et al. [24] | MSM and trans women in three CA metropolitan areas (N = 30) | Those who expressed interest in PrEP thought they are able to fit PrEP into their daily routine and able to deal with side-effects. Less interested in PrEP participants thought they will not be able to budget for PrEP and once-a-day regimen did not seem realistic for them |
| John et al. [107] | Nationwide sample of 906 HIV-negative, PrEP-naïve GBM | The majority of participants would prefer using home based PrEP instead of obtaining PrEP from a provider |
For this table we searched for studies taking place in the US and followed FDA approval of PrEP (2012—onward)
Subjective information refers to PrEP related beliefs. This assessment comprises both medical and psychological benefits of PrEP such as expecting to feel safe during sex, ability to have control over one’s own protection, having more closeness or intimacy during sex [56]. Subjective knowledge is the extent to which men who have sex with men perceive that they know about PrEP and the various costs associated with being on PrEP. Previous research shows that preventive behavior is influenced by patients’ feeling of competence and, therefore, perceived familiarity with what it takes to be on PrEP may positively influence PrEP uptake [57].
In addition to PrEP related knowledge (both objective and subjective), individuals also need to be adequately informed about HIV transmission and prevention to ensure adequate uptake of PrEP. Objective knowledge about HIV incidence, prevalence and acquisition (for example, “sexually active gay men are at high risk of HIV acquisition”), as well as facts relevant to HIV prevention (for example “frequent HIV testing is an important form of HIV prevention”) are moderators for PrEP uptake [35]. Knowledge about HIV prevention modalities is important because use of PrEP presumes knowledge and use of some prevention strategies (routine HIV testing) and it may influence practice of previously adapted modalities (i.e. seropositioning) [58]. Furthermore, in their assessment of HIV risks people often rely on HIV heuristics or rules of thumb. HIV prevention heuristics are simple decision rules which reduce cognitive load from decisions about use of prevention but may often lead to incorrect decisions [59] (for example “monogamous sex is safe sex” or “known partners are safe partners”). Reliance on HIV heuristics may play a detrimental role in PrEP uptake.
The relationship between PrEP knowledge and PrEP intentions was documented in several empirical studies. Most of the studies conducted in 2013–2016 among large samples of US MSM have consistently shown low levels of knowledge about PrEP among MSM. Studies estimate awareness about PrEP in MSM communities range from 23 [41] to 58% [23] (2015 sample of 228 MSM in Pittsburgh—21%, Boston 36%, San Juan 19%; [36] 2016 sample of 2168 MSM in Washington state—58% (and 86% among high risk MSM); [23] 2015 sample of 436 African American MSM 23%; [41] 2013 online sample of young MSM 27%; [52] 480 MSM participating in 2014 NYC pride—38%; [74] MSM recruited from a sexual networking site—in 2013 PrEP awareness 38%, 4759 in 2014 PrEP awareness 49% [75]). The relatively high level of awareness in Washington state can be explained by implementation of a state wide PrEP program. Additionally, there are studies that discuss not only objective, but also subjective knowledge about PrEP. For instance, a study of San Francisco bay area MSM couples (N = 164) [26] highlighted subjects’ perception that PrEP use will affect their sexual decision-making by reducing worries about HIV infection, complacency in talking to partners about HIV risks, and may result in less condom use. Similarly, Gamarel and Golub [39] show that subjective knowledge about use of PrEP resulting in more intimacy during sex may lead to PrEP intentions.
PrEP Motivation and PrEP Uptake
Motivation is a very important construct of the IMB model. It is generally described as the internal force that determines the direction and intensity of efforts to change behavior. In the context of PrEP, motivation results from perceived risk of contracting HIV and the perceived impact of having HIV on one’s quality of life. For an individual to be motivated to take PrEP, his perceived risk of HIV should outweigh the rewards associated with engaging in risky behaviors. Motivation is also determined by several other components such as personal intentions, personal attitudes, and social norms. Personal intentions capture the motivational forces that influence a protective behavior or how hard people are willing to try to achieve the desired level of HIV protection independent of perceived risk [60]. Personal attitudes refer to one’s affective response to the idea of performing the protective behavior as well as individual beliefs about positive or negative consequences resulting from the behavior [61]. Finally, social norms describe the perception of what others do and the importance of others’ approval. Sexual behavior is interactive at its core and, therefore, perceptions of what peers are doing and of potential (or actual) partners’ attitudes are important predictors of HIV protective behavior and PrEP uptake [62].
The risk perception subdomain of PrEP motivation is comprised of perceived risk for HIV, prevention status quo, anticipated regret from HIV risk behavior and anticipated stigma related to both HIV and use of PrEP. Perceived risk for acquiring a disease is an important motivating factor leading individuals to seek diagnostic testing and other preventive services. In the case of men who have sex with men, a lack of perceived risk for acquiring HIV may result in missed opportunities to use PrEP for prevention. For instance, in the recent study of PrEP uptake among men who have sex with men, the investigators found that 80% of 505 participants were candidates for PrEP based on their HIV risk profiles. However, from this group of candidates, 78% of men did not consider themselves at great enough risk to qualify for PrEP [63]. Similarly, individuals are motivated to engage in preventive behavior when they are less satisfied with their prevention status quo or the current state of affairs. The more an individual is satisfied with the current level of HIV protection, the less he would want to initiate PrEP [64]. Anticipated regret is a negative, cognitive-based emotion that is experienced when we realize or imagine that the present situation could have been better had we acted differently. Anticipated regret from engaging in HV risk behavior is an important determinant of attitudes and intentions to start PrEP [65]. Finally, it has been demonstrated that anticipated HIV stigma—the expectation of rejection or discrimination against by others in the event of seroconversion—has a strong negative influence on motivation to undergo regular HIV testing. It is assumed that it may have a similar impact on the motivation to start a PrEP regimen [66]. PrEP-related stigma and shaming are also potential barriers to PrEP implementation. One demonstration project of 261 men who have sex with men in San Francisco reported that PrEP stigma poses a barrier to uptake and retention in PrEP program. The study concluded with a call for interventions aiming to combat PREP-related stigma [11]. Golub et al. identified two types of PrEP-related stereotypes that were reported in 80% of 160 qualitative interviews of men who have sex with men in New York City. One stereotype was the assumption that PrEP users are actually HIV-infected and lying about it, while another is that PrEP users are highly promiscuous and resistant to condom use [67].
Personal attitudes towards initiating PrEP regimen are based upon the individual’s beliefs (i.e. subjective knowledge) about the outcomes of PrEP and evaluations of those outcomes. For instance, if an individual believes that PrEP is unsafe or has many negative side effects, and evaluates these consequences as negative, he may have negative attitudes toward PrEP use [68]. Attitudes toward healthcare can be another predictor of PrEP use. As PrEP signifies a shift from behavioral to medicalized prevention methods, medical mistrust may contribute to slow uptake especially among minority groups [69]. The initial data from PrEP demonstration studies among men who have sex with men show that men who choose to take PrEP tend to be those who report episodes of unprotected anal intercourse. Therefore, negative condom attitudes may be correlated with intention to take PrEP [70]. Additionally, PrEP users have reported that PrEP enhances sexual pleasure, and that this is an important motivator for using PrEP. PrEP reduces worries about contracting HIV and increases intimacy, spontaneity, and adventure as a part of sexual experience. These sex expectancies can be another powerful motivator to start PrEP [56]. Finally, a body of research on preventive behaviors among men who have sex with men suggests that adoption of prevention strategies is strongly associated with prior intentions to practice safer sex. In this model, safer sex intentions are linked with motivation to engage in PrEP [70].
Social norms for PrEP uptake involve perceptions of others’ opinions about PrEP and willingness to comply with other’s wishes. For example, if one believes that his partner or friends would like him to use PrEP, then social norms for PrEP may be high. Endorsement of PrEP by one’s partner can be a significant motivator for PrEP [71], thus highlighting the importance of dyadic decision-making about PrEP. Dyadic decision-making is also important because one-third of HIV infections among men who have sex with men occurs within primary partnerships [72], pointing to the need of studying PrEP motivation in light of partnership dynamics. This need is supported by Gamarel and Golub in their study of dyadic decision making and use of PrEP which concludes as follows: “Intimacy motivations may play a central role in PrEP adoption for MSM couples. Incorporating relationship dynamics into biomedical strategies is a promising avenue for research and intervention” [56]. Furthermore, one’s motivation to reduce personal risk of HIV stems not only from self-interest but also from concern for others. Prevention altruism, defined by Nimmons [73] as “the values, motivations, and practices of caretaking in one’s sexual behavior, which arise out of a concern for others,” can be a useful predictor of one’s motivation to start PrEP. An emerging body of literature on predictors of PrEP uptake is consistent with this adapted IMB model’s assertion that perceived risk of acquiring HIV; personal attitudes about PrEP, healthcare, and condoms; individual intention to practice safer sex; and social motivation are extremely relevant to PrEP uptake.
There is a growing body of literature on motivations to use PrEP. A number of studies have shown that perceived risk of HIV correlates with PrEP intention. For instance, in the national US sample of 1071 MSM [27], willingness to take PrEP was highest among MSM who perceive themselves being at risk for HIV. Similarly, in a 2015 study of 564 MSM in New Orleans [77], the most commonly cited reason for not taking PrEP was not feeling at risk for HIV. Elsesser et al. [48] found from their study of 7305 MSM that intent to take PrEP correlates with periods of increased risk and anticipated regret from risk activities. Kwakwa et al. [47] in their study of 5606 MSM undergoing rapid testing in Philadelphia found that the main driver for PrEP intent was respondents’ desire to change their status quo when it comes to personal protection from HIV. Anticipated HIV and PrEP stigma have influence on PrEP intentions. Oldenburg et al. [49, 67] conclude both of their studies with the suggestion that HIV stigma may represent a significant barrier to PrEP uptake. Biello et al. [57] and Liu et al. [11] found that PrEP stigma can pose a barrier to uptake and retention in PrEP programs.
Several studies point to the fact that PrEP attitudes and perceived difficulties in accessing PrEP and managing potential side-effects are reasons for declining PrEP in several large nationwide samples [29, 65]. Two additional sets of attitudes—towards healthcare and condom use—shown to be important in forming PrEP intentions. PrEP initiation requires individuals to disclose risk behavior to clinicians, but medical mistrust may limit disclosure, according to studies conducted by Underhill et al. [25] and Taylor et al. [63]. Two studies by Hoff et al. [54] and Brooks et al. [28] mention condom fatigue as the predictor of intention to use PrEP. Additionally, two 2015 studies of 16 [9, 43] and 254 MSM [67] suggest that expectations of a worry-free sex (sex expectancies) and more intimacy during sex may serve as motivators to start PrEP. Studies in New Orleans (N = 564) [70] and New York (N = 480) [74] concluded that social norms drive PrEP intentions. Men who believed that some of their friends use PrEP were interested in using it themselves. While peer influence is important, the desire to protect one’s partner (prevention altruism) and ability to negotiate PrEP with one’s partner (dyadic decision-making) influence PrEP intentions. Several qualitative studies in LA [28] and Atlanta [78] highlight the importance of sexual agreement and negotiation of PrEP use with the partner. Two studies in New York [66] and San Francisco [54] report that aside from personal protection, desire to protect partners is a motivator to engage in PrEP.
PrEP Behavioral Skills and PrEP Uptake
The behavioral skills component deals with the ease or difficulty of engaging in PrEP regimen and with people’s confidence that they can obtain/fill their prescription and sustain PrEP use. This component of the IMB model adapted for PrEP uptake consists of an individual’s objective abilities as well as his or her self-efficacy concerning a number of behaviors needed to initiate PrEP use. Ajzen suggests that self-efficacy or behavioral skills “involve people’s beliefs that they have control over the behavior, that performance or non-performance of the behavior is up to them” [74]. In other words, behavioral skills determine the extent to which knowledgeable and motivated individuals are able to initiate PrEP regimen. Bandura, who first introduced the concept of self-efficacy, suggested that self-efficacy is a self-regulating cognition that determine whether behaviors will be initiated, how much effort will be expended, and how long it will be sustained in the face of obstacles [75]. Therefore, behavioral skills and self-efficacy beliefs have a direct impact upon PrEP uptake. The direct link is explained by the fact that positive self-beliefs predict actual behavior.
The situated application of the IMB model asserts that PrEP related knowledge and motivation to take PrEP work through behavioral skills to influence PrEP uptake. Essentially, the effects of PrEP knowledge and motivation to take PrEP are expressed through the application of behavioral skills (obtaining or filling the prescription for PrEP, sustaining PrEP use) to initiate PrEP. The behavioral skills involved in PrEP use include objective and perceived ability to discuss PrEP use with a provider [27]; to obtain, refill, and remember to take PrEP as prescribed [76]; budget for PrEP [77]; avoid or manage potential side effects [78]; use PrEP discreetly or to negotiate its use with sexual partners [79]; and overcome potential challenges such as PrEP related stigma [11], and other barriers to PrEP uptake. A number of studies of PrEP acceptability and PrEP uptake describe lack of these self-efficacy beliefs as a major detriment to PrEP uptake among at-risk populations. For instance, concerns about side-effects and perceived inability to manage these side-effects in case of their occurrence was a significant barrier to PrEP uptake in PrEP demonstration projects and delivery programs rolled out in San Francisco [11]. Perceived inability to negotiate PrEP use with a partner may also undermine one’s decision to start PrEP ((“I will not take PrEP because my partner will think I am cheating on him”) [80]. Furthermore, a number of PrEP implementation studies report that those who refused to take PrEP were questioning their ability to take a daily medication for an extended period of time (“I am not a pill-taker kind” belief) [81].
Most theories of human behavior (including the IMB model) focus on the antecedents of intention assuming that intention itself is the closest predictor of behavior. This assumption was recently challenged by researchers, suggesting the need for additional constructs to mediate the intention-behavior gap. For instance, a meta-analysis of meta-analyses [82] indicated that intentions explain 28% of the variance on average in future behavior. This measurement demonstrates the extent of the ‘gap’ between behavior and intentions. Although people may develop an intention to start PrEP regimen, they might not take any action. Translating an intention into behavior requires self-regulative strategies that entail both cognitive and enactive acts, strategies that are called action planning. Action planning is an effective way of bridging the intention-behavior gap. Therefore, the adapted IMB model includes two planning constructs that are not a part of the original IMB model—action planning and coping planning—to bridge the gap between behavioral intentions and health behavior. Action planning is described as a process of linking goal-directed behaviors to certain environmental cues by specifying when, where, and how to act [83]. Intentions are precursors of action planning. In the context of PrEP, action planning may include outlining specific plans to schedule an initial visit with a provider, to sustain use of PrEP, and to engage support from a partner. Coping planning is a barrier-focused self-regulation strategy. It represents a mental link between anticipated risk situations and suitable coping responses [84]. For example, ‘When I start taking PrEP and my partner will dislike it, I will find ways to use PrEP covertly.’
Several studies highlight the importance of behavioral skills in forming PrEP intentions. These studies [44, 63] demonstrate PrEP adoption intention correlates with self-efficacy for obtaining/filling prescription and managing potential side effects. Stack et al. [79] in their 2016 study of 3217 MSM recruited online found that PrEP preferences are associated with the sexual frequency and planning behavior of potential users. Golub et al. [40] report a number of behavioral skills that predict PrEP intentions such as self-efficacy for navigating condom use in the context of PrEP, ability to discuss PrEP with a provider, and ability to take daily pill/manage potential side effects.
Moderating Factors
In addition to describing the influence of PrEP related information, motivation, and behavioral skills on PrEP uptake, the adapted IMB model outlines a number of contextual factors that may moderate the outcome either indirectly, via their impact on IMB model constructs, or directly, via unmediated impact on PrEP uptake. The example of the former would be lack of insurance coverage or high out-of-pocket prices for PrEP that may impact one’s personal attitudes (considering PrEP unattainable) and behavioral skills (needing skills to secure funding for PrEP). Similarly, inadequate access to healthcare may result in medical mistrust and require additional skills needed to find a PrEP-friendly provider. On the other hand, some contextual factors such as chemical dependency, psychological ill-health, poverty, and unstable living situation may directly affect PrEP uptake. For instance, in the study of 132 stimulant-using men who have sex with men, more than half of respondents (62%) agreed that their substance use would affect their ability to take PrEP as prescribed [85]. In a study of 1507 young men who have sex with men, 53% of respondents reported that they would not be able to afford PrEP if they did not have insurance [77]. When not addressed, these factors may also moderate knowledge, motivation, and behavioral skills to start and sustain PrEP. For example, men who have sex with men who engaged in sex work report more medical mistrust and healthcare discrimination due to issues beyond men who have sex with men behavior or identity (homelessness, substance use, poverty). Medical mistrust and perceived discrimination create barriers for sexual behavior disclosure to clinicians, potentially impeding access to PrEP [27].
This situated IMB model of PrEP uptake recognizes that PrEP initiation is tied to the social, cultural, and cognitive-affective context in which potential PrEP users finds themselves. The IMB model, developed by Fisher and Fisher in 1992 [86], has been since adapted to various populations with specific content being added to each core construct in order to reflect the uniqueness of the population and context. Similarly, Amico has developed a situated IMB model of care initiation and maintenance [87], in which she underlined the importance of a situated approach. As a result of adopting a similar situated approach to this IMB model of PrEP uptake, we added a number of constructs that may not be common among IMB models but reflect the context in which MSM make decisions about PrEP initiation. The domain of information included knowledge about HIV prevention modalities and subjective information or perceived familiarity with what it takes to be on PrEP. The domain of motivation included prevention altruism or adoption of prevention practices out of concerns for others and anticipated regret from engaging in HIV risky behavior. The domain of behavioral skills included action planning and coping planning constructs to mediate for intention-behavior gap.
IMB Approach to PrEP Promotion
Despite evidence that PrEP is effective, a review of the recent HIV prevention intervention advances demonstrated a number of issues that significantly restrict the impact of PrEP programs. Most interventions are designed intuitively and they fail to engage conceptual frameworks for HIV risk behavior change (such as the adaptation of the IMB model proposed here) [88]. In addition, few interventions have systematically assessed subjects’ pre-existing HIV knowledge, HIV risk reduction motivation, and their behavioral skills with respect to HIV prevention, in order to design the program according to pre-existing or future needs [89]. Furthermore, programs often fail to motivate their clients to modify risky behaviors or help them acquire and retain the knowledge and skills necessary for sustained change [90]. Finally, most of these interventions have not been rigorously evaluated [91]. The limitations described above can be addressed by grounding interventions in a theoretical approach to individual-level behavioral change such as the adapted IMB model proposed in this article. While IMB model-based research has been successfully applied to a number public health initiatives, including promotion of safer sex practices among diverse population, it has not been applied in intervention efforts to promote PrEP uptake.
Based on results of this study, it is possible to conclude that future interventions to increase PrEP uptake may be most effective if intervention components target: (1) PrEP-related information (e.g., knowledge about PrEP effectiveness, side effects, adherence, perceived affordability, and risk compensation). This can be achieved through education campaigns, advertisements in key areas/clubs/magazines visited by men who have sex with men, social media, and informational websites (2) personal motivation (e.g., sexual expectancies, acceptability, anticipated HIV stigma, safer sex intentions, perceived and controlled risk of HIV) and social motivation (e.g., prevention altruism, peer values and medication use, peer sex norms, dyadic decision making). This can be achieved through motivational interviews with providers, addressing potential PrEP stigma, and using gay social mobile apps to promote PrEP use at a communal level. (3) The development of practical behavioral skills in adhering to PrEP, managing side effects, negotiating PrEP use, sustaining motivation, and safer sex practices in the context of PrEP. We believe this adaptation of the IMB model may provide a broad conceptual and practical approach to PrEP promotion interventions intended to strengthen the information, motivation and behavioral skills determinants, as well as to circumvent information, motivation, and behavioral skills barriers to PrEP uptake.
This study has a number of limitations. There is a need for multivariate correlational evidence in order to support the assumption of this adaptation of the IMB model. This research may include evaluation of the IMB constructs and their influence on initiation of PrEP. Empirical research is also needed to determine whether the targeted intervention developed based on this adaptation of the IMB model have intended effects on PrEP related information, motivation, and behavioral skills. There are potential relationships between information and motivation constructs as well as between motivation and behavioral skills constructs that may need to be further delineated and explored. The model implies that well-informed people are not always well-motivated and vice versa meaning these constructs may or may not be independent. Additionally, behavioral skills may influence motivation because people are usually motivated to engage in behaviors they perceive to be within their control.
Funding
Financial support for this study was provided in part by the National Institute on Drug Abuse (K24 DA017072, Altice) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (AR060231-05, Fraenkel). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Conflict of interest Alex Dubov, Frederick Altice and Liana Fraenkel declares that they have no conflict of interest.
Ethical Approval This article does not contain any studies with human participants performed by any of the authors.
References
- 1.Grant RM, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baeten JM, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thigpen MC, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. [DOI] [PubMed] [Google Scholar]
- 4.Choopanya K, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90. [DOI] [PubMed] [Google Scholar]
- 5.Fonner VA, Dalglish SL, Kennedy CE, et al. Effectiveness and safety of oral HIV pre-exposure prophylaxis (PrEP) for all populations: a systematic review and meta-analysis. AIDS. 1973;2016:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmes D. FDA paves the way for pre-exposure HIV prophylaxis. Lancet. 2012;380(9839):325. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Guidance on oral pre-exposure prophylaxis (PrEP) for serodiscordant couples, men and transgender women who have sex with men at high risk of HIV: recommendations for use in the context of demonstration projects, July 2012. Geneva: World Health Organization; 2012. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States-2014: a clinical practice guideline. Atlanta: Centers for Disease Control and Prevention; 2014. p. 67. [Google Scholar]
- 9.Bush S, et al. Significant uptake of Truvada for pre-exposure prophylaxis (PrEP) utilization in the US in late 2014–1Q 2015. IAPAC Treatment, Prevention, and Adherence Conference. 2015. [Google Scholar]
- 10.Edelstein Z, Newton-Dame R, Myers J, Jacobson L. Pre-exposure prophylaxis (PrEP) in ambulatory care clinics, New York City, 2012–2014. International Association of Physicians in AIDS Care Conference 2015. [Google Scholar]
- 11.Liu A, et al. Early experiences implementing pre-exposure prophylaxis (PrEP) for HIV prevention in San Francisco. PLoS Med. 2014;11(3):e1001613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volk JE, et al. No new HIV infections with increasing use of HIV preexposure prophylaxis in a clinical practice setting. Clin Infect Dis. 2015;61(10):1601–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith DK, et al. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition-United States, 2015. Morb Mortal Wkly Rep. 2015;64(46):1291–5. [DOI] [PubMed] [Google Scholar]
- 14.Bush S, Magnuson D, Rawlings MK, et al. Racial characteristics of FTC/TDF for pre-exposure prophylaxis users in the U.S Paper presented at: 2016 ASM Microbe; June 16–20, 2016; Boston. Session 371. [Google Scholar]
- 15.Fisher J, Fisher W. Theoretical approaches to individual-level change in HIV risk behavior. In: DiClemente R, editor. Handbook of HIV Prevention. New York: Springer; 2000. p. 3–55. [Google Scholar]
- 16.Fisher JD, et al. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21(2):177. [PubMed] [Google Scholar]
- 17.Fisher JD, et al. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13(3):238. [DOI] [PubMed] [Google Scholar]
- 18.Fisher JD, et al. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996;15(2):114. [DOI] [PubMed] [Google Scholar]
- 19.Karim QA, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329(5996):1168–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kashuba ADM, et al. Pre-exposure prophylaxis for HIV prevention: how to predict success. Lancet. 2012;379(9835):2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grant RM, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;2010(363):2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rivet Amico K, et al. Adherence support approaches in biomedical HIV prevention trials: experiences, insights and future directions from four multisite prevention trials. AIDS Behav. 2013;17(6):2143–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shrestha R, et al. Willingness to use pre-exposure prophylaxis (PrEP): an empirical test of the information-motivation-behavioral skills (IMB) model among high-risk drug users in treatment. AIDS Behav. 2017;21(5):1299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fisher JD, Fisher WA. The information-motivation-behavioral skills model. Emerging theories in health promotion practice and research: strategies for improving public health. 2002;1:40–70. [Google Scholar]
- 25.Hood JE, et al. Dramatic increase in preexposure prophylaxis use among MSM in Washington state. AIDS. 2016;30(3):515–9. [DOI] [PubMed] [Google Scholar]
- 26.Cohen SE, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP Demonstration Project. J Acquir Immune Defic Syndr. 2015;68(4):439–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Underhill K, et al. A qualitative study of medical mistrust, perceived discrimination, and risk behavior disclosure to clinicians by US male sex workers and other men who have sex with men: implications for biomedical HIV prevention. J Urban Health. 2015;92(4):667–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saberi P, et al. Ambiguity, ambivalence, and apprehensions of taking HIV-1 pre-exposure prophylaxis among male couples in San Francisco: a mixed methods study. PLoS ONE. 2012;7(11):e50061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galindo GR, et al. Community member perspectives from transgender women and men who have sex with men on pre-exposure prophylaxis as an HIV prevention strategy: implications for implementation. Implement Sci. 2012;7(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brooks RA, et al. Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: a mixed methods study. AIDS Pat Care STDs. 2012;26(2):87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.King HL, et al. Pre-exposure prophylaxis accessibility research and evaluation (PrEPARE Study). AIDS Behav. 2014;18(9):1722–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fisher JD, Fisher WA. The information-motivation-behavioral skills model. Emerg Theor Health Promot Pract Res. 2002;1:40–70. [Google Scholar]
- 33.Kirby T, Thornber-Dunwell M. Uptake of PrEP for HIV slow among MSM. Lancet. 2014;383(9915):399–400. [DOI] [PubMed] [Google Scholar]
- 34.Mayer KH, Douglas SK. If PrEP decreases HIV transmission, what is impeding its uptake. Clin Infect Dis. 2015;61:1598Á600.26270688 [Google Scholar]
- 35.Eaton LA, et al. Minimal awareness and stalled uptake of preexposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Pat Care STDs. 2015;29(8):423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKenney J, et al. Optimal costs of HIV pre-exposure prophylaxis for men who have sex with men. PLoS ONE. 2017;12(6):e0178170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Doblecki-Lewis S, et al. Healthcare access and PrEP continuation in San Francisco and Miami after the US PrEP demo project. JAIDS J Acquir Immune Def Syndr. 2017;74(5):531–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parisi D, et al. A multicomponent approach to evaluating a pre-exposure prophylaxis (PrEP) implementation program in five agencies in New York. J Assoc Nurses AIDS Care. 2018;29(1):10–9. [DOI] [PubMed] [Google Scholar]
- 39.Chen A, Dowdy DW. Clinical effectiveness and cost-effectiveness of HIV pre-exposure prophylaxis in men who have sex with men: risk calculators for real-world decision-making. PLoS ONE. 2014;9(10):e108742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Arnold T, et al. Social, structural, behavioral and clinical factors influencing retention in Pre-Exposure Prophylaxis (PrEP) care in Mississippi. PLoS ONE. 2017;12(2):e0172354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whitfield THF, et al. Why i quit pre-exposure prophylaxis (PrEP)? A mixed-method study exploring reasons for PrEP discontinuation and potential re-initiation among gay and bisexual men. AIDS Behav. 2018. 10.1007/s10461-018-2045-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Glidden DV, et al. Symptoms, side effects and adherence in the iPrEx open-label extension. Clin Infect Dis. 2016;62(9):1172–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shrestha R, et al. Measuring acceptability and preferences for implementation of pre-exposure prophylaxis (PrEP) using conjoint analysis: an application to primary HIV prevention among high risk drug users. AIDS Behav. 2017. 10.1007/s10461-017-1851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kebaabetswe PM, et al. Factors associated with adherence and concordance between measurement strategies in an HIV daily oral tenofovir/emtricitibine as pre-exposure prophylaxis (Prep) clinical trial, Botswana, 2007–2010. AIDS Behav. 2015;19(5):758–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hacker E, et al. HIV Pre-Exposure Prophylaxis (PrEP) Uptake, Initiation, and Persistence in the Detroit Public Health STD Clinic. Open forum infectious diseases. vol. 4. No. suppl_1. US: Oxford University Press, 2017. [Google Scholar]
- 46.Ellorin E, et al. Barriers to Health Insurance Coverage and Intention to Continue Pre-exposure Prophylaxis (PrEP) Reported by Men Who Have Sex With Men (MSM) in a PrEP Demonstration Project. Open Forum Infectious Diseases. vol. 2. No. suppl 1. Oxford University Press, 2015. [Google Scholar]
- 47.Carlo Hojilla J, et al. Sexual behavior, risk compensation, and HIV prevention strategies among participants in the San Francisco PrEP demonstration project: a qualitative analysis of counseling notes. AIDS Behav. 2016;20(7):1461–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu AY, et al. Preexposure prophylaxis for HIV infection integrated with municipal-and community-based sexual health services. JAMA Intern Med. 2016;176(1):75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cáceres CF, et al. Implementation of pre-exposure prophylaxis for human immunodeficiency virus infection: progress and emerging issues in research and policy. J Int AIDS Soc. 2016;19:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tan DHS, et al. Self-administered screening for syndemic mental health problems should be routinely implemented among MSM PrEP users. J Gay Lesbian Mental Health. 2016;20(1):13–20. [Google Scholar]
- 51.Dolezal C, et al. Awareness of post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP) is low but interest is high among men engaging in condomless anal sex with men in Boston, Pittsburgh, and San Juan. AIDS Educ Prev. 2015;27(4):289–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oliva G, Rienks J, McDermid M. What high-risk women are telling us about access to primary and reproductive health care and HIV prevention services. AIDS Educ Prev. 1999;11(6):513. [PubMed] [Google Scholar]
- 53.Goedel WC, et al. Correlates of awareness of and willingness to use pre-exposure prophylaxis (PrEP) in gay, bisexual, and other men who have sex with men who use geosocial-networking smartphone applications in New York City. AIDS Behav. 2016;20:1–8. [DOI] [PubMed] [Google Scholar]
- 54.Janis IL. Improving adherence to medical recommendations: prescriptive hypotheses derived from recent research in social psychology. Handbook Psychol Health. 1984;4:113–48. [Google Scholar]
- 55.Christensen AJ, Moran PJ, Wiebe JS. Assessment of irrational health beliefs: relation to health practices and medical regimen adherence. Health Psychol. 1999;18(2):169. [DOI] [PubMed] [Google Scholar]
- 56.Gamarel KE, Golub SA. Intimacy motivations and pre-exposure prophylaxis (PrEP) adoption intentions among HIV-negative men who have sex with men (MSM) in romantic relationships. Ann Behav Med. 2015;49(2):177–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Golub SA, et al. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Pat Care and TDs. 2013;27(4):248–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen Y-H, et al. Pre-exposure prophylaxis (PrEP) use, seroadaptation, and sexual behavior among men who have sex with men, San Francisco, 2004–2014. AIDS Behav. 2016;20(12):2791–7. [DOI] [PubMed] [Google Scholar]
- 59.Thorburn S, Harvey SM, Ryan EA. HIV prevention heuristics and condom use among African-Americans at risk for HIV. AIDS care. 2005;17(3):335–44. [DOI] [PubMed] [Google Scholar]
- 60.Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV behavior. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. New York: Kluwer Academic; 2000. p. 3–56. [Google Scholar]
- 61.Fisher Jeffrey D, Fisher William A, Shuper Paul A. The information-motivation-behavioral skills model of HIV preventive behavior. Emerg Theor Health Prom Pract Res. 2009;2:21–64. [Google Scholar]
- 62.Fisher JD, et al. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462. [DOI] [PubMed] [Google Scholar]
- 63.Gallagher T, et al. Self-perception of HIV risk and candidacy for pre-exposure prophylaxis among men who have sex with men testing for HIV at commercial sex venues in New York City. LGBT Health. 2014;1:218–24. [DOI] [PubMed] [Google Scholar]
- 64.Kwakwa HA, et al. Attitudes toward HIV pre-exposure prophylaxis in a United States urban clinic population. AIDS Behav. 2016;20:1–8. [DOI] [PubMed] [Google Scholar]
- 65.Elsesser SA, et al. Seasons of risk: anticipated behavior on vacation and interest in episodic antiretroviral pre-exposure prophylaxis (PrEP) Among a large national sample of US men who have sex with men (MSM). AIDS Behav. 2015;20:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Oldenburg CE, et al. State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS. 2015;29:837–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Golub SA, Gamarel KE, Surace A. Demographic differences in PrEP-related stereotypes: implications for implementation. AIDS Behav. 2015;5:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bauermeister JA, et al. PrEP awareness and perceived barriers among single young men who have sex with men in the United States. Curr HIV Res. 2013;11:520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brooks RA, et al. Perceptions of and intentions to adopt HIV pre-exposure prophylaxis among black men who have sex with men in Los Angeles. Int J STD AIDS. 2015;26:1040–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hoff CC, et al. Attitudes towards PrEP and anticipated condom use among concordant HIV-negative and HIV-discordant male couples. AIDS Pat Care STDs. 2015;29(7):408–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Biello KB, et al. The “Safe Sex” conundrum: anticipated stigma from sexual partners as a barrier to PrEP use among substance using MSM engaging in transactional sex. AIDS Behav. 2016;21:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sullivan PS, et al. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. Aids. 2009;23(9):1153–62. [DOI] [PubMed] [Google Scholar]
- 73.Nimmons D, Folkman S. Other-sensitive motivation for safer sex among gay men: expanding paradigms for HIV prevention. AIDS Behav. 1999;3(4):313–24. [Google Scholar]
- 74.Aizen I The construction of a standard questionnaire for the theory of planned behavior. Retrieved from the World Wisd Web: http://www.unix.it.umass.edu/~ejzen (2000).
- 75.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191. [DOI] [PubMed] [Google Scholar]
- 76.Taylor SW, et al. Optimizing content for pre-exposure prophylaxis (PrEP) counseling for men who have sex with men: perspectives of PrEP users and high-risk PrEP naive men. AIDS Behav. 2014;18(5):871–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bauermeister JA, et al. PrEP awareness and perceived barriers among single young men who have sex with men in the United States. Curr HIV Res. 2013;11(7):520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Stein M, Thurmond P, Bailey G. Willingness to use HIV pre-exposure prophylaxis among opiate users. AIDS Behav. 2014;18(9):1694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gamarel K. Relationship dynamics and pre-exposure prophylaxis (PrEP) adherence self-efficacy among men who have sex with men (MSM) in romantic relationships. 2015 APHA Annual Meeting & Expo (Oct. 31–Nov. 4, 2015). APHA, 2015. [Google Scholar]
- 80.Dubov A, et al. Stigma and shame experiences by MSM who take PrEP for HIV prevention: A qualitative study. PLoS One, forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Smith DK, et al. Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PrEP). AIDS Educ Prev. 2012;24(5):408–21. [DOI] [PubMed] [Google Scholar]
- 82.Sheeran P. Intention—behavior relations: a conceptual and empirical review. Eur Rev Soc Psychol. 2002;12(1):1–36. [Google Scholar]
- 83.Sniehotta FF, et al. Action planning and coping planning for long-term lifestyle change: theory and assessment. Eur J Soc Psychol. 2005;35(4):565–76. [Google Scholar]
- 84.Gollwitzer PM. Implementation intentions: strong effects of simple plans. Am Psychol. 1999;54:493. [Google Scholar]
- 85.Oldenburg CE, et al. Differences in attitudes about HIV pre-exposure prophylaxis use among stimulant versus alcohol using men who have sex with men. AIDS Behav. 2015;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455. [DOI] [PubMed] [Google Scholar]
- 87.Amico KR. A situated-information motivation behavioral skills model of care initiation and maintenance (sIMB-CIM): an IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. J Health Psychol. 2011;16(7):1071–81. [DOI] [PubMed] [Google Scholar]
- 88.Blashill AJ, et al. Optimizing adherence to preexposure and postexposure prophylaxis: the need for an integrated biobehavioral approach. Clin Infect Dis. 2015;60(suppl 3):S187–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mayer KH, et al. Antiretroviral pre-exposure prophylaxis implementation in the United States: a work in progress. J Int AIDS Soc. 2015;18(4 Suppl 3):19980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Auerbach JD, Hoppe TA. Beyond “getting drugs into bodies”: social science perspectives on pre-exposure prophylaxis for HIV. J Int AIDS Soc. 2015;18(4 Suppl 3):19983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Marcus JL, et al. Helping our patients take HIV pre-exposure prophylaxis (PrEP): a systematic review of adherence interventions. HIV medicine. 2014;15(7):385–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Borges C. Limited Knowledge, but High Interest in HIV Pre-Exposure Prophylaxis Among Patients Attending New York City Health Department STD Clinics, 2013–2014. 2014 National STD Prevention Conference. CDC, 2014. [Google Scholar]
- 93.Mantell JE, et al. Knowledge and attitudes about Pre-Exposure Prophylaxis (PrEP) among sexually active men who have sex with men (MSM) participating in New York City gay pride events. LGBT health. 2014;1(2):93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mayer KH, et al. Differences in PrEP knowledge and use in US MSM users of a popular sexual networking site surveyed in August 2013 and January 2014. AIDS Res Hum Retroviruses. 2014;30:A91–2. [Google Scholar]
- 95.Garnett M, et al. Limited awareness of pre-exposure prophylaxis among black men who have sex with men and transgender women in New York city. AIDS care. 2018;30:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Parsons JT, et al. Familiarity with and preferences for oral and long-acting injectable hiv pre-exposure prophylaxis (PrEP) in a national sample of gay and bisexual men in the US. AIDS Behav. 2016;20:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Krakower DS, et al. Limited awareness and low immediate uptake of pre-exposure prophylaxis among men who have sex with men using an internet social networking site. PLoS ONE. 2012;7:e33119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zarwell M. Usage and perceptions of PrEP among men who have sex with men (MSM) in New Orleans, 2014. 2015 APHA Annual Meeting & Expo (Oct. 31–Nov. 4, 2015). APHA, 2015. [Google Scholar]
- 99.Uthappa CK, et al. Pre-exposure prophylaxis: awareness, acceptability and risk compensation behaviour among men who have sex with men and the transgender population. HIV Med. 2017. 10.1111/hiv.12572. [DOI] [PubMed] [Google Scholar]
- 100.Golub SA, Gamarel KE, Surace A. Demographic differences in PrEP-related stereotypes: implications for implementation. AIDS Behav. 2017;21(5):1229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Holloway IW, et al. Facilitators and barriers to pre-exposure prophylaxis willingness among young men who have sex with men who use geosocial networking applications in California. AIDS Pat Care STDs. 2017;31(12):517–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Grov C, et al. Changes in familiarity with and willingness to take preexposure prophylaxis in a longitudinal study of highly sexually active gay and bisexual men. LGBT Health. 2016;3:252–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kuhns LM, et al. Use of pre-exposure prophylaxis (PrEP) in young men who have sex with men is associated with race, sexual risk behavior and peer network size. AIDS Behav. 2017;21:1376–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Young LE, et al. PrEP Chicago: a randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clin Trials. 2017;15:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mitchell JW, et al. HIV-negative male couples’ attitudes about pre-exposure prophylaxis (PrEP) and using PrEP with a sexual agreement. AIDS Care. 2016;28:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Stack C, et al. Sexual behavior patterns and PrEP dosing preferences in a large sample of North American men who have sex with men. JAIDS J Acquir Immune Defic Syndr. 2016;71:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.John SA, et al. Home-based pre-exposure prophylaxis (PrEP) services for gay and bisexual men: an opportunity to address barriers to PrEP uptake and persistence. PLoS ONE. 2017;12:e0189794. [DOI] [PMC free article] [PubMed] [Google Scholar]


