Abstract
Objective:
Advancing understanding of how early adversity arises, manifests, and contributes to health difficulties depends on accurate measurement of children’s experiences. In early life, exposure to adversity is often intertwined with that of one’s caregivers. We present preliminary psychometric properties of a novel measure of adversity, the Assessment of Parent and Child Adversity (APCA), which simultaneously characterizes parents’ and children’s adversity.
Methods:
During pregnancy, women reported their past adverse experiences. When their children were ages 3–5 years (47% female), 97 mothers (71% White, 17% Hispanic/Latinx) completed the APCA, the Childhood Trauma Questionnaire, and the Benevolent Childhood Experiences scale. They reported their current symptoms of depression and anxiety and their child’s emotional and behavioral problems. Using the APCA, we distinguished between maternal adversity during different life periods and obtained metrics of child witnessing of and direct exposure to adversity.
Results:
The APCA demonstrated validity with other measures of maternal adverse experiences, maternal positive childhood experiences, and maternal symptoms of psychopathology. Children whose mothers experienced greater adversity, particularly in the prenatal period, had more emotional and behavioral problems, as did children who were directly exposed to greater adversity.
Conclusions:
The APCA has good usability and validity. Leveraging the ability of the APCA to distinguish between adversity during different life stages and originating from different sources, our findings highlight potentially distinct effects of different aspects of maternal and child adversity on difficulties in maternal and child mental health.
Keywords: adversity, stress, assessment, parent, caregiver, child
Introduction
There is extensive evidence that exposure to adversity during early life contributes to health difficulties across the lifespan and fosters social inequality in health outcomes (Felitti et al., 1998; Green et al., 2010; Umberson et al., 2014). Questions remain, however, about the sources, dimensions, or developmental timing of adverse experiences (Gabard-Durnam & McLaughlin, 2020; May & Wisco, 2016; McLaughlin et al., 2014). Accurate assessment of these aspects of adversity is essential for answering these questions, and, ultimately, for determining when, how, and for whom we should deliver interventions aimed at preventing or mitigating the negative consequences of adversity.
Most research examining childhood adversity has focused on children’s direct experiences of adversity. The positive association between greater direct exposure to childhood adversity and health difficulties is well-documented. For example, in a meta-analysis of 57 studies of early adversity and depression, LeMoult et al. (2019) found that children and adolescents exposed to early adversity were over twice as likely to develop depression as were their non-exposed peers. Most of the studies included in this meta-analysis focused on children’s direct experiences, such as abuse and other violence. There are issues, however, in focusing solely on children’s direct adversity, particularly when measuring adversity in infants and young children. Specifically, because infants and young children are so dependent on their caregivers, children of this age may be especially susceptible to indirect exposure to adversity through their caregivers. Focusing solely on direct adversity may lead to underestimating environmental risk for children of any age, but particularly for children for infants and young children, posing challenges for studying the impact of adversity during a developmental period when neurobiological plasticity confers high sensitivity to the environment (Nelson & Gabard-Durnam, 2020).
Infants and young children may be indirectly exposed to adversity affecting those close to them in a manner that enhances their risk for future health difficulties. For example, they may see, hear, and/or learn about their parents’ adverse experiences, or, more distally, they may experience changes to their environment associated with their caregiver’s exposure to adversity even when they have no knowledge of this exposure. For example, caregiver exposure to adversity may affect the caregiver’s ability to engage in perspective taking with their child in a manner that affects their caregiving behavior and, in turn, the everyday environments of children (King et al., 2021). In a powerful demonstration of how caregiver exposure to a stressor, even in the absence of the child, may be “contagious,” Waters et al. (2014) found that the infants of mothers exposed to a laboratory stressor mirrored their mothers’ physiological reactivity upon reunion. Such effects evince the intimate relationship between caregivers and their children, particularly their infants and young children, with whom experiences of the world and the consequences of these experiences are shared dyadically. Nevertheless, assessments of parent and child adversity are most often separate. Although existing measures of life adversity in children assess whether children have witnessed experiences that may involve caregivers, such as violence between family members (e.g., the Traumatic Events Screening Inventory; Ford et al., 2002; Ippen et al., 2002]), they do not explicitly inquire about the caregivers’ experiences of adversity during the child’s lifetime that may indirectly affect the child.
In addition to caregiver adverse experiences that occur during the child’s lifetime, caregivers’ experiences prior to the birth of their child may indirectly affect their child’s development through several pathways (Bowers & Yehuda, 2016). Mothers’ exposure prior to the child’s birth may affect postnatal co-regulatory dyadic functioning (Roubinov et al., 2021). For example, maternal exposure to childhood adversity has been associated with less emotional availability during interactions with their infants (Fuchs et al., 2015), and parents who were exposed to maltreatment are at increased risk for maltreating their own child or for having a child who is maltreated by someone else (Madigan et al., 2019). Mothers’ exposure to adversity during her own childhood, prior to the conception of her child, and during pregnancy with the child may also influence children’s outcomes through epigenetic processes, alterations to gametes, and deviations in the intrauterine milieu that may affect birth outcomes and fetal neurodevelopment (Bowers & Yehuda, 2016; Entringer et al., 2015; Roubinov et al., 2021). In fact, there is extensive evidence that maternal life adversity prior to the birth of the child is associated with increased risk for both behavioral problems in offspring (Collishaw et al., 2007) and adult mood disorders (Kleinhaus et al., 2013). Nonetheless, as recently highlighted by Narayan et al. (2021), frameworks for targeting early adversity disseminated by leading public health institutions (e.g., the CDC’s Essentials for Childhood Framework; CDC, 2019), largely ignore the role of parents’ histories of adversity in determining child health, perhaps in part because science in this area is limited by the ability of existing measures to disentangle maternal adversity during different life stages prior to the birth of the child from the child’s indirect and direct experiences of adversity postnatally.
The goal of the current study was to introduce the Assessment of Parent and Child Adversity (APCA), which addresses limitations of existing measures to better characterize parents’ and children’s adverse experiences and to distinguish aspects of these experiences that may moderate children’s outcomes. The APCA, which is free for use with available modification and scoring provided at https://osf.io/tgmpz/, is based on the premise that children’s experiences, especially those of infants and young children, are intertwined with those of their primary caregivers (most often, their parents). Given that both child direct exposure to adversity and child indirect exposure to caregiver adversity experienced prior to the child’s birth and/or during the child’s lifetime may contribute additively or in distinct ways to children’s functioning, the APCA integrates the assessment of caregiver and child adversity to provide a more comprehensive assessment of children’s environmental risk.
Here, we provide preliminary validation of the APCA in a sample of mothers and their 3- to 5-year-old children. This developmental stage was selected because we can reliably detect, and therefore predict, early signs of psychopathology in children of this age (Sterba et al., 2007; Zero to Three, 2016). Distinguishing between maternal adversity during different life stages (in childhood, in adulthood prior to conception of the focal child, during pregnancy, and since the birth of the focal child), and between child indirect and direct exposure to adversity, we examined the convergent validity of the APCA by testing associations with existing measures of adversity and the criterion validity of the APCA by testing associations with other theoretically relevant constructs (Clark & Watson, 2019). First, we examined the convergent validity of the APCA—specifically maternal childhood adversity measured by the APCA and maternal adversity prior to conception of the child—with external measures of childhood maltreatment and adversity. Second, we investigated whether APCA measures of maternal adversity across life stages have criterion validity with mothers’ positive childhood experiences, mothers’ symptoms of psychopathology, and children’s emotional and behavioral problems, and whether APCA measures of child indirect and direct exposure to adversity have criterion validity with children’s emotional and behavioral problems. We explored potential differential effects of maternal developmental timing of adversity and of child indirect versus direct exposure to adversity on mothers’ and children’s mental health difficulties.
Method
Participants
Mothers were originally recruited during pregnancy to participate in a study of biopsychosocial factors associated with uncomplicated and pathological pregnancies conducted by the March of Dimes Prematurity Research Center (PRC) at Stanford University (Ghaemi et al., 2019; Wise et al., 2017). Stanford University is located in Santa Clara County, CA, USA. The data presented in the current study were drawn from a follow-up assessment of a subset of these mothers and their young children (3.00–5.99 years) with whom they were pregnant when they were originally recruited to the PRC project. Of the 451 women who participated in the larger PRC project during pregnancy, 226 were eligible for this follow-up assessment (see Procedure for criteria), of whom 97 completed the APCA and were included in the current analyses. One mother completed the APCA but did not complete the other questionnaires analyzed.
Procedure
This project was approved by the Stanford Institutional Review Board (approval # 36366). Mothers provided informed written consent for themselves and their children and were compensated for their time. Mothers were recruited during pregnancy to the larger PRC project after presenting at the Obstetrics Clinics of the Lucile Packard Children’s Hospital at Stanford University. Inclusion criteria for the larger PRC study were that women were ≥18 years of age and in their first trimester of pregnancy. Inclusion criteria for the follow-up assessment were that women had a live birth, that their child was currently age 3.00–5.99 years, and that mothers were fluent in English. Exclusion criteria for the follow-up assessment were premature birth, child or mother disability that would interfere with the ability to complete the study assessments, child severe medical illness, and child traumatic brain injury. During pregnancy, women provided blood samples in each trimester of pregnancy, and responded to questionnaires about their demographics, environments, and health. Mothers were contacted by phone to schedule the follow-up assessment. For the follow-up assessment, mothers completed the APCA and responded to questionnaires about their demographics, environments, and their own and their child’s psychological functioning. A subset of mothers and their children (46 of the 97 included in the current study) also attended a laboratory session at which children underwent functional near infrared spectroscopy (fNIRS) brain imaging and completed a series of behavioral tasks (not reported here).
Measures
Demographic Characteristics
Maternal and child ages were calculated as the difference in years between their birth dates and the date of the assessment. Mothers reported their race, whether they identified as Hispanic or Latinx, their education level, their annual household income, and their child’s sex. We calculated family income-to-federal poverty level (FPL) ratios by dividing annual household income by the FPL specific to the number of children and adults that mothers reported were in their household. Four mothers declined to report their household income.
Assessment of Parent and Child Adversity
Mothers completed the APCA (King, 2019; https://osf.io/tgmpz/) to assess their own and their child’s lifetime exposure to adversity. The APCA was developed to allow for the simultaneous assessment of both the parent’s and the focal child’s exposure to adversity, including the developmental timing of parent and child adverse experiences and the child’s indirect exposure to parental adverse experiences. The APCA is a computerized assessment currently hosted on the web-based platform, REDCap (Harris et al., 2009) and licensed under the Creative Commons Attribution 4.0 International License (see http://creativecommons.org/licenses/by-nc-sa/4.0/). Although the APCA was administered as a questionnaire, programmed branching logic ensured that mothers were presented only with questions that were relevant to their previous answers.
In the first section of the APCA, mothers responded (yes or no) to whether they had been exposed to each of 40 types of adversity (listed in Table 2), and, to capture other adverse experiences that were not explicitly assessed, to whether any of these adversities had “happened to someone close to you,” and to whether they had experienced “any other frightening or stressful events.” We provide detailed information about item development in the Supplementary Material. Briefly, we initially reviewed a larger pool of 126 items from the Crisis in Family Systems–Revised (CRISYS; Berry, Quinn, Shalowitz, & Wolf, 2001), the Life Stressor Checklist–Revised (LSC-R; Wolfe, Kimerling, Brown, Chrestman, & Levin, 1996), and the Traumatic Events Screening Inventory—Parent Report Revised (TESI-PRR; Ippen et al., 2002). We selected these measures to catalog adversities because they each assess an extensive range of experiences, but are also complementary; that is, the CRISYS includes adverse experiences that may not rise to the level of trauma, whereas the LSC-R and TESI-PRR focus on potentially traumatic experiences as defined by the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013). We eliminated items that did not meet a guiding definition of adversity as external experiences that may serve as psychosocial hazards (Humphreys & Zeanah, 2015; McLaughlin & Sheridan, 2016; Nelson & Gabard-Durnam, 2020) and we revised the remaining items to maximize efficiency, clarity, and specificity. Although witnessing caregiver psychopathology may be an adversity for the child, given that the APCA is also an assessment of caregiver adversity, we did not include items assessing the target caregiver’s experience of psychopathology, including substance abuse, because doing so conflates a response to adversity with exposure to adversity, thereby biasing estimates of associations between adversity and psychopathology (Harkness & Monroe, 2016). We suggest that researchers interested in caregiver psychopathology use independent validated measures designed to assess this construct. We also developed a small number of novel items based on our experience conducting and coding interviews with caregivers about their adversity histories (e.g., “Has a partner ever insisted on controlling your behavior?” [partner coercive control]). Finally, we conducted internal pilot testing by members of our labs to ensure readability and clarity of the items.
Table 2.
Descriptive statistics for maternal exposure to adversity and child indirect exposure.
| Type of Maternal Adversity | Lifetime Exposure |
M[SD] age of onset | Since birth | Age of child | Child witnessed |
|---|---|---|---|---|---|
| Abortion/miscarriage | 51% | 29.04[6.66] | 19% | 2.57[0.94] | 7% |
| Accident | 21% | 22.55[8.81] | 3% | 2.33[1.15] | 2% |
| Accident (W) | 27% | 23.44[7.70] | 5% | 2.60[1.14] | 3% |
| Adoption/foster care (childhood) | 1% | 0.00 | |||
| Arrested/jailed | 4% | 22.00[2.58] | 0% | ||
| Authority problems | 22% | 20.77[8.93] | 6% | 0.92[1.11] | 0% |
| Bullying (childhood) | 28% | 8.42[3.67] | |||
| Caregiver for ill person | 19% | 30.67[10.05] | 9% | 1.36[1.29] | 7% |
| Death | 64% | 22.87[9.64] | 18% | 1.98[1.43] | 7% |
| Disaster | 21% | 12.33[9.17] | 4% | 2.54[1.84] | 2% |
| Discrimination | 35% | 18.15[9.57] | 13% | 1.08[1.85] | 3% |
| Divorce | 14% | 29.64[6.06] | 2% | 2.00[1.41] | 1% |
| Emotional abuse | 16% | 10.07[7.41] | 3% | 1.33[2.31] | 0% |
| Emotional neglect | 21% | 15.20[13.15] | 6% | 0.50[1.22] | 4% |
| Family arrested/jailed | 14% | 18.38[12.38] | 3% | 1.33[1.15] | 2% |
| Family verbal fighting (W) | 56% | 8.11[6.65] | 6% | 0.92[1.02] | 2% |
| Family violence (W) | 24% | 8.74[6.76] | 0% | ||
| Financial problems | 31% | 25.45[8.97] | 12% | 1.52[1.29] | NA |
| Fired/laid-off | 11% | 26.27[3.77] | 2% | 3.00[2.83] | NA |
| Immigration | 39% | 21.14[8.60] | 6% | 1.44[1.40] | 5% |
| Language barriers | 18% | 18.25[7.86] | 6% | 1.00[1.67] | 0% |
| Legal problems | 19% | 27.44[5.89] | 7% | 1.43[1.27] | 1% |
| Mental illness (W) | 53% | 16.58[13.20] | 20% | 0.95[1.47] | 9% |
| Neighborhood danger | 27% | 21.85[10.25] | 10% | 1.40[1.07] | 2% |
| Other exposure | 9% | 19.44[10.70] | 0% | ||
| Parental divorce | 33% | 11.06[10.44] | 2% | 1.50[2.12] | 2% |
| Partner coercive control | 11% | 22.92[4.87] | 3% | 0.03[0.05] | 1% |
| Partner disagreement | 38% | 32.47[5.26] | 35% | 0.51[0.93] | 20% |
| Partner drug abuse | 16% | 21.81[5.34] | 5% | 0.40[0.89] | 2% |
| Partner verbal fighting | 47% | 26.84[7.11] | 22% | 1.10[1.45] | 11% |
| Physical abuse | 12% | 16.08[8.92] | 0% | ||
| Physical illness | 22% | 29.29[11.99] | 12% | 2.09[1.72] | 10% |
| Physical illness (W) | 49% | 27.09[8.77] | 14% | 1.12[1.56] | 9% |
| Physical neglect | 4% | 2.25[3.86] | 0% | ||
| Police discrimination | 3% | 18.33[4.93] | 0% | ||
| Rape | 18% | 18.88[8.49] | 1% | 3.00 | 0% |
| Robbery, mugging, attack | 11% | 22.36[5.80] | 1% | 3.00 | 0% |
| Robbery, mugging, attack (W) | 12% | 26.42[7.79] | 1% | 3.00 | 0% |
| Separation from child | 3% | 29.67[7.57] | 3% | 1.50[2.12] | 2% |
| Sexual harassment | 31% | 18.93[5.41] | 3% | 1.33[1.53] | 1% |
| Sexual molestation | 24% | 13.39[7.87] | 1% | 3.00 | 0% |
| Someone else exposed | 11% | 22.00[10.13] | 4% | 2.00[1.83] | 0% |
N=97. “Exposed in pregnancy” indicates mother was exposed when pregnant with the focal child. Maternal and child age in years. M=mean. SD=standard deviation. (W) indicates mother witnessed the adversity. “Since birth” indicates the maternal adversity occurred since the birth of the focal child. “Child witnessed” indicates that mother endorsed that the child saw or heard about the adversity. “Other exposure” and refers to open-ended question, ““Have you experienced any other frightening or stressful events that we did not include?”
In the second section of the APCA, mothers responded to a series of follow-up questions pertaining to each of the adversities for which they had endorsed exposure in the first section. Follow-up questions included whether the adversity occurred when the mother was pregnant with the focal child; the frequency of the adversity; whether the adversity was ongoing; the earliest and latest ages of the mother when the adversity occurred (i.e., age of onset and offset); the perceived severity of the adversity; whether the adversity had occurred since the birth of the focal child; the age of the focal child when the adversity occurred; and whether the child saw or heard about the adversity. Researchers using the APCA in other settings may wish to omit some of these follow-up questions depending on their goals for balancing participant time with specificity of measurement.
In the final section of the APCA, mothers responded (yes or no) to whether their child had been exposed to 15 types of adversity (listed in Table 3) for which the child was the primary individual exposed to the adversity and to which the child may have been exposed in the absence of the mother (e.g., bullying, accident). For each of these 15 adverse experiences, mothers responded to a series of follow-up questions, including the age of the child when the adversity occurred and the mother’s perception of the severity of the adversity for the child.
Table 3.
Descriptive statistics for child direct exposure to adversity.
| Type of adversity | Exposed | M[SD] age at occurrence |
|---|---|---|
| Accident | 1% | 3.00 |
| Accident (W) | 1% | 2.00 |
| Adoption/foster care | 1% | 3.00 |
| Attack by stranger | 0% | |
| Bullying | 7% | 3.14[1.68] |
| Disaster | 0% | |
| Emotional abuse | 8% | 3.12[1.25] |
| Emotional neglect | 2% | 1.00[1.41] |
| Immigration | 1% | 0.83 |
| Physical abuse | 4% | 2.00[0.00] |
| Physical illness | 10% | 1.20[1.13] |
| Physical neglect | 0% | |
| Separation from caregiver | 1% | 3.00 |
| Sexual abuse | 0% | |
| Spanking | 20% | 2.63[0.96] |
N=97. Whereas child indirect exposure (Table 2) indicates that a maternal adversity occurred during the child’s lifetime and/or the child witnessed the mother’s adversity, child direct exposure indicates that the child was the primary victim of the adversity and/or witnessed the adversity in the absence of the mother. Age is in years. M=mean. SD=standard deviation. (W) indicates child witnessed the adversity happen in the absence of the mother.
Multiple aspects of adversity can be quantified using the APCA that help to disentangle the effects of maternal adversity experienced at different life stages, child witnessing of maternal adversity, and child direct exposure to adversity. In the current study we focused on the following seven summary scores:
Maternal childhood adversity: the total number of adverse experiences that the mother reported experiencing at <18 years of age.
Maternal preconception adversity: the total number of adverse experiences that the mother reported experiencing in adulthood (i.e., ≥18 years of age) but not since they were pregnant with the focal child.
Maternal prenatal adversity: the number of adverse experiences that the mother reported occurred during her pregnancy with the focal child.
Maternal adversity since the child’s birth: the number of adverse experiences that the mother reported experiencing since the birth of the focal child.
Maternal cumulative adversity: the total number of types of adversity that the mother reported experiencing in her lifetime.
Child witnessed adversity: the number of maternal adverse experiences that the mother reported the child saw, heard, or heard about.
Child direct adversity: the number of adverse experiences for which the child was the primary individual exposed.
Preexisting Measures of Maternal Life Experiences
Maternal Exposure to Childhood Maltreatment.
Mothers completed the Childhood Trauma Questionnaire–Short Form (CTQ), which has been validated in a community sample of adults (Bernstein et al., 2003). The CTQ is a 25-item assessment of exposure to emotional, physical, and sexual abuse and emotional and physical neglect in. The CTQ instructed mothers to rate the degree to which they were exposed to maltreatment experiences in childhood on 5-point scale ranging from 0 (never) to 5 (very often true), with higher scores indicating greater severity of exposure to childhood maltreatment (Cronbach’s α=.95).
Maternal Life Adversity Reported 3–5 Years Earlier.
During the first trimester of their pregnancy with the focal child, mothers completed a checklist of adverse life events administered as part of the Dhabhar Quick-Assessment Questionnaire for Stress and Psychosocial Factors (DQAQ-SPF; Becker et al., 2021). Mothers indicated (yes or no) to whether they had been exposed to each of 14 adverse experiences, including death of a loved one, serious accident, and divorce. We summed mothers’ responses to obtain a count of lifetime adversity.
Maternal Exposure to Positive Childhood Experiences.
Mothers completed the Benevolent Childhood Experiences (BCEs) scale, which has been validated in samples of parents and pregnant women (Merrick et al., 2019; Narayan et al., 2018). The BCEs instructed mothers to indicate whether they were exposed (yes or no) to each of ten positive experiences “when you were growing up, during your first 18 years of life.” Higher scores indicate a greater number of positive experiences.
Maternal and Child Mental Health Difficulties
Maternal Symptoms of Psychopathology.
To assess maternal depressive symptoms, mothers completed the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977), which has been validated in samples of parents (Atkins, 2014; Orme et al., 1984). The CES-D asks mothers to consider the past week and respond to each of 20 items on a 4-point scale from 0 (rarely or none of the time) to 3 (most or all of the time), with higher scores representing greater depressive symptoms (Cronbach’s α=.87).
To assess maternal anxiety symptoms, mothers completed the Beck Anxiety Inventory (BAI; Beck & Steer, 1993), which has been validated in a community sample of adults (Osman et al., 1993). The BAI asks mothers to consider the past month and rate each of 21 items on 4-point scale from 0 (not at all) to severely (bothered me a lot), with higher scores indicating greater anxiety symptoms (Cronbach’s α=.88).
Child Behavioral and Emotional Problems.
To assess their child’s emotional and behavioral problems, mothers completed the Child Behavior Checklist for ages 1.5–5 years (CBCL/1.5–5; Achenbach & Rescorla, 2000), which has been validated in several epidemiological samples (Ivanova et al., 2010). The CBCL/1.5–5 asks mothers to consider the past 2 months and respond to 99 questions about their child’s emotions and behaviors on a scale of 0 (not true) to 2 (very true or often true). We focused on the raw total problems score, which is the sum of responses to questions assessing internalizing, externalizing, sleep, and stress problems, with higher scores indicating more severe problems (Cronbach’s α=.92).
Statistical Analyses
All analyses were conducted in R version 4.1.1 (R Core Team, 2021). Data and code are available at https://github.com/lucysking/MoD/tree/master/king_APCA_validation. For all regression models, we used the “performance” and “parameters” packages to examine model diagnostics and output (Lüdecke et al., 2019; Lüdecke et al., 2020).
We used Pearson’s correlation tests (continuous variables), Spearman’s correlation tests (count variables), or Welch’s t-tests (binary variables) to examine associations among the APCA variables and demographic characteristics, including maternal age, child age, family income-to-FPL ratio, maternal racial identity (minority vs. White), maternal ethnic identity (Latinx vs. not), and child sex. We also examined associations of measures of maternal symptoms of psychopathology and children’s total emotional and behavioral problems with demographic characteristics.
We assessed convergent validity by analyzing associations of APCA variables of maternal adversity with existing measures of adversity (Clark & Watson, 2019). Specifically, we tested: (1) whether maternal childhood maltreatment, measured by the CTQ, was positively associated with maternal childhood adversity, measured by the APCA; and (2) whether maternal life adversity, measured using the DQAQ-SPF, was positively associated with maternal childhood and preconception adversity, measured by the APCA. We used Spearman’s correlation tests to examine the bivariate associations between these variables. To complement the results of the Spearman’s correlation tests and estimate more interpretable effect sizes for these analyses in which the dependent variables reflected counts, we also used negative binomial regression conducted using the “MASS” package (Venables & Ripley, 2002). These models yielded the predicted incidence rate ratios based on the CTQ and the DQAQ-SPF for maternal childhood and maternal preconception adversity measured by the APCA, respectively. We selected negative binomial regression over Poisson regression because model diagnostic tests indicated overdispersion (Gelman & Hill, 2007). Given that the APCA variables tended to be positively skewed and to contain many zeros (see Supplementary Material), future research with this measure should also consider modeling approaches that account for zero-inflation. Given the presence of extreme outlying values in the CTQ total score, we winsorized CTQ scores prior to analysis by replacing values >3SD from the mean with the mean + 3SD value. To evaluate the impact of winsorizing, we reran analyses involving the CTQ using the raw scores; although conclusions were the same, regression model fit was poorer (see Supplementary Materials).
We assessed criterion validity by analyzing associations of APCA variables with measures of other theoretically relevant constructs (Clark & Watson, 2019). First, we tested whether maternal positive childhood experiences, measured by the BCEs scale, were negatively associated with maternal childhood adversity, measured by the APCA. Here, too, we used Spearman’s correlation tests and negative binomial regression to test the association between these variables. Second, we tested whether maternal cumulative adversity was positively associated with maternal symptoms of depression and anxiety. We used Spearman’s correlation tests to examine the bivariate associations between these variables. We explored the relative strength of associations with maternal symptoms of depression and anxiety based on when the adversity occurred (childhood, preconception, prenatal, since the birth of the focal child). We calculated Bayes factors using the “BayesFactor” package in R (Morey, 2019) to characterize relative effect sizes and, in a multiple OLS regression, examined the unique associations of maternal adversity during each life stage with maternal symptoms, adjusting for maternal adversity in other life stages. Bayes factors quantify the strength of evidence in the data for the alternative hypothesis (in this case, that the association ≠ 0), compared to the null hypothesis (in this case, that the association = 0). For example, derived from the ratio of the marginal likelihoods of the alternative and null models, a Bayes factor of 10 indicates that the support in the data for the alternative hypothesis is 10 times greater than the support for the null hypothesis. Bayes factors from 1–3 are considered “anecdotal” evidence for the alternative hypothesis, from 3–10 as “moderate” evidence, from 10–30 as “strong” evidence, and from 30–100 as “very strong” evidence, and ≥100 as “extreme” evidence (Quintana & Williams, 2018). Thus, in addition to statistical significance, Bayes factors provide a complementary method of evaluating support in the data for the presence of non-zero associations among variables.
Finally, we explored associations of maternal cumulative adversity, maternal adversity during each life stage, and child witnessed and direct adversity with children’s total emotional and behavioral problems. We used Spearman’s correlation tests to examine the bivariate associations between each of these APCA variables and children’s problems. Once again, we calculated Bayes factors to characterize relative effect sizes and, in separate multiple OLS regression models, examined the unique associations of maternal adversity during each life stage with children’s problems, and of child witnessed and direct adversity with children’s problems.
Results
Sample Characteristics
Sample characteristics are presented in Table 1. Most mothers identified as White or Asian American. Overall, 32% of mothers reported racial or ethnic identities that are minorities in the U.S. (i.e., Latinx ethnicity or a race that is not White). Mothers tended to be highly educated. Fifteen percent of mothers had depressive symptoms scores on the CES-D ≥16, indicating risk for clinical depression (Lewinsohn et al., 1997), and 6% had anxiety symptom scores on the BAI ≥16, indicating risk for clinical anxiety (Beck & Steer, 1993). Eight percent of children had total emotional and behavioral problems scores on the CBCL in the borderline clinical or clinical range (T-scores ≥60). Family annual income ranged from ≤$10,000 to >$250,000, with 10% of families designated as “low income” (<200% of the FPL).
Table 1.
Sample characteristics.
| Measure | M[SD] or % | Range |
|---|---|---|
| Maternal age (years) | 37.19[4.56] | 23.40–49.26 |
| Child age (years) | 4.19[0.87] | 3.05–5.99 |
| Income-to-FPL ratio | 6.44[3.26] | 0.33–14.60 |
| APCA Variables | ||
| Maternal cumulative adversity | 9.90[5.93] | 0–27 |
| Maternal childhood adversity | 3.59[3.33] | 0–16 |
| Maternal preconception adversity | 2.89[2.64] | 0–10 |
| Maternal prenatal adversity | 1.24[1.82] | 0–9 |
| Maternal adversity since child’s birth | 2.70[2.71] | 0–13 |
| Child witnessed adversity | 1.18[1.50] | 0–8 |
| Child direct adversity | 0.57[0.92] | 0–4 |
| Time to complete (minutes) | 18.23[12.82] | 0–63 |
| Maternal childhood maltreatment (CTQ) | 7.48[14.37] | 0–94 |
| Maternal adverse experiences assessed 3–5 years earlier (DQAQ-SPF) |
2.20[1.74] | 0–10 |
| Maternal positive childhood experiences | 9.39[1.13] | 4–10 |
| Maternal depressive symptoms | 9.68[6.83] | 0–32 |
| Maternal anxiety symptoms | 5.25[5.88] | 0–35 |
| Child total emotional and behavioral problems | 25.31[15.69] | 0–75 |
| Child female sex | 47% | |
| Maternal race | ||
| American Indian or Alaskan Native | 2% | |
| Asian or Asian American | 22% | |
| Black or African American | 4% | |
| Native Hawaiian or Pacific Islander | 0% | |
| White | 71% | |
| “Other” race | 5% | |
| Maternal Hispanic/Latinx ethnicity | 17% | |
| Maternal education | ||
| <4-year college degree | 19% | |
| Bachelor’s degree | 26% | |
| Graduate degree | 55% |
N=97. Mothers could identify with more than race. Income-to-FPL=income-to-federal poverty level based on number of adults and children in the household. CTQ=Childhood Trauma Questionnaire – Short Form (Bernstein et al., 2003).
APCA Descriptive Statistics
As presented in Table 1, on average, mothers completed the APCA in ~18 minutes (median=15.00, interquartile range=9.00–23.00) and reported ~10 lifetime adverse experiences. Only 1 mother discontinued the APCA before completing it.
In Table 2 we present descriptive statistics for maternal exposure to adversity and child indirect exposure to maternal adversity measured by the APCA. The age of onset for maternal adversity ranged from 0–48 years (M[SD]=20.62[11.01]). Thirteen percent of the adverse experiences that mothers reported began in infancy or young childhood (<age 6 years), 11% in middle childhood (ages 6–11 years), 12% in adolescence (12–17 years), 23% in emerging adulthood (18–24 years), and 41% in adulthood (≥25 years). Fifty-two percent of women reported at least one adversity during pregnancy with the focal child.
In Table 2, we also present descriptive statistics for child witnessed adversity. Supporting the formulation that children often are exposed to adverse experiences to which their caregivers are primarily exposed, children witnessed an average of 43% (range=0–100%) of the adverse experiences that their mother reported had occurred since the child’s birth. On average, children witnessed maternal adversity for the first time at age 1.37 years (SD=1.45, range=0–5).
Finally, in Table 3, we present descriptive statistics for child direct adversity. As we anticipated, endorsement of child direct adversity was generally low. On average, children were directly exposed to adversity for the first time at age 2.40 years (SD=1.28, range=0–5).
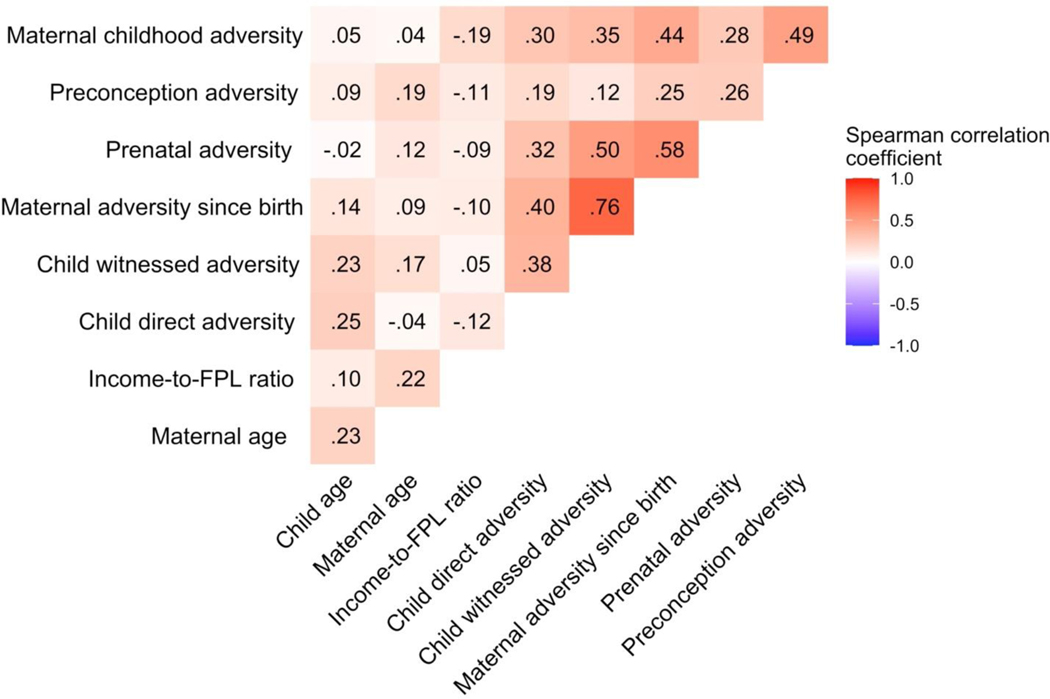
Associations Among APCA Variables and Demographic Variables
In Figure 1, we present bivariate correlations among each of the APCA variables and maternal age, child age, and family income-to-FPL ratio. Measures of maternal and child adversity were significantly positively intercorrelated: mothers who reported exposure to a greater number of adverse experiences in their own childhood and during pregnancy also tended to report that their child had witnessed and been directly exposed to a greater number of adversities. In contrast, maternal preconception adversity was not significantly associated with child witnessed or direct adversity.
Figure 1. Correlations among APCA measures of maternal and child adversity and demographic variables.
Child age was significantly positively associated and child witnessed and direct adversity. Maternal age was not significantly associated with maternal preconception adversity. Income-to-FPL ratio was not significantly associated with any of the APCA variables. Further, Welch’s t-tests indicated that scores on the APCA variables did not differ based on maternal racial or ethnic identity or the child’s sex.
Associations Among Maternal Symptoms of Psychopathology, Child Behavioral and Emotional Problems, and Demographic Variables
Maternal symptoms of depression and anxiety were significantly positively correlated (Pearson’s r=.69, 95% CI[.56, .78]), and maternal age was significantly negatively associated with symptoms of anxiety (Pearson’s r=−.22, 95% CI[−.41, −.02]). Maternal symptoms of psychopathology were not associated with child age, family income-to-FPL ratio, maternal racial identity, maternal ethnic identity, or the child’s sex. Children’s emotional and behavioral problems were positively associated with maternal symptoms of psychopathology (depression: Pearson’s r=.30, 95% CI[.10, .47]; anxiety: r=.24, 95% CI[.04, .42]). Children’s problems were not associated with maternal age, child age, family income-to-FPL ratio, maternal racial or ethnic identity, or the child’s sex.
Convergent Validity of the APCA
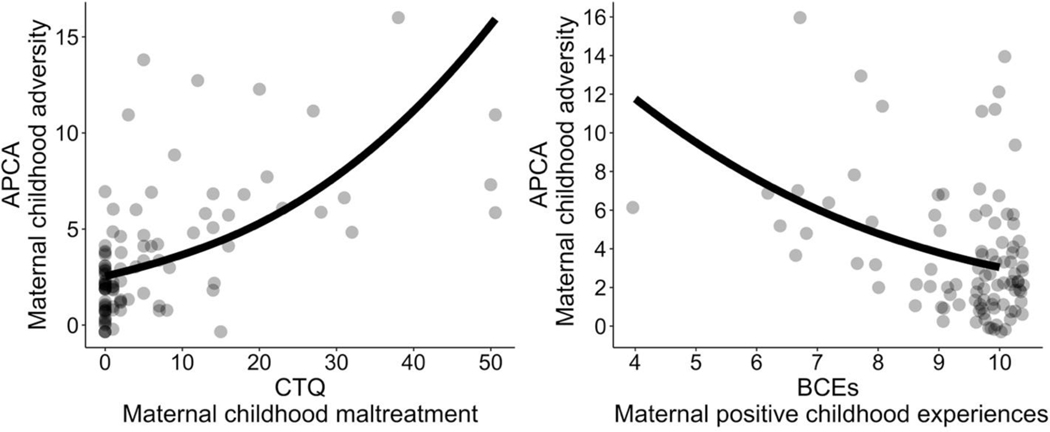
Maternal exposure to childhood maltreatment, measured by the CTQ, was strongly positively associated with maternal childhood adversity measured by the APCA (Spearman’s 𝜌=.58, 95% CI[.43, .70], BF= 26,759,799.28). Mothers who reported exposure to more severe maltreatment in childhood reported exposure to a higher number of adverse experiences during childhood on the APCA. Based on the results of a negative binomial regression, we identified an incidence rate ratio of 1.04 (95% CI[1.02, 1.05], Nagelkerke’s R2=.41) for the association of maternal childhood maltreatment measured by the CTQ with maternal childhood adversity measured by the APCA. We depict the predicted counts of maternal childhood adversity based on CTQ scores in Figure 2.
Figure 2. Association of maternal childhood adversity assessed by the APCA with other measures of maternal childhood maltreatment and positive childhood experiences.
Left panel depicts association with total scores on the Childhood Trauma Questionnaire – Short Form (CTQ; Bernstein et al., 2003). Right panel depicts association with total scores on the Benevolent Childhood Experiences (BCEs) scale (Narayan et al., 2018). Points are raw observed values and lines are the predicted associations from negative binomial regression models.
Maternal responses to the DQAQ-SPF were positively associated with maternal childhood adversity and maternal preconception adversity measured by the APCA (childhood: Spearman’s 𝜌=.29, 95% CI[.08, .48], BF=6.33; preconception: Spearman’s 𝜌=.28, 95% CI[.06, .47], BF=31.64). Mothers who reported more lifetime adversity 3–5 years earlier reported on the APCA that they were exposed to more adverse experiences during childhood and prior to pregnancy. Based on the results of negative binomial regression models, we identified incidence rate ratios of 1.14 (95% CI[1.03, 1.29], Nagelkerke’s R2=.11) and 1.16 (95% CI[1.04, 1.33], Nagelkerke’s R2=.12) for the respective associations of maternal lifetime adversity reported 3–5 years earlier with maternal childhood adversity and with preconception adversity reported on the APCA.
Criterion Validity
Maternal Positive Childhood Experiences
Maternal childhood adversity was negatively associated with maternal positive childhood experiences, measured by the BCEs scale (Spearman’s 𝜌=−.31, 95% CI[−.48 −.12], BF=46.88). Mothers who reported having fewer positive experiences in childhood reported being exposed to a higher number of adverse experiences in childhood on the APCA. A negative binomial regression of maternal childhood adversity on the number of childhood experiences measured by BCEs scale yielded an incident rate ratio of 0.80 (95% CI [0.69, 0.92]; Nagelkerke’s R2=.15). We depict the predicted counts of maternal childhood adversity based on BCEs scores in Figure 2.
Maternal Symptoms of Psychopathology
In the Supplementary Material, we depict the unadjusted associations of maternal adversity during each life period measured by the APCA with maternal symptoms of depression and anxiety, and present additional statistics for associations between maternal adversity during each life stage and maternal symptoms.
Maternal cumulative adversity was significantly positively associated with maternal symptoms of depression (Spearman’s 𝜌=.28, 95% CI[.09, .46], BF=14.22). Maternal childhood adversity was not significantly associated with mothers’ current symptoms of depression (Spearman’s 𝜌=.13, 95% CI[−.07, .32]), but maternal adversity in every other life stage was significantly positively associated with symptoms of depression (preconception: Spearman’s 𝜌=.28, 95% CI[.08, .45]; prenatal: 𝜌=.20, 95% CI[<.01, .39]; since birth: 𝜌=.26, 95% CI[.07, .44). Based on Bayes factors, evidence was strongest for the association of maternal depressive symptoms with maternal adversity since the child’s birth (BF=16.81, strong evidence). In an OLS regression in which the measures of maternal adversity in childhood, prior to conception, prenatally, and since birth were entered together as statistical predictors of maternal depressive symptoms, maternal preconception adversity and maternal adversity since the child’s birth remained significantly associated with depressive symptoms whereas associations with maternal childhood and prenatal adversity were not significant (see Supplementary Material). Collectively, measures of maternal adversity explained 16% of the variance in mothers’ depressive symptoms.
Maternal cumulative adversity was also significantly positively associated with maternal symptoms of anxiety (Spearman’s 𝜌=.31, 95% CI[.12, .48], BF=358.49). Maternal adversity in every life period was significantly positively associated with maternal symptoms of anxiety (childhood: Spearman’s 𝜌=.36, 95% CI[.17, .52]; preconception: 𝜌=.23, 95% CI[.03, .41]; prenatal: 𝜌=.23, 95% CI[.03, .41]; since birth: 𝜌=.29, 95% CI[.10, .46). Based on Bayes factors, evidence was strongest for the association of maternal symptoms of anxiety with maternal childhood adversity (BF=3,285.77, extreme evidence). In an OLS regression in which all measures of maternal adversity were entered together as statistical predictors of maternal anxiety symptoms, only maternal childhood adversity remained significantly associated with maternal anxiety symptoms whereas adversity during other life periods was not (see Supplementary Material). Collectively, measures of maternal adversity explained 24% of the variance in mothers’ anxiety symptoms.
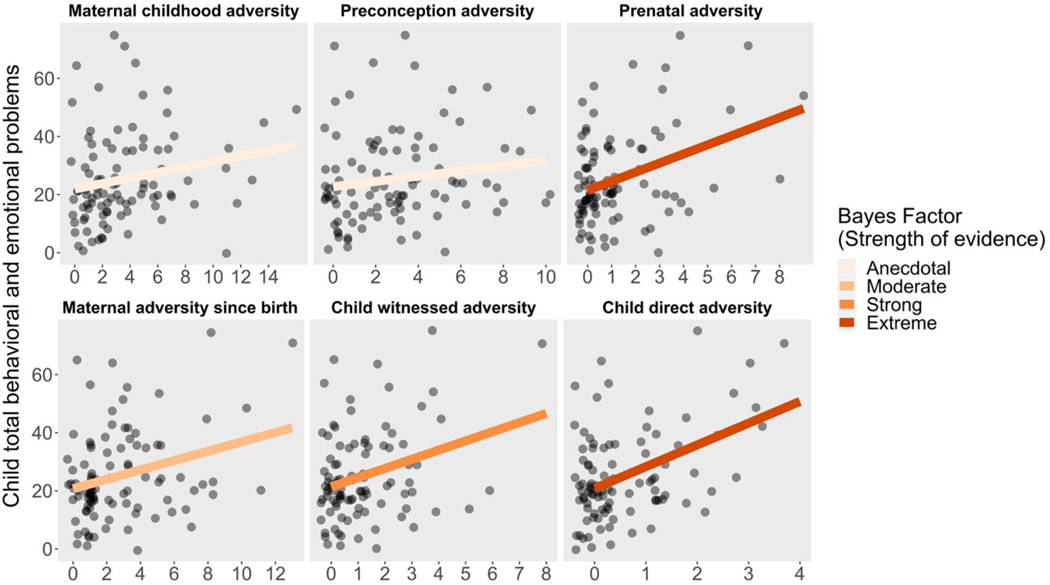
Child emotional and behavioral problems
Maternal cumulative adversity was significantly positively associated with children’s emotional and behavioral problems (Spearman’s 𝜌=.36, 95% CI[.18, .53], BF=41.99), as were maternal childhood adversity and prenatal adversity (childhood: Spearman’s 𝜌=.27, 95% CI[.07, .44]; prenatal: 𝜌=.24, 95% CI[.04, .42]). Maternal preconception adversity was not significantly associated with children’s emotional and behavioral problems (Spearman’s 𝜌=.19, 95% CI[−.01, .38]). The number of maternal adverse experiences that had occurred since the child’s birth was significantly positively associated with children’s emotional and behavioral problems (Spearman’s 𝜌=.21, 95% CI[.01, .40]), but the number of adverse experiences that the mother reported the child had witnessed was not (Spearman’s 𝜌=.19, 95% CI[−.01, .39]). Child direct exposure to adversity was positively associated with their emotional and behavioral problems (Spearman’s 𝜌=.30, 95% CI[.11, .47]). Based on the Bayes factors, evidence was strongest in favor of the association of children’s emotional and behavioral problems with child direct adversity (BF=3,453.77 extreme evidence), followed by prenatal adversity (BF=136.23, very strong evidence), child witnessed adversity (BF=16.73, strong evidence), adversity since the child’s birth (BF=8.47, moderate evidence), maternal childhood adversity (BF=1.47, anecdotal evidence), and preconception adversity (BF=0.66, anecdotal evidence in favor of the null hypothesis).
We conducted separate OLS regression models to examine the associations of maternal adversity during different life stages and child witnessed and direct adversity with children’s emotional and behavioral problems when adjusting for maternal symptoms of depression and anxiety. In the first model, in which we entered all measures of maternal adversity together as statistical predictors of children’s emotional and behavioral problems, only prenatal adversity remained significantly positively associated with children’s problems above and beyond maternal adversity in other life stages and maternal symptoms of psychopathology (B=5.03, 𝛽=0.32, SE=2.13, 95%CI[0.80, 9.25], t(88)=2.36, p=.020). Maternal adversity during other life periods was not significantly associated with children’s emotional and behavioral problems (childhood: B=0.39, 𝛽=0.08, SE=0.64, 95% CI[−0.88, 1.66], t(88)=0.61, p=.544); preconception: B=-<0.01, 𝛽=<0.01, SE=0.71, 95% CI[−1.41, 1.41], t(88)=-<0.01, p=.997; since birth: B=−0.32, 𝛽=−0.02, SE=2.22, 95% CI[−4.73, 4.09], t(88)=−0.14, p=.887). Collectively, measures of maternal adversity explained 5% of the variance in children’s emotional and behavioral problems.
In the second model, in which we entered child witnessed and direct adversity together as statistical predictors of children’s emotional and behavioral problems, child direct adversity remained significantly positively associated with children’s problems above and beyond maternal symptoms of psychopathology (B=5.26, 𝛽=0.34, SE=1.70, 95%CI[1.88, 8.63], t(90)=3.09, p=.003) whereas child witnessed adversity was not significantly associated with children’s problems (B=1.74, 𝛽=0.11, SE=1.67, 95%CI[−1.58, 5.05], t(90)=1.04, p=.300). Collectively, measures of child adversity explained 12% of the variance in children’s emotional and behavioral problems.
Discussion
In this study, we introduced and provided preliminary validation data for a novel measure of adversity, the APCA, in a sample of mothers and their 3- to 5-year-old children. Based on the formulation that the parent–child relationship is unique in the extent to which experiences of the world and the consequences of these experiences are shared dyadically, we developed the APCA to allow for the simultaneous assessment of both the parent’s and the focal child’s exposure to adversity. Overall, our findings indicated that the APCA has convergent and criterion validity. Leveraging the ability of the APCA to distinguish between adversity occurring during different life stages and originating from different sources, our findings also highlighted potentially distinct effects of different aspects of maternal and child adversity on maternal and child mental health difficulties.
Descriptively, at least one mother in our sample endorsed exposure to each of the 40 types of adversity we assessed, with many mothers reporting experiences viewed as objectively severe (e.g., 42% reported sexual assault). For most types of maternal adversity, at least one mother reported that the adversity had occurred within the child’s lifetime and that the child had seen, heard, or heard about the adversity. Reporting of child direct adversity was generally low. However, children whose mothers experienced greater adversity prior to the child’s birth, including during the mother’s own childhood, in adulthood prior to conception, and during pregnancy, were more likely to experience greater direct adversity. These findings support the formulation that young children share the adverse experiences of their parents. Further, they reflect those of prior research indicating that there is a “cycle” of adversity across generations (Madigan et al., 2019)
Maternal exposure to adversity during childhood assessed by the APCA demonstrated convergent validity with another commonly used measured of childhood adversity, the CTQ (Bernstein et al., 2003). For each 1-point increase in the CTQ total score, the estimated number of maternal childhood adverse experiences reported on the APCA increased by 3%. Mothers’ reports on the APCA converged with their responses to a checklist of a limited number of adverse life events administered years earlier, when they were in their first trimester of pregnancy with the focal child. Demonstrating criterion validity, maternal childhood adversity assessed by the APCA was negatively associated with a measure of positive childhood experiences, the BCEs scale (Narayan et al., 2018). Specifically, for each additional positive childhood experience mothers reported on the BCEs scale, the estimated number of maternal childhood adverse experiences reported on the APCA decreased by 20%.
Measures of maternal adversity derived from the APCA also demonstrated criterion with mothers’ self-reported symptoms of depression and anxiety. Although prospective assessments of adversity are ideal for testing sensitive period models (Gabard-Durnam & McLaughlin, 2019), our results suggested developmental timing effects of maternal adversity on symptoms of psychopathology that differed based on the dimension of psychopathology. Specifically, above and beyond adversity during other life stages, more recent maternal adversity occurring since the child’s birth remained significantly associated with mothers’ current depressive symptoms and this association was largest in magnitude. In contrast, above and beyond adversity during later life stages, maternal adversity in childhood remained significantly associated with mothers’ current symptoms of anxiety and had the largest effect size. Findings have been mixed regarding whether the impact of adversity on adult psychopathology depends on its developmental timing, and, if so, when in development adversity is most impactful (Dunn et al., 2017, 2018; Kuhn et al., 2016). Further, these timing effects may depend on the current life stage of the sample. For example, it is possible that childhood adversity is more strongly associated with anxiety during the childbearing years because early adverse experiences invoke stress related to caregiving (so called “ghosts in the nursery”; Fraiberg et al., 1975).
The APCA also demonstrated criterion validity with children’s emotional and behavioral problems. Children whose mothers had been exposed to greater adversity and who had been directly exposed to greater adversity had more emotional and behavioral problems even after controlling for maternal symptoms of psychopathology. Once again, when we explored associations of children’s problems with maternal adversity during different life periods, our findings suggested developmental timing effects. Above and beyond maternal adversity during other life periods, including since the child’s birth, maternal adversity during pregnancy with the focal child remained significantly associated with children’s emotional and behavioral problems and had the largest effect size. Although limited research has compared effects of maternal adversity during different life periods on children’s risk for psychopathology, research examining prenatal “programming” of health and disease suggests that adversity during pregnancy increases offspring’s vulnerability to psychopathology through effects on fetal development (Entringer et al., 2015; Humphreys et al., 2020). Collectively, however, measures of child adversity explained greater variance in children’s problems than did maternal adversity. Despite limited reporting of child direct adversity, children’s direct experiences of adversity remained significantly associated with their emotional and behavioral problems when adjusting for their experiences of seeing, hearing, or hearing about maternal adverse experiences, which were not significantly associated with their problems. In future research with larger samples, the APCA may be used to test hypotheses regarding interactions between prenatal adversity and child direct adversity, including whether prenatal exposure increases vulnerability to direct exposure postnatally (Daskalakis et al., 2013).
Limitations of the current study include the cross-sectional design, the relatively small sample size, limitations due to sample diversity, and reliance on maternal report. For these reasons, and because it is advised that novel assessment instruments be tested in multiple samples and that validation is an ongoing process (Clark & Watson, 2019), the current validation should be considered preliminary. Because our analyses were cross-sectional, future research is needed to determine whether APCA measures of adversity predict children’s developmental trajectories of functioning, including their mental health difficulties. Relatedly, although the APCA converged with another measure of adversity administered years earlier, we do not have information about the test-retest reliability of the APCA. Although we were well-powered to detect the effect sizes of interest, our sample size of 97 mothers from the San Francisco Bay Area limits the generalizability of our findings, and additional research is necessary to examine the validity of the APCA in larger samples with different backgrounds and in different geographic areas. In particular, in our sample mothers were highly educated and there were few Black mothers; mothers with other educational backgrounds and mothers who are Black may report different experiences that are associated differently with external measures. It is possible that in higher risk samples associations with theoretically relevant constructs like symptoms of psychopathology would be stronger because these samples would better represent individuals with the most adverse environments and the most severe psychosocial problems. All the measures included in the current study were obtained through maternal report, possibly introducing common method variance. Nonetheless, we found that maternal and child adversity measured by the APCA were associated with children’s emotional and behavioral problems above and beyond mothers’ reports of their symptoms of depression and anxiety, suggesting that effects of adversity were distinct from the method of measurement.
Finally, the current study used a “cumulative risk” approach to quantify adversity, counting the number of types of adverse experiences to which caregivers and children were exposed (Evans et al., 2013). Limitations to this approach include that it weights equally experiences that may differ from each other in severity and chronicity and combines different types of experiences that may have distinct psychobiological consequences (McLaughlin et al., 2021). Future research with the APCA may consider alternative frameworks, including weighting counts by the subjective severity or frequency of experiences or separating items based on theoretical frameworks that propose distinct dimensions of adversity (McLaughlin & Sheridan, 2016).
The APCA allows the simultaneous assessment of parent and child adversity, and efficiently captures extensive information about parent and child adversity. The present data highlight the validity of the APCA and indicate that it is robustly associated with mothers’ reports of their and their young children’s symptoms of psychopathology. Although scientists have long recognized that adverse experiences of parents and their children are intertwined, the APCA addresses a gap in methods to assess adversity at the level of the parent–child dyad. This novel measure, which is openly accessible, will help researchers to parse important aspects of experiences in order to answer fundamental questions about how the nature of the early environment influences children’s development. With additional research, the APCA may be clinically useful in evaluating children’s risk for psychological difficulties associated with adversity and/or for understanding the etiology of children’s current difficulties. The APCA may be especially useful in treatments that are delivered at the level of the parent–child dyad, providing an initial means to identify parents’ and children’s adverse experiences that can be processed in detail with the therapist. For example, Child–Parent Psychotherapy (CPP) addresses adverse experiences such as intimate partner violence that can lead to trauma symptoms in both parents and children (Lieberman et al., 2015). In this context, a comprehensive history of both the caregiver’s and the child’s exposure to adversity may help guide the therapist to support the child in sharing their story and to support the caregiver in processing their own exposure. Because caregiver and child adversity may affect caregiving behavior and attachment (Baer & Martinez, 2006; Savage et al., 2019), the APCA may be useful for evaluation in any intervention focused on enhancing the caregiver–child relationship.
Supplementary Material
Figure 3. Associations of maternal and child adversity with child total emotional and behavioral problems.
Maternal childhood adversity, preconception adversity, prenatal adversity, and adversity since birth are measures of maternal adversity during different life stages. Points are raw observed values and lines are regression lines of best fit. Bayes Factor indicates strength of the evidence in favor of the alternative hypothesis that the association is non-zero: BFs 1–3=anecdotal evidence, ≥3 and <10=moderate evidence, ≥10 and <30=strong evidence, ≥30 and <100=very strong evidence, and ≥100=extreme evidence (Quintana & Williams, 2018).
Acknowledgements
Funding was provided by the Stanford Maternal & Child Health Research Institute (IHG, Transdisciplinary Initiatives Program), the Jacobs Foundation (KLH, Early Career Research Fellowship 2017–1261-05), the Stanford Institute for Research in the Social Sciences (LSK, Dissertation Fellowship), Bill and Melinda Gates Foundation (GMS, DKS), the March of Dimes Prematurity Research Center at Stanford University (GMS, DKS), the Christopher Hess Research Fund (DKS), the Charles B. and Ann L. Johnson Endowed Fund (DKS), the Prematurity Research Fund (DKS), and the National Institute of Child Health and Human Development (LSK, F32HD105385). We thank David Cole for his feedback on the statistical analysis plan for this paper. We thank Ana Campos, Jonas Miller, Daisy Feddoes, Jillian Segarra, and Ronald Wong for their assistance in recruitment, project management, and data collection, as well as the families who participated in this research.
Footnotes
Data Availability Statement
Data are available at https://github.com/lucysking/MoD/tree/master/king_APCA_validation.
References
- Achenbach TM, & Rescorla LA (2000). Manual for the ASEBA Preschool Forms & Profiles. University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- American Psychiatric Association (institution). (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) (5th ed.). American Psychiatric Publishing. [Google Scholar]
- Atkins R. (2014). Validation of the center for epidemiologic studies depression scale in black single mothers. Journal of Nursing Measurement, 22(3), 511–524. 10.1891/1061-3749.22.3.511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, & Steer RA (1993). Beck Anxiety Inventory Manual. Psychological Corporation. [Google Scholar]
- Becker M, Mayo ÃJA, Phogat ÃNK, Quaintance MSCC, Laborde A, King BAL, Gotlib BAIH, Gaudilliere B, Angst MS, Shaw GM, Stevenson DK, Aghaeepour N, & Dhabhar FS (2021). Deleterious and Protective Psychosocial and Stress-Related Factors Predict Risk of Spontaneous Preterm Birth. American Journal of Perinatology, 33136. [DOI] [PMC free article] [PubMed]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, & Zule W. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. 10.1016/S0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Berry C, Quinn K, Shalowitz M, & Wolf R. (2001). Validation of the Crisis in Family Systems–Revised, a contemporary measure of life stressors. Psychological Reports, 88(3), 713–724. 10.2466/pr0.2001.88.3.713 [DOI] [PubMed] [Google Scholar]
- Bowers ME, & Yehuda R. (2016). Intergenerational transmission of stress in humans. Neuropsychopharmacology, 41(1), 232–244. 10.1038/npp.2015.247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2019). Creating safe, stable, nurturing relationships and environments for all children. https://www.cdc.gov/violenceprevention/pdf/essentials-for-childhood-framework508.pdf
- Clark LA, & Watson D. (2019). Constructing validity: New developments in creating objective measuring instruments. Psychological Assessment, 31(12), 1412–1427. 10.1037/pas0000626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collishaw S, Dunn J, O’Connor TG, Golding J, & Avon Longitudinal Study of Parents and Children Study Team. (2007). Maternal childhood abuse and offspring adjustment over time. Development and Psychopathology, 19(02), 367–383. 10.1017/S0954579407070186 [DOI] [PubMed] [Google Scholar]
- Daskalakis NP, Bagot RC, Parker KJ, Vinkers CH, & Kloet E. R. de. (2013). The three-hit concept of vulnerability and resilience: towards understanding adaptation to early-life adversity outcome. Psychoneuroendocrinology, 38(9), 1858–1873. 10.1016/j.psyneuen.2013.06.008.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, Nishimi K, Gomez SH, Powers A, & Bradley B. (2018). Developmental timing of trauma exposure and emotion dysregulation in adulthood: Are there sensitive periods when trauma is most harmful? Journal of Affective Disorders, 227(August 2017), 869–877. 10.1016/j.jad.2017.10.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, Nishimi K, Powers A, & Bradley B. (2017). Is developmental timing of trauma exposure associated with depressive and post-traumatic stress disorder symptoms in adulthood? Journal of Psychiatric Research, 84, 119–127. 10.1016/j.jpsychires.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entringer S, Buss C, & Wadhwa PD (2015). Prenatal stress, development, health and disease risk: A psychobiological perspective. Psychoneuroendocrinology, 62, 366–375. 10.1016/j.psyneuen.2015.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Li D, & Whipple SS (2013). Cumulative risk and child development. Psychological Bulletin, 139(6), 1342–1396. 10.1037/a0031808 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Ford JD, Racusin R, Rogers K, Ellis C, Schiffman J, Ribbe D, & Edwards J. (2002). Traumatic Events Screening Inventory for Children (TESI-C). National Center for PTSD and Dartmouth Child Psychiatry Research Group. [Google Scholar]
- Fraiberg S, Adelson E, & Shapiro V. (1975). Ghosts in the nursery: A psychoanalytic approach to the problem of impaired infant-mother relationships. Journal of the American Academy of Child and Adolescent Psychiatry, 14, 387–422. 10.1016/S0002-7138(09)61442-4 [DOI] [PubMed] [Google Scholar]
- Fuchs A, Möhler E, Resch F, & Kaess M. (2015). Impact of a maternal history of childhood abuse on the development of mother–infant interaction during the first year of life. Child Abuse & Neglect, 48, 179–189. 10.1016/j.chiabu.2015.05.023 [DOI] [PubMed] [Google Scholar]
- Gabard-Durnam L, & McLaughlin KA (2019). Do sensitive periods exist for exposure to adversity? Biological Psychiatry, 85(10), 789–791. 10.1016/j.biopsych.2019.03.975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabard-Durnam L, & McLaughlin KA (2020). Sensitive periods in human development: Charting a course for the future. Current Opinion in Behavioral Sciences, 36, 120–128. 10.1016/j.cobeha.2020.09.003 [DOI] [Google Scholar]
- Gelman A, & Hill J. (2007). Data Analysis Using Regression and Multilevel/Hierarchical Models. Cambridge University Press. [Google Scholar]
- Ghaemi MS, DiGiulio DB, Contrepois K, Callahan B, Ngo TTM, Lee-Mcmullen B, Lehallier B, Robaczewska A, McIlwain D, Rosenberg-Hasson Y, Wong RJ, Quaintance C, Culos A, Stanley N, Tanada A, Tsai A, Gaudilliere D, Ganio E, Han X, … Aghaeepour N. (2019). Multiomics modeling of the immunome, transcriptome, microbiome, proteome and metabolome adaptations during human pregnancy. Bioinformatics, 35(1), 95–103. 10.1093/bioinformatics/bty537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, Mclaughlin K. a, Berglund P. a, Gruber MJ, Sampson N. a, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I. Archives of General Psychiatry, 67(2), 113–123. 10.1001/archgenpsychiatry.2009.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness KL, & Monroe SM (2016). The assessment and measurement of adult life stress: Basic premises, operational principles, and design requirements. Journal of Abnormal Psychology, 125(5), 727–745. 10.1037/abn0000178 [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzales N, & Conde JG (2009). Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics suppor. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Camacho MC, Roth MC, & Estes EC (2020). Prenatal stress exposure and multimodal assessment of amygdala–medial prefrontal cortex connectivity in infants. Developmental Cognitive Neuroscience, 46, 100877. 10.1016/j.dcn.2020.100877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, & Zeanah CH (2015). Deviations from the expectable environment in early childhood and emerging psychopathology. Neuropsychopharmacology, 40(1), 154–170. 10.1038/npp.2014.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ippen CG, Ford J, Racusin R, Acker M, Bosquet K, Ellis C, Schiffman J, Ribbe D, Cone P, Lukovitz M, & Edwards J. (2002). Traumatic Events Screening Inventory - Parent Report Revised. National Center for PTSD and Dartmouth Child Psychiatry Research Group. [Google Scholar]
- Ivanova MY, Achenbach TM, Rescorla LA, Harder VS, Ang RP, Bilenberg N, Bjarnadottir G, Capron C, De Pauw SSW, Dias P, Dobrean A, Doepfner M, Duyme M, Eapen V, Erol N, Esmaeili EM, Ezpeleta L, Frigerio A, Gonalves MM, … Verhulst FC (2010). Preschool psychopathology reported by parents in 23 societies: Testing the seven-syndrome model of the child behavior checklist for ages 1.5–5. Journal of the American Academy of Child and Adolescent Psychiatry, 49(12), 1215–1224. 10.1016/j.jaac.2010.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LS (2019). The Assessment of Parent and Child Adversity (APCA). https://osf.io/tgmpz/ [DOI] [PMC free article] [PubMed]
- King LS, Salo VC, Kujawa A, & Humphreys KL (2021). Advancing the RDoC initiative through the assessment of caregiver social processes. Development and Psychopathology, in press. [DOI] [PMC free article] [PubMed]
- Kleinhaus K, Harlap S, Perrin M, Manor O, Margalit-Calderon R, Opler M, Friedlander Y, & Malaspina D. (2013). Prenatal stress and affective disorders in a population birth cohort. Bipolar Disorders, 15(1), 92–99. 10.1111/bdi.12015 [DOI] [PubMed] [Google Scholar]
- Kuhn M, Scharfenort R, Schümann D, Schiele MA, Münsterkötter AL, Deckert J, Domschke K, Haaker J, Kalisch R, Pauli P, Reif A, Romanos M, Zwanzger P, & Lonsdorf TB (2016). Mismatch or allostatic load? Timing of life adversity differentially shapes gray matter volume and anxious temperament. Social Cognitive and Affective Neuroscience, 11(4), 537–547. 10.1093/scan/nsv137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeMoult J, Humphreys KL, Tracy A, Hoffmeister JA, Ip E, & Gotlib IH (2020). Meta-analysis: Exposure to early life stress and risk for depression in childhood and adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 59(7), 842–855. 10.1016/j.jaac.2019.10.011 [DOI] [PubMed] [Google Scholar]
- Lewinsohn P, Seeley JR, Roberts RE, & Allen NB (1997). Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychology and Aging, 12(2), 277–287. [DOI] [PubMed] [Google Scholar]
- Lüdecke D, Waggoner PD, & Makowski D. (2019). insight: A Unified Interface to Access Information from Model Objects in R. Journal of Open Source Software, 4, 1412. 10.21105/joss.01412 [DOI] [Google Scholar]
- Lüdecke Daniel, Makowski D, Waggoner P, & Patil I. (2020). performance: Assessment of regression models performance. CRAN Repository. 10.5281/zenodo.3952174 [DOI] [Google Scholar]
- Madigan S, Cyr C, Eirich R, Fearon RMP, Ly A, Rash C, Poole JC, & Alink LRA (2019). Testing the cycle of maltreatment hypothesis: Meta-analytic evidence of the intergenerational transmission of child maltreatment. Development and Psychopathology, 31, 23–51. 10.1017/S0954579418001700 [DOI] [PubMed] [Google Scholar]
- May CL, & Wisco BE (2016). Defining Trauma: How level of exposure and proximity affect risk for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 8(2), 233–240. http://web.a.ebscohost.com.proxy.lib.sfu.ca/ehost/pdfviewer/pdfviewer?vid=10&sid=8f792acd-5543-4174-a35b-4ed31dbb1490%40sessionmgr4009 [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, Humphreys KL, Belsky J, & Ellis BJ (2021). The value of dimensional models of early experience: Thinking clearly about concepts and categories. Perspectives on Psychological Science, December. 10.1177/1745691621992346 [DOI] [PMC free article] [PubMed]
- McLaughlin KA, Sheridan MA, & Lambert HK (2014). Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience and Biobehavioral Reviews, 47, 578–591. 10.1016/j.neubiorev.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrick JS, Narayan AJ, DePasquale CE, & Masten AS (2019). Benevolent Childhood Experiences (BCEs) in homeless parents: A validation and replication study. Journal of Family Psychology, 33(4), 493–498. 10.1037/fam0000521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey RD (2019). Computation of Bayes factors for common designs [R package BayesFactor version 0.9.12–4.2]. CRAN Repository. https://cran.r-project.org/web/packages/BayesFactor/index.html [Google Scholar]
- Narayan AJ, Lieberman AF, & Masten AS (2021). Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clinical Psychology Review, 85(November 2020), 101997. 10.1016/j.cpr.2021.101997 [DOI] [PubMed] [Google Scholar]
- Narayan AJ, Rivera LM, Bernstein RE, Harris WW, & Lieberman AF (2018). Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse & Neglect, 17, 19–30. 10.1016/J.CHIABU.2017.09.022 [DOI] [PubMed] [Google Scholar]
- Nelson CA, & Gabard-Durnam LJ (2020). Early adversity and critical periods: Neurodevelopmental consequences of violating the expectable environment. Trends in Neurosciences, 43(3), 133–143. 10.1016/j.tins.2020.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orme JG, Reis J, & Herz EJ (1984). Factorial and discriminant validity of the Center for Epidemiological Studies Depression (CES-D) scale. Journal of Clinical Psychology, 42(1), 28–33. [DOI] [PubMed] [Google Scholar]
- Osman A, Barrios FX, Aukes D, Osman JR, & Markway K. (1993). The Beck Anxiety Inventory: Psychometric properties in a community population. Journal of Psychopathology and Behavioral Assessment, 15(4), 287–297. 10.1007/BF00965034 [DOI] [Google Scholar]
- Quintana DS, & Williams DR (2018). Bayesian alternatives for common null-hypothesis significance tests in psychiatry: A non-technical guide using JASP. BMC Psychiatry, 18–178. 10.1186/s12888-018-1761-4 [DOI] [PMC free article] [PubMed]
- R Core Team. (2021). R: A language and environment for statistical computing. (4.0.0). R Foundation for Statistical Computing. https://www.r-project.org/ [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Journal of Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Roubinov DS, Luecken LJ, Curci SG, Somers JA, & Winstone LK (2021). A prenatal programming perspective on the intergenerational transmission of maternal adverse childhood experiences to offspring health problems. The American Psychologist, 76(2), 337–349. 10.1037/amp0000762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterba S, Egger HL, & Angold A. (2007). Diagnostic specificity and nonspecificity in the dimensions of preschool psychopathology. Journal of Child Psychology and Psychiatry and Allied Disciplines, 48(10), 1005–1013. 10.1111/j.1469-7610.2007.01770.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Williams K, Thomas PA, Liu H, & Thomeer MB (2014). Race, gender, and chains of disadvantage: Childhood adversity, social relationships, and health. Journal of Health and Social Behavior, 55(1), 20–38. 10.1177/0022146514521426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venables W, & Ripley B. (2002). Modern applied statistics with S. (Fourth). Springer. http://www.stats.ox.ac.uk/pub/MASS4 [Google Scholar]
- Waters SF, West TV, & Mendes WB (2014). Stress contagion: physiological covariation between mothers and infants. Psychological Science, 25(4), 934–942. 10.1177/0956797613518352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise PH, Shaw GM, Druzin ML, Darmstadt GL, Quaintance C, Mäkinen E, Relman DA, Quake SR, Butte AJ, Angst MS, Muglia LJ, Macones G, Driscoll D, Ober C, Simpson JL, Katz M, Howse J, & Stevenson DK (2017). Risky Business: Meeting the Structural Needs of Transdisciplinary Science. Journal of Pediatrics, 191, 255–258. 10.1016/j.jpeds.2017.08.072 [DOI] [PubMed] [Google Scholar]
- Wolfe J, Kimerling R, Brown PJ, Chrestman KR, & Levin K. (1996). Psychometric review of the Life Stressor Checklist-Revised. Measurement of Stress, Trauma, and Adaptation, 198–201.
- Zero to Three. (2016). DC:0–5: Diagnostic Classification of Mental Health and Developental Disorders of Infancy and Early Childhood.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.