Abstract
Objective
Both‐column acetabular fracture is a type that accumulates both the pelvis and acetabulum with complex fracture line alignment and has variant fracture fragments. The selection of different reduction landmarks and sequences produces different qualities of reduction. This study aims to compare the operation‐related items, quality of reduction, and hip functional outcome by using different reduction landmarks and sequences for management of both‐column acetabular fractures (BCAF).
Methods
A consecutive cohort of 42 patients from January 2013 to January 2019 with BCAF were treated operatively with different reduction landmarks and sequences: pelvic ring fractures reduction first (PRFRF group) and acetabular fractures reduction first (AFRF group). Preoperative computer visual surgical procedures were applied. There were 22 patients in PRFRF group and 20 patients in AFRF group. The surgical details, complications, radiographic and clinical results were recorded. The quality of reduction was assessed by the Matta scoring system. The functional outcome was evaluated by the modified Merle d'Aubigné and Postel scoring system. The measurement data were analyzed using the t‐test of independent samples and rank‐sum test of ranked data.
Results
The real reduction sequence in both groups was almost identical to the preoperative surgical procedures. The excellent/good quality of reduction in PRFRF group (21/22) was better than AFRF group (17/20). Operative time (152.3 ± 16.3 mins) and intra‐operative blood loss (639.5 ± 109.9ml) were significantly reduced in PRFRF group (p < 0.05). The incidence of deep vein thrombosis in PRFRF group (2/22) was less than AFRF group (4/20), but without statistical signification.
Conclusion
Selection of an appropriate reduction landmark and sequence could result in better quality of reduction, operative time, and decreased blood loss during treatment of BCAF.
Keywords: acetabular fractures, both‐column, computer simulation, foundation, reduction
Selection of an appropriate reduction landmark and sequence could improve surgical efficiency.
Introduction
Both‐column acetabular fractures (BCAF) are the second most frequent type of acetabular fracture with an incidence of 20% 1 , 2 . They are complex acetabular injuries involving multiple planes and characteristically present with separation of the entire acetabulum from the sacroiliac joint, resulting in a floating acetabulum 3 . Open reduction and internal fixation still remain the gold standard for the treatment of this type of injury 1 , 4 , 5 , besides, the prognosis of this injury is closely related to the quality of bone reduction 4 , 6 . It is challenging for surgeons to manage and the prognosis varies because the bone morphology of the pelvis is quite complex and can be displaced to any space in different directions for different fracture types 7 , 8 . Even for experienced surgeons, it can still take a long time to reposition, and the fracture position cannot be guaranteed. As you can imagine, less experienced surgeons will have to spend more time on the fracture reduction step.
BCAF are T‐ or Y‐shaped, formed by two fracture lines that converge on the acetabular roof, one from the greater sciatic notch and the other from the superior or anterior edge of the ilium, which then descend vertically together 3 , 9 . In other words, BCAF accumulate in both the acetabulum and the pelvis. Different acetabular fractures have different fracture line alignments, and the fracture lines of BCAF are especially complex. In this case, the normal acetabular anatomy has been severely destroyed, and it is exceptionally difficult to restore its continuity. Therefore, it is a challenge to effectively reduce this type of fracture.
Recently, some studies have applied computer visual technique for preoperative planning of the patient's imaging data for surgery 10 , 11 . This technique allows the surgeon to more easily identify the main fracture components and their spatial relationship to each other. The application of this technique in acetabular fractures has yielded relatively good clinical results 12 .
However, few studies have reported on the reduction sequence of complex acetabular fractures. Besides, complex acetabular fractures will result in variant fragments, how to select an appropriate reduction landmark was quite puzzling. Therefore, our team summarized and proposed a reduction method for the treatment of acetabular fractures involving both pelvis and acetabulum. A reduction landmark is selected and used as the basis for the reduction of the fractures using computer simulation before operation, followed by intra‐operative repositioning in a predesigned sequence.
The aims of this study were: (i) to propose a specific reduction landmark and sequence; and (ii) to identify the feasibility of clinical application.
Materials and Methods
Inclusion and Exclusion Criteria
Inclusion criteria were as follows: (i) patients suffering from closed BCAF as defined by Letournal classification.
Exclusion criteria were as follows: (i) delayed or open acetabular fractures; (ii) combined with femoral head fractures; (iii) patients with preoperative range of motion deficiency of the hip; (iv) age <18 years.
According to the above exclusion and inclusion criteria, 42 patients with BCAF treated in our hospital from January 2013 to January 2019 were selected and compared the operation‐related items, quality of repositioning, and functional recovery outcomes. PRFRF group used the “foundation” reduction method to firstly reduce the pelvic ring fractures, and AFRF group was treated with the acetabular fracture reductions first. The computer simulation was applied to the preoperative surgical visual procedures for each patient. The operative time, intra‐operative bleeding, quality of reduction, and postoperative functional recovery outcomes were collected for these patients. Each patient signed an informed consent form before operation and the study received approval from the institutional review board (S1060).
Preoperative Preparation
PRFRF Group
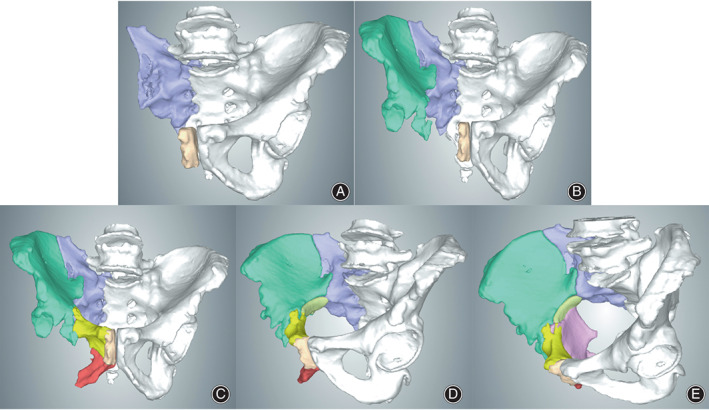
Computer‐Assisted Virtual Surgical Procedure
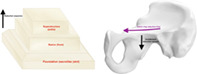
CT data from all patients were collected and stored in Dicom format, subsequently imported into 20.0 mimics software for 3D image reconstruction. Each fracture was labeled with different colors and converted into an individual object according to rotation and shift in different directions to simulate operative reduction. The sacroiliac joint was considered as the “foundation” of reduction, and the fractures were gradually reduced in the direction from the sacroiliac joint to the pubic symphysis (Fig. 1). The fractures located in quadrilateral surface were reduced last (Fig. 1).
Fig. 1.
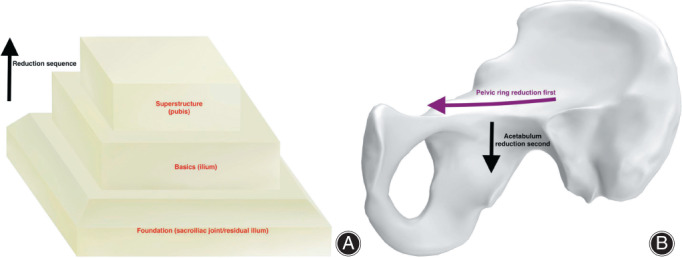
Diagram showing the reduction sequence of the “foundation” reduction method. (A) The origin of the “foundation” reduction method, which selected anatomical structure with larger contact area as a landmark to guide reduction. If the sacroiliac joint injury existed, the sacroiliac joint was selected as a foundation. If the sacroiliac joint injury was not existing, the residual ilium was selected as foundation. (B) The reduction sequence of BCAF.
Surgical Technique
In general, the patient is placed in supine position, and the approach of surgery can be selected according to the real location of acetabular fractures. Flat radiolucent operative table is used intra‐operatively to enable all intra‐operative pelvic position imaging to be acquired. The surgeon stands on the opposite side of the affected side. The supra‐ilioinguinal approach is selected as the anterior surgical approach and the exposure of different bone surface can be achieved according to constant window switching 13 . As planned preoperatively, a bony landmark is first selected as a reduction landmark. Generally, the sacroiliac joint is chosen as the landmark of the reduction and the extent of exposure is determined by the existing sacroiliac dislocation or the location of iliac fracture (Figure 2A). If there is a sacroiliac joint injury, the surgical exposure needs to be exposed to the surface of sacroiliac joint to facilitate placement of a plate in front of the sacroiliac joint. If there is no sacroiliac joint injury, the residual ilium attached to the ipsilateral sacroiliac joint is selected as the “foundation” for reduction. If the lines of iliac fractures were located at high location, the iliopsoas needs to be stripped for advanced reduction and fixation. Once the visualization of the individual fractures is achieved, the fractures can be gradually reduced in the direction from the sacroiliac joint to pubic symphysis using the pre‐selected bony landmark as the “foundation” and fixed with reconstruction plates (Figure 2‐B–D). If the medial displacement of quadrilateral surface exists, a quadrilateral buttress plate should be placed for fixation. After the reduction of all fractures are achieved, the active bleeding should be checked (Figure 2E). At last, a drainage tube is placed and the incision is closed layer by layer.
Fig. 2.
The steps of operation using the “foundation” reduction method. (A) The residual ilium was selected as a landmark for reduction. (B) The ilium was selected as a basics. (C) The pubis was selected as the superstructure. (D,E) The part of acetabulum was reduced at last.
AFRF Group
This group of patients also underwent preoperative computer simulation of visual surgical procedures but did not follow the “foundation” method for fracture reduction. The reduction sequence addressed the acetabular fracture first. Other preoperative preparations were the same with PRFRF group. The ilioinguinal approach was also selected as anterior surgical approach 13 .
Assessment Parameters
Based on radiographs in the anterior‐posterior and Judet positions and computed tomography scans of the pelvis, the quality of reduction was evaluated according to the scoring system published by Matta 14 : excellent (0–1 mm), good (2–3 mm), or poor (>3 mm). The final follow‐up clinical outcome was evaluated with the modified Merle d'Aubigné and Postel score to estimate the functional outcomes 15 . The sum of the individual scores (pain, gait, and range of motion of the hip) was classified as excellent (18 points), good (17–15 points), fair (15–13 points), or poor (<13 points).
Statistical Analysis
All data were processed and analyzed using SPSS (version 26.0; SPSS). The measurement data were analyzed using the t‐test of independent samples or paired samples, and the rest of ranked data were analyzed by the rank‐sum test. A value of p < 0.05 was considered as statistical significance.
Results
Follow‐Up
All patients were followed up at least for 1 year according to outpatient department or telephone at 1, 3, 6 months and 1 year postoperatively, and then annually thereafter.
General Results
A total of 42 cases were finally obtained according to the exclusion and inclusion criteria, of which 22 patients were treated according to the “foundation” method with pelvic ring fracture reduction first (PRFRF group) and 20 patients were treated with acetabular fractures reduction first (AFRF group). The mean age of PRFRF group was 47.1 ± 14.0 years and that of AFRF group was 41.7 ± 12.9 years. (Table.1) The male/female ratio was 14:8 for PRFRF group and 12:8 for AFRF group. The mean time from injury to operation was 8.5 ± 2.4 days in PRFRF group and 8.8 ± 4.8 days in AFRF group (Table 1). There was no statistically significant difference between the above relevant data, indicating that the comparability between PRFRF group and AFRF group was feasible (Figure 3).
Table 1.
Patient demographics of PRFRF and AFRF groups
| Variable | ORIF(n = 22) | ORIF(n = 20) |
|---|---|---|
| Age (year) | 47.1 ± 14.0 | 41.7 ± 12.9 |
| Gender (Male:Female) | 14:8 | 12:8 |
| Injury to operation (day) | 8.5 ± 2.4 | 8.8 ± 4.8 |
| Operative time (min) | 152.3 ± 16.3 | 183.0 ± 35.3 |
| Blood loss (ml) | 639.5 ± 109.9 | 793.9 ± 172.6 |
| Matta | ||
| Excellent | 16 | 13 |
| Good | 5 | 4 |
| Poor | 1 | 3 |
| Merle | ||
| Excellent | 10 | 9 |
| Good | 11 | 8 |
| Poor | 1 | 3 |
| Complication | ||
| Deep vein thrombosis | 2 | 4 |
| Infect | 1 | 3 |
Fig. 3.
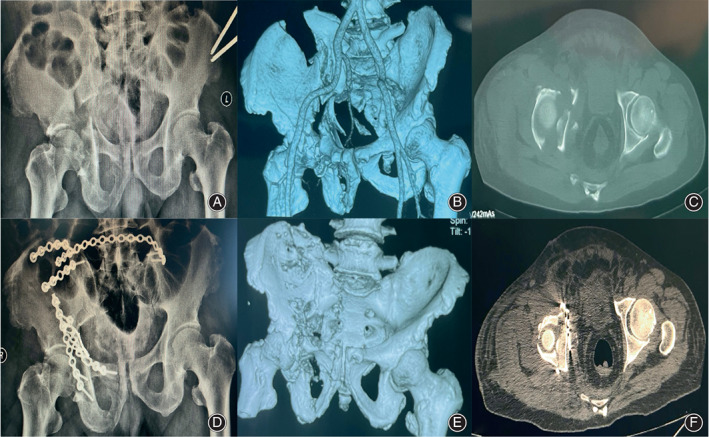
One case: a 56‐year‐old patient with BCAF. (A–C) Preoperative X‐ray, 3D reconstruction, and CT scan. (D–F) Postoperative X‐ray, 3D reconstruction, and CT scan.
Intra‐Operative Blood Loss
The mean intra‐operative blood loss was 639.5 ± 109.9ml in PRFRF group and 793.0 ± 172.6ml in AFRF group. It could be found that the intra‐operative blood loss in PRFRF group was less than that in AFRF group. There was a statistically significant difference between the two groups (p < 0.05).
Surgical Time
The mean operative time in PRFRF group (152.3 ± 16.3 mins) was less than that in AFRF group (183.0 ± 35.3 mins). There was a statistically significant difference between the two groups (p < 0.05).
Quality of Reduction
According to the Matta scoring system, 16 patients (72.7%) were scored excellent, five patients (22.7%) were scored good, and one patient (4.5%) was scored poor in PRFRF group. AFRF group had 13 patients (65.0%) with excellent level, four patients (20.0%) with good level, and three patients (15.0%) with poor level. The ratio of excellent/good in PRFRF group was 21/22, slightly higher than AFRF group (17/20).
Scoring of Hip Function
The patients' functional outcome was scored according to the Merle d'Aubigné scoring system. The ratio of excellent/good in PRFRF group was 21/22, slightly higher than AFRF group (17/20).
Complications
The incidence of deep vein thrombosis in PRFRF group was 2/22, which was less than AFRF group (4/20). The deep vein thrombosis was found at 3‐ and 6‐month follow‐ups, but no special treatment was performed. Wound superficial infection occurred in both groups at 1 week after surgery, 1/22 in PRFRF group, 3/20 in AFRF group. No reinfection occurred after debridement was performed in each patient.
Discussion
The management of complex acetabular fractures is very challenging for orthopaedic surgeons and often leads to serious complications such as femoral head necrosis and traumatic arthritis. In some long‐term follow‐up studies, traumatic arthritis was the most common complication with an incidence of 20% 2 , 16 . Especially, the quality of reduction is the only independent risk factor to evaluate the prognostic outcome 17 , 18 , 19 , 20 . Therefore, in the treatment of this type of fracture, it is necessary to ensure anatomic reduction of the fractures as much as possible. And in this study, it can also be found that AFRF group with relatively poor quality of reduction had a lower functional outcome compared to PRFRF group.
Importance of Selecting Appropriate Reduction Landmark and Sequence
The technique and sequence of BCAF reduction can improve the quality of the reduction. For the treatment of unstable pelvic ring fractures, fixation of the posterior ring was particularly important and was often treated preferentially 21 , 22 . However, BCAF involved both fractures of pelvis ring and acetabulum, but is pelvic ring reduction first or acetabulum? Pierannunzii et al. 3 indicated a different sequence of reduction for BCAF: if the posterior column was more severely separated, the posterior column should be performed first according to posterior approach, and if the anterior column was more severely separated, the anterior column should be performed first according to anterior approach. However, the two combined approaches would result in more complications 13 . Giordano et al. 23 suggested that the reduction of BCAF should start with the proximal iliac wing, but did not provide a description of the anatomical landmarks and did not considered the sacroiliac joint injury. In this study, it was found that PRFRF group had a better quality of reduction than AFRF group, because PRFRF group possessed a precise reduction landmark and sequence. Therefore, the “foundation” theory could improve the quality of reduction.
Characteristics of Structures
In normal physiological conditions, the articular surfaces of the sacroiliac joint and pubic symphysis are parallel to the force direction of the two joints during activity, hence, the surrounding ligaments play a very important role in maintaining stability. The sacroiliac joint is a micro‐movement joint composed of the auricular surface of the ilium and the sacrum, constituting the main part of posterior ring of pelvis, its stability is mainly maintained by the anterior sacroiliac ligament, sacrospinal ligament, ligament of sacral tubercle, and sacroiliac ligament. The pubic symphysis is formed by the ends of the pubis on both sides by fibrocartilage, constituting the main part of anterior ring of pelvis. Compared to pubic symphysis, the sacroiliac joint has a larger contact area. If the pubic symphysis is considered as a point, the sacroiliac joint can be considered as a plane. BCAF is combined with fractures of both pelvic anterior and posterior rings 3 , 9 and it is important to select the correct landmark and sequence of reduction. If the pubic symphysis is used as the landmark of reduction, the sequence of reduction from the anterior ring to the posterior ring may result in the wrong correction of displacement and rotation because the cross‐sectional area of the anterior ring is relatively small. However, if the posterior ring is selected as reduction landmark, this situation can be avoided because the posterior ring has a larger cross‐sectional area. Since most acetabular fracture dislocations are a result of the impingement of femoral head, and the structures that constitute the posterior ring are not directly related to the femoral head, hence, they can maintain their normal anatomic position 3 . Moreover, once the posterior ring is reduced and stabilized, the mobility of the anterior ring is limited to a narrow range 24 . After the anatomical integrity of the pelvis was restored firstly, the acetabular fractures could be reduced to obtain a better joint reduction 25 . Therefore, we propose the “foundation” reduction method, in which the reduction of complex acetabular fractures is like building a house, where a solid foundation is required to ensure the subsequent steps to be stable. This reduction method also strictly follows the anatomy of the pelvis.
Characteristics of Force Transmission
The pelvic structure carried the downward mechanical transmission of force from spine and the upward mechanical transmission from lower limbs, playing an important role in the stable maintenance of various postures 26 . Some studies performed pelvic biomechanics for normal standing position and found that the force was gradually transmitted along the lumbar spine‐sacrum‐sacroiliac joint‐pectineal line‐acetabulum‐femoral head and finally to lower limbs 27 , 28 , 29 . The direction of mechanical transmission of pelvis was exactly as well as the direction of our “foundation” reduction method, which firstly reduced the weight‐bearing part (pelvis) and finally reduction the functional part (acetabulum). Hence, the “foundation” reduction method strictly followed the mechanical characteristics of the pelvis. Besides, the pelvic injury was related with sexual dysfunctions 30 . The posterior and anterior ring could be fixed using percutaneous screw technique to reduce iatrogenic injury if the pelvic fractures were present only 31 , 32 , 33 .
Comparative Analysis of Two Groups
A comparative analysis of PRFRF group and AFRF group showed that patients in PRFRF group had lower operative time (152.3 ± 16.3 vs 183.0 ± 35.3 mins) and blood loss (639.5 ± 109.9 vs 793.9 ± 172.6 ml), suggesting that the reduction method could significantly shorten operative time and thus reduce intra‐operative blood loss. Besides, the PRFRF group also had better quality of reduction and postoperative functional outcome compared to AFRF group, indicating that the reduction method could effectively guide the reduction of fractures. In other words, the functional outcome was related with the quality of reduction. In addition, the incidence of deep vein thrombosis in the lower limbs was lower in PRFRF group (2/22 vs 4/20), which might be a result of the fact that good quality of reduction allowed patients to perform functional exercises early.
Advantages of Computer Simulation
Fractures were simulated and reduced through an application of computer simulation for preoperative surgical procedures. The 3D reconstruction of the patient's CT using computer simulation allowed surgeons to comprehend the complex fracture patterns and thus facilitate the selection of an appropriate surgical approach and fixation method 9 , 11 , 34 . Especially in severe complex acetabular fractures, surgeons could distinguish these variant tiny fragments before operation according to this technique, which avoided ignoring these tiny fragments. Besides, the surgeons could manipulate the bone fragments freely to facilitate the intra‐operative reduction of the fractures. Moreover, after the computer simulation model was established, 3D printing could be performed to produce a full‐scale personalized model, which facilitated the preoperative pre‐bending of the plate but requires a lot of preoperative time 35 .
Strengths and Limitations
Our study confirmed the feasibility of “foundation” reduction method in BCAF surgery in detail and applied the computer simulation in preoperative surgical procedures. Preoperative computer simulation was a time‐consuming process, and in this study, we needed at least 2 h or even longer to process the patient's CT data and to reposition the bone fragments. In addition, this study provided a comparative analysis of patients only with BCAF, the other types of acetabular fractures involving both pelvis and acetabulum such as anterior posterior hemi‐transverse and T‐shaped fractures were not included. Therefore, subsequent studies are required to compare other types of fractures involving both pelvis and acetabulum to demonstrate the general applicability of the “foundation” reduction method.
Conclusion
The “foundation” reduction method can effectively shorten operative time, reduce surgical blood loss, and simplify the surgical steps, ultimately improving the quality of the reduction. This reduction method has a good prospect of application in the treatment of complex acetabular fractures, but it still needs further promotion. In addition, computer simulation is a highly orthopaedic‐relevant technique, especially in treatment of complex acetabular fractures, which improves the efficiency of operation.
Author contributions
Xiaodong Guo and Yizhou Wan designed the study; Lian Zeng and Keda Yu performed the data collection and analysis; Kaifang Chen helped perform the analysis with constructive discussions; Yi Xu and Ziming Zhang completed the evaluation of postoperative reduction quality and hip function; Yan Ma helped to draw the figures; Qinghua Song and Zhenchun Yin processed the English editing. All authors read and approved the final manuscript and consented to publish this manuscript.
Conflict of Interest
All authors declared that there are no competing interests.
Consent for publication
No applicable.
Ethics Statement
All participants in this study were informed and confirmed their participation in this clinical trial, and written informed consent was obtained. All procedures performed in this study involving human were consistent with the ethical standards of the institutional and the national research committee (Ethics Committee of the Union Hospital, Tongji Medical College, Huazhong University of Science and Technology) and the 1964 Declaration of Helsinki and its later amendments.
Funding Information
This work was financially supported by the National Natural Science Foundation of China (grant No. 81873999 and 82072446).
Data Availability Statement
All data generated and/or analyzed during this study are available from the corresponding author by reasonable request.
Acknowledgements
No applicable.
Contributor Information
Kaifang Chen, Email: ckf@hust.edu.cn.
Xiaodong Guo, Email: xiaodongguo@hust.edu.cn.
References
- 1. Laird A, Keating JF. Acetabular fractures: a 16‐year prospective epidemiological study. J Bone Joint Surg Br. 2005;87:969–73. [DOI] [PubMed] [Google Scholar]
- 2. Kelly J, Ladurner A, Rickman M. Surgical management of acetabular fractures—a contemporary literature review. Injury. 2020;51:2267–77. [DOI] [PubMed] [Google Scholar]
- 3. Pierannunzii L, Fischer F, Tagliabue L, Calori GM, d'Imporzano M. Acetabular both‐column fractures: essentials of operative management. Injury. 2010;41:1145–9. [DOI] [PubMed] [Google Scholar]
- 4. Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years' follow‐up. J Bone Joint Surg Br. 2011;93:229–36. [DOI] [PubMed] [Google Scholar]
- 5. Tannast M, Najibi S, Matta JM. Two to twenty‐year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012;94:1559–67. [DOI] [PubMed] [Google Scholar]
- 6. Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;173‐86:173–86. [DOI] [PubMed] [Google Scholar]
- 7. Yang Y, Zou C, Fang Y. Mapping of both column acetabular fractures with three‐dimensional computed tomography and implications on surgical management. BMC Musculoskelet Disord. 2019;20:255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang Y, Zou C, Fang Y. A study on fracture lines of the quadrilateral plate based on fracture mapping. J Orthop Surg Res. 2019;14:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yin Y, Zhang R, Hou Z, Fan S, Zhuang Y, Yi C, et al. Fracture mapping of both‐column acetabular fractures. J Orthop Trauma. 2022;36:e189–94. [DOI] [PubMed] [Google Scholar]
- 10. Hu Y, Li H, Qiao G, Liu H, Ji A, Ye F. Computer‐assisted virtual surgical procedure for acetabular fractures based on real CT data. Injury. 2011;42:1121–4. [DOI] [PubMed] [Google Scholar]
- 11. Chen K, Yang F, Yao S, Xiong Z, Sun T, Zhu F, et al. Application of computer‐assisted virtual surgical procedures and three‐dimensional printing of patient‐specific pre‐contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019;105:877–84. [DOI] [PubMed] [Google Scholar]
- 12. Cimerman M, Kristan A. Preoperative planning in pelvic and acetabular surgery: the value of advanced computerised planning modules. Injury. 2007;38:442–9. [DOI] [PubMed] [Google Scholar]
- 13. Chen KF, Ji YH, Huang ZF, Navinduth R, Yang F, Sun TF, et al. Single modified ilioinguinal approach for the treatment of acetabular fractures involving both columns. J Orthop Trauma. 2018;32:E428–E34. [DOI] [PubMed] [Google Scholar]
- 14. Matta JM. Operative treatment of acetabular fractures through the ilioinguinal approach: a 10‐year perspective. J Orthop Trauma. 2006;20:S20–9. [PubMed] [Google Scholar]
- 15. Matta JM, Anderson LM, Epstein HC, Hendricks P. Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res. 1986;205:230–40. [PubMed] [Google Scholar]
- 16. Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta‐analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 17. Lichte P, Sellei RM, Kobbe P, Dombroski DG, Gansslen A, Pape HC. Predictors of poor outcome after both column acetabular fractures: a 30‐year retrospective cohort study. Patient Saf Surg. 2013;7:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Firoozabadi R, Hamilton B, Toogood P, Routt MC, Shearer D. Risk factors for conversion to Total hip arthroplasty after acetabular fractures involving the Posterior Wall. J Orthop Trauma. 2018;32:607–11. [DOI] [PubMed] [Google Scholar]
- 19. Joseph NM, Flanagan CD, Heimke IM, Cho E, Pothireddy S, Scarcella N, et al. Factors influencing functional outcomes following open reduction internal fixation of acetabular fractures. Injury. 2021;52:1396–402. [DOI] [PubMed] [Google Scholar]
- 20. Yao S, Chen K, Zhu F, Liu J, Wang Y, Zeng L, et al. Internal fixation of anterior acetabular fractures with a limited pararectus approach and the anatomical plates: preliminary results. BMC Musculoskelet Disord. 2021;22:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Avilucea FR, Whiting PS, Mir H. Posterior fixation of APC‐2 pelvic ring injuries decreases rates of anterior plate failure and malunion. J Bone Joint Surg Am. 2016;98:944–51. [DOI] [PubMed] [Google Scholar]
- 22. Vaidya R, Martin AJ, Roth M, Tonnos F, Oliphant B, Carlson J. Midterm radiographic and functional outcomes of the anterior subcutaneous internal pelvic fixator (INFIX) for pelvic ring injuries. J Orthop Trauma. 2017;31:252–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Giordano V, Acharya MR, Pires RE, Giannoudis PV. Associated both‐column acetabular fracture: An overview of operative steps and surgical technique. J Clin Orthop Trauma. 2020;11:1031–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Giraldez‐Sanchez MA, Lazaro‐Gonzalvez A, Martinez‐Reina J, Serrano‐Toledano D, Navarro‐Robles A, Cano‐Luis P, et al. Percutaneous iliosacral fixation in external rotational pelvic fractures. A biomechanical analysis. Injury. 2015;46:327–32. [DOI] [PubMed] [Google Scholar]
- 25. Meccariello L, Razzano C, De Dominicis C, Herrera‐Molpeceres JA, Liuzza F, Erasmo R, et al. A new prognostic pelvic injury outcome score. Med Glas (Zenica). 2021;18:299–308. [DOI] [PubMed] [Google Scholar]
- 26. Kai S, Sato T, Koga Y, Omori G, Kobayashi K, Sakamoto M, et al. Automatic construction of an anatomical coordinate system for three‐dimensional bone models of the lower extremities—Pelvis, femur, and tibia. J Biomech. 2014;47:1229–33. [DOI] [PubMed] [Google Scholar]
- 27. Roussouly P, Pinheiro‐Franco JL. Biomechanical analysis of the spino‐pelvic organization and adaptation in pathology. Eur Spine J. 2011;20(Suppl 5):609–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bagwell JJ, Fukuda TY, Powers CM. Sagittal plane pelvis motion influences transverse plane motion of the femur: kinematic coupling at the hip joint. Gait Posture. 2016;43:120–4. [DOI] [PubMed] [Google Scholar]
- 29. Muzii VF, Rollo G, Rocca G, Erasmo R, Falzarano G, Liuzza F, et al. Radiographic and functional outcome of complex acetabular fractures: implications of open reduction in spinopelvic balance, gait and quality of life. Med Glas (Zenica). 2021;18:273–9. [DOI] [PubMed] [Google Scholar]
- 30. Rovere G, Perna A, Meccariello L, De Mauro D, Smimmo A, Proietti L, et al. Epidemiology and aetiology of male and female sexual dysfunctions related to pelvic ring injuries: a systematic review. Int Orthop. 2021;45:2687–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Falzarano G, Rollo G, Bisaccia M, Pace V, Lanzetti RM, Garcia‐Prieto E, et al. Percutaneous screws CT guided to fix sacroiliac joint in tile C pelvic injury. Outcomes at 5 years of follow‐up. SICOT J. 2018;4:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Florio M, Capasso L, Olivi A, Vitiello C, Leone A, Liuzza F. 3D—Navigated percutaneous screw fixation of pelvic ring injuries—a pilot study. Injury. 2020;51(Suppl 3):S28–33. [DOI] [PubMed] [Google Scholar]
- 33. Ciolli G, Caviglia D, Vitiello C, Lucchesi S, Pinelli C, De Mauro D, et al. Navigated percutaneous screw fixation of the pelvis with O‐arm 2: two years' experience. Med Glas (Zenica). 2021;18:309–15. [DOI] [PubMed] [Google Scholar]
- 34. Ye K, Broertjes K, Qin H, Zhan Y, An Z. Intra‐articular fragment mapping in associated both‐column acetabular fractures. Arch Orthop Trauma Surg. 2022. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 35. Hung CC, Li YT, Chou YC, Chen JE, Wu CC, Shen HC, et al. Conventional plate fixation method versus pre‐operative virtual simulation and three‐dimensional printing‐assisted contoured plate fixation method in the treatment of anterior pelvic ring fracture. Int Orthop. 2019;43:425–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated and/or analyzed during this study are available from the corresponding author by reasonable request.


