Abstract
Biliodigestive anastomosis between the extrahepatic bile duct and the intestine for bile duct disease is a gastrointestinal reconstruction that abolishes duodenal papilla function and frequently causes retrograde cholangitis. This chronic inflammation can cause liver dysfunction, liver abscess, and even bile duct cancer. Although research has been conducted for over 100 years to directly repair bile duct defects with alternatives, no bile duct substitute (BDS) has been developed. This narrative review confirms our understanding of why bile duct alternatives have not been developed and explains the clinical applicability of BDSs in the near future. We searched the PubMed electronic database to identify studies conducted to develop BDSs until December 2021 and identified studies in English. Two independent reviewers reviewed studies on large animals with 8 or more cases. Four types of BDSs prevail: Autologous tissue, non-bioabsorbable material, bioabsorbable material, and others (decellularized tissue, 3D-printed structures, etc.). In most studies, BDSs failed due to obstruction of the lumen or stenosis of the anastomosis with the native bile duct. BDS has not been developed primarily because control of bile duct wound healing and regeneration has not been elucidated. A BDS expected to be clinically applied in the near future incorporates a bioabsorbable material that allows for regeneration of the bile duct outside the BDS.
Keywords: Bile duct alternative, Bile duct substitute, Biliary regeneration, Bile duct reconstruction, Peribiliary gland, Bioabsorbable polymer
Core Tip: The bile duct-intestinal anastomosis eliminating the function of the papilla of Vater causes chronic inflammation due to the reflux of bile and is not an ideal reconstruction method. Bile duct alternatives for bile duct defects have not been developed for over 100 years. In the present situation where the wound healing of the bile duct defect cannot be controlled, only the use of a bioabsorbable material, such as a scaffold, and the regeneration of the bile duct outside the scaffold can be expected as a bile duct substitute.
INTRODUCTION
The treatment of gastrointestinal diseases in the 21st century involves robotic and endoscopic surgeries, which aim to minimize potential risks and side effects[1-3]. Minimally invasive endoscopic treatments have been developed to facilitate functional preservation[4,5]. For diseases of the biliary system, the use of laparoscopic cholecystectomy as a treatment for cholelithiasis has become widespread, and minimally invasive approaches have been pursued[6]. In contrast, the incidence of severe iatrogenic extrahepatic bile duct injury due to laparoscopic cholecystectomy has increased significantly worldwide compared to that due to laparotomy surgery[7]. With regard to bile duct injuries, there is currently no bile duct substitute (BDS) for partially defective or damaged parts of the bile duct. Reconstruction by anastomosis of the hepatic bile duct and intestine is typically performed[8].
Bile duct-intestinal anastomosis is a biliary tract reconstruction procedure that was first performed by von Winiwater in 1880[9]. However, liver abscess, cirrhosis, and liver dysfunction were often observed in patients who underwent this anastomosis. In the early 20th century, retrograde cholangitis tended to cause chronic inflammation if duodenal papilla function was not preserved[10,11]. The suboptimal nature of this approach resulted in attempts to preserve papilla function and to develop alternatives for addressing bile duct defects and injury. Chronic inflammation caused by abnormal pancreatic-bile duct junctions, intrahepatic stones[12,13], and exposure to organic solvents from the printing industry is considered a high-risk factor for cholangiocarcinoma[14]. Therefore, the development of BDS has emerged as a critical, unmet need. To date, various alternatives, including autologous tissue[10,15-18], non-bioabsorbable[19-23], bioabsorbable materials[24-28], and decellularized tissue[29,30], have been investigated. Nevertheless, BDSs with widespread clinical applications have not yet been developed. In this review, we discuss potential factors underpinning the failure to develop clinically usable products despite efforts to develop BDSs for more than a century. Furthermore, we highlight the types of BDSs that may be clinically applied in the near future.
MATERIALS AND METHODS
We searched the PubMed electronic database to identify studies conducted to develop bile duct alternatives until December 2021 and identified studies in English. The following search items for the data relevant to “why has a product that can replace bile ducts not been developed?” were included: “bile duct alternative”, “bile duct substitute”, “bile duct regeneration”, “biliary alternative”, “extrahepatic bile duct”, “biliary regeneration”, and “bile duct reconstruction”. Studies using large animals such as dogs, pigs, and goats were included, whereas studies using small animals such as rats and mice were excluded. To evaluate the efficacy of the BDS, the “type of substitute”, “shape and length of substitute”, “method of reconstruction of the bile duct by substitute”, and “observation period” were included as search terms. The items to be examined were “presence or absence of regeneration process”, “localization of regenerated bile duct to substitute”, “number of large animals that could be sacrificed and killed intentionally”, and “cause of narrowing of substitute”. We also cited high-quality articles in Reference Citation Analysis (https://www.referencecitationanalysis.com).
For studies in which the items could be determined from the abstract or text, the number of experimental large animals used was eight or more. The full text was reviewed by two researchers (Miyazawa M, Takashima J). In each of these studies, the cases in which BDS transplantation was successful were as follows: These cases were sacrificed as planned before BDS transplantation, no stenosis was observed at the anastomotic site between the BDS transplantation site and the natural bile duct, and there was no liver dysfunction after BDS transplantation.
Animal type
In small animals, such as rats, jaundice is unlikely to occur even if the extrahepatic bile duct is narrowed, and liver dysfunction may be difficult to evaluate. As such, BDS transplantation may be difficult[31]. Accordingly, only large-animal studies were considered.
Size of BDS
If the length of the BDS implantation segment was less than 1 cm, tissues such as the omentum may migrate around it after inserting the T-tube into the defective bile duct segment[32]. Therefore, BDSs ≤ 1 cm and > 1 cm in length were considered separately. For the same reason, patch-like or circular implantation of the BDS was examined separately. Regarding the implantation method, the site of BDS implantation (between the common bile duct or between the common bile duct and intestine) was examined separately because it affects the patency of the BDS lumen.
Observation period after BDS implantation
Early after BDS transplantation, stenosis of the BDS may not occur in the event of retrograde cholangitis or severe inflammation at the alternative transplant site. After chronic inflammation, the bile duct becomes narrowed due to the gradual hyperplasia of connective tissue around the substitute[33]. After stent insertion into the BDS, bile may flow through the stent and a bile plug may not be formed in the BDS in the early stage of BDS transplantation[34]. As anastomotic stenosis was considered less likely to occur when a stent was inserted, the observation period after BDS transplantation was included in the examination items.
Bile duct regeneration
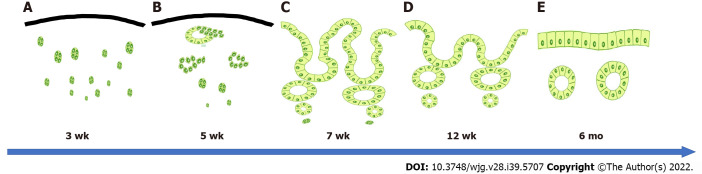
After the formation of connective tissue in the shape of the bile duct, the BDS lumen does not become completely stenotic early after BDS transplantation, even if bile duct regeneration does not occur and bile remains in the lumen. However, stenosis tends to occur after a prolonged period[35]. Tissue regeneration in the defective bile duct area occurs due to wound healing[35]. The mature bile duct takes time (3 mo or more) to regenerate from bile duct stem cells[25,36,37] (Figure 1). Therefore, to examine the effectiveness of BDS for inducing bile duct regeneration, histological images of bile duct regeneration at the BDS transplantation site were included in the examination. If the study did not report neo-bile duct regeneration and the histology was similar to that of the native bile duct, the tissue was excluded from evaluation. The histology of the anastomotic site between the BDS and native bile duct was examined because the bile duct epithelium is continuous at the anastomotic site if stenosis of the anastomotic site does not occur[38].
Figure 1.
Ideal bile duct regeneration process. A: Bile duct regeneration at approximately 3 wk. Numerous cell masses appear in the stroma that are thought to form peribiliary glands; B: Bile duct regeneration at approximately 5 wk. A ring-shaped peribiliary gland-like structure is observed, in which cell masses that are thought to form peribiliary glands are fused; C: Bile duct regeneration at approximately 7 wk. Numerous bile duct-attached glandular structures are observed on the bile passage surface, and the epithelial surface exhibits a high papillary morphology; D: Bile duct regeneration at approximately 12 wk. The number of peribiliary glands on the bile passage surface is decreased, the peribiliary glands become fused, and the epithelial surface becomes more even; E: Approximately 6 mo after bile duct regeneration. Similar to the native bile duct, the epithelial surface becomes a single layer of cubic columnar epithelium.
Localization of bile duct regeneration with respect to BDS implants
We did not identify any reports of bile duct regeneration on the inner surface of the T-tube when it was placed in the injured part of the bile duct. This suggests that the bile duct does not regenerate on the inner surface of non-bioabsorbable BDSs. However, it is important from the viewpoint of wound healing whether the localization of the regenerated bile duct is the outer surface of the BDS, the part of the BDS itself, or the inner surface of the BDS (only the bile passage surface). For these reasons, the site where the regenerated bile duct regenerates was included in the examination items for the BDS transplantation site. When the localization of bile duct regeneration was not specified, it was judged from the BDS implantation site and bile passage position in the paper.
Causes of stenosis
Narrowing of the anastomotic site between the BDS and the native bile duct or the BDS lumen was evaluated as a separate cause of wound healing. We also examined the stenotic tissue type. For BDS lumen and anastomotic site stenosis, scar contraction was considered to occur over a prolonged period if granulation or connective tissue growth was reported[35,39,40].
BDS REPORTED TO DATE
The literature search enabled the classification of BDSs into four categories: Autologous tissues[10,15-18], non-bioabsorbable materials[19-23], bioabsorbable materials[24-28], and others (decellularized tissues[29,30], structures made with 3D printers[41,42], etc.).
BDS using autologous tissue
Tissues with a similar morphology to that of the extrahepatic bile duct and lumen have been investigated as BDSs. In practice, arteries[43], veins[15,17-19,44], ureters[45], skin[46], and jejunum[16] have been used as grafts. Due to the thickness of the extrahepatic bile duct and wall, the femoral vein was often used. In BDSs using these autologous tissues, necrosis of the substitute in the early stage of transplantation and obstruction due to attachment of the bile plug to the substitute in the middle stage of transplantation were common[10,17,18,44,47]. In the long term, scar contraction occurs due to the growth of connective tissue around the substitute and at the anastomotic site[10,17-19,44]. To address these issues, attempts have been made to wrap the omentum around the substitute to supply blood flow or to use stents and cuffs to prevent obstruction of the BDS lumen and anastomotic site[17,48,49]. As the BDS did not regenerate to the extent of the native bile duct, few BDSs were successful, and no clinically usable product was developed[48,49]. The localization of neo-bile ducts to the BDS, which attempted to promote bile duct regeneration, formed a part of the autologous tissue itself.
The most commonly used species in these studies was dog. Pearce et al[10] investigated autologous alternative veins as a BDS and concluded that 1 in 32 successful cases over 3 mo was insufficient for the use of autologous tissue as a BDS. A study by Dunphy and Stephens[19] using large animals (44 sheep and 8 pigs) evaluated autologous arteries, veins, and homozygous arteries. Only sheep that received autologous arteries as a BDS survived for 6 mo or more, but bile duct dilation on the liver side was observed. Myers et al[18] conducted a circular transplantation experiment using autologous bile ducts, arteries, veins, and genomic grafts to treat bile duct defects in 28 dogs. All homografts were rejected, and the dogs that received transplants died within 13 d.
Even in transplantations using autologous tissue, histological assessment revealed that the bile duct epithelium did not regenerate on the epithelial surface, fibrous connective tissue was increased on the epithelial surface, and the BDS transplantation site became stenotic. The authors concluded that self-organization is not possible in BDS. In 2009, Palmes et al[48] reported a high success rate of transplantation of the external jugular vein and a bioabsorbable stent as a BDS in pigs. However, histological changes in the bile ducts of autologous veins have not been reported (Table 1).
Table 1.
Bile duct substitute using autologous tissue
|
Ref.
|
Journal
|
Substitute (n)
|
Stent (n)
|
Animal type (n)
|
Size of BDS (cm)
|
Method of reconstruction of bile duct by BDS (n)
|
Observation period after implantation
|
Localization of regenerated bile duct
|
Causes of stenosis
|
Note (planned sacrificial death and epithelialization)
|
| Shea and Hubay[15], 1948 | Ann Surg | Femoral vein (21) | Vitallium tube | Dog (21) | Ring (1.5) | CBC (21) | Maximum 208 d | BDS itself | Necrosis of BDS itself, narrowing of the BDS lumen, and narrowing of the anastomosis with the native bile duct | Although 14 out of 21 dogs were intentionally killed, the tissue of the regenerated bile duct was shown only as a result, and the process of bile duct regeneration was not demonstrated |
| Kirby and Fitts[16], 1950 | Arch Surg (1920) | Jejunum (9) | T-tube | Dog (9) | Jejunum (2.5) | GBC (5); CBC (4) | Maximum 13 mo | BDS itself | BDS stenosis was not observed when the T-tube was inserted | Seven out of nine dogs were intentionally killed; however, no epithelial regeneration was observed at the anastomotic site. The procedure was too complicated |
| Pearce et al[10], 1951 | Ann Surg | Femoral vein (32) | Lord and blakemore tube | Dog (32) | Ring (1.0) | CBC (10); CBJ (20); GBC (2) | Maximum 6 mo | BDS itself | Necrosis of autologous tissue, narrowing of the lumen of autologous tissue, narrowing of the anastomosis with the native bile duct, necrosis of BDS itself, narrowing of the BDS lumen, and narrowing of the anastomosis with the native bile duct | Only 1 of the 32 dogs survived for more than 6 mo. It was investigated in 32 dogs; however, in the end, fibrosis of the vein and stenosis of the anastomotic site with the native site occurred, and bile duct epithelial regeneration was not observed. It was concluded that the vein was not suitable for BDS |
| Ulin et al[17], 1955 | Ann Surg | Vascularised jugular vein (10) | Polyethylene tube | Dog (10) | Ring (2.0-5.0) | CBC (10) | Maximum 10 mo | BDS itself | Necrosis of autologous tissue, narrowing of the lumen of autologous tissue, narrowing of the anastomosis with the native bile duct, necrosis of BDS itself, narrowing of the lumen of BDS, and narrowing of the anastomosis with the native bile duct | The omentum was used to maintain blood flow to the BDS, but in some cases, it functioned as a BDS only during the period when the stent was in place (6 out of 10 dogs). Bile duct regeneration process was not studied. No regeneration of the bile duct epithelium was observed |
| Myers et al[18], 1960 | Ann Surg | Femoral vein and artery, bile duct (17), and homologous bile duct (6) | Polyethylene tube | Dog (28) | Ring (unknown) | CBC (23) | Maximum 449 d | BDS itself | Necrosis of autologous tissue, narrowing of the lumen of autologous tissue, narrowing of the anastomosis with the native bile duct, necrosis of BDS itself, narrowing of the BDS lumen, and narrowing of the anastomosis with the native bile duct | BDS using autologous veins, arteries, or allogeneic arteries also narrowed shortly after transplantation. No bile duct epithelial regeneration was observed |
| Dunphy and Stephens[19], 1962 | Ann Surg | Autologous vein and artery (20), and homologous artery (32) | T-tube | Goat (44), dog (8) | Ring (1.0) | CBC (52) | Maximum 9 mo | BDS itself | Necrosis of autologous tissue, narrowing of the lumen of autologous tissue, narrowing of the anastomosis with the native bile duct, necrosis of BDS itself, narrowing of the BDS lumen, and narrowing of the anastomosis with the native bile duct | In an experiment using autologous veins and T-tube as BDS, 2 dogs survived for more than 6 mo; however, both dogs demonstrated dilation of the bile duct on the liver side. No bile duct epithelial regeneration was observed |
| Belzer et al[44], 1965 | Ann Surg | Femoral vein (20) | T-tube | Goat (20) | Patch (3.0-4.0) | Patch (20) | Maximum 11 mo | BDS itself | Necrosis of autologous tissue, narrowing of the lumen of autologous tissue, narrowing of the anastomosis with the native bile duct, necrosis of BDS itself, narrowing of the BDS lumen, and narrowing of the anastomosis with the native bile duct | Only 3 out of 20 dogs were intentionally killed, but no good bile duct epithelial regeneration was observed |
| Lindenauer and Child[47], 1966 | Ann Surg | Vascularized jugular vein (14) | (-) | Dog (14) | Ring (unknown) | CBC (14) | Maximum 18 mo | BDS itself | The omentum increased blood flow to the BDS; however, it resulted in scar contraction. Necrosis of BDS itself, narrowing of the BDS lumen, and narrowing of the anastomosis with the native bile duct | No dog survived for more than 3.5 mo, although the omentum was used to maintain BDS blood flow |
| Palmes et al[48], 2009 | J Invest Surg | External jugular vein (18) | PLA stent (12) | Pig (18) | Ring (2.0) | CBC (18) | Maximum 6 mo | BDS itself | When the stent was not inserted, the BDS was necrotic. When the stent was inserted, the BDS lumen was preserved, but eventually, it became necrotic and narrowed | Of the 18 dogs, all 12 stented dogs were deliberately killed. However, the process of regeneration of veins into the bile duct was not reported |
| Liang et al[49], 2012 | World J Gastroenterol | Omentum (8) | Bioabsorbable stent | Pig (8) | Ring (0.5-1.0) | CBC (8) | Maximum 4 mo | BDS itself | The BDS lumen was preserved when the stent was inserted | The bile duct defect was repaired with an omentum, which was similar to inserting a T-tube into the defect. Bile duct regeneration was also poorly demonstrated |
BDS: Bile duct substitute; CBC: Common bile duct to bile duct substitute to common bile duct; CBJ: Common bile duct to bile duct substitute to jejunum; GBC: Gallbladder to bile duct substitute to common bile duct; PLA: Polylactide acid.
Due to the lack of blood supply in autologous tissue BDSs, the tissue becomes necrotic, and the anastomotic site is scar-contracted. A BDS capable of allowing bile to flow freely into the duodenum over a prolonged period has not yet been developed. It is unlikely that autologous tissue will resemble the native bile duct in the context of wound healing[40,50,51]. Stenting through the anastomotic site was effective in preventing narrowing[17,48,49]. High success rates have been reported when bioabsorbable stents are placed in the venous lumen; however, it is unclear how autologous venous tissue is induced for good bile duct regeneration. These findings suggested that autologous tissue cannot be used as a BDS.
BDS using non-bioabsorbable material
Since the 1930s, polyvinyl sponge[20], polytetrafluorethylene[22,23], Teflon[19,52], Dacron[53], and polyethylene[54,55] have been used as non-bioabsorbable BDS materials. These alternatives were used experimentally as patches or rings, but most studies reported high rejection rates early in transplantation and varying degrees of cholangitis, narrowing of the alternative lumen, and stenosis of the anastomotic site with the native bile duct[19,27,28]. Although partial success has been reported, the bile duct epithelium failed to regenerate on either the medial side (bile passage surface) or lateral side of these alternatives[29,30]. As a result, the perimeter of these BDSs was covered with fibrous connective tissue, and the luminal surface was clogged with bile plugs[19-22]. This resulted in stenosis of the anastomosis with the native bile duct, which prevented bile passage. As such, research on cyclic BDS made solely from non-bioabsorbable materials has ceased.
Sherman et al[21] transplanted a BDS made from acrylamide into dogs. In the stented group, 7 of the 33 cases were successful over 3 mo. However, bile duct regeneration has not been reported. Bergan et al[20] attached blood vessels to a BDS composed of polyvinyl sponge in dogs. Of the 12 dogs examined, 4 survived for more than 60 d, but the transplant was ultimately unsuccessful due to the formation of bile plugs inside the substitute. Dunphy and Stephens[19] examined Teflon as a BDS in four dogs and four sheep, but all failed because of severe rejection early in the transplantation. Recently, Gómez et al[23] investigated Gore-Tex as a BDS in 12 dogs and reported that 11 cases were successful. However, BDS was surrounded by strong fibrotic tissue and exhibited narrowing, indicating that it was not clinically usable in the long term (Table 2).
Table 2.
Bile duct substitute using non-bioabsorbable material
|
Ref.
|
Journal
|
Substitute (n)
|
Stent
|
Animal type (n)
|
Size of BDS (cm)
|
Method of reconstruction of bile duct by BDS (n)
|
Observation period after implantation
|
Localization of regenerated bile duct
|
Causes of stenosis
|
Note (planned sacrificial death and epithelialization)
|
| Dunphy and Stephens[19], 1962 | Ann Surg | Teflon (8) | (-) | Dog (4), goat (4) | Ring (1.0) | CBC (8) | Maximum 7 wk | BDS outside | Narrowing of the anastomosis with the native bile duct; narrowing of the lumen of BDS | In all cases, the hepatobiliary enzyme levels increased, and no survivors were observed for more than 7 wk after transplantation |
| Bergan et al[20], 1962 | Arch Surg | Vascularized polyvinyl sponge (21) | (-) | Dog (21) | Ring (0.5) | CBC (21) | Maximum 14 mo | BDS outside | Narrowing of the anastomosis with the native bile duct; narrowing of the lumen of BDS | Four out of 21 dogs survived for > 60 d after transplantation, and four of them had stenosis of BDS |
| Sherman et al[21], 1963 | Ann Surg | Acrylamide with Dacron (33) | (-) | Dog (33) | Ring (1.5-3.5) | CBC (33) | Maximum 31 mo | BDS outside | Narrowing of the anastomosis with the native bile duct; narrowing of the lumen of BDS | Twenty-six out of 33 dogs died within 3 mo. In all cases, fibrotic thickening around the BDS and severe scar contraction had occurred at the site of anastomosis |
| Mendelowitz et al[22], 1982 | Am J Surg | Gore-Tex (6), dacron (2) | (-) | Dog (8) | Ring (2.0-3.0), patch (2.0 cm × 1.0 cm) | Patch (Gore-Tex) (2), CBJ (Gore-Tex) (2), CBC (Gore-Tex) (1), CBC (Dacron) (2), GBJ (Gore-Tex) (1) | Maximum 40 d | BDS outside | Narrowing of the anastomosis with the native bile duct; narrowing of the lumen of BDS | In all cases, a bile plug was found in the lumen of the BDS, and a high degree of fibrotic thickening was found around the site of anastomosis |
| Gómez et al[23], 2002 | J Gastrointest Surg | Gore-Tex (12) | (-) | Dog (12) | Ring (2.0-3.0) | CBC (12) | Maximum 3 mo | BDS outside | Narrowing of the lumen of BDS | Eleven out of 12 dogs were intentionally killed, but severe fibrotic thickening was observed around the BDS |
BDS: Bile duct substitute; CBC: Common bile duct to bile duct substitute to common bile duct; CBJ: Common bile duct to bile duct substitute to jejunum; GBJ: Gallbladder to bile duct substitute to jejunum.
Currently, cyclic non-absorbable materials, such as polytetrafluoroethylene, are used clinically as artificial blood vessels. Anticoagulants are used to prevent blood from coagulating in artificial blood vessels when the blood vessel diameter is small[56]. Compared to blood, bile is more viscous and has a slower flow velocity. The bile duct diameter is similar to that of small blood vessels[57]. As such, this material may be unsuitable because the BDS lumen may be blocked by a bile plug[21,22]. In addition, the epithelium does not regenerate continuously at the anastomotic site between the BDS and native bile duct, scar contraction occurs in the long term after transplantation[38]. A bile plug may form if a tubular stent is inserted to secure bile passage, even when using non-bioabsorbable materials. This phenomenon is similar to current endoscopic stenting for bile duct stenosis[58,59].
BDS using bioabsorbable material
Due to the failure to develop clinically applicable BDSs made from autologous tissue or non-bioabsorbable materials, increasing focus has been placed on bioabsorbable materials as BDSs. This concept is based on the technique of tissue engineering proposed by Langer and Vacanti[60] in 1993 for bile duct regeneration. The complex formed by the bioabsorbable material and cells attached to the material is absorbed in the body while the bioabsorbable material acts as a scaffold to maintain the environment and shape of the organ[60,61]. Concurrently, the cells attached to the scaffold regenerate the target organ. Natural polymers (particularly collagen)[24,27,28] and engineered synthetic polymers[25,26,62-64] have been investigated as BDSs based on bioabsorbable materials.
BDS using natural polymers
Alternative natural polymers to collagen have been investigated, such as the small intestinal submucosa (SIS) using porcine submucosa. Using this SIS, Rosen et al[24] reported that 9 cases of patch-like transplantation and 6 cases of circular transplantation were performed as BDS, and 13 of them were successful. However, bile duct regeneration was not observed as a pathological finding. On the other hand, in another study using SIS as a BDS, scar contraction was high[65]. As such, this material has not been clinically applied as a BDS (Table 3).
Table 3.
Bile duct substitute using bioabsorbable material
|
Ref.
|
Journal
|
Substitute
|
Stent
|
Animal type (n)
|
Size of BDS (cm)
|
Method of reconstruction of bile duct by BDS (n)
|
Observation period after implantation
|
Localization of regenerated bile duct
|
Causes of stenosis
|
Note (planned sacrificial death and epithelialization)
|
| Rosen et al[24], 2002 | Surgery | SIS | (-) | Dog (15) | Patch: (2.0 cm × 1.0 cm), ring: (2.0-3.0) | Patch (9), CBC (6) | Maximum 5 mo | BDS itself | Scar contraction at the site of anastomosis on the duodenal side | Thirteen out of 15 dogs were intentionally killed. The regenerated bile duct tissue was shown consequently, and the process of regenerating the bile duct was not shown |
| Miyazawa et al[25], 2005 | Am J Transplant | P (CL/LLA) with PGA | (-) | Pig (18) | Ring (3.0) | CBJ (18) | Maximum 6 mo | BDS outside | No narrowed BDS | All pigs were intentionally killed. A good bile duct regeneration process was shown |
| Nau et al[26], 2011 | HPB (Oxford) | PGA and TMC | 5 Fr pancreatic stent | Dog (11) | Ring (1.0) | CBC (11) | Maximum 12 mo | BDS itself | Narrowing of the BDS lumen | Ten out of 11 dogs were intentionally killed. No good bile duct epithelial regeneration was observed |
| Li et al[27], 2012 | Biomaterials | Collagen with bFGF | (-) | Pig (26) | Patch (2.0 cm × 1.0 cm) | Patch (26) | Maximum 6 mo | BDS itself | No narrowed BDS | All pigs were intentionally killed. The regenerated bile duct tissue was shown consequently, while the process of regenerating the bile duct was not shown |
| Tao et al[28], 2015 | Artif Organs | Collagen | Plastic stent | Pig (20) | Patch (2.0 cm × 0.6 cm) | Patch (12) | Maximum 12 wk | BDS itself | No narrowed BDS | All pigs were intentionally killed. The regenerated bile duct tissue was observed consequently, while the process of regenerating the bile duct was not shown |
| Tanimoto et al[62], 2016 | Langenbecks Arch Surg | P (CL/LLA) | T-tube | Pig (11) | Ring (2.0) | CBC (11) | Maximum 6 mo | BDS itself | No narrowed BDS | All pigs were intentionally killed. A high degree of fibrosis was observed in the regenerated bile duct tissue |
| de Abreu et al[63], 2020 | J Biomater Appl | Bacterial cellulose film | T-tube | Pig (10) | Patch (2.0 cm × 1.0 cm) | CBC (20) | Maximum 330 d | BDS itself | No narrowed BDS | All pigs were intentionally killed. No process of bile duct regeneration was shown |
BDS: Bile duct substitute; bFGF: Basic fibroblast growth factor; CBC: Common bile duct to bile duct substitute to common bile duct; CBJ: Common bile duct to bile duct substitute to jejunum; P(CL/LLA): Polyε-caprolactone/poly l-lactide; PGA: Polyglycolic acid; SIS: Small intestinal submucosa; TMC: Trimethylene carbonate.
Nakashima et al[66] reported the successful use of collagen as a BDS in consideration of cell adhesion. However, collagen was attached to a non-bioabsorbable material (polypropylene) to maintain the hardness of this BDS; therefore, it may not be a strictly bioabsorbable BDS. The BDS scaffold was sutured to the native bile duct. As bile passes through the lumen, the scaffold must maintain an annular shape and therefore a degree of hardness. Collagen tends to lose its shape when immersed in water[66,67]. Collagen-based BDSs require hardness in other substances to maintain the scaffold hardness, resulting in an absorption period longer than several months. For this reason, SIS uses collagen and submucosal tissue to maintain hardness[24].
To promote bile duct regeneration within the bioabsorbable material itself, the period of in vivo absorption of the bioabsorbable material is important for suppressing scar contraction. In the case of artificial skin using collagen for skin regeneration, it has been reported that the half-life of the bioabsorbable material, which most strongly suppresses scar contraction, is approximately 14 d[67]. If a BDS made of a bioabsorbable material has a half-life of 3-4 wk or more, scar contraction may be high. When bioabsorbable materials other than the skin are used as alternatives for bile duct regeneration, the absorption period of such materials must also be considered, but this is not the case for SIS[24].
In collagen-based BDSs, the density of the material ligand is important for cell adhesion to promote bile duct regeneration[68]. However, there is a paucity of research in this area. If attempts are made for bile duct regeneration within the bioabsorbable material itself, scar contraction of the BDS part cannot be suppressed after transplantation unless these points are taken into consideration.
BDS using synthetic polymers
BDSs based on synthetic polymers are predominantly composed of polyglycolic acid (PGA)[26] and polycaprolactone[24,62], BDSs produced using PGA fibers may fail to maintain their radial shape. In many studies, the major axis of the bile duct has been replaced by approximately 1 cm. The absorption period of PGA is approximately 3 mo; as such, chronic inflammation occurs, and bile duct regeneration occurs at the implanted site. As such, attempts to regenerate the bile duct epithelium on the inner surface (bile passage surface) of this BDS eventually cause scar contraction similar to that of non-bioabsorbable BDS, and previous efforts have been unsuccessful[24,61].
Studies employing polycaprolactone-based BDSs have reported good bile duct regeneration outside the BDS implant. The material in these studies comprised a 50:50 copolymer of lactic acid and caprolactone, which was reinforced with latticed PGA fibers to facilitate suturing[25]. Generally, the absorption period is 6-8 wk, and the material becomes vulnerable in vivo for approximately 3 wk. After the BDS becomes fragile and sheds into the duodenum, a bile duct thicker than the outer circumference of the BDS regenerates outside the BDS. Cells migrating to the BDS as a foreign body reaction may promote bile duct regeneration[25]. Previous studies have reported good results, including BDS experiments in infectious reservoirs[69]. The occurrence of bile duct regeneration on the outside of the BDS resembles bile duct regeneration after insertion of a T-tube into a defective bile duct followed by T-tube removal (Table 3).
As BDSs using synthetic polymers can be engineered, the period of absorption in the body can be adjusted[70]. However, if the BDS is hard to maintain the shape of the bile duct, the absorption period may be prolonged. As BDS results in longer chronic inflammation due to a foreign body reaction, the results are likely to be similar to those of non-bioabsorbable materials. In contrast, if the absorption period is too short, the BDS transplantation site becomes fragile and is destroyed after transplantation. Bile may flow out of the BDS transplantation site, making this material unsuitable for BDS. With regard to cell adhesion, the scaffold itself (for example, PGA only) has lower cell adhesion compared to collagen-based scaffolds owing to the lack of receptors for cell adhesion[38]. Therefore, to regenerate the scaffold itself within the bile duct, materials in which receptors are added to the scaffold have been investigated[38]. Failure of the bile duct to regenerate in the scaffold part while being absorbed prevents clinical application as a BDS; hence, these materials remain in the development stage.
BDS made of other materials
In recent years, attempts have been made to utilize decellularized tissues as BDSs because of the lack of an immune reaction when transplanted into a living organism[29,30]. The use of decellularized tissues as scaffolds for liver regeneration has been investigated. The bile was reported to drain into the duodenum as a tube for a prolonged period and functioned while the stent was inserted. However, reports of long-term bile duct regeneration and function after stent removal are lacking.
Scaffolds of the same shape as that of the extrahepatic bile duct have been produced using 3D printing[41,42]. The extrahepatic bile duct has been reported to regenerate in a ring shape, but no studies to date have examined bile duct regeneration using these BDSs. Furthermore, there have been efforts to develop an actual bile duct as an organoid in vitro for transplantation[70]. However, it has not been possible to produce organoids of a certain length in the longitudinal direction for clinical use and with a length that can be sutured.
FACTORS TO CONSIDER FOR BDS DEVELOPMENT
Below, we discuss the factors that should be considered in the development of clinically applicable BDSs.
Bile duct wound healing
Bile duct regeneration must occur concurrently with wound healing[40,50,51]. Notably, the natural course of wound healing involves scar contraction. Therefore, if the BDS does not reduce scar contraction, the migrating cell mass results in scar contraction and lumen narrowing after removal of the BDS or decomposition and absorption[35,51]. For the BDS to promote bile duct regeneration, the BDS implant must be guided into the regeneration process while maintaining the shape of the bile duct rather than increasing scarring of the cell mass[40]. As such, which allows the cell mass that regenerates the bile duct to maintain the shape of the bile duct when the BDS is absorbed or removed.
A BDS made of a non-bioabsorbable material that has been present in the body for a prolonged period retains its shape until the BDS is removed, but the lumen is prone to clogging by bile plugs[20-22]. Further, the anastomotic site with the native bile duct will be narrowed due to connective tissue growth[50,51]. Current bile duct regeneration methods using BDSs suggest that after the cell mass gathers around the foreign body and the BDS forms the shape of the bile duct, the cell mass regenerates as a bile duct after BDS removal[25]. If the BDS cannot maintain the shape of the bile duct, a stent may be used instead.
Studies have demonstrated that bone marrow-derived and adipose-derived cells are effective in suppressing scar contraction[72,73]. In addition, it has been reported that fibrosis is suppressed by controlling the function of macrophages that have migrated to the injured region during the remodeling period of wound healing[40,51]. However, methods for reliably suppressing scar contraction have yet to be developed[72,73]. For bile duct regeneration and retention of normal tissue structure, it is necessary for the dynamics and function of multiple types of cells that have migrated around the BDS to be tightly regulated and to reduce scar contraction.
Bile properties
Compared to blood, bile is more viscous and has a slower velocity[57]. If a BDS is not absorbed in the body, a bile plug may adhere to the BDS at the anastomosis site with the lumen or native bile duct. This results in impaired bile flow and narrowing of the lumen. In studies using Teflon (a non-bioabsorbable material) as a BDS, anticoagulants are often used even for blood. Therefore, further measures are required to prevent bile plug formation. This resembles the insertion of metal or tube stents for the treatment of bile duct stenosis, which often clogs the stent with a bile plug[58,59].
Bile duct regeneration
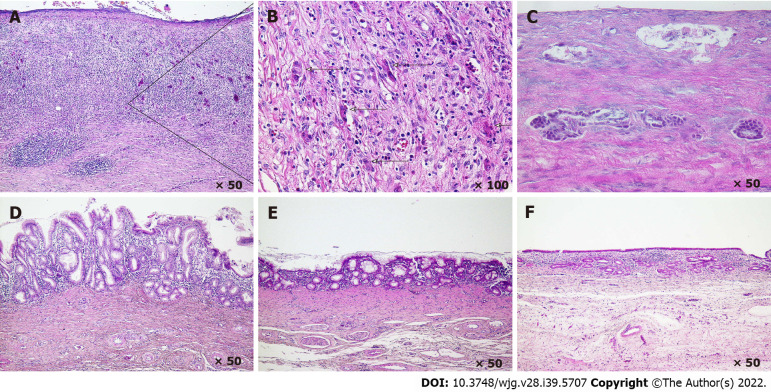
The extrahepatic bile duct is a component of the digestive tract, and the mature bile duct is regenerated via a regeneration process similar to that of the stomach and intestine[36,74,75]. In pigs, it takes approximately 6 mo for bile duct stem/progenitor cells to undergo regeneration to form a mature bile duct similar to the native bile duct. Furthermore, the bile duct epithelium is covered with a layer of cubic columnar epithelial cells[25] (Figures 1 and 2). Therefore, it is controversial in studies that do not show the process of bile duct regeneration, even if BDS transplantation is reported to be successful. For example, in the subsequent regeneration of the T-tube insertion site, the portion of the hole with the T-tube inserted reproduced well without any narrowing. This suggests that small partial bile duct regeneration often occurs without stenosis even if a patch of omentum or blood vessel is applied externally[76]. However, if bile duct defects are extensive and the BDS is placed between the native bile ducts, the cell mass must undergo substantial regeneration from the early stage of bile duct regeneration to regenerate the bile duct without stenosis. Studies have demonstrated that cells attached to the bioabsorbable material regenerate the bile ducts, but the mechanisms by which these cells undergo bile duct regeneration in the presence of the bioabsorbable material remain unclear[24].
Figure 2.
Histology of bile duct regeneration on the outside of the short-term absorption type bile duct substitute. A and B: At 3 wk after bile duct substitute (BDS) implantation, a cell population in the stroma that may comprise the origin of the peribiliary gland is observed; C: At 5 wk after BDS implantation, a ring-shaped biliary gland-like structure is observed in which cell masses that are thought to form peribiliary glands are fused; D: At 7 wk after BDS implantation, many bile duct appendages are observed on the bile passage surface, and the epithelial surface exhibits a high papillary morphology; E: At 12 wk after BDS implantation, the number of peribiliary gland on the bile passage surface is decreased, the appendages begin to fuse, and the epithelial surface becomes more even; F: At 6 mo after BDS implantation, the epithelial surface becomes a single layer of cubic columnar epithelium, similar to the native bile duct.
Immature cells attached to the scaffold migrate using the scaffold of the BDS as a foreign substance[40,50]. These cell masses first form an assembly of the peribiliary gland[25,74,75]. When good bile duct regeneration is achieved approximately 2 mo after the initial stage of regeneration, a tall papillary shape is formed on the inner surface through which bile passes. In pigs, after approximately 3 mo of bile duct regeneration, these peribiliary glands fuse and the epithelial cells become shorter; within approximately 6 mo, these structures mature into bile ducts that are similar to native bile ducts (Figures 1 and 2)[25].
With regard to the mechanisms of bile duct regeneration in the injured part of the bile duct, activated bile duct cells mobilize immune cells, vascular cells, and mesenchymal cells to the inflamed region as a ductular reaction during bile duct ligation and inflammation[77]. This process is involved in regeneration of the inflamed area. Inflammation-activated bile duct cells secrete chemokines, cytokines, and angiogenic factors, which are involved in wound healing[35,50,51]. Furthermore, reactive ductal cells generated via complex mechanisms depend on the nature and intensity of bile duct injury[35,50,51]. However, further investigations of bile duct regeneration mechanisms in various bile duct injuries, such as circular transplantation of BDS, are required to develop effective BDSs.
Regeneration of anastomotic site
When the anastomosis between a BDS and the native bile duct is narrowed, the flow of bile into the duodenum is obstructed, which limits the clinical application of the BDS. In a normal gastrointestinal anastomosis, a large anastomotic hole and fixed shape that does not experience deformation are prerequisites to prevent narrowing of the anastomosis[78]. Therefore, in surgical practice, a stent is inserted when the anastomotic hole is small[78]. For BDSs made from non-bioabsorbable materials, the extrahepatic bile duct is thin; hence, the anastomotic site with the native bile duct is likely to be narrowed by connective tissue in the absence of stent insertion. To prevent anastomotic stenosis between the BDS and the native bile duct, it may be necessary to insert a stent through the anastomotic site to maintain its shape. Even for BDSs made from bioabsorbable materials, it may be difficult to maintain the shape of the anastomotic site and stent insertion is recommended to prevent stenosis.
Localization of bile duct regeneration to BDS
Three regenerative localizations of the neo-bile duct with respect to the BDS have been identified: Outside the BDS, within part of the BDS itself, and inside the BDS (bile passage surface). If the BDS is present for a prolonged period, chronic inflammation will persist[50,51]. As such, it is unlikely that the cell mass that has migrated due to detection of the BDS as a foreign substance will regenerate into a structure similar to the native bile duct at the site of the BDS in the context of wound healing[20-22,51].
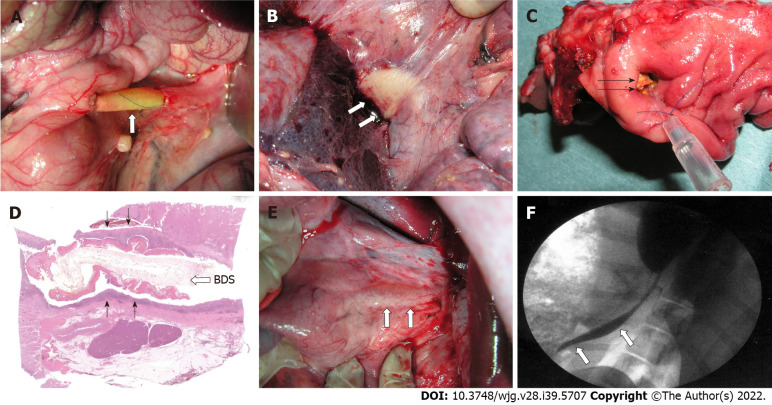
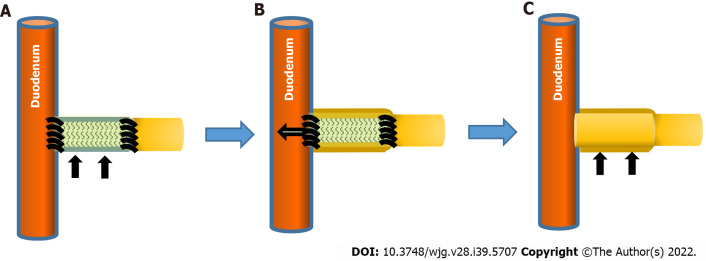
If the BDS is present for a prolonged period, the bile duct does not regenerate outside the BDS or as part of the BDS itself. Bile duct stem cells do not appear to adhere to the luminal surface of non-living non-absorbable materials, such as T-tubes. Given that the bile duct does not tend to narrow after T-tube removal, a cell mass that has migrated outside the BDS is formed. In the absence of BDS, the cell mass is exposed to fresh bile and regenerates as a bile duct, which may promote good bile duct regeneration at the BDS transplant site[25] (Figures 3 and 4).
Figure 3.
Bile duct substitutes using bioabsorbable material (synthetic polymer with short absorption period). A: A bile duct substitute (BDS) using bioabsorbable material is implanted to bypass the extrahepatic bile duct (3 cm in size). Three weeks post-BDS implantation; B: White cell clusters are observed on the outside of the BDS; C: A vulnerable BDS is observed from the duodenal side; D: Dark purple connective tissue is noted on the outside of the BDS; E: At 6 mo after BDS implantation, the neo-bile duct is macroscopically similar to the natural common bile duct have been regenerated (arrow); F: Cholangiography (6 mo after BDS implantation). The BDS implant and anastomotic site become unknown, and the contrast medium flows smoothly into the duodenum (white arrows).
Figure 4.
Regeneration of the neo-bile duct outside the short-term absorption type bile duct substitute. A: Bile duct substitute (BDS) (black arrows) is anastomosed to the native extrahepatic bile duct; B: Immature cells attach around the BDS, forming a cylindrical cell mass outside the BDS. The bioabsorbable polymer that comprise BDS becomes fragile in the living body from approximately 3 wk and sheds to the duodenal side; C: After BDS is no longer present at the transplant site, immature cell clusters mature as bile duct cells and the bile ducts are regenerated as tissue (black arrows).
The use of decellularized tissue as a BDS is thought to promote bile duct regeneration by cell adhesion to the luminal surface or inside the scaffold[29,30]. For BDSs made of bioabsorbable materials with a short absorption period, cell clusters contributing to bile duct regeneration migrate to the outside of the BDS and regenerate the bile duct. This bioabsorbable material may become fragile in approximately 3 wk and shed to the duodenal side, after which the cells surrounding the BDS regenerate the bile duct[25] (Figures 3 and 4). Although further research is needed, the extant literature suggests that the cell mass forms a ring-shaped structure more rapidly than during chronic inflammation and subsequently disappears from the site. Collectively, these findings suggest that bioabsorbable materials that induce good bile duct regeneration may be harnessed as effective BDSs.
RESEARCH LIMITATIONS
One study reported that when a stent was placed in the BDS, bile flowed through the stent for a certain period, resulting in a successful BDS. However, the study did not demonstrate bile duct regeneration. This process is similar to that of stent insertion during the treatment of benign bile duct stenosis. Nevertheless, the alternative portion eventually becomes stenotic and clinically unusable over a prolonged period. Our analysis was unable to identify these issues accurately. Although numerous studies using various BDSs have been conducted, the lack of success highlights the limitations of the field. Moreover, we did not analyze successful cases in small animals or studies using a small number of large animals.
FUTURE PERSPECTIVES
Extant research has provided novel insights into the mechanisms of repair after tissue damage[75]. If the injured area does not undergo normal repair, a high degree of fibrosis will occur in the injured area, resulting in scar formation at the site. For bile duct injuries, the injured area or the BDS implant may become stenotic. For the regeneration of a bile duct similar to the native bile duct at the injury site, cells that have migrated to the bile duct injury site must suppress scar contraction, similar to the regeneration of other organs. In this regard, it is necessary to create a niche for bile duct regeneration similar to that of the native bile duct[73,75]. In addition, chronic inflammation is associated with prolonged and severe fibrosis, resulting in scar formation. Therefore, a BDS should not remain at the transplantation site for a prolonged period.
Based on these caveats, two methods can be considered for regenerating a bile duct similar to the native bile duct at the BDS transplantation site. The first involves the use of a short-term absorption type of bioabsorbable BDS, in which cells that have migrated to repair bile duct injury (BDS transplantation site) form the shape of the bile duct via a foreign body reaction. Ultimately, the BDS will no longer be present at that site and chronic inflammation does not occur (i.e., the bile duct regenerates outside the BDS)[25] (Figure 4). The second method involves bile duct stem/progenitor cells adhering to part of the BDS itself, and wound healing is regulated such that bile duct regeneration progresses well while the BDS is being absorbed. Therefore, it is necessary to develop a method to control wound healing so that the scaffold portion of the decellularized tissue and adhering cells do not cause scar contraction. In summary, bioabsorbable BDSs for bile duct regeneration outside the bile duct constitute a promising development that will be clinically useful in the future.
CONCLUSION
To date, successful BDSs have not been developed. This is predominantly due to poor mechanistic understanding and lack of methods for regulating bile duct wound healing and bile duct regeneration. As an alternative to the extrahepatic bile duct, bioabsorbable materials can be used to form the shape of the bile duct, and the cell mass forming the shape of the bile duct can migrate to the external surface of this structure. Once the cell mass was able to maintain the shape of the bile duct, the BDS acting as a scaffold was removed. The development of BDSs that enable this process will permit the treatment of a wide range of bile duct defects.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Naoe Akimoto for her excellent technical assistance.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: May 24, 2022
First decision: August 1, 2022
Article in press: September 22, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Feier F, Brazil; Ferreira GSA, Brazil; Qin J, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
Contributor Information
Mitsuo Miyazawa, Department of Surgery, Teikyo University Mizonokuch Hospital, Kanagawa 213-8507, Japan. mmiyazawa@med.teikyo-u.ac.jp.
Masayasu Aikawa, Department of Surgery, Saitama Medical University International Medical Center, Saitama 350-1298, Japan.
Junpei Takashima, Department of Surgery, Teikyo University Mizonokuch Hospital, Kanagawa 213-8507, Japan.
Hirotoshi Kobayashi, Department of Surgery, Teikyo University Mizonokuch Hospital, Kanagawa 213-8507, Japan.
Shunsuke Ohnishi, Department of Gastroenterology and Hepatology, Hokkaido University Faculty of Medicine and Graduate School of Medicine, Sapporo 060-8638, Japan.
Yoshito Ikada, Department of Bioenvironmental Medicine, Nara Medical University, Nara 634-8521, Japan.
References
- 1.Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, D'Angelica MI, Balduzzi A, Bassi C, Björnsson B, Boggi U, Callery MP, Del Chiaro M, Coimbra FJ, Conrad C, Cook A, Coppola A, Dervenis C, Dokmak S, Edil BH, Edwin B, Giulianotti PC, Han HS, Hansen PD, van der Heijde N, van Hilst J, Hester CA, Hogg ME, Jarufe N, Jeyarajah DR, Keck T, Kim SC, Khatkov IE, Kokudo N, Kooby DA, Korrel M, de Leon FJ, Lluis N, Lof S, Machado MA, Demartines N, Martinie JB, Merchant NB, Molenaar IQ, Moravek C, Mou YP, Nakamura M, Nealon WH, Palanivelu C, Pessaux P, Pitt HA, Polanco PM, Primrose JN, Rawashdeh A, Sanford DE, Senthilnathan P, Shrikhande SV, Stauffer JA, Takaori K, Talamonti MS, Tang CN, Vollmer CM, Wakabayashi G, Walsh RM, Wang SE, Zinner MJ, Wolfgang CL, Zureikat AH, Zwart MJ, Conlon KC, Kendrick ML, Zeh HJ, Hilal MA, Besselink MG International Study Group on Minimally Invasive Pancreas Surgery (I-MIPS) The Miami International Evidence-based Guidelines on Minimally Invasive Pancreas Resection. Ann Surg. 2020;271:1–14. doi: 10.1097/SLA.0000000000003590. [DOI] [PubMed] [Google Scholar]
- 2.Suda K, Nakauchi M, Inaba K, Ishida Y, Uyama I. Minimally invasive surgery for upper gastrointestinal cancer: Our experience and review of the literature. World J Gastroenterol. 2016;22:4626–4637. doi: 10.3748/wjg.v22.i19.4626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hui VW, Guillem JG. Minimal access surgery for rectal cancer: an update. Nat Rev Gastroenterol Hepatol. 2014;11:158–165. doi: 10.1038/nrgastro.2013.203. [DOI] [PubMed] [Google Scholar]
- 4.di Pietro M, Canto MI, Fitzgerald RC. Endoscopic Management of Early Adenocarcinoma and Squamous Cell Carcinoma of the Esophagus: Screening, Diagnosis, and Therapy. Gastroenterology. 2018;154:421–436. doi: 10.1053/j.gastro.2017.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mönig S, Chevallay M, Niclauss N, Zilli T, Fang W, Bansal A, Hoeppner J. Early esophageal cancer: the significance of surgery, endoscopy, and chemoradiation. Ann N Y Acad Sci. 2018;1434:115–123. doi: 10.1111/nyas.13955. [DOI] [PubMed] [Google Scholar]
- 6.Strasberg SM. A three-step conceptual roadmap for avoiding bile duct injury in laparoscopic cholecystectomy: an invited perspective review. J Hepatobiliary Pancreat Sci. 2019;26:123–127. doi: 10.1002/jhbp.616. [DOI] [PubMed] [Google Scholar]
- 7.Rystedt J, Lindell G, Montgomery A. Bile Duct Injuries Associated With 55,134 Cholecystectomies: Treatment and Outcome from a National Perspective. World J Surg. 2016;40:73–80. doi: 10.1007/s00268-015-3281-4. [DOI] [PubMed] [Google Scholar]
- 8.Rose JB, Bilderback P, Raphaeli T, Traverso W, Helton S, Ryan JA Jr, Biehl T. Use the duodenum, it’s right there: a retrospective cohort study comparing biliary reconstruction using either the jejunum or the duodenum. JAMA Surg. 2013;148:860–865. doi: 10.1001/jamasurg.2013.2701. [DOI] [PubMed] [Google Scholar]
- 9.Horgan E. Reconstruction of the Common Bile Duct by end-to-end Anastomosis. Ann Surg. 1931;93:1162–1166. doi: 10.1097/00000658-193106000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pearce AE, Ulin AW, Entine JH, Froio GF. Experimental reconstruction of the extrahepatic biliary system using free venous grafts. Ann Surg. 1951;134:808–814. doi: 10.1097/00000658-195111000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brewer GE. VIII. Hepaticoduodenal Anastomosis. Ann Surg. 1910;51:830–833. doi: 10.1097/00000658-191006000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clements O, Eliahoo J, Kim JU, Taylor-Robinson SD, Khan SA. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: A systematic review and meta-analysis. J Hepatol. 2020;72:95–103. doi: 10.1016/j.jhep.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Tocchi A, Mazzoni G, Liotta G, Lepre L, Cassini D, Miccini M. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1,000 patients. Ann Surg. 2001;234:210–214. doi: 10.1097/00000658-200108000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kubo S, Kinoshita M, Takemura S, Tanaka S, Shinkawa H, Nishioka T, Hamano G, Ito T, Abue M, Aoki M, Nakagawa K, Unno M, Hijioka S, Fujiyoshi T, Shimizu Y, Mizuguchi T, Shirabe K, Nishie A, Oda Y, Takenaka K, Kobarai T, Hisano T, Saiura A, Numao H, Toda M, Kuwae Y, Nakanuma Y, Endo G. Characteristics of printing company workers newly diagnosed with occupational cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2014;21:809–817. doi: 10.1002/jhbp.137. [DOI] [PubMed] [Google Scholar]
- 15.Shea PC Jr, Hubay CA. Experimental Repair of Common Duct Defects Utilizing a Free Vein Graft Over Blakemore-Lord Tubes. Ann Surg. 1948;128:21–29. doi: 10.1097/00000658-194807000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirby CK, Fitts WT Jr. Reconstruction of the bile ducts with an isolated segment of jejunum; an experimental study. Arch Surg (1920) 1950;61:462–468. doi: 10.1001/archsurg.1950.01250020467006. [DOI] [PubMed] [Google Scholar]
- 17.Ulin AW, Shoemaker WC, Entine JH. Vascularized venous grafts in the experimental reconstruction of the common bile duct. Ann Surg. 1955;142:279–282. doi: 10.1097/00000658-195508000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myers RT, Meredith JH, Rhodes J, Gilbert JW. The fate of free grafts in the common bile duct. Ann Surg. 1960;151:776–782. [PMC free article] [PubMed] [Google Scholar]
- 19.Dunphy JE, Stephens FO. Experimental Study of the Effect of Grafts in the Common Duct on Biliary and Hepartic Function. Ann Surg. 1962;155:906–919. doi: 10.1097/00000658-196206000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bergan JJ, Anderson MC, Lounsbury BF. Vascularized polyvinyl sponge prosthesis. Its use to replace the canine common bile duct. Arch Surg. 1962;84:301–305. doi: 10.1001/archsurg.1962.01300210035007. [DOI] [PubMed] [Google Scholar]
- 21.Sherman RT, Jackson TM, Nielson CA, Wilson H. Reconstruction of the common bile duct with an acrylate-amide prosthesis. Ann Surg. 1963;158:420–430. doi: 10.1097/00000658-196309000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mendelowitz DS, Beal JM. Expanded polytetrafluoroethylene in reconstruction of the canine biliary system. Am J Surg. 1982;143:221–224. doi: 10.1016/0002-9610(82)90073-3. [DOI] [PubMed] [Google Scholar]
- 23.Gómez NA, Alvarez LR, Mite A, Andrade JP, Alvarez JR, Vargas PE, Tomalá NE, Vivas AF, Zapatier JA. Repair of bile duct injuries with Gore-Tex vascular grafts: experimental study in dogs. J Gastrointest Surg. 2002;6:116–120. doi: 10.1016/s1091-255x(01)00038-5. [DOI] [PubMed] [Google Scholar]
- 24.Rosen M, Ponsky J, Petras R, Fanning A, Brody F, Duperier F. Small intestinal submucosa as a bioscaffold for biliary tract regeneration. Surgery. 2002;132:480–486. doi: 10.1067/msy.2002.126505. [DOI] [PubMed] [Google Scholar]
- 25.Miyazawa M, Torii T, Toshimitsu Y, Okada K, Koyama I, Ikada Y. A tissue-engineered artificial bile duct grown to resemble the native bile duct. Am J Transplant. 2005;5:1541–1547. doi: 10.1111/j.1600-6143.2005.00845.x. [DOI] [PubMed] [Google Scholar]
- 26.Nau P, Liu J, Ellison EC, Hazey JW, Henn M, Muscarella P, Narula VK, Melvin WS. Novel reconstruction of the extrahepatic biliary tree with a biosynthetic absorbable graft. HPB (Oxford) 2011;13:573–578. doi: 10.1111/j.1477-2574.2011.00337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Q, Tao L, Chen B, Ren H, Hou X, Zhou S, Zhou J, Sun X, Dai J, Ding Y. Extrahepatic bile duct regeneration in pigs using collagen scaffolds loaded with human collagen-binding bFGF. Biomaterials. 2012;33:4298–4308. doi: 10.1016/j.biomaterials.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Tao L, Li Q, Ren H, Chen B, Hou X, Mou L, Zhou S, Zhou J, Sun X, Dai J, Ding Y. Repair of extrahepatic bile duct defect using a collagen patch in a Swine model. Artif Organs. 2015;39:352–360. doi: 10.1111/aor.12388. [DOI] [PubMed] [Google Scholar]
- 29.Cheng Y, Xiong XZ, Zhou RX, Deng YL, Jin YW, Lu J, Li FY, Cheng NS. Repair of a common bile duct defect with a decellularized ureteral graft. World J Gastroenterol. 2016;22:10575–10583. doi: 10.3748/wjg.v22.i48.10575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chakhunashvili K, Kiladze M, G Chakhunashvili D, Karalashvili L, Kakabadze Z. A three-dimensional scaffold from decellularized human umbilical artery for bile duct reconstruction. Ann Ital Chir. 2019;90:165–173. [PubMed] [Google Scholar]
- 31.Rodríguez-Garay EA, Agüero RM, Pisani G, Trbojevich RA, Farroni A, Viglianco RA. Rat model of mild stenosis of the common bile duct. Res Exp Med (Berl) 1996;196:105–116. doi: 10.1007/BF02576832. [DOI] [PubMed] [Google Scholar]
- 32.Şahiner İT, Kendirci M. Retrospective Clinical Study of the Effects of T-Tube Placement for Bile Duct Stricture. Med Sci Monit. 2017;23:4328–4333. doi: 10.12659/MSM.906630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singhi AD, Nikiforova MN, Chennat J, Papachristou GI, Khalid A, Rabinovitz M, Das R, Sarkaria S, Ayasso MS, Wald AI, Monaco SE, Nalesnik M, Ohori NP, Geller D, Tsung A, Zureikat AH, Zeh H, Marsh JW, Hogg M, Lee K, Bartlett DL, Pingpank JF, Humar A, Bahary N, Dasyam AK, Brand R, Fasanella KE, McGrath K, Slivka A. Integrating next-generation sequencing to endoscopic retrograde cholangiopancreatography (ERCP)-obtained biliary specimens improves the detection and management of patients with malignant bile duct strictures. Gut. 2020;69:52–61. doi: 10.1136/gutjnl-2018-317817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bill JG, Mullady DK. Stenting for Benign and Malignant Biliary Strictures. Gastrointest Endosc Clin N Am. 2019;29:215–235. doi: 10.1016/j.giec.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 35.Wynn TA, Ramalingam TR. Mechanisms of fibrosis: therapeutic translation for fibrotic disease. Nat Med. 2012;18:1028–1040. doi: 10.1038/nm.2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cardinale V, Wang Y, Carpino G, Mendel G, Alpini G, Gaudio E, Reid LM, Alvaro D. The biliary tree--a reservoir of multipotent stem cells. Nat Rev Gastroenterol Hepatol. 2012;9:231–240. doi: 10.1038/nrgastro.2012.23. [DOI] [PubMed] [Google Scholar]
- 37.Sutton ME, op den Dries S, Koster MH, Lisman T, Gouw AS, Porte RJ. Regeneration of human extrahepatic biliary epithelium: the peribiliary glands as progenitor cell compartment. Liver Int. 2012;32:554–559. doi: 10.1111/j.1478-3231.2011.02721.x. [DOI] [PubMed] [Google Scholar]
- 38.Barber WH. Choledocho-enterostomy and postoperative dilation of the bile-ducts: An experimental study. Ann Surg. 1919;70:530–534. doi: 10.1097/00000658-191911000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yannas IV, Tzeranis DS, So PTC. Regeneration of injured skin and peripheral nerves requires control of wound contraction, not scar formation. Wound Repair Regen. 2017;25:177–191. doi: 10.1111/wrr.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature. 2008;453:314–321. doi: 10.1038/nature07039. [DOI] [PubMed] [Google Scholar]
- 41.Li H, Yin Y, Xiang Y, Liu H, Guo R. A novel 3D printing PCL/GelMA scaffold containing USPIO for MRI-guided bile duct repair. Biomed Mater. 2020;15:045004. doi: 10.1088/1748-605X/ab797a. [DOI] [PubMed] [Google Scholar]
- 42.Dhir V, Itoi T, Fockens P, Perez-Miranda M, Khashab MA, Seo DW, Yang AM, Lawrence KY, Maydeo A. Novel ex vivo model for hands-on teaching of and training in EUS-guided biliary drainage: creation of "Mumbai EUS" stereolithography/3D printing bile duct prototype (with videos) Gastrointest Endosc. 2015;81:440–446. doi: 10.1016/j.gie.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 43.Santos M, Smith ML, Hughes CW, Riley PA Jr. Reconstruction of the bile ducts: an experimental study using free arterial grafts and nylon mesh tubes. Surgery. 1957;42:462–473. [PubMed] [Google Scholar]
- 44.Belzer FO, Watts JM, Ross HB, Dunphy JE. Auto-reconstruction of the common bile duct after venous patch graft. Ann Surg. 1965;162:346–355. doi: 10.1097/00000658-196509000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rieger IT, Wahl FJ, Hass GM. Experimental substitution of the common bile duct with an autologous ureteral graft. J Urol. 1953;69:487–491. doi: 10.1016/S0022-5347(17)68099-6. [DOI] [PubMed] [Google Scholar]
- 46.Schatten WE, Cramer LM, Herbsman H, Swarm RL. Experimental reconstruction of the common bile duct with split thickness skin grafts. Surg Gynecol Obstet. 1957;105:747–753. [PubMed] [Google Scholar]
- 47.Lindenauer SM, Child CG 3rd. Vascularized venous autografts in common bile duct reconstruction. Arch Surg. 1966;92:749–751. doi: 10.1001/archsurg.1966.01320230097018. [DOI] [PubMed] [Google Scholar]
- 48.Palmes D, Wolters H, Spiegel HU, M Ller E, Minin E, Heistermann HP. Morphological changes during creation of a neo-bile duct using a vein and a biodegradable endoluminal stent. J Invest Surg. 2009;22:435–444. doi: 10.3109/08941930903410791. [DOI] [PubMed] [Google Scholar]
- 49.Liang YL, Yu YC, Liu K, Wang WJ, Ying JB, Wang YF, Cai XJ. Repair of bile duct defect with degradable stent and autologous tissue in a porcine model. World J Gastroenterol. 2012;18:5205–5210. doi: 10.3748/wjg.v18.i37.5205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roehlen N, Crouchet E, Baumert TF. Liver Fibrosis: Mechanistic Concepts and Therapeutic Perspectives. Cells. 2020;9 doi: 10.3390/cells9040875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tomasek JJ, Gabbiani G, Hinz B, Chaponnier C, Brown RA. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat Rev Mol Cell Biol. 2002;3:349–363. doi: 10.1038/nrm809. [DOI] [PubMed] [Google Scholar]
- 52.Thomas JP, Metropol HJ, Myers RT. Teflon patch graft for reconstruction of the extrahepatic bile ducts. Ann Surg. 1964;160:967–970. doi: 10.1097/00000658-196412000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cochran EB, Ferguson EF Jr, Moseley T. Reconstruction of the common bile duct with a collagen-dacron prosthesis: mucosal regeneration in dogs. Am Surg. 1966;32:757–761. [PubMed] [Google Scholar]
- 54.Grindlay JH. Method of making tubes of polyethylene film for use in anastomosis of the common bile duct, trachea, and pelvic colon. Surgery. 1948;24:22–29. [PubMed] [Google Scholar]
- 55.Reynolds RM, Reynolds RP. Choledochoduodenostomy using a polyethylene tube prosthesis. J Mich State Med Soc. 1958;57:1724–1726. [PubMed] [Google Scholar]
- 56.Abir F, Barkhordarian S, Sumpio BE. Efficacy of dextran solutions in vascular surgery. Vasc Endovascular Surg. 2004;38:483–491. doi: 10.1177/153857440403800601. [DOI] [PubMed] [Google Scholar]
- 57.Minh NN, Obara H. Porcine bile viscosity is proportional to density. Biorheology. 2020;57:27–36. doi: 10.3233/BIR-190238. [DOI] [PubMed] [Google Scholar]
- 58.Schreuder AM, Busch OR, Besselink MG, Ignatavicius P, Gulbinas A, Barauskas G, Gouma DJ, van Gulik TM. Long-Term Impact of Iatrogenic Bile Duct Injury. Dig Surg. 2020;37:10–21. doi: 10.1159/000496432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Berkel AM, van Marle J, Groen AK, Bruno MJ. Mechanisms of biliary stent clogging: confocal laser scanning and scanning electron microscopy. Endoscopy. 2005;37:729–734. doi: 10.1055/s-2005-870131. [DOI] [PubMed] [Google Scholar]
- 60.Langer R, Vacanti JP. Tissue engineering. Science. 1993;260:920–926. doi: 10.1126/science.8493529. [DOI] [PubMed] [Google Scholar]
- 61.Zhang L, Hui L. Bioengineering: Bile ducts regenerated. Nature. 2017;547:171–172. doi: 10.1038/547171a. [DOI] [PubMed] [Google Scholar]
- 62.Tanimoto Y, Tashiro H, Mikuriya Y, Kuroda S, Hashimoto M, Kobayashi T, Taniura T, Ohdan H. Radiopaque biodegradable stent for duct-to-duct biliary reconstruction in pigs. Langenbecks Arch Surg. 2016;401:513–517. doi: 10.1007/s00423-016-1442-z. [DOI] [PubMed] [Google Scholar]
- 63.de Abreu GF, Batista LL, Adeodato DC, de Albuquerque AV, Ferraz-Carvalho RS, de Lima RP, de Souza VS, de Carvalho GL, Aguiar J. Use of bacterial cellulose film for repair of bile duct injury in pigs. J Biomater Appl. 2020;35:331–341. doi: 10.1177/0885328220928221. [DOI] [PubMed] [Google Scholar]
- 64.Pérez Alonso AJ, Del Olmo Rivas C, Romero IM, Cañizares Garcia FJ, Poyatos PT. Tissue-engineering repair of extrahepatic bile ducts. J Surg Res. 2013;179:18–21. doi: 10.1016/j.jss.2012.08.035. [DOI] [PubMed] [Google Scholar]
- 65.Gómez NA, Zapatier JA, Vargas PE. Re: "Small intestinal submucosa as a bioscaffold for biliary tract regeneration". Surgery. 2004;135:460. doi: 10.1016/j.surg.2003.06.004. [DOI] [PubMed] [Google Scholar]
- 66.Nakashima S, Nakamura T, Miyagawa K, Yoshikawa T, Kin S, Kuriu Y, Nakase Y, Sakakura C, Otsuji E, Hagiwara A, Yamagishi H. In situ tissue engineering of the bile duct using polypropylene mesh-collagen tubes. Int J Artif Organs. 2007;30:75–85. doi: 10.1177/039139880703000110. [DOI] [PubMed] [Google Scholar]
- 67.Takimoto Y, Dixit V, Arthur M, Gitnick G. De novo liver tissue formation in rats using a novel collagen-polypropylene scaffold. Cell Transplant. 2003;12:413–421. doi: 10.3727/000000003108746966. [DOI] [PubMed] [Google Scholar]
- 68.Yannas IV, Tzeranis D, So PT. Surface biology of collagen scaffold explains blocking of wound contraction and regeneration of skin and peripheral nerves. Biomed Mater. 2015;11:014106. doi: 10.1088/1748-6041/11/1/014106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Miyazawa M, Aikawa M, Okada K, Watanabe Y, Okamoto K, Santosh S, Yamaguchi S, Koyama I, Ikada Y. An Artificial Bile Duct Made of Bioabsorbable Polymer: A Viable Substitute for Narrowed Portion of the Extrahepatic Bile Duct. Int Surg. 2015;100:1408–1413. [Google Scholar]
- 70.Langer R. Implantable controlled release systems. Pharmacol Ther. 1983;21:35–51. doi: 10.1016/0163-7258(83)90066-9. [DOI] [PubMed] [Google Scholar]
- 71.Sampaziotis F, Muraro D, Tysoe OC, Sawiak S, Beach TE, Godfrey EM, Upponi SS, Brevini T, Wesley BT, Garcia-Bernardo J, Mahbubani K, Canu G, Gieseck R 3rd, Berntsen NL, Mulcahy VL, Crick K, Fear C, Robinson S, Swift L, Gambardella L, Bargehr J, Ortmann D, Brown SE, Osnato A, Murphy MP, Corbett G, Gelson WTH, Mells GF, Humphreys P, Davies SE, Amin I, Gibbs P, Sinha S, Teichmann SA, Butler AJ, See TC, Melum E, Watson CJE, Saeb-Parsy K, Vallier L. Cholangiocyte organoids can repair bile ducts after transplantation in the human liver. Science. 2021;371:839–846. doi: 10.1126/science.aaz6964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fu X, Liu G, Halim A, Ju Y, Luo Q, Song AG. Mesenchymal Stem Cell Migration and Tissue Repair. Cells. 2019;8 doi: 10.3390/cells8080784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ding BS, Cao Z, Lis R, Nolan DJ, Guo P, Simons M, Penfold ME, Shido K, Rabbany SY, Rafii S. Divergent angiocrine signals from vascular niche balance liver regeneration and fibrosis. Nature. 2014;505:97–102. doi: 10.1038/nature12681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.de Jong IEM, Matton APM, van Praagh JB, van Haaften WT, Wiersema-Buist J, van Wijk LA, Oosterhuis D, Iswandana R, Suriguga S, Overi D, Lisman T, Carpino G, Gouw ASH, Olinga P, Gaudio E, Porte RJ. Peribiliary Glands Are Key in Regeneration of the Human Biliary Epithelium After Severe Bile Duct Injury. Hepatology. 2019;69:1719–1734. doi: 10.1002/hep.30365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Carpino G, Nevi L, Overi D, Cardinale V, Lu WY, Di Matteo S, Safarikia S, Berloco PB, Venere R, Onori P, Franchitto A, Forbes SJ, Alvaro D, Gaudio E. Peribiliary Gland Niche Participates in Biliary Tree Regeneration in Mouse and in Human Primary Sclerosing Cholangitis. Hepatology. 2020;71:972–989. doi: 10.1002/hep.30871. [DOI] [PubMed] [Google Scholar]
- 76.Wang AW, Prieto JM, Cauvi DM, Bickler SW, De Maio A. The Greater Omentum-A Vibrant and Enigmatic Immunologic Organ Involved in Injury and Infection Resolution. Shock. 2020;53:384–390. doi: 10.1097/SHK.0000000000001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Alvaro D, Mancino MG, Glaser S, Gaudio E, Marzioni M, Francis H, Alpini G. Proliferating cholangiocytes: a neuroendocrine compartment in the diseased liver. Gastroenterology. 2007;132:415–431. doi: 10.1053/j.gastro.2006.07.023. [DOI] [PubMed] [Google Scholar]
- 78.Peng SY, Wang JW, Hong DF, Liu YB, Wang YF. Binding pancreaticoenteric anastomosis: from binding pancreaticojejunostomy to binding pancreaticogastrostomy. Updates Surg. 2011;63:69–74. doi: 10.1007/s13304-011-0067-6. [DOI] [PubMed] [Google Scholar]