Abstract
Background
The optimal side branch (SB) treatment strategy after simple crossover stenting in bifurcation lesions is still controversial.
Objectives
The purpose of this study was to compare the long-term outcomes of a 1-stent strategy with simple crossover alone versus with an additional SB–opening procedure in patients with left main (LM) and non-LM coronary bifurcation lesions.
Methods
Patients who underwent percutaneous coronary intervention with a 1-stent strategy for bifurcation lesions including LM were selected from the COBIS (Coronary Bifurcation Stenting) III registry and divided into the simple crossover–alone group and SB-opening group. Clinical outcomes were assessed by the 5-year rate of target lesion failure (a composite of cardiac death, target vessel myocardial infarction, and target lesion repeat revascularization).
Results
Among 2,194 patients who underwent the 1-stent strategy, 1,685 (76.8%) patients were treated with simple crossover alone, and 509 (23.2%) patients were treated with an additional SB-opening procedure. Although the baseline SB angiographic disease was more severe in the SB-opening group, the final lumen diameter of the SB was larger. The 5-year observed target lesion failure rate was similar between the 2 groups (7.0% in the simple crossover vs. 6.7% in SB-opening group; hazard ratio: 0.99; 95% confidence interval: 0.66 to 1.48; p = 0.947), even in the subgroup analyses including LM (9.5% vs. 11.3%; p = 0.442) and true bifurcation (5.3% vs. 7.8%; p = 0.362). The results were not changed after an inverse probability of treatment weighting adjustment. There was no difference in the overall and SB-related target lesion revascularization rate in both groups.
Conclusions
The long-term clinical outcome of the 1-stent strategy with simple crossover alone for coronary bifurcation lesions was acceptable compared to those of additional SB-opening procedures. (Korean Coronary Bifurcation Stenting [COBIS] Registry III [COBIS III]; NCT03068494)
Key Words: bifurcation disease, clinical outcome, percutaneous coronary intervention
Abbreviations and Acronyms: CI, confidence interval; DES, drug-eluting stent(s); DS, diameter stenosis; FKI, final kissing inflation; HR, hazard ratio; IPTW, inverse probability of treatment weighting; LM, left main; MI, myocardial infarction; MLD, minimum lumen diameter; MV, main vessel; PCI, percutaneous coronary intervention; POT, proximal optimizing technique; QCA, quantitative coronary angiography; RVD, reference vessel diameter; SB, side branch; TLF, target lesion failure; TLR, target lesion repeat revascularization
Central Illustration
With the results of randomized trials, which demonstrated that the routine 2-stent strategy did not show better clinical outcomes than the 1-stent strategy in bifurcation lesions (1,2), the usual percutaneous coronary intervention (PCI) strategy for coronary bifurcation disease is a provisional approach. However, the standard technique of the provisional strategy is not clear, and there are limited data on the long-term outcome of the side branch (SB) treatment strategy after the 1-stent strategy with simple main vessel (MV) crossover in bifurcation lesions. Because there were several studies showing completely opposite results about the clinical outcome after SB opening (3, 4, 5, 6), and a functional anatomic discrepancy has been confirmed in the angiographically compromised SB after simple crossover stenting in bifurcation lesions (7, 8, 9), a routine SB-opening procedure after simple MV crossover stenting in non–left main (LM) bifurcation lesions is generally not recommended (10). There are also limited clinical outcome data on the role of SB-opening procedures after the 1-stent strategy in LM bifurcation lesions (8). Therefore, the present study sought to compare the long-term outcomes of the 1-stent strategy with simple crossover alone versus with an additional SB-opening procedure in a real-world, large bifurcation registry including LM and non-LM bifurcation lesions.
Methods
Study design and population
The COBIS III (Coronary Bifurcation Stenting III) registry is a retrospective, multicenter, observational, real-world registry of patients with bifurcation lesions who underwent PCI with second-generation drug-eluting stents (DES) (NCT03068494). Between January 2010 and December 2014, a total of 2,648 patients were consecutively enrolled from 21 centers in the Republic of Korea. In the analysis of this study, the patients who underwent PCI with the 1-stent strategy without additional SB stenting were enrolled. The patients who underwent the 2-stent strategy were excluded, and their features are described in Supplemental Tables 1 and 2. The patients were divided into 2 groups, including a simple crossover–alone group and SB-opening group, and the 5-year clinical outcomes were compared. This registry included patients who were at least 19 years old and had any type of coronary bifurcation lesion in a major epicardial artery treated solely with second-generation DESs and an MV diameter of ≥2.5 mm and SB diameter of ≥2.3 mm confirmed by core laboratory quantitative coronary angiography (QCA) analysis. The major exclusion criteria were cardiogenic shock or cardiopulmonary resuscitation during hospitalization, protected LM disease, and severe left ventricular systolic dysfunction (ejection fraction: <30%). This registry was supported by the Korean Bifurcation Club and Korean Society of Interventional Cardiology. The Institutional Review Board of each hospital approved the study protocol and waived the requirement for written informed consent due to the retrospective nature of the study.
PCI procedure
Coronary interventions were performed in accordance with the relevant standard guidelines at the time of each procedure. All patients received loading doses of aspirin (300 mg) and P2Y12 inhibitors (clopidogrel 300 to 600 mg, prasugrel 60 mg, or ticagrelor 180 mg) before the PCI unless they had previously received these antiplatelet medications. Anticoagulation was performed using low-molecular-weight heparin or unfractionated heparin to achieve an activated clotting time of 250 to 300 s during the PCI. The treatment strategies after a 1-stent technique (proximal optimization technique [POT], final kissing inflation [FKI] with or without POT, and only SB opening), access site, type of DES, use of glycoprotein IIb/IIIa inhibitors, and use of intravascular imaging or an invasive physiologic assessment were all left to the operators’ discretion. After the procedure, 100 mg of aspirin was continued indefinitely, and the maintenance duration of clopidogrel (75 mg/day), prasugrel (10 mg/day), or ticagrelor (90 mg twice daily) was also at the operators’ discretion.
Data collection and QCA analysis
Information about the patient demographics, medications, laboratory data, angiographic data, procedural data, and outcomes was collected using a web-based reporting system. Additional information was obtained by further inquiry into the medical records or by telephone contact, if necessary.
All baseline and procedural coronary angiograms were reviewed and analyzed quantitatively by an angiographic core laboratory (Heart Vascular Stroke Institute, Samsung Medical Center, Seoul, Republic of Korea) with a validated automated edge-detection system (Centricity CA 1000, GE, Waukesha, Wisconsin). Bifurcation lesions were classified according to the Medina classification and divided into 3 segments for a QCA analysis: proximal MV, distal MV, and SB (11). True bifurcation lesions were defined as Medina classification types 1.1.1, 1.0.1, and 0.1.1. For both the pre- and post-procedures, the minimum lumen diameter (MLD), reference vessel diameter (RVD), and lesion length for each vessel were measured, and the percent diameter stenosis (%DS) for each vessel was calculated as: 100 × (RVD − MLD)/RVD.
Study outcomes and definitions
The primary clinical outcome was a target lesion failure (TLF)—the composite endpoint of death from cardiac causes, a target vessel myocardial infarction (MI), or target lesion repeat revascularization (TLR). Various secondary clinical outcomes were also assessed, including death (any cause, cardiac cause, or noncardiac cause), MI (any cause or target vessel MI), target vessel revascularization, TLR, and stent thrombosis. Death was considered as having a cardiac cause unless an unequivocal noncardiac cause could be established. A spontaneous MI was defined as an elevation of a creatine kinase–myocardial band or a troponin level greater than the upper limit of normal with concomitant ischemic symptoms or electrocardiography findings indicative of ischemia that was not related to the index procedure. TLR was defined as a repeat revascularization with a PCI or coronary artery bypass surgery for restenosis of the entire segment involving the implanted stent and within 5 mm of the distal and proximal margins of the stent and SB ostium. The definition of a stent thrombosis was assessed according to the Academic Research Consortium definition (12).
Statistical analysis
Continuous variables were compared between the groups using Student’s t-test and are presented as the mean ± SD. Categorical data were compared between the groups using the chi-square test and are presented as numbers and relative frequencies. The cumulative incidence of clinical events are presented as a Kaplan-Meier estimate, and the significance level was assessed with a log-rank test. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using Cox proportional hazard models, and the proportional hazards assumptions of the HRs in the Cox proportional hazards models were graphically inspected in the “log minus log” plot and were also tested by Schoenfeld residuals. We fitted weighted Cox proportional hazards models using the inverse probability of treatment weighting (IPTW) approach (13). The propensity scores were estimated without regard to the outcomes with a multiple logistic regression analysis. The distribution of the propensity score is provided in Supplemental Figure 1 for both groups. A full nonparsimonious model was developed that includes the covariates in Tables 1 and 2 except QCA data. All probability values are 2-sided, and p values of <0.05 were considered statistically significant. Statistical analyses were performed using R statistical software, version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria).
Table 1.
Baseline Characteristics of Patients
| Simple Crossover (n = 1685) | SB Opening (n = 509) | p Value | |
|---|---|---|---|
| Age, yrs | 63.38 ± 11.09 | 63.67 ± 10.58 | 0.595 |
| Men | 1,282 (76.1) | 400 (78.6) | 0.267 |
| Hypertension | 961 (57.0) | 289 (56.8) | 0.960 |
| Diabetes mellitus | 562 (33.4) | 167 (32.8) | 0.861 |
| Dyslipidemia | 628 (37.3) | 207 (40.7) | 0.183 |
| Current smoker | 527 (31.3) | 152 (29.9) | 0.582 |
| Previous PCI | 187 (11.1) | 70 (13.8) | 0.120 |
| Previous stroke | 122 (7.2) | 28 (5.5) | 0.207 |
| Previous heart failure | 11 (0.7) | 4 (0.8) | 0.760 |
| Ejection fraction, % | 58.43 ± 10.17 | 59.41 ± 8.77 | 0.048 |
| Clinical presentation | 0.091 | ||
| Stable angina | 636 (37.7) | 214 (42.0) | |
| Acute coronary syndrome | 1,049 (62.3) | 295 (58.0) | |
| Discharge medications | |||
| Aspirin | 1,660 (98.5) | 500 (98.6) | 0.998 |
| P2Y12 inhibitor | 1,664 (98.8) | 502 (99.0) | 0.804 |
| Beta-blocker | 1,035 (61.4) | 285 (56.0) | 0.032 |
| Calcium-channel blocker | 130 (7.7) | 44 (8.7) | 0.544 |
| ACE inhibitor or ARB | 1,050 (62.3) | 297 (58.3) | 0.119 |
| Statin | 1,514 (89.9) | 449 (88.2) | 0.330 |
Values are mean ± SD or n (%).
ACE = angiotensin-converting enzyme; ARB = angiotensin receptor blocker; PCI = percutaneous coronary intervention.
Table 2.
Baseline Lesion and Procedural Characteristics
| Simple Crossover (n = 1,685) | SB Opening (n = 509) | p Value | |
|---|---|---|---|
| Location of bifurcated vessel | <0.001 | ||
| LM | 489 (29.0) | 193 (37.9) | |
| LAD | 796 (47.2) | 241 (47.3) | |
| LCx | 276 (16.4) | 50 (9.8) | |
| RCA | 124 (7.4) | 25 (4.9) | |
| Medina classification | <0.001 | ||
| 0.0.1 | 14 (0.8) | 31 (6.1) | |
| 0.1.0 | 468 (27.8) | 90 (17.7) | |
| 0.1.1 | 113 (6.7) | 42 (8.3) | |
| 1.0.0 | 263 (15.6) | 26 (5.1) | |
| 1.0.1 | 97 (5.8) | 38 (7.5) | |
| 1.1.0 | 340 (20.2) | 65 (12.8) | |
| 1.1.1 | 390 (23.1) | 217 (42.6) | |
| True bifurcation (SB disease) | 600 (35.6) | 297 (58.3) | <0.001 |
| DES type | 0.039 | ||
| EES | 799 (47.4) | 236 (46.4) | |
| ZES | 459 (27.2) | 151 (29.7) | |
| BES | 339 (20.1) | 110 (21.6) | |
| Others | 88 (5.2) | 12 (2.4) | |
| Maximal diameter of MV stents, mm | 3.34 ± 0.62 | 3.42 ± 0.62 | 0.014 |
| Cumulative length of MV stents, mm | 28.87 ± 13.79 | 27.36 ± 12.52 | 0.022 |
| Final kissing balloon | 0 (0.0) | 391 (76.8) | <0.001 |
| Proximal optimization technique | 485 (28.8) | 146 (28.7) | 0.998 |
| Use of intravascular ultrasound | 601 (35.7) | 215 (42.2) | 0.008 |
| QCA | |||
| Pre-procedure | |||
| Reference diameter of PV, mm | 3.56 ± 0.62 | 3.63 ± 0.61 | 0.116 |
| Reference diameter of MV, mm | 3.22 ± 0.48 | 3.26 ± 0.46 | 0.106 |
| Reference diameter of SB, mm | 2.57 ± 0.44 | 2.63 ± 0.43 | 0.013 |
| MLD of PV, mm | 1.79 ± 1.18 | 1.73 ± 1.04 | 0.306 |
| MLD of MV, mm | 0.81 ± 0.48 | 0.86 ± 0.43 | 0.022 |
| MLD of SB, mm | 1.65 ± 0.82 | 1.44 ± 0.81 | <0.001 |
| Diameter stenosis of PV, % | 50.60 ± 29.69 | 52.52 ± 26.71 | 0.166 |
| Diameter stenosis of MV, % | 74.83 ± 14.40 | 73.51 ± 12.53 | 0.046 |
| Diameter stenosis of SB, % | 37.49 ± 26.06 | 46.61 ± 25.90 | <0.001 |
| Lesion length of MV, mm | 19.40 ± 10.38 | 16.82 ± 8.94 | <0.001 |
| Lesion length of SB, mm | 3.80 ± 5.94 | 5.20 ± 5.90 | <0.001 |
| Final | |||
| MLD of PV, mm | 3.59 ± 0.60 | 3.67 ± 0.58 | 0.007 |
| MLD of MV, mm | 2.77 ± 0.49 | 2.78 ± 0.42 | 0.758 |
| MLD of SB, mm | 1.52 ± 0.81 | 1.69 ± 0.70 | <0.001 |
| Diameter stenosis of PV, % | 11.26 ± 9.02 | 10.16 ± 9.00 | 0.015 |
| Diameter stenosis of MV, % | 15.26 ± 10.36 | 15.86 ± 9.22 | 0.213 |
| Diameter stenosis of SB, % | 42.56 ± 26.23 | 37.21 ± 21.84 | <0.001 |
Values are n (%) or mean ± SD. The number, length, and diameter of the stents were all calculated per lesion.
Results
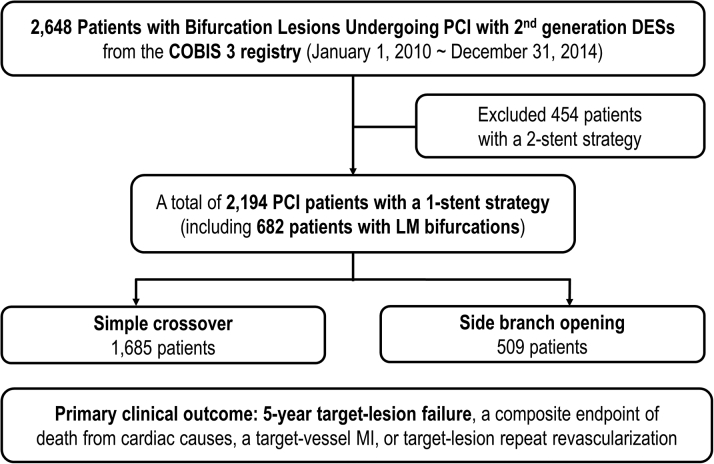
Characteristics of the study patients and lesions
A total of 2,194 patients who underwent PCI with the 1-stent strategy for bifurcation lesions were enrolled from the COBIS III registry. Among them, 1,685 (76.8%) patients were treated with simple crossover alone, and 509 (23.2%) patients were treated with an additional SB-opening procedure (Figure 1). The baseline demographics and clinical characteristics of the study population are shown in Table 1. There was no significant difference in the patients’ clinical characteristics except the ejection fraction between the 2 groups. Table 2 shows the lesion characteristics and procedural results of the study population. At the lesion level before the PCI, the RVD of the SB, MLD of the MV, and %DS of the SB were smaller, and the lesion length of the SB was shorter in the simple crossover group. In addition, the incidence of a true bifurcation was lower in the simple crossover group (simple crossover vs. SB opening: 35.6% vs. 58.3%, p < 0.001). The final MLD of the SB was smaller (1.52 mm vs. 1.69 mm; p < 0.001) and %DS of the SB was larger (42.56% vs. 37.21%; p < 0.001) in the simple crossover group. Intravascular ultrasound was used more frequently in the SB-opening group than the simple crossover group (45.2% vs. 35.7%; p = 0.008).
Figure 1.
Study Flow Chart
COBIS = Coronary Bifurcation Stenting; DES = drug-eluting stent; FKI = final kissing inflation; LM = left main; MI = myocardial infarction; PCI = percutaneous coronary intervention; POT = proximal optimization technique; SB = side branch.
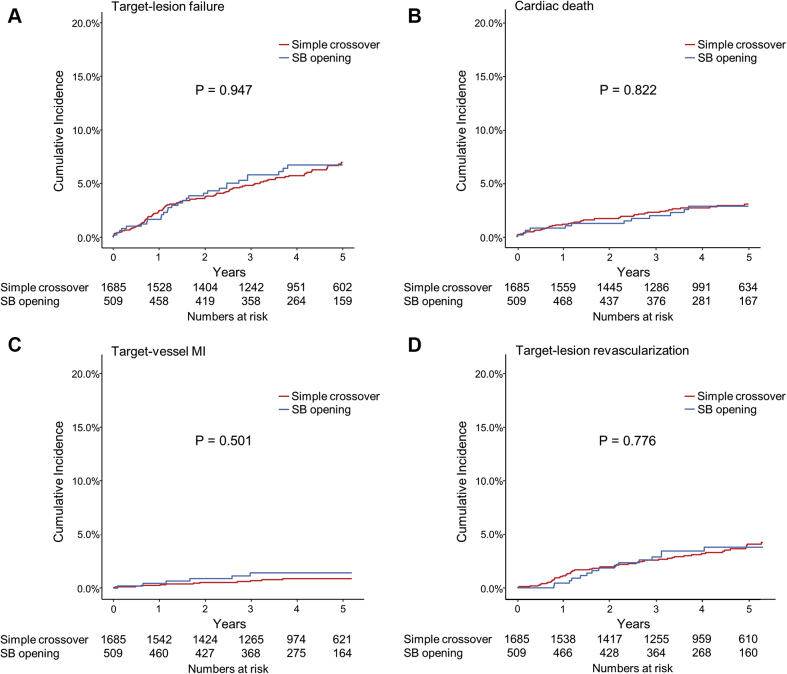
Clinical impact of the additional SB-opening procedure after simple crossover stenting
The median duration of the clinical follow-up was 53 months (interquartile range: 37 to 68 months). The 5-year observed TLF rate in the 1-stent strategy with simple crossover group did not statistically differ from that of the SB-opening group (simple crossover vs. SB opening: 7.0% vs. 6.7%; HR: 0.99; 95% CI: 0.66 to 1.48; p = 0.947), and the result did not change after an IPTW adjustment. The incidence of 5-year cardiac death (3.0% vs. 2.8%; HR: 0.93; 95% CI: 0.50 to 1.72; p = 0.822), target vessel MI (0.8% vs. 1.4%; HR: 1.38; 95% CI: 0.54 to 3.57; p = 0.501), and TLR (4.0% vs. 3.5%; HR: 0.92; 95% CI: 0.52 to 1.63; p = 0.776) did not differ between the 2 groups (Table 3, Figure 2).
Table 3.
Unadjusted and Adjusted Clinical Outcomes According to an Additional SB-Opening Procedure
| Event Rates∗ at 5 Years |
Unadjusted |
IPTW Adjusted |
||||
|---|---|---|---|---|---|---|
| Simple Crossover (n = 1,685) | SB Opening (n = 509) | HR† (95% CI) | p Value | HR† (95% CI) | p Value | |
| Primary outcome | ||||||
| Target lesion failure‡ | 95 (7.0) | 29 (6.7) | 0.99 (0.66–1.48) | 0.947 | 0.68 (0.37–1.26) | 0.218 |
| Secondary outcomes | ||||||
| Death from any cause | 77 (5.4) | 17 (3.9) | 0.75 (0.46–1.23) | 0.252 | 0.77 (0.37–1.62) | 0.494 |
| Cardiac | 43 (3.0) | 12 (2.8) | 0.93 (0.5–1.72) | 0.822 | 0.98 (0.41–2.38) | 0.970 |
| Noncardiac | 32 (2.3) | 5 (1.1) | 0.53 (0.23–1.26) | 0.150 | 0.52 (0.13–2.04) | 0.346 |
| MI | 22 (1.5) | 11 (2.4) | 1.36 (0.68–2.74) | 0.386 | 1.45 (0.51–4.08) | 0.482 |
| Target vessel MI | 12 (0.8) | 6 (1.4) | 1.38 (0.54–3.57) | 0.501 | 1.36 (0.33–5.55) | 0.670 |
| Any revascularization | 133 (9.7) | 42 (9.7) | 1.01 (0.72–1.42) | 0.955 | 0.83 (0.49–1.42) | 0.502 |
| Target lesion | 52 (4.0) | 15 (3.5) | 0.92 (0.52–1.63) | 0.776 | 0.59 (0.24–1.43) | 0.244 |
| Target vessel | 86 (6.4) | 30 (7.0) | 1.15 (0.76–1.72) | 0.514 | 0.75 (0.4–1.38) | 0.351 |
| Definite stent thrombosis | 16 (1.0) | 3 (0.7) | 0.76 (0.26–2.26) | 0.626 | 0.98 (0.21–4.59) | 0.985 |
Values are n (%) unless noted otherwise.
HR = hazard ratio; IPTW = inverse probability of treatment weighting; other abbreviation as in Figures 1 and 3.
Event rates are based on Kaplan-Meier estimates.
HRs are for the SB-opening group compared with the simple crossover group.
Target lesion failure was defined as a composite of death by cardiac causes, target vessel MI, or target lesion revascularization.
Figure 2.
Outcomes According to Additional SB Opening After Simple Crossover Stenting
The 5-year cumulative-incidence curves are shown for target-lesion failures according to an additional SB-opening procedure after the 1-stent strategy with simple crossover. Target-lesion failure was defined as a composite of death from (A) cardiac causes, target vessel MI, or target vessel revascularization; (B) cardiac death; (C) target vessel MI, (D) and target lesion revascularization. Abbreviations as in Figure 1.
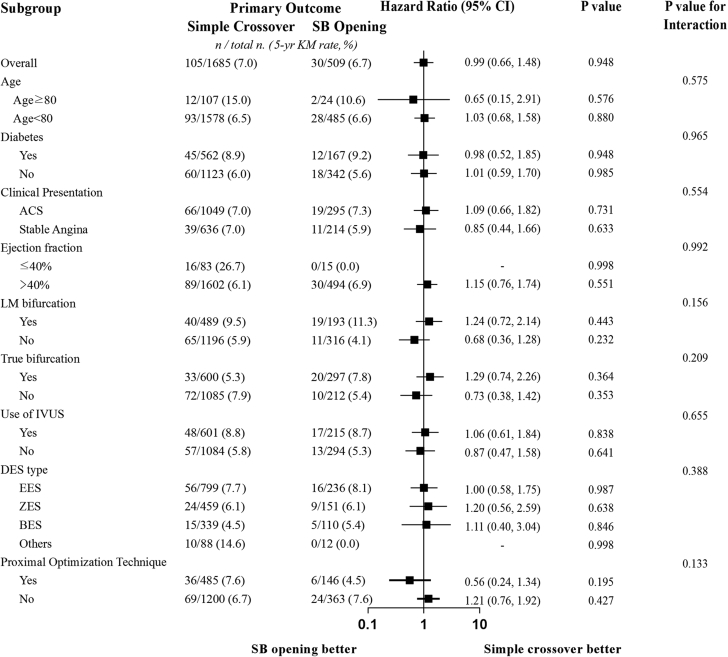
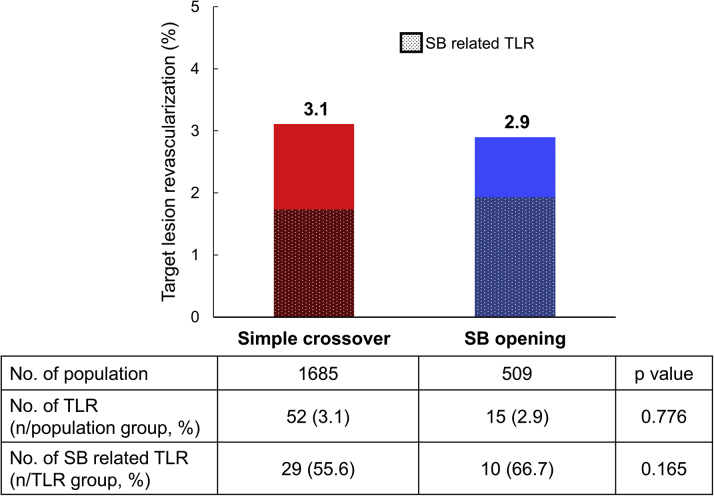
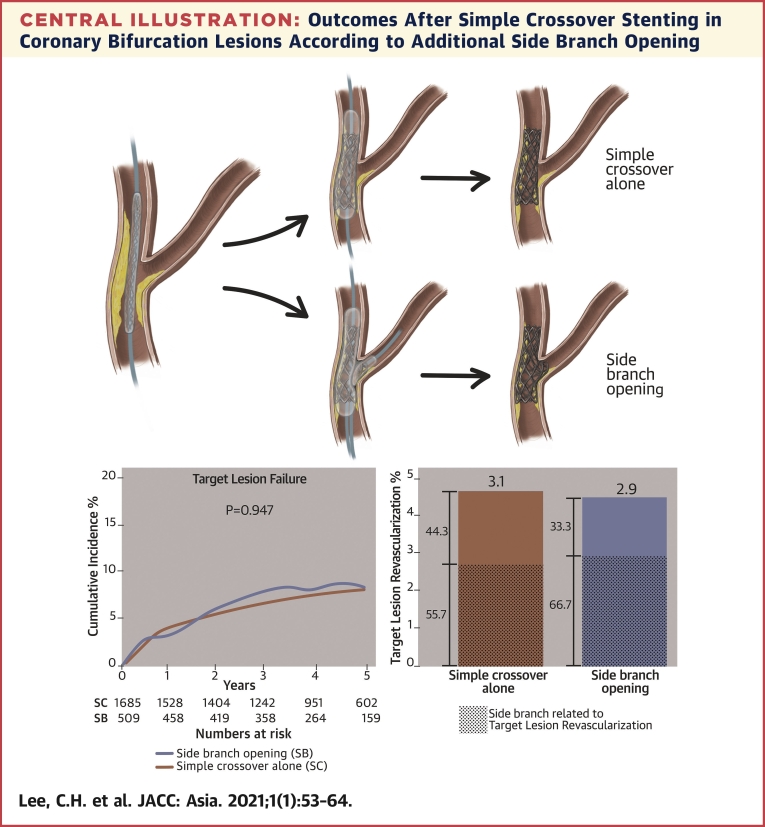
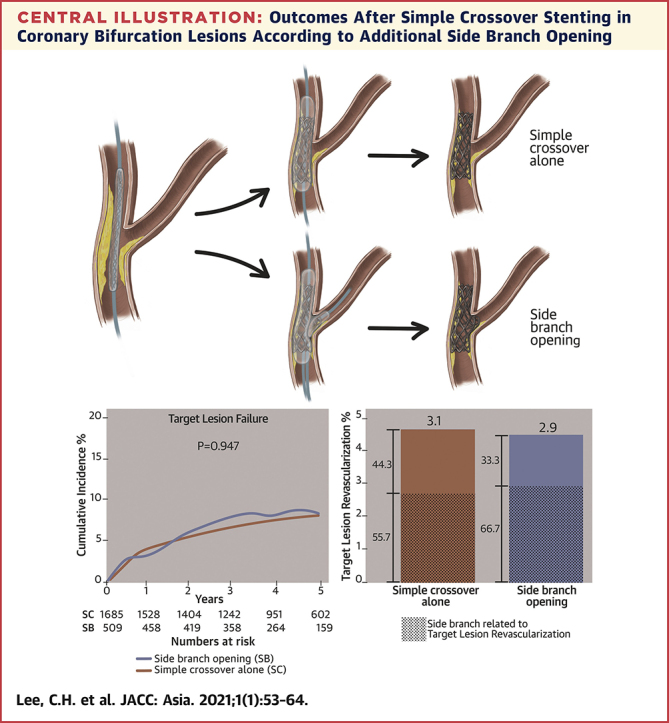
Figure 3 presents the subgroup analyses of the primary endpoint. We found little evidence of the HRs differing across each subgroup, including use of intravascular ultrasound and POT. The overall TLR rates were similar in both groups. Among them, there was also no difference in SB-related TLR events (55.7% of the simple crossover group and 66.7% in the SB-opening group; p = 0.165) (Figure 4).
Figure 3.
Subgroup Analysis
Hazard ratios are for the SB opening compared to the simple crossover. ACS = acute coronary syndrome; BES = biolimus-eluting stent; CI = confidence interval; EES = everolimus-eluting stent; IVUS = intravascular ultrasound; ZES = zotarolimus-eluting stent; other abbreviations as in Figure 1.
Figure 4.
Analysis of SB Restenosis
SB = side branch; TLR = target lesion repeat revascularization.
Clinical impact of the additional SB-opening procedure after simple crossover stenting in LM and true bifurcation lesions
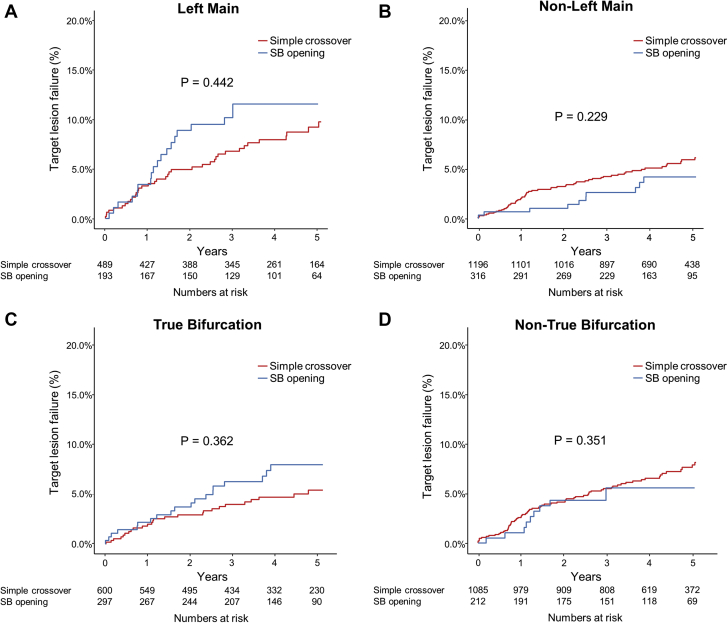
When only the LM bifurcation lesions were stratified, the 5-year rates of TLF (simple crossover vs. SB opening: 9.5% vs. 11.3%; HR: 1.24; 95% CI: 0.72 to 2.14; p = 0.442) and TLR (4.8% vs. 7.3%; HR: 1.53; 95% CI: 0.75 to 3.14; p = 0.241) were not different, and the same results were shown after an IPTW adjustment (Table 4, Figure 5). Although the incidence of a target vessel revascularization was higher in the SB-opening group, there was no statistical significance after an IPTW adjustment (7.1% vs. 11.9%; IPTW-adjusted HR: 1.30; 95% CI: 0.59 to 2.89; p = 0.519). Although a numerically high rate of stent thrombosis was observed in the LM simple crossover group, there was only 1 ostial left circumflex–related stent thrombosis, and the clinical presentation at the index procedure was acute coronary syndrome in all cases.
Table 4.
Unadjusted Clinical Outcomes According to an Additional SB-Opening Procedure for LM or True Bifurcation Lesions
| Event Rates∗ at 5-year |
Unadjusted |
IPTW Adjusted |
||||
|---|---|---|---|---|---|---|
| Simple Crossover | SB Opening | HR† (95% CI) | p Value | HR† (95% CI) | p Value | |
| LM lesion | 489 | 193 | ||||
| Target lesion failure‡ | 37 (9.5) | 19 (11.3) | 1.24 (0.72–2.14) | 0.442 | 0.92 (0.41–2.06) | 0.836 |
| Death from any cause | 33 (8.2) | 7 (4.1) | 0.49 (0.22–1.11) | 0.086 | 0.83 (0.27–2.56) | 0.741 |
| Cardiac | 20 (5.1) | 5 (3.0) | 0.60 (0.23–1.59) | 0.303 | 0.79 (0.19–3.36) | 0.755 |
| Noncardiac | 12 (3.1) | 2 (1.1) | 0.33 (0.08–1.46) | 0.145 | 0.84 (0.13–5.41) | 0.854 |
| MI | 8 (1.9) | 8 (4.7) | 2.27 (0.88–5.88) | 0.092 | 3.62 (1.05–12.44) | 0.041 |
| Target-vessel MI | 6 (1.4) | 5 (3.0) | 1.82 (0.58–5.74) | 0.306 | 2.44 (0.51–11.56) | 0.261 |
| Any revascularization | 43 (11.2) | 25 (15.0) | 1.50 (0.93–2.43) | 0.100 | 1.50 (0.73–3.09) | 0.271 |
| Target lesion | 18 (4.8) | 12 (7.3) | 1.53 (0.75–3.14) | 0.241 | 1.34 (0.47–3.81) | 0.580 |
| Target vessel | 27 (7.1) | 20 (11.9) | 1.87 (1.07–3.28) | 0.029 | 1.30 (0.59–2.89) | 0.519 |
| Definite stent thrombosis | 7 (1.6) | 0 (0) | 0.32 (0.04–2.56) | 0.282 | 1.44 (0.24–8.7) | 0.692 |
| True bifurcation | 1,196 | 316 | ||||
| Target-lesion failure† | 26 (5.3) | 19 (7.8) | 1.29 (0.74–2.26) | 0.362 | 0.93 (0.43–2.01) | 0.854 |
| Death from any cause | 29 (5.8) | 11 (4.4) | 0.74 (0.38–1.43) | 0.372 | 0.68 (0.27–1.76) | 0.432 |
| Cardiac | 16 (3.1) | 9 (3.7) | 1.07 (0.5–2.29) | 0.856 | 1.10 (0.39–3.11) | 0.864 |
| Noncardiac | 13 (2.8) | 2 (0.8) | 0.29 (0.07–1.28) | 0.103 | 0.13 (0.03–0.57) | 0.007 |
| MI | 6 (1.3) | 4 (1.5) | 1.06 (0.32–3.53) | 0.921 | 0.46 (0.14–1.56) | 0.214 |
| Target vessel MI | 3 (0.5) | 3 (1.2) | 1.56 (0.35–6.99) | 0.559 | 0.64 (0.14–2.88) | 0.561 |
| Any revascularization | 41 (8.2) | 23 (9.4) | 0.98 (0.6–1.6) | 0.928 | 0.63 (0.3–1.3) | 0.210 |
| Target lesion | 11 (2.4) | 8 (3.4) | 1.24 (0.52–2.97) | 0.622 | 0.55 (0.22–1.33) | 0.181 |
| Target vessel | 23 (4.8) | 15 (6.3) | 1.17 (0.62–2.19) | 0.632 | 0.58 (0.28–1.19) | 0.140 |
| Definite stent thrombosis | 4 (0.7) | 2 (0.8) | 1.28 (0.3–5.35) | 0.739 | 2.09 (0.37–11.85) | 0.405 |
Values are n or n (%), unless noted otherwise.
Event rates are based on Kaplan-Meier estimates.
Hazard ratios are for the SB-opening group compared to the simple crossover group.
Target lesion failure was defined as a composite of death by cardiac causes, target vessel MI, or target lesion revascularization.
Figure 5.
Outcomes According to Additional SB Opening, Stratified by LM and True Bifurcation Lesions
In each figure, the 5-year of cumulative-incidence curves are shown for the target lesion failure according to an additional SB-opening procedure after the 1-stent strategy with simple crossover. Target lesion failure was defined as a composite of death from cardiac causes, target vessel myocardial infractions, or target-vessel revascularization with (A) LM bifurcation lesions, (B) non-LM bifurcation lesions, (C) true bifurcation lesions, and (D) non–true bifurcation lesions. Abbreviations as in Figure 1.
When only the true bifurcation was stratified, the SB-opening group did not exhibit an improvement in the clinical outcome compared to the simple crossover group in the 5-year TLF (simple crossover vs. SB opening: 5.3% vs. 7.8%, HR: 1.29; 95% CI: 0.74 to 2.26; p = 0.362).
Discussion
The major findings from the present study, which investigated the long-term outcomes of a 1-stent strategy with simple crossover alone versus with an additional SB-opening procedure for coronary bifurcation lesions, are as follows:
-
•
There were various different baseline angiographic characteristics between the 2 groups, and the SB-opening group showed better post-procedural angiographic results in the SB.
-
•
However, an additional procedure for SB opening did not exhibit improvement in the long-term clinical outcomes compared to simple crossover alone, and the results did not change after an IPTW adjustment.
-
•
Even in the various subgroup analyses, including LM and true bifurcation lesion subsets, the outcomes were not different between the 2 groups.
-
•
There were similar 5-year overall and SB-related TLR rates in both groups.
In the treatment of bifurcation lesions, a provisional strategy is generally recommended, because the 1-stent strategy had better or similar long-term clinical outcomes than the 2-stent strategy in several randomized and registry trials (1,2,14,15). Apart from the 1-stent strategy for bifurcation lesions, there is still controversy over a SB-opening treatment after simple MV stenting because of conflicting results. In the Nordic-Baltic Bifurcation Study III, the CROSS (Choice of Optimal Strategy for Bifurcation Lesions With Normal Side Branch) study, and the COBIS I study, SB opening by FKI after simple MV stenting did not show a better clinical outcome compared to simple crossover alone. Furthermore, the simple crossover group had a reduced use of contrast media and shorter procedure and fluoroscopy times (4,5,16). On the other hand, in the COBIS II study, which included LM and non-LM bifurcation lesions, SB opening with FKI was associated with a favorable long-term clinical outcome, mainly driven by the reduction in TLR in the MV (adjusted HR: 0.51; 95% CI: 0.28 to 0.93; p = 0.03) as a result of an increase in the MLD of the MV (3). Because of this limited clinical evidence about the role of SB opening after simple crossover stenting, a routine SB opening is mandatorily recommended only with the 2-stent strategy (17), and there is controversy over the 1-stent strategy.
The current study was a large, multicenter, real-world registry of patients with bifurcation lesions including LM bifurcation lesions. In this registry, physicians choose SB opening for the patients with large SB territory or complex anatomy such as LM or true bifurcation lesions and preferred to complete the procedure with simple crossover alone in the patients who had low ejection fraction or presented with acute coronary syndrome. Although the SB opening could improve the immediate angiographic results in the SB, the 5-year clinical outcomes of SB opening after simple crossover stenting did not differ compared to the simple crossover group after an IPTW adjustment, even in various subgroup analyses, including the LM and true bifurcation lesions. An additional important finding of our current study was that there were similar overall TLR rates in both groups and no difference in SB-related TLR events by analyzing the angiographic locations of the patients who had TLR (Central Illustration). SB-related TLR events were consistently similar in previous studies such as CROSS (routine SB opening with FKI vs. leave alone: 1.3% vs. 1.3%; p = 0.97), COBIS I (FKI vs. non-FKI: 2.1% vs. 0.0%), and COBIS II studies (FKI vs. non-FKI: 2.1% vs. 2.2%; p = 0.62) (3,5,16). Therefore, the routine additional SB-opening procedure may not prevent an SB-related TLR event after the 1-stent strategy in coronary bifurcation lesions. However, the current study included patients who had relatively simple bifurcation lesions, such as mild to moderate stenosis and short lesion length of the SB, and excluded patients who had been treated with a 2-stent strategy because of highly complex bifurcation lesions, such as tight stenosis with longer lesion length in a large SB. This concept should be cautiously applied and not used for all bifurcation lesions.
Central Illustration.
Outcomes After Simple Crossover Stenting in Coronary Bifurcation Lesions According to Additional Side Branch Opening
An additional side branch–opening procedure after simple main vessel stenting for coronary bifurcation lesions did not exhibit an improvement in the 5-year observed target lesion failure rate compared to simple crossover alone. Furthermore, similar overall and SB-related target lesion revascularization rates were seen in both groups. Therefore, the long-term clinical outcomes after the 1-stent strategy with simple crossover for coronary bifurcation lesions was acceptable.
The issue of the SB-opening procedure was well demonstrated by an optical coherence tomography study. An inappropriate rewiring location over the ostial SB strut guided by only angiography may lead to a worse result after the SB opening with FKI (18,19). Computational fluid dynamics analysis also demonstrated that the SB-opening procedure increased the very low wall shear stress area in the MV, suggesting the possibility of neointimal hyperplasia progression (20). Similarly, a recent meta-analysis showed that SB opening with an FKI strategy increased the risk of MV restenosis (21).
Although the SB-opening procedure with FKI can provide an optimal expansion of the MV, POT has replaced this effect, which can not only make an optimal stent expansion but also restore the elliptical deformation of the stent struts and reduce the malapposition of the stent proximal segment (22). In addition, the incidence of POT was similar in both groups of the current study. However, this concept should be confirmed by an independent study focused on the POT itself.
Furthermore, previous fractional flow reserve studies in a jailed SB after simple MV stenting well demonstrated the discrepancy between angiographic jailing of the SB and the functional significance. An additional SB opening procedure could not achieve a better outcome compared to only medical therapy in a jailed SB deferred by fractional flow reserve guidance (7,10). Even after LM simple crossover stenting, similar results were observed in the jailed left circumflex lesions (8,9). In that study, the angiographic acute luminal gain of the MV, not that of the SB after stenting, and the functional significance of a jailed SB were reported as major determinants of the long-term clinical outcome after simple crossover stenting (8). Therefore, the maximal optimization of the MV might be more important than the SB-opening procedure itself in a bifurcation PCI with simple crossover stenting. An SB opening with additional complex procedures, which need more resources and have a risk of procedural complications, might be waived by a provisional strategy with a functional evaluation and be performed in ischemic and clinically relevant SBs.
Study limitations
First, this was a nonrandomized, retrospective, observational study, which may have affected the results because of confounding factors. Although we performed multiple sensitivity analyses, including an IPTW adjustment, to reduce the potential confounders, we could not correct for the unmeasured variables. Second, the choice of treatment strategy, use of intravascular imaging, vascular access, type of stent, and concomitant medications might have reflected individual physicians’ preferences. For this reason, information on the rate and clinical outcomes of bail-out stenting on the SB after single stenting were limited. Third, because of the low rate of POT, the procedural optimization of the SB-opening group may not have been complete. However, that was a similar ratio in the simple crossover group, which was a result of comparing similar conditions. However, our data showed the long-term clinical outcome for the previously underreported effects of the SB-opening procedure after the 1-stent strategy with simple crossover and could play a hypothesis-generating role for future research and reduce unnecessary procedures with bifurcation lesions of coronary artery disease.
Conclusions
The long-term clinical outcomes of the simple crossover 1-stent strategy without an additional SB-opening procedure in patients with coronary bifurcation lesions was acceptable, even for LM or true bifurcation lesions. Therefore, an additional complex procedure for SB opening may not be mandatory for simple crossover stenting bifurcation lesions.
Perspectives.
COMPENTENCY IN MEDICAL KNOWLEDGE: This study investigated the long-term outcomes of a 1-stent strategy with simple crossover alone versus with additional an SB-opening procedure for coronary bifurcation lesions. The 5-year observed TLF rate was similar between the simple crossover–alone and SB-opening groups, and there were similar 5-year overall and SB-related TLR rates in both groups. SB opening with additional complex procedures, which need more resources and have a risk of procedural complications, might be waived by a provisional strategy and be performed only in ischemic and clinically relevant SB.
TRANSLATIONAL OUTLOOK: Further large randomized studies are needed to clarify the impact of an additional SB-opening procedure in more complex bifurcation lesions.
Funding Support and Author Disclosures
This work was supported by the Korean Bifurcation Club and Korean Society of Interventional Cardiology. The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors thank Jin-Seob Kim, MD, MPH, for his statistical support.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables and a figure, please see the online version of this paper.
Contributor Information
Chang-Wook Nam, Email: ncwcv@dsmc.or.kr.
Seung-Ho Hur, Email: shur@dsmc.or.kr.
Appendix
References
- 1.Steigen T.K., Maeng M., Wiseth R., et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006;114:1955–1961. doi: 10.1161/CIRCULATIONAHA.106.664920. [DOI] [PubMed] [Google Scholar]
- 2.Hildick-Smith D., de Belder A.J., Cooter N., et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010;121:1235–1243. doi: 10.1161/CIRCULATIONAHA.109.888297. [DOI] [PubMed] [Google Scholar]
- 3.Yu C.W., Yang J.H., Song Y.B., et al. Long-term clinical outcomes of final kissing ballooning in coronary bifurcation lesions treated with the 1-stent technique: results from the COBIS II Registry (Korean Coronary Bifurcation Stenting Registry) J Am Coll Cardiol Intv. 2015;8:1297–1307. doi: 10.1016/j.jcin.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Niemelä M., Kervinen K., Erglis A., et al. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011;123:79–86. doi: 10.1161/CIRCULATIONAHA.110.966879. [DOI] [PubMed] [Google Scholar]
- 5.Kim Y.H., Lee J.H., Roh J.H., et al. Randomized comparisons between different stenting approaches for bifurcation coronary lesions with or without side branch stenosis. J Am Coll Cardiol Intv. 2015;8:550–560. doi: 10.1016/j.jcin.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Song Y.B., Park T.K., Hahn J.Y., et al. Optimal strategy for provisional side branch intervention in coronary bifurcation lesions: 3-year outcomes of the SMART-STRATEGY randomized trial. J Am Coll Cardiol Intv. 2016;9:517–526. doi: 10.1016/j.jcin.2015.11.037. [DOI] [PubMed] [Google Scholar]
- 7.Koo B.K., Kang H.J., Youn T.J., et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46:633–637. doi: 10.1016/j.jacc.2005.04.054. [DOI] [PubMed] [Google Scholar]
- 8.Lee C.H., Choi S.W., Hwang J., et al. 5-year outcomes according to FFR of left circumflex coronary artery after left main crossover stenting. J Am Coll Cardiol Intv. 2019;12:847–855. doi: 10.1016/j.jcin.2019.02.037. [DOI] [PubMed] [Google Scholar]
- 9.Nam C.W., Hur S.H., Koo B.K., et al. Fractional flow reserve versus angiography in left circumflex ostial intervention after left main crossover stenting. Korean Circ J. 2011;41:304–307. doi: 10.4070/kcj.2011.41.6.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koo B.K., Park K.W., Kang H.J., et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008;29:726–732. doi: 10.1093/eurheartj/ehn045. [DOI] [PubMed] [Google Scholar]
- 11.Medina A., Suárez de Lezo J., Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol. 2006;59:183. [PubMed] [Google Scholar]
- 12.Laskey W.K., Yancy C.W., Maisel W.H. Thrombosis in coronary drug-eluting stents: report from the meeting of the Circulatory System Medical Devices Advisory Panel of the Food and Drug Administration Center for Devices and Radiologic Health, December 7-8, 2006. Circulation. 2007;115:2352–2357. doi: 10.1161/CIRCULATIONAHA.107.688416. [DOI] [PubMed] [Google Scholar]
- 13.Robins J.M., Hernán M.A., Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Behan M.W., Holm N.R., de Belder A.J., et al. Coronary bifurcation lesions treated with simple or complex stenting: 5-year survival from patient-level pooled analysis of the Nordic Bifurcation Study and the British Bifurcation Coronary Study. Eur Heart J. 2016;37:1923–1928. doi: 10.1093/eurheartj/ehw170. [DOI] [PubMed] [Google Scholar]
- 15.Gwon H.C., Choi S.H., Song Y.B., et al. Long-term clinical results and predictors of adverse outcomes after drug-eluting stent implantation for bifurcation lesions in a real-world practice: the COBIS (Coronary Bifurcation Stenting) registry. Circ J. 2010;74:2322–2328. doi: 10.1253/circj.cj-10-0352. [DOI] [PubMed] [Google Scholar]
- 16.Gwon H.C., Hahn J.Y., Koo B.K., et al. Final kissing ballooning and long-term clinical outcomes in coronary bifurcation lesions treated with 1-stent technique: results from the COBIS registry. Heart. 2012;98:225–231. doi: 10.1136/heartjnl-2011-300322. [DOI] [PubMed] [Google Scholar]
- 17.Rab T., Sheiban I., Louvard Y., Sawaya F.J., Zhang J.J., Chen S.L. Current interventions for the left main bifurcation. J Am Coll Cardiol Intv. 2017;10:849–865. doi: 10.1016/j.jcin.2017.02.037. [DOI] [PubMed] [Google Scholar]
- 18.Nagoshi R., Okamura T., Murasato Y., et al. Feasibility and usefulness of three-dimensional optical coherence tomography guidance for optimal side branch treatment in coronary bifurcation stenting. Int J Cardiol. 2018;250:270–274. doi: 10.1016/j.ijcard.2017.09.197. [DOI] [PubMed] [Google Scholar]
- 19.Okamura T., Nagoshi R., Fujimura T., et al. Impact of guidewire recrossing point into stent jailed side branch for optimal kissing balloon dilatation: core lab 3D optical coherence tomography analysis. EuroIntervention. 2018;13:e1785–e1793. doi: 10.4244/EIJ-D-17-00591. [DOI] [PubMed] [Google Scholar]
- 20.Williams A.R., Koo B.K., Gundert T.J., Fitzgerald P.J., LaDisa J.F., Jr. Local hemodynamic changes caused by main branch stent implantation and subsequent virtual side branch balloon angioplasty in a representative coronary bifurcation. J Appl Physiol (1985) 2010;109:532–540. doi: 10.1152/japplphysiol.00086.2010. [DOI] [PubMed] [Google Scholar]
- 21.Zhong M., Tang B., Zhao Q., Cheng J., Jin Q., Fu S. Should kissing balloon inflation after main vessel stenting be routine in the one-stent approach? A systematic review and meta-analysis of randomized trials. PLoS One. 2018;13 doi: 10.1371/journal.pone.0197580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dérimay F., Finet G., Souteyrand G., et al. Benefit of a new provisional stenting strategy, the re-proximal optimisation technique: the rePOT clinical study. EuroIntervention. 2018;14:e325–e332. doi: 10.4244/EIJ-D-17-00941. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.