Abstract
Background
The coronavirus disease-2019 (COVID-19) pandemic significantly affected management of cardiovascular disease around the world. The effect of the pandemic on volume of cardiovascular diagnostic procedures is not known.
Objectives
This study sought to evaluate the effects of the early phase of the COVID-19 pandemic on cardiovascular diagnostic procedures and safety practices in Asia.
Methods
The International Atomic Energy Agency conducted a worldwide survey to assess changes in cardiovascular procedure volume and safety practices caused by COVID-19. Testing volumes were reported for March 2020 and April 2020 and were compared to those from March 2019. Data from 180 centers across 33 Asian countries were grouped into 4 subregions for comparison.
Results
Procedure volumes decreased by 47% from March 2019 to March 2020, showing recovery from March 2020 to April 2020 in Eastern Asia, particularly in China. The majority of centers cancelled outpatient activities and increased time per study. Practice changes included implementing physical distancing and restricting visitors. Although COVID testing was not commonly performed, it was conducted in one-third of facilities in Eastern Asia. The most severe reductions in procedure volumes were observed in lower-income countries, where volumes decreased 81% from March 2019 to April 2020.
Conclusions
The COVID-19 pandemic in Asia caused significant reductions in cardiovascular diagnostic procedures, particularly in low-income countries. Further studies on effects of COVID-19 on cardiovascular outcomes and changes in care delivery are warranted.
Key Words: cardiac testing, cardiovascular disease, coronavirus, COVID-19, global health
Abbreviations and Acronyms: CMR, cardiac magnetic resonance; COVID-19, coronavirus disease-19; CTA, computed tomographic angiography; ICA, invasive coronary angiography; PET, positron emission tomography; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2; TTE, transthoracic echocardiography
Central Illustration
The coronavirus disease-2019 (COVID-19), caused by the novel coronavirus severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), was first identified in China in December 2019; it initially affected Eastern Asia and quickly spread to the rest of Asia and across the globe. The World Health Organization declared a COVID-19 pandemic on March 11, 2020 (1). COVID-19 is a contagious disease with highly variable clinical presentations and manifestations (2), and figures of COVID-19 cases, deaths, and mortality rates vary significantly from country to country (3). The pandemic has necessitated extraordinary actions by governments and the global medical community to maintain medical supplies and prevent rapid transmission. These responses have had an untoward impact on economies and fundamentally changed the practice of medicine and delivery of health care, including management of cardiovascular disease (CVD). CVD remains the leading cause of morbidity and mortality worldwide in all countries regardless of socioeconomic status (4,5). In recent decades, health care professionals have attempted to optimize the diagnosis and treatment of CVD (5,6), significantly reducing mortality and incidence of major cardiovascular events (7, 8, 9, 10). The COVID-19 pandemic holds potential to halt that progress by delaying the application of advanced diagnostic procedures that guide detection and treatment of CVD.
SARS-CoV-2 can infect people of all ages. However, the virus poses a particular risk for people over the age of 60 years and those with pre-existing medical conditions. Development of severe disease is known to be higher in patients with CVD (11). Patients with COVID-19 and CVD have higher mortality than those without comorbidity (12). Moreover, efforts to prevent the spread of COVID-19 have redirected critical health care resources and changed conventional practice patterns for routine CVD care (13, 14, 15, 16). With a global estimated 17.9 million annual deaths caused by CVD (17,18), the negative impact of the pandemic on patients treated for CVD cannot be overstated. Indeed, a recent study from Italy reported that inpatient cardiac deaths have increased during the COVID-19 pandemic (19).
A key objective of the International Atomic Energy Agency (IAEA) Division of Human Health is to support Member States’ fight against cancer, CVDs, malnutrition, and other diseases using nuclear and nuclear-related techniques (20,21). Various diagnostic modalities employed by cardiologists rely upon the use of ionizing radiation. In efforts led by the IAEA Division of Human Health, the INCAPS (IAEA Non-invasive Cardiology Protocols Study) COVID Investigators Group (Supplemental Appendix) conducted a large-scale global survey to assess changes in noninvasive and invasive diagnostic procedure volumes and clinical safety practices caused by the COVID-19 pandemic, referred to as the INCAPS COVID study (22).
COVID-19 began to spread from Asia and affected other countries at different times. Mortality rates, infection rates, infection control methods, and response policies vary widely between countries and regions (23,24). Comparisons of the impact of COVID-19 on cardiovascular practices and health resource supplies across the globe will be informative for identifying the requirements for recovery from the pandemic and the development of proper strategies for future outbreaks of emerging infectious diseases (25,26). The aim of this analysis was to identify differences in the impact of the COVID-19 pandemic on cardiovascular diagnostic procedure volumes and practices between Asia and the rest of the world, and among Asian subregions.
Methods
Study design
The study was conducted under the IAEA INCAPS Group, which has conducted numerous studies on practice variations in cardiovascular diagnostic procedures (27, 28, 29, 30, 31, 32, 33, 34). The study design has been described in detail elsewhere (22). A web-based survey questionnaire was performed to assess the impact of the COVID-19 pandemic on cardiovascular diagnostic care delivery. The questionnaire included the following subsections: 1) descriptors of participating health care facilities and health care professionals; 2) the use of personal protective equipment and strategic plans for reopening; and 3) changes in procedural volumes for a range of cardiovascular diagnostic procedures. The latter included transthoracic echocardiography (TTE) and transesophageal echocardiography, nonstress cardiac magnetic resonance (CMR), stress testing (stress electrocardiography, echocardiography, single-photon emission computed tomography, positron emission tomography [PET], and CMR), PET infection studies, coronary artery calcium scanning, coronary computed tomographic angiography (CTA), and invasive coronary angiography (ICA). Data were obtained from each participating site for March 2020 and April 2020 and were compared to March 2019, which served as a baseline. Data were aggregated by country and region. In this subanalysis, the Asian participating countries of the INCAPS COVID study were divided into 4 subregions (Eastern, Southeastern, Southern, and Central and Western) according to the United Nations’ geoscheme (35), which is specified in the Supplemental Appendix. Countries were classified into 4 categories by income status (low, lower-middle, upper-middle, and high) in accordance with the World Bank classification (36).
Data collection
Candidate facilities were invited to participate using various methods, including e-mails from the IAEA INCAPS COVID executive committee and national coordinators (37), e-mails from IAEA to cardiology and imaging societies (listed in the Supplemental Appendix), communications from professional societies to their members, and social media platforms (Twitter, LinkedIn, and Facebook). An electronic data entry system was devised to collect data on the impact of the COVID-19 pandemic on cardiovascular diagnostic procedures. The IAEA employs a secure software platform, the International Research Integration System (38), for questionnaire data collection. In INCAPS COVID, no patient-specific personal information or confidential data were collected, and all study sites participated voluntarily; therefore, review by an ethics committee was not required. The present study complied with the Declaration of Helsinki.
Throughout the enrollment period (May 11, 2020, to May 30, 2020), the Data Coordination Committee reviewed entries on a daily basis and reached out to participating health care personnel with questions regarding missing data or duplicate entries from the same institution. Only 1 entry from a given center was included in the final data set, and entries were excluded if data were missing or incomplete. Final database cleaning was completed on July 1, 2020.
Statistical analysis
Nonparametric statistical analysis using the Kruskal-Wallis test with asymptotic 2-sided P values was conducted on differences in test volumes between 2019 and 2020 and on continuous variables between Asia and the rest of the world, and among Asian subregions. The chi-square test was used to compare center characteristics between world regions. Statistical analyses were performed using Stata version 16 (Stata Corporation, LLC) and Microsoft Excel (2016). Maps were created using rnaturalearth and tmap packages in R (R Foundation for Statistical Computing) (39,40).
Results
Center characteristics
Data from 180 centers in 33 Asian countries were obtained. According to the United Nations’ geoscheme, Asian countries were separated into 4 subregions: Eastern Asia (4 countries, 81 facilities), Southeastern Asia (10 countries, 36 facilities), Southern Asia (7 countries, 38 facilities), and Western and Central Asia (12 countries, 25 facilities). A list of the countries in each subregion is shown in the Supplemental Appendix, and center characteristics are summarized in Table 1. A total of 395,598 cardiac diagnostic procedures were performed at participating centers in Asia during the 3 months (March 2019, March 2020, and April 2020) considered.
Table 1.
Characteristics of Participating Centers and Procedure Numbers
| Asian Region |
Worldwide |
|||||||
|---|---|---|---|---|---|---|---|---|
| Eastern | South-Eastern | Southern | Western and Central | P Value | Asia | RoW | P Value | |
| Number of centers | 81 | 36 | 38 | 25 | 180 | 729 | ||
| Number of countries | 4 | 10 | 7 | 12 | 33 | 75 | ||
| Number of procedures | ||||||||
| March 2019 | 130,909 | 19,250 | 29,488 | 12,556 | 192,203 | 486,435 | ||
| March 2020 | 69,034 | 13,140 | 12,418 | 6,500 | 101,092 | 293,533 | ||
| April 2020 | 88,170 | 7,567 | 3,013 | 3,553 | 102,303 | 142,133 | ||
| Procedures per center | ||||||||
| March 2019 | 632 (219-1,233) | 120 (19-795) | 190 (73-810) | 252 (115-507) | <0.01 | 367 (93-1,067) | 248 (78-812) | 0.09 |
| March 2020 | 472 (150-935) | 41 (11-418) | 122 (52-390) | 93 (26-233) | <0.01 | 188 (52-764) | 126 (41-451) | 0.03 |
| April 2020 | 578 (227-1,055) | 29 (1-81) | 38 (0-173) | 29 (2-118) | <0.01 | 139 (10-571) | 57 (13-232) | <0.01 |
| Hospital beds | 914 (613-2,500) | 673 (250-1,000) | 350 (200-924) | 600 (400-950) | <0.01 | 751 (350-1,368) | 460 (200-800) | <0.01 |
| Inpatient center | 80 (99) | 33 (92) | 34 (89) | 25 (100) | 0.04 | 172 (96) | 567 (78) | <0.01 |
| Teaching institution | 62 (77) | 26 (72) | 20 (53) | 21 (84) | 0.03 | 129 (72) | 468 (64) | 0.04 |
| Economic level by center | ||||||||
| Low | — | — | 2 (5) | — | <0.01 | 2 (1) | 2 (0.3) | <0.01 |
| Lower-middle | 1 (1) | 28 (78) | 28 (74) | 1 (4) | 58 (32) | 28 (4) | ||
| Upper-middle | 30 (37) | 3 (8) | 8 (21) | 5 (20) | 46 (26) | 236 (32) | ||
| Upper | 50 (62) | 5 (14) | — | 19 (76) | 74 (41) | 463 (64) | ||
Values are n, median (interquartile range), or n (%). Procedure counts are for centers performing testing in March 2019.
RoW = rest of world.
Procedure reductions
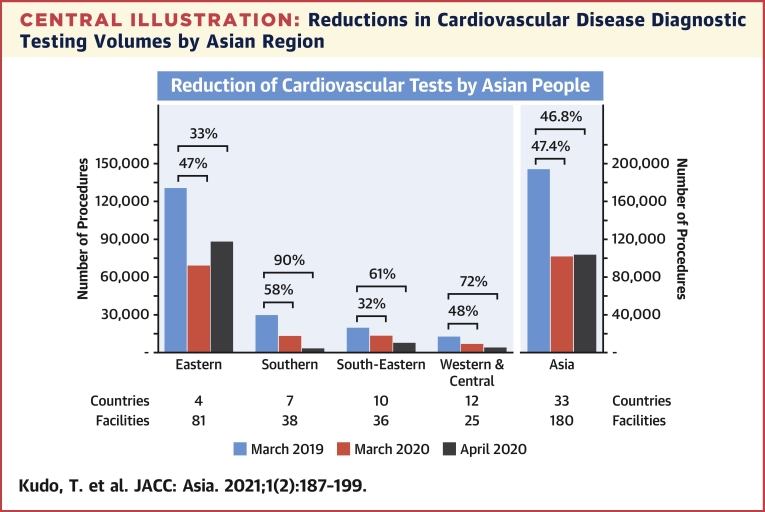
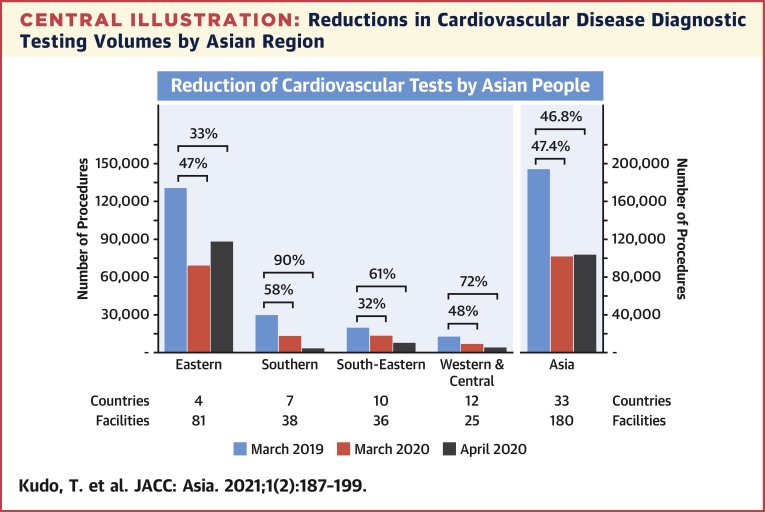
In Asia, cardiac diagnostic procedure volumes decreased by 47% in March 2020 compared with March 2019 (Table 1, Central Illustration). However, recovery by nearly 1% was noted between March 2020 and April 2020. This differed from the rest of the world, which showed a continuous decline (52%) between March 2020 and April 2020. At the subregion level, recovery was driven entirely by procedures performed in Eastern Asia, with the other 3 subregions (South-Eastern, Southern, and Western and Central) showing no recovery (Central Illustration). Figure 1 shows maps of the total procedure reduction over the study period, with clear regional differences (top panel: March 2019 to April 2020, middle panel: March 2019 to March 2020, bottom panel: March 2020 to April 2020). In the Eastern Asian subregion, more than 95% of procedure volume data obtained came from China, Korea, and Japan; the trends among these 3 countries differed widely (Supplemental Table 1). In China, the number of examinations had already decreased in March 2020 (60% reduction), whereas recovery was observed in April 2020 from March 2020 (58% increase). In Korea, the number of examinations decreased in March 2020 (10% reduction), with no marked changes in the number of examinations performed in April 2020 (1% reduction). In Japan, the number of examinations conducted only slightly decreased in March 2020 (2% reduction), whereas a substantial decrease was observed in April 2020 (18% reduction). Therefore, the recovery observed in April 2020 was mainly driven by the recovery in China. This difference in procedure reduction was also visible on the map shown in Figure 1, with clear regional differences. In terms of the number of procedures analyzed per center, there was no recovery between March 2020 and April 2020, but the decline slowed. In April 2020, procedure numbers per center in Asia were significantly larger than those in the rest of the world (Table 1).
Central Illustration.
Reductions in Cardiovascular Disease Diagnostic Testing Volumes by Asian Region
The numbers of included countries and facilities in each subregion are shown in the bottom table.
Figure 1.
Asian Map Showing Reductions in Total Cardiovascular Procedural Volumes
(Top) Change from March 2019 to April 2020, indicating total change during this study period. (Middle) Change from March 2019 to March 2020, indicating the impact of the very early phase of the pandemic. (Bottom) Change from March 2020 to April 2020, indicating short-term trends during the very early phase of pandemic. Countries or territories of a country in gray did not have data available. Darker blue color indicates severe reduction. Warmer color indicates recovery.
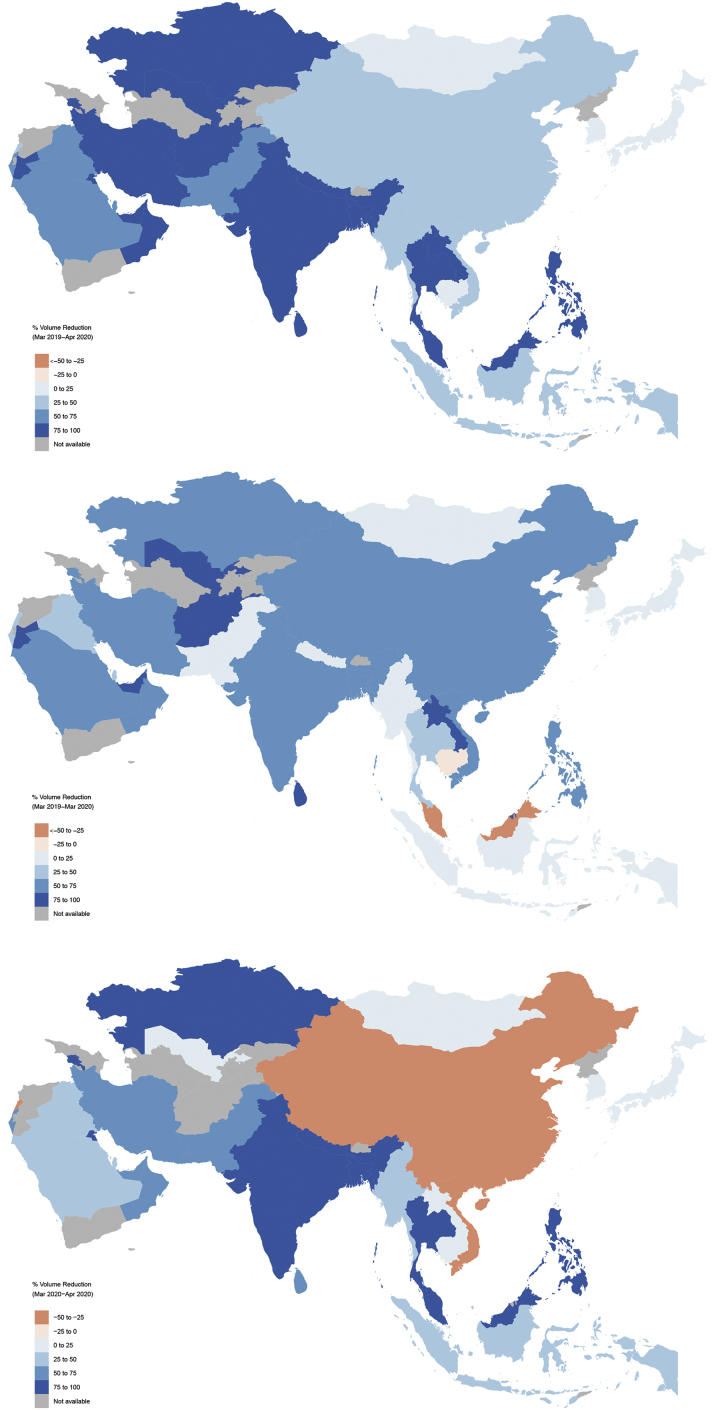
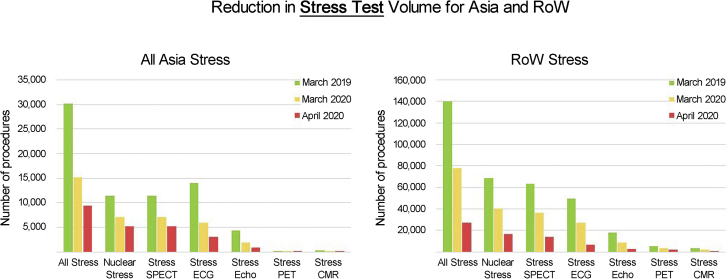
Decreases in procedure volume also varied between the various imaging modalities. As shown in Figure 2, the volume of all diagnostic modalities decreased between March 2019 and March 2020 in Asia. Total procedure volume across all imaging modalities fell by 47% from March 2019 to March 2020; the median number of procedures performed per participating center fell from 367 to 188 during this time period (Table 1). However, by April 2020, coronary CTA volume had recovered, whereas TTE and ICA volumes remained reduced. No such recovery was observed in the rest of the world, which saw further reductions across all modalities from March 2020 to April 2020. In Asia, stress testing volume across all modalities saw a year-over-year decline from March 2019 to March 2020 and continued to decrease into April 2020 (Figure 3).
Figure 2.
Reductions in Each Cardiac Procedure Modality
The number of each procedure type in Asia (left) and in the rest of the world (ROW) (right) at March 2019, March 2020, and April 2020. All types of stress test modalities (exercise electrocardiography, stress echocardiography, nuclear stress imaging [single-photon emission computed tomography and positron emission tomography], and stress cardiac magnetic resonance [CMR]) are grouped together. Note the recovery of coronary computed tomography angiography (CTA) was observed in Asia but not in the rest of the world. CAC = coronary artery calcium; TEE = transesophageal echocardiography; TTE = transthoracic echocardiography.
Figure 3.
Reductions in Stress Test Volumes
The number of each stress procedure in Asia (left) and in the ROW (right) at March 2019, March 2020, and April 2020. ECG = electrocardiogram; Echo = echocardiography; PET = positron emission tomography; SPECT = single-photon emission computed tomography; other abbreviations as in Figure 2.
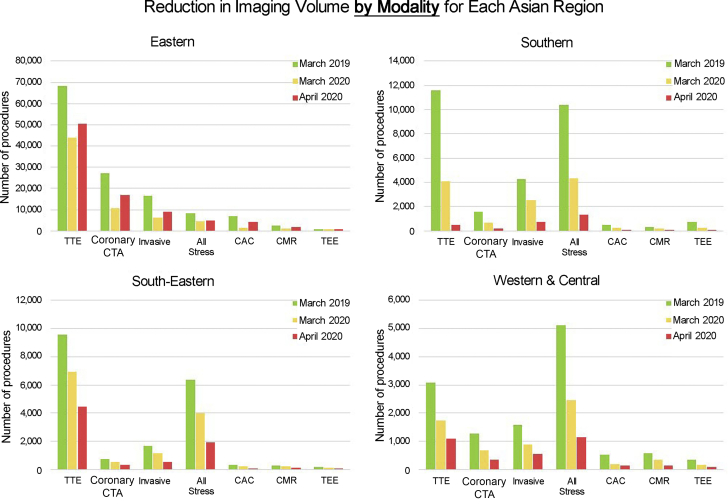
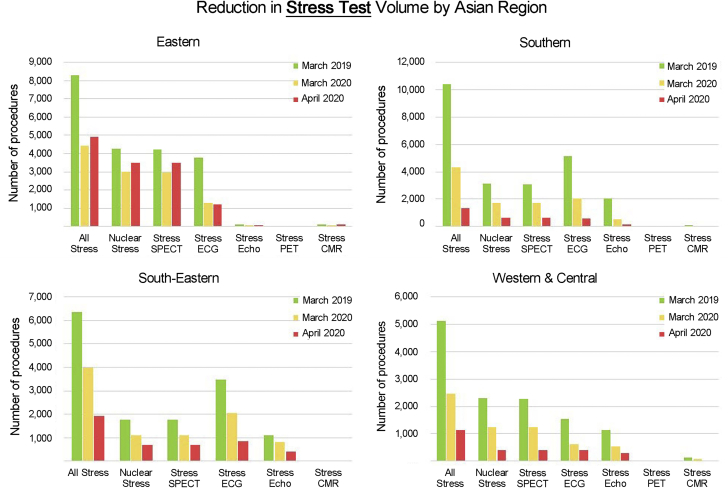
When divided into 4 subregions (Figures 4 and 5), recovery of several procedures (TTE, coronary CTA, ICA, nuclear stress test) was observed in Eastern Asia: 14%, 59%, 45%, and 17% increase from March 2020 to April 2020 in volume of TTE, coronary CTA, ICA, and nuclear stress test volumes, respectively. In contrast, all other subregions saw continued decline in volume of these procedures over the same period. Stress PET and stress CMR were performed in very low numbers in all 4 subregions compared with before the pandemic: only 106 stress PET and 316 stress CMR were reported in all of Asia in March 2019, which declined by 57% and 31%, respectively, by March 2020. Interestingly, compared with the other 3 subregions in Asia, the volume of stress echocardiography was very low both before and during the pandemic in Eastern Asia (Figure 5). In March 2019 as well as March 2020, just 3% of all reported stress TTE in Asia were performed in Eastern Asia.
Figure 4.
Reductions in Individual Cardiac Procedure Modality in Each Subregion
Reductions in the number of each procedure type in each Asian subregion. Note the different y-axis for each subregion. Abbreviations as in Figure 2.
Figure 5.
Reductions in Stress Tests Volume in Each Subregion
Reductions in the number of each stress procedure in each Asian subregion. Note the different y-axis for each subregion. Abbreviations as in Figures 2 and 3.
Center capacity and practice
We questioned whether any changes in center capacity and practices occurred during the enrollment period compared with the pre-COVID period. Numerous changes were observed in Asian facilities (Table 2). “Some outpatient activity canceled” was experienced in the majority of centers (78%), although slightly less often than in the rest of the world (85%; P = 0.038). Although the majority of centers allowed increased time per study for cleaning and disinfection (57%) and eliminated protocols requiring close contact (51%), those changes were less common than in the rest of the world (77%; P < 0.001; 65%; P = 0.001, respectively). Indicators of additional workload for medical workers, such as extended hours (17%) and new weekend hours (13%), were not common, which was similar to the rest of the world.
Table 2.
Changes in Center Capacity and Practice
| Eastern | South-Eastern | Southern | Western and Central | P Value | Asia | RoW | P Value | |
|---|---|---|---|---|---|---|---|---|
| Change in capacity | ||||||||
| Some outpatient activities cancelled | 59 (73) | 31 (86) | 29 (81) | 20 (80) | 0.449 | 139 (78) | 613 (85) | 0.038 |
| All outpatient activities cancelled | 27 (34) | 20 (56) | 22 (61) | 11 (46) | 0.024 | 80 (45) | 325 (45) | 0.952 |
| Phased reopening after peak pandemic | 48 (59) | 19 (53) | 23 (66) | 10 (40) | 0.218 | 100 (56) | 382 (53) | 0.381 |
| Extended hours | 15 (19) | 5 (14) | 4 (11) | 6 (24) | 0.543 | 30 (17) | 93 (13) | 0.161 |
| New weekend hours | 11 (14) | 5 (14) | 4 (11) | 3 (12) | 0.977 | 23 (13) | 63 (9) | 0.085 |
| Use of telehealth for patient care | 45 (56) | 19 (53) | 21 (58) | 12 (48) | 0.855 | 97 (55) | 406 (56) | 0.731 |
| Increased time per study for cleaning/disinfection | 47 (58) | 15 (42) | 25 (66) | 16 (64) | 0.158 | 103 (57) | 554 (77) | <0.001 |
| Eliminate protocols requiring close contact | 27 (33) | 22 (61) | 27 (71) | 15 (60) | <0.001 | 91 (51) | 466 (65) | 0.001 |
| Change in practice | ||||||||
| Physical distancing | 67 (83) | 32 (89) | 30 (83) | 21 (84) | <0.001 | 150 (84) | 655 (91) | 0.014 |
| Separate spaces for COVID-19+/− | 68 (84) | 31 (86) | 29 (81) | 16 (64) | 0.874 | 144 (81) | 573 (80) | 0.820 |
| Reduced waiting room time | 51 (63) | 33 (92) | 27 (75) | 18 (72) | 0.155 | 129 (72) | 610 (84) | <0.001 |
| Limit visitors | 74 (91) | 32 (89) | 32 (89) | 20 (80) | 0.010 | 158 (89) | 676 (93) | 0.031 |
| Temperature checks | 72 (89) | 30 (83) | 29 (81) | 18 (72) | 0.445 | 149 (84) | 462 (64) | <0.001 |
| Symptom screening | 72 (89) | 31 (86) | 27 (75) | 15 (63) | 0.212 | 145 (82) | 562 (78) | 0.247 |
| COVID-19 testing | 27 (33) | 3 (8) | 7 (19) | 4 (16) | 0.018 | 41 (23) | 96 (13) | 0.001 |
| Require masks | 63 (78) | 26 (72) | 28 (74) | 19 (76) | 0.016 | 136 (76) | 544 (75) | 0.840 |
Values are actual facility number (% to total facility number).
COVID-19 = coronavirus disease-2019.
Adoption of infection prevention and control measures, such as separate spaces for COVID-19–positive patients (81%), restricting visitors (89%), screening for symptoms (82%), and requiring masks (76%), were implemented in most centers in Asia as well as in the rest of the world. However, physical distancing (84%) and reducing wait room times (72%) were less often implemented, and checking temperatures (84%) was more often implemented compared with the rest of the world (P = 0.014, P < 0.001, and P < 0.001, respectively). COVID-19 testing was not commonly performed in Asia (23%), but its frequency was still significantly higher (P = 0.001) than in the rest of the world (13%). Similar results were observed among all 4 subregions of Asia, except for COVID-19 testing, which was performed most frequently in Eastern Asia (33% of centers) and less frequently elsewhere (Southeastern 8%, Southern 19%, Western and Central 16%; P = 0.018).
Differences between types of centers
A pattern was observed in the types of facilities and changes in overall procedure volumes (Table 3). University-affiliated teaching facilities showed a smaller reduction (45%) to nonteaching centers (55%). Small hospitals showed greater reductions than larger hospitals (69% reduction in the lowest tertile of number of beds, 35% in the middle tertile, and 42% in the highest tertile). Similar results were obtained in the rest of the world, but reductions tended to be smaller in Asia compared with the rest of the world.
Table 3.
Overall Percent Reductions in Cardiovascular Diagnostic Procedures by the Type of Center
| TTE | TEE | CMR | PET Infection | CAC | Coronary CTA | ICA | Stress Tests |
Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ECG | Echo | SPECT | PET | CMR | |||||||||
| Type of facility | |||||||||||||
| Inpatient | 39/66 | 60/78 | 42/69 | 50/63 | 46/89 | 42/68 | 54/58 | 78/86 | 80/83 | 54/79 | 58/54 | 48/74 | 47/70 |
| Outpatient | 39/72 | 100/82 | —/80 | —/69 | 0/85 | −15/62 | 56/52 | 70/85 | 100/85 | 58/74 | —/62 | —/73 | 48/75 |
| Teaching center status | |||||||||||||
| Teaching | 38/65 | 57/78 | 42/70 | 57/63 | 44/89 | 42/66 | 54/57 | 77/87 | 74/84 | 56/80 | 79/58 | 44/69 | 45/70 |
| Nonteaching | 43/71 | 74/78 | 49/74 | 29/63 | 74/87 | 41/69 | 55/62 | 80/84 | 87/80 | 49/75 | 23/53 | 60/82 | 55/74 |
| Hospital beds | |||||||||||||
| Lowest Tertile | 60/75 | 77/79 | 63/76 | 47/77 | 75/81 | 51/71 | 67/60 | 84/87 | 89/82 | 75/82 | 78/66 | 100/77 | 69/77 |
| Middle Tertile | 26/62 | 39/81 | 17/72 | 47/70 | 74/90 | 18/63 | 26/58 | 73/84 | 75/82 | 63/78 | 51/58 | 36/80 | 35/69 |
| Highest Tertile | 37/65 | 45/78 | 35/62 | 61/56 | 42/88 | 43/67 | 49/58 | 72/88 | 66/82 | 44/80 | 81/50 | 58/60 | 42/68 |
Numbers are presented as Asia/RoW.
CAC = coronary artery calcium; CMR = cardiac magnetic resonance; CTA = computed tomography angiography; ECG = electrocardiogram; Echo = echocardiography; ICA = invasive coronary angiography; PET = positron emission tomography; RoW = rest of the world; SPECT = single-photon emission computed tomography; TEE = transesophageal echocardiography; TTE = transthoracic echocardiography.
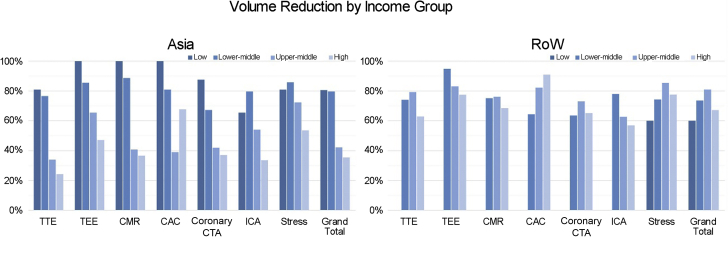
Disparities by income levels
Differences were observed in procedure reductions between countries in Asia based on the World Bank income groups (Table 1, Figure 6). COVID-19–associated reductions in cardiac diagnostic procedures were more prominent in countries with lower per capita income. Data for low-income countries were available for only 4 countries worldwide and 2 in Asia, and data for 1 Asian low-income country was incomplete, making it difficult to compare data between low-income countries in Asia and the rest of the world. However, in the 3 other categories—upper-middle income (9 countries), lower-middle income (12 countries), and high income (10 countries)—Asian countries with lower per capita income clearly experienced greater procedure reductions than high-income Asian countries across procedure types.
Figure 6.
Reductions in Cardiac Diagnostic Procedures by Income Levels
Reductions in the number of cardiac diagnostic procedures in low, lower-middle, upper-middle, and high-income countries between March 2019 and April 2020. ICA = invasive coronary angiography; other abbreviations as in Figure 2.
Discussion
The rapid global spread of COVID-19 has changed the global economy and social environment and has had a negative impact on routine medical practice, particularly the diagnostic evaluation of CVD (13,41, 42, 43). The magnitude of COVID-19’s impact on procedure volumes for evaluation of CVD has not yet been quantitatively evaluated. Led by the IAEA, INCAPS COVID is the first international survey conducted to assess this knowledge gap (22). The present study is a subanalysis of data collected in Asia, which was the first region to be affected by COVID-19. Although our subanalysis revealed that many effects of the COVID-19 pandemic were similar in Asia and the rest of the world, the following differences were noted: 1) early recovery in the number of examinations performed, which was specific to the Eastern Asia subregion; 2) important regional differences in the magnitude of the impact, with Eastern Asia experiencing a smaller impact; and 3) differences in procedure volume reduction observed based on economic status, with lower-income countries being more adversely affected.
The negative impact of the pandemic was reflected by a reduced number of diagnostic procedures and changes in capacities and clinical safety practices, such as physical distancing, temperature checking, and limiting patient volumes. Small centers and low-income countries were most negatively impacted by the pandemic. Similar results were observed between Asia and the rest of the world. However, the Eastern Asian region experienced some recovery of procedure volume from March 2020 to April 2020. This observation may be attributable to the temporal spread of COVID-19 in Asia. In China, the number of examinations had already severely decreased by March 2020, whereas a recovery of diagnostic procedure volume was observed in April 2020. In Korea, the nadir occurred between March 2020 and April 2020. In Japan, the number of examinations had not yet decreased in March 2020, but then markedly declined in April 2020. This result corresponds to the differential arrival of the first wave of COVID-19 spread in these countries. The first wave peaked in February 2020 in China, March 2020 in Korea, and April 2020 in Japan, indicating a general coincidence in the order of peak infection rate and decline in the number of examinations (18,44,45). These observations suggest that decreases in cardiac examinations caused by COVID-19 will become more severe as the number of patients with COVID-19 increases, a pattern that may be attenuated with appropriate responses and countermeasures.
Interestingly, this relationship between the convergence of the first wave of COVID-19 and the stabilization of the cardiac procedure volume was not seen in all Asian subregions. Southern Asia, which includes India and Iran, showed the greatest reductions in procedure numbers among the 4 Asian subregions (Central Illustration, Table 1), whereas most of the countries in this region, except Iran, did not experience a first wave of the COVID-19 pandemic during the study period of March 2020 to April 2020 (18,44). The reasons for the large reductions in procedure volumes preceding an increase in COVID-19 patients in this subregion are not clear. It is possible that reduced volume reflects a proactive measure as centers prepared for the arrival of the first wave, rather than a reactive one. In the unique case of Cambodia, which as of November 2020 has reported 308 cases and no COVID-19 deaths (18), almost no reduction in procedure volume was observed. Its apparent success in containing the coronavirus while simultaneously maintaining other health care services will surely be a topic of much investigation and discussion in the months and years to come.
The observed decrease in the number of procedures was similar when looking specifically at stress testing. However, stress testing procedures did not recover to the same extent as nonstress testing. This may be related to the potential risk of aerosolization during exercise stress testing. It is also possible that the response to COVID-19 caused a paradigm shift in cardiac testing, prompting a shift away from exercise testing. It is interesting to note that a recovery of nuclear stress tests was observed in Eastern Asia. Nuclear stress tests are generally performed with exercise or pharmacological agents, with a preference for pharmacological stress testing in recent years (9). This shift to pharmacological stress testing may have been accelerated in the process of responding to COVID-19. However, there is a lack of published comparisons between volume and types of examinations conducted before and after the COVID-19 era.
The relationship between income status and procedure volume markedly differed between Asia and the rest of the world. The initial INCAPS COVID survey showed greater procedure volume declines in low-income countries than in high-income countries, and it appears that much of this difference was driven by data from Asia. Indeed, when data from Asia are excluded, the relationship between economic status and procedure volume reductions in our survey becomes significantly less pronounced. The reasons for this relationship between income and reduction in procedure volumes in Asia remain unclear. One possibility is that these differences may have emerged because Asia was the first region to be affected by COVID-19. It is also possible that the relationship between economic status and the reduction of cardiovascular procedures might be related to the source of health care funding (eg, government, socialized health support, private insurance, or personal out-of-pocket), which requires more detailed analysis. In any case, these results may contribute to the establishment of a common international understanding of how to allocate health care resource support. Countries with low economic status tend to have population centers that experience overcrowding and limited infrastructure, making it difficult to adhere to public health rules such as social distancing (46). They also tend to have fewer health care resources than developed countries, which may make them more susceptible to the impact of COVID-19 (47,48). The association we observed between a country’s per capita income and reduction in cardiovascular diagnostic procedures may suggest a need to reallocate global health support to poorer countries. Further research on the long-term impact of COVID-19 on cardiovascular testing in low- and middle-income countries is needed.
Study limitations
A major limitation of the present study is the relatively narrow temporal range of data obtained. The data are limited to March 2020 and April 2020, whereas the peak of the first wave of COVID-19 occurred before March 2020 in China and after April 2020 in other countries. The COVID-19 pandemic is ongoing, and long-term changes in the use of cardiac testing are expected. Additionally, recognition of “long covid” (post-acute sequelae of SARS CoV-2) may lead to increased cardiac testing use. Continued data collection and analyses are needed to clarify those effects. The INCAPS COVID Investigators Group is planning to perform a second survey (INCAPS COVID 2) to evaluate those unanswered questions. Another limitation is that participation in the study was voluntary, and therefore the density of the data varied significantly between countries and may not be generalizable. In some countries, data were only available from a single facility, which is unlikely to be representative of the prevailing conditions across the country as a whole. To compensate for this limitation, the Asian region was divided into 4 subregions, each comprised of multiple countries, as comparison at the country level was not feasible. However, heterogeneity in the density of the data persisted even when countries were grouped together into 4 subregions; indeed, data from Eastern Asia accounted for approximately 70% of all Asian data. Because the data were based on a voluntary survey, the information cannot be validated for errors or inaccuracies. Despite these limitations, the data obtained provide important and timely insight on the impact of the ongoing global COVID-19 pandemic on cardiovascular diagnostic procedures.
Conclusions
COVID-19 caused a significant reduction of cardiovascular diagnostic procedures in Asia. Lower-income countries showed greater reductions than higher-income countries, and this trend was more prominent in Asia than in the rest of the world. Significant differences between Asian subregions were also observed. In Eastern Asia, a recovery of procedure volumes was observed as of April 2020, particularly in China, whereas a further decline was observed in other regions. Further study is warranted to determine the impact of the COVID-19 pandemic on CVD morbidity and mortality, as well as to develop strategies to maintain essential health care services like cardiac diagnostics in a resurgence of COVID-19 or in future pandemics.
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE: The COVID-19 pandemic was associated with severe reductions in cardiovascular diagnostic procedural volumes in Asia, with a particularly pronounced impact on countries with lower socioeconomic status.
TRANSLATIONAL OUTLOOK: The effects of reduced procedural volume on CVD morbidity and mortality are not known at this point, and further study is warranted to address this gap in knowledge as well as to develop strategies for maintaining the availability of cardiac diagnostics in the event of a resurgence of COVID-19 or another pandemic.
Funding Support And Author Disclosures
This work was supported by the International Atomic Energy Agency (IAEA). The INCAPS-COVID study was led by the IAEA, which provided the required infrastructure for data collection. Information from participating centers was provided on a voluntary basis and no compensation was paid. The IAEA covers the cost of open access of any published manuscript. Dr Kudo has received consulting fees from Nihon mediphysics and FUJIFILM Toyama Chemical; and his institution has received grants from Nihon mediphysics and FUJIFILM Toyama Chemical, all unrelated to the current work. Dr Dorbala has received honoraria from Pfizer and GE Healthcare; and her institution has received grants from Pfizer and GE Healthcare, all unrelated to the current work. Dr Einstein has received consulting fees from W. L. Gore and Associates; has received fees for lecturing from Ionetix; and his institution has grants/grants pending from Canon Medical Systems, Eidos Therapeutics, GE Healthcare, Roche Medical Systems, W. L. Gore and Associates, and XyloCor Therapeutics, all unrelated to the current work. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
Laurence S. Sperling, MD, served as Guest Associate Editor for this paper. Nathan Wong, PhD, served as Guest Editor-in-Chief for this paper.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For the INCAPS COVID Investigators Group members, cooperating societies, and Asian countries included in the Asia substudy as well as a supplemental table, please see the online version of this paper.
Contributor Information
Takashi Kudo, Email: tkudo123@nagasaki-u.ac.jp.
Andrew J. Einstein, Email: ae2214@cumc.columbia.edu.
INCAPS COVID Investigators Group:
Andrew J. Einstein, Diana Paez, Maurizio Dondi, Nathan Better, Rodrigo Cerci, Sharmila Dorbala, Thomas N.B. Pascual, Paolo Raggi, Leslee J. Shaw, Todd C. Villines, Joao V. Vitola, Michelle C. Williams, Yaroslav Pynda, Gerd Hinterleitner, Yao Lu, Olga Morozova, Zhuoran Xu, Cole B. Hirschfeld, Yosef Cohen, Benjamin Goebel, Eli Malkovskiy, Michael Randazzo, Andrew Choi, Juan Lopez-Mattei, Purvi Parwani, Mohammad Nawaz Nasery, Artan Goda, Ervina Shirka, Rabie Benlabgaa, Salah Bouyoucef, Abdelkader Medjahedi, Qais Nailli, Mariela Agolti, Roberto Nicolas Aguero, Maria del Carmen Alak, Lucia Graciela Alberguina, Guillermo Arroñada, Andrea Astesiano, Alfredo Astesiano, Carolina Bas Norton, Pablo Benteo, Juan Blanco, Juan Manuel Bonelli, Jose Javier Bustos, Raul Cabrejas, Jorge Cachero, Roxana Campisi, Alejandro Canderoli, Silvia Carames, Patrícia Carrascosa, Ricardo Castro, Oscar Cendoya, Luciano Martin Cognigni, Carlos Collaud, Carlos Collaud, Claudia Cortes, Javier Courtis, Daniel Cragnolino, Mariana Daicz, Alejandro De La Vega, Silvia Teresa De Maria, Horacio Del Riego, Fernando Dettori, Alejandro Deviggiano, Laura Dragonetti, Mario Embon, Ruben Emilio Enriquez, Jorge Ensinas, Fernando Faccio, Adolfo Facello, Diego Garofalo, Ricardo Geronazzo, Natalia Gonza, Lucas Gutierrez, Miguel Angel Guzzo, Miguel Angel Guzzo, Victor Hasbani, Melina Huerin, Victor Jäger, Julio Manuel Lewkowicz, Maria Nieves A. López De Munaín, Jose Maria Lotti, Alejandra Marquez, Osvaldo Masoli, Osvaldo Horacio Masoli, Edgardo Mastrovito, Matias Mayoraz, Graciela Eva Melado, Anibal Mele, Maria Fernanda Merani, Alejandro Horacio Meretta, Susana Molteni, Marcos Montecinos, Eduardo Noguera, Carlos Novoa, Claudio Pereyra Sueldo, Sebastian Perez Ascani, Pablo Pollono, Maria Paula Pujol, Alejandro Radzinschi, Gustavo Raimondi, Marcela Redruello, Marina Rodríguez, Matías Rodríguez, Romina Lorena Romero, Arturo Romero Acuña, Federico Rovaletti, Lucas San Miguel, Lucrecia Solari, Bruno Strada, Sonia Traverso, Sonia Simona Traverzo, Maria del Huerto Velazquez Espeche, Juan Sebastian Weihmuller, Juan Wolcan, Susana Zeffiro, Mari Sakanyan, Scott Beuzeville, Raef Boktor, Patrick Butler, Jennifer Calcott, Loretta Carr, Virgil Chan, Charles Chao, Woon Chong, Mark Dobson, D'Arne Downie, Girish Dwivedi, Barry Elison, Jean Engela, Roslyn Francis, Anand Gaikwad, Ashok Gangasandra Basavaraj, Bruce Goodwin, Robert Greenough, Christian Hamilton-Craig, Victar Hsieh, Subodh Joshi, Karin Lederer, Kenneth Lee, Joseph Lee, John Magnussen, Nghi Mai, Gordon Mander, Fiona Murton, Dee Nandurkar, Johanne Neill, Edward O'Rourke, Patricia O'Sullivan, George Pandos, Kunthi Pathmaraj, Alexander Pitman, Rohan Poulter, Manuja Premaratne, David Prior, Lloyd Ridley, Natalie Rutherford, Hamid Salehi, Connor Saunders, Luke Scarlett, Sujith Seneviratne, Deepa Shetty, Ganesh Shrestha, Jonathan Shulman, Vijay Solanki, Tony Stanton, Murch Stuart, Michael Stubbs, Ian Swainson, Kim Taubman, Andrew Taylor, Paul Thomas, Steven Unger, Anthony Upton, Shankar Vamadevan, William Van Gaal, Johan Verjans, Demetrius Voutnis, Victor Wayne, Peter Wilson, David Wong, Kirby Wong, John Younger, Gudrun Feuchtner, Siroos Mirzaei, Konrad Weiss, Natallia Maroz-Vadalazhskaya, Olivier Gheysens, Filip Homans, Rodrigo Moreno-Reyes, Agnès Pasquet, Veronique Roelants, Caroline M. Van De Heyning, Raúl Araujo Ríos, Valentina Soldat-Stankovic, Sinisa Stankovic, Maria Helena Albernaz Siqueira, Augusto Almeida, Paulo Henrique Alves Togni, Jose Henrique Andrade, Luciana Andrade, Carlos Anselmi, Roberta Araújo, Guilherme Azevedo, Sabbrina Bezerra, Rodrigo Biancardi, Gabriel Blacher Grossman, Simone Brandão, Diego Bromfman Pianta, Lara Carreira, Bruno Castro, Tien Chang, Fernando Cunali, Jr., Roberto Cury, Roberto Dantas, Fernando de Amorim Fernandes, Andrea De Lorenzo, Robson De Macedo Filho, Fernanda Erthal, Fabio Fernandes, Juliano Fernandes, Fabio Fernandes, Thiago Ferreira De Souza, Wilson Furlan Alves, Bruno Ghini, Luiz Goncalves, Ilan Gottlieb, Marcelo Hadlich, Vinícius Kameoka, Ronaldo Lima, Adna Lima, Rafael Willain Lopes, Ricardo Machado e Silva, Tiago Magalhães, Fábio Martins Silva, Luiz Eduardo Mastrocola, Fábio Medeiros, José Claudio Meneghetti, Vania Naue, Danilo Naves, Roberto Nolasco, Cesar Nomura, Joao Bruno Oliveira, Eduardo Paixao, Filipe Penna De Carvalho, Ibraim Pinto, Priscila Possetti, Mayra Quinta, Rodrigo Rizzo Nogueira Ramos, Ricardo Rocha, Alfredo Rodrigues, Carlos Rodrigues, Leila Romantini, Adelina Sanches, Sara Santana, Leonardo Sara da Silva, Paulo Schvartzman, Cristina Sebastião Matushita, Tiago Senra, Afonso Shiozaki, Maria Eduarda Menezes de Siqueira, Cristiano Siqueira, Paola Smanio, Carlos Eduardo Soares, José Soares Junior, Marcio Sommer Bittencourt, Bernardo Spiro, Cláudio Tinoco Mesquita, Jorge Torreao, Rafael Torres, Marly Uellendahl, Guilherme Urpia Monte, Otávia Veríssimo, Estevan Vieira Cabeda, Felipe Villela Pedras, Roberto Waltrick, Marcello Zapparoli, Hamid Naseer, Marina Garcheva-Tsacheva, Irena Kostadinova, Youdaline Theng, Gad Abikhzer, Rene Barette, Benjamin Chow, Dominique Dabreo, Matthias Friedrich, Ria Garg, Mohammed Nassoh Hafez, Chris Johnson, Marla Kiess, Jonathon Leipsic, Eugene Leung, Robert Miller, Anastasia Oikonomou, Stephan Probst, Idan Roifman, Gary Small, Vikas Tandon, Adwait Trivedi, James White, Katherine Zukotynski, Jose Canessa, Gabriel Castro Muñoz, Carmen Concha, Pablo Hidalgo, Cesar Lovera, Teresa Massardo, Luis Salazar Vargas, Pedro Abad, Harold Arturo, Sandra Ayala, Luis Benitez, Alberto Cadena, Carlos Caicedo, Antonio Calderón Moncayo, Antonio Calderón Moncayo, Sharon Gomez, Claudia T. Gutierrez Villamil, Claudia Jaimes, Juan Londoño, Juan Luis Londoño Blair, Luz Pabon, Mauricio Pineda, Juan Carlos Rojas, Diego Ruiz, Manuel Valencia Escobar, Andres Vasquez, Damiana Vergel, Alejandro Zuluaga, Isabel Berrocal Gamboa, Gabriel Castro, Ulises González, Ana Baric, Tonci Batinic, Maja Franceschi, Maja Hrabak Paar, Mladen Jukic, Petar Medakovic, Viktor Persic, Marina Prpic, Ante Punda, Juan Felipe Batista, Juan Manuel Gómez Lauchy, Yamile Marcos Gutierrez, Yamile Marcos Gutierrez, Rayner Menéndez, Amalia Peix, Luis Rochela, Christoforos Panagidis, Ioannis Petrou, Vaclav Engelmann, Milan Kaminek, Vladimír Kincl, Otto Lang, Milan Simanek, Jawdat Abdulla, Morten Bøttcher, Mette Christensen, Lars Christian Gormsen, Philip Hasbak, Søren Hess, Paw Holdgaard, Allan Johansen, Kasper Kyhl, Bjarne Linde Norgaard, Kristian Altern Øvrehus, Niels Peter Rønnow Sand, Rolf Steffensen, Anders Thomassen, Bo Zerahn, Alfredo Perez, Giovanni Alejandro Escorza Velez, Mayra Sanchez Velez, Islam Shawky Abdel Aziz, Mahasen Abougabal, Taghreed Ahmed, Adel Allam, Ahmed Asfour, Mona Hassan, Alia Hassan, Ahmed Ibrahim, Sameh Kaffas, Ahmed Kandeel, Mohamed Mandour Ali, Ahmad Mansy, Hany Maurice, Sherif Nabil, Mahmoud Shaaban, Ana Camila Flores, Anne Poksi, Juhani Knuuti, Velipekka Kokkonen, Martti Larikka, Valtteri Uusitalo, Matthieu Bailly, Samuel Burg, Jean-François Deux, Vincent Habouzit, Fabien Hyafil, Olivier Lairez, Franck Proffit, Hamza Regaieg, Laure Sarda-Mantel, Vania Tacher, Roman P. Schneider, Harold Ayetey, George Angelidis, Aikaterini Archontaki, Sofia Chatziioannou, Ioannis Datseris, Christina Fragkaki, Panagiotis Georgoulias, Sophia Koukouraki, Maria Koutelou, Eleni Kyrozi, Evangelos Repasos, Petros Stavrou, Pipitsa Valsamaki, Carla Gonzalez, Goleat Gutierrez, Alejandro Maldonado, Klara Buga, Ildiko Garai, Pál Maurovich-Horvat, Erzsébet Schmidt, Balint Szilveszter, Edit Várady, Nilesh Banthia, Jinendra Kumar Bhagat, Rishi Bhargava, Vivek Bhat, Mona Bhatia, Partha Choudhury, Vijay Sai Chowdekar, Aparna Irodi, Shashank Jain, Elizabeth Joseph, Sukriti Kumar, Prof Dr Girijanandan Mahapatra, Deepanjan Mitra, Bhagwant Rai Mittal, Ahmad Ozair, Chetan Patel, Tapan Patel, Ravi Patel, Shivani Patel, Sudhir Saxena, Shantanu Sengupta, Santosh Singh, Bhanupriya Singh, Ashwani Sood, Atul Verma, Erwin Affandi, Padma Savenadia Alam, Edison Edison, Gani Gunawan, Habusari Hapkido, Basuki Hidayat, Aulia Huda, Anggoro Praja Mukti, Djoko Prawiro, Erwin Affandi Soeriadi, Hilman Syawaluddin, Amjed Albadr, Majid Assadi, Farshad Emami, Golnaz Houshmand, Majid Maleki, Maryam Tajik Rostami, Seyed Rasoul Zakavi, Eed Abu Zaid, Svetlana Agranovich, Yoav Arnson, Rachel Bar-Shalom, Alex Frenkel, Galit Knafo, Rachel Lugassi, Israel Shlomo Maor Moalem, Maya Mor, Noam Muskal, Sara Ranser, Aryeh Shalev, Domenico Albano, Pierpaolo Alongi, Gaspare Arnone, Elisa Bagatin, Sergio Baldari, Matteo Bauckneht, Paolo Bertelli, Francesco Bianco, Rachele Bonfiglioli, Roberto Boni, Andrea Bruno, Isabella Bruno, Elena Busnardo, Elena Califaretti, Luca Camoni, Aldo Carnevale, Roberta Casoni, Armando Ugo Cavallo, Giorgio Cavenaghi, Franca Chierichetti, Marcello Chiocchi, Corrado Cittanti, Mauro Colletta, Umberto Conti, Alberto Cossu, Alberto Cuocolo, Marco Cuzzocrea, Maria Luisa De Rimini, Giuseppe De Vincentis, Eleonora Del Giudice, Alberico Del Torto, Veronica Della Tommasina, Rexhep Durmo, Paola Anna Erba, Laura Evangelista, Riccardo Faletti, Evelina Faragasso, Mohsen Farsad, Paola Ferro, Luigia Florimonte, Viviana Frantellizzi, Fabio Massimo Fringuelli, Marco Gatti, Angela Gaudiano, Alessia Gimelli, Raffaele Giubbini, Francesca Giuffrida, Salvatore Ialuna, Riccardo Laudicella, Lucia Leccisotti, Lucia Leva, Riccardo Liga, Carlo Liguori, Giampiero Longo, Margherita Maffione, Maria Elisabetta Mancini, Claudio Marcassa, Elisa Milan, Barbara Nardi, Sara Pacella, Giovanna Pepe, Gianluca Pontone, Sabina Pulizzi, Natale Quartuccio, Lucia Rampin, Fabrizio Ricci, Pierluigi Rossini, Giuseppe Rubini, Vincenzo Russo, Gian Mauro Sacchetti, Gianmario Sambuceti, Massimo Scarano, Roberto Sciagrà, Massimiliano Sperandio, Antonella Stefanelli, Guido Ventroni, Stefania Zoboli, Dainia Baugh, Duane Chambers, Ernest Madu, Felix Nunura, Hiroshi Asano, Chimura Misato Chimura, Shinichiro Fujimoto, Koichiro Fujisue, Tomohisa Fukunaga, Yoshimitsu Fukushima, Kae Fukuyama, Jun Hashimoto, Yasutaka Ichikawa, Nobuo Iguchi, Masamichi Imai, Anri Inaki, Hayato Ishimura, Satoshi Isobe, Toshiaki Kadokami, Takao Kato, Takashi Kudo, Shinichiro Kumita, Hirotaka Maruno, Hiroyuki Mataki, Masao Miyagawa, Ryota Morimoto, Masao Moroi, Shigeki Nagamachi, Kenichi Nakajima, Tomoaki Nakata, Ryo Nakazato, Mamoru Nanasato, Masanao Naya, Takashi Norikane, Yasutoshi Ohta, Satoshi Okayama, Atsutaka Okizaki, Yoichi Otomi, Hideki Otsuka, Masaki Saito, Sakata Yasushi Sakata, Masayoshi Sarai, Daisuke Sato, Shinya Shiraishi, Yoshinobu Suwa, Kentaro Takanami, Kazuya Takehana, Junichi Taki, Nagara Tamaki, Yasuyo Taniguchi, Hiroki Teragawa, Nobuo Tomizawa, Kenichi Tsujita, Kyoko Umeji, Yasushi Wakabayashi, Shinichiro Yamada, Shinya Yamazaki, Tatsuya Yoneyama, Mohammad Rawashdeh, Daultai Batyrkhanov, Tairkhan Dautov, Khalid Makhdomi, Kevin Ombati, Faridah Alkandari, Masoud Garashi, Tchoyoson Lim Coie, Sonexay Rajvong, Artem Kalinin, Marika Kalnina, Mohamad Haidar, Renata Komiagiene, Giedre Kviecinskiene, Mindaugas Mataciunas, Donatas Vajauskas, Christian Picard, Noor Khairiah A. Karim, Luise Reichmuth, Anthony Samuel, Mohammad Aaftaab Allarakha, Ambedhkar Shantaram Naojee, Erick Alexanderson-Rosas, Erika Barragan, Alejandro Becerril González-Montecinos, Manuel Cabada, Daniel Calderon Rodriguez, Isabel Carvajal-Juarez, Violeta Cortés, Filiberto Cortés, Erasmo De La Peña, Manlio Gama-Moreno, Luis González, Nelsy Gonzalez Ramírez, Moisés Jiménez-Santos, Luis Matos, Edgar Monroy, Martha Morelos, Mario Ornelas, Jose Alberto Ortga Ramirez, Andrés Preciado-Anaya, Óscar Ulises Preciado-Gutiérrez, Adriana Puente Barragan, Sandra Graciela Rosales Uvera, Sigelinda Sandoval, Miguel Santaularia Tomas, Lilia M. Sierra-Galan, Lilia M. Sierra-Galan, Silvia Siu, Enrique Vallejo, Mario Valles, Marc Faraggi, Erdenechimeg Sereegotov, Srdja Ilic, Nozha Ben-Rais, Nadia Ismaili Alaoui, Sara Taleb, Khin Pa Pa Myo, Phyo Si Thu, Ram Kumar Ghimire, Bijoy Rajbanshi, Peter Barneveld, Andor Glaudemans, Jesse Habets, Klaas Pieter Koopmans, Jeroen Manders, Stefan Pool, Arthur Scholte, Asbjørn Scholtens, Riemer Slart, Paul Thimister, Erik-Jan Van Asperen, Niels Veltman, Derk Verschure, Nils Wagenaar, John Edmond, Chris Ellis, Kerryanne Johnson, Ross Keenan, Shaw Hua (Anthony) Kueh, Christopher Occleshaw, Alexander Sasse, Andrew To, Niels Van Pelt, Calum Young, Teresa Cuadra, Hector Bladimir Roque Vanegas, Idrissa Adamou Soli, Djibrillou Moussa Issoufou, Tolulope Ayodele, Chibuzo Madu, Yetunde Onimode, Elen Efros-Monsen, Signe Helene Forsdahl, Jenni-Mari Hildre Dimmen, Arve Jørgensen, Isabel Krohn, Pål Løvhaugen, Anders Tjellaug Bråten, Humoud Al Dhuhli, Faiza Al Kindi, Naeema Al-Bulushi, Zabah Jawa, Naima Tag, Muhammad Shehzad Afzal, Shazia Fatima, Muhammad Numair Younis, Musab Riaz, Mohammad Saadullah, Yariela Herrera, Dora Lenturut-Katal, Manuel Castillo Vázquez, José Ortellado, Afroza Akhter, Dianbo Cao, Stephen Cheung, Xu Dai, Lianggeng Gong, Dan Han, Yang Hou, Caiying Li, Tao Li, Dong Li, Sijin Li, Jinkang Liu, Hui Liu, Bin Lu, Ming Yen Ng, Kai Sun, Gongshun Tang, Jian Wang, Ximing Wang, Zhao-Qian Wang, Yining Wang, Yifan Wang, Jiang Wu, Zhifang Wu, Liming Xia, Jiangxi Xiao, Lei Xu, Youyou Yang, Wu Yin, Jianqun Yu, Li Yuan, Tong Zhang, Longjiang Zhang, Yong-Gao Zhang, Xiaoli Zhang, Li Zhu, Ana Alfaro, Paz Abrihan, Asela Barroso, Eric Cruz, Marie Rhiamar Gomez, Vincent Peter Magboo, John Michael Medina, Jerry Obaldo, Davidson Pastrana, Christian Michael Pawhay, Alvin Quinon, Jeanelle Margareth Tang, Bettina Tecson, Kristine Joy Uson, Mila Uy, Magdalena Kostkiewicz, Jolanta Kunikowska, Nuno Bettencourt, Guilhermina Cantinho, Antonio Ferreira, Ghulam Syed, Samer Arnous, Said Atyani, Angela Byrne, Tadhg Gleeson, David Kerins, Conor Meehan, David Murphy, Mark Murphy, John Murray, Julie O'Brien, Ji-In Bang, Henry Bom, Sang-Geon Cho, Chae Moon Hong, Su Jin Jang, Yong Hyu Jeong, Won Jun Kang, Ji-Young Kim, Jaetae Lee, Chang Kyeong Namgung, Young So, Kyoung Sook Won, Venjamin Majstorov, Marija Vavlukis, Barbara Gužic Salobir, Monika Štalc, Theodora Benedek, Imre Benedek, Raluca Mititelu, Claudiu Adrian Stan, Alexey Ansheles, Olga Dariy, Olga Drozdova, Nina Gagarina, Vsevolod Milyevich Gulyaev, Irina Itskovich, Anatoly Karalkin, Alexander Kokov, Ekaterina Migunova, Viktor Pospelov, Daria Ryzhkova, Guzaliya Saifullina, Svetlana Sazonova, Vladimir Sergienko, Irina Shurupova, Tatjana Trifonova, Wladimir Yurievich Ussov, Margarita Vakhromeeva, Nailya Valiullina, Konstantin Zavadovsky, Kirill Zhuravlev, Mirvat Alasnag, Subhani Okarvi, Dragana Sobic Saranovic, Felix Keng, Jia Hao Jason See, Ramkumar Sekar, Min Sen Yew, Andrej Vondrak, Shereen Bejai, George Bennie, Ria Bester, Gerrit Engelbrecht, Osayande Evbuomwan, Harlem Gongxeka, Magritha Jv Vuuren, Mitchell Kaplan, Purbhoo Khushica, Hoosen Lakhi, Lizette Louw, Nico Malan, Katarina Milos, Moshe Modiselle, Stuart More, Mathava Naidoo, Leonie Scholtz, Mboyo Vangu, Santiago Aguadé-Bruix, Isabel Blanco, Antonio Cabrera, Alicia Camarero, Irene Casáns-Tormo, Hug Cuellar-Calabria, Albert Flotats, Maria Eugenia Fuentes Cañamero, María Elia García, Amelia Jimenez-Heffernan, Rubén Leta, Javier Lopez Diaz, Luis Lumbreras, Juan Javier Marquez-Cabeza, Francisco Martin, Anxo Martinez de Alegria, Francisco Medina, Maria Pedrera Canal, Virginia Peiro, Virginia Pubul-Nuñez, Juan Ignacio Rayo Madrid, Cristina Rodríguez Rey, Ricardo Ruano Perez, Joaquín Ruiz, Gertrudis Sabatel Hernández, Ana Sevilla, Nahla Zeidán, Damayanthi Nanayakkara, Chandraguptha Udugama, Magnus Simonsson, Hatem Alkadhi, Ronny Ralf Buechel, Peter Burger, Luca Ceriani, Bart De Boeck, Christoph Gräni, Alix Juillet de Saint Lager Lucas, Christel H. Kamani, Nadine Kawel-Boehm, Robert Manka, John O. Prior, Axel Rominger, Jean-Paul Vallée, Benjapa Khiewvan, Teerapon Premprabha, Tanyaluck Thientunyakit, Ali Sellem, Kemal Metin Kir, Haluk Sayman, Mugisha Julius Sebikali, Zerida Muyinda, Yaroslav Kmetyuk, Pavlo Korol, Olena Mykhalchenko, Volodymyr Pliatsek, Maryna Satyr, Batool Albalooshi, Mohamed Ismail Ahmed Hassan, Jill Anderson, Punit Bedi, Thomas Biggans, Anda Bularga, Russell Bull, Rajesh Burgul, John-Paul Carpenter, Duncan Coles, David Cusack, Aparna Deshpande, John Dougan, Timothy Fairbairn, Alexia Farrugia, Deepa Gopalan, Alistair Gummow, Prasad Guntur Ramkumar, Mark Hamilton, Mark Harbinson, Thomas Hartley, Benjamin Hudson, Nikhil Joshi, Michael Kay, Andrew Kelion, Azhar Khokhar, Jamie Kitt, Ken Lee, Chen Low, Sze Mun Mak, Ntouskou Marousa, Jon Martin, Elisa Mcalindon, Leon Menezes, Gareth Morgan-Hughes, Alastair Moss, Anthony Murray, Edward Nicol, Dilip Patel, Charles Peebles, Francesca Pugliese, Jonathan Carl Luis Rodrigues, Christopher Rofe, Nikant Sabharwal, Rebecca Schofield, Thomas Semple, Naveen Sharma, Peter Strouhal, Deepak Subedi, William Topping, Katharine Tweed, Jonathan Weir-Mccall, Suhny Abbara, Taimur Abbasi, Brian Abbott, Shady Abohashem, Sandra Abramson, Tarek Al-Abboud, Mouaz Al-Mallah, Omar Almousalli, Karthikeyan Ananthasubramaniam, Mohan Ashok Kumar, Jeffrey Askew, Lea Attanasio, Mallory Balmer-Swain, Richard R. Bayer, Adam Bernheim, Sabha Bhatti, Erik Bieging, Ron Blankstein, Stephen Bloom, Sean Blue, David Bluemke, Andressa Borges, Kelley Branch, Paco Bravo, Jessica Brothers, Matthew Budoff, Renée Bullock-Palmer, Angela Burandt, Floyd W. Burke, Kelvin Bush, Candace Candela, Elizabeth Capasso, Joao Cavalcante, Donald Chang, Saurav Chatterjee, Yiannis Chatzizisis, Michael Cheezum, Tiffany Chen, Jennifer Chen, Marcus Chen, Andrew Choi, James Clarcq, Ayreen Cordero, Matthew Crim, Sorin Danciu, Bruce Decter, Nimish Dhruva, Neil Doherty, Rami Doukky, Anjori Dunbar, William Duvall, Rachael Edwards, Kerry Esquitin, Husam Farah, Emilio Fentanes, Maros Ferencik, Daniel Fisher, Daniel Fitzpatrick, Cameron Foster, Tony Fuisz, Michael Gannon, Lori Gastner, Myron Gerson, Brian Ghoshhajra, Alan Goldberg, Brian Goldner, Jorge Gonzalez, Rosco Gore, Sandra Gracia-López, Fadi Hage, Agha Haider, Sofia Haider, Yasmin Hamirani, Karen Hassen, Mallory Hatfield, Carolyn Hawkins, Katie Hawthorne, Nicholas Heath, Robert Hendel, Phillip Hernandez, Gregory Hill, Stephen Horgan, Jeff Huffman, Lynne Hurwitz, Ami Iskandrian, Rajesh Janardhanan, Christine Jellis, Scott Jerome, Dinesh Kalra, Summanther Kaviratne, Fernando Kay, Faith Kelly, Omar Khalique, Mona Kinkhabwala, George Kinzfogl Iii, Jacqueline Kircher, Rachael Kirkbride, Michael Kontos, Anupama Kottam, Joseph Krepp, Jay Layer, Steven H. Lee, Jeffrey Leppo, John Lesser, Steve Leung, Howard Lewin, Diana Litmanovich, Yiyan Liu, Juan Lopez-Mattei, Kathleen Magurany, Jeremy Markowitz, Amanda Marn, Stephen E. Matis, Michael Mckenna, Tony Mcrae, Fernando Mendoza, Michael Merhige, David Min, Chanan Moffitt, Karen Moncher, Warren Moore, Shamil Morayati, Michael Morris, Mahmud Mossa-Basha, Zorana Mrsic, Venkatesh Murthy, Prashant Nagpal, Kyle Napier, Katarina Nelson, Prabhjot Nijjar, Medhat Osman, Purvi Parwani, Edward Passen, Amit Patel, Pravin Patil, Ryan Paul, Lawrence Phillips, Venkateshwar Polsani, Rajaram Poludasu, Brian Pomerantz, Thomas Porter, Ryan Prentice, Amit Pursnani, Mark Rabbat, Suresh Ramamurti, Florence Rich, Hiram Rivera Luna, Austin Robinson, Kim Robles, Cesar Rodríguez, Mark Rorie, John Rumberger, Raymond Russell, Philip Sabra, Diego Sadler, Mary Schemmer, U. Joseph Schoepf, Samir Shah, Nishant Shah, Sujata Shanbhag, Gaurav Sharma, Steven Shayani, Jamshid Shirani, Pushpa Shivaram, Steven Sigman, Mitch Simon, Ahmad Slim, David Smith, Alexandra Smith, Prem Soman, Aditya Sood, Monvadi Barbara Srichai-Parsia, James Streeter, Albert T, Ahmed Tawakol, Dustin Thomas, Randall Thompson, Tara Torbet, Desiree Trinidad, Shawn Ullery, Samuel Unzek, Seth Uretsky, Srikanth Vallurupalli, Vikas Verma, Alfonso Waller, Ellen Wang, Parker Ward, Gaby Weissman, George Wesbey, Kelly White, David Winchester, David Wolinsky, Sandra Yost, Michael Zgaljardic, Omar Alonso, Mario Beretta, Rodolfo Ferrando, Miguel Kapitan, Fernando Mut, Omoa Djuraev, Gulnora Rozikhodjaeva, Ha Le Ngoc, Son Hong Mai, and Xuan Canh Nguyen
Appendix
References
- 1.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19. March 11, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Accessed July 25, 2021.
- 2.Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 3.Toyoshima Y., Nemoto K., Matsumoto S., Nakamura Y., Kiyotani K. SARS-CoV-2 genomic variations associated with mortality rate of COVID-19. J Hum Genet. 2020;65:1075–1082. doi: 10.1038/s10038-020-0808-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Disease burden and mortality estimates: World Health Organization. https://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html Accessed October 28, 2020.
- 5.Yusuf S., Rangarajan S., Teo K., et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371:818–827. doi: 10.1056/NEJMoa1311890. [DOI] [PubMed] [Google Scholar]
- 6.Ford E.S., Ajani U.A., Croft J.B., et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 7.Fuster V., Frazer J., Snair M., Vedanthan R., Dzau V. The future role of the United States in global health: emphasis on cardiovascular disease. J Am Coll Cardiol. 2017;70:3140–3156. doi: 10.1016/j.jacc.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Dzau V., Fuster V., Frazer J., Snair M. Investing in global health for our future. N Engl J Med. 2017;377:1292–1296. doi: 10.1056/NEJMsr1707974. [DOI] [PubMed] [Google Scholar]
- 9.Rozanski A., Gransar H., Hayes S.W., et al. Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. J Am Coll Cardiol. 2013;61:1054–1065. doi: 10.1016/j.jacc.2012.11.056. [DOI] [PubMed] [Google Scholar]
- 10.Shah N.S., Molsberry R., Rana J.S., et al. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999-2018: observational analysis of vital statistics. BMJ. 2020;370:m2688. doi: 10.1136/bmj.m2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li B., Yang J., Zhao F., et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu Z., McGoogan J.M. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 13.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 14.Kirkpatrick J.N., Hull S.C., Fedson S., Mullen B., Goodlin S.J. Scarce-resource allocation and patient triage during the COVID-19 pandemic: JACC review topic of the week. J Am Coll Cardiol. 2020;76:85–92. doi: 10.1016/j.jacc.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lantelme P., Couray Targe S., Metral P., et al. Worrying decrease in hospital admissions for myocardial infarction during the COVID-19 pandemic. Arch Cardiovasc Dis. 2020;113:443–447. doi: 10.1016/j.acvd.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mafham M.M., Spata E., Goldacre R., et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roth G.A., Johnson C., Abajobir A., et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization Coronavirus disease (COVID-19) dashboard. https://covid19.who.int Accessed November 28, 2020.
- 19.Baldi E., Sechi G.M., Mare C., et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41:3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Atomic Energy Agency The statute of the IAEA. https://www.iaea.org/about/statute Accessed October 28, 2020.
- 21.International Atomic Energy Agency Division of Human Health. https://www.iaea.org/about/organizational-structure/department-of-nuclear-sciences-and-applications/division-of-human-health Accessed October 28, 2020.
- 22.Einstein A.J., Shaw L.J., Hirschfeld C.B., et al. International impact of COVID-19 on the diagnosis of heart disease. J Am Coll Cardiol. 2021;77:173–185. doi: 10.1016/j.jacc.2020.10.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Idogawa M., Tange S., Nakase H., Tokino T. Interactive web-based graphs of coronavirus disease 2019 cases and deaths per population by country. Clin Infect Dis. 2020;71:902–903. doi: 10.1093/cid/ciaa500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization weekly epidemiological update. October 20, 2020. https://www.who.int/publications/m/item/weekly-epidemiological-update---20-october-2020 Accessed July 25, 2021.
- 25.World Health Organization COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 March 2020. https://apps.who.int/iris/handle/10665/331561 Accessed July 25, 2021.
- 26.International Atomic Energy Agency COVID-19 pandemic: technical guidance for nuclear medicine departments, July 2020. https://www-pub.iaea.org/MTCD/Publications/PDF/COVID19_web.pdf Accessed July 26, 2021.
- 27.Einstein A.J., Pascual T.N., Mercuri M., et al. Current worldwide nuclear cardiology practices and radiation exposure: results from the 65 country IAEA Nuclear Cardiology Protocols Cross-Sectional Study (INCAPS) Eur Heart J. 2015;36:1689–1696. doi: 10.1093/eurheartj/ehv117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lindner O., Pascual T.N., Mercuri M., et al. Nuclear cardiology practice and associated radiation doses in Europe: results of the IAEA Nuclear Cardiology Protocols Study (INCAPS) for the 27 European countries. Eur J Nucl Med Mol Imaging. 2016;43:718–728. doi: 10.1007/s00259-015-3270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shi L., Dorbala S., Paez D., et al. Gender differences in radiation dose from nuclear cardiology studies across the world: findings from the INCAPS registry. J Am Coll Cardiol Img. 2016;9:376–384. doi: 10.1016/j.jcmg.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Biswas S., Better N., Pascual T.N., et al. Nuclear cardiology practices and radiation exposure in the Oceania Region: results from the IAEA Nuclear Cardiology Protocols Study (INCAPS) Heart Lung Circ. 2017;26:25–34. doi: 10.1016/j.hlc.2016.05.112. [DOI] [PubMed] [Google Scholar]
- 31.Bouyoucef S.E., Mercuri M., Pascual T.N., et al. Nuclear cardiology practices and radiation exposure in Africa: results from the IAEA Nuclear Cardiology Protocols Study (INCAPS) Cardiovasc J Afr. 2017;28:229–234. doi: 10.5830/CVJA-2016-091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pascual T.N., Mercuri M., El-Haj N., et al. Nuclear cardiology practice in Asia: analysis of radiation exposure and best practice for myocardial perfusion imaging- results from the IAEA Nuclear Cardiology Protocols Cross-Sectional Study (INCAPS) Circ J. 2017;81:501–510. doi: 10.1253/circj.CJ-16-0677. [DOI] [PubMed] [Google Scholar]
- 33.Vitola J.V., Mut F., Alexanderson E., et al. Opportunities for improvement on current nuclear cardiology practices and radiation exposure in Latin America: findings from the 65-country IAEA Nuclear Cardiology Protocols cross-sectional Study (INCAPS) J Nucl Cardiol. 2017;24:851–859. doi: 10.1007/s12350-016-0433-3. [DOI] [PubMed] [Google Scholar]
- 34.Al-Mallah M.H., Pascual T.N.B., Mercuri M., et al. Impact of age on the selection of nuclear cardiology stress protocols: The INCAPS (IAEA nuclear cardiology protocols) study. Int J Cardiol. 2018;259:222–226. doi: 10.1016/j.ijcard.2018.02.060. [DOI] [PubMed] [Google Scholar]
- 35.United Nations Statistics Division Standard country or area codes for statistical use (M49) https://unstats.un.org/unsd/methodology/m49/ Accessed October 28, 2020.
- 36.World Bank Data Team World Bank country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-countryand-lending-groups Accessed October 28, 2020.
- 37.NUclear Medicine DataBase (NUMDAB) https://www.iaea.org/resources/databases/numdab Accessed October 28, 2020.
- 38.IAEA IRIS International Research Integration System. https://iris.iaea.org Accessed July 26, 2021.
- 39.Tennekes M. tmap: thematic maps in R. J Stat Soft. 2018;84:1–39. doi: 10.18637/jss.v084.i06. [DOI] [Google Scholar]
- 40.Ooms J. rnaturalearth. https://cran.r-project.org/web/packages/rnaturalearth
- 41.Barach P., Fisher S.D., Adams M.J., et al. Disruption of healthcare: will the COVID pandemic worsen non-COVID outcomes and disease outbreaks? Prog Pediatr Cardiol. 2020;59:101254. doi: 10.1016/j.ppedcard.2020.101254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages - the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382:e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 43.Horton R. Offline: COVID-19 is not a pandemic. Lancet. 2020;396:874. doi: 10.1016/S0140-6736(20)32000-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Institute for Health Metrics and Evaluation University of Washington. COVID-19 Projections. https://covid19.healthdata.org/global Accessed October 28, 2020.
- 45.Reuters COVID-19 Global Tracker. https://graphics.reuters.com/world-coronavirus-tracker-and-maps/ Accessed October 28, 2020.
- 46.Brauer M., Zhao J.T., Bennitt F.B., Stanaway J.D. Global access to handwashing: implications for COVID-19 control in low-income countries. Environ Health Perspect. 2020;128:57005. doi: 10.1289/EHP7200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bong C.L., Brasher C., Chikumba E., McDougall R., Mellin-Olsen J., Enright A. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg. 2020;131:86–92. doi: 10.1213/ANE.0000000000004846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McMahon D.E., Peters G.A., Ivers L.C., Freeman E.E. Global resource shortages during COVID-19: bad news for low-income countries. PLoS Negl Trop Dis. 2020;14:e0008412. doi: 10.1371/journal.pntd.0008412. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.