Corresponding Author
Key Words: bifurcation, PCI, single-stent technique
Coronary bifurcations remain 1 of the most technically challenging lesions treated by interventional cardiologists (1,2). Selecting the optimal technique for the wide range of coronary bifurcations remains an area of ongoing debate and investigation (1,2). Implantation of a stent in the main vessel (MV) across the side branch (SB) ostium (ie, “crossover” stenting), with stenting of the SB reserved in case of suboptimal results with either no treatment or balloon angioplasty (ie, 1-stent provisional stenting [PS]), is superior to a planned 2-stent approach for non-complex bifurcation lesions (1, 2, 3). Conversely, in complex distal left main and non-left main bifurcation lesions a 2-stent strategy using a planned double-kissing crush technique has been shown to be superior to a PS strategy (4,5).
Among patients undergoing PS, the optimal treatment of the SB remains uncertain. One issue is whether to perform a final kissing balloon dilatation (KBD) in the MV and SB. In the Nordic-Baltic Bifurcation Study III, patients with bifurcation lesions undergoing a PS strategy were randomized to a final KBD or no KBD (6). At 8 months of follow-up, final KBD resulted in lower rates of angiographic binary restenosis of the SB, but there were no significant differences in binary restenosis in the entire bifurcation lesion and major adverse cardiac events (6). More recently, in a secondary analysis from the EXCEL (Evaluation of XIENCE versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial, the performance of final KBD after percutaneous coronary intervention (PCI) of distal left main coronary artery bifurcation lesions was not associated with improved 4-year clinical outcomes regardless of whether 1 stent or 2 stents were implanted (7).
A second issue, which has received less direct attention, is whether balloon angioplasty of the SB is even necessary in many non-complex bifurcation lesions. This question is particularly relevant because many SBs supply a small amount of myocardium, and many moderate SB stenoses are not flow-limiting. In this issue of JACC: Asia, Lee et al (8) examined the outcomes of bifurcation lesions treated with a PS strategy with or without additional balloon side-branch opening (SBO) from the COBIS (COronary Bifurcation Stenting) III registry. COBIS III is a retrospective, multicenter, observational, real-world registry of patients with bifurcation lesions who underwent PCI with second-generation drug-eluting stents (DES) at 21 centers in the Republic of Korea (3). Both left main and non-left main coronary bifurcations were included. Eligible patients had a MV diameter ≥2.5 mm and SB diameter ≥2.3 mm confirmed by a quantitative coronary angiography core laboratory. For the present analysis, bifurcation lesions treated with 2 stents were excluded, even if the original intent was PS. Access site, type of DES implanted, performance of proximal optimization technique (POT) in both groups or final KBD in the SBO group, and use of SB intravascular imaging or invasive physiological assessment were all left to the operators’ discretion.
A total of 2,194 patients who underwent PCI with a single stent were included; 1,685 (76.8%) bifurcations were treated with stent crossover alone (without SBO), whereas 509 (23.2%) also had SBO. Bifurcation lesions treated with SBO were more complex. They more frequently were true bifurcations (eg, Medina class 1:1:1 or 0:1:1), were distal left main lesions, and had a larger SB reference vessel diameter with greater percent diameter stenosis (DS) and longer lesion length than those not treated with SBO. Intravascular ultrasound and final KBD were used more frequently in the SBO group. The post-procedure SB percent DS was lower after SBO treatment. However, at 5 years, there were no significant differences in the primary composite endpoint of target lesion failure between the SBO and non-SBO groups in both unadjusted (7.0% vs 6.7%; HR: 0.99; 95% CI: 0.66-1.48) and inverse probability of treatment weighting–adjusted (adjusted HR: 0.68; 95% CI: 0.37-1.26) analyses. Nor were there significant differences in target lesion failure in relevant subgroups of patients including left main bifurcations, true bifurcations, and whether intravascular ultrasound or POT were used. The investigators concluded that “the long-term clinical outcome of one stent strategy with simple crossover alone without SBO for coronary bifurcation lesions was acceptable,”
Strengths of the present study are its large sample size, relatively long follow-up time, and use of pre- and post-intervention quantitative coronary angiography. However, several limitations should be recognized. First, the nonrandomized, retrospective nature of the study introduces substantial confounding that cannot be fully accounted for by inverse probability of treatment weighting adjustment. Specifically, patients with more-complex bifurcation lesions were more likely to have SBO, reflecting current beliefs. The choice of the treatment strategy, as well as vascular access, type of DES, and use of intravascular imaging and physiological assessment, was left to the operator discretion, introducing additional biases. Moreover, unmeasured confounders that dictated use of one technique versus the other cannot be accounted for in any nonrandomized trial. Second, no details were reported on MV lesion preparation (eg, atherectomy or atherotomy). The rates of POT were low in both groups, contrary to current practice by many. POT is particularly important when performing final KBD to avoid major geometric distortion in the proximal MV stent (1,2). Third and perhaps most importantly the present analysis is “as treated”—that is, patients who received versus did not receive SBO. An “intention to treat” analysis would have been more informative. Unfortunately, the intent and timing of SBO were not reported. What proportion of SBO cases were intended versus were unplanned but required after MV pre-dilatation or stent implantation? Were such crossovers in intent for simple SB narrowing or SB closure? Furthermore, all cases treated with 2 stents were excluded from the present analysis, including those in whom the initial intent was SBO or non-SBO. How frequently was a SB stent required with each approach? Also unexplored from the present report is whether in cases in which SBO is intended, should it be first performed before or after MV stenting. Finally, it is unclear whether physiological testing was used to evaluate the need to treat the SB either at baseline or after MV stenting. Often there is discordance between the angiographic DS and functional significance (9), although fractional flow reserve–guided SB treatment was not shown to improve clinical outcomes in a randomized trial (10).
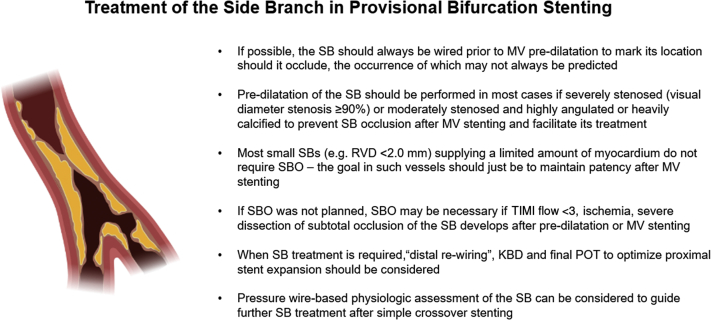
In summary, the present study suggests that a SBO strategy during PS of noncomplex bifurcations may not always be necessary nor associated with improved clinical outcomes compared with simple cross-over stenting without SBO. Thus, notwithstanding the limitations of the present study, it is plausible that many bifurcation lesions can be treated with a PS approach with SB treatment reserved for selected clinical scenarios (Figure 1). However, additional randomized controlled trials are needed to further refine the optimal treatment strategies for coronary bifurcation lesions.
Figure 1.
When to Treat the Side Branch During Provisional Bifurcation Stenting
KBD = kissing balloon dilation; MV = main vessel; POT = proximal optimization technique; RVD = reference vessel diameter; SB = side branch; SBO = side branch opening; TIMI = Thrombolysis In Myocardial Infarction. Created with BioRender.com.
Funding Support and Author Disclosures
Dr. Stone has received speaker or other honoraria from Terumo, Cook; has served as a consultant to Valfix, TherOx, Robocath, HeartFlow, Ablative Solutions, Vectorious, Miracor, Neovasc, Abiomed, Ancora, Elucid Bio, Occlutech, CorFlow, Reva, Matrizyme, MAIA Pharmaceuticals, Vascular Dynamics, Shockwave, V-Wave, Cardiomech, and Gore; and has equity/options from Ancora, Cagent, Applied Therapeutics, Biostar family of funds, SpectraWave, Orchestra Biomed, Aria, Cardiac Success, Valfix, and MedFocus family of funds. Dr. Giustino has reported that he has no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Sawaya F.J., Lefevre T., Chevalier B., et al. Contemporary approach to coronary bifurcation lesion treatment. J Am Coll Cardiol Intv. 2016;9:1861–1878. doi: 10.1016/j.jcin.2016.06.056. [DOI] [PubMed] [Google Scholar]
- 2.Burzotta F., Lassen J.F., Lefevre T., et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15(th) consensus document from the European Bifurcation Club. EuroIntervention. 2021;16:1307–1317. doi: 10.4244/EIJ-D-20-00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi K.H., Song Y.B., Lee J.M., et al. Prognostic effects of treatment strategies for left main versus non-left main bifurcation percutaneous coronary intervention with current-generation drug-eluting stent. Circ Cardiovasc Interv. 2020;13 doi: 10.1161/CIRCINTERVENTIONS.119.008543. [DOI] [PubMed] [Google Scholar]
- 4.Chen S.L., Zhang J.J., Han Y., et al. Double Kissing Crush Versus Provisional Stenting for Left Main Distal Bifurcation Lesions: DKCRUSH-V randomized trial. J Am Coll Cardiol. 2017;70:2605–2617. doi: 10.1016/j.jacc.2017.09.1066. [DOI] [PubMed] [Google Scholar]
- 5.Zhang J.J., Ye F., Xu K., et al. Multicentre, randomized comparison of two-stent and provisional stenting techniques in patients with complex coronary bifurcation lesions: the DEFINITION II trial. Eur Heart J. 2020;41:2523–2536. doi: 10.1093/eurheartj/ehaa543. [DOI] [PubMed] [Google Scholar]
- 6.Niemela M., Kervinen K., Erglis A., et al. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011;123:79–86. doi: 10.1161/CIRCULATIONAHA.110.966879. [DOI] [PubMed] [Google Scholar]
- 7.Kini A.S., Dangas G.D., Baber U., et al. Influence of final kissing balloon inflation on long-term outcomes after PCI of distal left main bifurcation lesions in the EXCEL trial. EuroIntervention. 2020;16:218–224. doi: 10.4244/EIJ-D-19-00851. [DOI] [PubMed] [Google Scholar]
- 8.Lee C.H., Nam C.W., Cho Y.K., et al. 5-year outcome of simple crossover stenting in coronary bifurcation lesions, compared with side branch opening. JACC: Asia. 2021;1:53–64. doi: 10.1016/j.jacasi.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee C.H., Choi S.W., Hwang J., et al. 5-Year outcomes according to FFR of left circumflex coronary artery after left main crossover stenting. J Am Coll Cardiol Intv. 2019;12:847–855. doi: 10.1016/j.jcin.2019.02.037. [DOI] [PubMed] [Google Scholar]
- 10.Chen S.L., Ye F., Zhang J.J., et al. Randomized comparison of FFR-guided and angiography-guided provisional stenting of true coronary bifurcation lesions: the DKCRUSH-VI trial (Double Kissing Crush Versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions VI) J Am Coll Cardiol Intv. 2015;8:536–546. doi: 10.1016/j.jcin.2014.12.221. [DOI] [PubMed] [Google Scholar]