Abstract
Previous studies have shown that experiences of childhood trauma disproportionally impact incarcerated youth and may decrease self-regulation skills including identification of emotions and ability to control behaviors.
Purpose: The current study aimed to investigate changes in emotional state identified by incarcerated youth after receiving sensory-based occupational therapy treatment.
Methods: A quasi-experimental retrospective chart review design was used in addition to surveys.
Results: Participants had an average ACE score of 5.91 traumatic experiences and at least three mental health diagnoses. Results showed a statistically significant change between pre-and post-session emotions via a Likert scale as well as a decrease in the frequency of negative words used to identify emotions. When surveyed, participants reported a calmer body state after occupational therapy and highlighted the importance of learning coping strategies.
Conclusion: Results suggest that sensory-based occupational therapy may be an effective, trauma-informed intervention to improve self-regulation and support daily function of these incarcerated youth.
Keywords: trauma, self-regulation, occupational therapy, sensory-based interventions, juvenile corrections
Introduction
Incarcerated youth disproportionally experience trauma and have high rates of mental health disorders (Baglivio et al., 2014; Dowdy et al., 2020; Kowalski, 2019). These experiences may change neural development and function, impacting the ability to label emotions and manage emotions in an adaptive manner (Chen et al., 2017). Incarcerated youth who have experienced trauma also have pervasive difficulties in self-regulation which is essential for daily function (Perry et al., 2018). Addressing these functional challenges with a trauma-informed approach means that providers recognize traumatic experiences, their impact on function, and then select interventions that address these experiences (Cutuli et al., 2019). Sensory-based interventions are often selected in a trauma-informed approach for treatment as they facilitate a calm, safe state in which youth can practice adaptive strategies for self-regulation (Fraser et al., 2017). Occupational therapists are well-positioned to provide these interventions due to their training in sensory processing, ability to assess daily function, and focus on client-centered care (Alers, 2014). Despite their skill set and scope of practice, occupational therapists are being under-utilized in meeting this need in the juvenile justice system. The aim of the current study was to investigate the impact of sensory-based occupational therapy on participants’ ability to identify a change in emotions as well as to document research participants’ perspectives of sensory-based occupational therapy. The current study adds to a gap in the literature about the impact of sensory-based interventions in addressing skill deficits impacted by trauma.
Complex Trauma
Childhood trauma was defined by the Adverse Childhood Experience (ACE) study as experiences of physical, sexual, and psychological abuse as well as household dysfunction which includes neglect, domestic violence, separation of parents, substance use, mental illness, suicide, and incarceration (Anda et al., 2009; Felitti et al., 1998). When trauma occurs frequently or for long periods of time, especially in the absence of safe adult relationships, it is referred to as complex trauma (Shonkoff & Garner, 2012). Complex trauma dysregulates the neurological stress response system at varying levels depending on age of exposure, type of trauma, duration, number of adversities, interaction among adversities, pre-existing conditions, and protective factors such as supportive caregivers (Nelson et al., 2020; Perry, 2009). Complex trauma that occurs during sensitive periods of development may alter the structure and function of the amygdala, prefrontal cortex, and hippocampus (Shonkoff & Garner, 2012; Teicher et al., 2003). The literature associates these changes with various maladaptive conditions including propensities for mental health diagnoses, increased aggression, poor impulse control, diminished adaptive arousal reactions, and decreased ability to perceive and/or express emotions (Ford et al., 2012; Nelson et al., 2020; Teicher et al., 2003; Thomason & Marusak, 2017).
Juvenile Justice & Complex Trauma
Young people involved in the juvenile justice system have experiences of trauma along with mental health challenges at rates higher than individuals not involved in the criminal justice system (Chen et al., 2017; Hayes & O’Reilly, 2013; Logan-Greene et al., 2017; Baglivio et al., 2014) found that incarcerated youth are four times more likely to experience four or more ACEs and 13 times less likely to report no ACEs than individuals from the original Felitti study (1998). Additionally, Kowalski (2019) found that over 80% of incarcerated youth with mental health issues reported four or more ACEs while nearly 64% of incarcerated youth without mental health diagnoses still reported four or more traumatic events from childhood. The high rates of trauma and mental illness in this population must be addressed as these factors are correlated with a reduction in overall functioning (Duron et al., 2021) and with higher rates of violence in criminal activity (Fox et al., 2015; Kowalski, 2019; Perez et al., 2016). Many incarcerated youth come from environments described as “hot spots” for crime, have been victims of violence, perpetrate violence, and continue to live in violent and traumatic environments in the criminal justice system (Roach, 2013). Their brains must adapt to survive continual trauma and subsequently they appear proactively aggressive, replace fear with anger, and have difficulty with self-regulation (Ford, 2012; Roach 2013).
Trauma’s Impact on Emotions & Self-Regulation
Complex trauma in early life is associated with changes in neural circuits that impact emotional intelligence, defined as one’s ability to recognize, identify, and manage one’s own feelings (Reeves, 2005; Thomason & Marusak, 2017). Incarcerated juveniles who have experienced trauma not only have more difficulty naming their emotions (Chen et al., 2017), but may also struggle to feel their suppressed emotions, an adaptation which they have learned as a coping mechanism (Hodgdon et al., 2013; Roach, 2013). These may manifest as explosive behavior and difficulty calming after stress. The complex trauma incarcerated youth have experienced correlates with an overall disconnection from emotional experiences including lack of body awareness, misinterpretation of emotions expressed by others, and deficits in the ability to control their own arousal levels (Ardizzi et al., 2016; Hart & Rubia, 2012; Pihet et al., 2012; Sharma et al., 2015; Hayes & O’Reilly, 2013) compared emotional identification abilities of juvenile offenders to adolescents with and without identified mental health diagnoses. The results of their study indicated that young detainees had significantly lower abilities to recognize emotions in both themselves and in other people. Emotional identification is important for effective communication, relationship-building, and in one’s ability to achieve self-regulation (Reeves, 2005).
Self-regulation is defined as the ability to control one’s emotions and actions in the context of environmental demands and higher goals (Langer et al., 2018; Perry et al., 2018). Individuals who have experienced complex trauma at an early age are easily dysregulated and may not develop the skills needed to modulate emotions, inhibit impulses, and redirect attention (Evans-Chase, 2014). This is important to note as self-regulation skills start during early periods of development and as such can be accurately predicted as early as the age of five (Perry et al., 2018). However, research shows that aggressive and destructive behaviors often associated with delinquency can be reduced if deficits in emotional management and inhibitory control are addressed in treatment (Perry et al., 2018).
Crucial Role of Sensory Input
The literature supports the premise that both trauma and emotions are processed at a somatosensory level, meaning that the sensory input individuals receive from the environment impacts how traumatic and emotional experiences are perceived, stored, and used to make decisions (Evans & Kim, 2013; Fraser et al., 2017; Mirolli et al., 2010). Chronic stress dysregulates sensory processing so significantly that it has been correlated with sensory patterns of low registration and sensory avoidance (Dowdy et al., 2020; Engel-Yeger et al., 2013). When these patterns and preferences are considered, sensory input can be used strategically to help young people reach a state of self-regulation allowing them to increase body awareness, connect with their emotions, and increase overall ability to cope with the demands of their environment in an adaptive manner (Sutton et al., 2013). Trauma treatment using sensory-based interventions to increase self-regulation is gaining momentum with limited but promising evidence (Fraser et al., 2017; Lynch et al., 2021).
Patterned, repetitive sensory activities can be used to facilitate self-regulation by calming the neural system prior to teaching language-based skills or providing cognitive interventions (Fraser et al., 2017; Perry, 2009). Sensory input may be provided using these repetitive activities, e.g. games, or simply by the input itself which may include calming music, weighted blankets, large muscle activities, stretching, guided imagery, colored lights, blowing bubbles, deep breathing, and much more (Perry, 2009; Sutton et al., 2013). After participating in these activities and reaching a state of calm, incarcerated youth are better able to appropriately participate in treatment groups and are more likely to demonstrate the motivation and attention needed to learn from language-based interventions (Ford et al., 2012; Warner et al., 2014).
Sensory input delivered through calming activities like painting or creating music has been shown to be beneficial in helping young offenders recognize, accept, and manage emotions related to trauma (Woodward et al., 2019). Interventions that address self-regulation with a positive, activity-based lens are lacking in the treatment of juvenile offenders where largely cognitive behavioral therapy (CBT) approaches are used (Logan-Greene et al., 2017). While some cognitive-based approaches have led to improvements in the ability to identify emotions and self-regulate (Brazão et al., 2018), CBT may not be as effective for young offenders with extensive trauma histories (Kowalski, 2019). In addition to classic cognitive approaches, sensory-based activities that facilitate practice in emotional management, impulse control, goal setting, and self-efficacy can be used to address deficits associated with complex trauma and mental health challenges (Logan-Greene et al., 2017).
Evidence supports the use of trauma-informed approaches that utilize sensory-based interventions to improve skills in self-regulation and emotional intelligence (Fraser et al., 2017; Raider et al., 2008). One study showed that incarcerated individuals who participated in a creative arts program demonstrated significant improvements in body awareness and social competence, two building blocks of self-regulation (Koch et al., 2015). Juvenile offenders in a mindfulness training program indicated they were better able to identify and regulate emotions as well as control behaviors after participating in sessions that utilized meditation with education and activities (Himelstein et al., 2012; Barrett, 2017) found similar results from a program that used meditation and yoga to reduce stress and improve emotional regulation. These studies support the importance of supplementing cognitive-based treatment approaches with activity-based techniques that target the sensory system in a trauma-informed manner (Barrett, 2017; Fraser et al., 2017; Himelstein et al., 2012).
Potential for Occupational Therapy Intervention
Occupational therapy is a profession that uses therapeutic activities to build skills and facilitate participation in everyday life routines such as hygiene or sleep preparation, and life roles such as employee, student, and leisure participant (AOTA, 2020). Occupational therapists are well-trained to provide sensory-based, meaningful activities that are client-centered and can address the negative impact of trauma and self-regulation deficits on everyday participation (Alers, 2014). In trauma-informed care it is important to do this using a holistic and strengths-based approach that builds trust, rather than targeting an individual behavior that needs to be corrected, such as fighting (Duron et al., 2021; Ford et al., 2016). While trauma treatment is complex and should be provided using an interdisciplinary team approach (Lynch et al., 2021; McGreevy & Boland, 2020), a review of sensory-based approaches to trauma treatment found that only 6 of 16 articles mentioned occupational therapy as part of the team (Fraser et al., 2017). Occupational therapists have a vital role to play in the assessment of sensory patterns, impact of trauma on daily function, and implementation of interventions that include both meaningful activity and sensory input at levels that promote successful participation in life activities (Alers, 2014).
Specifically, occupational therapy is utilized in some psychiatric settings to address trauma with sensory-based interventions to decrease seclusion and restraint as well as improve overall engagement in everyday activities (Champagne, 2011a; Scanlan & Novak, 2015; Sutton et al., 2013; Warner et al., 2013). Treatment interventions may include use of sensory rooms for de-escalation (West et al., 2017), sensory-based activities such as soothing music and tactile mazes (Arnsten et al., 2015), and modifications to the environment to facilitate adaptive self-regulation skills (Sutton et al., 2013). Despite the large percentage of juvenile offenders challenged by mental health disorders and histories of trauma (Baglivio et al., 2014; Hayes & O’Reilly, 2013), these intervention strategies and providing skilled occupational therapy services to decrease maladaptive trauma responses and increase self-regulation in the criminal justice system are rare.
While still uncommon, most occupational therapy interventions provided in the justice system are for adults and focus on building transitional skills for re-entry into the community (Muñoz et al., 2016). However, recent literature documents the effectiveness of sensory-based occupational therapy treatment services for youth in the criminal justice system (Dowdy et al., 2020) found that sensory-based occupational therapy helped youth decrease violence in a correctional facility. Further, the study elicited youth voices who verbalized the importance of sensory activities in learning to calm and thinking more positively about their futures (Dowdy et al., 2020; Shea & Siu, 2016) explored the way occupational therapists used activities like bracelet making, drawing, puzzles, and games as a meaningful and appropriate way to teach youth in detention interpersonal skills, self-awareness, and life skills. Regardless of the skills taught or age-group addressed, occupational therapy shows promise in criminal justice settings in providing client-centered treatment that offers choices of activity which are motivating for and valued by participants (Crabtree et al., 2016; Dowdy et al., 2020; Tan et al., 2015).
Method
Design and Sample
A quasi-experimental retrospective design (Jackson, 2015) was used with a naturally occurring group of incarcerated youth who were selected due to their previous or current participation in occupational therapy. Lacking was a comparison control group. The participants were a purposeful sample (Bowling & Ebrahim, 2005) of incarcerated youth ages 12–20 years old at two Midwestern juvenile correctional facilities who had sensory-based occupational therapy intervention focusing on self-regulation. Inclusion criteria for the retrospective chart review portion of the study were youth who have been referred to occupational therapy (e.g., for social skills or self-regulation difficulties) by staff at Facility A and Facility B (see Table 1). Inclusion criteria for the survey portion of the study was restricted to male youth at Facility A who participated in occupational therapy and were at least 18 years old and thus did not require parental or guardian consent to participate.
Table 1.
Data collection facilities
| ACE Scores | Mental Health Diagnoses | Emotions Intervention Tool | Survey | |
|---|---|---|---|---|
| Facility A | Yes (n = 34) | Yes (n = 34) | Yes (n = 34) | Yes (n = 11*) |
| Facility B | No (n = 0) | No (n = 0) | Yes (n = 25) | No (n = 0) |
*Survey participants were at least 18 years old. All other data collection included participants ages 12–20
Instrumentation
Mental Health Diagnoses, ACE Scores, and the Emotions Intervention Tool
Data collection tools included documentation of mental health diagnoses, ACE scores, and the Emotions Intervention Tool. For the purposes of this study and according to the current Diagnostic and Statical Manual (DSM-V), a mental health disorder is classified as any clinically diagnosed dysfunction in cognition, emotion regulation, or behavior (American Psychiatric Association, 2013). An ACE score is defined as a measure of an individual’s total number of adverse childhood experiences based on a widely used 10-category questionnaire where exposure to a common adverse experience counts as one point, and these points are summed together for a highest possible score of 10 (Anda et al., 2009; Kowalski 2019). Higher scores indicate a higher prevalence of traumatic experiences’ categories or types, but the measurement does not account for the frequency or duration of exposure to each category of trauma (Kowalski, 2019). The ACE score questionnaire has been shown to have strong criterion validity (Meinck et al., 2017).
Clinicians at the two facilities developed the Emotions Intervention Tool, adapted with permission from Tina Champagne’s work (2011b), for use at the beginning and end of intervention sessions per normal clinical procedures independent of this study. The tool asked youth to answer a Likert scale (Joshi et al., 2015) question to rate from zero to ten how they felt pre- and post-session and to write a word describing how they felt pre- and post-session (see Fig. 1). Youth were also asked to identify the sensory-based activity they wanted to use during the session. Clinicians documented the type of intervention provided and if it was conducted in an individual or group setting. Intervention types included sensory-based intervention, meaningful activity, and mixed intervention. Sensory-based interventions focused on modulating one’s responses to external sensory stimuli through activities such as listening to music. Meaningful activity was an activity selected by youth from a set offered by the clinician. The set of activities were age-appropriate, pro-social, leisure activities valued by the individual, such as playing a board game. A mixed intervention combined a meaningful activity with an intentional sensory component such as listening to music while playing a board game during an occupational therapy session. Psychometric testing has not been conducted on the Emotions Intervention Tool.
Fig. 1.
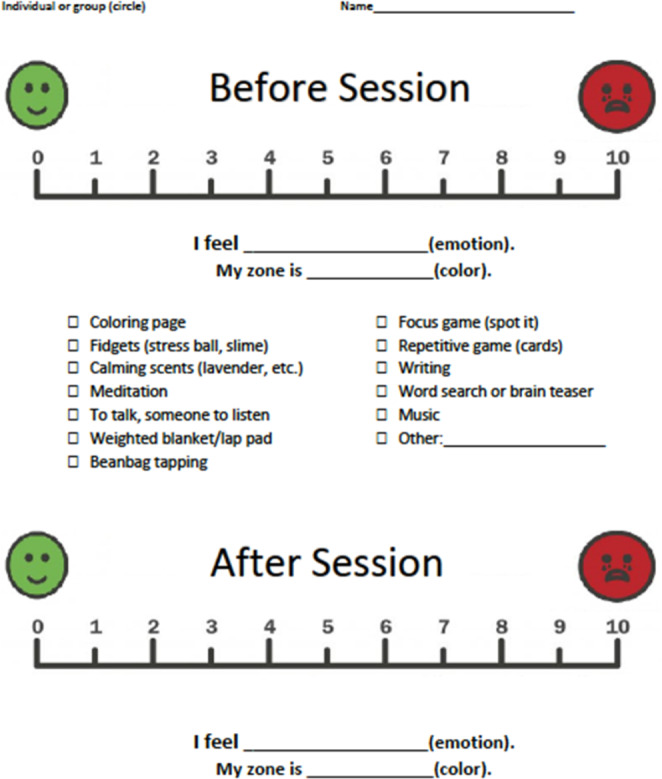
Pre- and post-session likert scale from emotions intervention tool
Survey
Student authors designed a written survey tailored to facilitate youth comprehension of questions asked. The survey consisted of 24 questions using four question formats. Half (i.e., 12) of the questions were open-ended and asked youth to describe experiences related to feeling states (e.g., sad, angry, feelings pre- and post-occupational therapy); ability to and experiences related to controlling emotions; and their perceptions about participating in occupational therapy (e.g., favorite activities, how occupational therapy helped them, and how they could use skills learned in occupational therapy at home).
The survey also included six Likert type (Joshi et al., 2015) scale questions asking for level of agreement to statements about the impact of participating in occupational therapy. Three response options were provided, i.e., strongly agree, somewhat agree, and disagree. A picture of a thumb emoji representing the written level of agreement was placed under each option to facilitate comprehension. Five additional Likert type (Joshi et al., 2015) scale questions asked youth for their level of agreement to statements about emotions identification. Question topics asked about typical emotional states, how well they can name their emotions, how well they can control their emotions, and their emotional states pre- and post-occupational therapy participation. The five response options ranged from ‘Bad’ to ‘Great’ with each of the five anchor points represented by a correlating facial expression emoji picture. Finally, one question asked youth to circle activities they participated in during occupational therapy from a list of 14 options. This question was followed by an open-ended question asking them to identify their two favorite activities.
Procedures
Record Review
Study procedures were approved by the host institution’s Institutional Review Board (IRB) for the protection of human subjects and participating facilities. Data were collected using a retrospective chart review and a survey at one or both facilities. An occupational therapist, also a member of the research team, completed a record review at Facility A (see Table 1) to attain youth ACE scores and mental health diagnoses, both of which were not accessible to researchers from Facility B. From the Fall of 2019 until the Fall of 2020, clinician members of the research team at both facilities kept records of the Emotions Intervention Tool sheets for clinical and documentation purposes. The clinicians recorded youth scores and intervention types from individual Emotions Intervention Tool sheets and converted the information into anonymous data points onto a study-specific Data Collection Spreadsheet as part of the retrospective data review process. There was no master code sheet linking participant identities to the data. Clinicians met quarterly to control for treatment fidelity (Krefting, 1991) across facilities by verifying consistency in identifying intervention types.
Survey
During the Fall of 2020, the first author read a recruitment script over Zoom Video Communications, Inc. (Zoom) inviting youth at Facility A (see Table 1) who were 18–20 years old and had or were participating in occupational therapy to complete a paper survey. Zoom meetings were utilized instead of face-to-face interviews due to facility COVID-19 restrictions prohibiting visitors. Youth who agreed to participate completed the survey during the recruitment Zoom meeting. A behavioral health staff member distributed the survey to the youth in a private room in the facility and then waited outside the door until the youth completed the survey. Via Zoom, the first author read the survey instructions and maintained presence to answer questions the youth might have. The youth were instructed to not provide any self-identifying information on the survey. The behavioral health staff member collected the survey from the youth to ensure confidentiality of their responses. To enhance credibility and dependability, the authors used triangulation of data sources through a sample of 11 surveys, a team of investigators, and expert review from the first and second authors (Krefting, 1991).
Analysis
ACE scores and frequencies of mental health diagnoses were analyzed using descriptive statistics to produce frequency counts. The Emotions Intervention Tool pre- and post-occupational therapy Likert scale (Joshi et al., 2015) question responses were analyzed using Statistical Package for the Social Sciences (SPSS®) to conduct a paired samples t-test, with alpha significance level pre-set at 0.05. Likert type (Joshi et al., 2015) question responses were analyzed to produce frequency counts. Usable open-ended question responses were grouped by similarities into categories and frequency of responses in each category was reported.
Results
Sample Size, Mental Health Diagnoses, and ACE Scores
Participant demographics were not collected to protect youth privacy. General demographics at Facility A as provided by Ohio Department of Youth Services (2019) include an average age of 18.1 years, 65% receiving services for mental health diagnoses, 53% black, 35% white, and 12% other. Mental health diagnoses and ACE scores were collected through record review for 34 male youth ages 12–20 who had received occupational therapy services at Facility A. The most prevalent mental health diagnoses were Cannabis Use Disorder (moderate to severe; 79.41%), attention deficit hyperactivity disorder (ADHD; 50%), Conduct Disorder (unspecified, childhood, or adolescent onset; 35.29%), Post-Traumatic Stress Disorder (PTSD; 23.53%), and Alcohol Use Disorder (moderate to severe; 23.53%). Among the youth who participated in the study, 88% had at least three mental health diagnoses (see Fig. 2). The frequencies of participants’ mental health diagnoses are presented in Table 2. The average ACE score among youth who received occupational therapy services was 5.91 (SD = 1.91).
Fig. 2.
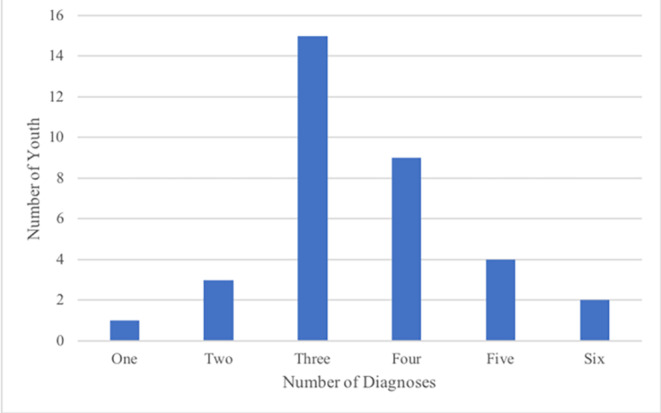
Distribution of mental health diagnoses per youth (N = 34)
Table 2.
Frequencies of youth mental health diagnoses (N = 106)
| Mental Health Diagnosis | n |
|---|---|
|
Cannabis Use Disorder (Moderate to Severe) ADHD (Combined Presentation) Conduct Disorder (Unspecified, Childhood, or Adolescent) PTSD Alcohol Use Disorder (Moderate to Severe) Antisocial Personality Disorder Disruptive Mood Regulation Disorder Opioid Use (Moderate to Severe) Depressive Disorder (Unspecified or Persistent) |
27 17 12 8 8 6 4 4 4 |
Note: Conditions with frequencies of 1, 2, or 3 included but were not limited to mood disorders, personality disorders, and depressive disorders. The ‘n’ total exceeded the number of participants as each had a range of 1 to 6 mental health diagnoses as depicted in Fig. 2
Emotions Intervention Tool Likert Scale
Data points were collected from 59 youth ages 12–20 and produced 413 Emotions Intervention Tool sheets, each representing data from an individual occupational therapy session at Facilities A and B. Of the youth, 32.3% participated in sensory-based intervention, 25.0% participated in meaningful activity, and 42.7% participated in mixed intervention over a one-year period (Fall 2019 – Fall 2020). For youth who participated in a sensory-based intervention, the most chosen activities included music, fidgets, putty, slime, or talking. For youth that participated in a meaningful activity intervention, the most chosen activities were crafts, discussing zones of regulation, playing games to better understand the zones of regulation, or playing a meme emotion game to increase awareness of emotions. For the youth who participated in a mixed intervention, the most chosen activities included music or scented lotion paired with talking, stress ball or fidget making, a focus game, or a craft.
On a scale of zero to ten, with zero anchored by a smiley face and ten anchored by a sad face, the average pre-session emotion number was 3.01 (SD = 2.50) and the average post-session emotion number was 1.45 (SD = 1.62). Out of 413 data points, 245 (59.3%) showed a decrease between pre-session and post-session emotion numbers. Data were filtered to remove data points that did not show a change because of the potential to artificially bias the t-test result. Among the filtered data set of 254 data points, the average pre-session emotion number was 4.31 (SD = 2.10) and the average post-session emotion number was 1.77 (SD = 1.62).
The difference between pre-session emotion and post-session emotion number was statistically significant in both the complete data set (from M = 3.01 to M = 1.45; t(412) = 17.05, p = .000) and the filtered data set (from M = 4.31 to M = 1.77; t(253) = 22.79, p = .000). The highest frequencies of emotion words stated pre-session were calm (n = 78), happy (n = 41), chill (n = 33), irritated (n = 25), and tired (n = 23). Additional words stated with less frequency included good, frustrated, angry, agitated, and aggravated. The highest frequencies of emotion words stated post-session were calm (n = 132), happy (n = 69), chill (n = 45), good (n = 35), and tired (n = 17). Additional words stated with less frequency included ok, relaxed, cool, excited, less stressed, and optimistic.
Survey
Eleven youth aged 18–20 at Facility A participated in the survey. To ascertain emotional vocabulary when asked about their most frequent emotions, youth who completed the survey chose chill (n = 6), annoyed (n = 5), focused (n = 4), tired (n = 4), frustrated (n = 4), out of control (n = 2), and lonely (n = 2) as their most experienced emotions. The most frequently reported activities youth participated in during occupational therapy included listening to music, talking to someone, coloring pages, playing repetitive games, and doing arts and crafts.
Open-Ended Question Responses
For questions asking about perceptions on the impact of their participation in occupational therapy, several youth mentioned that it taught them coping strategies, life skills, and how to talk about their emotions before acting. One youth stated, “I learned to talk about my anger and emotions instead of letting it all build up.” Another youth stated, “when I felt like hurting someone real bad but I remembered my coping methods from my sessions.” Without strategies to control their emotions, youth stated, “my feelings overpower my actions and judgment.” Multiple youth reported meditating, talking to staff, taking deep breaths, and expressing themselves creatively as methods that help control their emotions. Participating in activities during occupational therapy sessions helped youth to “focus on something positive,” “forget about my frustrations,” and “calm down.” After participating in occupational therapy, youth felt “focused” and motivated about their future. All (100%) of the 10 respondents who answered all 10 questions reported they have used something they learned in occupational therapy. This was further supported by short answer responses, as one participant stated, “I learned a lot in OT that I can use in many different situations at home.”
Likert Type Survey Questions
For questions about the impact of participating in occupational therapy, more than half of survey participants indicated that occupational therapy helped them “a lot” to recognize their emotions. All of survey participants indicated that occupational therapy helped youth to change their behaviors and control their emotions. Further results from Likert type questions about the impact of participating in occupational therapy are summarized in Table 3. For questions about emotion identification, youth responded typically feeling “bad /not very good” prior to an occupational therapy session and reported feeling “really good/great” at the end of the session. Further results from Likert type emotion identification questions are summarized in Table 4.
Table 3.
Impact of occupational therapy (N = 10)
| N | No | Yes, a little | Yes, a lot | |
|---|---|---|---|---|
| “How often do you use what you have learned in occupational therapy?” | 10 | 0 | 5 | 5 |
| “Has occupational therapy helped you to change your behaviors?” | 10 | 0 | 6 | 4 |
| “Has occupational therapy helped you control your emotions?” | 9* | 0 | 5 | 4 |
| “Has occupational therapy helped you to name or recognize your emotions?” | 10 | 1 | 3 | 6 |
*Not all 10 participants answered every question
Table 4.
Emotion identification (N = 11)
| Questions | Bad/Not very good | Okay | Really good/Great |
|---|---|---|---|
| “How well can you name your emotions?” | 1 | 4 | 6 |
| “How well can you control your emotions?” | 3 | 2 | 6 |
| “How do you typically feel before an occupational therapy session or group?” | 4 | 6 | 1 |
| “How do you typically feel at the end of an occupational therapy session or group?”* | 0 | 3 | 7 |
Note: Responses to Likert type scale questions were as follows: 1 = Bad, 2 = Not very good, 3 = Okay, 4 = Really good, 5 = Great
*Out of 10 respondents
Discussion
The aim of this study was to explore the impact of sensory-based occupational therapy implemented at two Midwestern juvenile correctional facilities. Specifically, this study showed incarcerated youth to have higher than average ACE scores and/or number of mental health diagnoses, an ability to identify a positive change in emotions following occupational therapy interventions designed to promote self-regulation, limited emotional vocabulary, and overall positive perceptions of the impact of participating in sensory-based occupational therapy.
Contributing Personal Factors: ACE Scores and Mental Health Diagnoses
The high average ACE score of study participants (5.9) is consistent with research showing that traumatic experiences are more prevalent in justice-involved youth as compared to the general population (Baglivio et al., 2014). These findings agree with other research which indicates that early childhood trauma experiences can cause neurological changes and functional impairments, resulting in maladaptive behaviors such as aggression and risk-taking (Lewis et al., 2019; Nelson et al., 2020) seen in juvenile offenders.
Youth presenting with multiple mental health diagnoses is not surprising given that early experiences of trauma are associated with incurring mental health diagnoses throughout life as well as higher rates of smoking, alcohol use, and cannabis use in adolescence (Afifi et al., 2020; Nelson et al., 2020). A disproportionate number of youth within the juvenile facility have at least one mental health diagnosis (Ohio Department of Youth Services, 2019) as compared to 16.5% of youth ages 0–17 in the general United States population (Whitney & Peterson, 2019). Higher rates of trauma experiences and mental health diagnoses among incarcerated youth points to the need to address the impact of these factors on their daily functioning.
Emotions Intervention Tool Data: Emotion Numbers and Emotion Words
Recognizing, labeling, and regulating one’s emotions can be difficult for individuals with trauma histories (Champagne, 2011a; Chen et al., 2017) or mental health concerns (Logan-Greene et al., 2017). This study utilized a numerical approach with the Emotions Intervention Tool Likert scale to aid youth to recognize a change in emotion. Youth in this study identified a numerical change in emotional state following occupational therapy sessions. This change between pre- and post-session emotion numbers was statistically significant, as 61.5% of youth showed a positive change following a sensory-based occupational therapy session. This is not surprising as past research showed the effectiveness of sensory-based interventions using non-invasive and self-directed methods to facilitate participation by helping youth who have mental health concerns manage their emotions in times of distress (Scanlan & Novak, 2015).
The study’s findings showed youth used the same four words (i.e., calm, happy, chill, and tired) most frequently to label both their pre- and post-occupational therapy session emotional states. Aside from the four most frequently stated emotion words, the wide variety of the remaining pre-session words contained a higher frequency of negative words (i.e., irritated, frustrated, mad) as compared to the remaining post-session words that contained a higher frequency of positive words (i.e., relaxed, cool, excited). Based on both the Emotions Intervention Tool Likert scale results and the emotion word results, youth participating in occupational therapy sessions identified a change in emotional state on the Likert scale but were inconsistently able to associate the change with a change in emotion word.
The Emotions Intervention Tool Likert scale seemed to help youth identify their own emotional states. Research suggests that youth with experiences of childhood trauma have difficulty understanding and effectively using language to label their emotional experience (Velotti et al., 2017; Warner et al., 2013). Individuals lacking the ability to recognize and label emotions cannot appropriately respond to their emotions and regulate their behavior accordingly (Roberton et al., 2014), such as when communicating with others during emotionally charged situations or managing conflict. This emphasizes the importance of providing youth with emotion identification and regulation strategies within a safe and predictable environment. The Emotions Intervention Tool Likert scale was more sensitive to detecting change in youths’ emotional state than asking them to independently identify an emotion word. Based on this study’s results, using a combination of visual tools and Likert scales could help youth understand the association between a change in emotional state and the paired emotion word label to describe the emotional state.
Youth Perceptions of Occupational Therapy
Generally, the literature lacks representation of incarcerated youth voices. In this study, youth voices support the effects of sensory-based occupational therapy in enhancing their ability to identify their emotions and implement self-regulation strategies. Specifically, youth in this study recognized that therapy was calming and beneficial for their future. Consistent with past research (Dowdy et al., 2020; Tan et al., 2015), participating in occupational therapy provided youth with an opportunity to express feelings and develop tangible ways to process their emotions in a predictable environment.
A Need for Occupational Therapy
Youth perceptions of occupational therapy in conjunction with Emotions Intervention Tool outcome data support occupational therapy’s value in providing meaningful engagement in a correctional facility. Youth in juvenile facilities have similar diagnoses as youth in psychiatric facilities (Hayes & O’Reilly, 2013) yet those in psychiatric facilities are more likely to receive occupational therapy as part of interdisciplinary team services. Youth in this study had diagnoses of substance use disorder, ADHD, PTSD, conduct disorder, and antisocial personality disorder, like diagnoses of youth in a psychiatric clinic which provided services to all the above diagnoses except antisocial personality disorder (Hayes & O’Reilly, 2013). Most youth incarcerated in juvenile facilities do not have occupational therapy as an available service. The lack of trauma-informed treatment within juvenile facilities (Fraser, 2017) leaves youth without mechanisms to regulate responses to effectively deal with changing emotional states and participate in daily activities. Occupational therapists can fill this gap as they consider person factors (AOTA, 2020) such as trauma history and mental health diagnoses when using sensory-based treatment and active participation in meaningful activities to treat self-regulation deficits (Dowdy et al., 2020; Lynch et al., 2021).
Occupational therapists use a trauma-informed lens when providing sensory-based interventions involving music, talking to someone, repetitive games, and arts and crafts, which address the neurological impact of trauma through targeting innervating neural sensory systems (Perry, 2009). Like evidence of sensory input regulating sensory arousal and creating behavioral changes (Sutton et al., 2013; Watling & Hauer, 2015), youth in this study reported a calmer body state after occupational therapy. Data showed that youth themselves acknowledged the importance of learning coping strategies and recognizing behavioral triggers to improve daily functioning with mental health diagnoses and histories of trauma. Occupational therapists are well-equipped to address self-regulation and the impact of trauma on functioning through adapting activities and providing strategies for emotion identification.
Limitations & Strengths
The survey data was limited to participants who were at least 18 years old due to the difficulty of obtaining parental consent for youth who were minors. Survey participants may have been relatively more mature because of their age and the amount of time spent in the facility, which makes this study less generalizable to a younger age group. The findings of the study may not be transferable to other correctional facilities due to the unique environment and services provided at each facility as well as the lack of information collected about frequency and duration of treatment. Another limitation of the study included a lack of a control group due to unethical implications of withholding treatment from youth. Finally, the COVID-19 pandemic limited in-person treatment and thus the number of data points collected.
Future studies might investigate a specific protocol for frequency and duration of sensory-based occupational therapy in residential settings. Additionally, the context of the facility might be examined to explore the impact of a trauma-informed environment and the potential role of occupational therapists training other staff members in trauma-informed care practices.
Strengths of the study included triangulation of data collection through survey and the Emotions Intervention Tool. The sample size for the Emotions Intervention Tool data was relatively large. The research was conducted by a team consisting of student researchers and a clinical tutor and faculty tutor, who provided expert review to the students. Finally, the study provided youth with a unique opportunity to have their voices heard as they expressed their perceptions of occupational therapy.
Practice Implications
The results of this study highlight the importance of addressing the neurological impact of trauma and mental health challenges on the daily functioning of youth within juvenile justice facilities. Sensory-based interventions provided by occupational therapists have been shown to be effective in treating individuals with experiences of trauma (Lynch et al., 2021; McGreevy & Boland, 2020). Occupational therapy can help youth develop self-regulation skills, such as emotion identification, and adjust arousal levels to be able to better cope within a stressful environment. When utilizing these skills, youth may be able to self-regulate and safely return from a heightened state of arousal to be able to interact with peers more appropriately as well as attend to classroom tasks with greater attention, focus, and impulse control. The results of this study point to the effectiveness of sensory-based interventions that are client-centered and tailored to the arousal level and cognitive ability of the youth in the juvenile justice setting. Occupational therapists that have training in trauma-informed care can apply their professional assessment, recommendation, and consultation skills to be valuable assets amongst an interdisciplinary mental health team. The presence of occupational therapy staff as members of interdisciplinary mental health teams needs to be expanded which requires funding support from correctional institutions.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Afifi, T. O., Taillieu, T., Salmon, S., Davila, I. G., Stewart-Tufescu, A., Fortier, J., Struck, S., Asmundson, G. J. G., Sareen, J., & MacMillan, H. L. (2020). Adverse childhood experiences (ACEs), peer victimization, and substance use among adolescents. Child Abuse & Neglect, 106. 10.1016/j.chiabu.2020.104504 [DOI] [PubMed]
- Alers, V. (2014). Trauma and its effects on children, adolescents and adults: The role of the occupational therapist. In R. Crouch & V. Alers (Eds.), Occupational Therapy in Psychiatry and Mental Health (5th ed., pp. 337–355). Wiley. 10.1002/9781118913536.ch21
- American Occupational Therapy Association (AOTA) (2020). Occupational therapy practice framework: Domain and process (4th ed.). American Journal of Occupational Therapy, 74 (Supplement 2). 10.5014/ajot.2020.74S2001
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596
- Anda RF, Dong M, Brown DW, Felitti VJ, Giles WH, Perry GS, Valerie EJ, Dube SR. The relationship of adverse childhood experiences to a history of premature death of family members. Bmc Public Health. 2009;16(9):106. doi: 10.1186/1471-2458-9-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardizzi, M., Umiltà, M. A., Evangelista, V., Di Liscia, A., Ravera, R., & Gallese, V. (2016). Less empathic and more reactive: The different impact of childhood maltreatment on facial mimicry and vagal regulation. Plos One, 11(9), 10.1371/journal.pone.0163853 [DOI] [PMC free article] [PubMed]
- Arnsten A, Raskind M, Taylor F, Connor D. The effects of stress exposure on prefrontal cortex: Translating basic research into successful treatment for post-traumatic stress disorder. Neurobiology of Stress. 2015;1:89–99. doi: 10.1016/j.ynstr.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baglivio M, Swartz K, Huq M, Sheer A, Hardt N. The prevalence of adverse childhood experiences in the lives of juvenile offenders. Journal of Juvenile Justice. 2014;3(2):12–34. doi: 10.1177/1541204014566286. [DOI] [Google Scholar]
- Barrett CJ. Mindfulness and rehabilitation: Teaching yoga and meditation to young men in an alternative to incarceration program. International Journal of Offender Therapy and Comparative Criminology. 2017;61(15):1719–1738. doi: 10.1177/0306624X16633667. [DOI] [PubMed] [Google Scholar]
- Bowling, A., & Ebrahim, S. (2005). Handbook of health research methods: Investigation, measurement and analysis. Open University Press
- Brazão N, Rijo D, Salvador MC, Pinto-Gouveia J. Promoting emotion and behavior regulation in male prison inmates: A secondary data analysis from a randomized controlled trial testing the efficacy of the growing pro-social program. Law and Human Behavior. 2018;42(1):57–70. doi: 10.1037/lhb0000267. [DOI] [PubMed] [Google Scholar]
- Champagne T. The influence of posttraumatic stress disorder, depression, and sensory processing patterns on occupational engagement: A case study. Work (Reading, Mass.) 2011;38(1):67–75. doi: 10.3233/WOR-2011-1105. [DOI] [PubMed] [Google Scholar]
- Champagne, T. (2011b). Sensory modulation & environment: Essential elements of occupation, (3rd Ed Rev). Pearson
- Chen L, Xu L, You W, Zhang X, Ling N. Prevalence and associated factors of alexithymia among adult prisoners in China: A cross-sectional study. Bmc Psychiatry. 2017;17:1–13. doi: 10.1186/s12888-017-1443-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crabtree JL, Ohm D, Wall JM, Ray J. Evaluation of a prison occupational therapy informal education program: A pilot study. Occupational Therapy International. 2016;23(4):401–411. doi: 10.1002/oti.1442. [DOI] [PubMed] [Google Scholar]
- Cutuli JJ, Alderfer MA, Marsac ML. Introduction to the special issue: Trauma-informed care for children and families. Psychological Services. 2019;16(1):1–6. doi: 10.1037/ser0000330. [DOI] [PubMed] [Google Scholar]
- Dowdy, R., Estes, J., Linkugel, M., & Dvornak, M. (2020). Trauma, sensory processing, and the impact of occupational therapy on youth behavior in juvenile corrections. Occupational Therapy in Mental Health, 1–21. 10.1080/0164212X.2020.1823930
- Duron J, Williams-Butler A, Liu FY, Nesi D, Pirozzolo Fay K, Kim BK. The influence of adverse childhood experiences (ACEs) on the functional impairment of justice-involved adolescents: A comparison of baseline to follow-up reports of adversity. Youth Violence and Juvenile Justice. 2021;19(4):384–401. doi: 10.1177/15412040211016035. [DOI] [Google Scholar]
- Engel-Yeger B, Palgy-Levin D, Lev-Wiesel R. The sensory profile of people with post-traumatic stress symptoms. Occupational Therapy in Mental Health. 2013;29(3):266–278. doi: 10.1080/0164212X.2013.819466. [DOI] [Google Scholar]
- Evans GW, Kim P. Childhood poverty, chronic stress, self-regulation, and coping. Child Development Perspectives. 2013;7(1):43–48. doi: 10.1111/cdep.12013. [DOI] [Google Scholar]
- Evans-Chase M. Addressing trauma and psychosocial development in juvenile justice-involved youth: A synthesis of the developmental neuroscience, juvenile justice and trauma literature. Laws. 2014;3:744–758. doi: 10.3390/laws3040744. [DOI] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Ford, J. D., Chapman, J., Connor, D. F., & Cruise, K. R. (2012). Complex trauma and aggression in secure juvenile justice settings. Journal of Criminal Justice and Behavior, 39(6), 694–72410.1177/0093854812436957
- Fox B, Perez N, Cass E, Baglivio M, Epps N. Trauma changes everything: Examining the relationship between adverse childhood experiences and serious, violent, and chronic juvenile offenders. Child Abuse & Neglect. 2015;46:163–173. doi: 10.1016/j.chiabu.2015.01.011. [DOI] [PubMed] [Google Scholar]
- Fraser K, MacKenzie D, Versnel J. Complex trauma in children and youth: A scoping review of sensory-based interventions. Occupational Therapy in Mental Health. 2017;33(3):199–216. doi: 10.1080/0164212X.2016.1265475. [DOI] [Google Scholar]
- Hart H, Rubia K. Neuroimaging of child abuse: A critical review. Frontiers in Human Neuroscience. 2012;6(52):1–24. doi: 10.3389/fnhum.2012.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes JM, O’Reilly G. Psychiatric disorder, IQ, and emotional intelligence among adolescent detainees: A comparative study. Legal and Criminological Psychology. 2013;18(1):30–47. doi: 10.1111/j.2044-8333.2011.02027.x. [DOI] [Google Scholar]
- Himelstein S, Hastings A, Shapiro S, Heery M. A qualitative investigation of the experience of a mindfulness-based intervention with incarcerated adolescents. Child and Adolescent Mental Health. 2012;17(4):231–237. doi: 10.1111/j.1475-3588.2011.00647.x. [DOI] [PubMed] [Google Scholar]
- Hodgdon HB, Kinniburgh K, Gabowitz D, Blaustein M, Spinazzola J. Development and implementation of trauma-informed programming in youth residential treatment centers using the ARC framework. Journal of Family Violence. 2013;28(7):679. doi: 10.1007/s10896-013-9531-z. [DOI] [Google Scholar]
- Jackson, S. L. (2015). Research methods and statistics: A critical thinking approach (5th ed.). Cengage Learning
- Joshi A, Kale S, Chandel S, Pal DK. Likert scale: Explored and explained. British Journal of Applied Science and Technology. 2015;7(4):396–403. doi: 10.9734/BJAST/2015/14975. [DOI] [Google Scholar]
- Koch, S., Ostermann, T., Steinhage, A., Kende, P., Haller, K., & Chyle, F. (2015). Breaking
- barriers: Evaluating an arts-based emotion regulation training in prison.The Arts in Psychotherapy, 42,41–49. 10.1016/j.aip.2014.10.008
- Kowalski MA. Adverse childhood experiences and justice-involved youth: The effect of trauma and programming on different recidivistic outcomes. Youth Violence and Juvenile Justice. 2019;17(4):354–384. doi: 10.1177/1541204018809836. [DOI] [Google Scholar]
- Krefting L. Rigor in qualitative research: The assessment of trustworthiness. American Journal of Occupational Therapy. 1991;45(2):214–222. doi: 10.5014/ajot.45.3.214. [DOI] [PubMed] [Google Scholar]
- Langer R, Leiberg S, Hoffstaedter F, Eickhoff SB. Towards a human self-regulation system: Common and distinct neural signatures of emotional and behavioural control. Neuroscience and Behavioral Reviews. 2018;90:400–410. doi: 10.1016/j.neubiorev.2018.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis SJ, Arseneault L, Caspi A, Fisher HL, Matthews T, Moffitt TE, Odgers CL, Stahl D, Teng JY, Danese A. The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. Lancet Psychiatry. 2019;6(3):247–256. doi: 10.1016/s2215-0366(19)300318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan-Greene P, Tennyson RL, Nurius PS, Borja S. Adverse childhood experiences, coping resources, and mental health problems among court-involved youth. Child & Youth Care Forum. 2017;46(6):923–946. doi: 10.1007/s10566-017-9413-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch, B. P., Brokamp, K. M., Scheerer, C. R., Bishop, M., Stauble, L., Hagedorn, B., & Endres, L. (2021). Outcomes of occupational therapy in trauma-informed care. Journal of Occupational Therapy, Schools, & Early Intervention10.1080/19411243.2021.2003733
- McGreevy S, Boland P. Sensory-based interventions with adult and adolescent trauma survivors: An integrative review of the occupational therapy literature. Irish Journal of Occupational Therapy. 2020;48(1):31–54. doi: 10.1108/IJOT-10-2019-0014. [DOI] [Google Scholar]
- Meinck F, Cosma AP, Mikton C, Baban A. Psychometric properties of the Adverse Childhood Experiences Abuse Short Form (ACE-ASF) among Romanian high school students. Child Abuse & Neglect. 2017;72:326–337. doi: 10.1016/j.chiabu.2017.08.016. [DOI] [PubMed] [Google Scholar]
- Mirolli M, Mannella F, Baldassarre G. The roles of the amygdala in the affective regulation of body, brain, and behaviour. Connection Science. 2010;22(3):215–245. doi: 10.1080/09540091003682553. [DOI] [Google Scholar]
- Muñoz JP, Farnworth L, Dieleman C. Harnessing the power of occupation to meet the needs of people in criminal justice settings. Occupational Therapy International. 2016;23(3):221–228. doi: 10.1002/oti.1439. [DOI] [PubMed] [Google Scholar]
- Nelson, C. A., Scott, R. D., Bhutta, Z. A., Harris, N. B., Danese, A., & Samara, M. (2020). Adversity in childhood is linked to mental and physical health throughout life. British Medical Journal, 371. 10.1136/bmj.m3048 [DOI] [PMC free article] [PubMed]
- Ohio Department of Youth Services (2019). Ohio department of youth services: December 2019 monthly factsheet [PDF File]. https://www.dys.ohio.gov/static/About+DYS/Communications/Reports/Monthly+Fact+Sheets/Mfs_201912.pdf
- Perez N, Jennings W, Baglivio M. A path to serious, violent chronic delinquency: The harmful aftermath of adverse childhood experiences. Crime & Delinquency. 2016;64(1):3–25. doi: 10.1177/0011128716684806. [DOI] [Google Scholar]
- Perry BD. Examining child maltreatment through a neurodevelopmental lens: Clinical applications of the neurosequential model of therapeutics. Journal of Loss and Trauma. 2009;14(4):240–255. doi: 10.1080/15325020903004350. [DOI] [Google Scholar]
- Perry NB, Calkins SD, Dollar JM, Keane SP, Shanahan L. Self-regulation as a predictor of patterns of change in externalizing behaviors from infancy to adolescence. Development and Psychopathology. 2018;30(2):497–510. doi: 10.1017/S0954579417000992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pihet S, Combremont M, Suter M, Stephan P. Cognitive and emotional deficits associated with minor and serious delinquency in high-risk adolescents. Psychiatry Psychology & Law. 2012;19(3):427–438. doi: 10.1080/13218719.2011.598634. [DOI] [Google Scholar]
- Raider, M. C., Steele, W., Delillo-Storey, M., Jacobs, J., & Kuban, C. (2008). Structured Sensory
- Therapy (SITCAP-ART) for traumatized adjudicated adolescents in residential treatment.Residential Treatment for Children & Youth, 25,167–185. 10.1080/08865710802310178
- Reeves A. Emotional intelligence: Recognizing and regulating emotions. Workplace Health & Safety Journal. 2005;53(4):172–176. [PubMed] [Google Scholar]
- Roach CB. Shallow affect, no remorse: The shadow of trauma in the inner city. Peace and Conflict: Journal of Peace Psychology. 2013;19(2):150–163. doi: 10.1037/a0032530. [DOI] [Google Scholar]
- Roberton T, Daffern M, Bucks RS. Maladaptive emotion regulation and aggression in adult offenders. Psychology Crime & Law. 2014;20(10):933–954. doi: 10.1080/1068316X.2014.893333. [DOI] [Google Scholar]
- Scanlan JN, Novak T. Sensory approaches in mental health: A scoping review. Australian Occupational Therapy Journal. 2015;62(5):277–285. doi: 10.1111/1440-1630.12224. [DOI] [PubMed] [Google Scholar]
- Sharma N, Prakash O, Sengar KS, Chaudhury S, Singh AR. The relationbetween emotional intelligence and criminal behavior: A study among convicted criminals. Industrial Psychiatry Journal. 2015;24(1):54–58. doi: 10.4103/0972-6748.160934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea CK, Siu AMH. Engagement in play activities as a means for youth in detention to acquire life skills. Occupational Therapy International. 2016;23(3):276–286. doi: 10.1002/oti.1432. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. American Journal of Pediatrics. 2012;129(1):232–246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Sutton D, Wilson M, Van Kessel K, Vanderpyl J. Optimizing arousal to manage aggression: A pilot study of sensory modulation. International Journal of Mental Health Nursing. 2013;22(6):500–511. doi: 10.1111/inm.12010. [DOI] [PubMed] [Google Scholar]
- Tan BL, Kumar VR, Devaraj P. Development of a new occupational therapy service in a Singapore prison. British Journal of Occupational Therapy. 2015;78(8):525–529. doi: 10.1177/0308022615571083. [DOI] [Google Scholar]
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neuroscience & Biobehavioral Reviews. 2003;27(1–2):33–44. doi: 10.1016/s0149-7634(03)00007. [DOI] [PubMed] [Google Scholar]
- Thomason ME, Marusak HA. Toward understanding the impact of trauma on the early developing human brain. Neuroscience. 2017;342:55–67. doi: 10.1016/j.neuroscience.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velotti P, Garofalo C, Callea A, Bucks RS, Roberton T, Daffern M. Exploring anger among offenders: The role of emotion dysregulation and alexithymia. Psychiatry Psychology and Law. 2017;24(1):128–138. doi: 10.1080/13218719.2016.1164639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner E, Koomar J, Lary B, Cook A. Can the body change the score? Application of sensory modulation principles in the treatment of traumatized adolescents in residential settings. Journal of Family Violence. 2013;28(7):729–738. doi: 10.1007/s10896-013-9535-8. [DOI] [Google Scholar]
- Warner E, Spinazzola J, Westcott A, Gunn C, Hodgdon H. The body can change the score: Empirical support for somatic regulation in the treatment of traumatized adolescents. Journal of Child & Adolescent Trauma. 2014;7(4):237–246. doi: 10.1007/s40653-014-0030-z. [DOI] [Google Scholar]
- Watling R, Hauer S. Effectiveness of Ayres Sensory Integration® and sensory-based interventions for people with autism spectrum disorder: A systematic review. The American Journal of Occupational Therapy. 2015;69(5):1–12. doi: 10.5014/ajot.2015.018051. [DOI] [PubMed] [Google Scholar]
- West M, Melvin G, McNamara F, Gordon M. An evaluation of the use and efficacy of a sensory room within an adolescent psychiatric inpatient unit. Australian Occupational Therapy Journal. 2017;64(3):253–263. doi: 10.1111/1440-1630.12358. [DOI] [PubMed] [Google Scholar]
- Whitney DG, Peterson MD. US national and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatrics. 2019;173(4):389–391. doi: 10.1001/jamapediatrics.2018.5399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward, E. C., Viana, A. G., Trent, E. S., Raines, E. M., Zvolensky, M. J., & Storch, E. A. (2019). Emotional nonacceptance, distraction coping and PTSD symptoms in a trauma- exposed adolescent inpatient sample. Cognitive Therapy and Research, 1–8. 10.1007/s10608-019-10065-4


