Abstract
Background
Brain 18F-FDG PET imaging has the potential to provide an objective assessment of brain involvement in post-COVID-19 conditions but previous studies of heterogeneous patient series yield inconsistent results. The current study aimed to investigate brain 18F-FDG PET findings in a homogeneous series of outpatients with post-COVID-19 conditions and to identify associations with clinical patient characteristics.
Methods
We retrospectively included 28 consecutive outpatients who presented with post-COVID-19 conditions between September 2020 and May 2022 and who satisfied the WHO definition, and had a brain 18F-FDG PET for suspected brain involvement but had not been hospitalized for COVID-19. A voxel-based group comparison with 28 age- and sex-matched healthy controls was performed (p-voxel at 0.005 uncorrected, p-cluster at 0.05 FWE corrected) and identified clusters were correlated with clinical characteristics.
Results
Outpatients with post-COVID-19 conditions exhibited diffuse hypometabolism predominantly involving right frontal and temporal lobes including the orbito-frontal cortex and internal temporal areas. Metabolism in these clusters was inversely correlated with the number of symptoms during the initial infection (r = − 0.44, p = 0.02) and with the duration of symptoms (r = − 0.39, p = 0.04). Asthenia and cardiovascular, digestive, and neurological disorders during the acute phase and asthenia and language disorders during the chronic phase (p ≤ 0.04) were associated with these hypometabolic clusters.
Conclusion
Outpatients with post-COVID-19 conditions exhibited extensive hypometabolic right fronto-temporal clusters. Patients with more numerous symptoms during the initial phase and with a longer duration of symptoms were at higher risk of persistent brain involvement.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00259-022-06013-2.
Keywords: FDG PET, PET, Long COVID, Post-COVID-19 conditions, COVID-19, Outpatients, Non-hospitalized, Brain involvement
Introduction
Brain 18F-FDG PET holds great promise to assess brain involvement in patients with post-COVID-19 conditions (PCC) and may help identify distinct prognoses and management strategies for these patients [1, 2]. PCC is defined by the World Health Organization (WHO) as a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis [3]. The current literature includes three brain 18F-FDG PET series of adult patients with long COVID [4–6]. Two of these studies found PCC-specific hypometabolic regions [4, 5] involving the fronto-orbital and olfactory regions as well as other limbic/paralimbic regions, the brainstem and the cerebellum [4], with significant associations of cortical, brainstem, and cerebellar hypometabolic regions and clinical characteristics such as the number and types of symptoms [4, 5]. The third study did not find any decreases in metabolic activity in patients with subjective complaints [6]. These inconsistent results may be due to the very heterogeneous populations examined: (i) different times of symptom onset (from 3 weeks to 3 months), (ii) in- and outpatients (54 to 100% of hospitalized patients, 15 to 40% of intensive care unit patients), and (iii) patients with complaints or deficits [7 for a review].
Even though WHO’s current definition of long COVID [3] encompasses a large range of conditions, there is an urgent need to characterize PCC in patients that have never been hospitalized for COVID. This group of PCC outpatients is younger and more socially active than PCC inpatients [8].
The current study aims to describe brain 18F-FDG PET findings in a homogeneous outpatient population with PCC and to identify associations with clinical characteristics.
Materials and methods
We retrospectively identified consecutive patients that presented with PCC between September 2020 and May 2022, satisfied the WHO definition [3], and had a brain 18F-FDG PET scan to investigate suspected brain involvement. All patients were referred from the Department of Infectious Diseases, Regional University Hospital of Nancy, and underwent a standardized clinical assessment, based on widely validated scales, at onset and at the time of the PCC consultation. Neurocognitive disorders, anxiety-depressive disorders, dyspnea, and fatigue were respectively quantified with the Montreal Cognitive Assessment (MoCA), the Hospital Anxiety and Depression (HAD), the modified Medical Research Council (mMRC), and the Chalder Fatigue scales (Table 1).
Table 1.
Patient characteristics
| N = 28 | |
|---|---|
| Female (%) | 21 (75) |
| Age (years old, mean ± SD) | 46.1 ± 9.8 |
| Health professional (%) (n = 27) | 13 (48) |
| Psychiatric history* (%) (n = 27)‡ | 7 (26) |
| Time from onset of symptoms to first post-COVID consultation (months, mean ± SD) | 8.3 (5.3) |
| COVID diagnosis confirmed by professional Antigenic or PCR test (%) | 19 (68) |
| COVID diagnosis confirmed by serology (%) | 17 (61) |
| Patients that have still not resumed work or their studies (n = 27) | 19 (70) |
| Initial COVID-19 phase | |
| Number of symptoms (mean ± SD) | 3.6 ± 1.7 |
| General symptoms (fever, anorexia) (%) | 18 (65) |
| Neurological symptoms (headaches, cognitive disorders, language disorders) (%) | 18 (64) |
| Asthenia (%) | 18 (64) |
| Respiratory signs (cough, dyspnea, shortness of breath) (%) | 17 (61) |
| Anosmia, ageusia (%) | 10 (36) |
| Arthro-muscular symptoms (aches, arthralgia, myalgia) (%) | 8 (29) |
| Digestive symptoms (nausea, vomiting, diarrhea) (%) | 6 (21) |
| Cardiovascular symptoms (chest pain, chest tightness, palpitations) (%) | 5 (18) |
| Post-COVID-19 condition | |
| Number of symptoms (mean ± SD) | 4.9 ± 1.7 |
| General symptoms (%) | 21 (75) |
|
Neurological symptoms (%) Headaches Cognitive disorders Language disorders |
28 (100) 13 (46) 28 (100) 11 (39) |
| Asthenia (%) | 24 (86) |
| Respiratory signs (%) | 19 (68) |
| Anosmia, ageusia (%) | 11 (39) |
| Arthro-muscular symptoms (%) | 15 (54) |
| Digestive symptoms (%) | 7 (25) |
| Cardiovascular symptoms (%) | 12 (43) |
| Hyperventilation syndrome (%) | 15 (54) |
| Psychological impact (anxiety, depressive syndrome) (%) | 12 (43) |
| Dysautonomic syndrome (%) | 8 (29) |
| Post-traumatic stress syndrome (%)** | 1 (3.5) |
| Clinical score scales | |
| MoCA (/30) (n = 12, mean ± SD) | 25.9 ± 2.7 |
| HAD (n = 13) | |
| On the anxious side (/21) (mean ± SD) | 7.0 ± 2.9 |
| On the depressive side (/21) (mean ± SD) | 6.6 ± 3.1 |
| mMRC (/4) (n = 13) (n = 13, mean ± SD) | 1.9 ± 1.1 |
| Chalder fatigue scale (n = 12) | |
| Overall score (/33) (mean ± SD) | 27.8 ± 3.7 |
| Physical score (/21) (mean ± SD) | 17.5 ± 3.1 |
| Psychological score (12) (mean ± SD) | 10.4 ± 1.5 |
| Ongoing medications ‡ | |
| None (%) | 12 (43) |
| Anxiolytic/antidepressant drug (%) | 7 (25) |
| Antihistamine drug (%) | 6 (21) |
| Beta-blocker/antianginal drug (%) | 4 (14) |
| Antiplatelet (%) | 4 (14) |
| Melatonin (%) | 3 (11) |
| Proton pump inhibitor (%) | 2 (7) |
| Curative anticoagulant (%) | 1 (3.5) |
| Anti-epileptic drug (%) | 1 (3.5) |
| Cerebral MRI results (n = 20) ‡ | |
| Normal (%) | 13 (65) |
| Mild aspecific vascular leukopathy (%) | 5 (25) |
| Olfactory bulb atrophy (%) | 1 (5) |
| Right parasagittal occipital meningioma (%) | 1 (5) |
*No psychiatric disease at the time of COVID infection (2 patients with antecedents of depressive disorders, 3 with anxiety-depressive disorders, 1 with a bipolar disorder, and 1 with an eating disorder), **post-traumatic stress syndrome evaluated in health workers after a clinical evaluation by a psychologist, ‡ no significant associations between presence/absence or normal/abnormal scans and neuropsychological test scores or metabolism of identified brain 18F-FDG PET clusters. HAD, hospital anxiety and depression; mMRC, modified Medical Research Council; MoCA, Montreal Cognitive Assessment; PCR, polymerase chain reaction; SD, standard deviation
Brain involvement was suspected when functional complaints potentially originating from the brain were reported. These included asthenia, anosmia/ageusia, neurological symptoms, and/or dysautonomia.
Twenty-eight, age- and sex-matched, healthy controls with no neuropsychiatric antecedents and normal neuropsychological tests (NCT03345290) (n = 28, 45.6 ± 11.4 years old, 21 women) were selected from a local database.
Brain 18F-FDG PET (Vereos, Philips®) was performed according to the European guidelines [9], recorded over a 10- to 15-min single-bed-position acquisition, 30–45 min after the injection of 2 MBq/kg of 18F-FDG and followed by a sensory rest period. All patients had blood glucose < 10 mmol/L and fasted at least 6 h prior to the injection. Patient and healthy control PET images were reconstructed with the iterative OSEM method and corrected for scatter, random coincidences, and attenuation with a CT scan, as per routine clinical practice.
After normalization of images to the MNI (Montreal National Institute) space and smoothing with a 8-mm Gaussian filter, voxel-based group comparisons were performed with SPM 12 (https://www.fil.ion.ucl.ac.uk/spm/software/spm12/) using age and sex as covariates, proportional scaling for the intensity normalization, and an inclusive grey-matter mask encompassing the brainstem and the cerebellum. The statistical threshold was set at a p-voxel value of 0.005, uncorrected, p-cluster value of 0.05, and corrected family-wise-error (FWE). Significant findings at a more constrained threshold of p < 0.05 corrected for voxel using the FWE method were also specified. Identified clusters were reported according to the anatomical automatic labelling (AAL) atlas (https://www.gin.cnrs.fr/en/tools/aal/), and the extraction of individual cluster values was performed with Marsbar (https://marsbar-toolbox.github.io/). Individual level metabolic values of orbito-frontal areas (fronto-orbital superior, middle and inferior, olfactory, and rectus gyri), internal temporal areas (amygdalae, hippocampus, and parahippocampus), pons, and cerebellum regions of interest were also extracted with Marsbar.
Continuous variable correlations between metabolic values of identified clusters and regions of interest, and clinical characteristics were calculated using Pearson’s correlation coefficients. Associations of unequal variances between metabolic values and clinical characteristics with discrete values were assessed using Student’s t-test and adjustments determined with Levene’s test. A p value ≤ 0.05 (not corrected for multiple comparisons) was considered significant. Statistical analyses were performed on SPSS Statistics (Version 20.0. Armonk, NY: IBM Corp).
Results
This study included 28 PCC outpatients (46.1 ± 9.8 years old, 21 women) who had a brain 18F-FDG PET 16.4 ± 5.9 months after the initial COVID-19 infection. Acute COVID-19 was confirmed in 25 patients (positive SARS-CoV-2 RT-PCR or anti-spike serology test, in the absence of vaccination) with the remaining 3 patients satisfying the WHO’s definition of acute COVID-19 [10] and with clinical characteristics providing convincing evidence of an acute COVID-19 infection (see supplementary Table 1 for more details). Asthenia and respiratory or digestive disorders at the initial diagnosis were associated with a longer interval from the onset of symptoms (p ≤ 0.02) while persistent asthenia, anosmia, and arthromyalgia were associated with more numerous initial symptoms (p ≤ 0.04). Women presented with a greater number of PCC symptoms than men (p = 0.03). Table 1 provides detailed characteristics of the population.
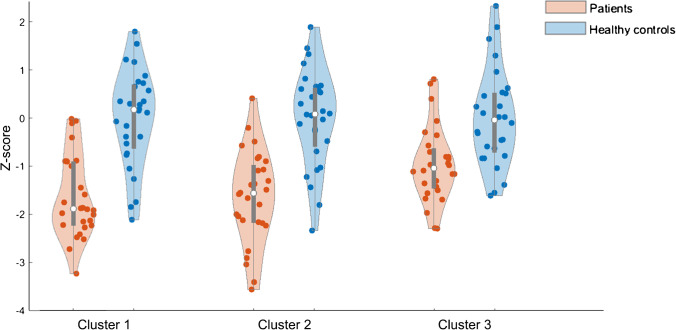
Figure 1 depicts three extensive hypometabolic clusters, found in PCC outpatients but not in healthy controls, predominantly located within the right frontal and temporal lobes, including the orbital and internal temporal areas. Interestingly, the brainstem and the cerebellum were not involved. Detailed distributions of the individual level metabolic values of these three clusters are given in Fig. 2. Table 2 provides detailed anatomical locations of these clusters. No hypermetabolism was observed.
Fig. 1.
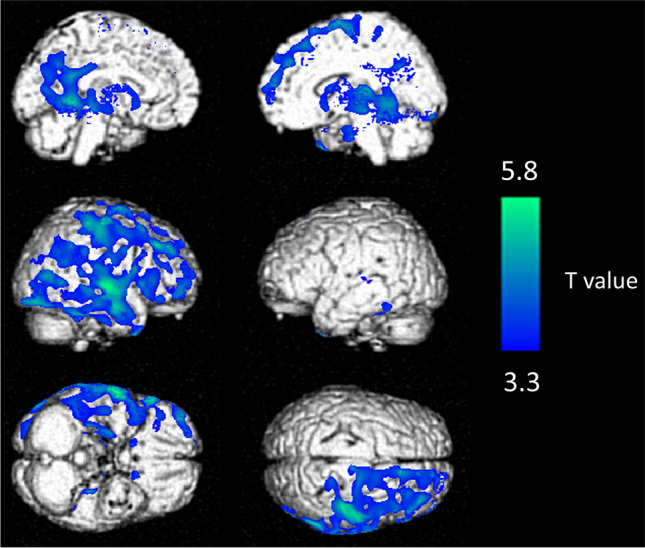
Anatomical localization of hypometabolic clusters in post-COVID-19 condition outpatients compared to healthy controls (p-voxel < 0.005, uncorrected, p-cluster < 0.05 FWE corrected), projected onto 3D volume-rendered images
Fig. 2.
Violin plots of the 3 identified metabolic clusters for patients and healthy controls expressed as Z-scores
Table 2.
Hypometabolic clusters identified from the voxel-based group comparisons between post-COVID-19 condition outpatients and healthy controls (p-voxel < 0.005, uncorrected, p-cluster < 0.05 FWE corrected)
| Localization | Cluster volume (mm3) | x | y | z | T-voxel max | |
|---|---|---|---|---|---|---|
| Cluster 1* |
Right frontal: superior, medium and inferior, orbital superior, opercular, precentral, paracentral, supplementary motor area Right temporal: superior, medium and inferior, polar superior and medium, Heschl’s gyrus, fusiform, hippocampus, parahippocampus Right parietal: paracentral and post central, supramarginal, angular, inferior, cingulum posterior, precuneus Right occipital: inferior, lingual Right insula Right thalamus, putamen, and pallidum Left hemisphere: fusiform, hippocampus, parahippocampus, lingual, calcarine, cingulum posterior, cingulum medium, precuneus, cuneus, thalamus |
137 239 | − 18 | − 46 | − 3 | 5.79 |
| Cluster 2* |
Right temporal: medium Right occipital: medium and inferior |
6 272 | 53 | − 79 | − 11 | 5.58 |
| Cluster 3 |
Left temporal: superior, Heschel gyrus Left insula Left caudate, putamen, pallidum, and thalamus |
5 754 | − 22 | − 12 | 4 | 3.48 |
*Still significant at p value < 0.05 corrected for voxel using the FWE method
Significant inverse correlations were identified between metabolic values of Clusters 1 and 2 and the number of initial symptoms reported (respective r of − 0.40 and − 0.44, p ≤ 0.04) while metabolic values of Cluster 3 were inversely correlated with the time from symptom onset (r = − 0.39, p = 0.04). Asthenia, cardiovascular and digestive complains, and neurological disorders at onset were respectively associated with lower metabolic values: Clusters 1, 2, and 3 (p ≤ 0.04), Cluster 1 (p ≤ 0.04), and Cluster 2 (p = 0.01). Persistent asthenia and language disorders were respectively associated with lower metabolic values: Cluster 1 and 3 (p ≤ 0.04) and Cluster 2 (p = 0.02).
It is noteworthy that metabolic values for the orbito-frontal, internal temporal areas and pons regions of interest were respectively correlated with the MOCA (r = 0.59), HAD (r = 0.57), and mMRC (r = 0.56) scales (p = 0.04).
Discussion
The current study reports brain involvement in a series of PCC outpatients. Extensive hypometabolic clusters, specifically involving the right frontal and temporal lobes, significantly correlated with clinical patient characteristics.
Our population is homogeneous since it only included outpatients that had never been hospitalized for COVID-19 and that satisfied the WHO’s current definition of PCC [3]. The mean interval from symptom onset was 16.4 months, with patients referred to our department after a standardized clinical investigation. Consistent with reports in the literature [11], the majority of PCC patients were women (75%). Hypometabolic clusters identified by brain 18F-FDG PET confirmed brain involvement in PCC outpatients and were consistent with results of two previous PET studies implicating the orbito-frontal cortex and internal temporal areas [4, 5]. However, the lack of pons and cerebellum region involvement in our study diverges from previous PET findings [4]. This may be related to the inclusion of a proportion of hospitalized patients that were mechanically ventilated in the previous PET study [4], with critical care hospitalization potentially leading to brain hypometabolism involving the brainstem and cerebellum [12]. It is noteworthy that brain hypometabolism in our study predominantly affected the right hemisphere of the brain (Fig. 1 and Table 2), which is consistent with brain 18F-FDG PET findings reported in the two previous PET studies which included PCC patients [4, 5]. The right hemisphere is implicated in awareness and emotional regulation [13], which may be related to the neuropsychiatric symptoms observed in PCC [14]. Further studies will be required to explain this right lateralization of brain involvement in patients with PCC.
Our study indicates that hypometabolism clusters are associated with a higher number of symptoms at the time of the initial infection. This is consistent with a prospective cohort of 4182 outpatients which found that patients reporting more than 5 symptoms at initial diagnosis were 3.5 times more likely to develop PCC [15]. This is also in line with the Guedj et al. study which identified significant inverse correlations of an increased number of functional complaints with brainstem and cerebellum metabolism [4]. In addition, our study identified that longer duration of symptoms was associated with lower metabolism in identified clusters, which suggests that post-COVID conditions are becoming chronic. This was also partially observed in the Guedj et al. study which noted a trend between PET hypometabolism and the duration of symptoms after the initial infection [4]. The correlations between metabolism in the orbito-frontal, internal temporal areas as well as the pons regions of interest and the MOCA, HAD, and mMRC scales, to respectively measure cognitive performances of the olfactory network [16], anxiety, or dyspnea underline the fact that brain 18F-FDG PET is useful to monitor clinical symptoms related to functional regions of the brain.
To conclude, our homogeneous PCC outpatient series confirms brain involvement by 18F-FDG PET and identifies a hypometabolic imaging pattern implicating the right fronto-temporal lobes. A greater number of clinical symptoms during the initial phase of infection and a longer duration of symptoms are risk factors for persistent brain involvement.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
All authors contributed significantly to the collection, analysis, and interpretation of the data (AB, SH, MD, SB, AC, FG, AV), to the writing of the manuscript (AB, SH, AV), and to the revision of the manuscript (SB, AC, FG, AV).
Data availability
Data that support the findings of this study may be requested from the corresponding author (AV).
Code availability
Not applicable.
Declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Regional University Hospital of Nancy (n°CO-27, August 1st 2022) and complied with the principles of the Declaration of Helsinki.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest/competing interests
The authors declare no competing interests.
Footnotes
This article is part of the Topical Collection on Neurology.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
François Goehringer and Alexandra Bruyere contributed equally.
References
- 1.Verger A, Kas A, Dudouet P, Goehringer F, Salmon-Ceron D, Guedj E. Visual interpretation of brain hypometabolism related to neurological long COVID: a French multicentric experience. Eur J Nucl Med Mol Imaging. 2022;49:3197–3202. doi: 10.1007/s00259-022-05753-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verger A, Barthel H, Tolboom N, Fraioli F, Cecchin D, Albert NL, et al. 2-[18F]-FDG PET for imaging brain involvement in patients with long COVID: perspective of the EANM Neuroimaging Committee. Eur J Nucl Med Mol Imaging. 2022;s00259–022–05913–7. [DOI] [PMC free article] [PubMed]
- 3.A clinical case definition of post COVID-19 condition by a Delphi consensus. World Health Organisation website. [Internet]. 2021. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021. Accessed 26 Sept 2022.
- 4.Guedj E, Campion JY, Dudouet P, Kaphan E, Bregeon F, Tissot-Dupont H, et al. 18F-FDG brain PET hypometabolism in patients with long COVID. Eur J Nucl Med Mol Imaging. 2021;48:2823–2833. doi: 10.1007/s00259-021-05215-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sollini M, Morbelli S, Ciccarelli M, Cecconi M, Aghemo A, Morelli P, et al. Long COVID hallmarks on [18F]FDG-PET/CT: a case-control study. Eur J Nucl Med Mol Imaging. 2021;48:3187–3197. doi: 10.1007/s00259-021-05294-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dressing A, Bormann T, Blazhenets G, Schroeter N, Walter LI, Thurow J, et al. Neuropsychological profiles and cerebral glucose metabolism in neurocognitive Long COVID-syndrome. J Nucl Med. 2021;jnumed.121.262677. [DOI] [PMC free article] [PubMed]
- 7.Meyer PT, Hellwig S, Blazhenets G, Hosp JA. Molecular imaging findings on acute and long-term effects of COVID-19 on the brain: a systematic review. J Nucl Med. 2022;jnumed.121.263085. [DOI] [PMC free article] [PubMed]
- 8.Augustin M, Schommers P, Stecher M, Dewald F, Gieselmann L, Gruell H, et al. Post-COVID syndrome in non-hospitalised patients with COVID-19: a longitudinal prospective cohort study. The Lancet Regional Health - Europe. 2021;6:100122. doi: 10.1016/j.lanepe.2021.100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guedj E, Varrone A, Boellaard R, Albert NL, Barthel H, van Berckel B, et al. EANM procedure guidelines for brain PET imaging using [18F]FDG, version 3. Eur J Nucl Med Mol Imaging. 2022;49:632–51. Accessed 26 Sept 2022. [DOI] [PMC free article] [PubMed]
- 10.WHO COVID-19: case definitions. World Health Organisation website. [Internet]. 2020. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2020.2. Accessed 26 Sept 2022.
- 11.Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, et al. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021;6:e005427. doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heiss W-D. PET in coma and in vegetative state: PET in coma and in vegetative state. Eur J Neurol. 2012;19:207–211. doi: 10.1111/j.1468-1331.2011.03489.x. [DOI] [PubMed] [Google Scholar]
- 13.Carota A, Bogousslavsky J. Minor hemisphere major syndromes. In: Bogousslavsky J, editor. Frontiers of Neurology and Neuroscience [Internet]. S. Karger AG; 2018 [cited 2022 Sep 26]. p. 1–13. Available from: https://www.karger.com/Article/FullText/475690 [DOI] [PubMed]
- 14.Fond G, Masson M, Lançon C, Richieri R, Guedj E. The neuroinflammatory pathways of post-SARS-CoV-2 psychiatric disorders. L’Encéphale. 2021;47:399–400. doi: 10.1016/j.encep.2021.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guedj E, Morbelli S, Kaphan E, Campion J-Y, Dudouet P, Ceccaldi M, et al. From early limbic inflammation to long COVID sequelae. Brain. 2021;144:e65–e65. doi: 10.1093/brain/awab215. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data that support the findings of this study may be requested from the corresponding author (AV).
Not applicable.