Abstract
Purpose
This study aims to understand parents’ experiences of school integration support for their child’s transition to K-12 schooling during or after cancer treatment.
Methods
This integrative literature review used PubMed, CINAHL, PsycINFO, and Embase databases and included articles from January 2000 to July 2022 describing parent experiences with support from healthcare providers, school faculty/systems, and school integration programs. This review was guided by an adapted School Re-Entry Model and used constant comparison to identify common themes and guide synthesis. The Johns Hopkins Evidence and Quality Guide was used to appraise article quality and level of evidence.
Results
Thirty-five articles were included in the final review: seventeen qualitative, fourteen quantitative, and four mixed or multi-method designs. Parents reported experiences receiving support from healthcare providers, school faculty/systems, school integration programs, and “other” sources. Parents reported both facilitators and barriers to communication, knowledge, and the process of receiving school integration support.
Conclusions
Parents found neuro/psychologists highly supportive but reported limited support from other healthcare providers. Most parents reported mixed experiences with school faculty and reported many barriers to school system support. Parents reported positive experiences with school integration programs; however, limited programs were available.
Implications for Cancer Survivors
Future programs and research should focus on addressing identified barriers and facilitators of school integration support. Further work is also needed to understand a wider range of parent experiences during school integration.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11764-022-01276-y.
Keywords: Cancer survivors, Parents, Return to school, Schools, Systematic review
Introduction
With advancements in research and treatment of pediatric cancer, more children are surviving than ever before [1]. Despite improved survival rates, there remain many long-term effects of cancer treatment that can begin during or after treatment and reduce a child’s quality of life [2]. Neurocognitive late effects include impaired working memory, concentration, processing speed, intelligence, and attention [3–7]. Neurocognitive late effects can also affect a child’s learning abilities, school achievement, and future employment opportunities [8]. It is estimated that over 90% of pediatric brain tumor survivors experience cognitive impairment post-treatment [9]. Additionally, 80% of adolescents from a combined brain tumor/acute lymphoblastic leukemia sample experienced cognitive impairments [10]. Many survivors experience neurocognitive late effects post-treatment and may benefit from classroom accommodations and/or special education services in school following diagnosis to optimize academic outcomes and to keep up with their same-aged peers. However, the process of obtaining special education services and navigating the school system can be daunting. Parents must advocate for their child’s eligibility and be aware of and knowledgeable about available supports and services [11]. Although many challenges accompany a child’s return to school, we found no review of the literature specifically focused on parents’ experiences of school integration support following their child’s cancer diagnosis.
Previous reviews examined perspectives of stakeholders other than parents on the return to school, including healthcare providers, school faculty, and the child [12, 13]. Vanclooster et al. [13] examined parent perspectives along with other stakeholders during the process of returning to school, focusing on communication. In contrast, the aim of this integrative literature review was to focus solely on parent experiences of receiving school integration support during their child’s transition to school during or after cancer treatment. The parent perspective was chosen because of the parent’s critical role as an intermediary between the medical team and the school faculty and as an advocate for their child. The review examined the following questions: (1) what experiences do parents have in receiving support from healthcare providers, school faculty, and school integration programs during their child’s post cancer diagnosis attendance at school? And (2) what are the parent perceived barriers and facilitators for receiving school integration support?
Methods
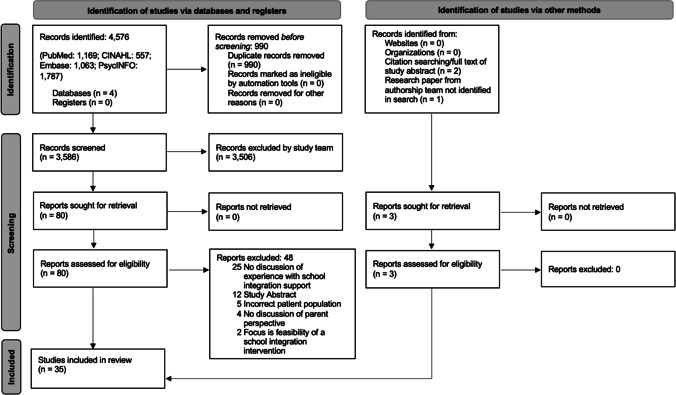
This review was guided by an adaptation of the School Re-Entry Model [11]. The School Re-Entry Model was created using a grounded theory approach based on the qualitative experiences of parents during their child’s re-entry to school after cancer [11]. This model was chosen because it outlines specific constructs that are key to the parent experience of school integration support. These constructs include communication across the medical team, education system, and family unit; stakeholder knowledge; and the process of school re-entry [11]. Our update, or the Adapted Parent Experiences of School Integration Support Model, includes these key constructs of communication, knowledge, and process (Fig. 1). The parent experience of communication and knowledge during the school entry process is influenced by their interactions with healthcare providers, school faculty/system, and school integration programs and their perceptions of how these groups interact with one another [11]. School integration programs were added into the adapted model as these programs have been shown to be helpful for the school entry process [12]. The adaptation reflects explicit inclusion of children diagnosed before they are school-aged — hence the shift to language of attendance, entry, or integration as opposed to re-entry or reintegration.
Fig. 1.
Adapted Parent Experiences of School Integration Support Model. Model definitions: communication, interactions “occurring between individuals or institutions [11];” knowledge, “information residing in an individual or stakeholder [11];” process, logistics of the transition to school and access to services [11], as influenced by the timing of support, actions of involved stakeholders, and available resources; healthcare professionals, trained care providers working with the survivor or family including, but not limited to, oncologists, primary care providers, oncology nurses, and neuro/psychologists. Healthcare professionals may work within the hospital, outpatient, or school setting (i.e., school nurse); school faculty, the individual staff at the school, such as a general education teacher, special education teacher, school principal, tutor, or school counselor; school system, institution where the child receives education; school integration program, an intervention, program, or model of care developed and implemented to help parents and children with the transition to school during or after active cancer treatment. This includes, but is not limited to, school liaison programs and school integration research interventions
Search strategy
We examined four databases (PubMed, CINAHL, PsycINFO, and Embase) to identify papers that discussed parent experiences of school integration support during their child’s attendance at school post cancer diagnosis. We used the following keywords and medical subject headings in our search: neoplasms, adolescent, child, parents, guardian, family, and schools. Please see supplemental information for full search terms used for each database. The reference lists of each article were reviewed for additional studies to be included.
Inclusion and exclusion criteria
Articles published between January 2000 and July 2022 were included. Older studies were excluded given the lower 5-year survival rate for pediatric cancer during this time [1, 14], and research prior to 2000 tended to focus on contemporary treatment strategies with more homogenous toxicity profiles. Studies were included if they described parent experiences and perspectives on the support that they received during their child’s attendance at school post cancer diagnosis. Attendance in school was defined as attending in-person K-12 schooling after a cancer diagnosis, during active cancer treatment, or in partial or complete remission. All malignant pediatric cancer types were included. Parent experience with school integration support was defined as any qualitative or quantitative report of support received from a healthcare provider, school faculty, or school integration program.
Studies were excluded from review if they were not retrievable in English or were gray literature. Studies were excluded if they focused primarily on a serious illness other than pediatric cancer or nonmalignant conditions. Studies that described perspectives of parents with children who had not begun attending school or perspectives from other stakeholders were also excluded. Both EP and CMP independently reviewed the titles/abstracts and full texts and met to reach consensus on article inclusion.
Critical appraisal
The Johns Hopkins Evidence and Quality Guide was used to critically appraise the level of evidence and quality of the articles included [15]. Each article was first reviewed for its level of evidence and subsequently reviewed for its quality as a qualitative, quantitative, or mixed/multi-methods design.
Article synthesis
Articles were synthesized using the constant comparison method to identify emerging themes and patterns according to the iterative process outlined by Miles and Huberman [16, 17]. EP and CMP used the constant comparison method to compare results across articles and synthesize themes across the constructs of the Adapted Parent Experiences of School Integration Support Model.
Results
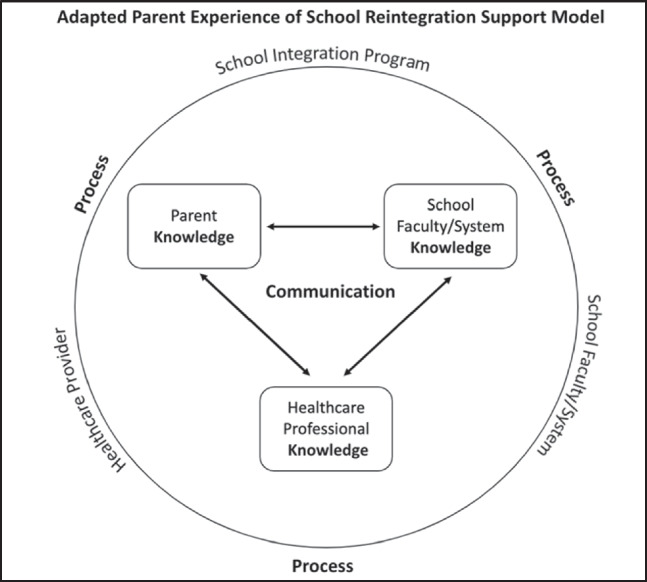
A total of 4576 results were produced from the database search. After screening by title/abstract, 80 full-text articles were reviewed resulting in 35 eligible studies (Fig. 2), including seventeen qualitative, fourteen quantitative, and four mixed or multi-method study designs, summarized in Table 1. In most studies, the term “parent” was an overarching term, which included biological parents or other caregivers. The studies were conducted in 11 different countries with parents of children with a variety of types of cancers. Only ten of the studies reported the race and ethnicity of the child or the parent. Results were categorized following the Adapted Parent Experiences of School Integration Support Model [11].
Fig. 2.
PRISMA flow diagram.
Source: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
Table 1.
Study characteristics
| Author and year | Country | Child age range at time of study (years) | Cancer type | Child race/ethnicity | Parent race/ethnicity | Parent sample size | Study design | Article quality | Relationship to the Adapted Parent Experiences of School Integration Support Model (Fig. 1) |
|---|---|---|---|---|---|---|---|---|---|
| Qualitative study designs (17) | |||||||||
| Beeler et al. (2020) [18] | USA | Median age 14* | ALL, brain tumor, other |
79.3% Caucasian 6.8% Black, 1.4% American Indian, Alaska Native 0.9% Asian, 0.9% Native Hawaiian and Pacific Islander 3.2% other, and 7.7% did not respond |
Not reported | 81 | Qualitative description, secondary analysis | Level III, quality A | School faculty/system — knowledge |
| Bruce et al. (2008) [19] | Canada | 7–20 | Brain tumor | Not reported | Not reported | 16 | Qualitative description | Level III, quality A |
Healthcare provider — communication School faculty/system — communication, knowledge, process |
| Bruce et al. (2012) [20] | Canada | 5–18 | Brain and spinal cord tumor | Not reported | Not reported | 9 families | Qualitative description | Level III, quality A | School integration program — communication, knowledge, process |
| Cheung et al. (2014) [21] | Australia | 0–16 | Brain tumor | Not reported | Not reported | 17 | Qualitative description | Level III, quality B |
Healthcare provider — communication, process School faculty/system — knowledge, process |
| Ellis et al. (2013) [22] | Australia | 8–13 | Leukemia, sarcoma, CNS tumor, aplastic anemia | Not reported | Not reported | 8 | Qualitative description | Level III, quality A | School integration program — process |
| Inhestern et al. (2020) [23] | Germany | 0–17 | Leukemia or CNS tumor | Not reported | Not reported | 49 | Qualitative description | Level III, quality A |
School faculty/system — communication, process School integration program — process |
| Hen (2022) [24] | Israel | 5–17 | Specific cancer type not reported | Not reported | Not reported | 15 | Qualitative description | Level III, quality B | School faculty/system — communication, knowledge |
| McLoone et al. (2011) [25] | Australia | 12–20 | Leukemia (ALL, AML, CML), lymphoma, sarcoma (Ewing, osteo), other | Not reported | Not reported | 36 | Qualitative description | Level III, quality A |
Healthcare provider — communication School faculty/system — communication, knowledge, process |
| McLoone et al. (2013) [26] | Australia | 3–12 | Leukemia (ALL, AML), Lymphoma, rhabdomyosarcoma, tumor (brain, liver, Wilms) | Not reported | Not reported | 42 | Qualitative description | Level III, quality A | School faculty/system — communication, process |
| Paré-Blagoev et al. (2019) [11] | USA | 8–19 | ALL, brain tumor |
80% White 10% Black 10% Hispanic |
Not reported | 9 | Grounded theory | Level III, quality A |
Healthcare provider — communication, knowledge School faculty/system — communication, knowledge, process |
| Rivero-Vergne et al. (2010) [27] | Puerto Rico | 6–17 | ALL | Not reported | Not reported | 7 | Phenomenology | Level III, quality B |
Healthcare provider — process School faculty/system — communication, knowledge, process |
| Slater et al. (2020) [28] | Australia | 0–19 | Solid tumor, leukemia, lymphoma, nonmalignant hematology | Not reported | Not reported | 25 | Discovery interviews | Level III, quality A | School faculty/system — process |
| Tresman et al. (2016) [29] | UK | 3–7 | Brain tumor (medulloblastoma) | Not reported | Not reported | 9 | Qualitative description | Level III, quality B | Healthcare provider — communication, process |
| Tsimicalis et al. (2018) [30] | Australia | < 1–19 | ALL, AML, lymphomas, CNS, and miscellaneous intracranial and intraspinal neoplasm, neuroblastoma, and other peripheral nervous cell tumors including retinoblastoma, renal tumors, malignant bone tumors, soft tissue, and other extraosseous sarcomas | Not reported | Not reported | 66 | Qualitative description | Level III, quality A | School faculty/system — communication, process |
| Vanclooster et al. (2018) [31] | Belgium | 7–10 | Brain tumor | Not reported | Not reported | 9 | Qualitative description | Level III, quality A | School faculty/system — communication, knowledge, process |
| Vanclooster et al. (2019) [32] | Belgium | 7–10 | Brain tumor | Not reported | Not reported | 9 | Qualitative description | Level III, quality A |
Healthcare provider — communication School faculty/system — communication, knowledge, process |
| Vanclooster et al. (2020) [33] | Belgium | 7–10 | Brain tumor | Not reported | Not reported |
9 (round 1 & 2) 7 (round 3) |
Qualitative description | Level III, quality A |
Healthcare provider — communication, process School faculty/system — communication, process |
| Quantitative study designs (14) | |||||||||
| Annett et al. (2009) [34] | USA | 6–12 | ALL | Not reported/insufficient information | Not reported/insufficient information | 7 families | Observational, case series | Level III, quality B | School integration program — process |
| Bava et al. (2016) [35] | USA | 5–18 | ALL |
6.1% White / Non-Hispanic 89.8% Latino 4.1% Asian Data reported as parent–child dyads |
6.1% White/Non-Hispanic 89.8% Latino 4.1% Asian Data reported as parent–child dyads |
49 parent–child dyads | Non-randomized prospective cohort study | Level III, quality B | School integration program — knowledge, process |
| Hauff et al. (2019) [36] | USA | 11–21 | Childhood cancers (ALL, solid tumor, Hodgkin and non-Hodgkin lymphomas) and CNS tumor | Not reported | Not reported | 47 | Cross-sectional | Level III, quality A | School faculty/system — knowledge |
| Hocking et al. (2017) [37] | USA | Pre-K to post- college* | Brain tumor, leukemia, lymphoma, non-CNS solid tumor | Not reported | Not reported | 102 families | Cross-sectional | Level III, quality B | School faculty/system — communication, process |
| Jacobson et al. (2020) [38] | USA | 4–18 | Brain tumor, leukemia, lymphoma, and other non-CNS cancer |
81.5% White 7.2% Black 4.6% Multiracial 1.0% Asian 1.5% Alaska Native or Hawaiian/Pacific Islander 4.6% unknown race/ethnicity |
Not reported | 195 | Cross-sectional | Level III, quality A |
Healthcare provider — knowledge, process School faculty/system — communication, knowledge, process |
| Lee et al. (2019) [39] | South Korea | ≥ 9 | No type specified | Not reported | Not reported | 210 | Cross-sectional | Level III, quality B | School faculty/system — communication, knowledge, process |
| Moore et al. (2009) [40] | USA | 6–19 | ALL, non-Hodgkin lymphoma | Not reported |
76.3% White Other not reported |
59 | Cross-sectional | Level III, quality A |
Healthcare provider — communication, process School faculty/system — communication, knowledge, process |
| Northman et al. (2018) [41] | USA | 5–17 | Leukemia, lymphoma, brain tumor, other |
97.8% White/Caucasian in SLP group 2.2% non-White/non-Caucasian Reported in aggregate with parents |
97.8% White/Caucasian in SLP group 2.2% non-white/non-Caucasian Reported in aggregate with children |
93 | Quasi-experimental, non-equivalent control groups (post-test only) | Level II, quality B |
Healthcare provider — process School integration program —communication, knowledge |
| Northman et al. (2015) [42] | USA | Elementary, middle, and high school* | Brain tumor, leukemia, Other | Not reported | Not reported | 57 | Cross-sectional | Level III, quality B |
Healthcare provider — communication School faculty/system — process School integration program — communication, knowledge, process |
| Patel et al. (2014) [43] | USA | 6–18 | ALL, non-ALL, AML, non-Hodgkin's lymphoma/lymphoblastic lymphoma, other | Not reported | 80% White (including Hispanic Americans and Anglo Americans) | 21 | RCT (pilot study) | Level I, quality A | School integration program — knowledge, process |
| Quillen et al. (2011) [44] | USA | 7–19 | Lymphoblastic leukemia, brain tumor, Wilm’s tumor, non-Hodgkin’s lymphoma, neuroblastoma, retinoblastoma | Not reported | Not reported | 20 | Cross-sectional | Level III, quality B |
Healthcare provider — process School faculty/system – communication, process |
| Rubens et al. (2016) [45] | USA | 5–17 | Brain tumor, leukemia, neuroblastoma, neurofibromatosis, other, none reported | Not reported |
87% Caucasian 2% non-Caucasian 4% Unknown |
93 | Cross-sectional | Level III, quality B | School integration program — knowledge, process |
| Ruble et al. (2019) [46] | USA | 13 median age* | ALL, lymphoma, non-Hodgkin’s lymphoma, brain tumor, AML, other |
83.3% Caucasian 6.9% Black/ African American 3.0% Mixed racial background 3.5% Other 3.9% Hispanic ethnicity |
Not reported | 203 | Cross-sectional | Level III, quality A | Healthcare provider — communication, knowledge |
| Van’t Hooft et al. (2016) [47] | Sweden | 0–17 | Brain tumor | Not reported | Not reported | 34 | Cross-sectional | Level III, quality B |
Healthcare provider — process School faculty/system — process School integration program — communication, process |
| Mixed or multi-method study designs (4) | |||||||||
| Donnan et al. (2015) [48] | Australia |
3–20 quantitative survey 4–20 qualitative focus groups |
ALL, AML, osteosarcoma, neuroblastoma, brain tumor, Ewing’s sarcoma, Hodgkin’s disease or lymphoma, clear cell sarcoma, rhabdomyosarcoma, other |
Not reported/insufficient information (75% born in Australia 25% born in country other than Australia) |
Not reported |
80 quantitative survey 24 qualitative focus groups |
Quantitative questionnaire followed by qualitative focus groups | Level III, quality B | School faculty/system — communication, knowledge, process |
| Patel et al. (2020) [49, 50] | USA |
6–21 (phase 1) 5–12 (phase 2) |
Leukemia | Not reported |
100% Latino Race not reported |
20 (phase I) 10 (phase 2) |
Pilot study with phase I: qualitative; phase II: non-experimental, one group (pre-test, post-test) | Level III, quality B | School integration program — knowledge, process |
| Soejima et al. (2015) [51] | Japan | 9–18 | Leukemia, lymphoma, osteosarcoma, other | Not reported | Not reported |
36 (quant) 3 (qual) |
Quantitative questionnaires followed by qualitative semi-structured interviews | Level III, quality B | School faculty/system — communication, knowledge |
| Thornton et al. (2022) [52] | USA | Not reported | ALL, lymphoma, brain tumor, AML, other non-CNS tumor |
82.1% White 6.9% Black 3.5% Multiple 1.7% Alaskan/Native American 1.2% Hawaiian/Pacific Islander 4.6% Other |
Not reported | 174 (qualitative interviews were with healthcare providers and not used for this study) | Explanatory mixed methods — quantitative survey followed by qualitative interviews | Level III, quality A |
Healthcare provider — communication, knowledge School faculty/system — process |
Key: ALL, acute lymphoblastic leukemia; AML, acute myelogenous leukemia; CNS, central nervous system; USA, United States of America; level I evidence, experimental study design/RCT; level II evidence, quasi-experimental study design; level III, non-experimental study design, qualitative study design; quality A/B, high or good quality
*Age range not reported
Healthcare providers
Sixteen of the included studies discussed parent experiences with communication, knowledge, and process of receiving support from healthcare providers.
Communication
Studies reported parent–healthcare professional communication about child neurocognitive needs. There was limited communication from the oncology team on the child’s neurocognitive needs. Many parents reported that they did not receive communication about future treatment-related neurocognitive challenges from their oncology team [11, 46]. Thornton et al. found that fewer than half of parents (49%) had conversations regarding the neurocognitive effects of therapy with primary care providers at every visit, and 12% reported never having these conversations [52]. However, parents did report receiving communication from neuro/psychologists, if referred for these services by the oncology team. Parents described written reports from the neuro/psychologist as a method of clear communication about their child’s neurocognitive needs. Parents in both qualitative and quantitative studies found that the reports were written in easily understandable language that included “laymen’s terms” and clear explanations of complex terminology [21, 38].
Knowledge
The neuropsychological report increased parent knowledge of available supports, such as specific assistance and accommodation strategies, as well as general knowledge about their child’s needs [11, 38]. In contrast, parents reported receiving limited information from the oncology team. Parents did not feel the oncology team fully comprehended or divulged the non-health aspects of school integration challenges, such as legal rights to educational access or additional resources to address learning difficulties [11, 46, 52]. Ruble et al. [46] reported that parents desired additional information on non-health aspects of school integration from their child’s oncology team but were rarely provided with this information.
Process
Parents frequently described their experience with neuropsychology evaluations [21–47] and found it to be an effective resource during the transition to school [21, 38]. Parents in a qualitative study completed in the USA reported that the neuropsychological reports lent authority to and helped establish validity for their requests for additional academic support [11]. Parents also described meetings with other healthcare professionals during their child’s transition to school, including physical and occupational therapists [33, 41], speech therapists [41], and psychologists [47, 33]; however, it was not clear from these studies whether these meetings with other providers were beneficial for school integration.
Parents reported desiring support from healthcare providers during the transition to school [40, 29]. However, they tended to find support from healthcare providers unsatisfactory or completely lacking [38, 47, 29, 27]. Regarding the support that did exist, parents reported that psychologists needed to provide more psychosocial support and guidance to parents [47], referrals from other healthcare providers to neuro/psychologists were infrequent [38], they felt abandoned by the oncology team after the completion of treatment [29], and that the healthcare team should provide education to school faculty on their child’s illness [40, 29]. Additionally, the timing of information received from healthcare providers was unhelpful — the information provided was too much all at once, and too early during the child's illness [46, 21].
School faculty and system
Twenty-five studies discussed parent experiences with school faculty or the school system, including communication with school faculty, school faculty knowledge, and the process of receiving support from school faculty and accessing resources in the school system.
Communication
There was a range of both negative and positive experiences with parent–school faculty communication. Parents who described negative experiences felt burdened with the responsibility of monitoring their child’s progress [11], reminding school faculty of their child’s needs [21, 38, 19], and taking the initiative to educate school faculty on their child’s illness [24]. Across studies, parents reported that teachers needed frequent reminders regarding their child’s needs and ongoing communication to get the appropriate support in place for their child [11, 21, 38, 19, 23]. Unfortunately, parents also perceived that teachers may not take their child’s needs seriously unless a healthcare provider communicated this information [25], which may be due to survivors not physically appearing to have a disability [19]. Some studies described fragmented communication. Many parents experienced the lack of a formal or systematic way for teachers to share information on their child’s needs. Particularly, systematic communication was lacking between teachers associated with a change in the child’s grade level and with parents regarding their child’s progress in school [11, 21, 33, 32–48].
Parents also reported positive experiences with teacher communication. One study reported frequent parent conversations with school faculty [37]. Other studies described that frequent communication and earlier identification of child needs may be facilitated through strong parent–teacher relationships [32, 26]. Positive experiences were also facilitated by communication and collaboration among teachers [27, 26]. In contrast to the barrier presented by fragmented communication, parents reported that it was helpful when teachers had a systematic method for identifying and sharing information about their child’s school needs. McLoone et al. [26] discussed that parents in Australia found it helpful when teachers placed their child’s photograph and a brief description of their school needs on the staff room notice board. Soejima et al. [51] reported positive experiences were further facilitated by teacher–child communication for parents in Japan; encouragement of the child by the teacher facilitated a positive experience for the child and in turn the parent [51].
School faculty–healthcare provider communication
Parents reported few instances of communication between school faculty and healthcare providers. Three studies found that parents appreciated when hospital outpatient clinics and nurse coordinators interacted with the school through in-person visits and establishing communication pathways [21, 19, 25]. Parents felt it was important for healthcare professionals to educate school faculty and student–peers about the child’s disease and its consequences [21, 40, 29, 31]. Parents struggled when they had to act as communication intermediaries, as they did not always feel confident explaining their child’s neurocognitive and other medical issues [11, 33, 31].
Knowledge
Parents reported lower confidence in teachers’ knowledge about cancer and its impacts on schooling. Many parents described that their child’s teachers lacked an understanding of long-term cancer treatment effects and how treatment may influence school performance [11, 19, 25, 32, 48, 18]. Teachers’ understanding of long-term treatment effects on schoolwork was an important facilitator in parents receiving transition support in Japan [51]. Parents attributed low teacher understanding to a limited expertise in healthcare, lack of knowledge concerning treatment effects, and their child’s absence of an outward appearance of being disabled [19, 25, 32]. In two studies, parents of survivors in the USA noted teachers appeared nervous or uncomfortable with having a survivor in the classroom due to a lack of understanding concerning their needs [11, 18].
Process
Parents reported experiences accessing resources during school integration. One resource was formal education support, to which parents reported limited access. Many parents struggled with obtaining and understanding the components of formal education support (Individualized Education Program or IEPs and 504 plans) and other accommodations within the classroom [11, 52, 38, 36]. Parents indicated that it would be helpful to have workshops or mandatory meetings on formal educational support, classroom accommodations, and planning for the child's future [47, 33, 36]. An additional resource affecting support was the school budget; limitations in school budgets led to shortages of trained faculty and assistive technology [40, 19]. The type of school was also viewed as a resource by parents in Australia. Parents reported that certain schools, such as private, Montessori, or Steiner schools, emphasized an individualized approach and were perceived to be supportive of the child’s social, emotional, and academic needs [27, 26]. Another study revealed that parents felt educational support offered was school dependent [48]. Parents expressed the desire for a standardized approach to supporting families during integration across schools, such as a protocol or liaison [24, 48].
Parents also described that the actions of school faculty influenced support. Teacher receptiveness toward health plans was important; teachers who did not follow health plans or recommendations from the neuropsychology report were perceived as barriers to support [38, 44, 33, 40]. Timing and frequency of the support received further influenced parent experiences. Across studies, parents reported that teachers facilitated school integration support by providing both frequent academic and emotional support [33, 19, 25, 30, 26, 28]. Additionally, support was facilitated when conversations about the child’s needs were held with school staff early in the integration process [32] and the school maintained continuous contact with the family during the child’s absence [24]. In a study conducted in South Korea, many parents reported a formal school integration program would have been helpful when their child initially returned to school [39]. Parents who reported receiving home-based teaching services prior to and during school integration felt that these services highly benefitted their children [52, 30].
School integration program
Overview
Eleven studies included parent experiences with school integration programs. Four articles discussed the use of School Liaison Programs (SLPs) to facilitate school integration. In a SLP, a School Liaison (SL), who is either an experienced educator or clinician, promotes interdisciplinary communication between healthcare providers, school faculty, and families; acts as an advocate for families; provides education on the child’s needs to the school and family; and continuously reassesses the needs of the family and child [42, 41, 20, 45]. Two studies focused on parent advocacy training to help parents understand potential school related challenges and how to access resources [35, 34]. Other studies discussed programs that socially connected children with peers while in the hospital to facilitate school integration [23, 22]. Ellis et al. [22] implemented a program in which children connected with their peers at school through videoconferencing, while Inhestern et al. [23] described a family rehabilitation program where children were able to interact with other children with cancer while in the hospital. Parents in two studies received self-efficacy training on how to help their child succeed in school and access school and community resources [43, 49]. One study detailed a medical follow-up program for the child and family post-cancer treatment to ensure families received the support they needed and included medical, educational, psychosocial, and neurocognitive follow-up [47].
Communication
SLPs were described as positively affecting parent experiences with communication. SLs acted as communication “bridges” across disciplines and allowed for engagement among parents, school faculty, and healthcare providers [42, 41, 20]. Parents also appreciated when educational, psychosocial, and neurocognitive information was communicated both verbally and in writing [47].
Knowledge
Six studies described programs designed to increase parent or school faculty knowledge. Programs included SLPs, meeting with a family advocate, and parent self-efficacy training to improve parent knowledge of available school resources, child school needs, and how to help their child in school [42, 41, 45, 35, 43, 49]. In one study describing a SLP, parents also reported increased school faculty knowledge of their child’s academic needs [42]. Additionally, one study noted that parents reported better understanding in how to obtain school support services if they had greater exposure to SLP services (3 years versus less than 1 year) [45].
Process
School integration programs provided parents with support resources during the transition to school. Most school integration programs facilitated support and empowered parents with knowledge of their child’s needs and how to advocate for their child [35, 34]. In Bava et al. [35], many parents requested IEPs or 504 plans following the advocacy program. Parents perceived that both they and their child benefited from the programs they received during school integration [42, 41, 23, 20, 22–49]. However, in van’t Hooft et al. [47], parents felt as though there was still a large burden on them to ensure follow-up for the child, especially as time progressed. Parents commented that they would have liked siblings to be included in the program as well [47].
The accessibility of these school integration program resources was also explored. In Annett et al. [34], the setting in which the program took place was important to parents; parents preferred the program to be completed in the hospital or clinic rather than their home. Accessibility of programs was also related to delivery method; in Ellis et al. [22], technological issues such as poor connection of the device became a barrier to receiving the program and its benefits.
Other formal and informal support
During article synthesis, we noticed trends in seven studies regarding formal and informal support systems that did not fit within the original model categories. Informal support systems tended to be friends and neighbors who provided information (knowledge), whereas formal support systems such as government programs provided procedural support (process).
Communication
Only one study commented on communication support from informal support systems. Parents discussed how neighbors from their community reached out to the school on their behalf as a form of support [24].
Knowledge
Parents relied on informal support systems for school integration, particularly their social network consisting of friends, neighbors, and chance meetings with other parents of children with cancer. Parents reported having friends with specific knowledge, including friends who were lawyers and could provide advice on available legal support and friends who happened to be school faculty or a parent of a child with special needs and could provide education system advice [18]. Parents in the USA reported that chance encounters with other parents of children with cancer were helpful in providing information about school integration [38].
Process
Formalized parent groups and government support were important sources of support for parents. Formalized parent groups were identified as an essential support for parents of survivors in making resources available. For example, local parent associations helped connect parents with resources and information about school integration [23], and service groups took action to obtain assistive technology for transportation to school or in the classroom [19]. Studies from Germany and Puerto Rico reported that government support structures, such as availability of disability compensation and government-based at-home teaching services, were identified by parents as essential process supports for school integration [27, 23]. In addition to formalized support groups, parents in one study commented that neighbors and friends were sources of financial and logistical support during the integration process [24].
Discussion
This integrative review explored 35 research articles detailing parent experiences with and perspectives of school integration support from healthcare providers, school faculty/system, school integration programs, and other formal and informal sources of support. The review fills a gap in the literature in describing parent experiences with school integration support and synthesizes parent perceived barriers and facilitators (Table 2). Overall, the results across quantitative, qualitative, and mixed/multi-method studies were broadly consistent with each other.
Table 2.
Synthesized barriers and facilitators to school integration support identified by parents
| Healthcare provider | School faculty and systems | School integration program | Other | |
|---|---|---|---|---|
| Communication | (-) Insufficient communication between healthcare providers and school faculty/systems about potential consequences of cancer treatment, including neurocognitive effects, and sharing the neuropsychological report.Quality A [n = 5], Quality B [n = 2] |
( +) School Liaison Programs acting as bridges of communication between school faculty, parents, and healthcare providers Quality A [n = 1], Quality B [n = 2] ( +) Verbal and written summaries of educational and psychosocial recommendations Quality B [n = 1] |
( +) Neighbors and community members reaching out to the school on behalf of the parents/child Quality B [n = 1] |
|
|
( +) Clearly written neuropsychology reports Quality A [n = 1], Quality B [n = 1] (-) Inappropriately timed communication about neurocognitive effects from cancer treatment Quality A [n = 1], Quality B [n = 1] |
( +) Frequent parent–teacher communication Quality B [n = 1] ( +) Strong parent–teacher relationships Quality A [n = 2] (-) Fragmented communication among school faculty on child needs Quality A [n = 4], Quality B [n = 2] (-) Burden of monitoring child academic progress falls on the parents rather than a collaborative effort with teachers Quality A [n = 3], Quality B [n = 1] |
|||
| Knowledge |
( +) Specific information about health-related learning difficulties and formal education support processes (IEP/504 plan) Quality A [n = 2] (-) Oncology team not fully comprehending or divulging non-health challenges of school reintegration such as legal rights or access to additional resources Quality A [n = 2] |
(-) Limited knowledge of cancer treatment and its consequences for child school functioning Quality A [n = 5], Quality B [n = 1] (-) Limited knowledge in working with children who have variable academic challenges resulting from complex medical conditions or treatment Quality A [n = 3] |
( +) Programs that improved parent advocacy skills and knowledge of child school needs postcancer treatment Quality A [n = 1], Quality B [n = 5] |
( +) Provide opportunities for informal networking to exchange knowledge between parents of cancer survivors Quality A [n = 2] |
| Process |
( +) Continue providing child’s neuropsychological evaluation and report to parents Quality A [n = 2], Quality B [n = 1] ( +) Improve parental access to other healthcare providers and specialists (physical, occupational, and speech therapists) as needed Quality A [n = 1], Quality B [n = 2] (-) Discontinuation of oncology team and other healthcare provider involvement in care and support after cancer treatment Quality A [n = 2], Quality B [n = 3] |
( +) School approach to education is individualized to student needs Quality A [n = 1], Quality B [n = 1] ( +) Frequent teacher academic and emotional encouragement Quality A [n = 6] (-) Difficulty accessing information and navigating formal education support and accommodations (IEP/504 plan) Quality A [n = 4] (-) Limited school budget for child accommodations and trained faculty Quality A [n = 2] (-) Negative teacher attitudes toward health plans or recommendations Quality A [n = 3], Quality B [n = 1] |
( +) Delivery of the program in the clinic or hospital setting Quality B [n = 1] (-) Technological issues for delivering program via technology Quality A [n = 1] (-) Lack of sibling inclusion in the program Quality B [n = 1] (-) Lack of long-term follow-through as needs continue Quality B [n = 1] |
( +) Identification of and connection to formal support structures, such as parent groups, government assistance, etc Quality A [n = 2], Quality B [n = 1] |
Key: ( +),facilitator to school reintegration; (-),barrier to school reentry. Quality A indicates a high-quality study, Quality B indicates a good-quality study
Healthcare providers
There is a gap in the information provided to families by the oncology team during the transition to school. Information does not consistently include a discussion of health-related learning difficulties, child legal rights, or formal education support processes (i.e., obtaining an IEP/504 plan) [46]. However, many providers report they do not receive formalized training in post-treatment cognitive and school issues [53, 54]. Oncology providers should have a basic knowledge of the intersection of the neurocognitive impacts of therapy and educational supports, and additional formalized training should be provided to improve oncology provider knowledge and clinical confidence [53]. Parents also reported feeling abandoned by the oncology team after cancer treatment [29] and desired more long-term support. One possibility for longer-term support could be from primary care providers (PCPs). Although PCPs are potentially poised to fill this gap, previous research demonstrates that PCPs do not feel adequately prepared to address survivor needs due to a lack of training and knowledge in survivorship care [55, 56].
Neuropsychology reports were broadly reported to be very helpful in school integration. Parents appreciated clear, easy-to-understand language and reviewing the report with the neuro/psychologist [11, 21, 38]. Referral for ongoing neuropsychological assessments is a standard of care for children who receive CNS-directed therapies [57], as they are essential for monitoring child health [58] and aid in providing support to parents during school integration [11, 21, 38]. However, studies have shown care is inconsistent with this standard. Jacobson et al. [38] reported low patient-reported referral rates by oncology providers and Ruble et al. [53] found that the majority of institutions do not have guidelines for neuropsychological assessment referral. Additionally, while neuropsychological assessments are typically covered by insurance (in the USA), these procedures are costly, and the individual co-insurance may still represent a barrier; thus, there is a dual concern that children who are eligible may not receive this recommended service and that the negative impact of being unable to benefit from such assessments could disproportionately affect families of more limited means [59, 60].
School faculty and system
Parents appreciated frequent parent–teacher communication to discuss child school needs [32, 37, 26, 39]. However, other parents experienced barriers to communication. Parents struggled with being a communication intermediary [11, 33, 31] and experienced fragmented communication among teachers and between healthcare professionals and school faculty [21, 38, 33, 32, 31]. Parents may benefit from more formalized methods of communication, such as the school reintegration protocol detailed in Tresman et al. [29]. The protocol detailed an individualized plan to educate and communicate child needs among school faculty, healthcare providers, and parents [29]. Strategies for implementing more formalized systems of sharing information should be assessed.
Parents reported that teachers had limited knowledge regarding working with survivors who have academic challenges [27, 19, 32]. Previous literature demonstrates that teachers feel they lack preparation in working with children who have chronic medical conditions [61]. Most children with academic difficulties, including those with chronic medical conditions, receive instruction in the general education setting as it is the least restrictive, most inclusive, environment [62]. Training programs preparing teachers may consider including specific strategies in helping children with medical complexities succeed in the classroom.
School integration programs
School integration programs were found to be helpful in facilitating support. Parents particularly appreciated SLPs and other programs in which they gained knowledge about how to help their child in school or advocate for their child [42, 41, 35, 43, 49]. SLPs were also perceived as helpful in bridging communication between healthcare providers and school faculty [42, 41, 20]. Unfortunately, SLPs are typically non-reimbursable by medical insurance in the USA and therefore not widely available to parents [46]. Additionally, although these programs are perceived as helpful, future work is needed to establish the effectiveness in optimizing child academic and psychosocial outcomes [63], which in turn may help to create policies that make these programs more widely available to families.
Other formal and informal supports
Parents of survivors found additional support in their child’s transition to school through informal social connections and formalized parent groups and government programs [38, 27, 19, 23, 18]. Surprisingly, access to online resources was not discussed in the included studies. A review of available parent-focused online resources about schooling after cancer suggests available tools are typically not comprehensive and are often written in a way that requires a fairly high education to be easily understood [64]. The current review demonstrates that parents seek additional support outside of the school and healthcare team, highlighting a need to create accessible online school integration resources that are comprehensive and readable across health literacy levels.
Strengths and limitations
A strength of this integrative review is its focus on parent experiences with school integration support, a previously under-studied group. In addition, this paper offers an adapted model of parent experiences with school integration that can be used by future researchers studying parent perspectives. One limitation of this review is the focus on school integration support in terms of parents’ understanding and receiving academic resources. Although academic success is an essential component of education, another crucial factor is the child’s social and emotional experience [65, 66]. Subsequent reviews should consider parent and child experiences of receiving social and emotional support. Another limitation of this review is that access to academic resources and programs may vary across countries. It is challenging to compare experiences of school integration resources and programs across countries whose healthcare and school systems have significant structural differences. However, all countries included in this review (Table 1) are classified as high income by the World Bank Classification of Income and have comparable economies [67]. Additionally, this review excluded literature that could not be found in English, limiting the international scope of this work.
Future directions
The identified barriers and facilitators provide a foundation for a model of care in delivering school integration support to parents. This review highlights the need for new communication platforms to be developed to support parents in their role as intermediary between the healthcare professionals and school faculty, for example, the use of school “passports” or protocols that share essential child medical information between the parents, school faculty, and healthcare professionals [29]. Another method to bridge this gap includes healthcare professionals meeting with parents and school faculty virtually to review the child’s learning needs. Both healthcare professionals and school faculty developed new expertise in holding virtual Internet-mediated meetings during the COVID-19 pandemic that can be an asset in school integration planning moving ahead. Future studies should explore the interest and capacity of healthcare providers, school faculty, and parents to engage in school integration planning in new ways to address parent concerns revealed in this review.
Additionally, there were only two qualitative studies conducted in the USA. Further qualitative research with parents would be beneficial to understand experiences with support specific to the resources within the USA’s healthcare and educational system. This review also highlights the need to understand experiences of school integration support from a more diverse parent population. Few studies examined and reported race and ethnicity. Of the 16 studies completed in the USA, only ten reported child or parent race and ethnicity. Additionally, the majority of the parents and children in these reported samples were White. It is essential to gain a diverse range of parent perspectives, as survivors from diverse racial and ethnic groups report more neurocognitive symptoms from cancer treatment [50] and are at risk for worse educational outcomes than their White peers [68, 69]. Future research should focus on reporting parent experiences with receiving school integration support while considering the influence of race/ethnicity as well as other social determinants of health [70]. Researchers may consider integrating our proposed model with others, such as Bronfenbrenner’s social ecological approach and Kazak’s social ecological model applied to child health [71], to understand parent experiences of school integration support within the context of social determinants of health. The majority of studies also did not distinguish between experiences of support among parents of elementary, middle school, and high school age children. The literature demonstrates that school integration support needs may vary across the lifespan. Younger children are at greater risk for developing neurocognitive late effects [72], and parents may benefit from receiving early, individualized support to promote their child’s development [73]; however, in adolescence, there is increased independence from parents, and social support may be an essential consideration in addition to academic support [73]. It will be imperative to explore how parent support needs differ across age groups and grade levels in future work.
Conclusions
This review synthesized parent-experienced barriers and facilitators to school integration support from healthcare providers, school faculty/systems, school integration programs, and other informal and formal sources. Parents found neuro/psychologists highly supportive; however, there was limited information on support from other healthcare providers. Parents reported both positive and negative experiences with teacher knowledge and communication. There were numerous reported barriers to navigating school system supports, particularly formal education support. Parents reported positive experiences with school integration programs; however, limited programs are available. School integration support is an important component of survivorship care and offers value to parents during school entry [57]. Hospitals should have school integration programs and resources more widely available to families, even if they are not reimbursable by a third-party payer. Further work is also needed to fully understand the experiences of a wider range of affected families and to address these identified barriers and facilitators to support parents and survivors during the transition to school.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
All authors contributed to the study conception and design. Literature search and analysis of articles were performed by Elaina Parrillo and Claire Petchler. The first draft of the manuscript was written by Elaina Parrillo and Claire Petchler, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
No datasets were generated for this manuscript.
Declarations
Ethics approval
This integrative review does not include research with human or animal subjects and does not require ethical approval.
Consent to participate
This integrative review does not include research with human subjects and does not require informed consent.
Consent for publication
This integrative review does not include an individual person’s data and does not require consent to publish.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Krull KR, Brinkman TM, Li C, Armstrong GT, Ness KK, Srivastava DK, et al. Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic leukemia: a report from the St Jude Lifetime Cohort Study. J Clin Oncol. 2013;31:4407–4415. doi: 10.1200/JCO.2012.48.2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer treatment and survivorship statistics, 2014. Ca Cancer J Clin. 2014;64:252–271. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 3.Wengenroth L, Rueegg CS, Michel G, Gianinazzi ME, Essig S, von der Weid NX, et al. Concentration, working speed and memory: cognitive problems in young childhood cancer survivors and their siblings. Pediatr Blood Cancer. 2015;62:875–882. doi: 10.1002/pbc.25396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stavinoha PL, Askins MA, Powell SK, Smiley NP, Robert RS. Neurocognitive and psychosocial outcomes in pediatric brain tumor survivors. Bioeng. 2018;5:73. doi: 10.3390/bioengineering5030073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phillips NS, Duke ES, Schofield H-LT, Ullrich NJ. Neurotoxic effects of childhood cancer therapy and its potential neurocognitive impact. J Clin Oncol. 2021;39:1752–65. doi: 10.1200/JCO.20.02533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner CD, Rey-Casserly C, Liptak CC, Chordas C. Late effects of therapy for pediatric brain tumor survivors. J Child Neurol. 2009;24:1455–1463. doi: 10.1177/0883073809341709. [DOI] [PubMed] [Google Scholar]
- 7.Krull KR, Hardy KK, Kahalley LS, Schuitema I, Kesler SR. Neurocognitive outcomes and interventions in long-term survivors of childhood cancer. J Clin Oncol. 2018;36:2181–2189. doi: 10.1200/JCO.2017.76.4696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Molcho M, D’Eath M, Thomas AA, Sharp L. Educational attainment of childhood cancer survivors: a systematic review. Cancer Med-us. 2019;8:3182–3195. doi: 10.1002/cam4.2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stensvold E, Stadskleiv K, Myklebust TÅ, Wesenberg F, Helseth E, Bechensteen AG, et al. Unmet rehabilitation needs in 86% of Norwegian paediatric embryonal brain tumour survivors. Acta Paediatr. 2020;109:1875–1886. doi: 10.1111/apa.15188. [DOI] [PubMed] [Google Scholar]
- 10.Kahalley LS, Wilson SJ, Tyc VL, Conklin HM, Hudson MM, Wu S, et al. Are the psychological needs of adolescent survivors of pediatric cancer adequately identified and treated? Psycho Oncol. 2013;22:447–458. doi: 10.1002/pon.3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paré-Blagoev EJ, Ruble K, Bryant C, Jacobson L. Schooling in survivorship: understanding caregiver challenges when survivors return to school. Psycho Oncol. 2019;28:847–853. doi: 10.1002/pon.5026. [DOI] [PubMed] [Google Scholar]
- 12.MartinezSantos A, del Fernandez-De-La-Iglesia JC, Sheaf G, Coyne I. A systematic review of the educational experiences and needs of children with cancer returning to school. J Adv Nurs. 2021;77:2971–94. doi: 10.1111/jan.14784. [DOI] [PubMed] [Google Scholar]
- 13.Vanclooster S, Benoot C, Bilsen J, Peremans L, Jansen A. Stakeholders’ perspectives on communication and collaboration following school reintegration of a seriously Ill child: a literature review. Child Youth Care For. 2018;47:583–612. doi: 10.1007/s10566-018-9443-4. [DOI] [Google Scholar]
- 14.Board I of M (US) and NRC (US) NCP, Hewitt, Weiner SL, Simone JV. Childhood cancer survivorship: improving care and quality of life. In: (US) NAP, editor. 2003. Available from: https://www.nap.edu/catalog/10767/childhood-cancer-survivorship-improving-care-and-quality-of-life. Accessed 11 Dec 2021. [PubMed]
- 15.Dearholt SL, Dang D. Johns Hopkins nursing evidence-based practice: model and guidelines. 3rd ed. Indianapolis, International. ISTT, editors. 2017.
- 16.Miles MB, Huberman AM. Qualitative data analysis. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- 17.Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 18.Beeler D, Paré-Blagoev EJ, Jacobson LA, Ruble K. Educating childhood cancer survivors- a qualitative analysis of parents mobilizing social and cultural capital. J Cancer Educ. 2020. [DOI] [PMC free article] [PubMed]
- 19.Bruce BS, Chapman A, MacDonald A, Newcombe J. School experiences of families of children with brain tumors. J Pediatr Oncol Nurs. 2008;25:331–339. doi: 10.1177/1043454208323619. [DOI] [PubMed] [Google Scholar]
- 20.Bruce BS, Newcombe J, Chapman A. School liaison program for children with brain tumors. J Pediatr Oncol Nurs. 2012;29:45–54. doi: 10.1177/1043454211432296. [DOI] [PubMed] [Google Scholar]
- 21.Cheung LLT, Wakefield CE, Ellis SJ, Mandalis A, Frow E, Cohn RJ. Neuropsychology reports for childhood brain tumor survivors: implementation of recommendations at home and school. Pediatr Blood Cancer. 2014;61:1080–1087. doi: 10.1002/pbc.24940. [DOI] [PubMed] [Google Scholar]
- 22.Ellis SJ, Drew D, Wakefield CE, Saikal SL, Punch D, Cohn RJ. Results of a nurse-led intervention. J Pediatr Oncol Nurs. 2013;30:333–341. doi: 10.1177/1043454213514633. [DOI] [PubMed] [Google Scholar]
- 23.Inhestern L, Peikert ML, Krauth KA, Escherich G, Rutkowski S, Kandels D, et al. Parents’ perception of their children’s process of reintegration after childhood cancer treatment. PLoS ONE. 2020;15:e0239967. doi: 10.1371/journal.pone.0239967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hen M. Mothers’ and teachers’ experience of school re-entry after a child’s prolonged absence due to severe illness. Psychol Schools. 2022;59:1122–1134. doi: 10.1002/pits.22666. [DOI] [Google Scholar]
- 25.McLoone JK, Wakefield CE, Butow P, Fleming C, Cohn RJ. Returning to school after adolescent cancer a qualitative examination of australian survivors’ and their families perspectives. J Adolesc Young Adult Oncol. 2011. [DOI] [PubMed]
- 26.McLoone JK, Wakefield CE, Cohn RJ. Childhood cancer survivors’ school (re)entry: Australian parents’ perceptions. Eur J Cancer Care. 2013;22:484–492. doi: 10.1111/ecc.12054. [DOI] [PubMed] [Google Scholar]
- 27.Rivero-Vergne A, EdD RB, EdD IR. The return to the community after cancer treatment: from safety to reality check. J Psychosoc Oncol. 2010;29:67–82. doi: 10.1080/07347332.2010.532300. [DOI] [PubMed] [Google Scholar]
- 28.Slater PJ. Telling the story of childhood cancer—the experience of families after treatment. J Patient Exp. 2020;7:570–576. doi: 10.1177/2374373519870363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tresman R, Brown M, Fraser F, Skinner R, Bailey S. A school passport as part of a protocol to assist educational reintegration after medulloblastoma treatment in childhood. Pediatr Blood Cancer. 2016;63:1636–1642. doi: 10.1002/pbc.26071. [DOI] [PubMed] [Google Scholar]
- 30.Tsimicalis A, Genest L, Stevens B, Ungar WJ, Barr R. The impact of a childhood cancer diagnosis on the children and siblings’ school attendance, performance, and activities: a qualitative descriptive study. J Pediatr Oncol Nurs. 2018;35:118–131. doi: 10.1177/1043454217741875. [DOI] [PubMed] [Google Scholar]
- 31.Vanclooster S, Bilsen J, Peremans L, der Bosch JVWT, Laureys G, Willems E, et al. Short-term perspectives of parents and teachers on school reintegration of childhood brain tumour survivors. Dev Neurorehabil. 2018;22:1–8. doi: 10.1080/17518423.2018.1498553. [DOI] [PubMed] [Google Scholar]
- 32.Vanclooster S, Bilsen J, Peremans L, der Bosch JVWT, Laureys G, Willems E, et al. Attending school after treatment for a brain tumor: experiences of children and key figures. J Health Psychol. 2019;24:1436–47. doi: 10.1177/1359105317733534. [DOI] [PubMed] [Google Scholar]
- 33.Vanclooster S, Hoeck KV, Peremans L, Bilsen J, Bosch JVDWT, Laureys G, et al. Reintegration into school of childhood brain tumor survivors: a qualitative study using the International Classification of Functioning, Disability and Health – Children and Youth framework. Disabil Rehabil. 2020;43:1–11. doi: 10.1080/09638288.2019.1708484. [DOI] [PubMed] [Google Scholar]
- 34.Annett RD, Erickson SJ. Feasibility of a school reintegration programme for children with acute lymphoblastic leukaemia. Eur J Cancer Care. 2009;18:421–428. doi: 10.1111/j.1365-2354.2009.01128.x. [DOI] [PubMed] [Google Scholar]
- 35.Bava L, Malvar J, Sposto R, Okada M, Gonzalez-Morkos B, Schweers LM, et al. A parent-directed intervention for addressing academic risk in Latino survivors of childhood leukemia: results of a pilot study. Psycho Oncol. 2016;25:1246–1249. doi: 10.1002/pon.4188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hauff M, Abel R, Hersh J, Isenberg J, Spoljaric D, Hayashi RJ, et al. Adolescent survivors’ information needs for transitions to postsecondary education and employment. Pediatr Blood Cancer. 2019;66:e27547. doi: 10.1002/pbc.27547. [DOI] [PubMed] [Google Scholar]
- 37.Hocking MC, Paltin I, Belasco C, Barakat LP. Parent perspectives on the educational barriers and unmet needs of children with cancer. Child Heal Care. 2017;47:261–274. doi: 10.1080/02739615.2017.1337516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jacobson LA, Paré-Blagoev EJ, Ruble K. Barriers to schooling in survivorship: the role of neuropsychological assessment. Jco Oncol Pract. 2020;16:e1516–e1523. doi: 10.1200/OP.20.00549. [DOI] [PubMed] [Google Scholar]
- 39.Lee JA, Lee JM, Park HJ, Park M, Park BK, Ju HY, et al. Korean parents’ perceptions of the challenges and needs on school re-entry during or after childhood and adolescent cancer: a multi-institutional survey by Korean Society of Pediatric Hematology and Oncology. Clin Exp Pediatrics. 2019;63:141–145. doi: 10.3345/kjp.2019.00696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moore JB, Kaffenberger C, Goldberg P, Oh KM, Hudspeth R. School reentry for children with cancer: perceptions of nurses, school personnel, and parents. J Pediatr Oncol Nurs. 2009;26:86–99. doi: 10.1177/1043454208328765. [DOI] [PubMed] [Google Scholar]
- 41.Northman L, Morris M, Loucas C, Ross S, Muriel AC, Guo D, et al. The effectiveness of a hospital-based school liaison program: a comparative study of parental perception of school supports for children with pediatric cancer and neurofibromatosis type 1. J Pediatr Oncol Nurs. 2018;35:276–286. doi: 10.1177/1043454218765140. [DOI] [PubMed] [Google Scholar]
- 42.Northman L, Ross S, Morris M, Tarquini S. Supporting pediatric cancer survivors with neurocognitive late effects. J Pediatr Oncol Nurs. 2015;32:134–142. doi: 10.1177/1043454214554012. [DOI] [PubMed] [Google Scholar]
- 43.Patel SK, Ross P, Cuevas M, Turk A, Kim H, Lo TTY, et al. Parent-directed intervention for children with cancer-related neurobehavioral late effects: a randomized pilot study. J Pediatr Psychol. 2014;39:1013–1027. doi: 10.1093/jpepsy/jsu045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Quillen J, Crawford E, Plummer B, Bradley H, Glidden R. Parental follow-through of neuropsychological recommendations for childhood-cancer survivors. J Pediatr Oncol Nurs. 2011;28:306–310. doi: 10.1177/1043454211418668. [DOI] [PubMed] [Google Scholar]
- 45.Rubens SL, Loucas CA, Morris M, Manley PE, Ullrich NJ, Muriel AC, et al. Parent-reported outcomes associated with utilization of a pediatric cancer school consultation program. Clin Pract Pediatric Psychology. 2016;4:383–395. doi: 10.1037/cpp0000150. [DOI] [Google Scholar]
- 46.Ruble K, Paré-Blagoev J, Cooper S, Martin A, Jacobson LA. Parent perspectives on oncology team communication regarding neurocognitive impacts of cancer therapy and school reentry. Pediatr Blood Cancer. 2019;66:e27427. doi: 10.1002/pbc.27427. [DOI] [PubMed] [Google Scholar]
- 47.van’t Hooft I, Norberg AL, Björklund A, Lönnerblad M, Strömberg B. Multiprofessional follow-up programmes are needed to address psychosocial, neurocognitive and educational issues in children with brain tumours. Acta Paediatr Oslo Nor 1992. 2016;105:676–83. doi: 10.1111/apa.13207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Donnan BM, Webster T, Wakefield CE, Dalla-Pozza L, Alvaro F, Lavoipierre J, et al. What about school? Educational challenges for children and adolescents with cancer. Australian Educ Dev Psychologist. 2015;32:23–40. doi: 10.1017/edp.2015.9. [DOI] [Google Scholar]
- 49.Patel SK, Miranda L, Delgado N, Barreto N, Nolty A, Kelly NC, et al. Adaptation of an intervention to reduce disparities in school HRQOL for Latino childhood cancer survivors. J Pediatr Psychol. 2020;45:921–932. doi: 10.1093/jpepsy/jsaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patel SK, Johansen C, Gold AO, Delgado N, Xu S, Dennis J. Social-ecological predictors of school functioning in Hispanic children treated for cancer with central nervous system–directed therapies. Pediatr Blood Cancer. 2020;67:e28320. doi: 10.1002/pbc.28320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Soejima T, Sato I, Takita J, Koh K, Maeda M, Ida K, et al. Support for school reentry and relationships between children with cancer, peers, and teachers. Pediatr Int. 2015;57:1101–1107. doi: 10.1111/ped.12730. [DOI] [PubMed] [Google Scholar]
- 52.Thornton CP, Henegan S, Carey LB, Milla K, Cork K, Cooper SL, et al. Addressing schooling in children with cancer—it’s everybody’s job, so it’s nobody’s job: an explanatory mixed-methods evaluation. J Pediatric Hematology Oncol Nurs. 2022;39:221–230. doi: 10.1177/27527530211073295. [DOI] [PubMed] [Google Scholar]
- 53.Ruble K, Paré-Blagoev J, Cooper S, Jacobson LA. Pediatric oncology provider perspectives and practices: supporting patients and families in schooling after cancer diagnosis. Pediatr Blood Cancer. 2020;67:e28166. doi: 10.1002/pbc.28166. [DOI] [PubMed] [Google Scholar]
- 54.Ellis SJ, Fardell JE, Wakefield CE, Schilstra CE, Burns MA, Donnan B, et al. Are we meeting the training needs of healthcare and education professionals supporting children with cancer in their return to school? Pediatr Blood Cancer. 2019;66:e27575. doi: 10.1002/pbc.27575. [DOI] [PubMed] [Google Scholar]
- 55.Signorelli C, Wakefield CE, Fardell JE, Foreman T, Johnston KA, Emery J, et al. The role of primary care physicians in childhood cancer survivorship care: multiperspective interviews. Oncol. 2019;24:710–719. doi: 10.1634/theoncologist.2018-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Iyer NS, Mitchell H-R, Zheng DJ, Ross WL, Kadan-Lottick NS. Experiences with the survivorship care plan in primary care providers of childhood cancer survivors: a mixed methods approach. Support Care Cancer. 2017;25:1547–1555. doi: 10.1007/s00520-016-3544-0. [DOI] [PubMed] [Google Scholar]
- 57.Wiener L, Kazak AE, Noll RB, Patenaude AF, Kupst MJ. Standards for the psychosocial care of children with cancer and their families: an introduction to the special issue. Pediatr Blood Cancer. 2015;62:S419–S424. doi: 10.1002/pbc.25675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Walsh KS, Noll RB, Annett RD, Patel SK, Patenaude AF, Embry L. Standard of care for neuropsychological monitoring in pediatric neuro-oncology: lessons from the Children’s Oncology Group (COG) Pediatr Blood Cancer. 2016;63:191–195. doi: 10.1002/pbc.25759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ngui EM, Flores G. Satisfaction with care and ease of using health care services among parents of children with special health care needs: the roles of race/ethnicity, insurance, language, and adequacy of family-centered care. Pediatrics. 2006;117:1184–1196. doi: 10.1542/peds.2005-1088. [DOI] [PubMed] [Google Scholar]
- 60.Miller LE, Kaseda ET, Koop JI, Mau KA, Heffelfinger AK. Differential access to neuropsychological evaluation in children with perinatal complications or autism spectrum disorder: impact of sociodemographic factors. Clin Neuropsychologist. 2020;35:1–21. doi: 10.1080/13854046.2020.1837247. [DOI] [PubMed] [Google Scholar]
- 61.Irwin MK, Elam M, Merianos A, Nabors L, Murphy C. Training and preparedness to meet the needs of students with a chronic health condition in the school setting. Phys Disabil Educ Relat Serv. 2018;37:34–59. [Google Scholar]
- 62.Flower A, McKenna JW, Haring CD. Behavior and classroom management: are teacher preparation programs really preparing our teachers? Prev Sch Fail Altern Educ Child Youth. 2016;61:1–7. [Google Scholar]
- 63.Burns MA, Fardell JE, Wakefield CE, Cohn RJ, Marshall GM, Lum A, et al. School and educational support programmes for paediatric oncology patients and survivors: a systematic review of evidence and recommendations for future research and practice. Psycho Oncol. 2021;30:431–443. doi: 10.1002/pon.5606. [DOI] [PubMed] [Google Scholar]
- 64.Ruble KJ, Paré-Blagoev EJ, Cooper SL, Jacobson LA. Assessment of online resources for returning to school during and after treatment of childhood cancer. J Cancer Educ. 2020;35:876–884. doi: 10.1007/s13187-019-01537-y. [DOI] [PubMed] [Google Scholar]
- 65.Lum A, Wakefield CE, Donnan B, Burns MA, Fardell JE, Jaffe A, et al. School students with chronic illness have unmet academic, social, and emotional school needs. Sch Psychology. 2019;34:627–636. doi: 10.1037/spq0000311. [DOI] [PubMed] [Google Scholar]
- 66.Janin MMH, Ellis SJ, Lum A, Wakefield CE, Fardell JE. Parents’ perspectives on their child’s social experience in the context of childhood chronic illness: a qualitative study. J Pediatric Nurs. 2018;42:e10–e18. doi: 10.1016/j.pedn.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 67.The world by income and region [Internet]. [cited 2022 May 17]. Available from: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html. Accessed 5 Aug 2022.
- 68.Education USD of. School composition and the black–white achievement gap. 2015.
- 69.Hemphill FC, Vanneman A, Rahman T. Achievement gaps: how Hispanic and White students in public schools perform in mathematics and reading on the national assessment of educational progress. 2011.
- 70.Paré-Blagoev EJ, Ruble K, Jacobson LA. Tools of the trade to address schooling related communication needs after childhood cancer: a mini-review with consideration of health disparity concerns. Semin Oncol. 2020;47:65–72. doi: 10.1053/j.seminoncol.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 71.Kazak AE. Pediatric psychosocial preventative health model (PPPHM): research, practice, and collaboration in pediatric family systems medicine. Fam Syst Heal. 2006;24:381–395. doi: 10.1037/1091-7527.24.4.381. [DOI] [Google Scholar]
- 72.Nathan PC, Patel SK, Dilley K, Goldsby R, Harvey J, Jacobsen C, et al. Guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: a report from the Children’s Oncology Group. Arch Pediat Adol Med. 2007;161:798–806. doi: 10.1001/archpedi.161.8.798. [DOI] [PubMed] [Google Scholar]
- 73.Rey-Casserly C, Meadows ME. Developmental perspectives on optimizing educational and vocational outcomes in child and adult survivors of cancer. Dev Disabil Res Rev. 2008;14:243–250. doi: 10.1002/ddrr.31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated for this manuscript.