Abstract
Financial capability, the combination of financial literacy (ability to act) and financial access (opportunity to act), improves people’s access to resources, and thus has the potential to improve health and well-being. This paper positions financial capability under the framework of social determinants of health and discusses theory and presents empirical evidence on the link between financial capability and health. Using data from the RAND American Life Panel and the structural equation modeling approach, we distinguish financial capability from the common socioeconomic position indicators such as income and education. We find that financial capability has a positive and longitudinal effect on health, independent of race/ethnicity, gender, income, education, and employment. This study demonstrates that financial capability is an independent social determinant of health. It can be theoretically and conceptually defined, empirically measured, and can inform clinical interventions that may improve population health and well-being. Implications for future research, practice, and policy are discussed.
Keywords: social determinants of health, financial capability, socioeconomic position, socioeconomic status, financial access, financial literacy
Introduction
Financial resources are essential to maintain health and well-being in individuals and households (Adler & Stewart, 2010; Link & Phlean, 1995; Sun et al., 2021; Williams & Collins 1995). Financial capability is receiving growing attention by both policymakers and social work practitioners as a viable area of intervention to increase financial resources, as well as reduce poverty and inequality (Fong et al., 2017; M.S. Sherraden et al., 2013). However, its health consequences are understudied. Social determinants of health—the conditions in which people live, work, and play that affect access to resources—contribute to health inequalities (Commission on Social Determinants of Health., 2008). Financial capability is one of the social determinants that could affect health through many pathways and mechanisms. Financial capability, the combination of the ability to act and the opportunity to act (Sherraden, 2013), could be related to multiple health-related risk and protective factors. For instance, through greater access to financial services and products and improved financial knowledge and skills, individuals can optimize their financial behavior. With higher levels of financial capability, individuals may be better equipped to manage financial stress, avoid material hardships, gain access to medical care, and increase healthy behaviors, such as affording gym memberships and fresh vegetables and fruits.
Why do we care about the relationship between financial capability and health? Shouldn’t income and wealth be enough when considering the effect of financial resources on health? First, financial capability offers a multidimensional and potentially comprehensive intervention that can address social disadvantages. As Braverman et al. (2011) point out, multifaceted social interventions can operate simultaneously to address social disadvantages and health inequalities. To elaborate, improving people’s financial capability is actionable, practical, and modifiable in ways that may reduce poverty and inequality in society. Second, the relationship between financial capability and health could inform financial capability policy design and implementation to better secure people’s well-being.
To the authors’ knowledge, the theoretical argument that financial capability is a social determinant of health has yet to be established. Further, there is a paucity of research that has empirically investigated the relationship between financial capability and health, independent of commonly studied social determinants such as race, gender, income, education, and employment.
This paper combines three U.S. national surveys in the RAND American Life Panel to investigate the relationship between financial capability and its health outcomes four years later in the general U.S. population. This paper advances current research by (a) discussing theories and conceptualizations that bridge financial capability and health, (b) isolating the effects of financial capability on health independent of income and other SEP indicators, and (c) empirically assessing the longitudinal relationship between financial capability and health. Below, we first conceptualize financial capability using the capability theory, then review empirical evidence on financial capability and health. To establish the theoretical link between financial capability and health, we position financial capability as a social determinant of health using the theory of fundamental causes and intersectionality. Next, we present the research aims and hypotheses of the present study.
Literature Review
Conceptualizing Financial Capability
Capability theory emphasizes that people’s combined capabilities are composed of both internal capabilities and external conditions(Nussbaum, 2001, 2011; Sen, 1987). The capability approach looks beyond an individualistic sense of well-being and focuses on “the real opportunities you have regarding the life you may lead” (Sen, 1987, p. 36). According to capability theory, people with enhanced knowledge and skills and access to social institutions and their external environment can take advantage of the opportunities that they have, maximize life chances, and build secure and fruitful lives (Nussbaum, 2002; Robeyns, 2005; Sen, 1993).
In this vein, financial capability has been defined as the interaction of people’s ability to act (knowledge and skills) and opportunity to act (financial inclusion in services, products, and policies) to improve financial well-being (Johnson & M.S. Sherraden, 2007). Financial capability is a person-in-environment approach that takes into account individual ability, and also what is possible, including access to safe and affordable financial products and services, and policies that offer financial access and build assets (Kondrat, 2002; M.S. Sherraden et al., 2018). In the financial capability framework, social and economic structures generate financial socialization and education opportunities, as well as financial policies, services, and products.
Equipped with financial knowledge and skills, and greater access to financial services and products, people with higher levels of financial capability have a wide range of positive outcomes. We propose a comprehensive approach to measure financial capability with latent constructs that include financial literacy (both objective and subjective) and financial access. In this paper, we extend the financial capability framework and look beyond the financial outcomes of financial capability to focus on health and well-being.
Empirical Evidence on Financial Capability and Health
Empirical studies that examine the relationship between financial capability and health have focused on individual knowledge and behavior. For example, one study conducted in Britain documented that financial capability—conceptualized as people’s abilities to make ends meet and their money management—has significant and substantial effects on psychological health beyond those associated with income and material well-being (Bennett et al., 2012; Taylor et al., 2011) examined the relationship between health literacy and financial literacy with respect to health-promoting behaviors and health status in older persons. Bennett et al. found that financial literacy is more strongly associated with mental health than health literacy. Meyer (2017) suggested that financial literacy should be included in patients’ healthcare decision-making and behavior. A recent study finds that financial health, conceptualized as spending, saving, borrowing, and planning, is associated with self-rated physical health and depressive symptoms (Weida et al., 2020). These studies focus on the relationship between individual financial literacy and financial behaviors and health. Another study found individual level financial factors (e.g., having a household budget, carrying a credit card balance) were associated with being unable to visit a doctor and medication nonadherence due to cost (Allmark & Machaczek, 2015; Mitchell, 2020) discussed the relationship between financial capability and disability and health from the perspective of the capability approach to welfare and justice. The authors conclude that the current approach to financial capability over-emphasizes individual factors and recommend more attention be given to social and environmental factors at various levels.
Regarding financial capability at the structural level, a growing body of research regarding financial inclusion and health has been emerging. Using data from the Health and Retirement Study, one study found that bank account ownership is associated with better mental health, but not physical health among older Hispanics in the United States (Aguila et al., 2016). Singh and colleagues (2019) ascertained that ownership of a bank account is associated with improved reproductive and maternal health services utilization and behavior in India. A study in Ghana found that financial inclusion is positively associated with self-rated health and negatively associated with psychological distress among older adults (Gyasi & Adam, 2020). Another study found that financial inclusion results in improved mental health of household heads in Nigeria (Ajefu et al., 2020).
Overall, the current state of research on the relationship between financial capability and health has three gaps. First, empirical studies generally lack theoretical discussion on the conceptual link between financial capability and health. Second, studies on financial capability pay more attention to individual ability than structural factors, such as financial access and financial inclusion. Third, researchers seldom take both individual factors (financial literacy) and structural factors (financial access) into account when measuring financial capability. The present study adds to this body of empirical evidence with a national U.S. sample, as well as a multidimensional measurement of financial capability. In the paragraphs below, we specify the social determinants of health framework, discuss the theory of fundamental causes and the intersectionality theory, and propose a conceptual model for the present study.
Theoretical Framework
Social Determinants of Health
Health, as defined by the World Health Organization (WHO), is “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (WHO, n.d., para.1). The WHO’s Commission on Social Determinants of Health (CSDH) defines social determinants of health as “the conditions in which people are born, grow, live, work and age” and “the fundamental drivers of these conditions’’ (CSDH, 2008, p.26). Upstream social determinants refer to the macro factors—such as economic resources, education, and racial discrimination—that fundamentally shape the downstream determinants, such as medical care, health-related knowledge, attitudes, beliefs, and behaviors (Braveman et al., 2011). Policymakers and academics have put increasing emphasis on understanding and addressing the fundamental causes, or upstream factors, of health inequities (Braveman et al., 2011). However, social determinants are complex and conceptual clarity should be established to inform interventions.
Theory of Fundamental Causes
According to the theory of fundamental causes, Link and Phelan (1995) define fundamental causes as access to resources that are linked to money, power, privilege, social support, and social networks. They help individuals avoid risks that can (a) affect multiple disease outcomes over time through multiple risk factors, and (b) continue to affect different outcomes when a person’s risk profile changes. These fundamental causes include, but are not limited to race/ethnicity, gender, or socioeconomic position (SEP). We hypothesize that financial capability, which combines people’s ability and opportunity to act, is associated with greater access to resources, which leads to desirable health effects. The link between financial capability and health may not be direct. Pathways may include material conditions, environmental factors, psychosocial conditions, health behaviors, and medical care (Sun et al., 2021).
Race, gender, and SEP are key social status categories that predict health disparities in society (Geiger, 2006; Krieger et al., 1993; Link & Phelan, 1995; Williams, 2005). Historical and contemporary structural inequalities that have resulted in differential access to financial resources have long-lasting effects on a population’s health. Below, we present how financial capability is fundamental to health by discussing its interaction with race, gender, and SEP using intersectionality theory.
Intersectionality
The concept of intersectionality or intersectional approach has become influential in contemporary social science research (Collins & Bilge, 2020; Homan et al., 2021). Briefly, intersectionality is a framework and analytic tool to conceptually reflects overlapping systems of oppression such as racism, sexism, classism, and other forms of oppression (Collins, 2000; Crenshaw, 1991). Intersectionality highlights social inequalities across socially constructed groups based on race, gender, and class (among others) shaped by the confluence of intersecting systems of oppression (Cho et al., 2013). Guided by intersectionality, below we discuss the intersections of race, gender, and financial capability, and how they are connected to health.
Race, Gender, Financial Capability, and Health
Race is at the forefront of the conceptualization of socioeconomic and health inequities (Sun et al., 2020). Indeed, research has identified racism as the root cause of health inequalities (Phelan & Link, 2015; Williams et al., 2019). Racial disparities in health are well documented (Link & Phelan, 1995; Markides & Coreil, 1986; Williams & Collins, 1995). It is not a coincidence that the COVID-19 pandemic’s weight falls disproportionately upon African Americans, Native Americans, and Latinx populations (Webb Hooper et al., 2020). Here, we emphasize inequalities in financial capability as manifestations of structural racism. Structural racism involves “macro level systems, social forces, institutions, ideologies, and processes that interact with one another to generate and reinforce inequities among racial and ethnic groups” (Gee & Ford, 2011, p. 116).
The history of financial capability and asset building policies is crucial to understanding how structural racism fuels contemporary socioeconomic inequity. Race and gender are primary social factors that are linked to the history of economic oppression and exploitation among vulnerable groups, especially Black Americans, Latinx Americans, Native Americans, and women (Sherraden et al., 2018). Through racist laws and practices, these groups have been systematically denied or stripped of assets in multiple forms, such as self, land, natural resources, possessions, culture, and money (Anderton & Brauer, 2016; Dewees & Foxworth, 2013; Oliver & Shapiro, 2006). Further, federal policies that were designed to build financial capability and assets, such as the Homestead Act, Social Security, minimum wage, Homeowners’ Loan Corporation, and the G.I. Bill, disproportionately benefit white Americans, but often exclude communities of color (Geisler, 2011; Katznelson, 2005; Rothstein, 2014; Williams Shanks et al., 2015).
This history contributes to the unequal distribution of resources that continue to yield long-lasting effects on socioeconomic and health inequities. Racial residential segregation today is a manifestation of racist policies that produced and perpetuate socioeconomic and health disadvantages through differential access to education, employment, asset building opportunities, and health-promoting resources (Williams, 2001). Geography matters, as illustrated by large differences in life expectancy by zip code, reaching 20 to 30 years in some cases, even among communities adjacent to each other (Robert Wood Johnson Foundation, n.d.).
Like race, gender reflects access to resources, power, and privileges. Women have fewer socioeconomic resources, as is evident in wage and wealth gaps (Chang, 2010; Deere & Doss, 2006). Gender intersects with race, which leaves women of color in a particularly disadvantaged position in financial capability and asset holding (Goldin, 1990; Harbury & Hitchens 1977; Pearce, 1978). For example, from their inception, cash assistance policies limited Black mothers’ access, especially in southern states (Neubeck & Cazenave, 2001).
Socioeconomic Position, Financial Capability, and Health
Like race and gender, socioeconomic position (SEP) is a fundamental determinant of health. Furthermore, race is linked to SEP (Braveman et al., 2005; Nuru-Jeter et al., 2018). SEP is complex and multifactorial, and one size does not fit all (Braveman, 2005). The most used measures of SEP are income, education, and occupational status. Researchers have suggested that wealth is an important SEP measure; however, it is difficult to measure in practice (Braveman et al., 2005; Pollack et al., 2007; Williams & Collins, 1995). Williams & Collins (1995) observe that each SEP measure has advantages and limitations, and evidence shows that failure to measure SEP comprehensively may lead to overlooking or obscuring the contribution of SEP to health, such as the etiology of racial/ethnic disparities (Pollack et al., 2007).
The financial capability and assets-based policy structure actively create inequality based on SEP. For example, asset building tax subsidies disproportionately benefit middle to high income households (Steuerle et al., 2014; Steuerle, 2016). Nearly 80% of the benefits for the four largest asset-building tax incentives (for homeownership, financial investment, retirement saving, and education) go to households in the top income quintile (Greer & Levin, 2014). The amount of subsidies is large, exceeding cash assistance to low-income people (Sherraden, 1991).
The Present Study
In this paper, we propose that financial capability (financial literacy and financial access combined) is an important SEP indicator that is rooted in history and continues to shape SEP distribution in the population. The key question is, can financial capability affect health independent of other commonly studied SEP indicators, such as income and education? If the answer is yes, financial capability should be clearly defined, conceptualized, and operationalized(independent of frequently measured social determinants), and be incorporated into population health research.
Research Aims and Hypotheses
To address the research gap, this paper aims to reconceptualize financial capability in health research by strengthening the understanding of structural context. To achieve this, we measure financial capability holistically using a latent construct that combines financial literacy, financial education, and financial access. The key question of this paper is whether financial capability is an independent social determinant of health, while controlling for other socioeconomic factors. We hypothesize that after controlling for other common indicators, financial capability has a positive and statistically significant longitudinal association with health.
Methods
Data and Sample
This study uses data from the 2012 National Financial Capability Study linked with the 2012 and 2016 American Life Panel (ALP) Effects of the Financial Crisis Survey. In 2012, the National Financial Capability Study administered an additional online survey to a nationally representative sample selected within the ALP. The final sample of ALP mirrors the demographic compositions in NFCS in terms of race, age, and income composition (Angrisani et al., 2016). The ALP is a probability sample–based panel of persons aged 18 and above, undertaken within the RAND Labor and Population (Pollard & Baird, 2017). Since November 2008, ALP Effects of Financial Crisis Survey has asked a series of questions relevant to the economic crisis at regular intervals, including indicators of emotion and physical health (e.g., happiness, depression, life satisfaction). Although ALP is internet-based, the sample does not have selection bias due to lack of internet access by providing Web TV with Internet access subscriptions, and email accounts for those who did not have the internet (Hurd & Rohwedder, 2010). In this study, we combined those three data sources from ALP to get respondents’ financial capability measured in 2012 and health (measured in both 2012 and 2016). The final analytic sample size is 3,803.
Measures
Financial capability. All the financial capability indicators come from the 2012 National Financial Capability Study. Guided by the financial capability framework, we measure financial capability to include financial literacy, financial access, and financial education. The latent construct of financial capability consists of nine indicators, including financial access, measured by ownership of four financial products (checking account, saving account, retirement plan, and credit cards; Birkenmaier & Fu 2019), three ordinal measures related to subjective financial literacy (good at math, good at day-to-day financial matters, self-rated financial knowledge; Xiao et al., 2015), and the sum of correctly answered six financial literacy questions (Lusardi & Mitchell, 2007; 2008), and one binary measure of whether the respondent has received financial education (yes or no).
Health. Health measures are extracted from the ALP Effects of Financial Crisis Survey in 2012 and 2016. The latent construct of health is measured by five indicators, including life satisfaction, self-rated health, depression, worn out, and happiness (Hurd & Rohwedder, 2010; Hurd et al., 2014). Life satisfaction is measured by the question “Taking all things together, how satisfied are you with your life as a whole these days?” Responses range from 1 (very satisfied) to 5 (very dissatisfied). Self-rated health is assessed by “Would you say your health is excellent, very good, good, fair, or poor?” Depression is measured by the question “Overall in the last 30 days, how much of a problem did you have with feeling sad, low, or depressed? Responses range from 1 (none) to 5 (extreme). Lastly, worn out and happiness are assessed by “Overall in the last 30 days, how much of the time have you felt worn out / been a happy person? Responses range from 1 (all of the time) to 6 (none of the time). Health measured as a latent variable in 2016 was modeled as the key dependent variable in this study. The latent variable of health measured in 2012 was controlled for as a time-lagged variable in the analysis.
Covariates. Following the theoretical discussion on social determinants of health, we control for race/ethnicity, gender, and other common SEP indicators, namely income, education, and employment. Additionally, we control for age, marital status, number of children in the household, and insurance coverage. All covariates were measured in 2012.
Statistical Analysis
The structural equation modeling (SEM) approach examines measurement as well as relationships between financial capability and health. SEM allows researchers to model relationships across latent constructs by accounting for measurement errors (Kline, 2015). As the model chi-square is sensitive to larger sample size, multiple model fit indices, such as comparative fit index (CFI), Tucker-Lewis index (TLI), and root mean square error of approximation (RMSEA) with a 90% confidence interval (CI), were used to select appropriate SEM model (Wang & Wang, 2012). According to Hu & Bentler (1999), a good SEM model is evaluated by a non-significant chi-square, CFI and TLI > 0.90, and RMSEA < 0.05 with upper bound of the 90% CI < 0.08.
A measurement model of financial capability and health was conducted first to see if the model has a reasonable fit. In this study, we construct three latent variables of financial capability (in 2012) and health (both in 2012 and 2016). We model health variables longitudinally, correlating the residuals for the same item across time. To examine how financial capability affects health in a four-year span, we use lag SEM model by controlling for latent health in 2012. All the latent variables are controlled for covariates in the SEM analyses. Both factor loadings and paths were presented in standardized estimates, and standardized paths should be at least 0.20 to be considered meaningful (Chin, 1998). Additionally, the Cohen’s f2 (Cohen, 1988) was used to assess the effect size of the paths using the cutoff points for small (f2 ≥ 0.02), medium (f2 ≥ 0.15), and large effect (f2 ≥ 0.35). As missing occurred in covariates and cannot be imputed using full information maximum likelihood estimation, we created 20 multiple imputation data sets to impute the missing values, and the results are aggregated using Rubins’ rule (Rubin, 1987). As the items of financial capability and health involved binary and ordinal measurement, the weighted least square mean and variance (WLSMV) adjusted estimator is used. All the analyses are performed using Mplus 7.4.
Results
Table 1 presents the sample demographic characteristics. The proportion of females (58%) was slightly greater than males (42%). The mean age of the sample was 49 years. Non-Hispanic Whites take up 71%, whereas Non-Hispanic Black and Hispanics take up around 10% and 15%, respectively. Most respondents were married (54%), currently at work (60%), had health insurance (84%), and had education levels below bachelor’s degree (60%). About a quarter of the respondents had income less than $25,000.
Table 1.
Sample characteristics
| Variable | % or M (SD) |
|---|---|
| Gender | |
| Male | 41.69 |
| Female | 58.31 |
| Age | 48.66 (16.09) |
| Race/ethnicity | |
| Non-Hispanic White | 71.11 |
| Non-Hispanic Black | 10.36 |
| Hispanic | 14.60 |
| Other | 4.21 |
| Marital status | |
| Married | 54.11 |
| Not married (single, separated, divorced) | 45.89 |
| Education | |
| College degree | 40.50 |
| No college degree | 59.50 |
| Household income | |
| Less than $5,000 | 3.30 |
| $5,000–$7,499 | 1.77 |
| $7,500–$9,999 | 2.25 |
| $10,000–$12,499 | 2.82 |
| $12,500–$14,999 | 2.68 |
| $15,000–$19,999 | 4.49 |
| $20,000–$24,999 | 6.17 |
| $25,000–$29,999 | 5.78 |
| $30,000–$34,999 | 6.60 |
| $35,000–$39,999 | 5.16 |
| $40,000–$49,999 | 9.85 |
| $50,000–$59,999 | 9.46 |
| $60,000–$74,999 | 11.14 |
| $75,000 or more | 28.54 |
| Numbers of children | 0.84 (1.19) |
| Working status | |
| Working (self-employed, work full-time, work part-time) | 60.29 |
| Not at work (homemaker, student, employed, retired) | 39.71 |
| Whether have health insurance | |
| Yes | 83.80 |
| No | 16.20 |
Measurement Model of Financial Capability and Health
The measurement model including three latent variables of financial capability and health yielded a good model fit (χ2 = 1106.018, p < .001; CFI = 0.978; TLI = 0.974; RMSEA = 0.042 [90% CI: 0.040–0.045]), and all factor loadings (in standardized estimates) were all significant at 0.001 level. The result showed that financial capability was positively correlated with health status, but the effect is stronger in 2012 (r = .43, p < .001) than in 2016 (r = .31, p < .001). The correlation between health in the two time points was 0.80. Table 2 presents these findings.
Table 2.
Results of Measurement Model
| Latent variables | Items | Estimates (λ or r) |
|---|---|---|
| Financial capability (2012) | (C1) Checking account | 0.93*** |
| (C2) Saving account | 0.70*** | |
| (C3) Retirement plan | 0.74*** | |
| (C4) Having credit card | 0.58*** | |
| (C5) Day to day financial matters | 0.53*** | |
| (C6) Good at math | 0.33*** | |
| (C7) Financial knowledge | 0.51*** | |
| (C8) Financial literacy questions | 0.62*** | |
| (C9) Financial education | 0.33*** | |
| Health status (2012) | (H1a) Life satisfaction | 0.72*** |
| (H2a) Self-rated health | 0.62*** | |
| (H3a) Depression | 0.83*** | |
| (H4a) Worn out | 0.64*** | |
| (H5a) Happy | 0.86*** | |
| Health status (2016) | (H1b) Life satisfaction | 0.73*** |
| (H2b) Self-rated health | 0.63*** | |
| (H3b) Depression | 0.78*** | |
| (H4b) Worn out | 0.63*** | |
| (H5b) Happy | 0.85*** | |
| Correlation | ||
| Financial capability (2012) ↔ Health status (2012) | 0.43*** | |
| Financial capability (2012) ↔ Health status (2016) | 0.31*** | |
| Health status (2012) ↔ Health status (2016) | 0.80*** | |
Note. λ = item factor loading (standardized) for latent variables; r = standardized correlation. Results were estimated using weighted least square to correct the categorical nature of indicators. Model fit: χ2 = 1106.018, p < .001; CFI = 0.978; TLI = 0.974; RMSEA = 0.042 (0.040–0.045)
***p < .001
Structural Model for the Effect of Financial Capability on Health
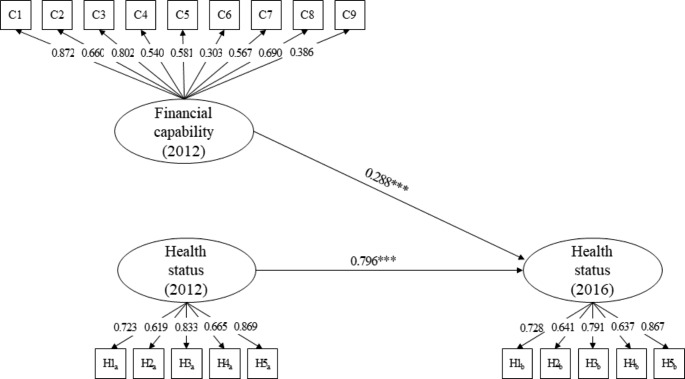
Figure 1 shows the results of the structural model of the effect of financial capability on health status based on 20 imputed data sets, and all the latent variables were controlled for covariates. The model also showed a good model fit (χ2 = 2358.014, p < .001; CFI = 0.953; TLI = 0.944; RMSEA = 0.041). Results showed that, controlling for the baseline health status, financial capability in 2012 was positively associated with health status in 2016 (β = 0.288, p < .001). The finding indicates that higher levels of financial capability led to better health status in four years, and the effect size for the effect of financial capability on health was between small to moderate level (Cohen’s f2 = 0.10).
Fig. 1.
Structural path model.
Note. Factor loadings for each latent construct were standardized, and all factor loading were significant at p < .001 level. Paths showed in figure were standardized estimates. All latent variables were controlled for covariates. Results were estimated using weighted least square (WLSMV) to correct the categorical nature of indicators with 20 imputed data sets. Model fit: χ2 = 2358.014***, p < .001; CFI = 0.953; TLI = 0.944; RMSEA = 0.041. ***p < .001
Table 3 presents the effects of covariates on latent variables of financial capability and health. Overall, age (β = 0.23, p < .001) and income (β = 0.44, p < .001) were positively correlated with financial capability. Furthermore, respondents who were male (β = 0.10, p < .001), had a college degree (β = 0.24, p < .001), were married (β = 0.06, p < .01), employed (β = 0.10, p < .001), and insured (β = 0.13, p < .001), were found to have higher levels of financial capability. Racial differences were also observed, as Non-Hispanic Black (β = −0.10, p < .001), Hispanic (β = −0.10, p < .001), and people in other racial groups (β = −0.04, p < .01) had lower levels of financial capability compared to Non-Hispanic White. As for the effects of covariates on health, findings show that gender, marital status, and income were correlated with health status. Males had better health status compared to their female counterparts at baseline (β = 0.07, p < .001). Married (β = 0.08, p < .01) and respondents with higher income (β = 0.25, p < .001) had better health at the baseline, but they had poor health in 2016.
Table 3.
Effects of Control Variables on Latent Variables of Financial Capability and Health Status
| Financial capability (2012) | Health status (2012) | Health status (2016) | |
|---|---|---|---|
| Latent variables | |||
| Financial capability (2012) | 0.29*** | ||
| Health status (2012) | 0.80*** | ||
| Control variables | |||
| Age | 0.23*** | 0.02 | −0.07 |
| Gender (ref: female) | 0.10*** | 0.07** | −0.05 |
| Race/ethnicity (ref: Non-Hispanic White) | |||
| Non-Hispanic Black | −0.10*** | 0.02 | 0.02 |
| Hispanic | −0.10*** | −0.01 | 0.02 |
| Other | −0.04** | 0.01 | −0.02 |
| Education (ref: no college degree) | 0.24*** | 0.03 | −0.05 |
| Marital status (ref: not married) | 0.06** | 0.08** | −0.09** |
| Employed (ref: not employed) | 0.10*** | 0.02 | 0.01 |
| Number of children | −0.04 | −0.04 | 0.02 |
| Income | 0.44*** | 0.25*** | −0.10* |
| Insured (ref: not insured) | 0.13*** | 0.03 | −0.05 |
Note. All the estimates were standardized estimates. Results were estimated using weighted least square (WLSMV) to correct the categorical nature of indicators with 20 imputed data sets
Model fit: χ2 = 2358.014***, p < .001; CFI = 0.953; TLI = 0.944; RMSEA = 0.041. ***p < .001
To summarize, we find that financial capability had a positive, longitudinal association with health, after controlling for other SEP and demographic factors, and lagged health. However, we did not find significant longitudinal associations between race, gender, and two other SEP indicators (education, and employment) and health. Income had a small yet negative association with health four years later.
Discussion, Implications, and Limitations
Using longitudinal data from the RAND American Life panel, we find that financial capability has a positive and longitudinal association with health, controlling for other SEP indicators. This study demonstrates that financial capability is an independent social determinant of health. It can be theoretically and conceptually defined, empirically measured, and can inform clinical interventions that may improve population health and well-being. The association between financial capability and health has profound implications for research, practice, and policy. Below, we discuss the implications and limitations of this study and future directions for research.
First, this study provides an empirical test of the relationship between financial capability and health. However, a limitation of this study is that it remains unclear whether the association is causal. There may be unobserved individual and structural factors not captured in the data used in this study—such as stressful life events, personality traits, and neighborhood effects—which could affect both respondents’ financial capability and their health. More empirical research should be conducted to examine whether the relationship between financial capability and health is causal. Data availability remains a primary challenge. Few datasets document both financial capability (especially the structural component) and health. Randomized controlled trials and quasi-experiments that improve financial capability could examine health impacts in addition to economic well-being. Panel surveys that examine financial capability and health should measure both financial capability and health to make research in this area possible.
Second, this study finds a positive and longitudinal association between financial capability and health. However, the nuances and mechanisms of the relationship are not addressed in this study because of data availability. Future research should test potential pathways and mechanisms to inform policy and practice. Theory and conceptual clarity play an important role in this regard. First, mediators between financial capability and health could help elucidate pathways and inform intervention. Empirical examinations should be guided by theories and mechanisms should be purposefully tested instead of only examining program input and expected measurable outcomes using a black box model. Second, given the theoretical framework and historical context of financial capability, it is highly likely that heterogeneous effects exist in the relationship between financial capability and health. Future research should seek to understand the potential moderating effects of race/ethnicity, gender, and other factors.
Third, the study has implications for conceptualization and measurements of financial capability in health studies. With regard to conceptualization, the impact of financial capability on health should be separated from more commonly used measures of socioeconomic indicators, such as income and education. Regarding measurement, we measured financial capability using a latent construct combining financial literacy and financial access. Whereas this approach is innovative by incorporating both individual and structural aspects of financial capability, one latent construct of financial capability precludes further examination of underlying mechanisms and the relative importance of various components of financial capability. To inform potential malleable policy levers, researchers should examine which aspect of financial capability should be targeted to improve health and wellbeing most effectively. Future research that evaluates financial capability should not only measure both financial literacy and financial access, but also model financial literacy and access as separate constructs. Financial capability is multidimensional and context-specific. Testing the nuance of subcomponents of financial capability and their relation to health can better inform actionable steps on how to improve financial capability to improve population health. For example, how to provide effective financial guidance and education, as well as how to make financial policies, products and services benefit vulnerable populations. Regarding health measures, a limitation of the current study is that we use self-reported health measures rather than clinical diagnoses in this study. Future research should consider moving beyond simple self-reported measures and consider adding clinical data to produce higher quality research evidence on the relationship between financial capability and health. To provide a more comprehensive picture of the health consequences of financial capability, researchers should examine an array of health outcomes.
Fourth, the study has implications for social work and public health practice. Based on these findings, social work and public health professionals should consider integrating financial capability and health services. For example, services could provide financial coaching, credit counseling, financial resources and guidance in clinic settings. Financial assessments could be integrated alongside health and psychological assessments into human service protocols, given the fundamental role of financial capability in shaping people’s physical and psychological health outcomes. It is important to know if clients have health insurance and if the health care is affordable. Furthermore, personnel serving low-income and other vulnerable populations in for-profit, nonprofit and public sectors should all receive financial capability content training and have the basic financial knowledge and professional capacity to be able to provide basic financial guidance.
Fifth, this study has policy implications. Future financial inclusion policies could help to achieve desirable outcomes that are beyond economic well-being. Implementation of FCAB policies could address upstream causes of health inequalities. Financial capability lies in both individual knowledge and skills, but also in the availability of financial policies, products, and services. Public health and social work professionals who seek to improve health and well-being should consider not only improving individual knowledge and skills, but also making financial policies, products, and services available, affordable, accessible, and appropriate. Friedline et al. (2020) recently reviewed research on families’ financial stress and well-being published in the Journal of Family and Economic Issues between 2010 and 2019. They recommend that future research should pay greater attention to the structural economy and economic environments.
Conclusion
This study provides a theoretical foundation for considering financial capability as an independent social determinant of health. Race is primary in this conceptualization. Indeed, socioeconomic and health inequities are rooted in historical socioeconomic injustices. We propose that financial capability is a separate construct from other SEP indicators, namely income, education, and employment.
This study is among the first efforts to empirically test the relationship between financial capability and health using a U.S. national sample. We find that controlling for other common SEP indicators and lagged health, financial capability is positively associated with health outcomes four years later. This paper suggests that financial capability is conceptually different from commonly used measures of SEP and can have multidimensional measurements that include both financial literacy and financial access.
Current policies and program efforts that aim to expand financial access and improve people’s financial knowledge and skills may have beneficial effects on health and well-being. Future policy and program evaluations should document health effects and test the relationship across diverse populations. Just as improving financial capability is not only changing individual financial behaviors, improving population health is not only changing individual health behaviors and medical care utilization. Both require the structural level change to reverse racial, socioeconomic, and health inequity. As Walters et al. (2016) stated, “health is not created in a clinic, and we cannot rely on traditional health services alone to heal the wrongs of history and persistent inequality” (p. 7). The current COVID-19 pandemic presents a timely opportunity for meaningful action by social work and public health professionals to advocate for continued and increased structural level interventions targeting financial capability to reverse inequality.
Acknowledgements
We are grateful for FCAB for all grand challenge network members across countries. We thank the Center for Social Development, the Financial Social Work Initiative, and FCAB Grand Challenge Network Leadership’s colleagues, including Margaret S. Sherraden, Julie Birkenmaier, Jin Huang, Jodi Frey, Christine Callahan, David Rothwell, Michael Sherraden, Gena Gunn McClendon, and Lissa Johnson for their leadership and continued support over the years. We thank Margaret S. Sherraden for her careful review and insightful comments on the manuscript. We thank Shenyang Guo for hands-on and effective methodology training on Structural Equation Modeling. In addition, we thank audiences from the FCAB 5th convening for their helpful feedback. Finally, we appreciate the reviewers’ comments, which improved an earlier version of this article.
Funding
The authors received no financial support for this research.
Data Availability
Data used in this research can be downloaded at: https://www.rand.org/research/data/alp.html.
Code Availability
NA.
Declarations
Ethics Approval
NA.
Consent to Participate
NA.
Consent for Publication
All authors have approved the manuscript and agree with its submission to the journal.
Disclosure of Potential Conflicts of Interest
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this research.
Research involving human participants and/or animals
Not applicable.
Informed Consent
Not applicable. This research utilizes secondary data.
Footnotes
This is one of several papers published together in Journal of Family and Economic Issues on the “Special Issue on the Financial capability and asset building”
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sicong Sun, Email: s-sun@ku.edu.
Yu-Chih Chen, Email: yuchih@hku.hk.
References
- Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Annals of the New York Academy of Sciences. 2010;1186(1):5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- Aguila E, Angrisani M, Blanco LR. Ownership of a bank account and health of older Hispanics. Economics Letters. 2016;144:41–44. doi: 10.1016/j.econlet.2016.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajefu JB, Demir A, Haghpanahan H. The impact of financial inclusion on mental health. SSM-Population Health. 2020;11:100630. doi: 10.1016/j.ssmph.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allmark P, Machaczek K. Financial capability, health and disability. Bmc Public Health. 2015;15:a243. doi: 10.1186/s12889-015-1589-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderton, C. H., & Brauer, J. (2016). Economic aspects of genocides, other mass atrocities, and their prevention. Oxford University Press
- Angrisani, M., Kapteyn, A., & Lusardi, A. (2016). The national financial capability study: Empirical findings from the American Life Panel survey. FINRA Investor Education Foundation. https://www.usfinancialcapability.org/downloads/NFCS_ALP_Report_Final.pdf
- Bennett JS, Boyle PA, James BD, Bennett DA. Correlates of health and financial literacy in older adults without dementia. BMC Geriatrics. 2012;12(1):a30. doi: 10.1186/1471-2318-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. Journal Of The American Medical Association. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annual Review of Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- Birkenmaier J, Fu QJ. Does consumer financial management behavior relate to their financial access? Journal of Consumer Policy. 2019;42(3):333–348. doi: 10.1007/s10603-019-09418-z. [DOI] [Google Scholar]
- Chang, M. (2010). Shortchanged: Why women have less wealth and what can be done about it. Oxford University Press
- Chin WW. Issues and opinion on structural equation modeling. MIS Quarterly. 1998;22(1):vii–xvi. [Google Scholar]
- Cho, S., Crenshaw, K. W., & McCall, L. (2013). Toward a field of intersectionality studies: Theory, applications, and praxis. Signs: Journal of Women in Culture and Society, 38(4), 785–810. 10.1086/669608
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates, Publishers
- Collins, P. H. (2000). Black feminist thought: Knowledge, consciousness, and the politics of empowerment. Routledge
- Collins, P. H., & Bilge, S. (2020). Intersectionality (2nd ed.). Polity Press
- Commission on Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determinants of health: Final report of the commission on social determinants of health. World Health Organization. https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1
- Crenshaw K. Mapping the margins: Identity politics, intersectionality, and violence against women. Stanford Law Review. 1991;43(6):1241–1299. doi: 10.2307/1229039. [DOI] [Google Scholar]
- Deere C, Doss CR. The gender asset gap: What do we know and why does it matter? Feminist Economics. 2006;12(1– 2):1–50. doi: 10.1080/13545700500508056. [DOI] [Google Scholar]
- Dewees, S., & Foxworth, R. (2013). The economics of inequality, poverty, and discrimination in the 21st century. Praeger
- Fong, R., Lubben, J., & Barth, R. P. (Eds.). (2017). Grand challenges for social work and society. Oxford University Press. 10.7312/columbia/9780231176682.001.0001
- Gee GC, Ford CL. Structural racism and health inequities: Old issues, new directions. Du Bois Review: Social Science Research on Race. 2011;8(1):115–132. doi: 10.1017/S1742058X11000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiger, H. J. (2006). Health disparities: What do we know? What do we need to know? What should we do?. In A. J. Schulz, & L. Mullings (Eds.), Gender, race, class, & health (pp. 261–288). John Wiley
- Geisler, C. C. (2011). Accumulating insecurity among illegal immigrants. In S. Feldman, C. Geisler, & G. A. Menon (Eds.), Accumulating insecurity: Violence and dispossession in the making of everyday life (pp. 240–260). University of Georgia Press
- Greer, J., & Levin, E. (2014). Upside down: Tax incentives to save and build wealth [CFED policy brief]. https://prosperitynow.org/sites/default/files/resources/Policy_Brief_-_Tax_Incentives.pdf
- Goldin, C. (1990). Understanding the gender gap: An economic history of American women. Oxford University Press
- Gyasi RM, Adam AM. Does financial inclusion predict a lower risk of loneliness in later life? Evidence from the AgeHeaPsyWel-HeaSeeB study 2016–2017. Aging & Mental Health. 2020;25(7):1254–1261. doi: 10.1080/13607863.2020.1786006. [DOI] [PubMed] [Google Scholar]
- Harbury C, Hitchens D. Women, wealth and inheritance. Economic Journal. 1977;87(345):124–131. doi: 10.2307/2231837. [DOI] [Google Scholar]
- Homan P, Brown TH, King B. Structural intersectionality as a new direction for health disparities research. Journal of Health and Social Behavior. 2021;62(3):350–370. doi: 10.1177/00221465211032947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooper MW, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. Journal Of The American Medical Association. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Hurd, M. D., & Rohwedder, S. (2010). Effects of the financial crisis and great recession on American households (NBER Working Paper Series No. w16407). National Bureau of Economic Research. 10.3386/w16407
- Hurd, M. D., Rohwedder, S., & Tassot, C. (2014). The impact of employment transitions on subjective wellbeing. https://www.rand.org/content/dam/rand/pubs/working_papers/WR1100/WR1127/RAND_WR1127.pdf
- Johnson E, Sherraden MS. From financial literacy to financial capability among youth. Journal of Sociology & Social Welfare. 2007;34(3):a7. [Google Scholar]
- Katznelson, I. (2005). When affirmative action was White: An untold history of racial inequality in twentieth- century America. W. W. Norton
- Kline, R. B. (2015). Principles and practice of structural equation modeling. Guilford
- Kondrat ME. Actor-centered social work: Re-visioning “person-in-environment” through a critical theory lens. Social Work. 2002;47(4):435–448. doi: 10.1093/sw/47.4.435. [DOI] [PubMed] [Google Scholar]
- Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. American Journal of Preventive Medicine. 1993;9:82–122. doi: 10.1016/S0749-3797(18)30666-4. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. doi: 10.2307/2626958. [DOI] [PubMed] [Google Scholar]
- Lusardi A, Mitchell O.S. Financial literacy and retirement preparedness: Evidence and implications for financial education. Business Economics. 2007;42(1):35–44. doi: 10.2145/20070104. [DOI] [Google Scholar]
- Lusardi A, Mitchell O. S. Planning and financial literacy. How do women fare? American Economic Review. 2008;98(2):413–417. doi: 10.1257/aer.98.2.413. [DOI] [Google Scholar]
- Markides KS, Coreil J. The health of Hispanics in the southwestern United States: An epidemiologic paradox. Public Health Reports. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- Meyer M. Is financial literacy a determinant of health? The Patient-Patient-Centered Outcomes Research. 2017;10(4):381–387. doi: 10.1007/s40271-016-0205-9. [DOI] [PubMed] [Google Scholar]
- Mitchell JP. Financial capability as a determinant of health. Journal of Personal Finance. 2020;19(1):67–79. [Google Scholar]
- Neubeck, K. J., & Cazenave, N. A. (2001). Welfare racism: Playing the race card against America’s poor. Psychology Press
- Nussbaum, M. C. (2001). Women and human development: The capabilities approach. Cambridge University Press
- Nussbaum, M. C. (2011). Creating capabilities. Harvard University Press
- Nussbaum, M. (2002). Capabilities and human rights. In De P. Greiff, & C. Cronin (Eds.), Global justice and transnational politics: Essays on the moral and political challenges of globalization (pp. 117–149). MIT Press
- Oliver, M. L. & Shapiro, T. M. (2006). Black wealth, White wealth: A new perspective on racial inequality. Taylor & Francis
- Pearce DM. The feminization of poverty: Women, work and welfare. The Urban and Social Change Review. 1978;11:28–36. [Google Scholar]
- Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annual Review of Sociology. 2015;41:311–330. doi: 10.1146/annurev-soc-073014-112305. [DOI] [Google Scholar]
- Pollard, M., & Baird, M. D. (2017). The RAND American life panel: Technical description.10.7249/RR1651
- Rubin, D. B. (1987). Multiple imputation for nonresponse in surveys. Wiley
- Robert Wood Johnson Foundation (2020). Life expectancy: Could where you live influence how long you live?https://www.rwjf.org/en/library/interactives/whereyouliveaffectshowlongyoulive.html
- Robeyns I. The capability approach: A theoretical survey. Journal of Human Development. 2005;6(1):93–114. doi: 10.1080/146498805200034266. [DOI] [Google Scholar]
- Rothstein, R. (2014). The making of Ferguson: Public policy and the root of its troubles. Economic Policy Institute
- Sen, A. (1993). Capability and well-being. In M. Nussbaum, & A. Sen (Eds.), The quality of life. Clarendon Press. 10.1093/0198287976.003.0005
- Sen, A. (1987). The standard of living: Lecture II, lives and capabilities. In G. Hawthorn (Ed.), The standard of living (pp. 20–38). Cambridge University Press
- Singh A, Kumar K, McDougal L, Silverman JG, Atmavilas Y, Gupta R, Raj A. Does owning a bank account improve reproductive and maternal health services utilization and behavior in India? Evidence from the National Family Health Survey 2015–16. SSM-Population Health. 2019;7:100396. doi: 10.1016/j.ssmph.2019.100396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherraden, M. S. (2013). Building blocks of financial capability. In J. Birkenmaier, J. Curley, & M. Sherraden (Eds.), Financial education and capability: Research, education, policy, and practice (pp. 3–43). 10.1093/acprof:oso/9780199755950.003.0012
- Sherraden, M., Birkenmaier, J., & Collins, J. M. (2018). Financial capability and asset building in vulnerable households: Theory and practice. Oxford University Press
- Sun S, Jackson A, Smith R, Hudson DL. Race at the forefront in social and economic inequities. Journal on Race Inequality and Social Mobility in America. 2020;2(1):a2. [Google Scholar]
- Sun S, Huang J, Hudson DL, Sherraden M. Cash transfers and health. Annual Review of Public Health. 2021;42:363–380. doi: 10.1146/annurev-publhealth-090419-102442. [DOI] [PubMed] [Google Scholar]
- Sherraden, M. W. (1991). Assets and the poor: A new American welfare policy. M.E. Sharpe
- Steuerle, C. E., Harris, B. H., McKernan, S. M., Quakenbush, C., & Ratcliffe, C. (2014). Who benefits from asset-building tax subsidies? Urban Institute. https://www.urban.org/research/publication/who-benefits-asset-building-tax-subsidies
- Steuerle, C. E. (2016). Prioritizing opportunity for all in the federal budget. Urban Institute. https://www.urban.org/sites/default/files/publication/80041/2000758-Prioritizing-Opportunity-for-All-in-the-Federal-Budget-A-Key-to-Both-Growth-in-and-Greater-Equality-of-Earnings-and-Wealth.pdf
- Taylor MP, Jenkins SP, Sacker A. Financial capability and psychological health. Journal of Economic Psychology. 2011;32(5):710–723. doi: 10.1016/j.joep.2011.05.006. [DOI] [Google Scholar]
- Walters, K. L., Spencer, M. S., Smukler, M., Allen, H. L., Andrews, C., Browne, T., Maramaldi, P., Wheeler, D. P., Zebrack, B., & Uehara, E. (2016). Eradicating health inequalities for future generations (Working Paper No. 19). http://aaswsw.org, https://grandchallengesforsocialwork.org/wp-content/ uploads/2016/01/WP19-with-cover2.pdf
- Wang, J., & Wang, X. (2012). Structural equation modeling: Applications using Mplus. John Wiley & Sons. 10.1002/9781118356258
- Williams, D. R. (2005). Patterns and causes of disparities in health. In D. Mechanic, L. B. Rogut, D. C. Colby, & J. R. Knickman (Eds.), Policy challenges in modern health care (pp. 115–134). Rutgers University Press
- World Health Organization. (n.d.). Constitution. https://www.who.int/about/governance/constitution
- Williams Shanks, T. R., Boddie, S. C., & Wynn, R. (2015). Wealth building in communities of color. In R. Wynn (Ed.), Race and social problems: Restructuring inequality (pp. 63–78). Springer Science Business Media. 10.1007/978-1-4939-0863-9_4
- Weida EB, Phojanakong P, Patel F, Chilton M. Financial health as a measurable social determinant of health. PloS One. 2020;15(5):e0233359. doi: 10.1371/journal.pone.0233359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21(1):349–386. doi: 10.1371/journal.pone.0233359. [DOI] [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports. 2001;116(5):404–416. doi: 10.1016/S0033-3549(04)50068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao JJ, Chen C, Sun L. Age differences in consumer financial capability. International Journal of Consumer Studies. 2015;39(4):387–395. doi: 10.1111/ijcs.12205. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used in this research can be downloaded at: https://www.rand.org/research/data/alp.html.
NA.