Abstract
Pancreatic pseudocyst is a well-known complication of both acute and chronic pancreatitis. Although extension into other anatomical sites is common, extension into the retrofascial space causing an iliopsoas abscess is exceedingly rare. Although its low incidence creates a diagnostic challenge for clinicians, early diagnosis is essential to prevent significant complications and poor patient outcomes. We present a case of iliopsoas abscess with unusual culture fluid growth in the setting of acute on chronic pancreatitis secondary to extension of a pancreatic pseudocyst. We also offer a brief review of the literature and pathophysiology of the condition.
Keywords: Infections, Gastrointestinal system, Infection (gastroenterology), Pancreatitis, Pancreas and biliary tract
Background
Acute pancreatitis is a relatively common condition with increasing worldwide incidence, noted to be as high as 3.67% in some studies.1 In untreated or significantly prolonged cases, sustained inflammation via enzymatic autodigestion of pancreatic parenchyma may result in fibrosis, stricture formation and irreversible structural damage resulting in chronic pancreatitis.2 Pseudocyst formation is a relatively common sequela of acute and chronic pancreatitis, especially in the setting of significant alcohol use, occurring up to 10%–26% and 20%–40%, respectively.3 However, although pseudocysts often extend into the lesser sac, retroperitoneum or mediastinum, extension into the retrofascial space resulting in iliopsoas abscess remains rare extremely rare.
Case presentation
A male patient in his 40s with an extensive past medical history of chronic pancreatitis with pseudocyst, cirrhosis with ascites, superior mesenteric vein and portal vein thrombosis, and alcohol use disorder presented for a 1-week history of epigastric and left lower quadrant abdominal pain and left flank pain associated with nausea, increased flatulence, and abdominal distension. Of note, the patient recently underwent paracentesis 4 months prior of which 750 mL of ascitic fluid was successfully removed. His surgical history includes a Roux-en-Y hepaticojejunostomy and open cholecystectomy for common bile duct stricture. On initial examination, the patient was tachycardic to 102 BPM but afebrile. He appeared emaciated, and palpation elicited severe tenderness in the epigastrium, left lower quadrant, and left flank. Splenomegaly was also present. Range of motion in the left lower extremity was limited on passive and active extension and flexion.
Investigations
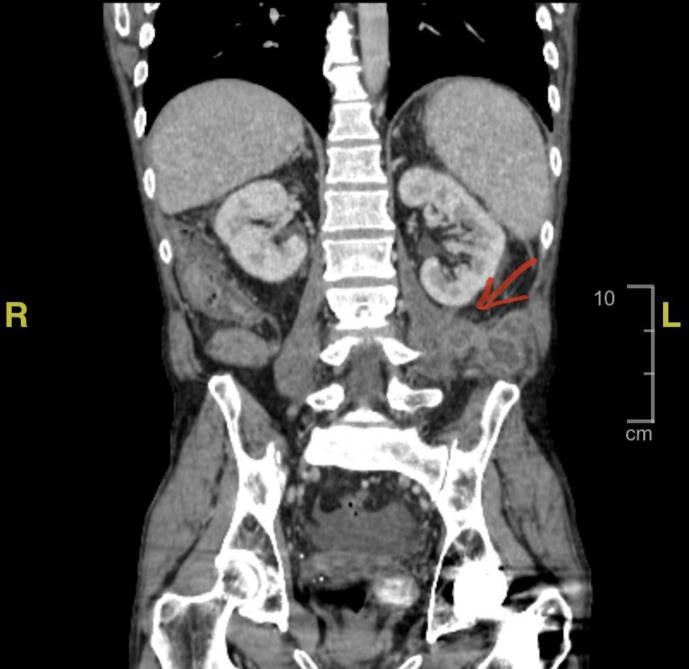
Initial laboratory testing revealed leucocytosis to 13.7 x 109/ L, with increased neutrophils, elevated serum lipase to 687 (25–125 IU/L), elevated lactic acid to 2.6 (normal range: 0.4–1.9 mmol/L) and elevated ALP to 773 (normal range: 20–130 U/L). Contrast-enhanced computed tomography (CT) of the abdomen and pelvis revealed inflammatory changes noted in the mesenteric pancreatic head and body (figure 1), with multiple well-circumscribed contrast-enhancing complex fluid collections consistent with pseudocyst extending as abscesses into the left lateral flank involving the left iliopsoas muscle group (figure 2). It was noted that these abscesses likely were slowly developing over the past few months.
Figure 1.

Axial contrast-enhanced CT showing inflammatory changes noted in the mesenteric pancreatic head and body consistent with acute pancreatitis (red arrow).
Figure 2.
Coronal contrast-enhanced CT demonstrating well-circumscribed enhancing complex fluid collections consistent with pseudocyst extending into the left lateral flank involving the left iliopsoas muscle group, the largest measuring 5 cm (red arrow).
Differential diagnosis
Given our patient’s history of chronic pancreatitis with pseudocyst, we suspected a recurrence based on his clinical symptomatology and investigative findings presented above. We also considered the possibility of a malignant or benign neoplastic process, especially in the setting of chronic alcohol abuse and his complex medical and surgical history. However, his reports of flank pain along with a clinical presentation of sepsis made us then suspect an infectious aetiology, with a presumed gastrointestinal, urinary or other retroperitoneal source. Other less common differential diagnoses in this setting included pancreatic necrosis or pseudocyst extension into the retroperitoneal space.
Treatment
We first initiated empiric antibiotic treatment with vancomycin, cefepime and metronidazole during his initial admission. After confirmation of the iliopsoas abscesses with CT imaging, ultrasound-guided percutaneous aspiration of the complex collection of the left flank was successfully achieved with an 8-French pigtail drain inserted into the left retroperitoneal/interfascial space tracking towards the subcutaneous space. 30 mL of gray-white purulent fluid was drained (figure 3), and fluid cultures were obtained. Although blood cultures remained negative, fluid cultures were positive for Mycobacterium abscessus, Enterobacter cloacae complex and Pseudomonas aeruginosa, which resulted in sepsis. He then began tailored antibiotic treatment with a complex regimen of intravenous amikacin, meropenem and clarithromycin for a duration of 3 months through a peripherally inserted central catheter and was eventually discharged with the percutaneous drain in place.
Figure 3.
Purulent fluid obtained following percutaneous drainage of iliopsoas abscess collections.
Outcome and follow-up
One week following discharge, our patient was unexpectedly readmitted for similar, yet milder complaints as his initial admission. After receiving consultation and recommendations from infectious disease specialists, we continued his antibiotic regimen as above. Postdrainage CT imaging acquired at this point was notable for mild resolution of the fluid complexes (figure 4). He was then discharged home after three inpatient days with the drain still in place and was instructed to continue these antibiotics as an outpatient. At the time of this submission on 2-month follow-up, the drain has been removed and our patient continues the same course of antibiotics. Fortunately, he has returned to normal daily activity and has not had any recent readmissions.
Figure 4.
Coronal contrast-enhanced CT postpercutaneous drainage, showing small residual rim-enhancing areas in lateral left psoas muscle measuring 1.8 cm and in superior left iliacus muscle measuring 1.9 cm, improved from previous images (red arrow).
Discussion
Pancreatic pseudocysts are well-associated with both acute and chronic pancreatitis, especially in the setting of alcohol use.3 The pathophysiology involves pancreatic enzyme extravasation into the biliary system, resulting in the accumulation of fluid collections with necrotic debris and granulation tissue, which may lead to permanent fibrosis.4 In previous cases, pseudocysts have extended beyond the retroperitoneum via contiguous or haematogenous spread to form collections in the psoas region requiring percutaneous drainage.5–8
To our knowledge, retrofascial extension of pseudocyst to cause iliopsoas abscess in this acute setting remains extremely rare and has only been described in a few case reports.9 10 The gold standard treatment remains percutaneous drainage, which was successfully achieved in these cases, followed by appropriate antibiotic therapy. Although iliopsoas abscess typically presents insidiously with back, flank, or abdominal pain in up to 92% of cases and with fever in 11% of cases,11 it may not immediately be considered in the initial differential diagnosis, especially during this unusual presentation in the setting of pancreatitis.
In a large community-based study, 27% of iliopsoas abscesses were found to be polymicrobial while only 7% contained Enterococcus spp.11 Furthermore, primary iliopsoas abscesses were fatal in 2.4% of patients, with percentages increasing as high as 19% in secondary abscesses.12 Our case is a unique contribution to the literature not only due to this rare extension and sequelae of the pseudocyst, but also because of the unusual microbiological composition of Mycobaterium abscessus, Enterococcus spp. and Pseudomonas aeruginosa present in the fluid collection.
The presence of Mycobacterium tuberculosis in soft tissue abscesses is well-described, typically in very immunocompromised patients worldwide, but this remains uncommon in the Western Hemisphere.12–15 However, M. abscessus is a non-tuberculosis mycobacterium often introduced nosocomially and is typically seen in pulmonary, central nervous system and skin and soft tissue infections (SSTIs). Though its incidence in SSTIs is increasing in the setting of cosmetic and nosocomial procedures, its relative rarity may pose problems for clinicians. Early detection is essential because it is often highly resistant to disinfectants and commonly used antibiotics, hence requiring very targeted therapies.13
Presumed contiguous spread of pseudocyst contents into the retrofascial space likely was complicated by the introduction of these rare bacteria to result in the formation of this iliopsoas abscess. Multiple inciting factors included our patient’s prolonged history of chronic pancreatitis with pseudocyst, recent history of paracentesis in the nosocomial setting,13 and his immunocompromised state resulting from concomitant cirrhosis.16 A long course of tailored intravenous antibiotic regimen of amikacin, clarithromycin and meropenem following percutaneous drainage remains the suggested antibiotic course for this pathogen, although side effects are common, and the doses or regimen may often require adjustment.17
Patient’s perspective.
During this time, I was experiencing the same pains in the centre of my abdomen as I was during prior episodes of pancreatitis. However, I was also feeling severe pain in the left side of my lower back, and I also was feeling quite nauseous. With my complex medical history, I was extremely concerned about a malignancy, severe infection, or other serious complication, so I immediately sought medical attention. I received excellent care and attention, which helped ease my worries, especially after the doctors ruled out a malignancy. After learning about the severity and rarity of the abscesses as a complication of my underlying conditions, I was hesitant at first to undergo the drainage procedure, but the team quickly reassured me and did a fantastic job. I began to feel improvement in my symptoms as quickly as the next day, although I did experience pain around the incision for 1 week after the intervention. It was difficult at first to adjust to the drain in place, and I had to alter my activities and not perform any heavy lifting or strenuous exercise. I did experience a readmission after I experienced a fever and more pain, which was quite worrisome for me. However, the team again gave me excellent care. The drain eventually was removed about 10 days after I was discharged from the hospital. At the time of this writing, I also remain on the recommended antibiotics which I am receiving at home through a PICC line. During every step, the physicians made me feel more at-ease, and they continue to follow-up with me to assess for any further complications.
This narrative was written by the patient. No translation was necessary.
Learning points.
Extension of a pancreatic pseudocyst into the retrofascial space causing iliopsoas abscess is an extremely rare sequela of acute or chronic pancreatitis.
In the setting of an immunocompromised patient with prior gastrointestinal comorbidities and procedural interventions, unusual microbiota may be introduced.
We emphasise that awareness, early suspicion and diagnosis are essential to mitigate future complications, include septic shock, preventable morbidity and mortality from recurrent readmissions, and widespread outbreak of this highly resistant bacteria.
Footnotes
Contributors: JDM, TP and VVQ contributed to conception and design of the study and manuscript. JDM drafted the original manuscript and performed the critical revisions. JDM, TP and VVQ contributed to the acquisition, analysis and interpretation of the data and the literature review. SI, TP and VVQ contributed by offering clinical guidance and expertise through the writing process and editing of the manuscript. JDM, TP, VVQ and SI reviewed the final manuscript and agree to its submission and publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Iannuzzi JP, King JA, Leong JH, et al. Global incidence of acute pancreatitis is increasing over time: a systematic review and meta-analysis. Gastroenterology 2022;162:122–34. 10.1053/j.gastro.2021.09.043 [DOI] [PubMed] [Google Scholar]
- 2.Brock C, Nielsen LM, Lelic D, et al. Pathophysiology of chronic pancreatitis. World J Gastroenterol 2013;19:7231–40. 10.3748/wjg.v19.i42.7231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andalib I, Dawod E, Kahaleh M. Modern management of pancreatic fluid collections. J Clin Gastroenterol 2018;52:97–104. 10.1097/MCG.0000000000000940 [DOI] [PubMed] [Google Scholar]
- 4.Habashi S, Draganov PV. Pancreatic pseudocyst. World J Gastroenterol 2009;15:38–47. 10.3748/wjg.15.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aswani Y, Anandpara KM, Hira P. Extension of pancreatic pseudocyst into psoas muscle in a setting of acute pancreatitis. Case Rep Child Meml Hosp Chic 2015;2015:bcr2014207822. 10.1136/bcr-2014-207822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doole E. A case of pancreatic pseudocyst as a rare cause of a cystic lesion within the psoas muscle. J Surg Case Rep 2021;2021:rjab499. 10.1093/jscr/rjab499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tajima Y, Mishima T, Kuroki T, et al. Huge pancreatic pseudocyst migrating to the psoas muscle and inguinal region. Surgery 2009;145:341–2. 10.1016/j.surg.2007.10.013 [DOI] [PubMed] [Google Scholar]
- 8.Alvarez-Castells A, Comet R, Alvarez-Moro J, et al. Psoas muscle pancreatic pseudocyst: CT--US diagnosis and percutaneous drainage. Gastrointest Radiol 1989;14:229–32. 10.1007/BF01889204 [DOI] [PubMed] [Google Scholar]
- 9.Harish K, Thomas V, Kumar S, et al. Infected pseudocyst in tropical pancreatitis presenting as psoas abscess. Indian J Gastroenterol 2006;25:260–1. [PubMed] [Google Scholar]
- 10.Hoţoleanu C, Bheecarry K. A rare presentation of a relatively common disease: psoas abscess as a complication of chronic pancreatitis. Rom J Intern Med 2014;52:50–2. [PubMed] [Google Scholar]
- 11.Ouellette L, Hamati M, Flannigan M, et al. Epidemiology of and risk factors for iliopsoas abscess in a large community-based study. Am J Emerg Med 2019;37:158–9. 10.1016/j.ajem.2018.05.021 [DOI] [PubMed] [Google Scholar]
- 12.Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J 2004;80:459–62. 10.1136/pgmj.2003.017665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee M-R, Sheng W-H, Hung C-C, et al. Mycobacterium abscessus complex infections in humans. Emerg Infect Dis 2015;21:1638–46. 10.3201/2109.141634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.López VN, Ramos JM, Meseguer V, et al. Microbiology and outcome of iliopsoas abscess in 124 patients. Medicine 2009;88:120–30. 10.1097/MD.0b013e31819d2748 [DOI] [PubMed] [Google Scholar]
- 15.Vasigh M, Karoobi M, Montazeri M, et al. Isolated psoas abscess caused by Mycobacterium tuberculosis: A rare case report. Clin Case Rep 2022;10:e05823. 10.1002/ccr3.5823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noor MT, Manoria P. Immune dysfunction in cirrhosis. J Clin Transl Hepatol 2017;XX:1–9. 10.14218/JCTH.2016.00056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Novosad SA, Beekmann SE, Polgreen PM, et al. Treatment of Mycobacterium abscessus infection. Emerg Infect Dis 2016;22:511–4. 10.3201/eid2203.150828 [DOI] [PMC free article] [PubMed] [Google Scholar]