Abstract
Purpose
The objective of this meta-synthesis was to identify, appraise, and synthesize patients and provider’s experiences while using telemedicine in cancer care during the COVID-19 pandemic.
Methods
The databases Medline, Embase, Cinahl, PsycInfo, Web of Science, and other related databases were searched. Reviewers followed the Joanna Briggs Institute (JBI) meta-aggregation method to identify categories and synthesized findings and to assign a level of confidence to synthesized findings. The listed quotations and the original author interpretations were synthesized using MAXQDA software.
Results
Nineteen studies were included in the meta-synthesis. Three synthesized findings emerged from 243 primary findings: telemedicine assists but cannot be a substitute for face-to-face appointments in a health care crisis and in the provision of routine care to stable patients with cancer, infrastructural drivers and healthcare provider’s support and attention affect patients’ experiences and feelings about telemedicine, and patients who use telemedicine expect their health care providers to devote enough time and consider emotional needs, the lack of which can develop a negative response. The methodological quality of the studies ranged between 4 and 10, and the overall level of confidence of the synthesized findings was determined to be low and medium.
Conclusion
The findings from this meta-synthesis gave a new insight to promoting the safe and evidence-based use of telemedicine during the current pandemic and future emergencies.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00520-022-07415-6.
Keywords: Telemedicine, Cancer, COVID-19, Qualitative research, Meta-synthesis
Introduction
Telemedicine includes any medical activity that is provided from a distance with the patient. The terms telehealth and e-health go beyond medical activities and include political and managerial content of the care [1]. Telemedicine is mainly introduced for its improved accessibility and reduced health care costs; however, concerns about the quality of care as well as organizational and bureaucratic difficulties still remain about this technology [2]. Telemedicine technology, despite having significant barriers as infrastructure, organizational support, and patient literacy, has been expanded in numerous areas such as cardiology, psychiatry, infectious disease, and oncology [3, 4].
In recent decades, the role of telemedicine has become increasingly important due to its advantages in the remote care of long-distance patients. This role multiplied with the appearance of the novel coronavirus diseases (COVID-19) and the importance of social distance and speeding up the treatment and care of patients. The US health system, which had already implemented telemedicine programs, was one of the first countries to respond to COVID-19 by leveraging these programs [5]. Telemedicine use in the USA in cancer care during COVID-19 expanded from less than 20 to 72% [6]. Most countries, however, do not have a framework to integrate telemedicine in emergencies. For example, the National Health Service (NHS) in Italy does not include telemedicine in the essential levels of care granted to all citizens [7].
Health systems with telemedicine assured continuity of care during pandemic orders as social distancing and “stay-at-home” [8]. This is important for not only COVID-19-infected people, but also for those elderly or with an underlying disease, that receive continued care without being at the risk of exposure to infected patients [9]. The possible delay in giving face-to-face diagnostic or treatment services for patients with cancer due to COVID-19 exposure risk and the probable increase in the number of patients with cancer after the outbreak due to this delay raise a critical concern for the health system [10].
COVID-19 is not the first pandemic, nor the last one it could be. However, the lessons learned from this outbreak about integrating telemedicine into the health systems should be taken into account for future health care emergencies. This meta-synthesis was conducted to provide patient’s experience of receiving telemedicine and health care provider’s experience of providing virtual care during the COVID-19 pandemic to promote evidence-based use of telemedicine for the current and future outbreaks.
Methods
The current study was a systematic review and meta-synthesis of the qualitative literature.
Inclusion criteria
Types of participants
This meta-synthesis included patients, caregivers (who are in the home helping a patient), and health care providers with any professional background who use and provides cancer care through telemedicine during the COVID-19 pandemic.
Phenomena of interest
The current meta-synthesis considered studies that described experiences facing telemedicine use for cancer care during the COVID-19 pandemic. Any medical activity for patients with cancer that was provided from a distance including audio-visual visits or phone calls was considered as telemedicine.
Context
Qualitative studies conducted in health care settings worldwide were included.
Types of studies
This meta-synthesis considered qualitative studies with all methodologies that include but are not limited to designs such as phenomenology, ethnography, case studies, grounded theory, and qualitative components of mixed-method studies. Also, we included qualitative data reported in the quantitative analyses.
Search strategy
The search strategy aimed to consider only published studies. A preliminary limited search of MEDLINE was undertaken to develop a search strategy. The main keywords for search, based on the research question, were telemedicine, telehealth, e-health, cancer, COVID-19, and SARS-CoV-2. Based on the main identified keywords, both free text with their synonyms and controlled vocabularies were searched across the included databases. The reference list of all the included studies was screened for any additional research.
This review was limited to studies published in English. The search strategy was limited to studies published between December 2019 and June 2021, since the emergence of COVID-19 was December 2019.
Information sources
The following databases were searched: MEDLINE (via Ovid), Embase, Pubmed, Cinahl (via Ebsco), PsycInfo (via Ebsco), Scopus, ISI Web of Knowledge, and Cochrane Library. Google Scholar was searched for any possible related articles. The search strategy was limited to studies published between December 2019 and June 2021, since the emergence of COVID-19 was December 2019. A full search strategy in Medline and Embase is available in Appendix 1.
Study selection
After collating and uploading all the identified citations into the Endnote X8 software, we removed duplicates. Two independent reviewers screened the titles and abstracts based on the inclusion criteria for the review. The studies that met the inclusion criteria were retrieved in full and assessed in detail.
Assessment of methodological quality
Two independent reviewers assessed included studies for methodological quality using JBI-Qualitative Appraisal Instrument [11]. Any disagreements between the reviewers were resolved through discussion, and if it did not help, they were referred to the third reviewer. The reviewers considered the papers with a score of seven and above as high-quality papers.
Data extraction
We used the standardized data extraction tool from JBI [11] to promote the extraction of similar data from all of the included studies. Data extraction in a meta-aggregation is a multi-phase process. The first phase considered the general details of papers including, study citation, study population, phenomena of interest, research methodology, the context of the study (clinical, cultural, and geographical), study methods (i.e., for data collection, data analysis, and sampling methods), study setting, and where applicable telemedicine platform. The second phase of the meta-aggregation data extraction included extracting findings from the results of the included studies along with their supporting data (e.g., a participant voice, or fieldwork observations, or other data). Quotations and primary author’s interpretations were transferred to the MAXQDA software (version.10) and further analyzed using open coding to develop the categories. The preliminary codes were then grouped and categorized according to their meanings, similarities, and differences, resulted in themes.
Level of credibility
Regarding the JBI manual for evidence synthesis [11], we allocated a level of credibility based on our perception of the degree of support each illustration offers for the specific finding it is associated with. The three levels of credibility included “unequivocal” if findings accompanied by an illustration that is beyond reasonable doubt and therefore not open to challenge, “credible” if findings accompanied by an illustration lacking clear association with it and consequently open to challenge, and “not supported” if the findings were not supported by the data. Findings with a “not supported” level of credibility were not included in the meta-synthesis; however, we reported their main characteristics and main findings in the related appendices.
Data synthesis
Data synthesis in a meta-aggregative review requires a three-step process. After extracting all findings from papers with an accompanying illustration and allocating a level of credibility, we grouped these findings based on their concepts and developed categories. Then, we developed synthesized findings based on the categories as the last phase of data synthesis. One of the reviewers extracted findings and developed categories, which were then checked for accuracy by other reviewers. We developed the synthesized findings through a consensus process between reviewers.
Assessing certainty in the findings
The final synthesized findings were graded according to the ConQual approach [12] for establishing confidence in the output of qualitative research synthesis. In the ConQual approach, each paper is graded for “dependability,” and “credibility.” The dependability score is based on the scores of five questions (2, 3, 4, 6, and 7) from the critical appraisal checklist [11]. The final ConQual score was then determined due to the levels of dependability and credibility.
Results
The process of study inclusion
We identified 1646 articles in the initial database search. After excluding articles form title and abstract, 27 were retained for investigation through full-texts. During data extraction, further five papers were excluded. The reasons for exclusion in this phase were as the following: the language of the article was not English [13], the articles did not have an original finding [14, 15], it was a conference abstract [16], and full text of the article was not available (the full text would be published online on October 2021) [17].
All of the 22 final qualitative studies were included in the meta-synthesis process except three [18–20], due to the “not supported” level of credibility in all of its findings. Figure 1 shows the PRISMA flowchart.
Fig. 1.
PRISMA flow diagram
Methodological quality of included studies
Table 1 indicates the results of methodological appraisal of included studies. The final score of methodological quality for the included studies in the current meta-synthesis appeared in the range of 4 [21] to 10 [22]. Although authors considered studies with a score of seven and higher, as a high-quality study, studies with a score of less than seven were not excluded from the final synthesis. However, the dependability scores in the final ConQual table reflect this issue and imply for users of this study about the finding’s total scores. Question number 6 in the quality appraisal instrument, which indicated “the statement locating the researcher culturally or theoretically,” was fully considered in only one study [22]. Also, question number 7 that implied “the influence of the researcher on the research and vice-versa” was addressed in three studies [22–24].
Table 1.
Critical appraisal results for included studies using the JBI-Qualitative Critical Appraisal Checklist
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alshamrani | Y | Y | Y | N | Y | U | U | N | Y | Y | 6 |
| Calton | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Colomer-Lahiguera | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Curigliano | Y | Y | Y | Y | Y | U | U | N | Y | Y | 7 |
| Dalby | Y | Y | Y | N | Y | U | U | Y | Y | Y | 7 |
| Di Lala | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Dieperink | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Drury | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | 9 |
| Franchini | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | 9 |
| Fraser | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Grossheim | Y | Y | U | N | N | U | U | U | Y | Y | 4 |
| Jazieh | Y | Y | Y | Y | Y | U | U | N | Y | Y | 7 |
| Krok-Schoen | Y | Y | Y | Y | Y | U | U | N | Y | Y | 7 |
| Lopez | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Olabumuyi | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Triantafillou | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Wiener | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
| Yim | Y | Y | Y | N | N | U | U | N | Y | Y | 5 |
| Zhang | Y | Y | Y | Y | Y | U | U | Y | Y | Y | 8 |
Q1. Congruity between the stated philosophical perspective and the research methodology. Q2. Congruity between the research methodology and the research objectives. Q3. Congruity between the research methodology and the methods used to collect the data. Q4. Congruity between the research methodology and the representation and analysis of data. Q5. Congruity between the research methodology and the interpretation of results. Q6. Statement locating the researcher culturally or theoretically. Q7. The influence of the researcher on the research, and vice-versa, is addressed. Q8. Participants, and their voices, are represented adequately. Q9. Research is ethical. Q10. Conclusions appear to flow from the analysis or interpretation of the data.
Main characteristics of the included studies
The studies included a total of 684 health care providers and 273 patients. Providers were leaders of cancer care centers, home care professionals, nurses, social workers, oncologists, geriatricians, advanced practice providers, case managers, dietitian, pharmacists, administrator/program leadership, navigators, physiatrists, occupational therapists, physiotherapists, kinesiologists, neuropsychologist, and dermatologists with different oncology background of medical oncology, radiation oncology, surgery, laboratory medicine, psychology, and research.
The patients’ population included one patient advocate, 16 caregiver of patients with cancer, 256 patients, and cancer survivors of lung cancer, breast cancer, colorectal cancer, head and neck cancer, and melanoma. Furthermore, one of the included studies [25] explored the experiences of patients, which were reflected in 230 online forum posts.
Three of the studies [26–28] used open-ended questions within a cross-sectional quantitative study. Three other studies [22, 29, 30] had a mixed-method design. Others had different descriptive approaches or did not report the qualitative methodology except for one grounded-theory [24]. Five of the studies collected data through a panel discussion of experts [15, 31–34]. Also, 11 studies used semi-structured interviews, all conducted by telephone [18–20, 22–24, 29, 35–38]. Data analysis in the included studies was conducted using thematic analysis [20, 22–25, 36, 38], content analysis [37], framework analysis [30], and rapid qualitative analysis [29]. Appendix 2 indicates the main characteristics of included studies.
Main findings of the review
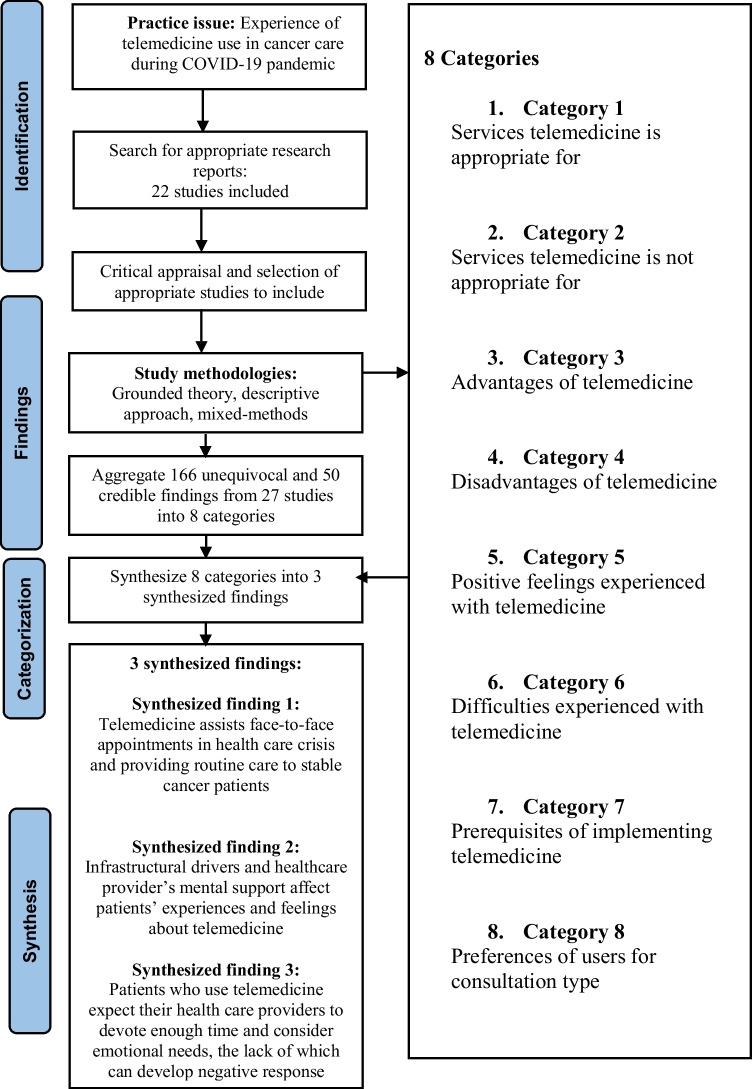
A total of 243 primary findings were extracted from the 22 included studies with the credibility levels as below: 166 unequivocal, 50 credible, and 27 not supported. The primary findings were categorized based on their concepts in eight categories of services telemedicine is appropriate for, services telemedicine is not appropriate for, advantages of telemedicine, disadvantages of telemedicine, positive feelings experienced with telemedicine, difficulties experienced with telemedicine, prerequisites of implementing telemedicine in a health system, and preferences of users for consultation type. Three synthesized findings emerged from these findings: telemedicine assists but cannot be a substitute for face-to-face appointments in a health care crisis and in the provision of routine care to stable patients with cancer, infrastructural drivers and healthcare provider’s support and attention affect patients’ experiences and feelings about telemedicine, and patients who use telemedicine expect their health care providers to devote enough time and consider emotional needs, the lack of which can develop a negative response. Appendixes 3 and 4 indicate the main findings and categories of the review with illustrations and levels of credibility and dependability. Figure 2 shows the meta-aggregative overview flowchart.
Fig. 2.
Meta-aggregative overview flowchart
Synthesized finding 1: Telemedicine assists but cannot be a substitute for face-to-face appointments in a health care crisis and in the provision of routine care to stable patients with cancer
This synthesized finding was aggregated from three categories. The category of “services telemedicine is appropriate for” includes findings from the primary studies for which telemedicine was perceived to be appropriate. These services mainly included primary care for patients with cancer, follow-up visits, and outpatients. One of the participants in the study by Wiener [28] mentioned that “It works well for some outpatients and there are some benefits of seeing them in their own home and not being interrupted by others walking into their hospital room or demanding their time in the clinic setting.” Also, one of the health care providers in the study by Triantafillou [37] told that “But if there are other visits, follow-ups, that the doctor thinks can be done by telemedicine and the patient agrees, then it would be fine.” A caregiver in one of the included studies [30] declared, “My husband is in a wheelchair and on a ventilator, video appointments avoid having to transport him for a visit.”
On the other hand, the category “services telemedicine is not appropriate for” indicated that telemedicine was not suitable for the first appointments and postoperative appointments. Also, telemedicine was not suitable for children and those patients with cancer whom are in complex settings and conditions, for example, those who are in ICU, having disease relapse or progression and patients with cancer metastatic. As one of the participants in the study by Curigliano [33] said that: “Patients with complex cancer needs should be considered for face-to-face consultation.” One of the participants in the study by Dalby [35] declared, “It was her first appointment after her surgery and she really needed the doctor to see the breast surgery site. She did not know whether the healing was ok.” Besides, findings showed that face-to-face visits were appropriate for the first appointments, since most of these appointments carry key cancer-related care.
The category “preferences of users for consultation type” included findings that directly mentioned by participants, whether they preferred telemedicine or face-to-face appointments. The content analysis of this category indicated that 15 findings supported the use of telemedicine, 14 supported face-to-face appointments, and three supported both telemedicine and face-to-face visits. Some of the quotes in support of face-to-face appointments in the studies are as below: “I like going to the office and getting the scope. It’s extra reassurance,” “Telemedicine seems like it would be way better for me because I live far away, but I’m old school and like the personal touch,” and “Sometimes I do think the ‘old way’ is better. For me personally, there is something to be said about human connection and responding to nonverbal cues in person.” Quotes that support telemedicine use in the included studies are as following, “I would definitely use telehealth again as long as there wasn’t something that needs a thorough examination,” and “If telehealth enables some physicians not needing to come into the office as often or for as long hours, it could be beneficial. If you could improve physician's quality of care that would mitigate burnout.” The full list of quotes is indicated in Appendix 4 .
Synthesized finding 2: Infrastructural drivers and healthcare provider’s support and attention affect patients’ experiences and feelings about telemedicine
Three categories of positive feelings experienced with telemedicine, difficulties experienced with telemedicine, and prerequisites of implementing telemedicine composed this synthesized finding. The positive feelings in words of satisfied, comfortable, less stressed, friendly, calm, convenient, and empowered were all experienced and described by patients in the primary studies. One of the patients in the study by Calton [30] declared about telemedicine “It’s more comfortable. You can be in your pajamas with a cup of coffee if you want. If the doctor is running late, I can do other things at my leisure at home.” Also, one of the caregivers in the same study told, “This is very convenient and helpful.” Another caregiver in the same study thought that telemedicine was a cost-saving method, “I was astonished to find out that [the video visit] was at no cost to us. It saved significant expense because it saved a drive, food, and a hotel for 2 nights.” A patient in the study by Dalby [35] notified that “Less stress knowing I did not have to leave home.” On the other hand, most of the problems experienced in telemedicine visits in terms of stressful, frustrated, awkward, and anxious were faced in discussing and understandings of pains or side effects. For example, one of the participants mentioned, “The pain has been unmanageable and phone calls have not helped him too much” [35]. One of the caregivers in the study by Triantafillou [37] declared, “His surgery is in the mouth so I was trying to position the phone and the light but that was hard.” A patient in the same study told, “I was anxious about connecting and how it was going to go but I had no problems. And I’m technology challenged.” One of the health care providers in an included study [24] mentioned, “Where no physical relationship with patients was possible, answering the phone calls and replying to messages were considered stressful.” Few problems were related to the hardware and infrastructures of telemedicine technology. For example, one of the patients in the study by Calton [30] said that “The technology might be hard for some people. Making the system as foolproof as possible would be a good idea. It was easy for me, but I can see how it could be frustrating for people with less tech experience.” A caregiver in the same study also declared, “Have an IT resource who can help patients and families who are having trouble, especially if people aren’t as familiar with video conferencing.”
In the category of “prerequisites of implementing telemedicine in a health system,” nearly all items focused on the information technology (IT) infrastructures related to telemedicine whether by patients, caregivers, or health care facilities. Based on the following quotes, by IT infrastructures, participants meant Wi-Fi connection, communication equipments such as smart phone or camera, and other related technologies. One of the health care providers in Wiener’s study [28] declared, “Socioeconomics obviously play a role–the family with access to the necessary technology (computer, tablet, smart phone), including a Wi-Fi connection are able to access telehealth more easily.” A health care provider in another study [34] mentioned, “Patients also need to have access to mobile devices with audio-visual capabilities, Internet access, and the ability to navigate the technology.” A caregiver in Calton’s study [30] told, “It requires that you have things at home to have a high quality video conference. Need good Wi-Fi, a good camera, a good screen” Countries in which studies of these findings were conducted included six African regions, Saudi Arabia, Colombia, the USA, and one international study.
Synthesized finding 3: Patients who use telemedicine expect their health care providers to devote enough time and consider emotional needs, the lack of which can develop a negative response.
This synthesized finding consisted of two categories advantages and disadvantages of telemedicine. As included studies assessed experiences of telemedicine use from different points of view (i.e., patients, caregivers, and healthcare providers), some aspects of telemedicine were considered to be an advantage from one point of view, while this was a disadvantage from another point of view. For example, lingual barriers were considered to be eliminated due to telemedicine. As one of the patients in the study by Dalby [35] mentioned, “Very good—she spoke to my daughter, as my English is not good.” However, the lingual barrier was perceived as a disadvantage of telemedicine because body language cannot be shown through the phone. One participant in the same study declared, “She felt that even through translation she was unable to get her side effects across to the doctor.”
Telemedicine was considered a time-consuming process for physicians while it was perceived to save time in six findings, three of which were from patients’ point of view. Radiation oncologists, focusing on better workflow with telemedicine, mentioned other three findings: [29] “I think workflow is better, there are few working parts. All I have to do is call the patient; there are no delays due to physically getting there.” In this study, the visits were categorized as in-person, telephone, or audiovisual/ telehealth; a telemedicine was conducted by the platforms of Doximity Dialer, FaceTime, and WhatsApp.
ConQual summary of findings
Analyzing the confidence level of synthesized findings, we found that the overall level of confidence was determined to be low for the synthesized findings 1 and 2 and medium for the synthesized finding 3. Table 2 shows the summary of findings that includes the major elements of the review and details how the ConQual score was developed for each synthesized finding.
Table 2.
ConQual summery of findings
| Meta-synthesis title: A meta-synthesis of experiences with telemedicine in cancer care during COVID-19 pandemic Population: Patients, caregivers, and health care providers with any professional background who uses and provides cancer care through telemedicine during the COVID-19 pandemic Phenomena of interest: Studies that described experiences facing in the telemedicine used for cancer care during COVID-19 pandemic Context: Qualitative studies conducted in health care settings worldwide were included | |||||
|---|---|---|---|---|---|
| Synthesized finding | Type of research | Dependability | Credibility | ConQual score | Comments |
| Telemedicine assists but cannot be a substitute for face-to-face appointments in health care crisis and providing routine care to stable patients with cancer | Qualitative | Moderate* | Downgraded 1 levels due to mix of unequivocal (U) and credible (C) findings: 52 U + 21 C | Low | Downgraded two levels due to dependability and credibility of primary studies |
| Infrastructural drivers and healthcare provider’s support and attention affect patients’ experiences and feelings about telemedicine | Qualitative | Moderate* | Downgraded 1 level due to mix of unequivocal (U) and credible (C): 64 U + 20 C | Low | Downgraded two levels due to dependability and credibility of primary studies |
| Patients who use telemedicine expect their health care providers to devote enough time and consider emotional needs, the lack of which can develop negative response | Qualitative | Moderate* | Downgraded 1 level due to mix of unequivocal (U) and credible (C): 50 U + 7 C | Medium | Downgraded one levels due to dependability and credibility of primary studies |
*For synthesized finding 1, of the 14 studies, three remained unchanged for dependability score, and 11 downgraded one level. So of the 14 studies, three had high level and 11 had moderate level of dependability and the total level of dependability for synthesized finding 1 is moderate. For synthesized finding 2, of the 14 studies, two remained unchanged for dependability score, one downgraded two levels, and 12 downgraded one level. So the total level of dependability for synthesized finding 2 is moderate. For synthesized finding 3, two of the studies remained unchanged for dependability score, eight downgraded one level, and one downgraded two levels. So the total level of dependability for synthesized finding 3 is moderate.
Discussion
We conducted the current meta-synthesis to assess experiences with telemedicine in cancer care during the COVID-19 pandemic. Using the meta-aggregation approach, we developed three synthesized findings. The first synthesized finding was “telemedicine assists but cannot be a substitute for face-to-face appointments in a health care crisis and in the provision of routine care to stable patients with cancer.” The second synthesized finding was “infrastructural drivers and healthcare provider’s support and attention affect patients’ experiences and feelings about telemedicine.” The last one included “patients who use telemedicine expect their health care providers to devote enough time and consider emotional needs, the lack of which can develop negative response.” A similar qualitative systematic review of cancer survivor’s experiences of telemedicine, using the thematic synthesis of findings, emerged three analytical themes of influence of telemedicine on the disrupted lives of cancer survivors, personalized care across physical distance, and a remote reassurance-a safety net of health care professional connection [39].
Results of the current meta-synthesis indicated that in a health crisis such as COVID-19, cancer patient’s preference of using telemedicine services was quite similar to that of face-to-face appointments. However, utilization of telemedicine, as a response to COVID-19, has been increased during the COVID-19 period [40]. The majority of patients with chronic liver disease at a tertiary care center in Italy indicated that they were satisfied and would be willing to continue telemedicine for their routine care during the COVID-19 pandemic, because it gave them the opportunity to continue their care with respect to social distancing rules [41]. Nevertheless, despite having critical advantages, telemedicine cannot replace traditional in-visits. The results of this meta-synthesis added to this evidence, suggesting that while telemedicine may not provide a qualified service as face-to-face appointments, it is preferred at the time of COVID-19. Also, participants’ narratives in the included studies of the current meta-synthesis reflect that they would rather choose video-based appointments to phone visits, showing that with improving IT infrastructures, policymakers in a health system can expand the use of these video-based telemedicine visits.
Telemedicine was found to be helpful in managing stable patients conducting follow-up visits in the current meta-synthesis. Similarly, telemedicine services were implemented for follow-up visits and screening for patients before admission to the hospital [41]. Also, telemedicine has been found to be a valuable option in the follow-up of patients with cancer during the pandemic [42–44]. Daily follow-up of hospitalized patients through video calls in medical rounds during this pandemic was found as one of the telemedicine applications in a scoping review [45]. Similar to the results of the current study, telemedicine was not a suitable option for new visits, resulting in lower patient satisfaction [46].
Inequity in access to telehealth due to different socioeconomic conditions was found in the current meta-synthesis as one of the barriers in implementing effective telemedicine services. Results of a cohort study conducted in the first phase of COVID-19 in the USA indicated that inequities existed in telemedicine use, in a way that older patients, Asian patients, and non-English-speaking patients had lower rates of telemedicine use [47]. Darrat and colleagues, in their study, found that socioeconomic disparities, including age, sex, median household income, insurance status, and marital status, had affected telemedicine use of patients during the COVID-19 pandemic [48]. Also, disparities in telemedicine use between respondents living in urban versus rural areas existed in the USA during this pandemic [49, 50]. Differences in the access to telemedicine services refer back to the context of health systems.
Infrastructures and prerequisites mentioned by the participants of the included studies focused mainly on IT-related factors and the existence of an organized team. Employing dedicated qualified personnel was found to have a critical role in the foundation for long-term sustainability and growth of telemedicine [51, 52]. Technology challenges with telemedicine were also consistent with previously reported findings [53, 54]. COVID-19 crisis was a turning point for countries with an appropriate framework for telemedicine services, to make them prepared and promote their telemedicine infrastructures for future pandemics or other healthcare crisis.
There was a mix of patient’s feelings in telemedicine communications. While some patients felt friendly, comfortable, and calm during phone calls, others reported that they were tendered, confused, frustrated, and stressful. Patients experienced a range of less stressful meeting via video consultations [55], to stressed, depressed, or anxious telemedicine visits before the COVID-19 pandemic [56, 57]. These different comments may relate to the health status of patients indicating that telemedicine can work successfully only if the provider team is aware of the needs and health status of the patients receiving these services. Also, the physical and psychological health of healthcare professionals due to fear of infection by coronavirus may lead to their mental health concerns, transferring to patients through phone calls.
Based on the findings of this study, some of the healthcare providers considered telemedicine a time-consuming process. It seems that financial reimbursement for providers of telemedicine services is helpful in attracting these providers and promoting telemedicine adherence in healthcare settings. Strong need for medical insurance coverage of telemedicine services was recommended by experts in one of the included studies of the current meta-synthesis, for providers to realize a return in investment. Results of a review study declared that rapid expansion of telemedicine because of the emergence of COVID-19 facilitated implementation of telemedicine in healthcare facilities, but the reimbursement of telemedicine services has been calmed down due to the economic downturn [58]. Findings from a study suggested clear guidelines for physicians providing telemedicine in order to ensure appropriate health insurance coverage for telemedicine encounters [59]. Also, inadequate funds were found to be a challenge faced in telemedicine in the COVID-19 pandemic [60].
Strengths and limitations
One strength of this meta-synthesis is that we recognized telemedicine advantages, disadvantages, prerequisites, and total preference of patients and providers through their lived experience, which is valuable data in improving healthcare services and is not possible to be captured by quantitative research and meta-analysis [61]. Also, we determined the level of confidence for each of the synthesized findings, which can be notified by policymakers and other users of this study to decide better based on the study findings. There were limitations in this study, as we limited the search strategy to English papers, and one study was excluded due to this inclusion criterion. Furthermore, due to the evolving literature on telemedicine use during the pandemic, it is likely that we have omitted publishing or peer-reviewed studies.
Conclusion
Patients and healthcare providers in the included studies of our meta-synthesis provided valuable insights on their experiences of telemedicine use. The results of this study highlighted that telemedicine is more effective in managing cancer patient’s primary health care needs and follow-up visits. In particular, this technology, although with minimal variation, was preferred in the current pandemic rather than face-to-face appointments, focusing on countries’ provision of infrastructures for implementing telemedicine in the current and future outbreaks. The results of this meta-synthesis allowed us to explore in-depth the experiences and feelings of telemedicine from different points of view. This, provides an unprecedented opportunity to develop integrated efforts from multiple stakeholders to better inform the design and improvement of telemedicine services in the health system context, which can facilitate not only a holistic approach to care but also reduces inequity in access to these services beyond the pandemic.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contribution
AM and SH supervised the whole study and revised the early draft of the manuscript. FS conducted the systematic search. NK and FS screened the included articles and assessed the methodological quality of studies. NK extracted data, conducted the meta-synthesis, and prepared the early draft of the manuscript. All authors confirmed the final manuscript.
Funding
This work was supported by Tabriz University of Medical Sciences.
Data availability
Not applicable.
Declarations
Ethics approval
This is a systematic review. The Research Ethics Committee of Tabriz University of Medical Sciences has confirmed that no ethical approval is required.
Consent to participate/publish
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wootton R. Telemedicine BMJ. 2001;323(7312):557–560. doi: 10.1136/bmj.323.7312.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hjelm N. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11(2):60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
- 3.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 4.Burbury K, Wong ZW, Yip D, Thomas H, Brooks P, Gilham L, et al. Telehealth in cancer care: during and beyond the COVID-19 pandemic. Intern Med J. 2021;51(1):125–133. doi: 10.1111/imj.15039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 6.Lonergan PE, Washington Iii SL, Branagan L, Gleason N, Pruthi RS, Carroll PR, et al. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: cross-sectional analysis. J Med Internet Res. 2020;22(7):e19322. doi: 10.2196/19322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6(2):e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20(1):1193. doi: 10.1186/s12889-020-09301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gatellier L, Shankar A, Dewi LKM, Hussain QM, Dendup Wangdi T, Sukumaran DB, et al. The impact of COVID-19 on cancer care in the post pandemic world: five major lessons learnt from challenges and countermeasures of major Asian cancer centres. Asian Pac J Cancer Prev Apjcp. 2021;22(3):681–690. doi: 10.31557/APJCP.2021.22.3.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.JBI. Joanna Briggs Institute Reviewers’ Manual: 2014 edition. AUSTRALIA: The Joanna Briggs InstituteThe University of Adelaide; 2014
- 12.Munn Z, Porritt K, Lockwood C, Aromataris E, Pearson A. Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol. 2014;14:108. doi: 10.1186/1471-2288-14-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Renault-Tessier E, Carton M, Meng MF, Milder M, Angellier E, Bouleuc C, et al. Experience of care and daily life during national sanitary confinement in patients followed and treated in Cancer Control Centers: the BaroCov Inquiry. Bull Cancer. 2021;108(5):481–489. doi: 10.1016/j.bulcan.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Di SaverioPata SF, GalloCarranoScorza GFA, Sileri P, et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020;22(6):625–634. doi: 10.1111/codi.15056. [DOI] [PubMed] [Google Scholar]
- 15.Olabumuyi AA, Ali-Gombe M, Biyi-Olutunde OA, Gbolahan O, Iwuji CO, Joseph AO, et al. Oncology practice in the COVID-19 pandemic: a report of a Nigerian expert panel discussion (oncology care in Nigeria during the COVID-19 pandemic) Pan Afr Med J. 2020;36:153. doi: 10.11604/pamj.2020.36.153.23662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eicher M, Bana M, Darnac C, Hellberg MN, Colomer-Lahiguera S. Oncology nurses’ experience in German and French-speaking Switzerland during the COVID-19 pandemic. Ann Oncol. 2020;31:S1138. doi: 10.1016/j.annonc.2020.08.2139. [DOI] [Google Scholar]
- 17.Booth C, Dyminski P, Rattray M, Quinn G, Nejadhamzeeigilani Z, Bickley L, et al. The case for mobile cancer care units: an NHS team’s experience. Br J Healthc Manag. 2021;27(5):152–155. doi: 10.12968/bjhc.2021.0024. [DOI] [Google Scholar]
- 18.Yim KM Yim RM Gaspard S MacDougall J Armstrong AW 2020 Strategies to maximize clinical efficiency while maintaining patient safety during the COVID-19 pandemic: an interview-based study from private practice dermatologists J Dermatolog Treat 1–4 [DOI] [PubMed]
- 19.Zhang B, Kim SY, Travers A, Bonaventura T. Impact of COVID-19 pandemic on multidisciplinary cancer workforce well-being: an Australian oncology centre experience. Asia Pac J Clin Oncol. 2020;16(SUPPL 2):46–47. [Google Scholar]
- 20.Wong BO Aslakson R Holdsworth LM Siden R Tabor H Verano M-R et al. 2021 Cancer care during Covid-19: a multi-institutional qualitative study on physician and patient perspectives on telemedicine Wolters Kluwer Health
- 21.Grossheim L, Ruff P, Ngoma T, Vanderpuye V, Mwango G, Ochieng P, et al. Cancer and COVID-19 experiences at African cancer centers: the silver lining. JCO global oncology. 2021;7:410–415. doi: 10.1200/GO.20.00564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dieperink KB, Ikander T, Appiah S, Tolstrup LK. The cost of living with cancer during the second wave of COVID-19: a mixed methods study of Danish cancer patients’ perspectives. Eur J Oncol Nurs. 2021;52:101958. doi: 10.1016/j.ejon.2021.101958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drury A, Eicher M, Dowling M 2021 Experiences of cancer care in COVID-19: phase 1 results of a longitudinal qualitative study [In Press] Int J Nurs Stud Adv 100030 [DOI] [PMC free article] [PubMed]
- 24.Franchini L, Varani S, Ostan R, Bocchi I, Pannuti R, Biasco G, et al. Home palliative care professionals perception of challenges during the Covid-19 outbreak: a qualitative study. Palliat Med. 2021;35(5):862–874. doi: 10.1177/02692163211008732. [DOI] [PubMed] [Google Scholar]
- 25.Colomer-Lahiguera S Ribi K Dunnack HJ Cooley ME Hammer MJ Miaskowski C et al 2021 Experiences of people affected by cancer during the outbreak of the COVID-19 pandemic: an exploratory qualitative analysis of public online forums Support Care Cancer 1–7 [DOI] [PMC free article] [PubMed]
- 26.Di Lalla V, Patrick H, Siriani-Ayoub N, Kildea J, Hijal T, Alfieri J. Satisfaction among cancer patients undergoing radiotherapy during the COVID-19 pandemic: an institutional experience. Current oncology (Toronto, Ont) 2021;28(2):1507–1517. doi: 10.3390/curroncol28020142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krok-Schoen JL, Pisegna JL, BrintzenhofeSzoc K, MacKenzie AR, Canin B, Plotkin E, et al. Experiences of healthcare providers of older adults with cancer during the COVID-19 pandemic. J Geriate Oncol. 2021;12(2):190–195. doi: 10.1016/j.jgo.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wiener L, Fry A, Pelletier W, Cincotta N, Jones B 2021 The impact of covid-19 on the professional and personal lives of pediatric oncology social workers J Psychosoc Oncol [DOI] [PMC free article] [PubMed]
- 29.Zhang H, Cha EE, Lynch K, Cahlon O, Gomez DR, Shaverdian N, et al. Radiation oncologist perceptions of telemedicine from consultation to treatment planning: a mixed-methods study. Int J Radiat Oncol Biol Phys. 2020;108(2):421–429. doi: 10.1016/j.ijrobp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calton B, Shibley WP, Cohen E, Pantilat SZ, Rabow MW, O'Riordan DL, et al. Patient and caregiver experience with outpatient palliative care telemedicine visits. Palliative Medicine Reports. 2020;1(1):339–346. doi: 10.1089/pmr.2020.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Comprehensive cancer centers and integrated delivery networks American Health & Drug Benefits 2020 13:45
- 32.Alshamrani M, AlHarbi A, Alkhudair N, AlNajjar F, Khan M, Obaid AB, et al. Practical strategies to manage cancer patients during the COVID-19 pandemic: Saudi Oncology Pharmacy Assembly Experts recommendations. J Oncol Pharm Pract. 2020;26(6):1429–1440. doi: 10.1177/1078155220935564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Curigliano G, Banerjee S, Cervantes A, Garassino MC, Garrido P, Girard N, et al. Managing cancer patients during the COVID-19 pandemic an ESMO multidisciplinary expert consensus. Ann Oncol. 2020;31(10):1320–1335. doi: 10.1016/j.annonc.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jazieh AR, Chan SL, Curigliano G, Dickson N, Eaton V, Garcia-Foncillas J, et al. Delivering cancer care during the COVID-19 pandemic: recommendations and lessons learned from ASCO global webinars. JCO global oncology. 2020;6:1461–1471. doi: 10.1200/GO.20.00423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dalby M, Hill A, Nabhani-Gebara S. Cancer patient experience of telephone clinics implemented in light of COVID-19. J Oncol Pharm Pract. 2021;27(3):644–649. doi: 10.1177/1078155221990101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lopez CJ, Edwards B, Langelier DM, Chang EK, Chafranskaia A, Jones JM (2021) Delivering virtual cancer rehabilitation programming during the first 90 days of the COVID-19 pandemic: a multimethod study. Arch Phys Med Rehabil 102(7):1283–93 [DOI] [PMC free article] [PubMed]
- 37.Triantafillou V, Layfield E, Prasad A, Deng J, Shanti RM, Newman JG, et al. Patient perceptions of head and neck ambulatory telemedicine visits: a qualitative study Otolaryngology head and neck surgery. Otolaryngol Head Neck Surg. 2021;164(5):923–31. doi: 10.1177/0194599820943523. [DOI] [PubMed] [Google Scholar]
- 38.Fraser A, Mc Neill R, Robinson J. Cancer care in a time of COVID: lung cancer patient’s experience of telehealth and connectedness 2021 [DOI] [PMC free article] [PubMed]
- 39.Cox A, Lucas G, Marcu A, Piano M, Grosvenor W, Mold F, et al. Cancer survivors’ experience with telehealth: a systematic review and thematic synthesis. J Med Internet Res. 2017;19(1):e11. doi: 10.2196/jmir.6575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siow MY, Walker JT, Britt E, Kozy JP, Zanzucchi A, Girard PJ, et al. What was the change in telehealth usage and proportion of no-show visits for an orthopaedic trauma clinic during the COVID-19 pandemic? Clin Orthop Relat Res. 2020;478(10):2257–2263. doi: 10.1097/CORR.0000000000001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guarino M, Cossiga V, Fiorentino A, Pontillo G, Morisco F. Use of telemedicine for chronic liver disease at a single care center during the COVID-19 pandemic: prospective observational study. J Med Internet Res. 2020;22(9):e20874. doi: 10.2196/20874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suc L, Daguenet E, Louati S, Gras M, Langrand-Escure J, Sotton S, et al. Telemedicine for prostate cancer during long-term radiotherapy follow-up: An opportunity for digital innovation in oncology. Cancer Radiother. 2021;25(1):45–50. doi: 10.1016/j.canrad.2020.06.038. [DOI] [PubMed] [Google Scholar]
- 43.Sonagli M, Cagnacci Neto R, Leite FPM, Makdissi FBA. The use of telemedicine to maintain breast cancer follow-up and surveillance during the COVID-19 pandemic. J Surg Oncol. 2021;123(2):371–374. doi: 10.1002/jso.26327. [DOI] [PubMed] [Google Scholar]
- 44.Qaderi SM, Vromen H, Dekker HM, Stommel MWJ, Bremers AJA, de Wilt JHW. Development and implementation of a remote follow-up plan for colorectal cancer patients. Eur J Surg Oncol. 2020;46(3):429–432. doi: 10.1016/j.ejso.2019.10.014. [DOI] [PubMed] [Google Scholar]
- 45.Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. 2020 Implementation and usefulness of telemedicine during the COVID-19 pandemic a scoping review J Prim Care Community Health 11:2150132720980612- [DOI] [PMC free article] [PubMed]
- 46.Ramaswamy A, Yu M, Drangsholt S, Ng E, Culligan PJ, Schlegel PN, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22(9):e20786. doi: 10.2196/20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2031640. doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic disparities in patient use of telehealth during the coronavirus disease 2019 surge. JAMA Otolaryngol Head Neck Surg. 2021;147(3):287–295. doi: 10.1001/jamaoto.2020.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jaffe DH, Lee L, Huynh S, Haskell TP. Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Popul Health Manag. 2020;23(5):368–377. doi: 10.1089/pop.2020.0186. [DOI] [PubMed] [Google Scholar]
- 50.Temesgen ZM, DeSimone DC, Mahmood M, Libertin CR, Varatharaj Palraj BR, Berbari EF. Health care after the COVID-19 pandemic and the influence of telemedicine. Mayo Clin Proc. 2020;95(9S):S66–S68. doi: 10.1016/j.mayocp.2020.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kreofsky BLH, Blegen RN, Lokken TG, Kapraun SM, Bushman MS, Demaerschalk BM. Sustainable telemedicine: designing and building infrastructure to support a comprehensive telemedicine practice. Telemed J E Health. 2018;24(12):1021–1025. doi: 10.1089/tmj.2017.0291. [DOI] [PubMed] [Google Scholar]
- 52.Lokken TG, Blegen RN, Hoff MD, Demaerschalk BM. Overview for implementation of telemedicine services in a large integrated multispecialty health care system. Telemed J E Health. 2020;26(4):382–387. doi: 10.1089/tmj.2019.0079. [DOI] [PubMed] [Google Scholar]
- 53.Uscher-Pines L, Kahn JM. Barriers and facilitators to pediatric emergency telemedicine in the United States. Telemed J E Health. 2014;20(11):990–996. doi: 10.1089/tmj.2014.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nissen L, Lindhardt T. A qualitative study of COPD-patients’ experience of a telemedicine intervention. Int J Med Inform. 2017;107:11–17. doi: 10.1016/j.ijmedinf.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 56.Quinn CC, Chard S, Roth EG, Eckert JK, Russman KM, Cross RK. The Telemedicine for Patients With Inflammatory Bowel Disease (TELE-IBD) clinical trial: qualitative assessment of participants’ perceptions. J Med Internet Res. 2019;21(6):e14165. doi: 10.2196/14165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sauers-Ford HS, Hamline MY, Gosdin MM, Kair LR, Weinberg GM, Marcin JP, et al. Acceptability, usability, and effectiveness: a qualitative study evaluating a pediatric telemedicine program. Acad Emerg Med. 2019;26(9):1022–1033. doi: 10.1111/acem.13763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bajowala SS, Milosch J, Bansal C. Telemedicine pays: billing and coding update. Curr Allergy Asthma Rep. 2020;20(10):60. doi: 10.1007/s11882-020-00956-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Implementing Telehealth in Practice Obstet Gynecol. 2020;135(2):e73–e79. doi: 10.1097/AOG.0000000000003671. [DOI] [PubMed] [Google Scholar]
- 60.Bokolo AJ. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7):132. doi: 10.1007/s10916-020-01596-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hasanpoor E, Hajebrahimi S, Janati A, Abedini Z, Haghgoshayie E. Barriers, Facilitators, process and sources of evidence for evidence-based management among health care managers: a qualitative systematic review. Ethiop J Health Sci. 2018;28(5):665–680. doi: 10.4314/ejhs.v28i5.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.