Abstract
Introduction
Intermittent preventive treatment in pregnancy with sulphadoxine pyrimethamine (IPTp) is a key malaria prevention strategy in sub-Saharan African countries. We conducted an anthropological study as part of a project aiming to evaluate a community-based approach to the delivery of IPTp (C-IPTp) through community health workers (CHWs) in four countries (the Democratic Republic of Congo, Madagascar, Mozambique and Nigeria), to understand the social context in order to identify key factors that could influence C-IPTp acceptability.
Methods
A total of 796 in-depth interviews and 265 focus group discussions were undertaken between 2018 and 2021 in the four countries with pregnant women, women of reproductive age, traditional and facility-based healthcare providers, community leaders, and relatives of pregnant women. These were combined with direct observations (388) including both community-based and facility-based IPTp delivery. Grounded theory guided the overall study design and data collection, and data were analysed following a combination of content and thematic analysis.
Results
A series of key factors were found to influence acceptability, delivery and uptake of C-IPTp in project countries. Cross-cutting findings include the alignment of the strategy with existing social norms surrounding pregnancy and maternal health-seeking practices, the active involvement of influential and trusted actors in implementation activities, existing and sustained trust in CHWs, the influence of husbands and other relatives in pregnant women’s care-seeking decision-making, the working conditions of CHWs, pregnant women’s perceptions of SP for IPTp and persistent barriers to facility-based antenatal care access.
Conclusions
The findings provide evidence on the reported acceptability of C-IPTp among a wide range of actors, as well as the barriers and facilitators for delivery and uptake of the intervention. Overall, C-IPTp was accepted by the targeted communities, supporting the public health value of community-based interventions, although the barriers identified should be examined if large-scale implementation of the intervention is considered.
Keywords: malaria, maternal health, public health, qualitative study
WHAT IS ALREADY KNOWN ON THIS TOPIC
The WHO recommends exploring community-based approaches to the delivery of the intermittent preventive treatment of malaria in pregnancy (IPTp) as an opportunity to expand its access and coverage.
IPTp delivery through community health workers has already been tested in small-scale pilots and shown positive results in increasing IPTp coverage, although evidence on the reported acceptability of the strategy is limited.
WHAT THIS STUDY ADDS
This qualitative study is part of the evaluation component of a large-scale 5-year project piloting the community-based delivery of IPTp (C-IPTp) in four sub-Saharan African countries.
The study uses a socioanthropological approach that contributes to examining C-IPTp delivery, uptake and acceptability from a multidimensional and longitudinal perspective.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The findings presented here provide meaningful insights into the factors that implementers and practitioners should consider when adopting the C-IPTp strategy in diverse settings.
With the identified factors adequately addressed, C-IPTp has the potential to contribute to the prevention of malaria in pregnancy with the acceptance and involvement of the communities it targets.
Introduction
Malaria infection is a major and persistent public health problem, particularly in endemic African countries. Pregnant women and children under 5 are among the most vulnerable, with malaria infection during pregnancy (MiP) entailing substantial risks for the mother, her fetus and the newborn.1 It is estimated that in Africa, 11.6 million pregnancies were exposed to the infection in 2020, resulting in 819 000 children born with low birth weight.2 The WHO recommends a package of interventions to prevent MiP, which includes use of insecticide-treated nets, administration of intermittent preventive treatment with sulphadoxine-pyrimethamine (IPTp-SP) during pregnancy and appropriate case management through prompt diagnosis and effective treatment of malaria.3 IPTp-SP should be administered as early as possible in the second trimester of pregnancy with doses given at least 1 month apart until the time of delivery.
WHO recommends IPTp to be administered during antenatal care (ANC) visits at health facilities. Although IPTp-SP has been shown to be a highly cost-effective strategy for the prevention of MiP, improving newborn and maternal health, and reducing neonatal mortality,4 coverage across SSA countries remain low. Based on data from 33 African countries, in 2020 uptake of IPTp1, IPTp2 and IPTp3 were 57%, 46% and 32%, respectively.2 To improve ANC service delivery, the WHO also recommends alternative and complementary approaches are tested, for instance, through lay health workers’ involvement.3 Interventions that involve community health workers (CHWs) for the delivery of maternal and infant healthcare services in general,5 6 and for malaria control specifically,7 8 have already been demonstrated to work in many settings. The community-based delivery of IPTp-SP (C-IPTp) has been tested in a few settings through small-scale pilots and shown positive results, both in terms of improved coverage of IPTp-SP and ANC services.9–15 In line with WHO recommendations, exploring a community-based approach to IPTp delivery can help gain a better understanding of the feasibility and acceptability of this approach as complementary to ANC and as an opportunity to expand access to IPTp.
The findings presented in this article are part of the results of the evaluation of a 5-year project that piloted C-IPTp in four sub-Saharan African countries, namely the Democratic Republic of Congo (DRC), Madagascar, Nigeria and Mozambique. The Transforming IPTp for Optimal Pregnancy project (https://www.tiptopmalaria.org/)), which was conceived in close collaboration with the WHO and with the commitment of countries’ Ministries of Health (MoH), was launched to broaden and strengthen the evidence base on the effectiveness of C-IPTp in increasing IPTp coverage without reducing ANC utilisation. The evidence being generated throughout the evaluation of the intervention was recurrently shared with the relevant MoH departments, as well as national and international stakeholders. In addition to testing the effectiveness of the C-IPTp approach,16 the project also evaluated its cost-effectiveness,17 acceptability and feasibility, as well as its impact on SP drug resistance. A qualitative study was undertaken to assess the acceptability and feasibility of C-IPTp in project areas. Specifically, the study sought to understand the social context where the project was being implemented in order to identify the factors that influence C-IPTp acceptability among pregnant women and the network of actors involved in the intervention, including the barriers and opportunities for its delivery and uptake. Substantial qualitative research literature has been generated on the role of CHWs in the promotion and delivery of maternal and child health services,18 19 including recent work that addresses the anticipated acceptability of the community distribution of IPTp.20 However, to our knowledge, this is the first longitudinal qualitative study that has focused specifically on the reported acceptability of the delivery of IPTp-SP via CHWs and studied it from the perspective of pregnant women, CHWs and the communities they serve.
Methods
Study design
The study design followed an inductive approach, based on grounded theory,21 whereby no theoretical framework was used to guide the research or inform its design. Instead, emphasis was placed on generating theory through the interpretation of the data collected, thus grounding theory in data. Research questions were reformulated throughout the research process, including data collection and analysis, in a continuous and iterative manner. The study design was longitudinal, with a total of four annual data collection phases starting before project implementation in 2018 and through the last full year of implementation in 2021. A total of four data collection phases were conducted throughout the 4 years, one per year, each one generating sets of data that informed the data collection approach to follow during the subsequent phases.
Although the overall approach that guided the research was inductive, the study design was founded on the notion that acceptability is ‘a multifaceted construct’.22 Furthermore, feasibility is understood in more structural systemic terms, in reference to the extent to which an intervention can be carried out,23 thus, ‘delivered’ and ‘taken-up’. Within the context of this study, it has been considered that acceptability, as a multifaceted construct, also addresses certain aspects of feasibility, which are captured in the study of the delivery and uptake of C-IPTp. In addition, the findings from the exploratory phase of data collection (ie, the first phase before implementation) led to the introduction of two conceptual frameworks that further guided the design to better address the study objectives, namely the barriers and opportunities analysis24 and the socioecological model.25 Data collected during the exploratory phase were analysed separately by the in-country research teams and then pooled by the research team at the coordinating institution. The pooled analysis consisted of identifying cross-cutting themes that then informed the choice of conceptual frameworks and their subsequent adaptation to the study aims and context.
The decision to introduce the socioecological model was informed by the emphasis placed across study sites on the importance of the social context wherein pregnant women are embedded in influencing their health-seeking patterns, as well as the realisation of the complexity of the decision-making processes that underpin these patterns. The decision to introduce the barriers and opportunities analysis was informed by the multiple thematic dimensions found to be relevant to the anticipated acceptability of C-IPTp, as it was foreseen prior to its implementation. This required the introduction of a framework that allowed us to simultaneously address multiple themes and that was adaptable to the research interests delineated in the exploratory phase and to themes emerging throughout subsequent phases (ie, sensitive to the iterative nature of the research process). The use of both frameworks facilitated the examination of C-IPTp delivery, uptake and acceptability from a multidimensional perspective, and for understanding pregnant women’s health-seeking pathway as embedded in a complex and layered social system.
Study settings
The study was carried out in the three areas per each of the four countries where the TIPTOP project was being implemented: Kenge, Bulungu and Kunda health zones (HZ) in the DRC; Mananjary, Vohipeno and Toliary II districts in Madagascar; Nhamatanda, Meconta and Murrupula districts in Mozambique; and Ohaukwu, Akure South and Bosso local government areas (LGA) in Nigeria (see figure 1). In all countries, malaria is one of the leading causes of maternal and child morbidity and mortality, while the CHW models vary across countries.
Figure 1.
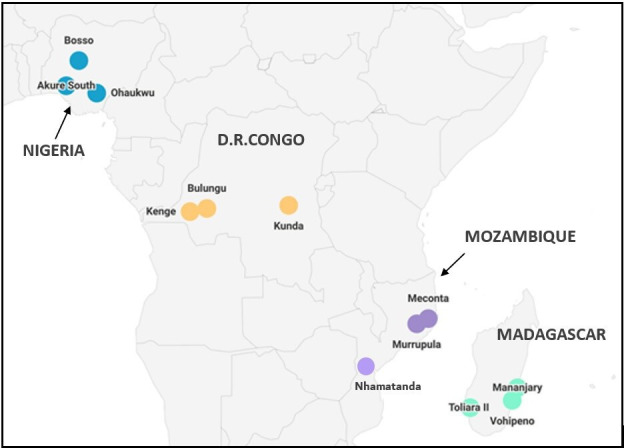
Map of study sites.
C-IPTp strategy
C-IPTp was implemented similarly across the four TIPTOP project countries, with CHWs trained to identify pregnant women in the community, screen them for IPTp eligibility, provide IPTp to eligible pregnant women, and refer all women to ANC. The latter ‘referral to ANC’ was a key component to ensure all pregnant women received comprehensive care. Based on national Ministry of Health (MoH) recommendations and guidelines on CHW roles, notable adaptations were made to the strategy, such as the administration of the first dose of IPTp-SP. In the DRC and Nigeria, CHWs were authorised to administer all doses of IPTp-SP, including the first one. Importantly, in these countries, CHW did not physically assess pregnant women for gestational age and only gave IPTp1 if the woman reported having experienced foetal movement. In Madagascar and Mozambique, CHWs were not authorised to administer the first dose of IPTp-SP but were able to administer subsequent doses. When identifying pregnant women that had not received any dose of IPTp-SP, CHWs were required to refer them to the health facility to receive their first dose during their routine ANC visit.
Although the C-IPTp strategy incorporated existing CHW cadres in all countries, an additional community-based role was introduced in Mozambique to support existing CHWs, given their relatively low ratio to pregnant women. This new category of volunteer health worker—called lay community counsellor (LCC)—was introduced to support the C-IPTp approach. LCCs were trained to perform CHW tasks related to C-IPTp, with the exception of administering SP and the addition of referring pregnant women to CHWs as well as to ANC. These tasks included the identification and mapping of pregnant women, conducting follow-up home visits, referring pregnant women to the health facility for continued ANC, and liaising between pregnant women and CHWs.
Sampling and data collection
The study involved a total of 3235 participants across the four countries (see table 1) over the 4-year duration of the project. Participants included pregnant women, women of reproductive age (15–45 years), ANC health providers, CHWs, traditional healers, health management representatives, traditional birth attendants (TBAs), community leaders and relatives of pregnant women. The identification of participants was based on non-probabilistic methods, following purposive sampling combined with snowballing. Complementary sampling strategies included opportunistic sampling and, to a lesser extent, convenience sampling. Although field entry strategies varied between countries, all research teams benefited from the support of local leaders, regional health authorities and healthcare workers during the sampling process. Informants meeting the aforementioned target group criteria were then invited to participate in research activities. Those willing to participate and provide written informed consent were enrolled. A local social scientist from each in-country partner institution coordinated research teams were composed of local guides, interviewers, facilitators, translators and transcribers. Research teams were trained to employ various sampling approaches and conduct data collection.
Table 1.
Participants recruited per site and phase (IDIs/FGDs)
| Data collection phase | DRC | Nigeria | Madagascar | Mozambique | Total | ||||||||
| Kenge | Bulungu | Kunda | Ohaukwu | Akure south | Bosso | Mananjary | Toliary II | Vohipeno | Nhamatanda | Meconta | Murrupula | ||
| I 2018 | 155 | 180 | N/A* | 80 | 80 | N/A* | 47 | 48 | N/A* | 104 | 103 | N/A* | 797 |
| II 2019 | 175 | 166 | 207 | 139 | 138 | 138 | 67 | 76 | 75 | N/A† | 75 | 79 | 1335 |
| III 2020 | 61 | 59 | 70 | 53 | 56 | 58 | 48 | 49 | 49 | 36 | 36 | 37 | 612 |
| IV 2021 | 48 | 47 | 47 | 41 | 48 | 49 | 40 | 42 | 42 | 29 | 30 | 28 | 491 |
*Although TIPTOP was piloted in three areas per country, in the early phases of the study research activities were planned to be conducted only in two areas per country. In order to strengthen the scientific value of the results, the third project area was included in the study design after the first phase of data collection.
†No fieldwork was carried out in Nhamatanda in 2019 due to cyclone Idai.
DRC, Democratic Republic of Congo; FGDs, focus group discussions; IDIs, in-depth interviews; NA, not available; TIPTOP, ransforming IPTp for Optimal Pregnancy.
The data collection techniques employed were drawn from qualitative methodologies and ethnography.26 These consisted of in-depth interviews (IDIs), focus group discussions (FGD), informal conversations and direct observations. IDIs and FGDs were conducted using semi-structured question guides to capture participants’ knowledge of maternal health, malaria prevention in pregnancy and IPTp, as well as perceptions of C-IPTp and potential barriers and facilitators that could influence the acceptability of the intervention. Template guides in English were adapted to meet local context specificities and translated into the relevant language of local use by in-country research teams. Researchers performed live translations into other local languages, where appropriate. FGDs and IDIs were conducted in the language preferred by the participant, digitally recorded and transcribed verbatim. As needed, transcriptions were then translated into English in Nigeria, Portuguese in Mozambique and French in Madagascar and the DRC.
Researchers conducted non-participant observations of the following activities: the delivery of ANC services, both at health facilities and in TBA’s homes; the administration of IPTp-SP by CHWs, whether delivered in pregnant women’s homes or in CHWs’ homes; communication activities for IPTp and maternal health promotion, carried out both in health facilities and communities; and the day-to-day activities of pregnant women. Observations were recorded in field notes, following observation guides to ensure notes were comprehensive and captured several key aspects: description of the physical space, people involved, performance of the activity, timing, dynamics between participants and the general mood. Informal conversations carried out spontaneously with key informants encountered during fieldwork activities were also captured in field-notes. In total, 265 FGDs, 796 IDIs and 388 observations were performed throughout the study phases and across sites (see table 2).
Table 2.
Data collection activities performed per tool, phase and site
| Data collection phase | DRC | Nigeria | Madagascar | Mozambique | Total | ||||||||
| Kenge | Bulungu | Kunda | Ohaukwu | Akure south | Bosso | Mananjary | Toliary II | Vohipeno | Nhamatanda | Meconta | Murrupula | ||
| I 2018 | 14 FGD | 14 FGD | N/A | 14 FGD | 14 FGD | N/A | 47 IDI | 48 IDI | N/A | 7 FGD | 7FGD | N/A | 70 FGD |
| 20 IDI | 20 IDI | 10 IDI | 10 IDI | * | * | 30 IDI | 30 IDI | 216 IDI | |||||
| II 2019 | 14 FGD | 12 FGD | 15 FGD | 12 FGD | 12 FGD | 12 FGD | 6 FGD | 8 FGD | 9 FGD | N/A† | 7 FGD | 7 FGD | 114 FGD |
| 11 IDI | 22 IDI | 24 IDI | 18 IDI | 18 IDI | 18 IDI | 24 IDI | 24 IDI | 20 IDI | 20 IDI | 20 IDI | 219 IDI | ||
| 9 OBS | 10 OBS | 13 OBS | 4 OBS | 9 OBS | 3 OBS | 8 OBS | 9 OBS | 8 OBS | 6 OBS | 14 OBS | 93 OBS | ||
| III 2020 | 4 FGD | 4 FGD | 4 FGD | 4 FGD | 4 FGD | 4 FGD | 4 FGD | 4 FGD | 4 FGD | 3 FGD | 3 FGD | 3 FGD | 45 FGD |
| 13 IDI | 11 IDI | 22 IDI | 17 IDI | 17 IDI | 18 IDI | 17 IDI | 16 IDI | 16 IDI | 18 IDI | 18 IDI | 19 IDI | 202 IDI | |
| 9 OBS | 15 OBS | 12 OBS | 9 OBS | 9 OBS | 8 OBS | 7 OBS | 9 OBS | 9 OBS | 24 OBS | 25 OBS | 27 OBS | 163 OBS | |
| IV 2021 | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 3 FGD | 36 FGD |
| 12 IDI | 11 IDI | 11 IDI | 12 IDI | 13 IDI | 13 IDI | 16 IDI | 17 IDI | 18 IDI | 12 IDI | 12 IDI | 12 IDI | 159 IDI | |
| 9 OBS | 9 OBS | 9 OBS | 13 OBS | 10 OBS | 14 OBS | 9 OBS | 8 OBS | 9 OBS | 15 OBS | 15 OBS | 12 OBS | 132 OBS | |
*No FGDs were conducted in the Madagascar sites during the first/baseline phase of data collection.
†No fieldwork was carried out in Nhamatanda in 2019 due to cyclone Idai.
DRC, Democratic Republic of Congo; FGD, focus group discussions; IDIs, in-depth interviews; NA, not available.
Data analysis
Given the iterative nature of the grounded theory approach, data collection and analysis progressed simultaneously, allowing the tools to be modified in light of themes emerging from ongoing analysis. The data collected was interpreted through a combination of content and thematic analysis.27 Content analysis involved categorising data based on the themes predetermined by the two conceptual frameworks introduced after the initial exploratory phase. Thematic analysis consisted of identifying emerging themes relevant to the study aims that subsequently contributed to further shaping the research process. Research teams coded the data manually. The social science team at the coordinating institution then compared the analyses from the different sites in order to elucidate commonalities and divergences. During this process, there was a constant interaction between research teams to resolve key interpretation issues. More information about the collaboration between research institutions and their involvement in the research process is presented in the authors reflexivity statement (see online supplemental appendix 1).
bmjgh-2022-010079supp001.pdf (281.9KB, pdf)
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
The examination of the data gathered along the different phases of the study suggests that the C-IPTp strategy as implemented by the TIPTOP project was largely accepted by pregnant women and other actors both at health facility and community levels. Throughout the analysis of the factors influencing the delivery, uptake and acceptability of the C-IPTp strategy (which includes the promotion of ANC uptake), the following key cross-cutting themes emerged: influences on pregnant women’s decision-making; perceptions of SP for IPTp; health-seeking pathways during pregnancy; trusting relationships; involvement of key actors; and CHWs’ working conditions (figure 2). The findings presented here are structured around the aforementioned themes, and in some cases also subthemes.
Figure 2.
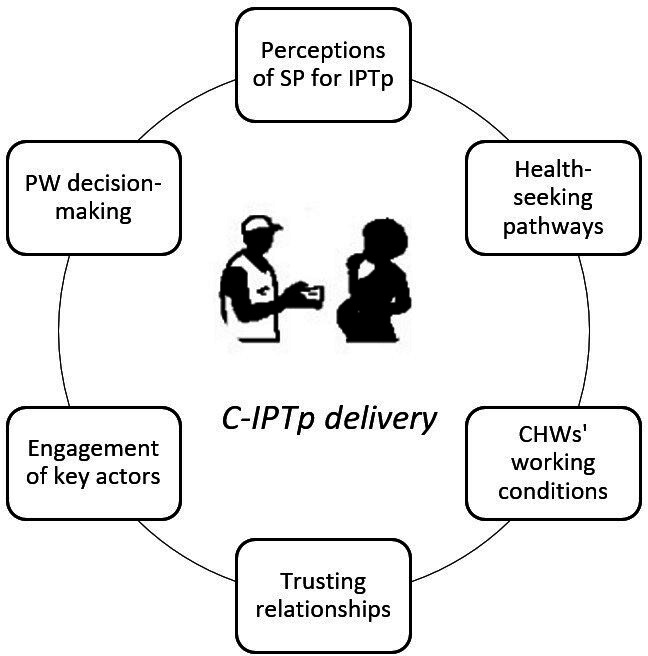
Factors influencing C-IPTp delivery. C-IPTp, community-based approach to the delivery of intermittent preventive treatment in pregnancy.*PW = pregnant women
Influences on pregnant women’s decision-making
A variety of actors were found to exert significant influence on pregnant women’s care-seeking decision-making processes. Findings showed that married pregnant women are commonly expected to seek their husbands’ permission to seek ANC, often related to women’s financial dependence. Insights from observations of CHW home visits revealed that CHWs’ interactions with pregnant women were mediated by similar norms, and CHWs were expected to obtain the husband’s consent prior to interacting with the pregnant women, particularly in the case of male CHWs.
Often it is their husbands that oppose ANC, some use as a pretext the lack of money. (IDI, woman of reproductive age, Mananjary, Madagascar, 2021)
Relatives, such as in-laws, or in the case of single pregnant adolescents—parents, also exerted influence in pregnant women’s care-seeking decisions. Their degree of influence varied depending on the sociocultural makeup of the given setting. For instance, different kinship systems may tilt the power balance in favour of one lineage over another, thus affecting which relatives are most influential. In the case of matrilineal societies found in Murrupula and Meconta districts (Nampula province, Mozambique), the relatives of the pregnant woman’s mother are more influential than the pregnant woman’s in-laws and the weight that their decisions carry is comparable to, and at times outweighs, that of the husband. This contrasts with patrilineal societies found in most study settings, where the husband and in-laws are the ultimate decision-makers.
Our culture says if a woman is going out she must take permission from her husband and if she doesn’t take permission, her husband will not [accept] it]. (IDI, community leader, Bosso, Nigeria, 2020)
Perceptions of SP for IPTp
Pregnant women’s perceptions of SP were both socially learnt and shaped by their embodied experiences with the drug. A variety of subthemes on the perceptions of SP are presented below
Side effects
SP was often perceived as causing side effects such as dizziness, vomiting, nausea and weakness. This perception was found to be both socially learnt through interactions with other pregnant women or female relatives, as well as rooted in pregnant women’s individual experiences using SP. Irrespective of the physiological causes behind the side effects, pregnant women generally associated these to consuming the drug on an empty stomach (an explanation commonly reproduced by health workers) or to the drug composition itself. This perception of SP as a drug that causes side effects is the most commonly reported justification for cases of treatment refusal identified in this study.
M: You prefer taking Fansidar [SP] in the hospital or you prefer that the CHW comes to your house to give it to you?
R—I don’t prefer anything, I just don’t want Fansidar [SP] because when I take it things happen, it hurts, it smells bad and makes me nauseous, I lose my appetite, I vomit all day, feel weak in my body and sleepy… (IDI, pregnant woman, Meconta, Mozambique, 2019)
Pregnant study participants that attributed side effects to consumption on an empty stomach were predominantly found in the Mozambican sites. It is also in these sites where C-IPTp was recognised as a way to avoid the perceived side effects since by receiving the treatment in their homes pregnant women have the chance to eat beforehand.
The idea of taking Fansidar [SP] here in the community is good because when we took it in the hospital we had problems with the pills because we left home without having eaten anything because of a lack of money to buy bread. (IDI, pregnant woman, Meconta, Mozambique, 2019)
Adverse pregnancy outcomes
Participants associated SP use with adverse pregnancy outcomes including miscarriages, delivery complications and infertility. The specific adverse outcomes identified were unique to the different study settings. For instance, the perception that SP could lead to overdue pregnancies and / or large babies resulting in delivery complications and potentially surgically interventions, was specific to the Mozambican sites, and to a lesser degree, in the DRC sites.
A friend told me that this product [SP] is not good, it fattens the baby in the belly and then during delivery the doctor has to recur to the caesarean, there won’t be a way to have a vaginal delivery; this is why I avoid it [SP]. (FGD, pregnant woman, Bulungu, DRC, 2019)
The perception that SP could inhibit fertility was unique to Bosso, Nigeria, and was coupled with the concern that IPTp-SP is a family planning tool aimed at population control. These perceptions are underpinned by existing conceptualisations of ‘Western’ medicine and mistrust in public health strategies. Based on participants’ accounts, these perceptions seemed to be a minority sentiment. Nevertheless, cases of IPTp refusal that were founded on this perception were identified during the study.
Drugs are mix by white men and you know they can mix things that can even kill a person […] now I hear that they want to reduce people, they can mix things and then give it to pregnant women, if you have headache they will tell you to pay for common Paracetamol, but when they say they should reduce childbirth the drugs are given freely. Me, my children are a gift from God. (IDI, pregnant woman, Bosso, Nigeria, 2020)
Efficacy
Study participants’ awareness of the purpose of SP as a drug that prevents MiP was uneven across study sites. SP is often conceived of in general terms as a drug that is beneficial for the pregnancy and the development of the fetus, and that is efficacious in ensuring a healthy pregnancy. Despite a lack of a disease-specific understanding of SP, participants broadly perceived SP as a drug that ‘works’ and rarely questioned its efficacy.
Quality
Participants across study sites generally did not express concerns over the quality of the SP delivered by CHWs. In fact, in the DRC sites, the SP delivered via CHWs was often perceived to be of superior quality as compared with the SP administered at health facilities during ANC. When comparing the SP administered via the different providers, pregnant women noted that the SP delivered by CHWs was packaged in a blister for each dose, while a dose of SP delivered at health facilities must be extracted by hand from a large tub of loose pills. This difference in packaging is due to the fact that the SP delivered by CHWs was sourced by the project which introduced innovative packaging for SP, while the SP delivered at the health facilities was sourced by the national public health system. Pregnant women interpreted the difference in packaging as an indication that the SP delivered by CHWs was of higher quality and more efficacious, while having fewer side effects. The attribution of superior quality to the SP delivered via CHWs was not limited to pregnant women but was also identified among CHWs.
Health-seeking pathways during pregnancy
The extent to which C-IPTp delivery can be nested in pregnant women’s existing health-seeking pathways may facilitate its uptake. Given the C-IPTp strategy involved both the delivery of IPTp by CHWs, and the promotion of ANC attendance at the health facility, the subthemes identified within this theme are pertinent to both community and facility-based delivery.
Pregnancy disclosure norms
According to participants across the four countries, local social norms and values, usually referred to as ‘the tradition’, frame women’s behaviours concerning maternity and pregnancy. These can entail reservations with regard to the disclosure of a pregnancy, usually to avoid generating envy that is believed to incite acts of witchcraft and result in misfortune. Thus, women feeling threatened may decide to keep their pregnancies hidden until the belly is clearly visible, leading to delays in the use of health services.
Moderator (M): Will you tell people that you are pregnant when the pregnancy is still new?
Respondent (R)3: No, I will not because some people can terminate your pregnancy if you tell them then
R7: No, because some people are wicked and they like to hear that you are pregnant or that you delivered a baby. So unless the pregnancy is giving problem, I will not tell anybody except doctors and nurses.
(FGD, Women of reproductive age, Ohaukwu, Nigeria, 2019)
During the exploratory phase of the study, participants anticipated ‘local norms’ leading to ‘hidden pregnancies’ as a potential barrier to C-IPTp. It was assumed that as part of the local social dynamics framing women’s health-seeking behaviours, pregnancy disclosure norms would have an impact on C-IPTp adherence and acceptability. Data collected in subsequent phases of the study showed this barrier was decreasingly salient in participants’ accounts and unevenly reported across countries. However, disclosure norms continued to be relevant at later stages of the research to the extent that they shaped the interaction between pregnant women and other actors involved in the intervention, particularly with regard to CHWs and their capacity to identify pregnant women at early stages of pregnancy.
Pregnant women at early stages of pregnancy, because of this prohibition that one cannot talk [about pregnancy] to anyone yet, etc., this is where we need CHWs’ skills in communication. (IDI, Health worker, Toliary II, Madagascar, 2021)
Structural factors determining ANC access
Limited transport options and distance to the health facility, coupled with the predominantly weak infrastructures found in the four countries can impact regular ANC visits.
We go by foot! In a canoe! And if the roads are difficult, we are really very tired… (FGD, Pregnant women, Vohipeno, Madagascar, 2021)
In some countries, ANC services (including IPTp-SP) are free-of-charge, while in others fees are attached to components of the service. Even where ANC services are free-of-charge, participants at times reported having been requested for additional, and sometimes unexpected, payments for certain services, tests, or treatments once at the health facility. Moreover, insufficient financial means to afford travel costs have been widely reported by pregnant women across all countries. Where fees are attached to ANC they add to the financial burden many pregnant women face when accessing maternal healthcare.
My pregnancy is six months but I have not started ANC yet because I have no money; I am happy with your project because you are going to give us free medicine against malaria. (FGD, Pregnant women, Bulungu, DRC, 2019)
The quality of the reception and services received at the health facility can also determine the willingness to attend ANC. Some pregnant women also referred to the time they lose when going to the health facility for their ANC visits.
I think it’s good [ANC], but if it wasn't for this delay-thing when we go there, we come back very late. We leave the house in the morning and return in the afternoon, even when we get up early, we get back at 2 pm. (IDI, pregnant woman, Meconta, Mozambique, 2021)
The exploratory phase pointed at all these factors as major barriers affecting ANC attendance. This initial finding was coupled with the widespread concern that C-IPTp would discourage ANC attendance. These concerns were, indeed, magnified by the aforementioned financial and logistical obstacles pregnant women encounter when attending ANC. As the study progressed, data did not indicate that C-IPTp itself was deterring women from attending ANC. Instead, pregnant women were generally aware that receiving IPTp-SP was only part of the ANC package and that comprehensive care required follow-up at the health facility. Yet, study participants still referred to structural factors as relevant limitations in pregnant women’s health-seeking pathways within the context of the C-IPTp itinerary, given that CHWs continuously referred them to the health facility for regular ANC. Furthermore, existing facility-based access barriers did condition pregnant women’s uptake of C-IPTp in the Malagasy and Mozambican sites, where IPTp1 must be taken at the health facility.
Medical pluralism
Diverse medical approaches, such as biomedicine, religious healing and herbalism, are widely adopted in the study sites. Pregnant women reported combining different sources of care, and the use of these different healing sources depends on the specific health needs.
For minor ailments, we contact the traditional birth attendant, but we go to the maternity hospital for the delivery (FGD, pregnant women, Mananjary, Madagascar, 2019)
Our findings suggest that C-IPTp uptake and ‘traditional medicine’ (using emic terms) seem to not be mutually exclusive. In the same vein, according to our participants’ accounts, traditional health practitioners (spiritual healers, herbalists and TBAs) seem not to advise pregnant women against the uptake of IPTp in general, or C-IPTp specifically.
We don’t have the grace to give them drugs, the grace we have is natural, but we tell them to go to health facility to register. After registration, they will do different tests they are supposed to do for them, and give them drug to take to make their unborn child develop well. Our own is to care naturally. (IDI, TBA, Akure South, Nigeria, 2021)
Although both medical systems coexist and seem to be largely compatible, some exceptions were reported. For instance, leaders from some religious denominations in some settings within Kunda HZ, DRC, explicitly forbid their followers to use healthcare services or to consume drugs from the biomedical system (including ANC and IPTp-SP). Other kinds of friction between medical systems were captured in Akure South and Ohaukwu LGAs, Nigeria. Although C-IPTp implementers built productive relationships with TBAs, some pregnant women reported preferring TBA services which are perceived to be a more ‘holistic’ service that is both clinical and spiritual. The notion that surgical deliveries are common in health facilities, as opposed to the ‘natural’ deliveries conducted by TBAs, amplifies this preference.
Trusting relationships
The exploratory phase revealed concerns in the study population regarding CHWs’ competence in administering SP and their presumed lack of specialised training in maternal healthcare. A retrospective analysis of the data indicates that, as the implementation of the strategy progressed, concerns over CHWs competence lessened. Overall, CHWs succeeded in building and sustaining trusting relationships with the pregnant women in their communities, and their role as IPTp-SP providers was appreciated by the community as a whole. Trust in CHWs stem both from their familiarity as fellow members of their respective communities, that is their social embeddedness, as well as from being visibly backed by the health system which in turn validates their competence in delivering IPTp-SP.
I accept taking Fanisdar [SP] at the CHW’s house because I trust him, when something happens to us we recur to him. (IDI, pregnant woman, Meconta, Mozambique, 2021)
Although study findings were relatively consistent across sites, some context-specific misconceptions disrupting trust-building were identified in Nigeria throughout the study. In primarily urban settings in Akure South, and to a lesser extent in Ohaukwu, some pregnant women were found to hold two key misconceptions about CHWs. First, CHWs were at times mistaken for informal drug vendors, and second, CHWs were not perceived to be validated by the health system. This resulted in CHWs in these settings needing to overcome initial mistrust when approaching some pregnant women by addressing concerns over their intentions (ie, potential profit-seeking), the quality of the drug they are administering (ie, whether it is fake), and their validation and competence (ie, whether they are indeed qualified and backed by the health system).
The reason is that it [SP] is very important and then when she [CHW] first came to me I was afraid because it is risk to just take any drug even though my husband said I should not take it so when I called aunty nurse where I registered [for ANC] she now told me to collect it that it is very important, so it was then that I now have rest of mind to collect it. (IDI, pregnant woman, Akure South, Nigeria, 2021)
Involvement of key actors
C-IPTp implementation included community engagement strategies that promoted the participation of key actors namely, TBAs, community, and religious leaders, and traditional and local authorities. In Madagascar, Mozambique and Nigeria, findings showed engagement strategies went beyond seeking communities’ buy-in and support through dissemination and communication activities. In these settings, TBAs and community leaders were actively involved in implementation tasks, such as mapping of pregnant women and referral procedures.
Prior to the introduction of C-IPTp in Madagascar, TBAs were already providing regular support to facility-based healthcare staff and acting as an important referral point for pregnant women to attend ANC. In this setting, TBAs are often the first step in pregnant women’s care-seeking pathway to confirm their pregnancy and to receive advice and pregnancy-related therapies, such as herbal teas or massages. In addition to encouraging pregnant women to seek ANC at the health facility, TBAs often accompanied them to the ANC visits and provided support to midwives in health facilities lacking sufficient staff. The C-IPTp strategy, as implemented in this project, expanded this pre-existing collaboration between TBAs and the health system by engaging TBAs to collaborate with CHWs and facilitate the identification of new pregnant women, in addition to the ANC referrals they already conducted.
Because the two, TBA and CHW really work together, they can intervene when there are meetings. If there are women’s meetings, TBAs tell women that there will be a meeting and the TBAs and CHWs are present there. (FGD, relatives of PW, Vohipeno, Madagascar, 2021)
As part of the C-IPTp strategy, TBAs in Nigeria were actively involved in the referral of pregnant women to the health facility for ANC. In Bosso and Akure South, TBAs were provided with the same ANC referral forms as CHWs. TBAs used these forms to refer their clients to the health facility as a complement to the care they provide. In Bosso, TBAs were also involved in identifying and approaching new pregnant women to participate in C-IPTp. TBAs not only informed CHWs of new pregnancies, but also accompanied them during their first interaction with the pregnant woman in order to facilitate it. In Nigeria, TBAs received a transport allowance to participate in monthly meetings with project stakeholders to discuss their referral work. This transport allowance may have served as an incentive for TBAs’ continued engagement in the strategy.
On this day, we followed the CHW during their house-to-house identification of pregnant women in “X” community […] we noticed the CHW was waiting for us with a TBA at the facility […] We observed that the CHW handed the pregnant woman one referral form, while the TBA also handed over her own referral form. The two forms were to be taken back to the facility to use and register the pregnant woman.(Observation notes, Bosso, Nigeria, 2021)
In Mozambique, community leaders were actively engaged in regular dissemination and sensitisation activities, but also in addressing cases of C-IPTp refusal. LCCs and CHWs sought support of community leaders to address concerns of pregnant women who refused to participate in C-IPTp and seek her acceptance. In addition, some community leaders were recruited as LCCs.
CHWs’ working conditions
CHWs’ working condition is a theme that recurrently emerged throughout the study and across sites. CHWs, other health providers and other lay participants referenced what they perceived to be insufficient and untimely provision of transport allowances, as well as in-kind support and other means to carry out their tasks (ie, bicycles). The specific working conditions referred to by participants, and consequently, their motivation to deliver IPTp, differed across countries and within country sites. CHWs’ concerns with the lack of transport available to them were particularly salient in contexts where the characteristics of the topography and population density entailed larger and more arduous terrains to cover. For instance, sites like the districts of Meconta and Murrupula in Mozambique and all three study sites in Madagascar, where populations are sparsely distributed, the terrain is sandy and only one central road is paved, are examples of sites where the lack of transportation available to CHWs significantly complicated their day-to-day work.
Our bicycles broke down, we would like the project to help us with means of transport so we can work easier (…), it’s just that we always get tired of walking, because it can interrupt us to go to area X today, but for lack of transport due to this rain here and I couldn’t [go]. But with transport or means of transport we can manage it. (IDI, CHW, Meconta, Mozambique, 2021)
In Nigeria, CHWs in Bosso LGA faced similar mobility challenges while their counterparts in Akure South LGA—a predominantly urban setting—did not. With regard to the transport allowances, the extent to which they can function as incentives for CHWs is evidently relative to the cost of living in their setting. For instance, in the case of Nigeria, the value that CHWs placed in the stipends they received was significantly higher in Bosso LGA in comparison to CHWs in Akure South LGA, where the cost of living is higher.
That stipend [CHW transport allowance] is too small they were complaining so if that remuneration can be more than that, then that one will give them extra strength, they will go extra miles then to buy hmmmm card to their phone to call their client. (IDI, health provider, Akure South, Nigeria 2021)
Discussion
Study findings suggest that, overall, the C-IPTp approach was widely accepted by the different profiles of study participants. Moreover, insights from the retrospective analysis indicate that the acceptability of the intervention evolved, and that some factors that initially were deemed to be detrimental to acceptability were eventually ruled out or overcome, while others persisted throughout. The present discussion focuses on the ways in which each of the factors described in the results section influence the delivery, uptake and acceptability of C-IPTp as implemented by the TIPTOP project.
Relatives’ influence on pregnant women’s care-seeking decision-making processes can constitute a barrier to the uptake and delivery of C-IPTp. Their absence during CHW home visits can delay pregnant women’s uptake of C-IPTp and complicate adherence, and their refusal can bar pregnant women from participating in C-IPTp. In this light, the acceptability of C-IPTp from the perspective of husbands and relatives is key to its success. Previous studies conducted in African countries28 have identified similar ‘complex’29 or ‘gendered’30 decision-making processes that can delay pregnant women’s search for care and determine the acceptance of maternal health interventions.31
Beyond husband’s and relatives’ perspectives, pregnant women’s perceptions of SP for use in IPTp also shape their acceptance of the C-IPTp strategy. The perception that SP can induce adverse effects was a recurrent finding throughout the study that is mirrored in other qualitative studies on MiP prevention strategies. The reported effects (nausea, vomiting and dizziness) overlap with those identified in other studies.32–34 This perception undoubtedly constrains acceptance of the treatment and constitutes a significant barrier to its delivery, both at the health facility and via CHWs. Yet, the C-IPTp strategy may be able to overcome this in cases where the experience of adverse effects is attributed to consumption on an empty stomach, given that the nature of the delivery mechanism (ie, in pregnant women’s home) provides an opportunity for avoiding this.
The perceived superior quality of the packaged SP versus the one stored loose in jars is consistent with findings from other studies conducted in similar settings.35 Although the positive impact of packaging on perceptions of drug quality and efficacy is commonly reported, the influence of trust in the health provider also plays a role and may at times outweigh the impact of packaging preferences. This indicates that multiple factors are at play in patients’ perceptions of drug quality and may partly explain why this preference for the packaged SP was not identified evenly across our study sites. In our study, the perceived superior quality of the packaged SP delivered by CHWs compared with the non-packaged one delivered at health facilities undoubtedly encourages acceptance of C-IPTp, yet it may be a misleading opportunity. The unintended consequences that a preference for the SP delivered through one mechanism over the other could entail are unknown, although it could ultimately constitute a barrier to the acceptability of facility-based IPTp delivery.
The unquestioned efficacy of SP as a prophylactic drug against malaria is a clear opportunity for its administration, regardless of the delivery mechanism. This finding contrasts with findings from research conducted in the same study settings indicating that healthcare providers doubt the effectiveness of SP in preventing MiP.36 This hesitancy was not captured among any of the health providers targeted by our study.
The fact that lay persons’ confidence in the treatment’s efficacy can go hand in hand with a limited or non-specific understanding of its purpose has been described in a recent mixed-methods study on C-IPTp conducted in Nigeria.20 Both qualitative and quantitative results of that study reported low levels of awareness of IPTp among lay persons (including pregnant women) while a majority agreed that C-IPTp would improve the prevention of MiP. Similarly, a study on the acceptability of preventive interventions in Mozambique found that few pregnant women could distinguish the drugs provided to them during ANC (which included IPTp-SP) or point at the health problems targeted by each,37 yet all accepted taking them. The conclusions from these studies are consistent with our findings and suggest that perceptions of treatment efficacy may not be rooted in competent knowledge of the treatment itself, and that a non-specific understanding of the treatment may suffice to consider it effective and drive acceptance. This contrasts with other studies that strongly associate IPTp-SP acceptance to the adequacy or completeness of pregnant women’s knowledge of the treatment.36 38
Although a non-specific notion of IPTp efficacy may suffice to accept the treatment, it is likely that this needs to be coupled with a high degree of trust in the provider. The important role that trust plays in patient-provider relations for treatment acceptance and adherence has been well documented,39 as well as the centrality of trust to CHW–community relations.18 19 40 The exploratory phase of the study identified two key mechanisms that underpin communities’ trust in the delivery of IPTp via CHWs: ‘perceived competence’ and ‘community and healthcare system integration’.41 Communities’ perception of CHWs’ competence shapes their trust in them, and integration depends on the promotion of socially embedded practices and the involvement of formal healthcare systems in CHWs’ work.
Significant barriers to trust-building were identified in the initial phases of the study that directly affected the perceived competence of CHWs, namely: concerns over CHWs’ competence in administering SP (for for example, their ability to manage adverse effects of SP) and their presumed lack of specialised training in maternal healthcare. CHWs’ success in overcoming these is likely the result of their sustained efforts in sensitising and engaging their communities throughout the life of the project. These efforts were realised via one-to-one interactions and recurrent follow-ups with individual pregnant women, as well as via larger gatherings and events that involved other respected actors (both from within and outside the health system) that served to further validate their competencies and qualifications. However, context-specific misconceptions were still found to disrupt the functioning of trust-building mechanisms by the end of the project in the Nigerian urban study sites. This may be due to the characteristics specific to urban settings where informal drug markets are extensive and communities are less tight-knit, thus affecting the degree of social embeddedness of CHWs as well as the reach of community engagement activities. Other studies have described differences in the way CHWs operate in rural versus urban settings,18 though none have specifically assessed these in terms of trust.
Differences between study findings drawn from urban and rural settings suggest that adaptations may need to be made when implementing C-IPTp in diverse settings. With regard to nurturing trust in CHWs, special efforts may need to be made to gain the trust of pregnant women living in urban settings, by for instance strengthening community engagement and expanding communication strategies. With regard to CHWs’ working conditions, implementers may need to consider cost of living disparities between urban and rural settings before designing a one-size-fits-all approach to determining transport allowances and incentives.
Concerns over CHWs’ working conditions and their implications for their motivation to deliver IPTp may constitute a barrier to the acceptability of the intervention among different sectors of the community. In our study, these concerns were not only expressed in CHWs’ accounts, but also in those of other study participants, indicating a general awareness of the efforts that their (usually) voluntary activities entail. Our results do not differ from previous works describing common problems experienced by CHWs, ranging from delays in payments, insufficient resources and materials, and an increased workload.42–44 A survey conducted in Madagascar specifically points at the difficulty CHWs encounter when trying to reconcile voluntary work with other activities that constitute their main source of income.45 This is particularly relevant in resource-poor environments. This finding necessarily leads to reflections on how to ensure sufficient and timely remuneration and incentives in CHW programmes, while being cost-effective and sustainable—a public health debate that remains unresolved.46
The factors influencing pregnant women’s health-seeking pathways identified in our study challenged the intervention in different ways. Pregnancy disclosure norms mediated women’s social interactions, especially with health providers, both facility-based and CHWs, and determined women’s decision to reveal their pregnancy. Multiple studies have described women’s reluctance to reveal their pregnancy and how disclosing the pregnancy too early is perceived to result in harm to their unborn child or a ‘failed pregnancy’. These fears shape both their interactions with CHWs and their use of ANC services during the first trimester.47 Although these fears were decreasingly salient in participants’ accounts, pregnancy disclosure norms may persist as a relevant barrier to C-IPTp because they hinder early ANC attendance (as encouraged by the intervention), and constrain CHW identification of pregnant women in the community. Nevertheless, data also suggest that pregnancy disclosure norms were not fully disrupted by the delivery of SP through CHWs, since IPTp should be administered from the second trimester, when the belly is increasingly visible and thus harder to hide. In this regard, the contribution of TBAs as an enabling actor supporting CHWs in the identification of pregnant women should not be dismissed. Therefore, our findings point at the alignment of C-IPTp with existing pregnancy-related local norms as an opportunity for its acceptability and suggest that C-IPTp can contribute to a ‘positive pregnancy experience’, defined by the WHO as maintaining ‘socio-cultural normality’.3
Prior to the start of C-IPTp implementation, the utilisation of so-called ‘traditional medicine’ among pregnant women was foreseen as one of the potential obstacles to the delivery and acceptability of the intervention. It is often assumed that the demand for health services offered by traditional healers and TBAs limits the use of those provided through the formal biomedical system.48 Despite our initial findings, the cumulative data indicate that pregnant women usually combine different sources of care, meaning that different medical paradigms co-exist and therapeutic practices are fluid. Our findings are supported by previous works arguing that access to biomedical and non-biomedical care is often driven by practical decisions (ibid.), and that ‘traditional healers’ often refer patients to the health facility when they consider ‘conventional therapy’ is appropriate.49 50 In fact, TBAs have played an important role in implementation activities in many of the study settings. TBAs have already participated in community-based programmes as CHWs,43 and their trusted position within their communities helps overcome barriers to the acceptability, utilisation and demand for maternal and newborn services.51 In line with these works, our findings disrupt the static dichotomy between traditional practices and biomedicine and indicate that, overall, C-IPTp uptake and the use of non-biomedical sources of maternal healthcare are not mutually exclusive. This is, then, an opportunity for the acceptability of the intervention among all members of the community. Furthermore, these findings also provide meaningful insights into how community-based interventions could liaise with traditional healthcare providers in order to ensure trust and acceptance of such interventions among targeted communities.
C-IPTp necessarily reduces obstacles for accessing IPTp, and improves pregnant women’s self-efficacy in reaching part of the ANC services. Moreover, study findings do not suggest that C-IPTp deters pregnant women from seeking facility-based ANC. Yet barriers for attending facility-based maternal healthcare, most of which have been well documented in the literature,52–54 continue to be relevant to C-IPTp uptake and delivery. In our study, ANC-related costs, directly or indirectly generated by attending ANC, have been identified together with the perceived burden of the time spent seeking ANC, which is aligned with the data from other studies evaluating the TIPTOP project (Cirera, L. et al. Cost-effectiveness of community-based distribution of intermittent preventive treatment of malaria in pregnancy. Unpublished, 2022 Since one of the goals of the intervention is to promote ANC attendance and ensure that pregnant women follow-up with ANC at the health facility, structural barriers should be considered when assessing the acceptability of the intervention as a whole. Moreover, ANC access barriers are notably relevant to the success of C-IPTp delivery in countries where the first dose of IPTp-SP must be taken at the health facility, like Madagascar and Mozambique. For pregnant women living in these contexts, accessing their first dose of IPTp continues to be constrained by existing structural barriers to facility-based ANC, despite the implementation of C-IPTp.
Conclusions
The findings presented here strengthen the existing evidence on the acceptability of C-IPTp among different actors, and support the public health value of community-based interventions across a wide range of geographical, social, and epidemiological African settings. The C-IPTp strategy as implemented by the TIPTOP project was largely accepted by the targeted communities. The research findings presented here suggest that a series of key factors have influenced the acceptability and feasibility of the strategy. These include the alignment of the strategy with existing social norms surrounding pregnancy and pluralist maternal healthcare practices, the active involvement of influential and trusted actors (community leaders, TBAs) in implementation activities beyond standard community mobilisation and sensitisation activities, the influence of husbands and other relatives in pregnant women’s care-seeking decision-making, existing and sustained trust in CHWs, the working conditions of CHWs, pregnant women’s perceptions of SP for IPTp, and persistent barriers to ANC access. Overall, the findings suggest that the acceptability and feasibility of C-IPTp is underpinned by multiple factors that find different expressions when implemented in diverse sociocultural settings. With the above-mentioned factors adequately considered and addressed, the C-IPTp strategy has the potential to strongly contribute to the prevention of malaria in pregnancy with the acceptance and involvement of the communities it targets.
The use of conceptual frameworks to guide data collection and analysis across study sites is both a strength and a limitation of the study design. It is a limitation to the extent that their use may have led to the loss of local nuances, notably so because the choice and adaptation of the frameworks was informed by cross-cutting findings drawn from the exploratory phase. It is, however, a strength because it proved to be a successful strategy to mitigate the risk of researcher bias that a multisited qualitative study implemented by diverse research teams is inherently prone to. An additional strength aimed at mitigating researcher bias was the participation of research teams in yearly workshops focused on data analysis, intended to harmonise data interpretation and validate findings across teams. Another limitation worth noting is the effects that desirability bias may have had on research findings, a frequent challenge in social research. The effects of desirability bias may have been exacerbated by the social asymmetry underscoring the relationship between researchers and study populations, particularly in resource-poor settings where inequalities are more pronounced and harder to bridge.
Acknowledgments
The authors would like to thank all respondents who generously devoted their time to participate in the study, as well as the four research teams and field data collectors for their commitment and perseverance. In particular, we are grateful to Didier Mbombo Ndombe, Alain Mayembe (BÉGIS, DRC), Isabelle Nirina (MANISA, Madagascar), Iwara Arikpo, Peter Onyenemerem Nnanemerem, Chibueze Meremikwu, and Anthony Okoro (UNICAL, Nigeria), for their role in performing and coordinating the field data collection. We thank Christina Maly (Jhpiego) for her continuous support and for her valuable comments on this paper. We acknowledge support from the Spanish Ministry of Science and Innovation and State Research Agency through the 'Centro de Excelencia Severo Ochoa 2019-2023' Programme (CEX2018-000806-S), and support from the Generalitat de Catalunya through the CERCA Program.
Footnotes
Handling editor: Stephanie M Topp
Contributors: KM, CE-F, YA, FP and CM conceived and designed the study; WL, AMR, NMR, EM, HO and UJA conducted the data collection, supported by YA and CE-F. Data analysis was conducted by WL, AMR, NMR, HO, UJA, ON, MM, NT, YA and CE-F, and reviewed by FP, CM, KM, CS and MFM'E. The manuscript was conceptualised by YA and CE-F. KM and CE-F should be considered joint senior authors. CE-F and YA are the guarantors of the content of this manuscript. All authors contributed to revising the manuscript and provided approval of the final version. All authors read and approved the final manuscript.
Funding: This study was supported by UNITAID (2017-13-TIPTOP) through a subaward signed with Jhpiego (17-SBA-101).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Author note: The reflexivity statement for this paper is submitted in a online supplemental file 1.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The anonymised data that support the findings of this study are available from the corresponding author, YA, on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the WHO Ethics Review Committee (Geneva, Switzerland) - ERC.00030092, the Research Ethics Committee of the Hospital Clinic (Barcelona, Spain) - HCB/2017/10623, the Ethics Committee of the School of Public Health at the University of Kinshasa (DRC) - ESP/CE/047/20174, the Ethical Review Committee of Ebonyi state (Nigeria) - SMOH/ERC/062/20175, the Ethical Review Committee of Ondo state (Nigeria) - OSHREC 10/08/2017/2806, the Ethical Review Committee of Niger state (Nigeria) - STA/495/Vol/1467, the Biomedical Research Ethics Committee of the Ministry of Health (Madagascar) - 038-MSANP/SG/AMM/CERBM8, and the Institutional Health Bioethics Committee of the Centro de Investigação em Saúde de Manhiça (Mozambique) - CIBS-CISM/038. Participants gave informed consent to participate in the study before taking part.
References
- 1.Steketee RW, Nahlen BL, Parise ME, et al. The burden of malaria in pregnancy in malaria-endemic areas. Am J Trop Med Hyg 2001;64:28–35. 10.4269/ajtmh.2001.64.28 [DOI] [PubMed] [Google Scholar]
- 2.WHO . World malaria report 2021. Geneva, 2021. [Google Scholar]
- 3.World Health Organization . WHO recommendations on antenatal care for a positive pregnancy experience. Geneva, 2016. [PubMed] [Google Scholar]
- 4.Sicuri E, Bardají A, Nhampossa T, et al. Cost-effectiveness of intermittent preventive treatment of malaria in pregnancy in Southern Mozambique. PLoS One 2010;5:e13407. 10.1371/journal.pone.0013407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perry HB, Zulliger R, Rogers MM. Community health workers in low-, middle-, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health 2014;35:399–421. 10.1146/annurev-publhealth-032013-182354 [DOI] [PubMed] [Google Scholar]
- 6.Lewin S, Munabi-Babigumira S, Glenton C, et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev 2010:CD004015. 10.1002/14651858.CD004015.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruizendaal E, Schallig HDFH, Scott S, et al. Evaluation of malaria screening during pregnancy with rapid diagnostic tests performed by community health workers in Burkina Faso. Am J Trop Med Hyg 2017;97:1190–7. 10.4269/ajtmh.17-0138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gies S, Coulibaly SO, Ky C, et al. Community-based promotional campaign to improve uptake of intermittent preventive antimalarial treatment in pregnancy in Burkina Faso. Am J Trop Med Hyg 2009;80:460–9. [PubMed] [Google Scholar]
- 9.Mbonye AK, Schultz Hansen K, Bygbjerg IC, et al. Effect of a community-based delivery of intermittent preventive treatment of malaria in pregnancy on treatment seeking for malaria at health units in Uganda. Public Health 2008;122:516–25. 10.1016/j.puhe.2007.07.024 [DOI] [PubMed] [Google Scholar]
- 10.Burke D, Tiendrebeogo J, Emerson C, et al. Community-based delivery of intermittent preventive treatment of malaria in pregnancy in Burkina Faso: a qualitative study. Malar J 2021;20:277. 10.1186/s12936-021-03814-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kinyina A, Glorialoveness L, Chamos S. Impact of community intermittent preventive treatment in pregnancy (C-IPTp) approach on the uptake of IPTp3+: a randomized controlled trial in Karagwe, Tanzania. South Sudan Med J 2020;13:175–7. [Google Scholar]
- 12.Okedo-Alex IN, Akamike IC, Alo CN, et al. Reaching the unreached: effectiveness and satisfaction with community-directed distribution of sulfadoxine-pyrimethamine for preventing malaria in pregnancy in rural south-east, Nigeria. Malar J 2020;19:394. 10.1186/s12936-020-03468-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mbonye AK, Bygbjerg IC, Magnussen P. A community-based delivery system of intermittent preventive treatment of malaria in pregnancy and its effect on use of essential maternity care at health units in Uganda. Trans R Soc Trop Med Hyg 2007;101:1088–95. 10.1016/j.trstmh.2007.06.017 [DOI] [PubMed] [Google Scholar]
- 14.Gutman JR, Stephens DK, Tiendrebeogo J, et al. A cluster randomized trial of delivery of intermittent preventive treatment of malaria in pregnancy at the community level in Burkina Faso. Malar J 2020;19:282. 10.1186/s12936-020-03356-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okeibunor JC, Orji BC, Brieger W, et al. Preventing malaria in pregnancy through community-directed interventions: evidence from Akwa Ibom state, Nigeria. Malar J 2011;10:227. 10.1186/1475-2875-10-227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pons-Duran C, Llach M, Sanz S, et al. Community delivery of malaria intermittent preventive treatment in pregnancy: protocol of a quasi-experimental evaluation through multistage cluster sampling household surveys in four sub-Saharan African countries. BMJ Open 2021;11:e044680. 10.1136/bmjopen-2020-044680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cirera-Crivillé L, Llach M, González R, et al. Cost-Effectiveness of community-based distribution of intermittent preventive treatment of malaria in pregnancy (unpublished) 2022.
- 18.Kok MC, Ormel H, Broerse JEW, et al. Optimising the benefits of community health workers' unique position between communities and the health sector: a comparative analysis of factors shaping relationships in four countries. Glob Public Health 2017;12:1404–32. 10.1080/17441692.2016.1174722 [DOI] [PubMed] [Google Scholar]
- 19.Kok MC, Kea AZ, Datiko DG, et al. A qualitative assessment of health extension workers' relationships with the community and health sector in Ethiopia: opportunities for enhancing maternal health performance. Hum Resour Health 2015;13:80. 10.1186/s12960-015-0077-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okedo-Alex IN, Akamike IC, Nwafor JI, et al. Community malaria knowledge, experiences, perceived roles, and acceptability of Community-Directed distribution of intermittent preventive therapy for pregnancy in rural Southeast Nigeria. J Parasitol Res 2022;2022:1–12. 10.1155/2022/8418917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Charmaz K. Constructing grounded theory. Thousand Oaks, CA: SAGE, 2006. [Google Scholar]
- 22.Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17:88. 10.1186/s12913-017-2031-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011;38:65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kittle B. A practical guide to conducting a barrier analysis. New York: Helen Keller International, 2017. [Google Scholar]
- 25.Golden SD, Earp JAL. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav 2012;39:364–72. 10.1177/1090198111418634 [DOI] [PubMed] [Google Scholar]
- 26.Hammersley M, Atkins P. What is ethnography, in ethnography: principles in practice. London and New York: Tavistock Publications, 1983. [Google Scholar]
- 27.Neuendorf KA. Content analysis and thematic analysis. In: Research methods for applied psychologists: design, analysis and reporting. Routledge, 2019: 211–23. [Google Scholar]
- 28.Colvin CJ, Smith HJ, Swartz A, et al. Understanding careseeking for child illness in sub-Saharan Africa: a systematic review and conceptual framework based on qualitative research of household recognition and response to child diarrhoea, pneumonia and malaria. Soc Sci Med 2013;86:66–78. 10.1016/j.socscimed.2013.02.031 [DOI] [PubMed] [Google Scholar]
- 29.Munguambe K, Boene H, Vidler M, et al. Barriers and facilitators to health care seeking behaviours in pregnancy in rural communities of southern Mozambique. Reprod Health 2016;13 Suppl 1:31. 10.1186/s12978-016-0141-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hildon ZJ-L, Escorcio-Ymayo M, Zulliger R, et al. "We have this, with my husband, we live in harmony": exploring the gendered decision-making matrix for malaria prevention and treatment in Nampula Province, Mozambique. Malar J 2020;19:133. 10.1186/s12936-020-03198-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Magowan S, Burgoine K, Ogara C, et al. Exploring the barriers and facilitators to the acceptability of donor human milk in eastern Uganda - a qualitative study. Int Breastfeed J 2020;15:28. 10.1186/s13006-020-00272-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mubyazi G, Bloch P, Kamugisha M, et al. Intermittent preventive treatment of malaria during pregnancy: a qualitative study of knowledge, attitudes and practices of district health managers, antenatal care staff and pregnant women in Korogwe district, north-eastern Tanzania. Malar J 2005;4:31. 10.1186/1475-2875-4-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pell C, Meñaca A, Chatio S, et al. The acceptability of intermittent screening and treatment versus intermittent preventive treatment during pregnancy: results from a qualitative study in northern Ghana. Malar J 2014;13:432. 10.1186/1475-2875-13-432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rassi C, Graham K, King R, et al. Assessing demand-side barriers to uptake of intermittent preventive treatment for malaria in pregnancy: a qualitative study in two regions of Uganda. Malar J 2016;15:530. 10.1186/s12936-016-1589-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rutebemberwa E, Nsabagasani X, Pariyo G, et al. Use of drugs, perceived drug efficacy and preferred providers for febrile children: implications for home management of fever. Malar J 2009;8:131. 10.1186/1475-2875-8-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Faye SLB, Lugand MM. Participatory research for the development of information, education and communication tools to promote intermittent preventive treatment of malaria in pregnancy in the Democratic Republic of the Congo, Nigeria and Mozambique. Malar J 2021;20:223. 10.1186/s12936-021-03765-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boene H, González R, Valá A, et al. Perceptions of malaria in pregnancy and acceptability of preventive interventions among Mozambican pregnant women: implications for effectiveness of malaria control in pregnancy. PLoS One 2014;9:e86038. 10.1371/journal.pone.0086038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diala CC, Pennas T, Marin C, et al. Perceptions of intermittent preventive treatment of malaria in pregnancy (IPTp) and barriers to adherence in Nasarawa and cross river states in Nigeria. Malar J 2013;12:342. 10.1186/1475-2875-12-342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chandra S, Mohammadnezhad M, Ward P. Trust and communication in a Doctor- patient relationship: a literature review. J Healthc Commun 2018;03:36. 10.4172/2472-1654.100146 [DOI] [Google Scholar]
- 40.Mishra A. 'Trust and teamwork matter': community health workers' experiences in integrated service delivery in India. Glob Public Health 2014;9:960–74. 10.1080/17441692.2014.934877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Enguita-Fernàndez C, Alonso Y, Lusengi W, et al. Trust, community health workers and delivery of intermittent preventive treatment of malaria in pregnancy: a comparative qualitative analysis of four sub-Saharan countries. Glob Public Health 2021;16:1889–903. 10.1080/17441692.2020.1851742 [DOI] [PubMed] [Google Scholar]
- 42.Giugliani C, Duncan BB, Harzheim E, et al. Community health workers programme in Luanda, Angola: an evaluation of the implementation process. Hum Resour Health 2014;12:68. 10.1186/1478-4491-12-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Glenton C, Colvin CJ, Carlsen B, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev 2013:CD010414. 10.1002/14651858.CD010414.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Preston A, Okebe J, Balen J, et al. Involving community health workers in disease-specific interventions: perspectives from the Gambia on the impact of this approach. J Glob Health Rep 2019;3:e2019084. 10.29392/joghr.3.e2019084 [DOI] [Google Scholar]
- 45.Brunie A, Mercer S, Chen M, et al. Expanding understanding of community health worker programs: a cross-sectional survey on the work, satisfaction, and Livelihoods of CHWs in Madagascar. Inquiry 2018;55:0046958018798493. 10.1177/0046958018798493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haines A, Sanders D, Lehmann U, et al. Achieving child survival goals: potential contribution of community health workers. Lancet 2007;369:2121–31. 10.1016/S0140-6736(07)60325-0 [DOI] [PubMed] [Google Scholar]
- 47.Frumence G, Goodman M, Chebet JJ, et al. Factors affecting early identification of pregnant women by community health workers in Morogoro, Tanzania. BMC Public Health 2019;19:895. 10.1186/s12889-019-7179-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Burtscher D, Maukner AC, Piatti M, et al. “Where my pocket can afford is where I will take my child”. The influence of structural factors on the health-seeking behaviour of the population in Gorama Mende and Wandor chiefdoms, Kenema district, Sierra Leone. SSM - Qualitative Research in Health 2022;2:100067. 10.1016/j.ssmqr.2022.100067 [DOI] [Google Scholar]
- 49.Williams HAHA, Jones COH. A critical review of behavioral issues related to malaria control in sub-Saharan Africa: what contributions have social scientists made? Soc Sci Med 2004;59:501–23. 10.1016/j.socscimed.2003.11.010 [DOI] [PubMed] [Google Scholar]
- 50.Dalglish SL, Straubinger S, Kavle JA, et al. Who are the real community health workers in Tshopo Province, Democratic Republic of the Congo? BMJ Glob Health 2019;4:e001529. 10.1136/bmjgh-2019-001529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Orya E, Adaji S, Pyone T, et al. Strengthening close to community provision of maternal health services in fragile settings: an exploration of the changing roles of TBAs in Sierra Leone and Somaliland. BMC Health Serv Res 2017;17:460. 10.1186/s12913-017-2400-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bohren MA, Hunter EC, Munthe-Kaas HM, et al. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reprod Health 2014;11:71. 10.1186/1742-4755-11-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hill J, Hoyt J, van Eijk AM, et al. Factors affecting the delivery, access, and use of interventions to prevent malaria in pregnancy in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med 2013;10:e1001488. 10.1371/journal.pmed.1001488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grand-Guillaume-Perrenoud JA, Origlia P, Cignacco E. Barriers and facilitators of maternal healthcare utilisation in the perinatal period among women with social disadvantage: a theory-guided systematic review. Midwifery 2022;105:103237. 10.1016/j.midw.2021.103237 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2022-010079supp001.pdf (281.9KB, pdf)
Data Availability Statement
Data are available on reasonable request. The anonymised data that support the findings of this study are available from the corresponding author, YA, on reasonable request.


