Abstract
Objective
Risk factors predisposing infants to community-acquired bacterial infections during the first 2 months of life are poorly understood in South Asia. Identifying risk factors for infection could lead to improved preventive measures and antibiotic stewardship.
Methods
Five sites in Bangladesh, India and Pakistan enrolled mother–child pairs via population-based pregnancy surveillance by community health workers. Medical, sociodemographic and epidemiological risk factor data were collected. Young infants aged 0–59 days with signs of possible serious bacterial infection (pSBI) and age-matched controls provided blood and respiratory specimens that were analysed by blood culture and real-time PCR. These tests were used to build a Bayesian partial latent class model (PLCM) capable of attributing the probable cause of each infant’s infection in the ANISA study. The collected risk factors from all mother–child pairs were classified and analysed against the PLCM using bivariate and stepwise logistic multivariable regression modelling to determine risk factors of probable bacterial infection.
Results
Among 63 114 infants born, 14 655 were assessed and 6022 had signs of pSBI; of these, 81% (4859) provided blood samples for culture, 71% (4216) provided blood samples for quantitative PCR (qPCR) and 86% (5209) provided respiratory qPCR samples. Risk factors associated with bacterial-attributed infections included: low (relative risk (RR) 1.73, 95% credible interval (CrI) 1.42 to 2.11) and very low birth weight (RR 5.77, 95% CrI 3.73 to 8.94), male sex (RR 1.27, 95% CrI 1.07 to 1.52), breathing problems at birth (RR 2.50, 95% CrI 1.96 to 3.18), premature rupture of membranes (PROMs) (RR 1.27, 95% CrI 1.03 to 1.58) and being in the lowest three socioeconomic status quintiles (first RR 1.52, 95% CrI 1.07 to 2.16; second RR 1.41, 95% CrI 1.00 to 1.97; third RR 1.42, 95% CrI 1.01 to 1.99).
Conclusion
Distinct risk factors: birth weight, male sex, breathing problems at birth and PROM were significantly associated with the development of bacterial sepsis across South Asian community settings, supporting refined clinical discernment and targeted use of antimicrobials.
Keywords: infections, diseases, disorders, injuries; cohort study; paediatrics; child health
WHAT IS ALREADY KNOWN ON THIS TOPIC
Several different risk factors for neonatal sepsis—determined from a constellation of symptoms in hospitalised infants often lacking access to modern diagnostic techniques in low resource settings—have been used in management guidelines for all sepsis arising in community settings.
WHAT THIS STUDY ADDS
This study analyses the risk factors associated with community-acquired young infant infections with bacterial aetiologies in five sites across three South Asian countries. These risk factors were used to construct multivariate models using stepwise regression for community-acquired bacterial infections by directly using a partial latent class model output derived from advanced laboratory diagnostics identifying aetiologies, building a common risk model for community-acquired neonatal sepsis across South Asia.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Given this study of the risk factors associated with bacterial infections in young infants among a heterogeneous community field sites in South Asia, these data and findings may factor into refinement of point-of-care risk scoring algorithms, improvement of traditional treatment algorithms and, if further validated, be used to provide appropriate and judicious use of antibiotics.
Introduction
Despite coordinated efforts to reduce child mortality over the past decade, deaths due to neonatal infections remain a major contributor to under-five mortality. With recent advances in other areas of child health, neonatal deaths comprise an increasing proportion of under-five mortality.1–3 Neonatal sepsis, pneumonia and meningitis have been estimated to cause a quarter of all newborn deaths,4 and this proportion might be even higher.5 South Asia and sub-Saharan Africa have the greatest burden of neonatal sepsis in the world.6 The Alliance for Maternal and Newborn Health Improvement (AMANHI) study found severe neonatal infections to be the second leading cause of neonatal deaths after perinatal asphyxia in South Asia (35%, 34–36) and sub-Saharan Africa (37%, 34–39).7 The WHO recognises sepsis as a global health priority in the coming decade,8 with the highest incidence of sepsis among neonates and young children. New solutions to address serious infections in young children are needed in order to achieve Sustainable Development Goal 3.2 to ‘End preventable deaths of newborns and children under age five years of age with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1000 live births and under-five mortality to at least as low as 25 per 1000 live births’.9
Data are scarce on risk factors and aetiology of community-acquired serious infections in developing countries.10–21 Laboratory confirmation of the aetiology of bacterial infections is particularly lacking in community (non-healthcare) settings where most infections take place. Empirical antibiotic treatment for a constellation of neonatal sepsis symptoms predominates21–25 and treatment regimens vary both between and within regions.24 Meanwhile, the use of neonatal risk factor scoring for guiding management decisions for possible serious bacterial infections (pSBI) has shown utility for improving antibiotic stewardship and reducing neonatal early-onset sepsis-based mortality.26–31 These approaches, however, are largely based on symptoms in hospitalised infants. High-quality community-based data regarding risk factors for infections may serve to inform preventive policies and clinical practices surrounding neonatal sepsis; possibly including improved scoring algorithms.
The Aetiology of Neonatal Infection in South Asia (ANISA) study was designed32–34 to increase understanding of factors that predispose young infants to, or protect them from, infections at the community level and to provide data to inform evidence-based strategies to reduce neonatal infections and mortality. Here we use data from five diverse community-based urban and rural ANISA sites to explore risk factors predisposing young infants in South Asia to contracting serious infections attributable to bacterial pathogens.34
Methods
ANISA was a longitudinal community-based prospective cohort study of mother–infant pairs drawn from five population-based sites in Bangladesh, India and Pakistan from 2011 to 2014. Study site characteristics and sepsis surveillance methodologies have been described elsewhere.32 In brief, active pregnancy surveillance was established by community health workers (CHWs) who registered all consenting married women of reproductive age in each catchment area. CHWs and study physicians collected a variety of information from mothers using standardised questionnaires administered during the earliest stages of pregnancy, shortly after childbirth and during 59-day longitudinal follow-up of infants. Data were collected on risk factors including participant demographics, home environment, pregnancy and birth history, postpartum maternal characteristics and neonatal characteristics at birth (see web online supplemental tables 1–5). CHWs visited mothers and newborns up to 10 times, thrice in the first week after birth and weekly thereafter until 59 days after birth. Infants presenting with one or more of seven clinical signs of pSBI were referred to study physicians. The signs used to identify pSBI included feeding poorly or not feeding at all, no movement at all or movement only when stimulated, fast breathing (≥60 breaths/min), elevated temperature (>38°C), hypothermia (<35.5°C), chest in-drawing and convulsions.31 32 On physician diagnosis of pSBI, blood specimens were taken for conventional blood culture and blood and nasopharyngeal (NP) swab specimens were taken for multipathogen quantitative real-time PCR (qPCR) analysis; detailed methods to determine aetiologies of infection are described elsewhere2 33 and these data are used in this analysis. Age-matched and site-matched control newborn infants were identified35 and were assessed by study physicians to rule out the presence of clinical signs of pSBI. Blood and NP swab samples were collected to identify the presence of pathogen-derived nucleic acid in non-symptomatic control infants using qPCR; conventional blood culture was not performed on control specimens.33 35 These control specimens were used to inform the false positivity rate in the Partial Latent Class Model (PLCM). Quality of field surveillance and laboratory procedures and processes was maintained by consistent monitoring of field and laboratory operations and tracking of specimens using a purpose-built digital tracking system at all sites as described previously.36
bmjgh-2022-009706supp001.pdf (170.2KB, pdf)
Patient and public involvement
The study was developed together with multidisciplinary teams based at each of the five study sites; a common protocol and questionnaire was developed and customised for use in the local languages and circumstances. CHWs were recruited from the local communities but patients (mother–child pairs) were not directly involved in the design of the questionnaires, study recruitment, diagnostic, scientific or statistical methods used to analyse their data. Findings will be disseminated by the local partners to clinics that serve the communities, and findings may be more broadly shared in their respective regions by the study site teams.
Statistical analysis
The risk factor analysis reported here directly used the ANISA Bayesian PLCM attribution data that have been reported previously. Wherein each young infant with pSBI (based on the presence of one or more of seven danger signs) underwent blood culture and both blood and respiratory qPCR assays; pathogen(s) may have been detected in one or more of these tests. Blood culture results were further characterised as definite pathogens versus contaminants using an expert panel that systematically reviewed clinical and diagnostic information on each case.37 In order to properly attribute a particular child’s pSBI to a specific pathogen type, the output from each of these analyses were integrated into a PLCM combining the multiple tests along with their different error rates as described previously.2 38 39 The output of this model was mean pathogen proportions of 28 target pathogens and two additional classes: other blood culture (all organisms isolated from blood culture that did not have a matching molecular assay test) and other/none (if no aetiology was attributed). These proportions were performed at individual level with 95% credible intervals (CrIs). Performance of this modelling was assessed by internal simulation studies; model convergence was assessed through trace and other diagnostic plots. The programming and computation of the PLCM was performed with R (V3.2.5), SAS (V.9.3) and Stata (V.13.1) and was reported previously.2
For the risk factor analysis reported here, 50 complete PLCM output sets were selected at random from a set of 2000 complete, stable, PLCM output runs; inclusion of additional sets was not found to stabilise or notably alter risk factor output. These iterations were then further randomly resorted for each child to produce 50 synthetic model outputs for analysis.
Multiple imputation function was used to perform and combine analyses of these randomised 50 model output sets against each of the potential risk factors using stepwise logistic multivariable multiple regression modelling; multiple imputation allowed for combining the resulting point estimates from 50 runs to account for the uncertainty in the outcome in the intervals around the given risk factor estimates.40 Multiple imputation was not used to correct for incomplete data in the underlying risk factor dataset, but rather to combine the PLCM estimates of pathogen attribution and given risk factor into a single estimate and variance, incorporating both the within-imputation and between-imputation variability.40 Bivariate analysis on each putative risk factor’s impact on bacterial infection was performed first. Using these outputs, a multivariable regression model was constructed within each of five predefined risk domains (neonatal, maternal, birth procedure, environmental and demographic factors), controlling for site. Nested, circular variables such as duration of hospitalisation after birth and whether a young infant was reportedly ever hospitalised were removed from multivariable modelling. Using stepwise elimination of non-significant factors, the remaining significant factors in each risk domain were then combined into the final risk model. Risk factors with p value ≤0.10 and relative risk (RR) values either above 1.1, signifying risk, or below 0.9090, signifying protection, were considered as having statistical significance. Models were then combined in the following order: neonatal health factors, maternal factors, birth procedure factors, environmental factors and finally demographic factors. This analysis was performed in Stata (V.13.1 SE).
Low birth weight (LBW) was defined as 1500–2500 g and very LBW (VLBW) as <1500 g. Nutritional risk status of mothers was defined by mid-upper-arm circumference, with high nutritional risk <20.7 cm and moderate nutritional risk <23 cm.41 Moderate/late preterm birth was defined as birth at 32–37 weeks’ gestation, and very and extremely preterm was defined as <32 weeks’ gestation. Premature rupture of membranes (PROM) was defined as water breaking before onset of labour pain. The country-specific wealth index and household wealth quintiles were calculated using information on durable household assets, construction materials, utilities, etc.42 43
Results
Population characteristics
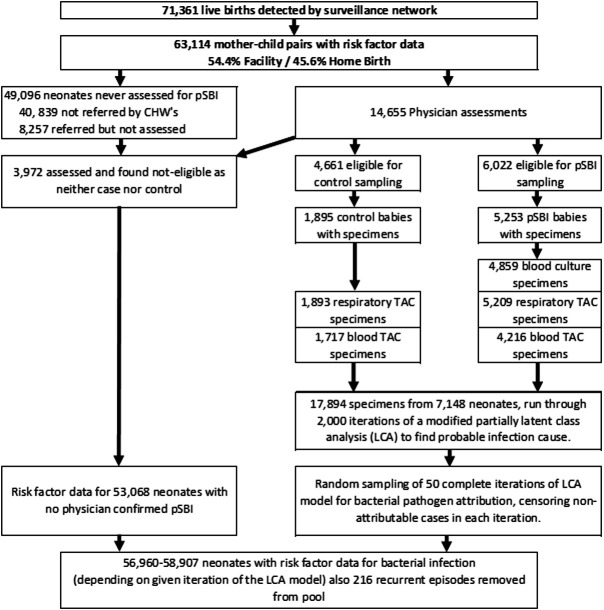
Between November 2011 and March 2014, we enrolled 63 114 newborn–mother pairs and followed them until the infants were 2 months old (figure 1); 73.9% (n=46 673) of the newborns were registered within 24 hours of birth and the rest (26.1%, n=16 441) between their second and seventh days after birth. Among the registered newborns, 51% (n=32 419) were male, 27% (n=16 832) were born with LBW and 19% (n=11 837) were preterm. Mothers of 47.3% (n=29 840) of the infants attended at least four antenatal care visits, 63.7% (n=40 186) of the deliveries took place in healthcare facilities and 67.6% (n=42 669) of infants received colostrum. There were 6022 pSBI episodes identified by study physicians, resulting in the collection and analysis of 4859 blood specimens (80.6% of those indicated) and 5209 respiratory specimens (86.5%). We also collected 1717 blood specimens and 1893 respiratory specimens from 4661 age-matched and site-matched healthy control participants.
Figure 1.
Characteristics of the infants enrolled and analysed in the ANISA study. ANISA, Aetiology of Neonatal Infection in South Asia; CHWs, community health workers; pSBI, possible serious bacterial infection; TAC, TaqMan® Array Card
Neonatal health status factors
We analysed eight neonatal factors, five of which were significantly associated with bacterial infection in bivariate analysis (online supplemental table 1). Multivariable analysis of neonatal factors alone, controlling for site, showed that LBW (RR 1.76, 95% CrI 1.45 to 2.13), VLBW (RR 6.20, 95% CrI 4.05 to 9.51), male sex (RR 1.27, 95% CrI 1.07 to 1.52) and problems with breathing initiation at birth (RR 2.54, 95% CrI 2.01 to 3.21) were associated with increased risk of bacterial infections (table 1).
Table 1.
Neonatal risk factors multivariate model – all sites
| Bacterial infection | |||
| Relative risk | P value | 95% CrI | |
| Sylhet, Bangladesh | 1.00 | ||
| Karachi, Pakistan | 1.23 | 0.110 | 0.95 to 1.60 |
| Matiari, Pakistan | 0.86 | 0.263 | 0.65 to 1.12 |
| Vellore, India | 1.35 | 0.098 | 0.95 to 1.91 |
| Odisha, India | 2.81 | 0.000*** | 2.17 to 3.63 |
| Birth weight (normal birth weight >2500 g baseline) | |||
| Low birth weight <2500 g | 1.78 | 0.000*** | 1.47 to 2.16 |
| Very low birth weight <1500 g | 6.19 | 0.000*** | 4.03 to 9.51 |
| Sex | |||
| Male | 1.28 | 0.006** | 1.07 to 1.53 |
| Breathing initiation problems at birth | 2.55 | 0.000*** | 2.01 to 3.24 |
| Constant | 0.01 | 0.000*** | 0.01 to 0.01 |
| Sample size variation | n=56 960–57 038 | ||
Exponentiated coefficients.
*P<0.05, **p<0.01, ***p<0.001.
CrI, credible interval.
Maternal factors
We analysed 24 maternal risk factors, and six were found to be associated with the development of bacterial infections in bivariate analysis (online supplemental table 2). Multivariable analysis of maternal factors alone, while controlling for site, revealed that having one (RR 0.73, 95% CrI 0.58 to 0.92) or two (RR 0.68, 95% CrI 0.51 to 0.92) prior births and having four or more antenatal care visits (RR 0.74, 95% CrI 0.57 to 0.96) were significantly protective against risk of bacterial infection (table 2).
Table 2.
Maternal risk factors multivariate model – all sites
| Bacterial infection | |||
| Relative risk | P value | 95% CrI | |
| Sylhet, Bangladesh | 1.00 | ||
| Karachi, Pakistan | 1.17 | 0.267 | 0.89 to 1.54 |
| Matiari, Pakistan | 1.05 | 0.734 | 0.79 to 1.40 |
| Vellore, India | 1.46 | 0.094 | 0.94 to 2.28 |
| Odisha, India | 2.47 | 0.000*** | 1.88 to 3.24 |
| Prior children | |||
| No prior children | |||
| 1 child | 0.73 | 0.008** | 0.58 to 0.92 |
| 2 children | 0.68 | 0.012* | 0.51 to 0.92 |
| 3+ children | 0.94 | 0.613 | 0.75 to 1.18 |
| Antenatal care visits (ANC) | |||
| No ANC visits | |||
| 1 ANC visit | 0.83 | 0.261 | 0.59 to 1.15 |
| 2 ANC visits | 0.94 | 0.692 | 0.69 to 1.28 |
| 3 ANC visits | 0.96 | 0.774 | 0.71 to 1.29 |
| 4+ ANC visits | 0.74 | 0.024* | 0.57 to 0.96 |
| Constant | 0.01 | 0.000*** | 0.01 to 0.02 |
| Sample size variation | n=57 974–58 058 | ||
Exponentiated coefficients.
*P<0.05, **p<0.01, ***p<0.001.
CrI, credible interval.
Birth procedure risk factors
Nineteen risk factors surrounding the birth event were analysed; six factors related to birth procedures and behaviours of the birth team were significant (online supplemental table 3). Multivariable analysis of birth procedure factors showed that presenting with PROM (RR 1.29, 95% CrI 1.04 to 1.60) was the only birth-procedure related factor that increased risk of bacterial infection (table 3).
Table 3.
Birth procedure risk factor multivariate model – all sites
| Bacterial infection | |||
| Relative risk | P value | 95% CrI | |
| Sylhet, Bangladesh | 1.00 | ||
| Karachi, Pakistan | 1.22 | 0.13 | 0.94 to 1.58 |
| Matiari, Pakistan | 0.99 | 0.94 | 0.76 to 1.30 |
| Vellore, India | 1.01 | 0.95 | 0.71 to 1.44 |
| Odisha, India | 2.16 | 0.000*** | 1.67 to 2.79 |
| Premature rupture of membranes | 1.29 | 0.019* | 1.04 to 1.60 |
| Constant | 0.01 | 0.000*** | 0.01 to 0.01 |
| Sample size variation | n=58 822–58 906 | ||
Exponentiated coefficients.
*P<0.05, **p<0.01, ***p<0.001.
CrI, credible interval.
Environmental factors
Twelve risks were analysed related to the immediate environment encountered following birth. Two factors were found to be independently significant (online supplemental table 4). Multivariable analysis of environmental factors showed that having unsanitary or no formal toilet facilities (RR 1.32, 95% CrI 1.01 to 1.71) and lack of household hand washing facilities (RR 1.34, 95% CrI 1.03 to 1.74) increased the risk of bacterial infections. Also, being situated in Odisha, India (RR 2.71, 95% CrI 1.97 to 3.74) and Karachi, Pakistan (RR 1.57, 95% CrI 1.15 to 2.15) showed significantly increased risk compared with Sylhet, Bangladesh (table 4).
Table 4.
Environmental risk factors multivariate model – all sites
| Bacterial infection | |||
| Relative risk | P value | 95% CrI | |
| Sylhet, Bangladesh | 1.00 | ||
| Karachi, Pakistan | 1.57 | 0.005** | 1.15 to 2.15 |
| Matiari, Pakistan | 1.24 | 0.154 | 0.92 to 1.66 |
| Vellore, India | 1.22 | 0.308 | 0.83 to 1.81 |
| Odisha, India | 2.71 | 0.000*** | 1.97 to 3.74 |
| Toilet facilities | |||
| Flush toilet | 1.00 | ||
| Latrine/VIP latrine | 1.32 | 0.041* | 1.01 to 1.71 |
| Unsanitary or no formal Toilet | 1.16 | 0.213 | 0.92 to 1.48 |
| Unknown | 0.75 | 0.647 | 0.22 to 2.56 |
| No hand washing facilities in home | 1.34 | 0.028* | 1.03 to 1.74 |
| Constant | 0.01 | 0.000*** | 0.01 to 0.01 |
| Sample size variation | n=58 823 –58 907 | ||
Exponentiated coefficients.
*P<0.05, **p<0.01, ***p<0.001.
CrI, credible interval.
Demographic factors
Five demographic risk factors were analysed related to parental education, maternal work and decision making in the household (online supplemental table 5). Only socioeconomic status (SES) was found to be independently significant. Bacterial infection risk was significantly elevated in Odisha (RR 2.32, 95% CrI 1.82 to 2.97) when compared with Sylhet. Multivariable analysis of demographic factors revealed that only low SES was associated with significantly elevated risk of bacterial infection in the first (RR 1.78, 95% CrI 1.35 to 2.36), second (RR 1.64, 95% CrI 1.24 to 2.19) and third (RR 1.62, 95% CrI 1.20 to 2.17) wealth quintiles when compared with the fifth (wealthiest) SES quintile (table 5).
Table 5.
Demographic risk factors multivariate model – all sites
| Bacterial infection | |||
| Relative risk | P value | 95% CrI | |
| Sylhet, Bangladesh | 1.00 | ||
| Karachi, Pakistan | 1.20 | 0.152 | 0.93 to 1.55 |
| Matiari, Pakistan | 1.10 | 0.471 | 0.85 to 1.43 |
| Vellore, India | 1.03 | 0.858 | 0.73 to1.45 |
| Odisha, India | 2.32 | 0.000*** | 1.82 to 2.97 |
| Socioeconomic status | |||
| Fifth quintile (highest) | |||
| Fourth quintile | 1.33 | 0.068 | 0.98 to 1.80 |
| Third quintile | 1.62 | 0.001*** | 1.20 to 2.17 |
| Second quintile | 1.64 | 0.001*** | 1.24 to 2.19 |
| First quintile (lowest) | 1.78 | 0.000*** | 1.35 to 2.36 |
| Constant | 0.01 | 0.000*** | 0.01 to 0.01 |
| Sample size variation | n=58 368–58 452 | ||
Exponentiated coefficients.
*P<0.05, **p<0.01, ***p<0.001.
CrI, credible interval.
Full multivariable model results
Pooled multivariable analysis showed that VLBW (<1500 g) increased risk of bacterial infection more than fivefold (RR 5.77, 95% CrI 3.73 to 8.94), and LBW (<1500–2500 g) remained a significantly elevated risk factor (RR 1.73, 95% CrI 1.42 to 2.11). Breathing initiation problems at birth (RR 2.50, 95% CrI 1.96 to 3.18) and male sex (RR 1.27, 95% CrI 1.07 to 1.52) also were associated with increased risk of bacterial infection (table 6). PROM was also a significant risk factor in the final model (RR 1.27, 95% CrI 1.03 to 1.58). Having one or two prior children, as well as a non-flush toilet and lack of hand washing facilities all lost significance with the addition of SES into the overall model. Being part of the lowest three SES quintiles, compared with the top/wealthiest quintile, remained a significant risk factor in the final model (first RR 1.52, 95% CrI 1.07 to 2.16; second RR 1.41, 95% CrI 1.00 to 1.97; third RR 1.42, 95% CrI 1.01 to 1.99).
Table 6.
Overall multivariate bacterial infection risk factor model
| Neonatal factors | + Maternal factors | + Birth procedure factors | + Environmental factors | + Demographic factors | ||||||
| Relative risk | 95% CrI | Relative risk | 95% CrI | Relative risk | 95% CrI | Relative risk | 95% CrI | Relative risk | 95% CrI | |
| Sylhet, Bangladesh | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . | 1.00 | . |
| Karachi, Pakistan | 1.23 | 0.95 to 1.60 | 1.28* | 0.98 to 1.68 | 1.29 | 0.98 to 1.69 | 1.62** | 1.18 to 2.26 | 1.49* | 1.06 to 2.09 |
| Matiari, Pakistan | 0.86 | 0.65 to 1.12 | 0.87 | 0.66 to 1.15 | 0.81 | 0.61 to 1.08 | 0.91 | 0.67 to 1.24 | 0.92 | 0.67 to 1.25 |
| Vellore, India | 1.35* | 0.95 to 1.91 | 1.65* | 1.11 to 2.47 | 1.67* | 1.12 to 2.50 | 1.96** | 1.26 to 3.04 | 1.84* | 1.18 to 2.88 |
| Odisha, India | 2.81*** | 2.17 to 3.63 | 3.21*** | 2.42 to 4.26 | 3.06*** | 2.30 to 4.08 | 3.47*** | 2.44 to 4.94 | 3.47*** | 2.42 to 4.96 |
| Birth weight (>2500 g baseline) | ||||||||||
| Low birth weight <2500 g | 1.78*** | 1.47 to 2.16 | 1.78*** | 1.46 to 2.17 | 1.78*** | 1.46 to 2.16 | 1.76*** | 1.45 to 2.15 | 1.73*** | 1.42 to 2.11 |
| Very low birth weight <1500 g | 6.19*** | 4.03 to 9.51 | 6.25*** | 4.07 to 9.60 | 6.24*** | 4.07 to 9.58 | 6.11*** | 3.98 to 9.39 | 5.77*** | 3.73 to 8.94 |
| Male sex | 1.28** | 1.07 to 1.53 | 1.27** | 1.07 to 1.52 | 1.27** | 1.07 to 1.52 | 1.27** | 1.07 to 1.52 | 1.27** | 1.07 to 1.52 |
| Breathing problems at birth | 2.55*** | 2.01 to 3.24 | 2.55*** | 2.01 to 3.24 | 2.53*** | 1.99 to 3.22 | 2.51*** | 1.98 to 3.20 | 2.50*** | 1.96 to 3.18 |
| Antenatal care visits (ANCs) (no visits baseline) | ||||||||||
| 1 ANC visit | 0.81 | 0.58 to 1.14 | 0.82* | 0.58 to 1.15 | 0.85 | 0.60 to 1.19 | 0.86 | 0.61 to 1.21 | ||
| 2 ANC visits | 0.95 | 0.69 to 1.29 | 0.94 | 0.69 to 1.29 | 0.97 | 0.71 to 1.33 | 0.99 | 0.72 to 1.37 | ||
| 3 ANC visits | 1.00 | 0.74 to 1.36 | 0.99 | 0.73 to 1.35 | 1.03 | 0.76 to 1.40 | 1.05 | 0.77 to 1.44 | ||
| 4+ ANC visits | 0.79* | 0.60 to 1.04 | 0.79* | 0.60 to 1.03 | 0.83 | 0.63 to 1.09 | 0.88 | 0.66 to 1.17 | ||
| Prior children (no prior children baseline) | ||||||||||
| 1 child | 0.81 | 0.64 to 1.02 | 0.81* | 0.64 to 1.03 | 0.81* | 0.64 to 1.02 | 0.80 | 0.63 to 1.02 | ||
| 2 children | 0.78 | 0.58 to 1.05 | 0.78 | 0.58 to 1.05 | 0.77* | 0.57 to 1.04 | 0.76 | 0.56 to 1.02 | ||
| 3+ children | 1.09 | 0.86 to 1.37 | 1.09 | 0.86 to 1.38 | 1.07 | 0.84 to 1.35 | 1.03 | 0.81 to 1.32 | ||
| PROM | 1.26* | 1.02 to 1.57 | 1.26* | 1.02 to 1.56 | 1.27* | 1.03 to 1.58 | ||||
| Toilet facilities (flush toilet baseline) | ||||||||||
| Latrine/VIP latrine | 1.27* | 0.97 to 1.66 | 1.15 | 0.86 to 1.53 | ||||||
| Unsanitary or no formal toilet | 1.09 | 0.85 to 1.40 | 0.94 | 0.71 to 1.25 | ||||||
| No handwashing station in home | 1.28* | 0.98 to 1.67 | 1.21 | 0.92 to 1.58 | ||||||
| Socioeconomic status (fifth/top quintile baseline) | ||||||||||
| Fourth quintile | 1.26 | 0.92 to 1.75 | ||||||||
| Third quintile | 1.42* | 1.01 to 1.99 | ||||||||
| Second quintile | 1.41* | 1.00 to 1.97 | ||||||||
| First (bottom) quintile | 1.52* | 1.07 to 2.16 | ||||||||
| Constant | 0.01*** | 0.01 to 0.01 | 0.02 | 0.01 to 0.01*** | 0.01*** | 0.01 to 0.01 | 0.01*** | 0.00 to 0.01 | 0.00*** | 0.00 to 0.01 |
| Sample variation across imputations | 56 960 to 57 038 | 56 147 to 56 229 | 56 146 to 56 228 | 56 146 to 56 228 | 55 719 to 55 801 | |||||
Exponentiated coefficients.
*P<0.10, **p<0.01, ***p<0.001.
CrI, credible interval; PROM, premature rupture of membrane.
Discussion
This analysis, through examination of risk factors in rural and urban communities across five sites in three countries, found that a small set of factors—VLBW/LBW, male sex, PROM and breathing problems at birth and SES—were significantly associated with laboratory-confirmed bacterial infections. These factors can be directly observed at birth, except for SES. These findings are congruent with simplified clinical decision making and may support development of algorithms that can be used to improve antibiotic stewardship in the Indian subcontinent. Taking clinical presentation of risk factors into decision making could allow for improved targeting of scarce resources and antibiotic therapy. Moreover, these findings suggest that aggressive strategies that combat poverty are important in reducing risk for bacterial infections.
Results from this analysis are consistent with other studies—including a recent systematic review and meta-analysis of 15 studies in India—that found that risk factors for neonatal sepsis included low gestational age, male sex, breathing problems at birth and PROM, among other factors such as home birth.19 20 44 Some results from this analysis were surprising, particularly that several reported birth procedure-related risk factors lost significance in multivariable analysis; non-facility/home birth, lack of use of a non-sterile instrument or materials to cut and tie the umbilicus were significant bivariate factors but lost significance in multivariable modelling. Similarly, maternal antenatal care and unsanitary or no formal toilet facilities and lack of household hand washing facilities lost significance in multivariable modelling. Other factors, such as frequent vaginal exams, the presence of skilled birth attendants, birth attendant hand washing and feeding of colostrum were not found to be significant risk factors, even during bivariate analysis. Other studies had previously identified unhygienic intrapartum and postnatal care, poor prelacteal feeding and contaminated foods and fluids as important contributors to the pathogenesis of neonatal infection and priorities in prevention of newborn infections.44 45
Male children have been shown to have a greater biological risk than females who often have heightened social risks for infection later in life.46–48 Future analysis stratifying by sex could add insight and contribute to corrective strategies. A similar risk factor analysis on viral aetiology within the ANISA study is forthcoming, along with other important related risk analyses, such as aetiology-specific (Respiratory Syncytial Virus, RSV & Group B Streptococcus, GBS), recurrent infections and mortality.
Over the past decades, a variety of management guidelines for neonatal infections have been developed to manage newborn infants with suspected infections. These guidelines were deliberately based on high sensitivity in identifying potential cases, leading to overtreatment and potentially contributing to concomitant high rates of antimicrobial resistance (AMR).49 50 Although community-based use of antibiotics for pSBI has been shown to reduce neonatal mortality,23 51–55 the fear of missing a potentially treatable infection leads to overprescription of broad-spectrum empirical antibiotics with the attendant potential for side effects and propagation of AMR.56 Our Bayesian PLCM analysis directly used the heterogeneous samples and test outputs from the ANISA study pathogen attribution. It used the true error rates to assign relative risks associated with bacterial infection in South Asia.
These findings provide important insights into those factors which, if addressed, have potential to target bacterial sepsis cases, reducing cost, morbidities and case fatalities among infants across the subcontinent and beyond. Importantly, most of these factors are readily detectable at birth, allowing early intervention using targeted protocols and training in the community setting. Improving targeting of empiric antibiotic treatments to the most at-risk infants early has the potential to improve case management, reduce morbidity and mortality and limit unnecessary empirical antibiotic treatment and potential emergence of AMR.
Limitations
Despite testing of both blood and respiratory samples, prior analysis showed that no cause could be attributed to 72% of pSBI episodes and only 11% of infants who died had samples taken within 7 days of death.2 This impacts the availability of pathogen data in the underlying attribution model, which feeds into this risk analysis. However, it should be noted that the number of attributable infections was nearly double among those babies who died compared with those who did not and more than 90% of those were bacterial infections and are thus included in this model. Design of new initiatives has already begun to fill this knowledge gap.57
For young children who were either born in medical facilities and stayed for long periods due to the detection of clinical symptoms at birth or neonates who contracted a nosocomial infection while in medical facilities and were kept for treatment, the risk factors collected regarding length of hospital stay became highly circular. This made it difficult to parse whether the hospital stay was the source of the infection (nosocomial) or hospitalisation was due to the community acquisition of the infection. Therefore, risk presented by ‘time spent in hospital’, although a major factor in risk for infection, was removed from multivariable analyses to avoid this bias in favour of community-based acquisition of infections (online supplemental table 3).
Specific timing of onset of symptoms, treatment course/duration, coinfections and other clinical factors were not considered in this aggregate analysis. Data on Apgar scores and caesarean section status were not collected, precluding comparison on these variables with studies that collected these data.
Conclusion
Motivated by the increasing proportion of neonatal deaths among under-five deaths, ANISA represents the largest community-based study of its kind, bridging the knowledge gap in aetiology of neonatal sepsis using intensive and early surveillance, state-of-the-art laboratory methods, appropriate controls and sophisticated modelling. This analysis provides important insights into the risk factors for neonatal sepsis in South Asia: a region where the preponderance of the world’s neonatal infections and deaths occur.58 59 Since all analyses were adjusted by site, this helps to control confounding in any given setting in the study population.
Risk factor data collected by ANISA could potentially be used to develop point-of-care algorithms to better target infants with high likelihood of bacterial infections in order to target simplified generalised antibiotic regimens employing conventional community-based strategies and/or data-driven risk scoring algorithms.28 29 60 If validated, such algorithms could be used to help ensure appropriate treatment of neonates at high risk for bacterial infection and limit unnecessary antibiotic use among neonates in whom bacterial infection is unlikely.
Acknowledgments
We would like to thank the technical advisory group members of the Aetiology of Neonatal Infection in South Asia (ANISA) project, the site principal investigators and the blood culture review committee members. We are indebted to the study participants and their caregivers and the study team members for their contributions. We would also like to thank Mahmudur Rahman for helping with data management and Mahfuza Marzan for helping with project coordination.
Footnotes
Handling editor: Seema Biswas
Twitter: @imran_nisar, @gdarmsta
Contributors: NEC coordinated and supervised study operations and development of data collection instruments, developed coding of risk factor variables for analysis and carried out the analysis, drafted the initial manuscript and reviewed and revised the manuscript. He was formerly affiliated with the Child Health Research Foundation (CHRF) during the study but affiliated with the London School of Hygiene and Tropical Medicine (LSHTM) during the analysis and writing phase and will act as the guarantor for this paper. MSI coordinated and supervised study operations and development of data collection instruments and reviewed and revised the manuscript. LCM and NS conceptualised the Bayesian partial latent class model data analysis approach and performed underlying analysis/modelling of pathogen attributions. ABa, ZAB, ABo, RI, DKM, IN, PP, KP, RS, SS and AKMZ designed the study implementation and supervised data collection at their respective study sites. QSR and TH provided data collection infrastructure and processing of raw and initial analytical datasets. JMW, MLA, MHD and JLW provided high-level oversight of quantitative PCR operations, output and interpretation. MWW, PH and DHH provided in-depth interpretation of blood culture and clinical course to refine attribution. ASMNUA, MI and MBH provided valuable support to paediatric care and logistics of data collection and laboratory operations. GLD critically reviewed the manuscript for important intellectual content. SEA, SJS, SAQ and SKS (the principal investigator) conceptualised, designed and executed the ANISA study, coordinated and supervised data collection and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding: All phases of this study were supported by a grant (OPPGH5307) from the Bill & Melinda Gates Foundation to the Child Health Research Foundation, Dhaka, Bangladesh.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention or WHO.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. The data collected as part of the ANISA study were shared with all participating collaborators but will not be made available to others.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the ethics committees or internal review boards of all participating organisations. This is a secondary analysis of the original data collected in the ANISA study published here: https://doi.org/10.1016/S0140-6736(18)31127-9.
References
- 1.GBD 2016 Causes of Death Collaborators . Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the global burden of disease study 2016. Lancet 2017;390:1151–210. 10.1016/S0140-6736(17)32152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saha SK, Schrag SJ, El Arifeen S, et al. Causes and incidence of community-acquired serious infections among young children in South Asia (ANISA): an observational cohort study. Lancet 2018;392:145–59. 10.1016/S0140-6736(18)31127-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharrow D, Hug L, Liu Y. Levels & trends in child mortality report 2020. Estimates developed by the UN inter-agency group for child mortality estimation. United Nations Inter-Agency Group for Child Mortality Estimation (UNIGME), 2020. [Google Scholar]
- 4.Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, et al. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med 2018;6:223–30. 10.1016/S2213-2600(18)30063-8 [DOI] [PubMed] [Google Scholar]
- 5.Kissoon N, Uyeki TM. Sepsis and the global burden of disease in children. JAMA Pediatr 2016;170:107–8. 10.1001/jamapediatrics.2015.3241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaurasia S, Sivanandan S, Agarwal R, et al. Neonatal sepsis in South Asia: huge burden and spiralling antimicrobial resistance. BMJ 2019;364:k5314. 10.1136/bmj.k5314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ahmed, I, Alliance for Maternal and Newborn Health Improvement (AMANHI) mortality study group . Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in South Asia and sub-Saharan Africa: a multi-country prospective cohort study. Lancet Glob Health 2018;6:e1297–308. 10.1016/S2214-109X(18)30385-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reinhart K, Daniels R, Kissoon N, et al. Recognizing sepsis as a global health priority—a WHO resolution. N Engl J Med 2017;377:414–7. 10.1056/NEJMp1707170 [DOI] [PubMed] [Google Scholar]
- 9.Global Maternal and Neonatal Sepsis Initiative Working Group. Electronic address: bonetm@who.int . The global maternal and neonatal sepsis initiative: a call for collaboration and action by 2030. Lancet Glob Health 2017;5:e390–1. 10.1016/S2214-109X(17)30020-7 [DOI] [PubMed] [Google Scholar]
- 10.Schrag SJ, Cutland CL, Zell ER, et al. Risk factors for neonatal sepsis and perinatal death among infants enrolled in the prevention of perinatal sepsis trial, Soweto, South Africa. Pediatr Infect Dis J 2012;31:821–6. 10.1097/INF.0b013e31825c4b5a [DOI] [PubMed] [Google Scholar]
- 11.Berkley JA, Lowe BS, Mwangi I, et al. Bacteremia among children admitted to a rural hospital in Kenya. N Engl J Med 2005;352:39–47. 10.1056/NEJMoa040275 [DOI] [PubMed] [Google Scholar]
- 12.Sigaúque B, Roca A, Mandomando I, et al. Community-acquired bacteremia among children admitted to a rural hospital in Mozambique. Pediatr Infect Dis J 2009;28:108–13. 10.1097/INF.0b013e318187a87d [DOI] [PubMed] [Google Scholar]
- 13.Nielsen MV, Sarpong N, Krumkamp R, et al. Incidence and characteristics of bacteremia among children in rural Ghana. PLoS One 2012;7:e44063. 10.1371/journal.pone.0044063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahwere P, Levy J, Hennart P, et al. Community-acquired bacteremia among hospitalized children in rural central Africa. Int J Infect Dis 2001;5:180–8. 10.1016/s1201-9712(01)90067-0 [DOI] [PubMed] [Google Scholar]
- 15.Enwere G, Biney E, Cheung YB, et al. Epidemiologic and clinical characteristics of community-acquired invasive bacterial infections in children aged 2-29 months in the Gambia. Pediatr Infect Dis J 2006;25:700–5. 10.1097/01.inf.0000226839.30925.a5 [DOI] [PubMed] [Google Scholar]
- 16.Darmstadt GL, Lawn JE, Costello A. Advancing the state of the world’s newborns. Bull World Health Organ 2003;81:224–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Darmstadt GL, Saha SK, Choi Y, et al. Population-based incidence and etiology of community-acquired neonatal bacteremia in Mirzapur, Bangladesh: an observational study. J Infect Dis 2009;200:906–15. 10.1086/605473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zakariya BP, Bhat B V, Harish BN, et al. Risk factors and predictors of mortality in culture proven neonatal sepsis. Indian J Pediatr 2012;79:358–61. 10.1007/s12098-011-0584-9 [DOI] [PubMed] [Google Scholar]
- 19.Murthy S, Godinho MA, Guddattu V, et al. Risk factors of neonatal sepsis in India: a systematic review and meta-analysis. PLoS One 2019;14:e0215683. 10.1371/journal.pone.0215683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adhikari N, Shah PK, Acharya G, et al. Bacteriological profile and associated risk factors of neonatal sepsis in Paropakar maternity and women's Hospital Thapathali, Kathmandu. Nepal Med Coll J 2014;16:161–4. [PubMed] [Google Scholar]
- 21.Waters D, Jawad I, Ahmad A, et al. Aetiology of community-acquired neonatal sepsis in low and middle income countries. J Glob Health 2011;1:154–70. [PMC free article] [PubMed] [Google Scholar]
- 22.Polin RA, Committee on Fetus and Newborn . Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics 2012;129:1006–15. 10.1542/peds.2012-0541 [DOI] [PubMed] [Google Scholar]
- 23.Bhutta ZA, Zaidi AKM, Thaver D, et al. Management of newborn infections in primary care settings: a review of the evidence and implications for policy? Pediatr Infect Dis J 2009;28:S22–30. 10.1097/INF.0b013e31819588ac [DOI] [PubMed] [Google Scholar]
- 24.Obiero CW, Seale AC, Berkley JA. Empiric treatment of neonatal sepsis in developing countries. Pediatr Infect Dis J 2015;34:659–61. 10.1097/INF.0000000000000692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization . Pocket book of hospital care for children: guidelines for the management of common childhood illnesses. World Health Organization, 2013. [PubMed] [Google Scholar]
- 26.Töllner U. Early diagnosis of septicemia in the newborn. Eur J Pediatr 1982;138:331–7. 10.1007/BF00442511 [DOI] [PubMed] [Google Scholar]
- 27.Strunk T, Buchiboyina A, Sharp M, et al. Implementation of the neonatal sepsis calculator in an Australian tertiary perinatal centre. Neonatology 2018;113:379–82. 10.1159/000487298 [DOI] [PubMed] [Google Scholar]
- 28.Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet 2017;390:1770–80. 10.1016/S0140-6736(17)31002-4 [DOI] [PubMed] [Google Scholar]
- 29.Kuzniewicz MW, Puopolo KM, Fischer A, et al. A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr 2017;171:365–71. 10.1001/jamapediatrics.2016.4678 [DOI] [PubMed] [Google Scholar]
- 30.Puopolo KM, Draper D, Wi S, et al. Estimating the probability of neonatal early-onset infection on the basis of maternal risk factors. Pediatrics 2011;128:e1155–63. 10.1542/peds.2010-3464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization . Guideline: managing possible serious bacterial infection in young infants when referral is not feasible 2015. [PubMed]
- 32.Islam MS, Baqui AH, Zaidi AK, et al. Infection surveillance protocol for a multicountry population-based study in South Asia to determine the incidence, etiology and risk factors for infections among young infants of 0 to 59 days old. Pediatr Infect Dis J 2016;35:S9–15. 10.1097/INF.0000000000001100 [DOI] [PubMed] [Google Scholar]
- 33.Saha SK, Islam MS, Qureshi SM, et al. Laboratory methods for determining etiology of neonatal infection at population-based sites in South Asia: the anisa study. Pediatr Infect Dis J 2016;35:S16–22. 10.1097/INF.0000000000001101 [DOI] [PubMed] [Google Scholar]
- 34.Saha SK, El Arifeen S, Schrag SJ. Aetiology of Neonatal Infection in South Asia (ANISA): an initiative to identify appropriate program priorities to save newborns. Pediatr Infect Dis J 2016;35:S6–8. 10.1097/INF.0000000000001099 [DOI] [PubMed] [Google Scholar]
- 35.Islam MS, Rahman QS-ur, Hossain T, et al. Using text messages for critical real-time data capture in the anisa study. Pediatr Infect Dis J 2016;35:S35–8. 10.1097/INF.0000000000001104 [DOI] [PubMed] [Google Scholar]
- 36.Connor NE, Hossain T, Rahman QS-ur, et al. Development and implementation of the anisa labeling and tracking system for biological specimens. Pediatr Infect Dis J 2016;35:S29–34. 10.1097/INF.0000000000001103 [DOI] [PubMed] [Google Scholar]
- 37.Hossain B, Weber MW, Hamer DH, et al. Classification of blood culture isolates into contaminants and pathogens on the basis of clinical and laboratory data. Pediatr Infect Dis J 2016;35:S52–4. 10.1097/INF.0000000000001107 [DOI] [PubMed] [Google Scholar]
- 38.Wu Z, Deloria-Knoll M, Hammitt LL, et al. Partially latent class models for case-control studies of childhood pneumonia aetiology. J R Stat Soc Ser C Appl Stat 2016;65:97–114. 10.1111/rssc.12101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deloria Knoll M, Fu W, Shi Q, et al. Bayesian estimation of pneumonia etiology: epidemiologic considerations and applications to the pneumonia etiology research for child health study. Clin Infect Dis 2017;64:S213–27. 10.1093/cid/cix144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhou X, Reiter JP. A note on Bayesian inference after multiple imputation. Am Stat 2010;64:159–63. 10.1198/tast.2010.09109 [DOI] [Google Scholar]
- 41.Sphere Association . The Sphere handbook: humanitarian charter and minimum standards in humanitarian response. 2018 edn. Geneva: Sphere Association, 2018. [Google Scholar]
- 42.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 2001;38:115–32. 10.1353/dem.2001.0003 [DOI] [PubMed] [Google Scholar]
- 43.Huda TM, Hayes A, El Arifeen S, et al. Social determinants of inequalities in child undernutrition in Bangladesh: a decomposition analysis. Matern Child Nutr 2018;14:12440 10.1111/mcn.12440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Edmond K, Zaidi A. New approaches to preventing, diagnosing, and treating neonatal sepsis. PLoS Med 2010;7:e1000213. 10.1371/journal.pmed.1000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bahl R, Martines J, Ali N, et al. Research priorities to reduce global mortality from newborn infections by 2015. Pediatr Infect Dis J 2009;28:S43–8. 10.1097/INF.0b013e31819588d7 [DOI] [PubMed] [Google Scholar]
- 46.Lawn JE, Blencowe H, Oza S, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet 2014;384:189–205. 10.1016/S0140-6736(14)60496-7 [DOI] [PubMed] [Google Scholar]
- 47.Seale AC, Blencowe H, Zaidi A, et al. Neonatal severe bacterial infection impairment estimates in South Asia, sub-Saharan Africa, and Latin America for 2010. Pediatr Res 2013;74:73–85. 10.1038/pr.2013.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Khera R, Jain S, Lodha R, et al. Gender bias in child care and child health: global patterns. Arch Dis Child 2014;99:369–74. 10.1136/archdischild-2013-303889 [DOI] [PubMed] [Google Scholar]
- 49.Zea-Vera A, Ochoa TJ. Challenges in the diagnosis and management of neonatal sepsis. J Trop Pediatr 2015;61:1–13. 10.1093/tropej/fmu079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sabtu N, Enoch DA, Brown NM. Antibiotic resistance: what, why, where, when and how? Br Med Bull 2015;116:105–13. 10.1093/bmb/ldv041 [DOI] [PubMed] [Google Scholar]
- 51.Baqui AH, El-Arifeen S, Darmstadt GL, et al. Effect of community-based newborn-care intervention package implemented through two service-delivery strategies in Sylhet district, Bangladesh: a cluster-randomised controlled trial. Lancet 2008;371:1936–44. 10.1016/S0140-6736(08)60835-1 [DOI] [PubMed] [Google Scholar]
- 52.Zaidi AKM, Tikmani SS, Warraich HJ, et al. Community-based treatment of serious bacterial infections in newborns and young infants: a randomized controlled trial assessing three antibiotic regimens. Pediatr Infect Dis J 2012;31:667–72. 10.1097/INF.0b013e318256f86c [DOI] [PubMed] [Google Scholar]
- 53.African Neonatal Sepsis Trial (AFRINEST) group, Tshefu A, Lokangaka A, et al. Simplified antibiotic regimens compared with injectable procaine benzylpenicillin plus gentamicin for treatment of neonates and young infants with clinical signs of possible serious bacterial infection when referral is not possible: a randomised, open-label, equivalence trial. Lancet 2015;385:1767–76. 10.1016/S0140-6736(14)62284-4 [DOI] [PubMed] [Google Scholar]
- 54.Mir F, Nisar I, Tikmani SS, et al. Simplified antibiotic regimens for treatment of clinical severe infection in the outpatient setting when referral is not possible for young infants in Pakistan (Simplified Antibiotic Therapy Trial [SATT]): a randomised, open-label, equivalence trial. Lancet Glob Health 2017;5:e177–85. 10.1016/S2214-109X(16)30335-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baqui AH, Saha SK, Ahmed ASMNU, et al. Safety and efficacy of alternative antibiotic regimens compared with 7 day injectable procaine benzylpenicillin and gentamicin for outpatient treatment of neonates and young infants with clinical signs of severe infection when referral is not possible: a randomised, open-label, equivalence trial. Lancet Glob Health 2015;3:e279–87. 10.1016/S2214-109X(14)70347-X [DOI] [PubMed] [Google Scholar]
- 56.Bedford Russell AR, Kumar R. Early onset neonatal sepsis: diagnostic dilemmas and practical management. Arch Dis Child Fetal Neonatal Ed 2015;100:F350–4. 10.1136/archdischild-2014-306193 [DOI] [PubMed] [Google Scholar]
- 57.Farag TH, Koplan JP, Breiman RF, et al. Precisely tracking childhood death. Am J Trop Med Hyg 2017;97:3–5. 10.4269/ajtmh.16-0302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lawn JE, Blencowe H, Pattinson R, et al. Stillbirths: where? when? why? How to make the data count? Lancet 2011;377:1448–63. 10.1016/S0140-6736(10)62187-3 [DOI] [PubMed] [Google Scholar]
- 59.Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016;388:3027–35. 10.1016/S0140-6736(16)31593-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yan RY. How Chinese clinicians contribute to the improvement of maternity care. Int J Gynaecol Obstet 1989;30:23–6. 10.1016/0020-7292(89)90209-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2022-009706supp001.pdf (170.2KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. The data collected as part of the ANISA study were shared with all participating collaborators but will not be made available to others.