A 46-year-old man presented to our hospital with abdominal pain and fever. In his medical history he reported three previous episodes of varicella zoster. On examination, he had a temperature of 38·3°C, small cervical lymph nodes, and some right upper quadrant tenderness.
A CT of the patient’s abdomen showed bilateral adrenalitis (figure). Laboratory investigations showed marked cholestatic hepatitis—including a raised alkaline phosphatase (1995 U/mL; normal 30–135).
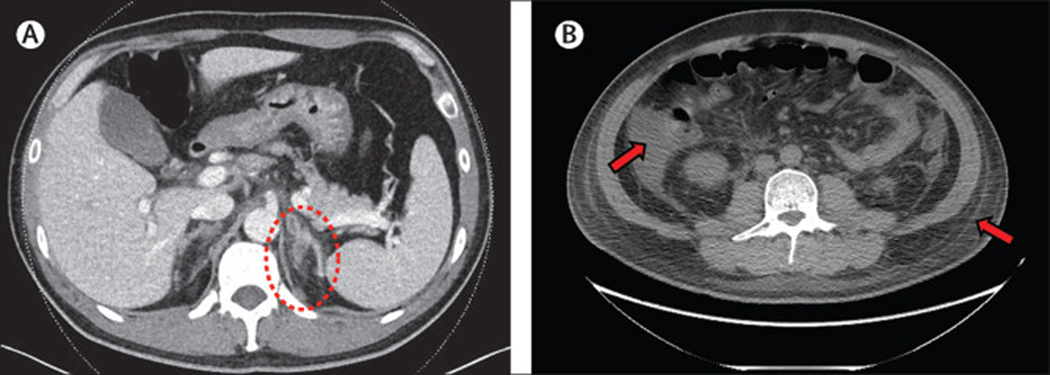
Figure: Features of a rare variant of idiopathic multicentric Castleman’s disease.
CT scan shows prominent adrenalitis with adjacent fat stranding (A; encircled). CT scan 12 days after presentation shows ascites (left arrow) and subcutaneous oedema (B; right arrow)
12 days later he developed thrombocytopenia (29×109 per L; normal 150–400), markedly elevated acute phase reactants—C-reactive protein concentration 266 mg/L (<3·1), D-dimer 12696 μg/L (<500), ferritin 8626 μg/L (<300), and soluble interleukin-2 receptor 2 481 U/mL (<846). We found him to have anasarca with pleural effusions, ascites, and subcutaneous oedema (figure).
Serum creatinine was 44 μmol/L, and urine microalbumin: creatinine ratio 387 (normal <2·0). Serum protein electrophoresis showed albumin 14 g/L, normal gamma globulins, and no monoclonal proteins. Interleukin-6 concentration was 39·6 pg/mL (<1·8) and vascular endothelial growth factor 212 pg/mL (31–86). SARS-CoV-2 nasal swabs, HIV, Epstein-Barr virus, cytomegalovirus, and human herpesvirus 8 (HHV-8) serology were negative.
18F-fluorodeoxyglucose PET/CT showed diffuse enlarged lymphadenopathy up to 3 cm, mild hepatosplenomegaly, and ascites, pleural effusions, and subcutaneous oedema. Oesophagogastroduodenoscopy and colonoscopy were normal; biopsy specimens taken from along the gastro- intestinal tract were normal. Bone marrow biopsy showed moderate haemophagocytosis with no fibrosis.
Excisional biopsy of the largest cervical lymph node showed many regressed germinal centres, prominent vascularity, very prominent follicular dendritic cells, and marked plasmacytosis (appendix); immunohistochemical stain for HHV-8 was negative.
Considering the patient in the round—thrombocyto- penia, anasarca, reticulin fibrosis of the bone marrow, renal dysfunction, and organomegaly, acronymed to TAFRO—we diagnosed a variant of idiopathic multi- centric Castleman’s disease.
The patient was treated with numerous agents and ultimately responded to a combination of bortezomib, dexamethasone, baricitinib, siltuximab, and ciclosporin.
TAFRO is an aggressive variant of idiopathic multicentric Castleman’s disease. The diagnosis is elusive; patients are often initially thought to have viral illness or haemophagocytic lymphohistiocytosis. The lymphadenopathy and organomegaly are typically mild, and gamma globulins often normal. Patients decline rapidly and may be refractory to initial therapy, so early diagnosis is essential. Adrenalitis can be an important early clue, but because an adrenal biopsy is often unhelpful, clinical recognition is essential (video).
video.
Supplementary Material
Multiple choice question.
Adrenalitis followed by anasarca, inflammation, and thrombocytopenia
- A 46-year-old man presented with abdominal pain and was found to have adrenalitis on CT. He then developed pleural effusions, ascites, and subcutaneous oedema, severe thrombocytopenia, fever with raised C-reactive protein, ferritin, and mild diffuse lymphadenopathy, with mild hepatosplenomegaly. Excisional biopsy of a cervical lymph node showed many regressed germinal centers, prominent vascularity, prominent follicular dendritic cells, and marked polyclonal plasmacytosis. Which is the correct diagnosis?
- Infectious mononucleosis
- Intravascular B cell lymphoma
- Idiopathic multicentric Castleman disease
- COVID-19 cytokine storm syndrome
Answer C)
Using CT images.
Footnotes
All authors were involved in editing and approving the final manuscript. Written permission was obtained from the patient.
Declaration of interests
We declare no competing interests.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.