Abstract
Introduction
Osteomyelitis of the pubic symphysis is a rare condition often occurring in patients with radiation therapy-related urethral strictures after prostate cancer treatment.
Material and methods
We retrospectively reviewed patients who presented with osteomyelitis of the pubic symphysis from November 2016 to September 2021. We investigated the factors leading to urosymphyseal fistulas, clinical presentation, radiological assessment, treatments, and outcomes.
Results
A total 4 cases were collected. All patients underwent surgery and adjuvant or salvage radiotherapy for prostate cancer. Subsequently, they developed stricture of the vesicourethral anastomosis which was initially treated conservatively. Symptoms of pubic bone osteomyelitis included pain in the pubic area, fever, difficulty walking, and recurrent urinary tract infections. In all cases, computed tomography and magnetic resonance imaging showed a urinary fistula arising from the vesicourethral anastomosis with the involvement of the pubic bone, and severe osteomyelitis. Due to the failure of conservative treatment, debridement of the pubic bone with cystectomy and ileal conduit was performed in 3 patients. One patient refused surgery and bilateral percutaneous nephrostomies were placed. Patients regained their original performance status 1 to 6 months after surgery.
Conclusions
General recommendations for the best diagnostic and therapeutic approach to osteomyelitis of the pubic symphysis due to urosymphyseal fistula still do not exist. Conservative treatment often fails and a surgical approach with definitive urinary diversion may be required.
Keywords: urinary fistula, urinary diversion, osteomyelitis, urethral stricture, prostatectomy
INTRODUCTION
Osteomyelitis of the pubic symphysis is a rare and poorly recognized infection of the pubic symphysis and the pubic rami with potentially devastating consequences.
Clinical presentation may be insidious consisting of pelvic and suprapubic pain, recurrent urinary tract infections, and difficulty walking [1].
Pubic bone osteomyelitis (PBO) is frequently reported as a rare complication of endoscopic treatments for urethral strictures or bladder neck contractures after multimodal therapy for prostate cancer (PCa) [2].
Furthermore, in the literature, pubic osteomyelitis has been associated with transurethral resection or photo vaporization of the prostate, chronic indwelling catheters, and bone-anchored slings for stress urinary incontinence [3–6].
Conservative treatment of urosymphyseal fistulas consists of long-term parenteral or oral administration of antibiotics, but this strategy is often ineffective [2].
In these cases, surgery may be the final solution, although there is not yet a general recommendation for the best course of action.
We present a series of patients diagnosed with PBO who had received multimodality prostate cancer treatment complicated by radiation-induced urethral strictures and urinary fistula.
We discuss the clinical presentation, diagnosis, surgical treatment alternatives, and outcomes.
MATERIAL AND METHODS
We retrospectively reviewed prostate cancer patients diagnosed with PBO at two different Institutions from November 2016 to September 2021. Data were retrieved from outpatient clinic records, inpatient charts, surgery, and histopathological reports. We collected details regarding demographic data, prostate cancer disease, and related treatments. In addition, information on oncologic and clinical follow-up was collected, with a focus on surgical or endoscopic procedures.
We documented the clinical presentation of PBO, radiological assessment, and clinical pathway for the management of this condition. Outcomes, and complications according to the Clavien Dindo classification, were evaluated [7].
Clinical evaluations and magnetic resonance imaging (MRI) of the pelvis were performed to assess the recovery status and resolution of the PBO. We relied on postoperative radiographs to evaluate the surgical debridement.
Postoperative pain assessment was carried out using the 11 item verbal numeric rating scale (NRS-11) in the inpatient wards, and at each outpatient consultation [8].
All patients provided written informed consent for research analysis and anonymous reporting of results in aggregate form.
RESULTS
Patients’ characteristics
Overall, 4 cases of PBO were collected (cases 1–4). The median age was 70 [interquartile range (IQR) 11] years at the time of the diagnosis. All patients had a history of prostate cancer.
Cases 1 and 2 were submitted to laparoscopic radical prostatectomy and pelvic lymphadenectomy as primary treatment. The histopathological reports of both case 1 and case 2 revealed locally advanced disease with a high Gleason score (case 1: pT3a pN0 R0, Gleason Score 4+5; case 2: pT3a pN0 R0, Gleason Score 4+4) [9]. Both patients received intensity-modulated radiation therapy (IMRT) at 76–78 Gy as part of local regional salvage therapy.
Case 3 presented with locally advanced prostate cancer (cT4 cN0 cM0), and the prostate biopsy showed poorly differentiated acinar adenocarcinoma with Gleason score of 4 + 4 [9].
The patient underwent IMRT in combination with androgen deprivation therapy without prophylactic pelvic lymph node irradiation as primary treatment for prostate cancer. He was subsequently submitted to radical salvage laparoscopic prostatectomy plus bilateral ureteral reimplantation because of trigonal infiltration and concomitant bilateral hydronephrosis with biochemical progression.
With regards to case 4, the histopathological report of both the whole specimen and the prostate biopsy was not available, and the patient underwent adjuvant radiotherapy because the pelvic nodes were positive and there was no organ-confined disease. No further details are available regarding the dose and the regimen.
Despite the different conditions, all patients underwent radiotherapy for prostate cancer. All patients developed symptomatic stricture of the vesicourethral anastomosis, which was initially treated conservatively with serial dilatations and endoscopic incisions. The median time between salvage therapy and stricture of the vesicourethral anastomosis was 30 [interquartile range (IQR) 36] months. One patient (case 4) began intermittent self-catheterizations 20 years after primary surgery for prostate cancer.
Clinical presentation of pubic bone osteomyelitis and diagnosis
Symptoms of PBO included pelvic and pubic pain, intermittent fever, difficulty walking, and recurrent urinary tract infections with positive urine culture in all patients. Physical examination revealed tenderness of the pubic bone in all cases. The time interval between the onset of symptoms and diagnosis was 2 months in both case 1 and case 2. Case 3 was referred to urology consultation 3 months after the first complaints.
Case 4 had the most devastating clinical presentation. He suffered from recurrent urinary tracts infections, suprapubic pain, and difficulty walking for 7 months. Finally, he was admitted to our emergency department because of bilateral groin abscess with cutaneous fissuring and septic status.
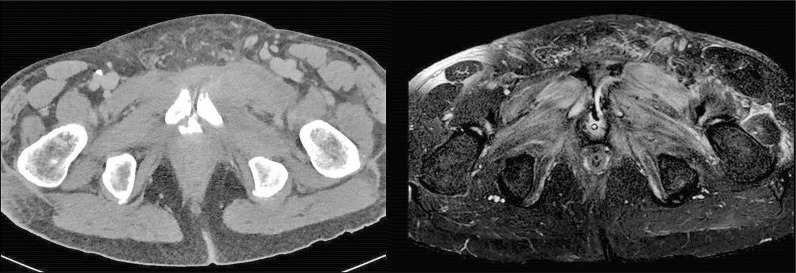
In all cases, abdominal-pelvic computed tomography (CT) scan and magnetic resonance imaging (MRI) showed a urinary fistula from the vesicourethral anastomosis involving the pubic bone, with severe osteomyelitis (Figures 1, 2).
Figure 1.
Urosymphyseal fistula as seen on computed tomography scan (left side) and pelvic magnetic resonance imaging (right side).
Figure 2.
Urosymphyseal fistula as seen on computed tomography scan.
Bone scan revealed a fracture of the left pubic bone in one case (case 3). All cases were evaluated by a multidisciplinary team involving urologists, radiologists, infectious disease specialists, and orthopedic surgeons.
Pubic bone osteomyelitis management
In all cases, an attempt at conservative treatment was made.
The initial approach consisted of placement of a transurethral bladder catheter and administration of targeted antibiotic therapy. Hyperbaric oxygen therapy was not recommended in any case.
In case 4, drainage of the inguinal abscess was performed by placing percutaneous drainage tubes bilaterally.
All patients were found to have persistent pain (NRS-11 = 5–8) and elevated inflammatory markers, requiring surgical treatment.
Case 1, 2, and 4 underwent combined cystectomy with ileal conduit and pubic bone debridement with removal of the necrotic portions of the affected pubic rami. The histopathological examination revealed transmural chronic cystitis, areas of chronic pelvic osteomyelitis, and foci of osteonecrosis.
Case 1, 2, and 4 were discharged on postoperative day 7, 8 and 22, respectively. No intra and post- operative major complications (Clavien Dindo III–V) [7] were recorded.
Case 4 had the longest hospital stay. On postoperative day 5, he presented with fever and a 6 cm pelvic abscess was detected on CT scan. A percutaneous drain was placed, and antibiotic treatment was administered according to the culture results. The drain was withdrawn after 7 days when clinical, laboratory and radiological improvements were observed on the CT scan and the daily drainage volume was less than 10 mL/24 h. The inguinal tubes were removed 6 days before hospital discharge.
Case 3 refused surgical treatment and indwelling bilateral percutaneous nephrostomies were placed. Tubes were changed every 40 days. The patient received intravenous antibiotic treatment for 2 weeks followed by oral antibiotics for 3 months based on positive blood cultures.
The time from PBO diagnosis to definitive treatment ranges from 5 to 7 weeks (Table 1).
Table 1.
Clinical and demographic data, treatments received, outcomes
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age (y) at the diagnosis of PBO | 66 | 68 | 72 | 80 |
| Comorbidities | Hypertension | No comorbidities | Hypertension, impaired fasting glucose | Hypertension, obesity, diabetes mellitus, dyslipidemia |
| PBO presentation | Fever, fatigue, sepsis, walking difficulties, pain, UTI | Fever, fatigue, sepsis, walking difficulties, pain, UTI | Fever, fatigue, sepsis, walking difficulties, pain, UTI | Fever, fatigue, sepsis, walking difficulties, pain, inguinal abscess, recurrent UTI |
| Previous PCa diagnosis | Yes | Yes | Yes | Yes |
| PCa staging | pT3a pN0 R0, Gleason Score 4+ | pT3a pN0 R0, Gleason Score 4+4 | cT4 cN0, Gleason Score 4+4 | N/A (Positive pelvic nodes and no organ-confined disease) |
| PCa primary treatment | LRP + LAD | LRP + LAD | ADT + EBRT | RRP + LAD + adjuvant EBRT |
| Recurrence | Biochemical | Biochemical | Local (trigonal infiltration and bilateral hydronephrosis) | No |
| Treatment of recurrence | Salvage radiotherapy (3 y after RP) | Salvage radiotherapy (4 y after RP) | Salvage radical prostatectomy + bilateral ureteral reimplantation (pT4 pN0 R0) | – |
| Time to vesicourethral anastomosis stenosis after salvage treatment (months) | 24 | 36 | 4 | 48 |
| Treatment of vesicourethral anastomosis stenosis | Endoscopic laser incision | Endoscopic laser incision, periodic dilatation | Endoscopic laser incision | Endoscopic incision, dilatation, intermittent self-catheterization |
| Time from PBO symptoms onset to diagnosis (months) | 2 | 2 | 3 | 7 |
| Time from the treatment of vesicourethral anastomosis stenosis to PBO (months) | 6 | 4 | 1 | Daily self-catheterization |
| Time radiotherapy to PBO (months) | 30 | 40 | 10 | 264 |
| Time from PBO diagnosis to definitive treatment (months) | 5 | 6 | 5 | 7 |
| Surgical treatment of PBO | Pubic debridement, cystectomy, and ileal conduit | Pubic debridement, cystectomy, and ileal conduit | Indwelling bilateral nephrostomies (periodical changes) | Pubic debridement, cystectomy, and ileal conduit |
| Duration of antibiotic therapy after surgery/procedure (weeks) | 2 | 2 | 12 | 4 |
| Time to resolution (months) | 1 | 1 | 6 | 1 |
| Postoperative day discharge (days) | 7 | 8 | No surgery performed | 22 |
PBO – pubic bone osteomyelitis; PCa – prostate cancer; UTI – urinary tract infection; LRP + LAD – laparoscopic radical prostatectomy + lymphadenectomy; ADT + EBRT – androgen deprivation therapy + external beam radiation therapy; RRP – retropubic radical prostatectomy; RP – radical prostatectomy; N/A – not applicable; y – years
Follow-up
The patients recovered the baseline performance status without local symptoms from 1 to 6 months after the PBO treatment (surgical debridement or placement of bilateral nephrostomies). Case 3 had the longest recovery period (Table 1).
At a median follow-up of 11,5 (IQR 12.75–10.25) months, the NRS-11 score was 0, in all cases.
In cases 1, 2, and 4, postoperative pelvic radiographs showed the results of surgery (Figure 3). In addition, all patients had radiographic resolution of osteomyelitis on MRI of the pelvis.
Figure 3.
Pelvic radiograph after pubic debridement.
All patients recovered completely from their morbidity and they were able to ambulate without assistance.
DISCUSSION
Osteomyelitis of the pubic symphysis is a rare entity accounting for less than 1% of all cases of osteomyelitis [10].
PBO is often an unexpected complication after PCa treatment. The vast majority of studies have identified a strong association between PBO and urosymphyseal fistula following endoscopic treatment for stenosis of the vesicourethral anastomosis after PCa management.
Matsushita et al. [11] retrospectively collected a sample of 12 patients who presented with a pubo-vesical fistula after PCa treatment over the course of 11 years at two different high-volume institutions. All patients had undergone radiation therapy (salvage or primary) and all cases developed bladder neck contracture requiring endoscopic procedures. A total of 10 out of 12 patients underwent cystectomy with urinary diversion due to failure of conservative treatment. The authors emphasized that radiotherapy-induced bladder neck contracture requiring endoscopic procedures is an important factor for the development of pubo-vesical fistula and that the likelihood of additional surgical treatment is increased. Radiotherapy is a common underlying risk factor for these disease processes. It is well documented that radiotherapy causes progressive obliterative endarteritis resulting in fibrotic tissue reaction. The microvascular damage leads to poor tissue perfusion and wound healing with a low chance of a successful outcome with a conservative approach in the case of fistula [12, 13].
Bugeja et al. reported a series of 16 patients treated for urosymphyseal fistulas following PCa treatment between January 2011 and April 2014 [2].
In 13 out of 16 cases, urinary leakage occurred after open or endoscopic surgical procedures to treat bladder neck contracture suggesting a potential association with fistulation into the pubic symphysis [2]. According to this data, it seems extremely important to carefully perform minor procedures such as urethrotomy, dilation, and bladder neck resection in this group of patients [2].
Pubo-vesical fistulas and radiotherapy are rarely not associated with PBO after PCa treatment.
Degheili et al. described the first case of PBO following robot-assisted radical prostatectomy in a patient without any radiation therapy exposure and any fistulous tract originating from the genito-urinary system [14].
In this case, the most reasonable etiology for PBO was unpredictable damage to the pubic bone mantle during suturing of the dorsal venous complex or suturing of the anterior portion of the urethrovesical anastomosis.
In our short series, all patients had undergone salvage or primary radiotherapy for PCa and endoscopic procedures for stenosis of the urethrovesical anastomosis. Our results are consistent the previous evidence, and it seems acceptable to consider both radiotherapy and endoscopic interventions for stenosis of the urethrovesical anastomosis as risk factors for pubo-vesical fistula and PBO.
Regarding the treatment of PBO, there is still considerable uncertainty given the small number of reported cases.
Conservative treatment with antibiotics and temporary urinary drainage is generally the initial treatment strategy [13].
In our cohort, surgical debridement of the pubic bone was recommended after the failure of the conservative approach.
This finding confirms previous literature supporting surgery as a potentially successful option [1, 2, 5, 11, 15, 16].
Despite the devastating consequences that may be associated with PBO, our patients recovered the baseline performance status with pain relief 1 to 6 months after surgery.
To overcome the limitations in knowledge about the management of PBO, Gupta S. et al. developed a multidisciplinary algorithm to support the decision-making process [1].
According to their research, the crucial point in the treatment of PBO is diagnosis. This complex syndrome is thought to be poorly recognized, and patients are often treated for intermittent urinary tract infections or chronic pelvic pain after PCa treatment, with an underlying osteomyelitis being misdiagnosed [1].
A fundamental diagnostic method is MRI of the pelvis [17, 18].
Pelvic MRI was shown to be far superior to plain radiography or CT in detecting PBO, which is characterized by strong signal on T2-weighted images and low signal on T1-weighted images of the involved pubic rami [18].
MRI should be recommended when PBO is suspected because it facilitates the identification of even the non-bony findings such as fistulas or fluid extravasations [1, 18].
The results of our study should be considered with caution, as some limitations can be highlighted.
First, we collected a very small sample, and we performed a retrospective analysis of medical records.
Moreover, the pathologic characteristics of the patients are heterogeneous, and they differ in terms of the timing and type of treatment received, including the regimen and the setting of radiotherapy.
Although the rarity of this condition inevitably affects the strength of evidence, we believe that our series can provide additional knowledge and raise awareness about this uncommon entity.
CONCLUSIONS
PBO following urinary fistula in patients with radiation therapy-associated urethral strictures after prostate cancer treatment is a rare and challenging condition. General recommendations for the best diagnostic and therapeutic approach still do not exist. In most cases, conservative treatments fails and a surgical approach with definitive urinary diversion may be required.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Gupta S, Zura RD, Hendershot EF, Peterson. Pubic symphysis osteomyelitis in the prostate cancer survivor: clinical presentation, evaluation, and management. Urology. 2015; 85: 684-690. [DOI] [PubMed] [Google Scholar]
- 2.Bugeja S, Andrich DE, Mundy AR. Fistulation into the Pubic Symphysis after Treatment of Prostate Cancer: An Important and Surgically Correctable Complication. J Urol. 2016; 195: 391-398. [DOI] [PubMed] [Google Scholar]
- 3.Garg G, Deliso M, Li S, Sharma P, Abdelbaki A, Gupta N. Prostatosymphyseal fistula after transurethral resection of the prostate (TURP), a rare and difficult to recognize complication. Urol Case Rep. 2018; 21: 70-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graham CW, Dmochowski RR, Faerber GJ, Clemens JQ, Westney. Pubic osteomyelitis following bladder neck surgery using bone anchors: a report of 9 cases. J Urol. 2002; 168: 2055-2057. [DOI] [PubMed] [Google Scholar]
- 5.Sanchez A, Rodríguez D, Cheng J-S, McGovern FJ, Tabatabaei S. Prostato-symphyseal fistula after photoselective vaporization of the prostate: case series and literature review of a rare complication. Urology. 2015; 85: 172-177. [DOI] [PubMed] [Google Scholar]
- 6.Stern JA, Clemens JQ. Osteomyelitis of the pubis: a complication of a chronic indwelling catheter. Urology. 2003; 61: 462. [DOI] [PubMed] [Google Scholar]
- 7.Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo Classification of Surgical Complications: Five-Year Experience. Ann Surg. 2009; 250: 187-196. [DOI] [PubMed] [Google Scholar]
- 8.Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J Pain Symptom Manage. 2011; 41: 1073-1093. [DOI] [PubMed] [Google Scholar]
- 9.Epstein JI, Egevad L, Amin MB, et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am J Surg Pathol. 2016; 40: 244-252. [DOI] [PubMed] [Google Scholar]
- 10.McHenry MC, Alfidi RJ, Wilde AH, Hawk WA. Hematogenous osteomyelitis: A changing disease. Cleve Clin Q. 1975; 42: 125-153. [DOI] [PubMed] [Google Scholar]
- 11.Matsushita K, Ginsburg L, Mian BM, et al. Pubovesical fistula: a rare complication after treatment of prostate cancer. Urology. 2012; 80: 446-451. [DOI] [PubMed] [Google Scholar]
- 12.Lobo N, Kulkarni M, Hughes S, Nair R, Khan MS, Thurairaja R. Urologic Complications Following Pelvic Radiotherapy. Urology. 2018; 122: 1-9 [DOI] [PubMed] [Google Scholar]
- 13.Angioli R, Penalver M, Muzii L, et al. Guidelines of how to manage vesicovaginal fistula. Crit Rev Oncol Hematol. 2003; 48: 295-304. [DOI] [PubMed] [Google Scholar]
- 14.Degheili JA, Mansour MM, Nasr RW. Symphysis Pubis Osteomyelitis: An Uncommon Complication after Robotic Assisted Radical Prostatectomy - Case Description with Literature Review. Case Rep Urol. 2018: 5648970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kahokehr AA, Boysen WR, et al. Urinary Pubic Symphysis Fistula Leads to Histopathologic Osteomyelitis in Prostate Cancer Survivors. Urology. 2021; 148: 297-301. [DOI] [PubMed] [Google Scholar]
- 16.Lavien G, Chery G, Zaid UB, Peterson. Pubic Bone Resection Provides Objective Pain Control in the Prostate Cancer Survivor With Pubic Bone Osteomyelitis With an Associated Urinary Tract to Pubic Symphysis Fistula. Urology. 2017; 100: 234-239. [DOI] [PubMed] [Google Scholar]
- 17.Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg. 2009; 23: 80-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sexton SJ, Lavien G, Said N, Eward W, Peterson AC, Gupta RT. Magnetic resonance imaging features of pubic symphysis urinary fistula with pubic bone osteomyelitis in the treated prostate cancer patient. Abdom Radiol (NY). 2019; 44: 1453-1460. [DOI] [PubMed] [Google Scholar]