Abstract
A method of one-stage rapid detection and differentiation of epidemiologically important variola virus (VARV), monkeypox virus (MPXV), and varicella-zoster virus (VZV) utilizing multiplex real-time TaqMan PCR assay was developed. Four hybridization probes with various fluorescent dyes and the corresponding fluorescence quenchers were simultaneously used for the assay. The hybridization probes specific for the VARV sequence contained FAM/BHQ1 as a dye/quencher pair; MPXV-specific, JOE/BHQ1; VZV-specific, TAMRA/BHQ2; and internal control-specific, Cy5/BHQ3. The specificity and sensitivity of the developed method were assessed by analyzing DNA of 32 strains belonging to orthopoxvirus and herpesvirus species.
Keywords: Variola virus, Monkeypox virus, Varicella-zoster virus, Real-time PCR
1. Introduction
Thirty-five years ago, the 33rd World Health Assembly declared the global eradication of smallpox, putting in cessation of vaccination against smallpox, taking into account the post-vaccination complications caused by classical live vaccinia virus (VACV) vaccine. Thus, worldwide, almost all individuals below 35 years of age have no immunity and older people that have been vaccinated against smallpox display a weakened immunity against orthopoxvirus infections. Human population year by year becomes ever more unprotected not only from a potential infection with variola virus (VARV) as a result of a bioterrorism attack or reemergence of the virus in nature, but also from infection with other closely related orthopoxviruses, such as monkeypox virus (MPXV), the natural reservoir of which is small rodents (Shchelkunov, 2013). Presumably, this is why the number of reported outbreaks of the human diseases caused by the zoonotic MPXV is increasing in Democratic Republic of Congo and its neighboring countries (Stephenson, 2003, Lewis-Jones, 2004, Rimoin et al., 2007, Rimoin et al., 2010). In such monkeypox-endemic regions diagnosis of varicella-zoster virus (VZV) and MPXV infections can be mistaken (Jezek et al., 1988). Diagnostic differences between these infections include centrifugal type of lesion distribution for human monkeypox, and centripetal − for chickenpox caused by VZV; presence of febrile prodrome and lymphadenopathy and occurrence of deep pustular lesions on the hand's palms and feet's soles for human monkeypox and their absence for chickenpox infection (MacNeil et al., 2009). But this is not sufficient for an accurate diagnosis, especially in the case of monkeypox atypical forms, which cannot be easily distinguished from VZV or VARV infections (MacNeil et al., 2009, Nalca et al., 2005).
Monkeypox by contrast to chickenpox in human is associated with severe complications and mortality rate up to 10% (Jezek et al., 1987). There is no doubt about the need for rapid and reliable method of differentiation of these infectious agents as an important first step in the complex chain of epidemiological and therapeutic measures for the prevention of outbreaks.
In this work, a method for identification and species-specific differentiation of human pathogenic variola and monkeypox viruses with simultaneous discrimination of varicella-zoster virus and using of the internal control (IC) in one reaction mixture of a multiplex real time TaqMan PCR assay is described.
2. Materials and methods
2.1. Viruses and DNA samples
The virus DNA samples used in this work are listed in Table 1 . Archive clinical samples (scabs) of VARV (strains Brazil 128, Brazil 131 and India 378) were obtained from human cases during the smallpox eradication program in 1970–1975 and have been preserved in the Russian collection of VARV (Table 1). Experimental samples of MPXV DNA were obtained from spleen, lungs, liver, blood, oral swabs, and pustules on 13th day after intranasal infection of marmots with 7.1 log10 plaque forming units of MPXV strain CDC#v79-I-005 (Sergeev et al., 2015). Virus DNA was extracted from clinical and experimental samples using QIAamp DNA Mini kit (Qiagen, USA) according to the manufacturer’s instruction. All manipulations with the samples containing VARV and MPXV were performed in a specialized high-level biocontainment laboratory certified as WHO Collaborating Center for Orthopoxvirus Diagnosis and Repository for Variola Virus Strains and DNA (Koltsovo, Russia).
Table 1.
The list of virus strains whose DNA was used in multiplex real-time PCR.
| Virus (family/genus/species) | Strain | Source of DNA | Avr positive Ct value for: |
||
|---|---|---|---|---|---|
| VARV | MPXV | VZV | |||
| Poxviridae | |||||
| Orthopoxvirus | |||||
| Variola virus | Brazil 128* | 1 | 18.2 | Neg | Neg |
| Brazil 131* | 1 | 27.3 | Neg | Neg | |
| Butler | 1 | 28.2 | Neg | Neg | |
| Congo 9 | 1 | 17.8 | Neg | Neg | |
| India 4a | 1 | 15.3 | Neg | Neg | |
| India 71 | 1 | 22.1 | Neg | Neg | |
| India 378* | 1 | 18.7 | Neg | Neg | |
| Kuwait 5 | 1 | 15.9 | Neg | Neg | |
| M-Gavr-60 | 1 | 15.5 | Neg | Neg | |
| Ngami | 1 | 16.8 | Neg | Neg | |
| Rw-18 | 1 | 15.2 | Neg | Neg | |
| 13/62 | 1 | 16.7 | Neg | Neg | |
| Jun-58 | 1 | 32.2 | Neg | Neg | |
| Monkeypox virus | CDC#v97-I-004 | 2 | Neg | 16.9 | Neg |
| CDC#v79-I-005 | 2 | Neg | 16.3 | Neg | |
| Cowpox virus | GRI-90 | 1 | Neg | Neg | Neg |
| OPV-Claus | 3 | Neg | Neg | Neg | |
| OPV-89/3 | 3 | Neg | Neg | Neg | |
| OPV-89/4 | 3 | Neg | Neg | Neg | |
| OPV-90/2 | 3 | Neg | Neg | Neg | |
| OPV-90/5 | 3 | Neg | Neg | Neg | |
| OPV-98/5 | 3 | Neg | Neg | Neg | |
| 88-Lunge | 3 | Neg | Neg | Neg | |
| Vaccinia virus | Elestree 3399 | 1 | Neg | Neg | Neg |
| LIVP | 1 | Neg | Neg | Neg | |
| Western Reserve | 1 | Neg | Neg | Neg | |
| Ectromelia virus | K1/2 | 1 | Neg | Neg | Neg |
| MP-2 | 3 | Neg | Neg | Neg | |
| Camelpox virus | CP-5 | 3 | Neg | Neg | Neg |
| Leporipoxvirus | |||||
| Myxoma virus | Lausanne | 4 | Neg | Neg | Neg |
| Avipoxvirus | |||||
| Fowlpox virus | FP9 | 5 | Neg | Neg | Neg |
| Herpesviridae | |||||
| Varicellovirus | |||||
| Varicella-zoster virus | VZV №4 | 6 | Neg | Neg | 21.6 |
| Simplexvirus | |||||
| Human herpesvirus 1 | HF | 6 | Neg | Neg | Neg |
| Human herpesvirus 2 | MS | 6 | Neg | Neg | Neg |
Notes: *—clinical specimens. (1)—virus DNAs were isolated from the strains deposited with the collection of the SRC VB “Vector”. Other viral DNAs were received from J.J. Esposito, Atlanta, United States (2); from H. Meyer, Munich, Germany (3); from G. McFadden, London, Canada (4); from M. Skinner, Newbury, UK (5); from M.A. Susloparov, SRC VB “Vector” (6).
2.2. Primer and probe design
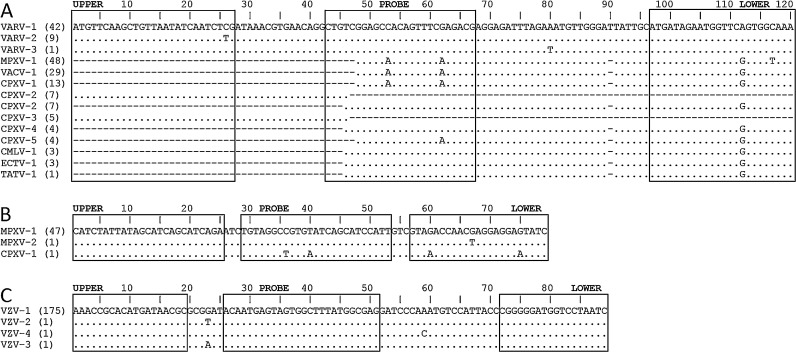
Selection of species-specific oligonucleotide primers and hybridization probes was performed from alignments, based on available nucleotide sequences of VZV and orthopoxvirus strains belonged to six species: VARV, MPXV, cowpox virus (CPXV), VACV, ectromelia virus (ECTV), camelpox virus (CMLV), in programs BioEdit v.7.0 and Muscle v.3.6. Based on obtained data, the species-specific regions in the genomes of these viruses were detected: the B12R gene region for VARV [according to the VARV India-1967 strain classification (Shchelkunov et al., 1993)]; gene F3L for MPXV [according to the MPXV Zaire-96-I-16 strain classification (Shchelkunov et al., 2002)]; and ORF38 for VZV [according to the VZV Ellen strain classification (Peters et al., 2012)].
Oligonucleotide primers and the corresponding hybridization probes for each selected region were calculated using the program Oligo (Table 2 ). Fluorescent dyes and the corresponding fluorescence quenchers were introduced into each hybridization probe: the hybridization probe specific for VARV sequence contained the FAM/BHQ1 dye/quencher pair; MPXV-specific probe – JOE/BHQ1; VZV-specific probe – TAMRA/BHQ2; and IC-specific probe – Cy5/BHQ3 pair. B12R gene region is present in most orthopoxviruses, but only VARV has no extensive deletions characteristic for other species, which allowed choosing the oligonucleotide primers and the corresponding hybridization probe specific for VARV (Fig. 1 A). Conversely, in 7 of the 36 CPXV strains (group CPXV-2 in Fig. 1A) this region is presented with extended insertions, allowing amplification of PCR products with lengths up to 7 kbp using VARV-specific primers, which ensures the absence of false-positive results for these CPXV strains using species-specific detection of VARV based on ORF B12R. MPXV F3L gene region has genetic homology with only one CPXV strain (Fig. 1B), herewith, the four nucleotide substitutions present in the sequences complementary for MPXV-specific oligonucleotide primer and hybridization probe would allow excluding any misdiagnosis. ORF38 region in VZV is completely species-specific (Fig. 1C). Sizes of fragments for selected PCR target genes are: B12R (VARV, 120 bp, 161552–161671 bp according to the VARV India-1967 strain), F3L (MPXV, 79 bp, 48362–48440 bp according to the MPXV Zaire-96-I-16 strain), ORF38 (VZV, 89 bp, 69295–69383 bp according to the VZV Ellen strain).
Table 2.
Oligonucleotide primers and hybridization probes used in multiplex real-time PCR.
| Virus | Viral ORF | Oligonucleotide name | Oligonucleotide sequence |
|---|---|---|---|
| VARV | B12R | VARV_B12R_probe | FAM-5′-CTGTCGGAGCCACAGTTTCGAGACG-3′-BHQ1 |
| VARV_B12R_upper | 5′-ATGTTCAAGCTGTTAATATCAATCTCG-3′ | ||
| VARV_B12R_lower | 5′-TTTGCCACTGAACCATTCTATCAT-3′ | ||
| MPXV | F3L | MPXV_F3L_probe | JOE-5′-TGTAGGCCGTGTATCAGCATCCATT-3′-BHQ1 |
| MPXV_F3L_upper | 5′-CATCTATTATAGCATCAGCATCAGA-3′ | ||
| MPXV_F3L_lower | 5′-GATACTCCTCCTCGTTGGTCTAC-3′ | ||
| VZV | ORF38 | VZV_ORF38_probe | TAMRA-5′-ACAATGAGTAGTGGCTTTATGGCGAG-3′-BHQ2 |
| VZV_ORF38_upper | 5′-AAACCGCACATGATAACGC-3′ | ||
| VZV_ORF38_lower | 5′-GATTAGGACCATCCCCCG-3′ | ||
| IC | – | IC_probe | Cy5-5′-TTGCTTGTCGTGCTCGTATCGTCC-3′-BHQ3 |
Fig. 1.
Sequence alignments of target regions for the VARV ORF B12R (A), MPXV ORF F3L (B) and VZV ORF38 (C). The alignments of 169 (A), 49 (B) and 178 (C) strains were made using BioEdit Sequence Alignment Editor. Strains within one species with identical target region were condensed (the number in parentheses represents the number of strains included). Dotes represent the identical nucleotides in the compared sequences of virus genomes relative to the reference sequences (A: VARV strain India-1967, B: MPXV strain Zaire-96-I-16 and C: VZV strain Ellen); dashes represent the nucleotide deletions. The nucleotide positions in analyzed DNA segments are shown above the nucleotide sequences (positions according to the virus DNA: A, 161552–161671 bp according to the VARV India-1967 strain; B, 48362–48440 bp according to the MPXV Zaire-96-I-16 strain; C, 69295–69383 bp according to the VZV Ellen strain). A: UPPER, VARV_B12R_upper; PROBE, VARV_B12R_probe; LOWER, VARV_B12R_lower. B: UPPER, MPXV_F3L_upper; PROBE, MPXV_F3L_probe; LOWER, MPXV_F3L_lower. C: UPPER, VZV_ORF38_upper; PROBE, VZV_ORF38_probe; LOWER, VZV_ORF38_lower.
2.3. Positive controls
Plasmids pVARV-B12R, pMPXV-F3L, pVZV-ORF38, containing fragments of VARV ORF B12R, MPXV ORF F3L, VZV ORF 38, respectively, were constructed. Fragments were obtained by annealing two long oligonucleotides with “sticky” ends corresponding for restriction enzymes SalI and BamHI, containing target region for each virus (Table 3 ). Fragments were further inserted into the pBluescript II SK (+) vector (Stratagene, USA) previously digested with SalI and BamHI, ligated and transformed into E. coli strain XL2blue. Recombinant plasmids were isolated using a QIAprep Spin Miniprep Kit (Qiagen, USA). The presence of the target insert in the selected hybrid plasmids was verified by PCR assay and sequencing. The concentration of plasmids was determined spectrophotometrically in an Ultrospec 3000 pro spectrophotometer (Biochrom, UK).
Table 3.
Oligonucleotide primers used for construction of positive controls.
 |
GATC—“sticky” ends of restriction enzyme BamHI.
TCGA—“sticky” ends of restriction enzyme SalI.
Nucleotide sequences that are complementary to the appropriate oligonucleotide primers and hybridization probe are marked gray (Table 2).
2.4. Internal control
The pIC plasmid was constructed previously (Maksyutov et al., 2015). To reduce the total number of oligonucleotides used in the mixture, the target region for internal control represents a unique sequence for IC-specific hybridization probe with flanking sequences complementary to VARV-specific oligonucleotide primers. The pIC plasmid is added to the lysis buffer prior DNA extraction in the quantity of 104 copies per sample (5 × 101–103 copies per the final reaction depending on extraction method and elution volume).
2.5. 5′ Nuclease PCR assay
The PCR assay with cleavage of the 5′-terminal label (TaqMan assay) was conducted in a Real-Time PCR System 7500 (Applied Biosystems, USA) device. The reaction mixture (25 μl) contained 2.5 μl 10 × TaqMan® Buffer A, 200 μM dNTP, 5 mM MgCl2, three primer pairs (300 nM each), four hybridization probes (250 nM each), 0.5 U AmpliTaq Gold® DNA polymerase, and 1 μl of analyzed DNA solution. The PCR with recording of fluorescence intensity was performed according to the following protocol: 10 min at 95 °C and 45 cycles of 15 s at 95 °C and 1 min at 63 °C.
3. Results
The analytical specificity in a multiplex format was determined using a panel of DNA specimens of 31 virus strains (Table 1). Various VARV, MPXV, and VZV strains were successfully identified in the multiplex real-time PCR. The used mixture of oligonucleotides gave no products in the PCR with DNAs of other orthopoxviruses (CPXV, VACV, ECTV and CMLV), DNAs of unrelated poxviruses, namely, rabbit myxoma virus (genus Leporipoxvirus) and fowlpox virus (genus Avipoxvirus), as well as with human genomic DNA and the DNAs of the human exanthemic pathogens, such as herpes simplex (HHV-1 and HHV-2) viruses. Thus, the analytical specificity of the multiplex real-time PCR assays in the conducted experiments equaled 100% (Table 1). The analytical specificity in a multiplex format was also determined using mixed specimens since double infections of MPXV and VZV have been reported (Dumont et al., 2014). Different combinations of mixed specimens (VARV + MPXV, MPXV + VZV and VARV + VZV) were successfully identified without significant decrease of Ct compared with samples containing one virus.
The diagnostic specificity was verified using 20 whole blood preparations from healthy humans. pIC was added to all blood samples to assess the possible inhibition issue. After isolation from whole blood, the DNA specimens were analyzed in the designed multiplex real-time PCR system, and none of the samples gave a positive result for VARV, MPXV or VZV. Wherein signal through Cy5 optical channel gave a positive result in specified Ct interval for all samples.
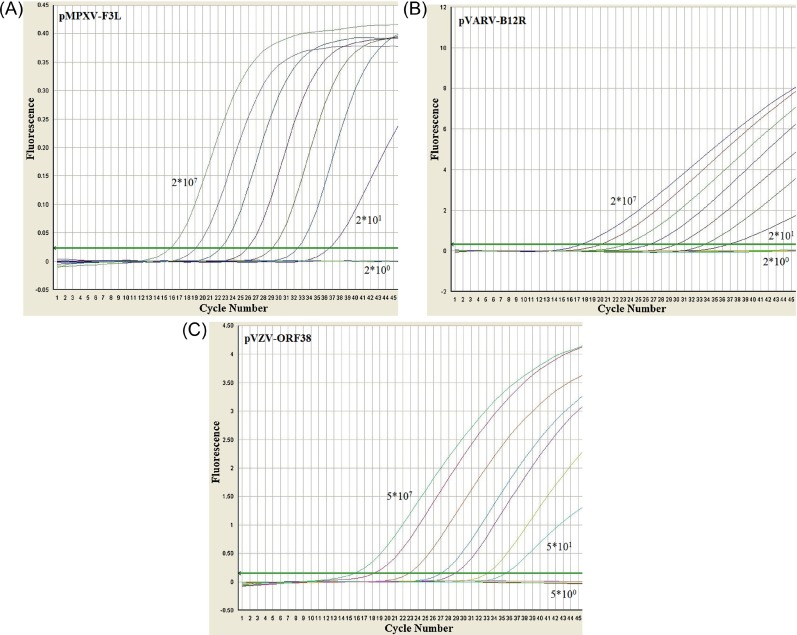
The limit of detection was assessed using the recombinant plasmids pVARV-B12R, pMPXV-F3L, and pVZV-ORF38. Tenfold dilutions in three independent replicates were prepared for each plasmid. The experiments demonstrated a reproducible detection of approximately 20 copies for VARV and MPXV and 50 copies for VZV DNAs per reaction (Fig. 2 ).
Fig. 2.
The dependence of fluorescence signal on the number of cycles in real-time PCR. The data were obtained using a Real-Time PCR System 7500 (Applied Biosystems) device with oligonucleotide primers and hybridization probes calculated for species-specific identification of VARV, MPXV, VZV using recombinant plasmids pVARV-B12R, pMPXV-F3L and pVZV-ORF38 (Table 2) (tenfold quantities of copies per reaction are marked). Data are shown for each optical channel used for fluorescence detection: the signal of FAM dye conjugated with VARV-specific hybridization probe, 518 nm; the signal of JOE conjugated with MPXV-specific hybridization probe, 548 nm; the signal of TAMRA conjugated with VZV-specific hybridization probe, 580 nm. Cycle Number – the number of cycles in real-time PCR. Fluorescence – the value of fluorescence signal.
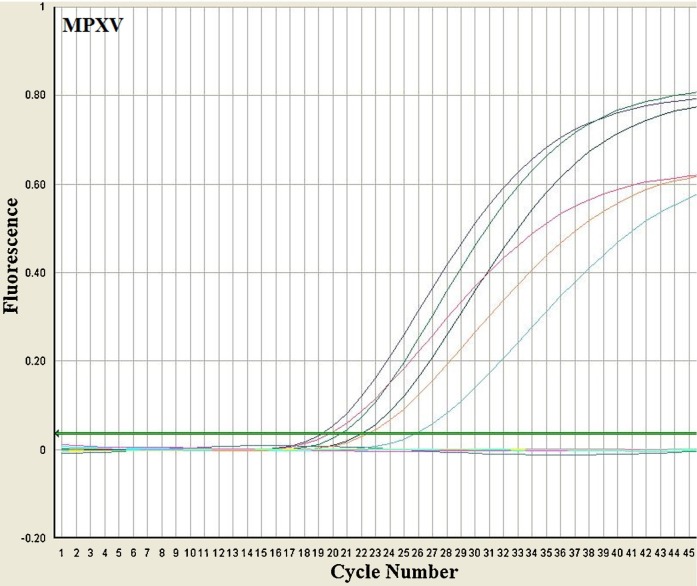
Applicability of the developed assay for diagnosing purposes was studied using clinical and experimental specimens. Archive clinical samples of VARV (scabs) obtained from human cases during the smallpox eradication program in 1970–1975 (Table 1) and experimental samples obtained after intranasal infection of marmot with MPXV (Sergeev et al., 2015) were successfully identified in these samples (Fig. 3 ).
Fig. 3.
The dependence of fluorescence signal on the number of cycles in real-time PCR. The data were obtained using a Real-Time PCR System 7500 (Applied Biosystems) device with the oligonucleotide primers and hybridization probes calculated for species-specific identification of VARV, MPXV, VZV. DNA samples were extracted from experimental specimens (spleen (Ct 22.1), lungs (Ct 19.8), liver (Ct 22.5), blood (Ct 25.9), oral swabs (Ct 20.5), pustules (Ct 19.2)) from marmots infected with MPXV strain CDC#V79-I-005. The data for 548 nm optical channel used for fluorescence detection of JOE conjugated with MPXV-specific hybridization probe are presented. Cycle Number – the number of cycles in real-time PCR. Fluorescence – the value of fluorescence signal.
4. Discussion
Improvement of methods for laboratory diagnostics of extremely dangerous infections is an integral part of epidemiological surveillance. The need for a rapid and accurate method for the diagnosis of smallpox is undisputed considering the possibility of emergence of a VARV-like virus as a result of natural evolution of the existing zoonotic orthopoxviruses (Shchelkunov, 2011, Shchelkunov, 2013) or deliberate reconstructing of VARV by synthetic biology. The major part of human population has no immunity not only to smallpox, but also to other orthopoxvirus infections caused by the zoonotic viruses, such as MPXV. This is demonstrated by more frequent outbreaks of human orthopoxvirus infections caused by this virus in several countries (Stephenson, 2003, Lewis-Jones, 2004, Rimoin et al., 2007, Rimoin et al., 2010). In addition, in the context of the global spread of virus infections, an urgent threat of appearance of such infections as monkeypox on the non-endemic territory remains. In order to develop a rapid response to prevent the spread of the infection, and given the similarity of the clinical manifestations of monkeypox with a widespread infection of chickenpox caused by VZV, it is necessary to conduct differential diagnostics of given infectious agents.
Thus, the creation of a convenient, fast, simple and reliable method of laboratory diagnostics of extremely dangerous and socially significant infections such as VARV, MPXV and VZV is timely and necessary. Previously, a complex procedure had been proposed for identification of all three agents: VARV, MPXV and VZV (Dumont et al., 2014). It consists of several independent methods and has a number of inaccuracies which could give a false-positive result as MPXV for ECTV sample. Also, a VARV-specific probe has a 1 nt change for 9 VARV strains with known DNA sequences, which could lead to false negative results.
In this work, a method for one-step, rapid and specific discrimination between rash illnesses outbreaks caused by variola, monkeypox or varicella-zoster viruses has been proposed. The target regions of virus genomes used for PCR analysis eliminate the possibility of false-positive and false-negative results that were experimentally confirmed on a panel of DNA specimens of 34 virus strains and 20 whole blood preparations from healthy humans. The multiplex format provides unification of the analytical procedure since the same protocol and reaction conditions are used for all pathogens. Considering that patient samples could also contain PCR-inhibiting substances, an internal control has been used for elimination of false-negative results. The possibility of using this method for diagnostics was successfully tested using clinical and experimental specimens. Since double infections of MPXV and VZV have been previously reported, the method was tested on different combinations of mixed specimens.
After a robust validation step on actual clinical samples (with the exception of VARV) and subsequent assay registration, the new developed method could be used for VZV and MPXV outbreaks control in monkeypox endemic territories with the potential use in weakly equipped laboratories of these countries.
Acknowledgements
Authors are sincerely grateful to L. Bulychev and S. Bodnev for performance of the experiment on infecting marmot with MPXV and H. Meyer, J. Esposito, G. McFadden, M. Susloparov, and M. Skinner for kindly provided specimens of virus DNAs.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jviromet.2016.07.024.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- Dumont C., Irenge L.M., Magazani E.K., Garin D., Muyembe J.J.T., Bentahir M., Gala J.L. Simple technique for in field samples collection in the cases of skin rash illness and subsequent PCR detection of orthopoxviruses and varicella zoster virus. PLoS One. 2014;9:e96930. doi: 10.1371/journal.pone.0096930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jezek Z., Szczeniowski M., Paluku K.M., Mutombo M. Human monkeypox: clinical features of 282 patients. J. Infect. Dis. 1987;156:293–298. doi: 10.1093/infdis/156.2.293. [DOI] [PubMed] [Google Scholar]
- Jezek Z., Szczeniowski M., Paluku K.M., Mutombo M., Grab B. Human monkeypox: confusion with chickenpox. Acta Trop. 1988;45:297–307. [PubMed] [Google Scholar]
- Lewis-Jones S. Zoonotic poxvirus infections in humans. Curr. Opin. Infect. Dis. 2004;17:81–89. doi: 10.1097/00001432-200404000-00003. [DOI] [PubMed] [Google Scholar]
- MacNeil A., Reynolds M.G., Carroll D.S., Karem K., Braden Z., Lash R., Moundeli A., Mombouli J.V., Jumaan A.O., Schmid D.S., Damon I.K. Monkeypox or varicella? Lessons from a rash outbreak investigation in the Republic of the Congo. Am. J. Trop. Med. Hyg. 2009;80:503–507. [PubMed] [Google Scholar]
- Maksyutov R.A., Gavrilova E.V., Meyer H., Shchelkunov S.N. Real-time PCR assay for specific detection of cowpox virus. J. Virol. Methods. 2015;211:8–11. doi: 10.1016/j.jviromet.2014.10.004. [DOI] [PubMed] [Google Scholar]
- Nalca A., Rimoin A.W., Bavari S., Whitehouse C.A. Reemergence of monkeypox: prevalence, diagnostics, and countermeasures. Clin. Infect. Dis. 2005;41:1765–1771. doi: 10.1086/498155. [DOI] [PubMed] [Google Scholar]
- Peters G.A., Tyler S.D., Carpenter J.E., Jackson W., Mori Y., Arvin A.M., Grose C. The attenuated genotype of varicella-zoster virus includes an ORF0 transitional stop codon mutation. J. Virol. 2012;86:10695–10703. doi: 10.1128/JVI.01067-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimoin A.W., Kisalu N., Kebela-Ilunga B., Mukaba T., Wright L.L., Formenty P., Wolfe N.D., Shongo R.L., Tshioko F., Okitolonda E., Muyembe J.J., Ryder R., Meyer H. Endemic human monkeypox, democratic republic of Congo, 2001–2004. Emerg. Infect. Dis. 2007;13:934–937. doi: 10.3201/eid1306.061540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimoin A.W., Mulembakani P.M., Jonston S.C., Smith J.O.L., Kisalu N.K., Kinkela T.L., Blumberg S., Thomassen H.A., Pike B.L., Fair J.N., Wolfe N.D., Shongo R.L., Graham B.S., Formenty P., Okitolonda E., Hensley L.E., Meyer H., Wright L.L., Muyembe J.J. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc. Natl. Acad. Sci. U. S. A. 2010;107:16262–16267. doi: 10.1073/pnas.1005769107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sergeev A.A., Kabanov A.S., Bulychev L.E., Sergeev A.A., Pyankov O.V., Bodnev S.A., Galahova D.O., Zamedyanskaya A.S., Titova K.A., Glotova T.I., Taranov O.S., Omigov V.V., Shishkina L.N., Agafonov A.P., Sergeev A.N. Using the ground squirrel (Marmota bobak) as an animal model to assess monkeypox drug efficacy. Transbound. Emerg. Dis. 2015 doi: 10.1111/tbed.12364. [DOI] [PubMed] [Google Scholar]
- Shchelkunov S.N., Resenchuk S.M., Totmenin A.V., Blinov V.M., Marennikova S.S., Sandakhchiev L.S. Comparison of the genetic maps of variola and vaccinia viruses. FEBS Lett. 1993;327:321–324. doi: 10.1016/0014-5793(93)81013-p. [DOI] [PubMed] [Google Scholar]
- Shchelkunov S.N., Totmenin A.V., Safronov P.F., Mikheev M.V., Gutorov V.V., Ryazankina O.I., Petrov N.A., Babkin I.V., Uvarova E.A., Sandakhchiev L.S., Sisler J.R., Esposito J.J., Damon I.K., Jahrling P.B., Moss B. Analysis of the monkeypox virus genome. Virology. 2002;297:172–194. doi: 10.1006/viro.2002.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shchelkunov S.N. Emergence and reemergence of smallpox: the need in development of a new generation smallpox vaccine. Vaccine. 2011;29:D49–D53. doi: 10.1016/j.vaccine.2011.05.037. [DOI] [PubMed] [Google Scholar]
- Shchelkunov S.N. An increasing danger of zoonotic orthopoxvirus infections. PLoS Pathog. 2013;9(12):e1003756. doi: 10.1371/journal.ppat.1003756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson J. Monkeypox outbreak a reminder of emerging infections vulnerabilities. J. Am. Med. Assoc. 2003;290:23–24. doi: 10.1001/jama.290.1.23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.