Abstract
Health care is undergoing a profound technological and digital transformation and has become increasingly complex. It is important for burns professionals and researchers to adapt to these developments which may require new ways of thinking and subsequent new strategies. As Einstein has put it: “We must learn to see the world anew.” The relatively new scientific discipline “Complexity science” can give more direction to this and is the metaphorical open door that should not go unnoticed in view of the burn care of the future. Complexity science studies “why the whole is more than the sum of the parts.” It studies how multiple separate components interact with each other and their environment and how these interactions lead to “behavior of the system.” Biological systems are always part of smaller and larger systems and exhibit the behavior of adaptivity, hence the name complex adaptive systems. From the perspective of complexity science, a severe burn injury is an extreme disruption of the “human body system.” But this disruption also applies to the systems at the organ and cellular levels. All these systems follow the principles of complex systems. Awareness of the scaling process at multilevel helps to understand and manage the complex situation when dealing with severe burn cases. This paper aims to create awareness of the concept of complexity and to demonstrate the value and possibilities of complexity science methods and tools for the future of burn care through examples from preclinical, clinical, and organizational perspectives in burn care.
Burn care has undergone a revolutionary development in recent decades. Where survival from a severe burn was an exception in the western world, it now has become the rule even for victims at the extremes of age.1 This progress has been facilitated by many relevant developments in science, medicine, nursing, microbiology, welfare (hygiene), engineering, and computer science. Care no longer focuses solely on survival and wound healing, but also to a large extent on the quality of life, psychological well-being, and reintegration of patients into society. Age and comorbidities, notably multifactorial chronic diseases, such as diabetes and obesity adversely influence the disease process and recovery of the patients.2 Burn care thus has become more complex. Although many burn care professionals do not realize this, working in a burn center means working in a complex adaptive system amid many other complex adaptive systems.
From the perspective of complexity science, the body can be considered as an operating complex adaptive system consisting of many complex adaptive systems on smaller scales (like organs, tissues, cells) and larger scales (society). The body’s systems are normally in balance and show recovery through self-organization and buffering. In a severe burn, multiple systems which are dynamically interconnected can become noticeably unbalanced leading to burn shock, acute renal failure, and/or psychological derailment, for example. Complex systems can be present at different levels and complexity science can also be used for research purposes to study processes at the cellular, physical, and societal levels. The individual cell is already a complex system with its own metabolism, division, communication, migration, DNA assembly, and so on. From a metalevel, human individuals can be studied as a complex system where every person is part of human networks and have interaction. It, therefore, means that not only burn care itself, but also the burn research can benefit from it.
This perspective paper is written to lift the tip of the veil in terms of the added value of complexity science for the future of burn care and its research. The aim is to raise awareness of the concept of complexity and the interesting similarities of its concept at macro-scale (society), human scale (patients), or microscale (like the cellular level). This will help to understand the overall processes of systems which burn care professionals have to deal with. The ultimate goal would be to improve burn care for the benefit of the individual patient. The basic principles of complex systems and complexity science will be discussed and their potentials for health care professionals via realistic examples.
COMPLEXITY SCIENCE AND COMPLEX SYSTEMS
Complexity Science
Complexity science is a relatively young science that can play an important role in scientific progress and understanding of the more complex physical, biological, and social systems than the traditionally applied reductionist thinking.3 It must be acknowledged that the classic reductionist approach has led to many scientific advances and discoveries in the past like anatomical dissection has provided a lot of knowledge about the components and structure of the human body. The reductionist approach means to understand “the whole” by studying individual components; however, it misses the interaction between the individual components. This interaction is crucial in many systems such as in biology where the whole is more than just the sum over all components. This is what makes complexity science so relevant in this modern era because it takes a more holistic view of systems. Complexity science sees natural systems as “open,” with boundaries that are not always evident, constantly adapting to the pressure of the environment.4 It regards small components as part of a larger whole and it accounts for the interactions between the components that give complex behavior. Knowledge and application of the principles of complexity theory make many situations more understandable and provide opportunities for adaptation and anticipation.5 On the other hand, understanding the principles of complex systems does not make the systems completely predictable, but it allows quantification of uncertainty in outcomes given different perturbations or signals affecting the state.
Complex (Adaptive) Systems
Complex systems, such as the human immune system, the neural network of our brains, the body itself, the Internet of Things, the global economy, stock markets, and traffic are omnipresent and are part of our daily life. Although totally different in subject matter, these systems show remarkable similarities in their structure and dynamics, which is so typical for complex systems.
There is no uniform definition for the concept of complex systems, but it can be described as systems in which large networks of components with no central control and simple rules of operation give rise to complex collective behavior, sophisticated information processing, and adaptation via learning or evolution.6
Complex systems have structural and dynamic characteristics. The structure contains multiple components, organized into networks that interact within the network and other networks at different levels, which is called multi-scaling. Dynamic features of such systems are nonlinearity, emergence, unpredictability or limited predictability, and buffering. Table 1 lists the most relevant features.
Table 1.
Characteristics of complex systems
| Characteristic | Description | Example |
|---|---|---|
| Multicomponent | Complex systems involve multiple components (also “agents” or “actors”), which are essential to define how the system works5,6 | Lymphocytes, neutrophils, monocytes, and macrophages form together the immune system with many other components |
| Network structure | The actors are interconnected in a network structure in the system51 | The human brain is made up of a complex network of neurons |
| Multi-scaling | In general, complex systems are made up of many interacting complex sub-systems which are themselves built upon multiple complex sub-systems (and so on) | The human body is a complex system that is made up of many complex sub-systems such as organs or tissues which are in turn made of complex systems (cells). These systems interact together at micro-, meso-, and macro scales to appear as a complex system operating at a higher level |
| Out of equilibrium systems | A complex system is generally robust and tends toward balance and homeostasis. Exhibits multiple stable states where the system can reside67 | Inflammation after an infection: systemic response increases, after a while decreases/stabilizes again at a new set point |
| Adaptiveness | Many biological, living systems show an adaptive behavior5,6 | In the human body, most systems are adaptive like the immune system and the neural network. People show adaptive behavior at individual level. In society, we can see adaptive behavior as well. These systems are, from an evolutionary point of view, a logical development because they can adapt their behavior to changes in the environment and are “adaptive” or “learning.” Hence, the name complex adaptive system (CAS) |
| Unpredictability | Unpredictability and uncertainty are normal features of complex systems67 | After a severe burn injury, many events can occur that are fairly unpredictable, such as the occurrence of pneumonia, thrombosis, wound infections, problematic scarring, psychological and social consequences, and so on |
| Nonlinearity | Nonlinearity means that the initial effect of a stressor on the complex system can be small, but the ultimate effect is enormous | The systematic hyperinflammatory response (burn shock) |
| Emergent | Many complex systems may also show emergent behavior: the arising of novel and coherent structures, patterns, or properties during the process of self-organization in complex systems68 | Life itself may be regarded as an example of emergence: the sum of loose components is much bigger than the parts through the interaction of the components of the system. Innovation and creative processes are often the results of emergence |
| Tipping points | In (biological) complex systems are in balance but also there a moment may arise when the state of the system suddenly changes. This is called the tipping point. If and when a tipping point occurs is fairly unpredictable69,70 | After a severe burn injury, the patient suddenly may become hemodynamically unstable |
| Randomness | A complex system can produce outcome without known and predicable order6 | The immune system employs randomness to allow each individual lymphocyte to recognize a range of shapes that differs from the range recognized by other lymphocytes in the population |
| Path dependency | A change in state of system may occur through a certain path, however, the change cannot be reversed following the same path in reverse71 | The process by which a burn turns into scar tissue |
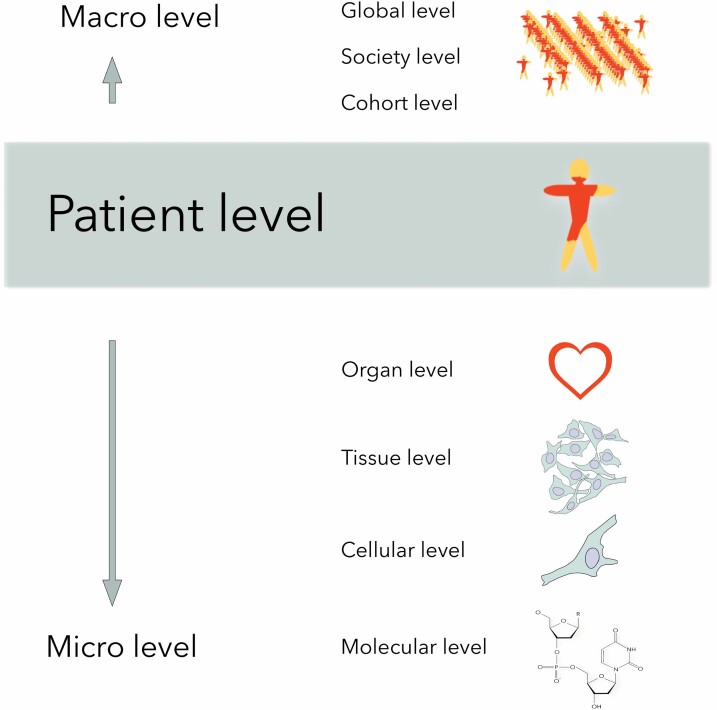
In biology, most complex systems are adaptive in nature. Such systems are called complex adaptive systems.7 The body is a complex adaptive system made up of many complex adaptive systems such as the immune system. The immune response of the body shows typical characteristics of a complex adaptive system because it consists of multiple actors, that is, “agents” (eg, cytokines, immune cells) acting independently to tackle a threat (inflammation). Depending on the task at hand, they influence the state of the body’s immune system and give rise to stable and meta-stable conditions, thereby exhibiting self-organization. These conditions emerge because of the agent interactions and cannot be attributed to the action of a single entity. The new system states in turn alter the agents themselves thus resulting in co-evolution of the system and actors involved. Such complex adaptive systems are not restricted to microscopic systems. They also spontaneously evolve at meso-level, (the human body) and at macroscopic level (such as the structure of a care organization and even on a global scale). Figure 1 illustrates the range from microscopic to macroscopic level of interest to health care professionals.
Figure 1.
Multi-scaling in health care. The figure illustrates the range from microscopic to macroscopic level of interest to health care professionals which ranges from the smallest (molecular) level to human (patient) level even up to society and global level. All the processes at all these levels work as complex (adaptive) systems.
The world has recently been confronted with the perfect example in this: the COVID-19 pandemic is a clear, noticeable, and sensible example of a complex adaptive system. A small incident at the end of 2019, where the coronavirus SARS-CoV-2 infected the first human somewhere on the globe, became a worldwide problem within only a few months. This example distinctly shows the nonlinearity of the system response and clearly demonstrates another characteristic of complexity: multi-scaling. Initially, the virus started evolving at its own (cellular) micro-level, then exploited a human body at macro-level, and the infections cascaded to disrupt a much larger system, the society, even beyond health care, including aviation and the whole global economy.
We have already established that the burn injury affects a patient as a complex system at multiple levels. So, it is time to have a closer look to provide examples from different perspectives:
- Clinical perspective on interventional strategies which would arise from treating burn care as a complex system, to improve medical decision-making and applied clinical research. It is also relevant to consider the organizational (meta-)perspective: the structure and dynamics of the burn care team that work in a complex system of hospital organization and the general health care system.
- The perspective of fundamental research. In this manuscript, we will take a closer look at the biological (microscopic) perspective: understanding processes at cellular and tissue levels with system biology and computational tools, which are available to model and simulate the complexities associated with burn wound healing.
COMPLEXITY IN THE PERSPECTIVE OF BURN CARE
A severe burn injury is a major life event for every patient that will affect physical, mental, and social functioning. In the acute phase, the impact of the injury and the complexity of the body’s response is illustrated by the systematic (hyper)inflammatory response, known as burn shock, which occurs within hours after injury. This is a complex condition where cytokines and other inflammatory mediators are released at the site of injury which will act on many organ systems and become systemic.8 Alongside the inflammatory mediators, stress hormones such as catecholamines and cortisones are released by the adrenal glands. A severe burn injury results in an abnormal uncontrolled distributive shock response.9,10 Microvascular changes such as increased vascular permeability and hydrostatic pressure will take place. A fluid shift occurs from intravascular to extracellular which leads to hypovolemic shock with low blood pressure and high pulse as well as edema at the same time. This will result in Inadequate oxygen delivery to organs and insufficient elimination of tissue metabolites.
From the point of view of complexity science, this systematic inflammatory response can be described as a nonlinear reaction in which a multicomponent network structure has become out of equilibrium. If a burn shock is not treated appropriately, it will have an impact on many organs and may even lead to death. By using the system biology approach, new ways to address the gap between basic scientific knowledge and therapy for sepsis can be explored.11
At skin level, on a burn wound, a burn shock may lead to burn wound progression by inadequate tissue perfusion and poor elimination of tissue metabolites.12 In other words, better shock treatment in the acute phase may lead to better scar quality in the long term in which case it will ultimately lead to a better quality of life and even a better reintegration of a patient into society.
In daily clinical practice, it is useful to be aware of the complexity of the situation. If we want to calculate and predict a priori the number of ventilation days in an intensive care unit for a 60-year-old man with 67% burned body surface and inhalation injury, we will most likely arrive at an inaccurate estimate. Why is it so difficult to predict accurately? Firstly, because countless numbers of other measurable and immeasurable relevant parameters also influence the disease process, and secondly, because the medical team is constantly acting on the changing parameters. And that is exactly what a multidisciplinary team at a burn center must do every day, where such complex situations must be constantly dealt with. Why is it then that the concept of complexity science is not recognized and embraced widely? This can be explained, at least in part, by the dated organizational foundations of hospitals that have functioned well in the past when health care was less complex. Modern, often technical, and ICT-oriented companies do not have this inhibiting lead from the past. In the technological world, startups are finding their own way to new organizational structures where the employees have more autonomy, there is a higher adaptability and higher efficiency. They make the networking and complexity concepts work for them and if they are successful and want to grow, they can adapt and expand. Therefore, the modern hospital systems should adapt and organize themselves to handle such complexities both at the clinical and organizational levels.13,14 The value-based health care approach is therefore interesting as it favors to center multidisciplinary care around one medical condition and enables personalized care.15 Complex burn care is ideally suited for this approach.
In the long term, the impact of the thermal injury is illustrated by the physical, mental, and social aspects during rehabilitation. Reintegration into society and a quality of life comparable to the population without burns are the highest possible long-term goals of our treatment. It is already obvious that the patient’s recovery path to this goal cannot be explained from linear causal models. We know, for example, that there is no single factor that is consistently predictive of quality of life after a burn accident apart from gender.16 Although the quality of life after burns is affected by the severity of burns and the psychological response to the trauma.17
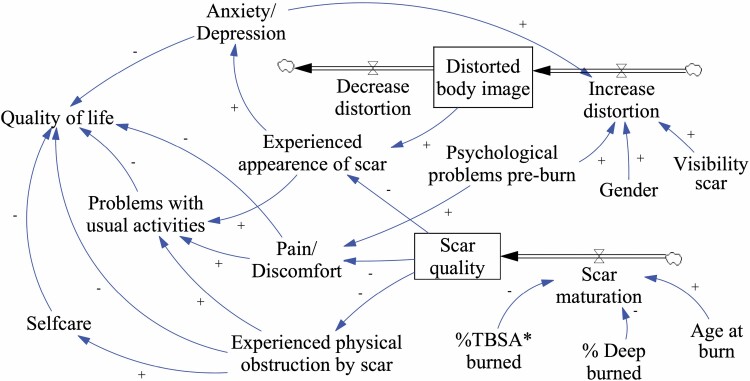
The eventual recovery of the patient might be explained by complex interactions between etiological, systems biology (how does your body adapt after burns), biomedical, health system, treatment, psychological, social, environmental, and behavioral factors. Interesting is the important role of coping self-efficacy in the recovery from traumatic stress following burn injuries.18 A preliminary model by our group showed the complexity that a burn wound entails for the patient which is summarized in Figure 2.
Figure 2.
Model of factors and interactions for recovery of a burn patient. Stock and flow diagram representing the system of outcome after burn injury in perspective of the patient. The diagram is based on a causal loop diagram.
Decision-support models and interactive computer-based systems may help with making decisions, utilizing available patient data and clinical knowledge. For example, by mapping essential nodes/ variables of an individual patient, a prediction can be made of recovery over time, and how much, where, and what support is needed for that recovery. This approach has also been advocated in the psychological sciences.19,20
If we want to get a better picture of whether and how the quality of the care provided from the patient’s point of view influences the long-term patient-relevant outcome (ie, value-based health care), complexity science may provide us with new insights and a cross-chain way of looking and acting. The patient, their health care environment, and society are complex systems, and the care provided in a burn center is a variable in relation to many others. For the benefit of the patient, it is therefore also relevant to collaborate with systems outside of a burn center, such as employers, social security systems, mental health care may be needed to achieve the best possible outcome for each patient.
Severe burn injuries have to be treated multidisciplinary, and physical, psychological, and social aspects have to be taken into account from the beginning of the treatment.21 The pursuit of providing the most effective, personalized care for the individual patient while taking all these aspects into account is a major challenge for burn care teams. Worldwide, many different treatments are used in burn care for many different situations, and it is hardly known which treatment is superior to another for which indication.
In general, teams mostly stick to their handling of choices based on experience gained in their burn center. Having experience with a product is a good thing, but it makes implementing new, potentially promising treatments difficult because there is always an experience lag. For each new treatment, a learning curve is inevitable, and this curve will create some barriers to implementation.
To create more consistency in treatments, national and international organizations have developed and implemented evidence-based guidelines to aid in all sorts of medical decision-making. Various international guidelines have now also become available for burn care.22,23
Although guidelines have been developed with good intentions, it can be said a priori that their role in burn care is limited. In fact, care must be taken not to over-apply the guidelines for complex burns. Why can we say this so confidently?
The clinical reality in a burn center is mostly too complex to be compressed into a guideline. When developing guidelines, the clinical situation is often simplified to a kind of linear causality, which often leads to overly simple decision-making processes. The evidence for the guideline comes from artificially controlled research that does not fit the realities of practice.24 There is a growing number of treatment options, and more and more patients have one or more multifactorial chronic diseases. This makes doctors and patients increasingly uncertain about the choices they make in the field of diagnostics and treatment.25,26
To anticipate the increasing complexity, burn centers should collaborate more intensively and work as a node in the network so that data and knowledge can be shared. Now some countries have a national outcome registry but ultimately and ideally this should become an international network.27 By using such (inter)national outcome registers in combination with value-based health care, it is possible to establish the value of care for patients at group level, but also to tailor treatment to each individual need. A plan-do-check-act cycle at patient level would enable to adjust and optimize the aftercare of each patient and at cohort level for analysis.
Organizational Perspective of Burn Care Team and Complexity
The work in burn centers worldwide is performed by multidisciplinary teams nowadays. This is a truly significant progress because burn patients became too complex to be treated effectively by a single specialist.21 Therefore, it has been suggested to organize burn care teams as complex adaptive systems.28 A plea has been made to evolve toward a nuanced system thinking where there is a continuous learning situation with stronger feedback loops and where system behavior can also be unbalanced, creating momentum for change.29
More frequently, the term “interdisciplinary” has been used instead of “multidisciplinary,” probably because it places more emphasis on the necessary interaction between team members (this might be considered a tautology). In line with complexity leadership, we embrace the term “metadisciplinary,” whereby each team member has their responsibility and will act based on their expertise, but he/she is also able to think for the entire group and other team members. It makes the team adaptable and able to respond well to new situations. Although it is more efficient to adapt strongly to real-time changes, the natural tendency of people faced with complexity is still to respond hierarchically and manage change from above.30 Health care itself is intrinsically dynamic, but it often appears to be at a stable state, because of deep-seated behaviors, cultures, and politics that tend to cause inertia.31 Institutions that focus more on complexity leadership build more adaptability in their systems and enable adaptive responses and emergence.
The role of new technological developments will certainly also play a major role in the changes in health care in the future. The COVID-19 pandemic demonstrated this well: forced by all restrictions, technologies for video calling and online teaching are being implemented at high speed. This brings about a crucial change in the way health care is organized. “Never let a good crisis go to waste” is a saying of Winston Churchill in the mid-1940s and fits perfectly into the current situation. Other technologies for monitoring parameters of the patient at the ICU or nowadays even at home also are being implemented.
Complexity is also a useful framework for optimizing safety and disaster management from a medical perspective.32 It is useful to look at developments in aviation where complexity science and disaster management are already more commonplace. The reason for this is that a disaster in aviation has much more impact. Many people die in a plane crash, including the flight crew. This is an important difference between aviation and health care because in health care there is no risk of a (near) fatality for professionals. In that respect, the COVID-19 pandemic is, again, exception to the rule because health workers are also at risk. The many disasters and fatalities from the past provided an intrinsic motivation in aviation to deal with safety and disaster management in a different way. At first, it was assumed that the pilot was mostly responsible for a crash. But disaster research showed that the pilot’s actions were only part of the bigger picture, and there were many factors that contributed to a tragic accident. In other words, the complexity of a disaster is better valued, so that the essence of the problem is better understood. An important conclusion was that accidents cannot just be explained by an error of the pilot, this way of thinking is far too simple. A paradigm shift followed and lead to more restorative questions to ask “how did it happen?” and “what are the needs of the persons involved?” instead of “who did it?” 33 The evaluation of the plane crashes played an important catalytic role toward just culture in aviation. Just culture is intended to address the anxiety about blame-free approaches on the one hand, and concerns about people’s willingness to continue reporting safety-related matters on the other hand.33
Medical situations are usually much more complex than in aviation. Health care can use the lessons learned in aviation and emulate aviation in its resourcing of staff who specialize in human factors and related psychological aspects of patient safety and staff well-being.34
COMPLEXITY IN THE PERSPECTIVE OF FUNDAMENTAL RESEARCH
Significant advances have been made in recent years in preclinical burn wound research, for example, investigating cellular and molecular processes responsible for burn wound healing and scarring.35–37 However, knowledge culminated from traditional preclinical studies alone, which are normally focused on just a small part of the entire mechanism, has limited the ability to sufficiently understand the underlying mechanism to predict system behavior.
Traditionally, biological systems were studied reductionistically, by taking them apart and collecting knowledge about the small subsystems. For instance, one of the main focuses has been the role of the tumor growth factor (TGF)-β in both wound healing and scar formation. Three isoforms were found, that is, TGF-β1, TGF-β2, and TGF-β3 with overlapping functions. Initially, it was suggested that TGF-β1 was responsible for fibrotic scarring, whereas TGF-β3 was related to scarless wound healing (seen in fetal wounds). However, the reality appears to be far more complex, and it is unlikely that simply altering the ratio of TGF-β isoforms will lead to scarless wound healing.38 This is because a burn wound is a complex systemic phenomenon at multiple levels. When a variant or pathway of a factor is discovered that could play a role in burn wound healing, a new subvariant/subpathway appears to be lying underneath, and this discovery process goes on and on. Of course, data generated from studies focusing on a part of the system, investigating subsystems, are very important. However, to integrate small parts into a larger whole, whereby all kinds of related biological facts are combined in a model to better understand the complexity of the entire biological system of burn wound healing, the systems biology approach is crucial.
To understand processes in the body’s response to a burn injury at a preclinical level, the systems biology approach can be employed. This approach uses preexisting data from the literature combined with newly generated data from laboratory experiments to develop representative models (eg, dynamic computational models) for processes involved in burn wound healing (eg, the postburn immune response).39,40
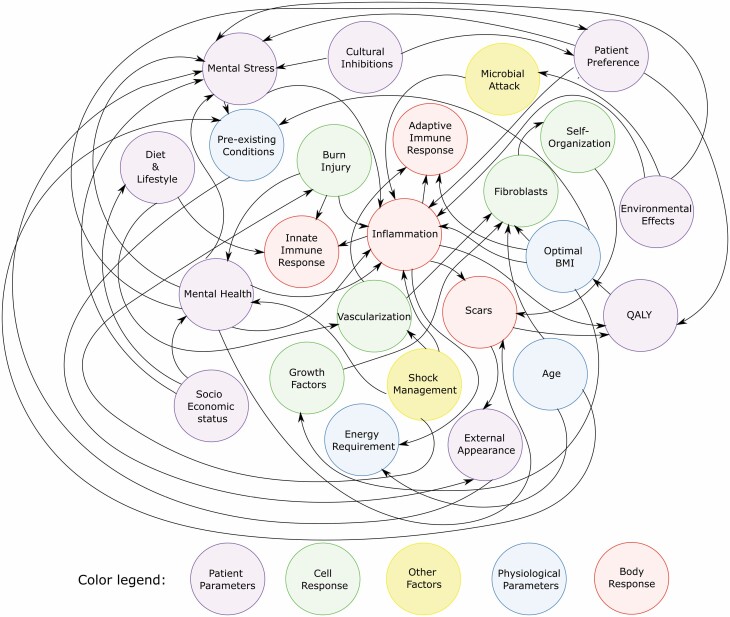
Using computational modeling, many small puzzle pieces of data about burn wound healing can be investigated to reveal and visualize hidden patterns and connections, which cannot be inferred directly by the human brain, which can result in new insights and better understanding. This will be described in the next section: “Perspective on the computational tools.” For this, it is crucial that there is a good interaction between preclinical burn wound research (eg, tissue engineering and organogenesis) and systems biology/complexity science in order to get more insight into the complexity of burn wound healing by investigating the “communication” and interactions between the cells and molecules within the burn wound (as shown in Figure 3).
Figure 3.
Model of factors and interactions for burn wound healing dynamics. Causal loop diagram displaying the complexity of burn wound healing by investigating the interactions between the cells and molecules within the burn wound.
Computational Tools to Model Burn Wound Complexity
Numerical modeling and simulations have been used in various fields to understand and predict the dynamics of complex systems.41–44 The scale or scales associated with the system should be considered before deciding on which computational tools to employ for the modeling process.
Burn wound healing is a multiscale process. The temporal scales (ie, time-related scales) involve microseconds for cytokines and other factors secretion, seconds for solute diffusion, minutes for immune cell chemotaxis, hours for blood clotting and necrosis, days for vascularization, and weeks for scar formation and months up to years for systemic inflammation reduction. Similarly, the spatial scales (ie, scales related to space) involve, proteins and factors at nanometer level, cells at micrometer level, and organs at decimeter level. A single computational tool may not suffice to handle these multiscale processes and interactions. However, an ensemble of numerical methods may be coupled at various scales to decode the underlying phenomena driving the healing process.
Computational models have already been developed for fibroblast migration and collagen deposition during wound repair,45 wound contraction,46–48 and hypertrophic scar formation.49,50 Moreover, hypotheses and several “what if” scenarios can be tested, so that preclinical experiments can be adapted accordingly.51–54 Therefore, it is crucial to develop preclinical in vitro models for burn wound healing also, for new data generation, validation, and improvement of computational models. In the past years, human physiologically relevant tissue-engineered skin models have been developed for wound healing advanced therapy medicinal products (ATMPs) and in vitro assays.55–58 These models can be used for validation and improvement of computational models and to collect new preclinical data. However, skin substitutes do not contain all skin cell types and therefore do not fully represent original skin physiology. A few of such major computational methods are discussed in the forthcoming sections.
Network Analysis
Most proteins and factors secreted by cells are interdependent for expression, and their actions are dependent on the actions and concentration levels of one another. One efficient way to handle such intricacies in numerical modeling is through network analysis models. In these models, the factors (proteins) are treated as nodes that are connected to other nodes through paths. These paths indicate an interaction between the factors or the cells expressing the factors. The expression levels can be quantified using weighted paths, where the probability of a factor stimulating another factor depends on the direction and weight of the path.59,60 Thereby, a snapshot of the network at any instant represents the state of the system and its associated paths. Such a network construction will enable the probing of systems to check for network robustness or resilience. One example would be varying the weight of path between mast cells and histamine to evaluate its impact on the initial response to wound-site inflammation. Similarly, network analysis can enable the identification of suitable target candidates for intervention, through the identification of crucial nodes in the network which may help reduce inflammation for better healing process or inhibiting shock.
System Dynamics Models
Complex systems are dynamical systems that vary based on the state changes and path changes occurring in the system. Since the process involved in these systems are functions of multiple actors, the system can be modeled using a set of mathematical equations. In a wound immune response model, the actors would encompass the immune cells, epithelial cells, and tissue at the wound site. The cells express cytokines and chemokines to attract other cells to the wound site. For instance, damaged skin cells secrete damage-associated molecular patterns (DAMPs) at wound site, skin-resident (immune) cells become activated and secrete inflammatory factors which recruit neutrophils, the neutrophils secrete pro-inflammatory cytokines, which attract macrophages to the tissue, macrophages get activated in tissue and further secrete cytokines attracting more neutrophils. This cascade process can be defined using (partial) differential equations, which describe the space-time-dependent concentrations of the pro- and anti-inflammatory cytokines, neutrophils, and macrophages. Such methods have already proven to be effective in modeling the immune response in cardiovascular patients. Most of the data used in such models are collected and analyzed as part of the existing clinical workflow.61 Even in conditions where the development of such quantitative models is not feasible, causal loop diagrams can come in useful. In short, causal loop diagrams describe positive and negative associations between the factors involved in the system dynamics. Thus, they can offer a way to qualitatively analyze the dynamics involved. It is important to notice that the system dynamics models are temporal scale-dependent, and a single set of equations may model for only one timescale. To overcome this timescale limitation, multiple sets of equations operating at different timescales may be coupled. For example, cytokine secretion can be modeled with equations operating in microseconds, and recruitment of individual macrophages can be modeled with equations in minute scale. From a mathematical perspective, this large difference in timescales results into a stiff system, which poses many numerical challenges. The cytokine secretion model can be solved until the concentration of cytokines reach a steady state. This concentration can be assumed to be the concentration after 1-minute interval, during which period there is no significant change in macrophage recruitment. Thus, the output from secretion model can be used as an input for macrophage recruitment model at every 1-minute interval. The resultant model is a time-coupled multiscale model.
Agent-Based Models
A primary limitation of the network analysis and system dynamics models is the absence of spatial information in the models. Spatial data play a critical role in the determination of the outcomes of burn wound healing process. The presence of vasculature, proximity of blood vessels, size, and geometry of wounds all play a critical role guiding the dynamics of the healing and scar formation process. Agent-based models act as a powerful tool to model the location-based actions of the actors involved in the system.62,63 In these models, cells can be considered as agents which are free to move around in a fixed discrete simulation domain. In the case of scar formation modeling, these agents may be fibroblasts and granulocytes exhibiting chemotaxis to various sites in a wound and secreting collagen for the repair process. The spatial output generated from this model would provide greater insight into spatial patterns arising from the scar formation process. The agent-based models can be further combined with multiscale system dynamics models to explore the entire dynamics involved in burn wound process from immune response to vasculature development to scar formation.64 Furthermore, these models can be further developed to define effective interventional strategies. The ability to rapidly assess the efficacy of interventional strategies for burn wounds is an urgent need. Preclinical in vitro models available in the literature are limited in their ability to define the temporal effects of interventions/therapies on simultaneous multicellular interactions. Integrating biological and computational modeling approaches can overcome this limitation. Patients’ specific information can be introduced into the computational model to predict the effect of interventions (eg, topical treatments; surgical interventions) on state evolution.
Computation Fluid Dynamics and Solute Dynamics
In addition to handling biological cells and factors, it is also necessary to simulate the physics/biophysics enabling such cells and factors to interact within the body.65,66 These enabling interactions could be simple diffusion of the secreted factors within the tissue or more complex blood flow transport of factors from various organs to the diseased tissues. There are various sophisticated models available in the literature to model and predict the outcome of such transport processes at different spatial and temporal scales. For instance, by simulation of the blood flow, one can investigate drug uptake pharmacodynamics and postburn thrombosis.
CONCLUDING REMARKS
With this perspective paper, we have set out the concept of complexity science and have given examples from the preclinical, clinical, and organizational perspectives in burn care. It has been shown that complex adaptive systems are not well known and understood, yet they are ubiquitous.
It is a utopia to obtain full grip on complex adaptive systems. Once we accept that unpredictability and uncertainty are part of our world, it will be much easier to deal with and embrace it. This certainly applies to burn care because of its complex and multidisciplinary nature. The complexity science perspective will lead to a deeper, more holistic, understanding because the whole is more than the sum of its parts. The emergence of the multiple interactions between the parts was missing in many equations so far in general but also in burn care. In this perspective, complexity science might be an excellent guide for the future of burn care.
ACKNOWLEDGEMENTS
The authors sincerely acknowledge the contribution of Jeroen G. N. van de Pauw Kraan, Titus R. Radstake, Ariette van Reekum, MD, PhD, Prof. Marcel G. M. Olde Rikkert, MD, PhD, Prof. Marinus de Kleuver, MD, PhD, Lieke C. van Zuijlen, and Rosalyn Rus during the realization of this manuscript.
Conflict of Interest: None.
Contributor Information
Paul P M van Zuijlen, Burn Center, Red Cross Hospital, Beverwijk, the Netherlands; Department of Plastic and Reconstructive Surgery, Red Cross Hospital, Beverwijk, the Netherlands; Department of Plastic Reconstructive and Hand Surgery, Amsterdam Movement Sciences (AMS) Institute, Amsterdam UMC, Location VUmc, the Netherlands; Paediatric Surgical Centre, Emma Children’s Hospital, Amsterdam UMC, location AMC, the Netherlands.
Halil Ibrahim Korkmaz, Burn Center, Red Cross Hospital, Beverwijk, the Netherlands; Department of Plastic Reconstructive and Hand Surgery, Amsterdam Movement Sciences (AMS) Institute, Amsterdam UMC, Location VUmc, the Netherlands; Department of Molecular Cell Biology and Immunology, Amsterdam UMC, Location VUmc, the Netherlands; Association of Dutch Burn Centres (ADBC), Beverwijk, the Netherlands.
Vivek M Sheraton, Institute for Advanced Study, University of Amsterdam, the Netherlands.
Tsjitske M Haanstra, National Health Care Institute (Zorginstituut, Nederland), Diemen, the Netherlands.
Anouk Pijpe, Burn Center, Red Cross Hospital, Beverwijk, the Netherlands.
Annebeth de Vries, Burn Center, Red Cross Hospital, Beverwijk, the Netherlands; Paediatric Surgical Centre, Emma Children’s Hospital, Amsterdam UMC, location AMC, the Netherlands; Department of Surgery, Red Cross Hospital, Beverwijk, the Netherlands.
Cornelis H van der Vlies, Burn Centre and Department of Surgery, Maasstad Ziekenhuis, Rotterdam, the Netherlands; Trauma Research Unit, Department of Surgery, Erasmus MC, University Medical Centre Rotterdam, the Netherlands.
Eelke Bosma, Burn Centre and Department of Surgery, Martini Ziekenhuis, Groningen, the Netherlands.
Evelien de Jong, Burn Center, Red Cross Hospital, Beverwijk, the Netherlands; Intensive Care Unit, Red Cross Hospital, Beverwijk, the Netherlands.
Esther Middelkoop, Burn Center, Red Cross Hospital, Beverwijk, the Netherlands; Department of Plastic Reconstructive and Hand Surgery, Amsterdam Movement Sciences (AMS) Institute, Amsterdam UMC, Location VUmc, the Netherlands; Association of Dutch Burn Centres (ADBC), Beverwijk, the Netherlands.
Fred J Vermolen, Delft Institute of Applied Mathematics, Delft University of Technology, the Netherlands; Computational Mathematics, Hasselt University, Diepenbeek, Belgium.
Peter M A Sloot, Institute for Advanced Study, University of Amsterdam, the Netherlands; Complexity Institute, Nanyang Technological University, Singapore, Singapore; ITMO University, Saint Petersburg, Russian Federation.
REFERENCES
- 1. Williams FN, Herndon DN, Hawkins HKet al. . The leading causes of death after burn injury in a single pediatric burn center. Crit Care 2009;13:R183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rani M, Schwacha MG. Aging and the pathogenic response to burn. Aging Dis 2012;3:171–80. [PMC free article] [PubMed] [Google Scholar]
- 3. Siegenfeld AF, Bar-Yam Y. An introduction to complex systems science and its applications. Complexity 2020;2020:16105872. [Google Scholar]
- 4. Jayasinghe S. Conceptualising population health: from mechanistic thinking to complexity science. Emerg Themes Epidemiol 2011;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Holland J. Complex adaptive systems. Daedalus 1992;121:17–30. A New Era in Computation (Winter, 1992). Published by: The MIT Press on behalf of American Academy of Arts & Sciences. http://research.acer.edu.au/cgi/viewcontent.cgi?article=1000&context=pisa. [Google Scholar]
- 6. Mitchell M, ProQuest (Firm). Complexity: a guided tour. Vol. XVI. Oxford (UK)/New York (NY): Oxford University Press; 2009. 349 p. [Google Scholar]
- 7. Gomersall T. Complex adaptive systems: a new approach for understanding health practices. Health Psychol Rev 2018;12:405–18. [DOI] [PubMed] [Google Scholar]
- 8. Guilabert P, Usua G, Martin Net al. . Fluid resuscitation management in patients with burns: update. Br J Anaesth 2016;117:284–96. [DOI] [PubMed] [Google Scholar]
- 9. Jeschke MG, van Baar ME, Choudhry MAet al. . Burn injury. Nat Rev Dis Primers 2020;6:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nielson CB, Duethman NC, Howard JMet al. . Burns: pathophysiology of systemic complications and current management. J Burn Care Res 2017;38:e469–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vodovotz Y, Csete M, Bartels Jet al. . Translational systems biology of inflammation. PLoS Comput Biol 2008;4:e1000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Singh V, Devgan L, Bhat Set al. . The pathogenesis of burn wound conversion. Ann Plast Surg 2007;59:109–15. [DOI] [PubMed] [Google Scholar]
- 13. Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care 2003;12:458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. West BJ, Clancy TR. Flash crashes, bursts, and black swans: parallels between financial markets and healthcare systems. J Nurs Adm 2010;40:456–9. [DOI] [PubMed] [Google Scholar]
- 15. Porter ME, Teisberg EO.. Redefining health care: creating value-based competition on results. Boston, (MA): Harvard Business School Press; 2006. [Google Scholar]
- 16. Legemate CM, Spronk I, Mokkink LBet al. . Evaluation of measurement properties of health-related quality of life instruments for burns: a systematic review. J Trauma Acute Care Surg 2020;88:555–71. [DOI] [PubMed] [Google Scholar]
- 17. Spronk I, Legemate CM, Dokter Jet al. . Predictors of health-related quality of life after burn injuries: a systematic review. Crit Care 2018;22:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bosmans MW, Hofland HW, De Jong AEet al. . Coping with burns: the role of coping self-efficacy in the recovery from traumatic stress following burn injuries. J Behav Med 2015;38:642–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Isvoranu A-M, Abdin E, Chong SAet al. . Extended network analysis: from psychopathology to chronic illness. BMC Psychiatry 2021;21:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Isvoranu AM, Borsboom D, van Os Jet al. . A network approach to environmental impact in psychotic disorder: brief theoretical framework. Schizophr Bull 2016;42:870–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Al-Mousawi AM, Mecott-Rivera GA, Jeschke MGet al. . Burn teams and burn centers: the importance of a comprehensive team approach to burn care. Clin Plast Surg 2009;36:547–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. ISBI Practice Guidelines Committee; Steering Subcommittee; Advisory Subcommittee. ISBI practice guidelines for burn care. Burns 2016;42:953–1021. [DOI] [PubMed] [Google Scholar]
- 23. Romanowski KS, Carson J, Pape Ket al. . American Burn Association guidelines on the management of acute pain in the adult burn patient: a review of the literature, a compilation of expert opinion and next steps. J Burn Care Res 2020;41:1152–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Green LW. Public health asks of systems science: to advance our evidence-based practice, can you help us get more practice-based evidence? Am J Public Health 2006;96:406–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stolper E, Van Royen P, Jack Eet al. . Embracing complexity with systems thinking in general practitioners’ clinical reasoning helps handling uncertainty. J Eval Clin Pract 2021;27:1175–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Olde Rikkert MGM, van Zuijlen PPM, de Kleuver Met al. . [Complexity of disease; a modern view in times of ageing populations and multimorbidity]. Ned Tijdschr Geneeskd 2019;163:D3970. [PubMed] [Google Scholar]
- 27. Haanstra TM, van Baar ME, van Loey NEEet al. . The Burn Centres Outcome Registry The Netherlands (BORN): development and first experiences. Wound Repair Regen 2018;26:A6. [Google Scholar]
- 28. Karam E, Levesque MC, Jacquemin Get al. . Building a multidisciplinary team for burn treatment—lessons learned from the Montreal tendon transfer experience. Ann Burns Fire Disasters 2014;27:3–7. [PMC free article] [PubMed] [Google Scholar]
- 29. Braithwaite J. Changing how we think about healthcare improvement. BMJ 2018;361:k2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Uhl-Bien M, Arena M. Complexity leadership: enabling people and organizations for adaptability. Organ Dyn 2017;46:9–20. [Google Scholar]
- 31. Coiera E. Social networks, social media, and social diseases. BMJ 2013;346:f3007. [DOI] [PubMed] [Google Scholar]
- 32. O’Sullivan TL, Kuziemsky CE, Toal-Sullivan Det al. . Unraveling the complexities of disaster management: a framework for critical social infrastructure to promote population health and resilience. Soc Sci Med 2013;93:238–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dekker SWA, Breakey H. “Just culture:” improving safety by achieving substantive, procedural and restorative justice. Saf Sci 2016;85:187–93. [Google Scholar]
- 34. Kapur N, Parand A, Soukup Tet al. . Aviation and healthcare: a comparative review with implications for patient safety. JRSM Open 2016;7:2054270415616548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Evers LH, Bhavsar D, Mailander P. The biology of burn injury. Exp Dermatol 2010;19:777–83. [DOI] [PubMed] [Google Scholar]
- 36. Korkmaz HI, Krijnen PAJ, Ulrich MMWet al. . The role of complement in the acute phase response after burns. Burns 2017;43:1390–99. [DOI] [PubMed] [Google Scholar]
- 37. Heideman M, Bengtsson A. The immunologic response to thermal injury. World J Surg 1992;16:53–6. [DOI] [PubMed] [Google Scholar]
- 38. Penn JW, Grobbelaar AO, Rolfe KJ. The role of the TGF-β family in wound healing, burns and scarring: a review. Int J Burns Trauma 2012;2:18–28. [PMC free article] [PubMed] [Google Scholar]
- 39. Kitano H. Systems biology: a brief overview. Science 2002;295:1662–4. [DOI] [PubMed] [Google Scholar]
- 40. Hazeldine J, Hampson P, Lord JM. The diagnostic and prognostic value of systems biology research in major traumatic and thermal injury: a review. Burns Trauma 2016;4:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Buganza Tepole A, Kuhl E. Computational modeling of chemo-bio-mechanical coupling: a systems-biology approach toward wound healing. Comput Methods Biomech Biomed Engin 2016;19:13–30. [DOI] [PubMed] [Google Scholar]
- 42. Martins-Green M, Vodovotz Y, Liu P. Systems biology applied to wound healing. Wound Repair Regen 2010;18:1–2. [DOI] [PubMed] [Google Scholar]
- 43. Narang V, Decraene J, Wong SYet al. . Systems immunology: a survey of modeling formalisms, applications and simulation tools. Immunol Res 2012;53:251–65. [DOI] [PubMed] [Google Scholar]
- 44. Bookholt FD, Monsuur HN, Gibbs Set al. . Mathematical modelling of angiogenesis using continuous cell-based models. Biomech Model Mechanobiol 2016;15:1577–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. McDougall S, Dallon J, Sherratt Jet al. . Fibroblast migration and collagen deposition during dermal wound healing: mathematical modelling and clinical implications. Philos Trans A Math Phys Eng Sci 2006;364:1385–405. [DOI] [PubMed] [Google Scholar]
- 46. Koppenol DC, Vermolen FJ, Koppenol-Gonzalez GVet al. . A mathematical model for the simulation of the contraction of burns. J Math Biol 2017;75:1–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Egberts G, Vermolen F, van Zuijlen P. Sensitivity and feasibility of a one-dimensional morphoelastic model for post-burn contraction. Biomech Model Mechanobiol 2021;20:2147–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Egberts G, Vermolen F, van Zuijlen P. Stability of a one-dimensional morphoelastic model for post-burn contraction. J Math Biol 2021;83:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Koppenol DC, Vermolen FJ, Niessen FBet al. . A mathematical model for the simulation of the formation and the subsequent regression of hypertrophic scar tissue after dermal wounding. Biomech Model Mechanobiol 2017;16:15–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ogawa R. The most current algorithms for the treatment and prevention of hypertrophic scars and keloids. Plast Reconstr Surg 2010;125:557–68. [DOI] [PubMed] [Google Scholar]
- 51. Sayama H. Introduction to the modeling and analysis of complex systems. New York (NY): Open SUNY Textbooks, Milne Library, State University of New York at Geneseo; 2015. [Google Scholar]
- 52. Ji Z, Yan K, Li Wet al. . Mathematical and computational modeling in complex biological systems. Biomed Res Int 2017;2017:5958321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. MacLeod M, Nersessian NJ. Modeling complexity: cognitive constraints and computational model-building in integrative systems biology. Hist Philos Life Sci 2018;40:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Soheilypour M, Mofrad MRK. Agent-based modeling in molecular systems biology. Bioessays 2018;40:1800020. [DOI] [PubMed] [Google Scholar]
- 55. Kazem S, Linssen EC, Gibbs S. Skin metabolism phase I and phase II enzymes in native and reconstructed human skin: a short review. Drug Discov Today 2019;24:1899–910. [DOI] [PubMed] [Google Scholar]
- 56. van den Broek LJ, Niessen FB, Scheper RJet al. . Development, validation and testing of a human tissue engineered hypertrophic scar model. ALTEX 2012;29:389–402. [DOI] [PubMed] [Google Scholar]
- 57. Bell E, Parenteau N, Gay Ret al. . The living skin equivalent: its manufacture, its organotypic properties and its responses to irritants. Toxicol In Vitro 1991;5:591–6. [DOI] [PubMed] [Google Scholar]
- 58. Kuroyanagi Y, Kenmochi M, Ishihara Set al. . A cultured skin substitute composed of fibroblasts and keratinocytes with a collagen matrix: preliminary results of clinical trials. Ann Plast Surg 1993;31:340–9; discussion 349. [DOI] [PubMed] [Google Scholar]
- 59. Horvath S. Weighted network analysis: applications in genomics and systems biology. 1st ed.New York, NY: Springer; 2011. 421 p. [Google Scholar]
- 60. Faust K, Dupont P, Callut Jet al. . Pathway discovery in metabolic networks by subgraph extraction. Bioinformatics 2010;26:1211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Presbitero A, Mancini E, Brands Ret al. . Supplemented alkaline phosphatase supports the immune response in patients undergoing cardiac surgery: clinical and computational evidence. Front Immunol 2018;9:2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Railsback SF, Grimm V.. Agent-based and individual-based modeling: a practical introduction. Princeton, NJ: Princeton University Press; 2019. [Google Scholar]
- 63. An G, Mi Q, Dutta-Moscato Jet al. . Agent-based models in translational systems biology. Wiley Interdiscip Rev Syst Biol Med 2009;1:159–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Peng Q, Vermolen F. Agent-based modelling and parameter sensitivity analysis with a finite-element method for skin contraction. Biomech Model Mechanobiol 2020;19:2525–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kaura P, Mishra T, Verma Net al. . Effects of combined chemotherapeutic drugs on the growth and survival of cancerous tumours—an in-silico study. J Comput Sci 2021;54:101421. [Google Scholar]
- 66. Croll TI, Gentz S, Mueller Ket al. . Modelling oxygen diffusion and cell growth in a porous, vascularising scaffold for soft tissue engineering applications. Chem Eng Sci 2005;60:4924–34. [Google Scholar]
- 67. Solé R,, Elena SF. Viruses as complex adaptive systems. Princeton University Press; 2018. [Google Scholar]
- 68. Goldstein J. . Emergence as a construct: history and issues. Emergence 1999;1:49–72. [Google Scholar]
- 69. Scheffer M. . Complex systems: foreseeing tipping points. Nature 2010;467:411–412. [DOI] [PubMed] [Google Scholar]
- 70. An G, Nieman G, Vodovotz Y. . Toward computational identification of multiscale “tipping points” in acute inflammation and multiple organ failure. Ann Biomed Eng 2012;40:2414–24. [DOI] [PubMed] [Google Scholar]
- 71. Bar-yam Y. . Dynamics of complex systems. 1st ed. CRC Press; 2019.https://www.perlego.com/book/1471976/dynamics-of-complex-systems-pdf. [Google Scholar]