Abstract
Background & objectives:
The delay in communicating the results to tuberculosis (TB) patients leads to increased rates of initial loss to follow up of treatment. The gap in communication among healthcare providers requires application of new tools that will address the challenges. Mobile phone technologies could be a useful tool in this context for the delivery of information. The objective was thus to evaluate communication by mobile applications such as the WhatsApp Messenger to decrease initial loss to follow up after initial treatment for TB.
Methods:
Indian Council of Medical Research-National Institute for Research in Tuberculosis, Chennai, India undertook a community prevalence survey to find the burden of TB. During this survey, mobile phone-based technology (WhatsApp messenger) was employed as an intervention among the healthcare providers and researchers involved for communicating. This was further evaluated for its usefulness by examining the initial loss to follow up and patients initiated on treatment.
Results:
The study covered four blocks of Thiruvallur district of Tamil Nadu, South India, namely Kadambathur, Poondi, Thiruvalangadu and Periyapalayam. The survey population was around 20,000 from each block, and the average patients diagnosed by community TB prevalence survey were 30 patients from each block. Among the patients diagnosed through this survey, in the first block, only 55 per cent were initiated on treatment; subsequently, with the intervention, the initial loss to follow up was significantly reduced from 45 to zero per cent.
Interpretation & conclusions:
After integrating of WhatsApp messenger application for communication among healthcare providers and researchers, the initial loss to follow up among patients being treated for TB was significantly decreased.
Keywords: Active case finding, loss to follow up, mobile phone technology, TB, WhatsApp
A systematic review and meta-analysis on the tuberculosis (TB) cascade of care in India’s public sector reported that only 53 per cent of the diagnosed TB cases were initiated on treatment1. As per the Global TB Report in 2019, the notification increased from 1.2 to 2.0 million between 2013 and 2018 (60%)2. Early and accurate diagnosis followed by prompt appropriate treatment is the cornerstone for ending TB. Patients with initial loss to follow up for treatment, i.e. patients diagnosed with microbiologically confirmed TB, but have no record of having started treatment, remain an infectious risk for close contacts and their community. Initial loss to follow up has also been reported as one of the ‘unresolved issues’ in TB control3,4 and is a vital gap in the treatment cascade which could enhance the transmission of TB in the community.
Indian Council of Medical Research (ICMR)-National Institute for Research in Tuberculosis (NIRT) conducted prevalence surveys to estimate the impact of TB prevalence in the present study, it was observed that there was a delay in communicating the results to the TB patients. This increased rates of initial loss to follow up. In the present study, we used communication by WhatsApp Messenger between National Tuberculosis Elimination Programme (NTEP) and community-based TB prevalence survey staff was enabled to decrease initial loss to follow up.
Material & Methods
Setting: This study was approved by the Institutional Ethics Committee of ICMR-NIRT, Chennai, India. ICMR-NIRT undertakes periodic community-based TB prevalence surveys in Thiruvallur district, Tamil Nadu. These surveys were conducted in TB units covering 100,000 population in five blocks of this rural district. All persons aged more than 15 yr were screened for chest symptoms, suggestive of TB and chest radiograph (MMR X-ray) for TB diagnosis. For those with an abnormal chest radiograph and/or chest symptoms, two sputum samples were collected and examined by fluorescent microscopy and culture for Mycobacterium tuberculosis. The diagnostic results were communicated to the programme personnel District TB Officer (DTO) and Senior Treatment Supervisor (STS) through referral slips. These patients were further followed up by NTEP.
Study design: In order to assess feasibility of the use of mobile phone-based applications such as the WhatsApp Messenger, the same was employed as an intervention in the ongoing community-based TB prevalence survey Thriuvallur rural district between April 2017 and March 2018. The sample which was estimated for prevalence survey was 84,000 population aged >15 yr. It was estimated assuming TB prevalence 255 per 100,000 population, a precision of 20 per cent, with 95 per cent confidence level, design effect of two and coverage of 90 per cent. Based on the field experience gained during the door-to-door community survey in one block, this intervention was conceptualized and subsequently implemented in the remaining four blocks, namely Perambakkam, Poondi, Thiruvalangadu and Periyapalayam. The survey population was around 20,000 from each block. All patients diagnosed by community TB prevalence survey formed the intervention population.
Intervention: The present intervention involved communication by WhatsApp Messenger to address the time delays occurring between the point of diagnosis in the TB prevalence survey and treatment initiation in NTEP. This intervention aimed to address the communication gaps between programme personnel district TB officer (DTO), senior treatment supervisor (STS) and researchers from the TB prevalence survey team. In the conventional method, the investigation results from the survey to patients and the programme personnel in the health system were communicated by referral slips (Figure).
Figure.
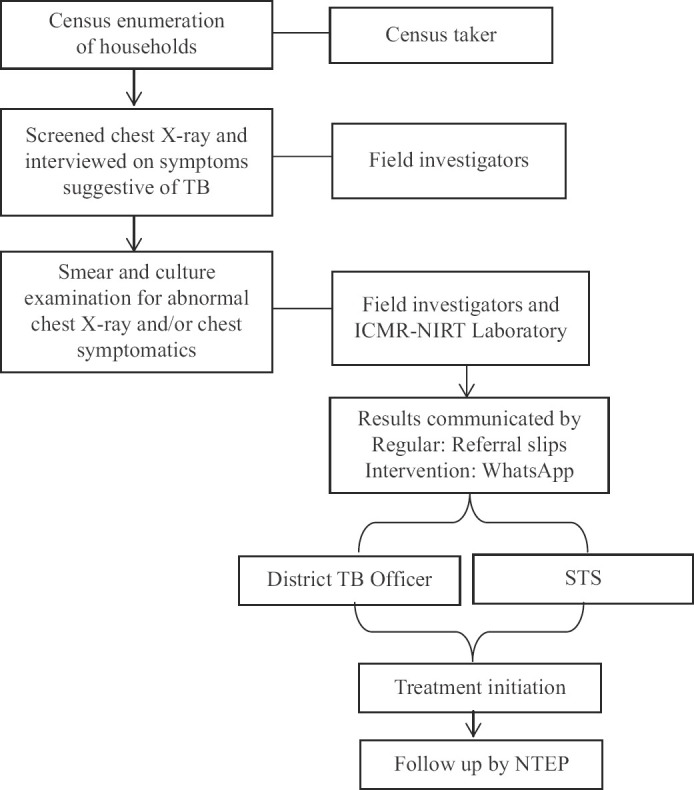
Study procedure and Intervention.
Intervention implementation: The intervention was introduced at one block initially (Perambakkam) for six months; further, based on the feedback and experiences of the study team, the intervention was extended to the second block (Poondi). Post-completion of intervention in these two blocks, third and fourth blocks were covered (Thiruvelangadu and Periyapalaym).
Data collection: All patients diagnosed through community survey were interviewed to find out the status of initiation of treatment. Treatment initiation of patients was validated by verifying with the TB treatment register.
Data analysis: Data were entered in Excel Sheet and analyzed using SPSS/PC version 20.0 (SPSS Inc., Chicago, IL, USA). Block-wise proportion of patients initiated on treatment was calculated. The trend Chi-square test was used to determine the significance of change in the number of patients whose treatment was initiated due to the intervention using mobile phone-based WhatsApp communication. A P<0.05 was considered significant.
Results and Discussion
ICMR-NIRT community TB prevalence survey (April 2017 and March 2018) diagnosed 42, 39, 30 and 38 TB patients in four blocks, namely Perambakkam, Poondi, Thiruvalangadu and Periyapalayam, respectively. In Perambakkam, of the 42 patients referred for treatment, only 23 (55%) patients were initiated on treatment under NTEP. Of the remaining 19 TB patients not initiated on treatment, four patients were untraceable, three patients died and 12 were not initiated on treatment (Table I).
Table I.
Status of tuberculosis patients diagnosed through community survey
| Name of the blocks | TB patients diagnosed by prevalence survey | TB treatment initiated under NTEP | TB treatment under private sector | TB treatment not initiated | Not traceable | Dead |
|---|---|---|---|---|---|---|
| Perambakkam | 42 | 23 | 0 | 12 | 4 | 3 |
| Poondi | 39 | 26 | 1 | 9 | 1 | 2 |
| Thiruvelangadu | 30 | 23 | 0 | 7 | 0 | 0 |
| Periyapalayam | 38 | 38 | 0 | 0 | 0 | 0 |
| Total | 149 | 110 | 1 | 28 | 5 | 5 |
TB, tuberculosis; NTEP, National Tuberculosis Elimination Programme
Due to the low proportion of patients initiated on timely treatment in study areas, the WhatsApp communication intervention was introduced. In Poondi block, after introduction of the WhatsApp-based results’ communication, of the total 39 patients diagnosed, 26 (67%) were registered for the treatment under NTEP. Of the remaining 13 TB patients, one patient was taking treatment from a private practitioner, nine were not initiated on treatment, two died and one was untraceable. Further, in Thiruvalangadu block, of the 30 patients diagnosed, 23 (77%) patients initiated the treatment under NTEP and seven were not on treatment. Over a period in Periyapalayam alone, of the total 38 patients diagnosed, all the 38 (100%) were registered for the treatment under NTEP.
This intervention was found to increase the proportion of patients registered for TB treatment under four centres of NTEP which ranged from 55 per cent in Perambakkam to 100 per cent in Periyapalayam, P<0.001 (Table II). Over a period, initial loss to follow up was reduced significantly from 45 to zero per cent from the start to the end of the survey.
Table II.
Tuberculosis patients diagnosed by community-based tuberculosis prevalence survey and initiated treatment under National Tuberculosis Elimination Programme
| Name of the blocks | TB patients diagnosed by prevalence survey (n) | TB treatment initiated under NTEP, n (%) | TB treatment not initiated under NTEP, n (%) |
|---|---|---|---|
| Perambakkam | 42 | 23 (55) | 23 (45) |
| Poondi | 39 | 26 (67) | 26 (33) |
| Thiruvelangadu | 30 | 23 (77) | 23 (23) |
| Periyapalayam | 38 | 38 (100) | 38 (0) |
| Total | 149 | 110 (74) | 110 (26) |
The key finding of this study was that a simple mobile phone-based (WhatsApp) communication intervention significantly reduced the initial loss to follow up of patients diagnosed with TB in a community survey setting in Tamil Nadu. This feasible intervention could be considered as a strategy to reduce initial loss to follow up in low-resource settings. Similarly, low-cost mobile phone-based interventions such as smartphone-enabled video-observed treatment for TB and mobile phone short message service have been used to address communication gaps in referral services, treatment adherence and effective monitoring and supervision5. In this study, for the first time, WhatsApp communication was utilized as a potential tool for health workers’ communication to address initial loss to follow up among patients with TB. The use of communication on mobile phones offers an efficient, unobtrusive and portable mode of communication for healthcare staff. The mobile phone-based technology can be implemented in any community-based TB prevalence surveys for effective functioning.
Various efforts have been made to reduce the delays in initiating treatment and reduce initial loss to follow up of TB patients. A study from Chennai found that maintaining legible and understandable hand-written documents, house number and patient contact information helped health workers to track and re-engage the initial loss to follow up TB patients in care6.
Systematic reviews on the impact of digital health technologies for improving patient care management found that digital treatment support can lead to better treatment results among diabetics9, TB patients10,11,12,13,14, people living with HIV15, improving maternal child health services16,17 and family planning services18,19. Our findings corroborate with the past evidence that utilizing mobile phone-based interventions could be cost-effective and could be an acceptable strategy for bringing in significant efficiency in programme performance.
Considering the stigma attached to TB and risks associated with disclosure of patients’ name, in our study, confidentially was maintained among NTEP staff and community prevalence survey staff.
The study was experimented only among the patients diagnosed through community-based TB prevalence survey in rural areas and may not, however, be generalizable. Furthermore, this was only a feasibility study for testing the introduction of WhatsApp Messenger and our study is limited in scope to control for confounders.
Overall, relapse and development of drug resistance and lack of communication with healthcare providers are important risk factors for loss to follow up in TB treatment. There is a clear need to develop and test affordable, innovative strategies and tools to provide timely communication among healthcare providers. Mobile phone-based technology is attractive in many low- and middle-income countries because of the high mobile phone penetration and network coverage that has occurred over the last decade. The current study provided preliminary evidence for enabling larger studies on this topic.
Acknowledgment: The authors thank the State Tuberculosis Officer, Government of Tamil Nadu, Thiruvallur DTO and other programme staff of the NTEP for their permission and support in conducting this study.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1.Subbaraman R, Nathavitharana RR, Satyanarayana S, Pai M, Thomas BE, Chadha VK, et al. The tuberculosis cascade of care in India's public sector:A systematic review and meta-analysis. PLoS Med. 2016;13:e1002149. doi: 10.1371/journal.pmed.1002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. Global tuberculosis report 2019. Geneva: WHO; 2019. [Google Scholar]
- 3.Harries AD, Rusen ID, Chiang CY, Hinderaker SG, Enarson DA. Registering initial defaulters and reporting on their treatment outcomes. Int J Tuberc Lung Dis. 2009;13:801–3. [PubMed] [Google Scholar]
- 4.Thomas BE, Subbaraman R, Sellappan S, Suresh C, Lavanya J, Lincy S, et al. Pretreatment loss to follow-up of tuberculosis patients in Chennai, India:A cohort study with implications for health systems strengthening. BMC Infect Dis. 2018;18:142. doi: 10.1186/s12879-018-3039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar AA, De Costa A, Das A, Srinivasa GA, D’Souza G, Rodrigues R. Mobile health for tuberculosis management in south India:Is video-based directly observed treatment an acceptable alternative? JMIR Mhealth Uhealth. 2019;(7):e11687. doi: 10.2196/11687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ngwatu BK, Nsengiyumva NP, Oxlade O, Mappin-Kasirer B, Nguyen NL, Jaramillo E, et al. The impact of digital health technologies on tuberculosis treatment:A systematic review. Eur Respir J. 2018;51:1701596. doi: 10.1183/13993003.01596-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verhoeven F, Tanja-Dijkstra K, Nijland N, Eysenbach G, van Gemert-Pijnen L. Asynchronous and synchronous teleconsultation for diabetes care:A systematic literature review. J Diabetes Sci Technol. 2010;4:666–84. doi: 10.1177/193229681000400323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verhoeven F, van Gemert-Pijnen L, Dijkstra K, Nijland N, Seydel E, Steehouder M. The contribution of teleconsultation and videoconferencing to diabetes care:A systematic literature review. J Med Internet Res. 2007;9:e37. doi: 10.2196/jmir.9.5.e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krishna S, Boren SA. Diabetes self-management care via cell phone:A systematic review. J Diabetes Sci Technol. 2008;2:509–17. doi: 10.1177/193229680800200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Story A, Aldridge RW, Smith CM, Garber E, Hall J, Ferenando G, et al. Smartphone-enabled video-observed versus directly observed treatment for tuberculosis:A multicentre, analyst-blinded, randomised, controlled superiority trial. Lancet. 2019;393:1216–24. doi: 10.1016/S0140-6736(18)32993-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lester R, Park JJ, Bolten LM, Enjetti A, Johnston JC, Schwartzman K, et al. Mobile phone short message service for adherence support and care of patients with tuberculosis infection:Evidence and opportunity. J Clin Tuberc Other Mycobact Dis. 2019;16:100108. doi: 10.1016/j.jctube.2019.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen TA, Pham MT, Nguyen TL, Nguyen VN, Pham DC, Nguyen BH, et al. Video directly observed therapy to support adherence with treatment for tuberculosis in Vietnam:A prospective cohort study. Int J Infect Dis. 2017;65:85–9. doi: 10.1016/j.ijid.2017.09.029. [DOI] [PubMed] [Google Scholar]
- 13.Story A, Garfein RS, Hayward A, Rusovich V, Dadu A, Soltan V, et al. Monitoring therapy compliance of tuberculosis patients by using video-enabled electronic devices. Emerg Infect Dis. 2016;22:538–40. doi: 10.3201/eid2203.151620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choun K, Achanta S, Naik B, Tripathy JP, Thai S, Lorent N, et al. Using mobile phones to ensure that referred tuberculosis patients reach their treatment facilities:A call that makes a difference. BMC Health Serv Res. 2017;17:575. doi: 10.1186/s12913-017-2511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gentry S, van-Velthoven MH, Tudor Car L, Car J. Telephone delivered interventions for reducing morbidity and mortality in people with HIV infection. Cochrane Database Syst Rev. 2013;2013:CD009189. doi: 10.1002/14651858.CD009189.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev. 2012;12:CD007457. doi: 10.1002/14651858.CD007457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ambia J, Mandala J. A systematic review of interventions to improve prevention of mother-to-child HIV transmission service delivery and promote retention. J Int AIDS Soc. 2016;19:20309. doi: 10.7448/IAS.19.1.20309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Castaño PM, Bynum JY, Andrés R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation:A randomized controlled trial. Obstet Gynecol. 2012;119:14–20. doi: 10.1097/AOG.0b013e31823d4167. [DOI] [PubMed] [Google Scholar]
- 19.Lund S, Hemed M, Nielsen BB, Said A, Said K, Makungu MH, et al. Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar:A cluster-randomised controlled trial. BJOG. 2012;119:12. doi: 10.1111/j.1471-0528.2012.03413.x. [DOI] [PubMed] [Google Scholar]


