Abstract
Background:
Bibliometrics is a methodology that measures the scientific output of an author, institution, or country. Visualized analysis is the transformation of data into visible form by software, highlighting important features, including commonalities and anomalies, allowing users to easily and quickly perceive significant aspects of their data.
Purpose:
To conduct a bibliometric analysis of the literature on anterior cruciate ligament (ACL) repair, with visualization of trends, in order to identify the areas of interest and the primary researchers involved in ACL repair.
Study Design:
Cross-sectional study.
Methods:
The PubMed database was queried on April 14, 2022, for publications that reported on ACL repair from 1960 onward. The initial search resulted in 1392 publications. Filter settings were applied to remove publications with weak correlation, such as those on meniscal repair and ACL reconstruction. Publication information, citations, authors, commonly used terms, and affiliated institutions and countries were analyzed by VOSviewer and Python.
Results:
A total of 553 articles were included for analysis. Three techniques were visualized: bridge-enhanced ACL repair, internal brace, and dynamic intraligamentary stabilization. The most published authors were Martha Murray (51 articles), Gregory Difelice (35 articles), and Braden Fleming (31 articles). The most cited article was “Collagen–Platelet Rich Plasma Hydrogel Enhances Primary Repair of the Porcine Anterior Cruciate Ligament” by Murray et al. The journals with the most publications on ACL repair were the American Journal of Sports Medicine (n = 49); Knee Surgery, Sports Traumatology, Arthroscopy (n = 49); and Arthroscopy (n = 48). The top 3 institutions by publication number were the Hospital for Special Surgery (n = 51), Boston Children’s Hospital (n = 49), and Brown University (n = 31), with the most publications coming from the United States (n = 242), Germany (n = 83), and the United Kingdom (n = 47).
Conclusion:
The results demonstrate that the research on ACL repair comes from a small number of authors and corresponding institutions; the top sports medicine journals and the developed countries have an interest in this topic.
Keywords: anterior cruciate ligament, ACL, bibliometrics, bridge-enhanced ACL repair, internal brace, dynamic intraligamentary stabilization
Although the existence of the anterior cruciate ligament (ACL) was recognized as early as the ancient Greeks, 32 operative treatment of ACL injury is not uncommon today. Mayo Robson 20 published a case report of the surgical repair of cruciate ligaments of a coal digger in 1903. ACL repair was sparingly performed over the remainder of the century, with Feagin and Curl 8 publishing a seminal report on the 5-year outcome of military cadets who underwent ACL repair, finding high rates of persistent instability with associated disability. Marshall et al 19 published a similar case series in 1982 but found more favorable outcomes using their described repair technique. However, the advent and refinement of ACL reconstruction offered more consistent outcomes than ACL repair. In a long-term study comparing 3 techniques for treating ACL injury, Drogset et al 6 found that the rate of revision after 1-stage ACL repair was much higher than that after ACL reconstruction with bone–patellar tendon–bone autograft. This coincided with the continued refinement of knee arthroscopy, 25 ushering in an era during which ACL reconstruction become standard of care for patients with ACL injuries who intended to return to sports.
Despite the advances made in ACL reconstruction, graft failure rates of approximately 5% are commonly reported, with higher rates noted in younger, competitively athletic populations. 9 Furthermore, radiographic evidence of osteoarthritis is found in more than 20% of patients at a minimum of 10 years after ACL reconstruction. 29 These limitations in contemporary ACL reconstruction have motivated continued research on novel methods to improve outcomes after ACL injury, with renewed interest in ACL repair. Indeed, publications on ACL repair have increased in recent years, including reports on novel surgical techniques and fixation devices, 11,16,18 biologic scaffolds, 17 and suture tape augmentation. 4
In this study, we sought to capture the trends in ACL repair by use of bibliometric analysis, 2,3 which more easily allows visualization of publication trends compared with systematic reviews. We aimed to trace the evolution of ACL repair in the literature, with a particular focus on the frequency and connectivity of keywords, authors, journals, publications, institution, and countries.
Methods
Search Strategy
We queried the PubMed database on April 14, 2022, for publications that reported on ACL repair from 1960 onward; the search strategy is detailed in Supplemental Table S1, available separately. All types of studies were considered in the initial screening, including those with evidence levels from 1 (high-quality prospective randomized trials) through 5 (expert opinions). The initial search resulted in 1392 publications, after which publications were further screened by title and abstract. Publications principally focused on techniques other than ACL repair, such as meniscal repair and ACL reconstruction, were excluded. Original articles, case reports, rapid communication, letters to the editor, comments, narrative reviews, systematic reviews, and meta-analyses focused on primary ACL repair were all included. Papers identified in searches were reviewed by the corresponding author (with more than 10 years of sports medicine experience). Journal Citation Reports 2021 was used to obtain the impact factor (IF) and the category quartile (Q) of relevant journals.
Data Processing
Python, GraphPad Prism, and VOSviewer were applied to analyze and plot the annual publication output. Python 28 (version 3.9.6; Guido van Rossum) was used to extract relevant characteristics of publications, including authors, institution, journal, and country. The code to perform this function is included in Supplemental Table S2. GraphPad Prism 21 (version 9.2.0) was used to visualize trends and to map the number of articles published by different authors. VOSviewer software 35 (version 1.6.17; Leiden University) was applied for constructing and visualizing bibliometric networks.
Results
A total of 553 publications were included in the final analysis. Two fit lines indicated the arithmetic distribution of the number of publications per year and the average number of publications per 3 years (Figure 1). There were 2 epochs of increasing publication frequency. From 1980 to 1993, the 3-year average number of articles on ACL repair increased before diminishing near the turn of the century. A second rise in publication frequency began in 2010 and continues through the present. Information on relevant authors and institutions for the 2 epochs of increasing publication frequency is provided in Supplemental Table S3.
Figure 1.
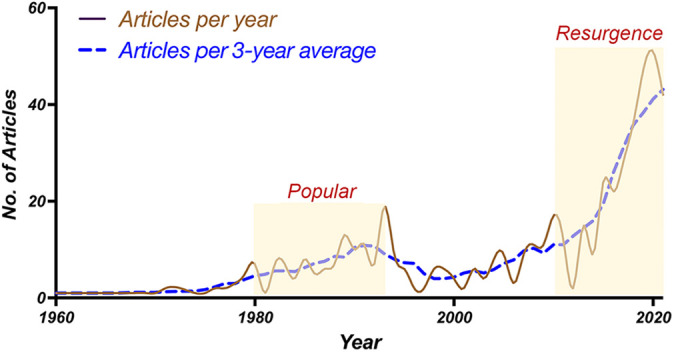
Yearly trend in publications on anterior cruciate ligament repair, 1960-2020, by articles per year and articles per 3-year average.
No consistent contribution trend from a single author was noticed. However, during the period from 1982 to 1993, among the top 10 researchers, 2 were from the Hospital for Special Surgery. Among the top 20 authors in terms of publication volume during the period from 2010 to 2022, 3 were from the Hospital for Special Surgery.
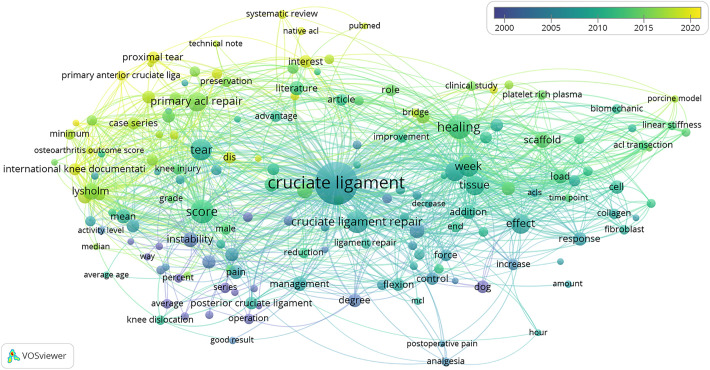
VOSviewer was used to determine the occurrence and relevance of the most frequent terms used in the title or abstract of publications of ACL repair (Table 1). The most commonly used terms were “cruciate ligament,” “healing,” “score,” “tear,” and “week.” VOSviewer was also used to visualize the connectivity of terms. In Figure 2, the changes in commonly used terms from 2000 to 2020 are shown. For example, “proximal tear” and “primary ACL repair” appeared more frequently in recent years, while “instability” and “operation” were more frequently used in older publications.
Table 1.
Frequency of Commonly Used Terms in ACL Repair Publications (top 46 terms) a
| Term | Occurrence | Relevance | Term | Occurrence | Relevance |
|---|---|---|---|---|---|
| Cruciate ligament | 382 | 0.02 | Degree | 39 | 0.31 |
| Healing | 119 | 0.55 | Study design | 39 | 0.29 |
| Score | 114 | 0.65 | Suture repair | 39 | 0.86 |
| Tear | 99 | 0.63 | Arthroscopy | 37 | 0.65 |
| Week | 83 | 0.44 | Cell | 37 | 2.62 |
| Effect | 78 | 0.91 | Examination | 37 | 0.56 |
| Tissue | 77 | 0.55 | Response | 37 | 1.95 |
| Primary ACL repair | 76 | 0.79 | ACL tear | 35 | 0.87 |
| Use | 75 | 0.41 | Interest | 35 | 0.29 |
| Lysholm | 56 | 1.47 | Control | 33 | 0.45 |
| Scaffold | 51 | 1.25 | Clinical outcome | 33 | 0.93 |
| Fixation | 49 | 0.35 | Development | 33 | 0.77 |
| Change | 48 | 0.29 | Flexion | 33 | 0.5 |
| Instability | 48 | 0.6 | Lachman test | 33 | 1.07 |
| Mean | 44 | 1.19 | Posterior cruciate ligament | 33 | 0.73 |
| Addition | 43 | 0.45 | Dog | 32 | 0.77 |
| Pain | 43 | 0.56 | Approach | 31 | 0.59 |
| Literature | 42 | 0.35 | Article | 31 | 0.26 |
| Fracture | 41 | 0.58 | Case series | 31 | 1.03 |
| Hypothesis | 41 | 0.48 | Tegner | 31 | 1.36 |
| IKDC | 41 | 1.53 | Proximal tear | 30 | 1.3 |
| Load | 41 | 1.67 | Role | 30 | 0.24 |
| Management | 40 | 0.4 | DIS | 29 | 0.55 |
a The occurrence attribute indicates the number of articles in which the term occurs at least once. Terms with a high relevance score tend to represent specific topics covered by the text data, while terms with a low relevance score tend to be of a general nature and not representative of any specific topic. ACL, anterior cruciate ligament; DIS, dynamic intraligamentary stabilization; IKDC, International Knee Documentation Committee.
Figure 2.
Distribution of commonly used terms according to time of appearance, 2000-2020. Blue indicates the terms that appeared earlier, whereas yellow reflects a later occurrence.
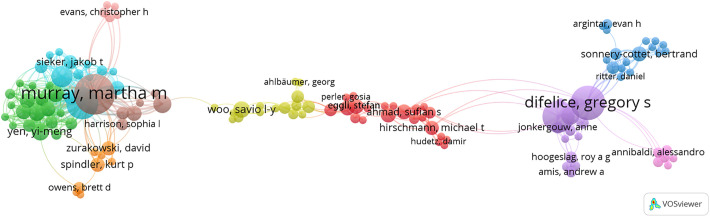
There were 1747 unique authors who contributed to the included publications on ACL repair, 250 of whom had written more than 2 articles, 43 more than 5 articles, and 7 more than 10 articles. The visual results of VOSviewer show 3 clusters of authors, corresponding primarily to 3 different ACL repair techniques: bridge-enhanced ACL repair (BEAR), dynamic intraligamentary stabilization (DIS), and anchors and suture tape augmentation (ie, internal bracing) (Figure 3). Author groupings were most commonly centered around 4 corresponding authors: Martha Murray, Gregory Difelice, Stefan Eggli, and Savio Woo (Figure 3).
Figure 3.
The visualization of authors involved in anterior cruciate ligament (ACL) repair publications was roughly divided into 3 clusters. The left cluster principally involved work on bridge-enhanced ACL repair, the central cluster involved dynamic intraligamentary stabilization, and the right cluster was related to the study of anchors and suture tape augmentation (internal bracing).
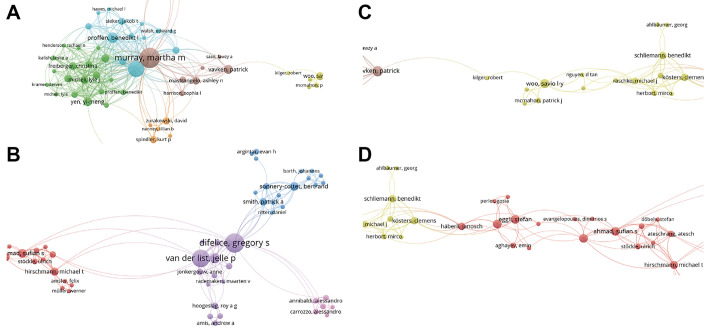
The network of authors for each of these corresponding authors is shown in Figure 4. As shown in Figure 5, the most published authors were (in descending order) Martha Murray, Gregory Difelice, and Braden Fleming.
Figure 4.
Networks of authors publishing on anterior cruciate ligament repair surgery. Shown are coauthors who published with (A) Martha Murray, (B) Gregory Difelice, (C) Savio Woo, and (D) Stefan Eggli.
Figure 5.
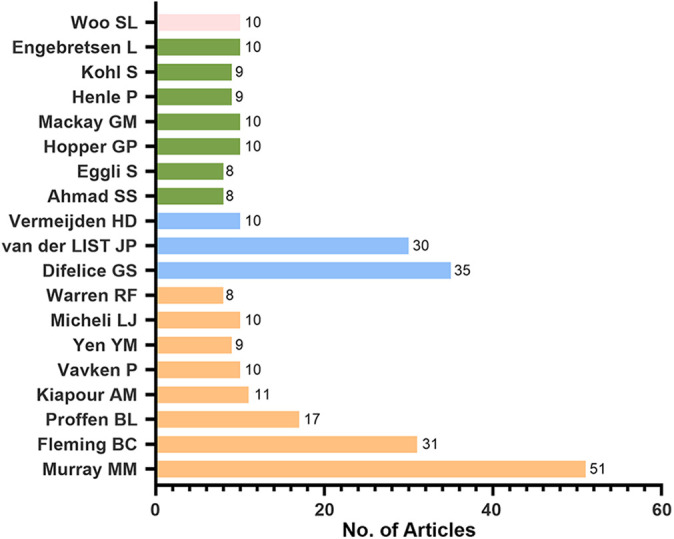
Number of articles on anterior cruciate ligament repair published by 19 authors. Affiliated coauthors are depicted by the same bar color.
The top 10 journals with the most publications related to ACL repair are listed in Table 2. The American Journal of Sports Medicine (IF, 7.01; Q1) and Knee Surgery, Sports Traumatology, Arthroscopy (IF, 4.11; Q1) had the largest number of publications, followed by Arthroscopy (IF, 5.97; Q1).
Table 2.
Top 10 Journals With the Most Publications Related to ACL Repair a
| Rank | Journal | No. of Publications |
|---|---|---|
| 1 | American Journal of Sports Medicine | 49 |
| 2 | Knee Surgery, Sports Traumatology, Arthroscopy | 49 |
| 3 | Arthroscopy | 48 |
| 4 | Arthroscopy Techniques | 36 |
| 5 | Journal of Orthopaedic Research | 31 |
| 6 | Clinical Orthopaedics and Related Research | 20 |
| 7 | Journal of Bone & Joint Surgery—American Volume | 19 |
| 8 | Knee | 19 |
| 9 | Orthopaedic Journal of Sports Medicine | 16 |
| 10 | Veterinary Surgery | 9 |
a ACL, anterior cruciate ligament.
The 16 most cited publications in descending order are listed in Appendix Table A1. The most highly cited publication was “Collagen–Platelet Rich Plasma Hydrogel Enhances Primary Repair of the Porcine Anterior Cruciate Ligament” by Murray et al, 24 with 119 citations. This study demonstrated that biomechanical properties measured after primary repair of the ACL transection in a porcine model were enhanced with use of a collagen–platelet-rich plasma hydrogel placed within the repair site. These results supported the hypothesis that an important mechanism for failure of the ACL to heal was a lack of appropriate provisional scaffold. The second most cited article was “Isolated Tear of the Anterior Cruciate Ligament: 5-Year Follow-up Study” by Feagin and Curl, 8 with 113 citations. In this study, the authors found that the failure rate of primary ACL repair with suture was high at the 5-year follow-up. A follow-up study on this small series 33 indicated that the patients had progressive knee deterioration, in part supporting the adoption of ACL reconstruction as the standard of care in the decades that followed.
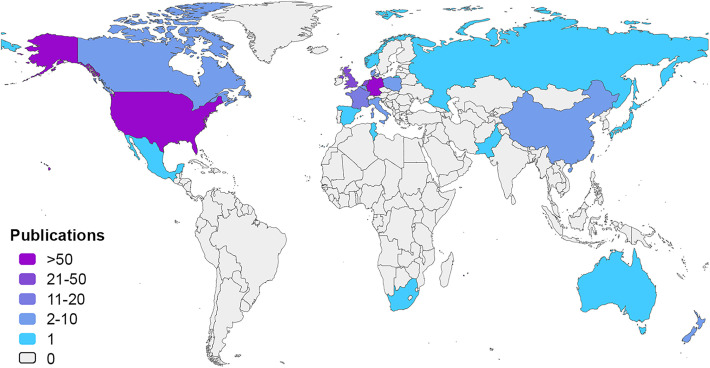
Table 3 lists affiliated institutions by number of publications. The Hospital for Special Surgery, Boston Children’s Hospital, and Brown University produced the most publications. Brown University is affiliated with the Rhode Island Hospital. All 4 organizations are located in the United States. The majority of publications were from the United States (n = 242) and Germany (n = 83), followed by the United Kingdom (n = 47), the Netherlands (n = 24), France (n = 16), Canada (n = 6), and China (n = 6) (Figure 6).
Table 3.
Ranking of ACL Repair Documents in Each Organization a
| Rank | Institution | No. of Publications |
|---|---|---|
| 1 | Hospital for Special Surgery | 51 |
| 2 | Boston Children’s Hospital | 49 |
| 3 | Brown University | 31 |
| 4 | University of Bern | 17 |
| 5 | University of Antwerp | 17 |
| 6 | University of Amsterdam | 17 |
| 7 | University of Pittsburgh | 15 |
| 8 | University Hospital Münster | 9 |
| 9 | Cedars-Sinai Kerlan-Jobe Institute | 8 |
| 10 | Sonnenhof Orthopaedic Center | 9 |
a ACL, anterior cruciate ligament.
Figure 6.
Distribution by country of publications on anterior cruciate ligament repair.
Discussion
In this study, we visualized the trends in research on ACL repair, finding periods of increased publication numbers from 1980 to 1993 and again from 2010 until the present day. The downward trend in the curve after 2020 was presumed to be due to the impact of the COVID-19 pandemic. Renewed interest in ACL repair has principally come from 3 surgical techniques, BEAR, DIS, and suture tape augmentation (internal bracing), which are associated with corresponding authors Martha Murray, Stefan Eggli, and Gregory Difelice, respectively. The American Journal of Sports Medicine; Knee Surgery, Sports Traumatology, Arthroscopy; and Arthroscopy had the most publications on ACL repair. The Hospital for Special Surgery, Boston Children’s Hospital, and Brown University represented the top 3 institutions by publication number, with the most publications coming from the United States, Germany, and the United Kingdom.
The BEAR technique, associated with Martha Murray, entails augmentation of an ACL repair with a collagen-platelet scaffold. 27 Numerous preclinical studies demonstrated that the BEAR technique reliably increased tissue formation at the tear site, largely restoring ACL structure and function, thereby restoring knee stability and diminishing osteoarthritic changes predicably seen with ACL insufficiency. 1,14 A first-in-human cohort study compared 10 patients undergoing BEAR matched with 10 patients who underwent ACL reconstruction with hamstring tendon autograft, finding no failures in either group with similar patient-reported outcomes and knee stability and function between the groups at the 2-year follow-up. 23 A subsequent prospective randomized controlled trial comparing BEAR (n = 65) against ACL reconstruction with hamstring tendon autograft (n = 35) found noninferiority in patient-reported outcomes and knee laxity with improved hamstring strength in the BEAR group, while 14% of patients who underwent BEAR and 6% of patients who underwent ACL reconstruction required a second ipsilateral ACL surgery. 22
Primary repair of proximal ACL tears with or without suture tape augmentation (internal bracing) has been recently advanced by the Gregory Difelice and colleagues. In 1991, Sherman et al 31 suggested that primary ACL suture repair yielded good results with particular ACL injury characteristics, notably, older patients with proximal ACL tears, good residual tissue quality, and “tight-jointedness” with mild preoperative flexion contracture. Building on this work, Vermeijden et al 36 demonstrated that ACL tear location and remnant length could be reliably measured on magnetic resonance imaging. In a cohort study of 56 consecutive patients with proximal ACL tears that underwent primary ACL repair with suture anchor fixation, good objective and subjective outcomes were obtained at the average 3.2-year follow-up, with 6 patients (10.7%) experiencing repair failure. 13 Of the first 11 consecutive patients, clinical outcomes were maintained at an average follow-up of 6 years. 5
DIS has been most commonly investigated in Europe by Stefan Eggli and colleagues. DIS employs a dynamic spiral spring mechanism to reduce aberrant anterior tibial translation in the ACL-injured knee, which is often combined with biological augmentation (eg, microfracture and/or platelet-rich plasma) at the tear site in an effort to promote neotissue formation. 7 DIS-mediated ACL healing was demonstrated first in a preclinical sheep model in 2013. 15 A subsequent case series of 105 patients who underwent DIS reported failure with a revision rate of 16.3% and residual side-to-side anterior-posterior laxity ≥3 mm in 18.2% of cases, which the authors noted were higher than the values typically reported after ACL reconstruction. 30 Similarly, Osti et al 26 found an overall complication rate of 57.9% in a case series of 59 patients undergoing DIS, with complications including rerupture (17.5%), new meniscal tear (15.4%), cyclops formation (30.8%), and restricted range of motion (53.8%). On the other hand, in a prospective randomized controlled trial comparing DIS versus ACL reconstruction, there was no statistically significant difference in failure requiring revision surgery (DIS 16.3% vs ACL reconstruction 12.5%) nor rates of recurrent objective or subjective instability or patient-reported outcome measures (ie, Tegner, International Knee Documentation Committee, or Lysholm score). 16
As visualized through this bibliometric analysis of the literature on ACL repair, the recent rise in publications on the topic has largely come from a small number of corresponding authors and their associated coauthors. Overcoming the past limitations of ACL repair to achieve a viable clinical strategy equal or superior to ACL reconstruction will require the involvement of more research groups, with collaboration and exchange among investigators. While the recent innovations in surgical techniques, devices, and biomaterials have likely contributed to the renewed interest in ACL repair, there is no consensus on indications for surgical repair, surgical technique, or rehabilitation protocols. 37 The level of evidence is low and there are limited studies reporting medium- or long-term outcomes. 12,34
Limitations
This study has some limitations. First, the analysis of global ACL research is somewhat flawed, as published articles are mostly written in English and there are many journals in other languages that are worth studying. Second, authors prefer to cite articles from the journal in which they intend to publish. This might bring in the bias of “incomplete citing” and “omission bias.” Finally, authors tend to use widely cited literature that they think is more reliable. This is called the snowball effect and tends to be biased.
Conclusion
This article summarized research topics, trends, and sources for ACL repair as well as outlined global research on its impact. It allows researchers who want to understand ACL repair to quickly grasp the development history, current status, and trends of the research field, and have a macro understanding of global ACL repair research. It also provides a general understanding of the current mainstream surgical methods and allows comparisons among authors and institutions with greater academic influence around the world, in turn guiding further study and research cooperation. Consequently, ACL reconstruction remains the gold-standard surgical option for patients with ACL tears. 12 An ongoing prospective randomized clinical trial comparing BEAR, DIS, internal brace augmentation, and ACL reconstruction will help clarify the relative merit of each approach. 10
Supplemental Material for this article is available at https://journals.sagepub.com/doi/full/10.1177/23259671221132564#supplementary-materials.
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671221132564 for Trends in Anterior Cruciate Ligament Repair: A Bibliometric and Visualized Analysis by Jinfei Li, Benjamin Rothrauff, Shuyi Chen, Shuying Zhao, Zhaoxi Wu, Qi Chen and Jinshen He in Orthopaedic Journal of Sports Medicine
Acknowledgment
The authors express their gratitude to Dr Freddie H. Fu at the University of Pittsburgh. Thank you, Dr Fu. You are so deeply missed.
Appendix
Table A1.
Most Cited Articles on ACL Repair a
| No. of Citations | |||
|---|---|---|---|
| Title | Authors | Overall | Excluding Self-Citations |
| Collagen–platelet rich plasma hydrogel enhances primary repair of the porcine anterior cruciate ligament | Murray MM, Spindler KP, Abreu E, Muller JA, Nedder A, Kelly M, Frino J, Zurakowski D, Valenza M, Snyder BD, Connolly SA, | 119 | 66 |
| Isolated tear of the anterior cruciate ligament: 5-year follow-up study | Feagin JA Jr, Curl WW | 113 | 113 |
| Enhanced histologic repair in a central wound in the anterior cruciate ligament with a collagen–platelet-rich plasma scaffold | Murray MM, Spindler KP, Ballard P, Welch TP, Zurakowski D, Nanney LB | 99 | 55 |
| Use of a collagen–platelet rich plasma scaffold to stimulate healing of a central defect in the canine ACL | Murray MM, Spindler KP, Devin C, Snyder BS, Muller J, Takahashi M, Ballard P, Nanney LB, Zurakowski D | 74 | 39 |
| Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: a randomized study with a 15-year follow-up | Meunier A, Odensten M, Good L | 73 | 73 |
| The long-term follow up of primary anterior cruciate ligament repair. Defining a rationale for augmentation | Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I | 73 | 72 |
| Use of a bioactive scaffold to stimulate anterior cruciate ligament healing also minimizes posttraumatic osteoarthritis after surgery | Murray MM, Fleming BC | 63 | 29 |
| Basic science of anterior cruciate ligament injury and repair | Kiapour AM, Murray MM | 79 | 72 |
| Collagen–platelet composite enhances biomechanical and histologic healing of the porcine anterior cruciate ligament | Joshi SM, Mastrangelo AN, Magarian EM, Fleming BC, Murray MM | 67 | 37 |
| Untreated ruptures of the anterior cruciate ligament. A follow-up study | McDaniel WJ Jr, Dameron TB Jr | 56 | 56 |
| The anterior cruciate ligament: a technique of repair and reconstruction | Marshall JL, Warren RF, Wickiewicz TL, Reider B | 62 | 61 |
| Platelet-rich plasma alone is not sufficient to enhance suture repair of the ACL in skeletally immature animals: an in vivo study | Murray MM, Palmer M, Abreu E, Spindler KP, Zurakowski D, Fleming BC | 61 | 30 |
| Ligament repair and reconstruction in traumatic dislocation of the knee | Liow RY, McNicholas MJ, Keating JF, Nutton RW | 58 | 58 |
| Biomechanical outcomes after bioenhanced anterior cruciate ligament repair and anterior cruciate ligament reconstruction are equal in a porcine model | Vavken P, Fleming BC, Mastrangelo AN, Machan JT, Murray MM | 55 | 31 |
| Indications for surgical treatment of tibial condyle fractures | Honkonen SE | 51 | 51 |
| Current status and potential of primary ACL repair | Murray MM | 49 | 41 |
a ACL, anterior cruciate ligament.
Footnotes
Final revision submitted August 9, 2022; accepted August 30, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: Support for this study was received from the Education Reform Foundation of Central South University (grant 2021JY188), the National Natural Science Foundation of China (grant 81802208), and the Natural Science Foundation of Hunan Province (grant 2021JJ40922). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Biercevicz AM, Proffen BL, Murray MM, Walsh EG, Fleming BC. T2* relaxometry and volume predict semi-quantitative histological scoring of an ACL bridge-enhanced primary repair in a porcine model. J Orthop Res. 2015;33(8):1180–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;101(suppl 1):5303–5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen C, Dubin R, Kim MC. Emerging trends and new developments in regenerative medicine: a scientometric update (2000-2014). Expert Opin Biol Ther. 2014;14(9):1295–1317. [DOI] [PubMed] [Google Scholar]
- 4. Dabis J, Yasen SK, Foster AJ, Pace JL, Wilson AJ. Paediatric proximal ACL tears managed with direct ACL repair is safe, effective and has excellent short-term outcomes. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2551–2556. [DOI] [PubMed] [Google Scholar]
- 5. DiFelice GS, van der List JP. Clinical outcomes of arthroscopic primary repair of proximal anterior cruciate ligament tears are maintained at mid-term follow-up. Arthroscopy. 2018;34(4):1085–1093. [DOI] [PubMed] [Google Scholar]
- 6. Drogset JO, Grøntvedt T, Robak OR, et al. A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 2006;88(5):944–952. [DOI] [PubMed] [Google Scholar]
- 7. Eggli S, Kohlhof H, Zumstein M, et al. Dynamic intraligamentary stabilization: novel technique for preserving the ruptured ACL. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1215–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Feagin JA, Jr, Curl WW. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med. 1976;4(3):95–100. [DOI] [PubMed] [Google Scholar]
- 9. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY study randomized clinical trial. Am J Sports Med. 2020;48(2):285–297. [DOI] [PubMed] [Google Scholar]
- 10. Heusdens CHW, Zazulia K, Roelant E, et al. Study protocol: a single-blind, multi-center, randomized controlled trial comparing dynamic intraligamentary stabilization, internal brace ligament augmentation and reconstruction in individuals with an acute anterior cruciate ligament rupture. LIBR study. BMC Musculoskelet Disord. 2019;20(1):547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hohmann E. Editorial commentary: renaissance of primary anterior cruciate ligament repair. Is history repeating itself? Arthroscopy. 2016;32(12):2570–2571. [DOI] [PubMed] [Google Scholar]
- 12. Hughes JD, Lawton CD, Nawabi DH, Pearle AD, Musahl V. Anterior cruciate ligament repair: the current status. J Bone Joint Surg Am. 2020;102(21):1900–1915. [DOI] [PubMed] [Google Scholar]
- 13. Jonkergouw A, van der List JP, DiFelice GS. Arthroscopic primary repair of proximal anterior cruciate ligament tears: outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):21–28. [DOI] [PubMed] [Google Scholar]
- 14. Kiapour AM, Fleming BC, Murray MM. Structural and anatomic restoration of the anterior cruciate ligament is associated with less cartilage damage 1 year after surgery: healing ligament properties affect cartilage damage. Orthop J Sports Med. 2017;5(8):2325967117723886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kohl S, Evangelopoulos DS, Kohlhof H, et al. Anterior crucial ligament rupture: self-healing through dynamic intraligamentary stabilization technique. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):599–605. [DOI] [PubMed] [Google Scholar]
- 16. Kösters C, Glasbrenner J, Spickermann L, et al. Repair with dynamic intraligamentary stabilization versus primary reconstruction of acute anterior cruciate ligament tears: 2-year results from a prospective randomized study. Am J Sports Med. 2020;48(5):1108–1116. [DOI] [PubMed] [Google Scholar]
- 17. LaPrade RF, Spalding T, Murray IR, et al. Knee arthroscopy: evidence for a targeted approach. Br J Sports Med. 2020;55(13):707–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liao W, Zhang Q. Is primary arthroscopic repair using the pulley technique an effective treatment for partial proximal ACL tears? Clin Orthop Relat Res. 2020;478(5):1031–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marshall JL, Warren RF, Wickiewicz TL. Primary surgical treatment of anterior cruciate ligament lesions. Am J Sports Med. 1982;10(2):103–107. [DOI] [PubMed] [Google Scholar]
- 20. Mayo Robson AW. VI: Ruptured crucial ligaments and their repair by operation. Ann Surg. 1903;37(5):716–718. [PMC free article] [PubMed] [Google Scholar]
- 21. Motulsky H. GraphPad Prism. Version 9.2.0. Accessed October 9, 2022. https://www.graphpad.com
- 22. Murray MM, Fleming BC, Badger GJ, et al. Bridge-enhanced anterior cruciate ligament repair is not inferior to autograft anterior cruciate ligament reconstruction at 2 years: results of a prospective randomized clinical trial. Am J Sports Med. 2020;48(6):1305–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Murray MM, Kalish LA, Fleming BC, et al. Bridge-enhanced anterior cruciate ligament repair: two-year results of a first-in-human study. Orthop J Sports Med. 2019;7(3):2325967118824356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Murray MM, Spindler KP, Abreu E, et al. Collagen–platelet rich plasma hydrogel enhances primary repair of the porcine anterior cruciate ligament. J Orthop Res. 2007;25(1):81–91. [DOI] [PubMed] [Google Scholar]
- 25. Musahl V, Karlsson J. Anterior cruciate ligament tear. N Engl J Med. 2019;380(24):2341–2348. [DOI] [PubMed] [Google Scholar]
- 26. Osti M, El Attal R, Doskar W, Höck P, Smekal V. High complication rate following dynamic intraligamentary stabilization for primary repair of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):29–36. [DOI] [PubMed] [Google Scholar]
- 27. Perrone GS, Proffen BL, Kiapour AM, et al. Bench-to-bedside: bridge-enhanced anterior cruciate ligament repair. J Orthop Res. 2017;35(12):2606–2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rossum GV. Python. Version 3.9.6. Accessed October 9, 2022. https://www.python.org/
- 29. Rothrauff BB, Jorge A, de Sa D, et al. Anatomic ACL reconstruction reduces risk of post-traumatic osteoarthritis: a systematic review with minimum 10-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1072–1084. [DOI] [PubMed] [Google Scholar]
- 30. Senftl M, Petek D, Jacobi M, et al. Occurrence of inadequate ACL healing after dynamic intraligamentary stabilization and functional outcome—a multicentre case series. Eur J Orthop Surg Traumatol. 2022;32(7):1265–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I. The long-term followup of primary anterior cruciate ligament repair: defining a rationale for augmentation. Am J Sports Med. 1991;19(3):243–255. [DOI] [PubMed] [Google Scholar]
- 32. Snook GA. A short history of the anterior cruciate ligament and the treatment of tears. Clin Orthop Relat Res. 1983;172:11–13. [PubMed] [Google Scholar]
- 33. Taylor DC, Posner M, Curl WW, Feagin JA. Isolated tears of the anterior cruciate ligament: over 30-year follow-up of patients treated with arthrotomy and primary repair. Am J Sports Med. 2009;37(1):65–71. [DOI] [PubMed] [Google Scholar]
- 34. van der List JP, Vermeijden HD, Sierevelt IN, et al. Arthroscopic primary repair of proximal anterior cruciate ligament tears seems safe but higher level of evidence is needed: a systematic review and meta-analysis of recent literature. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1946–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Vermeijden HD, Cerniglia B, Mintz DN, et al. Distal remnant length can be measured reliably and predicts primary repair of proximal anterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):2967–2975. [DOI] [PubMed] [Google Scholar]
- 37. Vermeijden HD, Yang XA, van der List JP, DiFelice GS. Large variation in indications, preferred surgical technique and rehabilitation protocol for primary anterior cruciate ligament repair: a survey among ESSKA members. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3613–3621. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671221132564 for Trends in Anterior Cruciate Ligament Repair: A Bibliometric and Visualized Analysis by Jinfei Li, Benjamin Rothrauff, Shuyi Chen, Shuying Zhao, Zhaoxi Wu, Qi Chen and Jinshen He in Orthopaedic Journal of Sports Medicine