Abstract
Purpose
The biplanar whole body imaging system (EOS) is a new tool for measuring the whole body sagittal alignment in a limited space. This tool may affect the sagittal balance of patients compared to conventional whole spine X-ray (WSX). This study aimed to investigate the difference in sagittal alignment between WSX and EOS.
Materials and Methods
We compared the spinal and pelvic sagittal parameters in 80 patients who underwent EOS and WSX within one month between July 2018 and September 2019. The patients were divided based on sagittally balanced and imbalanced groups according to pelvic tilt (PT) >20°, pelvic incidence-lumbar lordosis >10°, C7-sagittal vertical axis (SVA) >50 mm in WSX.
Results
In the sagittally imbalanced group, compared to WSX, the pelvic parameters demonstrated compensation in EOS with smaller PT (27.4±11.6° vs. 24.9±10.9°, p=0.003) and greater sacral slope (SS), and the patients tended to stand more upright with smaller C7-SVA (58.4±17.0 mm vs. 48.9±57.3 mm, p=0.018), T1-pelvic angle (TPA), T5-T12, and T2-T12. However, in the sagittally balanced group, these differences were less pronounced only with smaller PT (10.8±6.9° vs. 9.4±4.7°, p=0.040), TPA and T2-T12 angle, but with similar SS and C7-SVA (p>0.05).
Conclusion
EOS showed a negative SVA shift and lesser PT compared to WSX, especially in patients with sagittal imbalance. When preparing a surgical plan, surgeons should consider these differences between EOS and WSX.
Keywords: EOS, whole spine x-ray, compensatory mechanism, sagittal parameters
INTRODUCTION
Due to the correlation between self-reported pain and disability, accurate assessment of sagittal parameters of patients with spinal malalignment has become an important factor.1,2,3,4 Several studies tried to reveal a compensatory mechanism for the reciprocal change interrelationship between spine–pelvis–hip joint and lower extremities.5,6 To avoid translation of the gravity line of the body due to progressive disc degeneration and loss of disc height, there is frequent hyperextension of the adjacent segment at the thoracic and cervical levels. Cervical hyperlordosis and thoracic hypokyphosis result from the rebalancing efforts, as described by Dubousset7 in his concept of an “efficiency cone.” Patients use the retroversion mechanism at the level of pelvis, and this occasionally translates into extension of the hip joints.8,9,10,11 At the lower extremity level, small lumbar lordosis (LL) is associated with a large pelvic shift and compensatory knee flexion.12
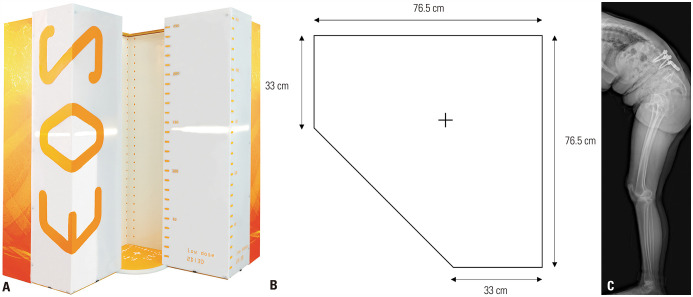
The EOS imaging system (EOS imaging, Paris, France), which uses an ultrasensitive multiwire proportional chamber detector, allows simultaneous anteroposterior (AP) and lateral 2D imaging of the whole body in a calibrated environment. However, since EOS whole body image is conducted in a narrow space, patients are required to maintain a standing balanced posture during examination (Fig. 1). Unlike in EOS examination, patients stand relatively free under instructions in open space during conventional whole spine X-ray (WSX) evaluation.13 Sagittal and spinopelvic parameters may vary significantly depending on the patient’s posture even in the same modality of radiographs.14,15,16
Fig. 1. (A) EOS imaging system (https://www.eos-imaging.com/professionals/materials). Perpendicularly placed, vertically moving, co-linked units of X-ray tubes producing very thin collimated X-ray beams collected by unique line detectors with Nobel Prize-winning technology resulted in simultaneously captured biplanar digital images of a patient in a standing, weight-bearing position. (B) A space on which the patient stands. The width and length were about 76.5 cm each. (C) A patient with severe sagittal deformity whose entire body could not be examined with an EOS system.
Before surgical treatments for deformity, patients are usually evaluated with EOS instead of WSX. The sagittal and spinopelvic parameters may differ between EOS and WSX, but we are not aware of any research on this topic. Therefore, this study was conducted to elucidate any sagittal parameter differences between WSX and EOS.
MATERIALS AND METHODS
Study design
We reviewed medical records of 113 patients who had undergone both EOS and WSX at a single institution between July 2018 and September 2019. Since EOS was first introduced to our hospital in 2018, the patients had undergone both WSX and EOS during the transition period. A total of 80 patients who satisfied the following criteria were enrolled in this study: patients aged 18 years or older, those whose examination interval between EOS and WSX was less than 1 month, and those who had not undergone surgery or suffered spinal infection prior to each examination. Exclusion criteria included the following: previous history of spine deformity, knee, or hip surgery; major coronal deformity (Cobb angle ≥30°); inability to stand unaided due to severe sagittal imbalance or weakness; traumatic fracture; malignancy; or congenital, neuromuscular, or connective tissue disorders. Furthermore, to demonstrate the sagittal imbalance differences between the two test modalities, we divided the patients into two groups: sagittally balanced group and sagittally imbalanced group. Sagittally imbalanced group was defined as patients who had any of pelvic incidence (PI)–LL >10°, C7-sagittal vertical axis (SVA) >5 cm, pelvic tilt (PT) >20° in either EOS or WSX; and the remaining patients were classified into sagittally balanced group. Institutional Review Board approval was received for this study with a waiver of informed consent (No. 2020-0031-001).
Radiologic examination
All eligible patients underwent both EOS and WSX in an upright standing position. In EOS, we followed the manual of other studies. We instructed the patients to place fingertips of both hands on zygomas with the upper arms at an angle of approximately 45° to vertical, and rest in a comfortable position for about 10 seconds before the examination 13. For WSX, our study used the Radiographic Measurement Manual introduced by the Scoliosis Research Society; 36-inch whole-spine AP and lateral plain radiographs were collected at a 72-inch distance from the film. The patients stood in a comfortable position with their knees locked, feet at shoulder width apart, looking straight ahead, with their elbows bent, and fists on clavicles.13,14
Data collection
Baseline demographics of age, sex, and body mass index (BMI) were recorded. The spinopelvic balance was evaluated at the C7-SVA and T1-pelvic angle (TPA), the angle between the line from the femoral head axis to the center of the T1 vertebra, and the line from the femoral head axis to the middle of the S1 superior endplate, respectively.
The following spinopelvic parameters were measured: PT, PI, sacral slope (SS), LL, PI minus LL, thoracic kyphosis (T2-T5, T5-T12, and T2-T12 Cobb angles), and thoracolumbar kyphosis (T10-L2 Cobb angle). The cervical parameters were C0-C2 angle (occiput to C2 Cobb angle); C2-C7 lordosis (C2-C7 Cobb angle); C2-C7 SVA, the horizontal distance between a plumb line dropped from C2 to the postero-superior corner of C7; and T1 slope, the angle between the superior endplate of T1 and a horizontal reference line.
The lower extremity parameter was the sacrofemoral angle (SFA), the angle formed between the bicoxofemoral axis and the line tangent to the superior endplate of S1, and the line between the bicoxofemoral axis and the femoral axis. Since there were no WSX measurement below the knees, the knee flexion angle or ankle dorsiflexion angle was not measured. The spinal balance parameter was the sagittal C2 (C7) plumb line, the distance between the plumb lines passing through HA and the plumb lines from the centroids of C2 (C7) vertebral bodies.
Each parameter was measured with imaging software (Centricity Enterprise Web V 3.0; GE Medical Systems, Milwaukee, WI, USA). All measurements were taken independently by two experienced spinal surgeons to assess inter-rater variability. For intra-rater reliability, measurements were made twice at 1-month intervals. The average value was used to minimize intra-rater and inter-rater errors.
Statistical analysis
Inter-rater and intra-rater reliability analysis between the measurers was performed using interclass correlation coefficients. All parameters were measured at values of 0.8 or higher, representing excellent reliability.17 To determine EOS and WSX differences, paired t-tests or Wilcoxon test were used on the measured data from all patients depending on the normality of distribution of each parameter. Data analysis of the sagittal imbalance group was performed separately. All statistical analysis was conducted using IBM SPSS Statistics ver. 25.0 (IBM Corp., Armonk, NY, USA), with statistical significance set at p<0.05 throughout.
RESULTS
Patient demographics
Overall, the average age of patients was 63.2 years, and there were 40 male and 40 female patients. The average patient BMI was 25.1±4.24 kg/m2. Degenerative spondylolisthesis and spondylotic stenosis were predominant (57 of 80). Fifty-two patients were in the sagittally imbalance group, and 28 patients were in the sagittal balanced group. In the sagittally imbalanced group, male/female sex ratio was higher (20/32) compared that in the sagittally balanced group (20/8), with older age (67.3 years to 55.5 years, p=0.010), lower height and weight, and similar BMI. In both WSX and EOS, the sagittally imbalance group had larger PI, PI-LL, and PT and smaller PT and SS compared to the sagittally balanced group (Table 1).
Table 1. Demographics and Sagittal Parameters of Study Patients.
| Demographics | All patients (n=80) | Sagittally balanced patients (n=28) | Sagittally imbalanced patients (n=52) | p value | ||
|---|---|---|---|---|---|---|
| Age (yr) | 63.2±13.3 | 55.5±14.0 | 67.3±11.0 | 0.010* | ||
| Sex (male/female) | 40/40 | 20/8 | 20/32 | 0.005 * | ||
| Weight (kg) | 64.8±13.3 | 68.3±9.0 | 62.9±12.9 | 0.051 | ||
| Height (cm) | 160.7±9.9 | 166.3±8.1 | 157.8±9.6 | 0.001* | ||
| BMI (kg/m2) | 25.1±4.24 | 24.7±2.7 | 25.3±4.9 | 0.582 | ||
| Pathology | ||||||
| Cervical myelopathy | 6 | 5 | 1 | |||
| Degenerative spondylolisthesis | 28 | 8 | 20 | |||
| Herniated lumbar disc | 8 | 2 | 6 | |||
| Lumbar degenerative kyphosis | 6 | 0 | 6 | |||
| Spondylolytic spondylolisthesis | 3 | 0 | 3 | |||
| Lumbar stenosis | 29 | 13 | 16 | |||
| Sagittal parameters | ||||||
| PI | ||||||
| WSX | 50.2±11.5 | 42.6±6.4 | 54.2±11.7 | <0.001* | ||
| EOS | 50.6±11.5 | 43.2±6.9 | 54.6±11.6 | <0.001* | ||
| LL | ||||||
| WSX | -35.3±14.5 | -44±7.9 | -30.5±15.1 | <0.001* | ||
| EOS | -35.5±14.4 | -44.3±8.9 | -30.8±14.6 | <0.001* | ||
| PI-LL | ||||||
| WSX | 14.9±18.8 | -1.4±6.7 | 23.7±17.3 | <0.001* | ||
| EOS | 15.1±18.9 | -1.1±7.0 | 24.0±17.3 | <0.001* | ||
| PT | ||||||
| WSX | 21.6±12.2 | 10.8±4.7 | 27.4±10.9 | <0.001* | ||
| EOS | 19.4±11.5 | 9.4±5.7 | 24.9±10.2 | <0.001* | ||
| SS | ||||||
| WSX | 28.6±8.7 | 32.6±7.0 | 26.5±8.9 | 0.002* | ||
| EOS | 30.8±8.1 | 33.9±5.9 | 29.2±8.7 | 0.014* | ||
BMI, body mass index; WSX, conventional whole spine X-ray; PI, pelvic incidence; LL, lumbar lordosis; PT, pelvic tilt; SS, sacral slope.
Descriptive data are presented as mean±standard deviation. Positive values signify an anterior position of the vertical plumb line with respect to the caudal landmark for translation measurements and kyphosis for angular measurements.
*p<0.05.
Comparison of sagittal balance, spinal curvature, spinopelvic parameters, and lower limb parameter between EOS and WSX in sagittally imbalanced group
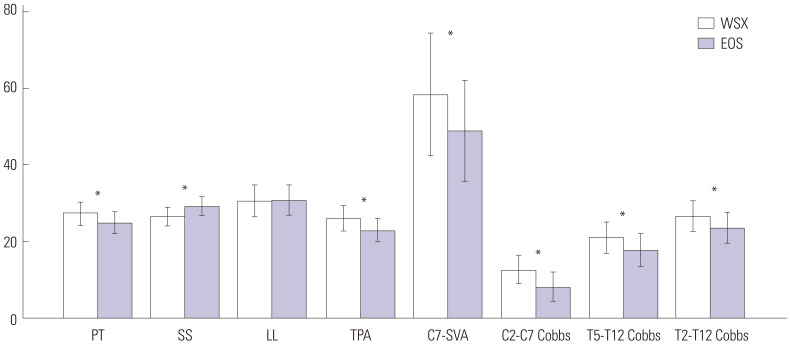
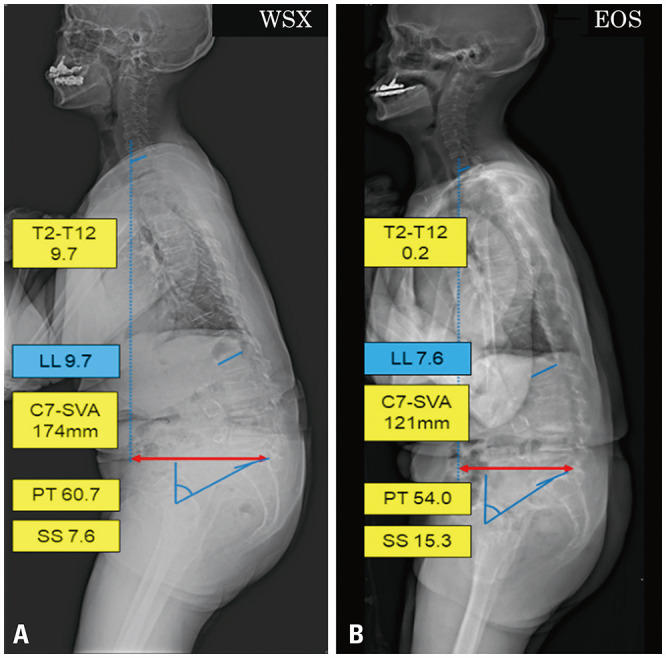
A number of significant radiological differences between EOS and WSX were observed. C7-SVA was significantly greater in WSX (58.4±17.0 mm) than in EOS (48.9±57.3 mm, p=0.018). WSX TPA was 26.1±13.9°, while that for EOS TPA was 22.9±12.0° (p=0.002). The kyphosis of T2-T12, T5-T12, and the lordosis of C2-C7 were decreased in EOS compared to WSX. The LLs were similar between the two tests, but spinopelvic parameters demonstrated compensation in EOS. EOS PT (24.9±10.9°) was decreased compared to WSX PT (27.4±11.6°, p=0.003), and EOS SS (29.2±8.9°) was increased compared to WSX SS (26.5±14.6°, p=0.006) (Table 2 and Fig. 2). Typical cases of the sagittally imbalanced patients are illustrated in Fig. 3.
Table 2. Comparison of Sagittal Balance, Spinal Curvature, Spinopelvic Parameters, and Lower Limb Parameters between WSX and EOS in Sagittally Imbalanced Patients†.
| WSX | EOS | p value | ||
|---|---|---|---|---|
| Sagittal balance | ||||
| C2-C7 SVA (mm) | 21±47.2 | 21.8±15.3 | 0.644 | |
| C2-HA (°) | 5.3±6.9 | 5.3±6.3 | 0.973 | |
| C7-HA (°) | 5.4±7.0 | 4.9±7.2 | 0.320 | |
| C7-SVA (mm) | 58.4±17.0 | 48.9±57.3 | 0.018* | |
| TPA (°) | 26.1±13.9 | 22.9±12.0 | 0.002* | |
| Spinal curvature (°) | ||||
| T1-slope | 21.7±11.1 | 20.9±10.7 | 0.352 | |
| C0-C2 angle | -30±10.2 | -28.1±12.8 | 0.461 | |
| C2-C7 lordosis | -12.6±14.8 | -8.2±13.7 | 0.008* | |
| T2-T5 angle | 9.5±15.9 | 10±9.9 | 0.456 | |
| T5-T12 angle | 21±14.4 | 17.7±14.4 | 0.001* | |
| T2-T12 angle | 26.6±14.6 | 23.6±14.5 | 0.010* | |
| T10-L2 angle | 11.3±10.6 | 8.9±16.7 | 0.133 | |
| Spinopelvic parameters (°) | ||||
| PI | 54.2±8.7 | 54.6±11.7 | 0.697 | |
| LL | -30.5±17.5 | -30.8±15.1 | 0.851 | |
| PI-LL | 23.7±9.8 | 23.9±17.3 | 0.837 | |
| PT | 27.4±11.6 | 24.9±10.9 | 0.003* | |
| SS | 26.5±14.6 | 29.2±8.9 | 0.006* | |
| Lower limb parameter (°) | ||||
| SFA | 150.4±51.5 | 152.5±23.4 | 0.519 | |
WSX, conventional whole spine X-ray; SVA, sagittal vertical axis; TPA, T1-pelvic angle; PI, pelvic incidence; LL, lumbar lordosis; PT, pelvic tilt; SS, sacral slope; SFA, sacrofemoral angle.
Descriptive data are presented as mean±standard deviation.
*p<0.05; †Sagittal imbalanced patients had one of the following conditions: PI-LL >10°, SVA >5 cm, and PT >20° on WSX. Positive values signify an anterior position of the vertical plumb line with respect to the caudal landmark for translation measurements and kyphosis for angular measurements.
Fig. 2. Comparisons of sagittal parameters between WSX and EOS in patients with sagittal imbalance. *Indicates significant differences in angles between WSX and EOS (p<0.05). For LL and C2-C7 Cobbs, positive values indicate lordosis and negative values indicate kyphosis. WSX, conventional whole spine X-ray; PT, pelvic tilt; SS, sacral slope; LL, lumbar lordosis (L1-S1 Cobbs angle); TPA, T1-pelvic angle; SVA, sagittal vertical axis.
Fig. 3. Typical case of the sagittally imbalanced group. Compared to WSX (A), EOS (B) showed smaller PT (60.7° to 54.0°), C7-SVA (174 to 121 mm), T2-T12 (9.7° to 0.2°), and larger SS (7.6° to 15.3°), indicating a compensation. WSX, conventional whole spine X-ray; PT, pelvic tilt; SS, sacral slope; SVA, sagittal vertical axis.
Subgroup comparison of EOS and WSX in sagittally balanced group
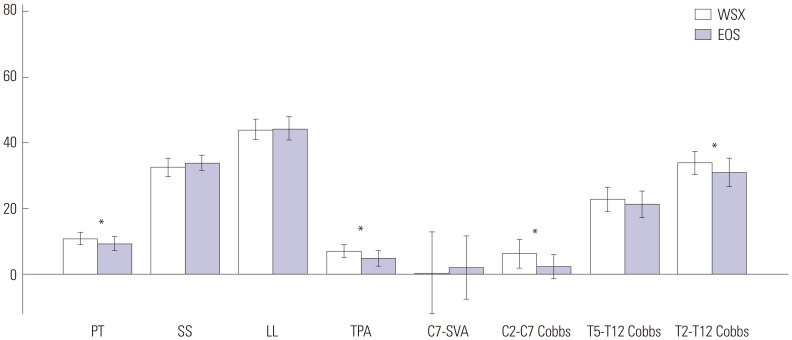
In sagittally balanced patients, EOS PT (10.8±6.9° vs. 9.4±4.7°, p=0.040), TPA (7.1±9.3° vs. 4.9±4.8°, p=0.010), C2-C7 lordosis (-6.3±13.4° vs. -2.4±11.2°, p=0.033), and T2-T12 angle (33.9±7.4° vs. 31.1±9°, p=0.042) were decreased compared to those of WSX. However, SS, C7-SVA, and T5-T12, which showed differences in the sagittal imbalanced group, did not show differences in EOS and WSX in the sagittal balanced group (Table 3 and Fig. 4).
Table 3. Comparison of Sagittal Balance, Spinal Curvature, Spinopelvic Parameters, and Lower Limb Parameter between WSX and EOS in Sagittally Balanced Patients†.
| WSX | EOS | p value | ||
|---|---|---|---|---|
| Sagittal balance | ||||
| C2-C7 SVA (mm)‡ | 21.1±25.1 | 18.4±9.3 | 0.244 | |
| C2-HA (°) | -0.7±3.2 | -0.5±3.3 | 0.819 | |
| C7-HA (°) | -1.9±7.0 | -1.6±3.2 | 0.489 | |
| C7-SVA (mm) | 0.3±10.2 | 2.0±32.0 | 0.763 | |
| TPA (°) | 7.1±9.3 | 4.9±4.8 | 0.010* | |
| Spinal curvature (°) | ||||
| T1-slope | 18.6±6.0 | 16.2±9.3 | 0.159 | |
| C0-C2 angle | -27.3±7.1 | -34.0±23.8 | 0.179 | |
| C2-C7 lordosis | -6.3±13.4 | -2.4±11.2 | 0.033* | |
| T2-T5 angle | 13.2±10.5 | 12.6±7.2 | 0.561 | |
| T5-T12 anglev | 22.8±11.3 | 21.3±9.8 | 0.241 | |
| T2-T12 angle | 33.9±7.4 | 31.1±9.0 | 0.042* | |
| T10-L2 angle | 6.3±8.1 | 5.2±8.0 | 0.171 | |
| Spinopelvic parameters (°) | ||||
| PI | 42.6±5.9 | 43.2±6.4 | 0.496 | |
| LL | -44±7.0 | -44.3±7.9 | 0.719 | |
| PI-LL | -1.4±9.9 | -1.1±6.7 | 0.668 | |
| PT | 10.8±6.9 | 9.4±4.7 | 0.040* | |
| SS | 32.6±8.9 | 33.9±7.0 | 0.158 | |
| Lower limb parameter (°) | ||||
| SFA | 163.8±30.9 | 162.7±7.0 | 0.473 | |
WSX, conventional whole spine X-ray; SVA, sagittal vertical axis; TPA, T1-pelvic angle; PI, pelvic incidence; LL, lumbar lordosis; PT, pelvic tilt; SS, sacral slope; SFA, sacrofemoral angle.
Descriptive data are presented as mean±standard deviation.
*p<0.05; †Sagittal balanced patients had none of the following conditions: PI-LL >10°, SVA >5 cm, and PT >20° on WSX. Positive values signify an anterior position of the vertical plumb line with respect to the caudal landmark for translation measurements and kyphosis for angular measurements; ‡Data did not follow a normal distribution, and Wilcoxon test was used.
Fig. 4. Comparisons of sagittal parameters between WSX and EOS in patients without sagittal imbalance. *Indicates significant differences in angle between WSX and EOS (p<0.05). For LL and C2-C7 Cobbs, positive values indicate lordosis and negative values indicate kyphosis. WSX, conventional whole spine X-ray; PT, pelvic tilt; SS, sacral slope; LL, lumbar lordosis (L1-S1 Cobbs angle); TPA, T1-pelvic angle; SVA, sagittal vertical axis.
DISCUSSION
For spinal deformity surgery, knowledge of whole-body alignment, including spine and lower extremities, is essential. This knowledge is the basis for decisions regarding spinal deformity treatment strategy. This knowledge also allows for the prediction of postoperative complications, such as proximal/distal junctional problem, mechanical failure, and poor surgical outcome.10,14,18,19,20
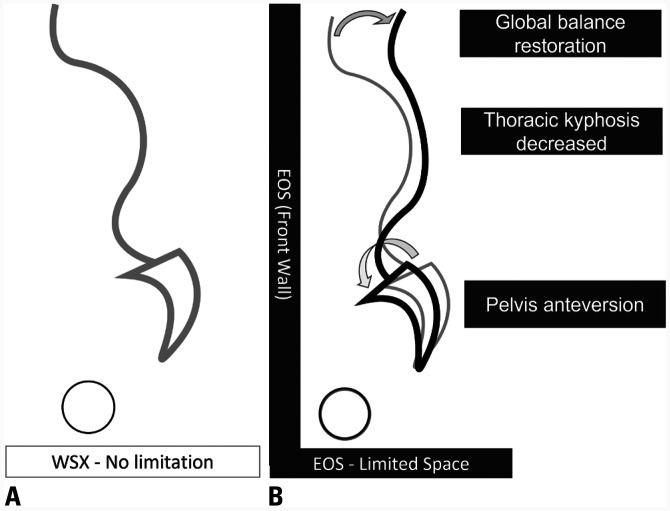
We found that the patient expression of compensatory mechanisms for balance was shown more in EOS than in WSX. Also, sagittally imbalanced patients showed more differences in sagittal parameters compared to sagittally balanced patients. Global balance, TPA, and C7-SVA were better restored in EOS than in WSX. In EOS, patients had more cervical lordosis, less thoracic kyphosis, less PT, and higher SS than in WSX. We believe that using more compensatory mechanisms in EOS resulted in restored TPA and C7-SVA (Fig. 5). However, in sagittally balanced patients, we observed smaller values in EOS only in TPA, PI, C2-C7 angle, and T2-T12 angle; on the other hand, SS and C7-SVA did not show any difference, as the sagittally balanced patients were already well-compensated. TPA, a known independent parameter from pelvic retroversion and knee flexion, differed from C7-SVA. Since the patients in this study did not undergo surgery, in contrast to the patients included in the Protopsaltis study, they had alterations in thoracic kyphosis, which is believed to be the reason for the differences in TPA between the two tests.21
Fig. 5. A figure showing the change of the entire spinal balance in EOS. (A) Directed standing in open space (conventional whole spine X-ray, gray line) vs. (B) Directed standing within limited space (EOS, black line). WSX, conventional whole spine X-ray.
The reason for the differences in sagittal parameters of the two tests is probably the change of patient alignment in limited space and anterior closed wall of the EOS apparatus. While attempting to stand in the limited space of EOS, patients would, consciously or unconsciously, use more compensatory mechanisms to move the gravity line posteriorly. Hey, et al.15 reported that, compared to directed standing, relaxed standing results in a more kyphotic sagittal profile that is marked by significantly smaller LL and SS and larger PT, thoracic kyphosis, and T1-slope. In our study, compared to the result of Hey, et al.15, EOS showed a similar radiographical change to directed standing, whereas WSX was similar to natural standing. When patients try to stand upright while undergoing EOS, the sagittal profiles are changed to less kyphotic and shows smaller PT and larger SS, and hips are more extended. In sagittally unbalanced patients, however, the difference between the two tests for PT and SS compared to the cervico-thoracic parameter are minor, requiring caution in interpretation of the results. To determine the precise difference of PT and SS between EOS and WSX, additional research with larger number of patients or trials including patients who have had thoracolumbar fixation are required.
While there were differences in LL between the two groups in Wong’s study, no difference was found in our study between the two groups of EOS and WSX. The reason for the different results in LL is likely due to the differences in study groups; for instance, the healthy population had an average age of 21 years, while patients with spinal disorders had an average age of 63.2 years. Loss of LL is an initial phenomenon in degeneration, not a result of compensation. Patients losing LL due to degenerative lumbar disease experience compensation in other areas.
There could be posture differences due to varying instructions. EOS patients were instructed to place their fingertips on the zygoma, while WSX patients were asked to place them in the clavicular fossa. Differences in the hand position may affect the various parameters of this study. There are debates that SVA or LL may vary depending on the hand position of patients.16,22 However, it is difficult to consider the results of this study as a change according to the position of the hand, as Kaneko, et al.23 reported that, compared to this study, there was no significant difference between the sagittal angles in the posture of raising the hand on the zygoma and raising the hand on the clavicle in EOS.
When planning the surgery, surgeons should consider the fact that the sagittal parameters measured by EOS are affected by the compensatory mechanism, which results from the effort of patients tying to stand upright in a limited space. In addition, when using EOS for post-operative evaluation, the sagittal imbalance may be evaluated as being less severe than the patient’s true state. If the patient’s sagittal imbalance is too severe, it should be recognized that the EOS scan may not fully reflect the patient’s imbalance. To solve these issues, it is essential to establish a precise indication for EOS. Also, further development of biplanar imaging system with open space would be helpful in obtaining accurate sagittal parameters.
The limitations of this study included its retrospective nature, small number of patients, lack of control group, no consideration of the radial X-ray properties of WSX, and the partial measurement of lower leg parameters in WSX, as it does not involve filming below the hip joint. However, we were able to compare SFA in our data, and there was no difference between the two tests. Sagittally imbalanced subgroup patients did not have severe sagittal deformity that requires surgical intervention. Due to the nature of EOS, obtaining the alignment angle from the severely malaligned patients who cannot stand in confined spaces was impossible. Therefore, we excluded these confounder patients from our study. Moreover, this study has no control group who did not have any spinal diseases. In addition, EOS and WSX were performed within 1 month, not simultaneously. This may have caused difficulties in making an accurate comparison due to the changes in patient condition or progression of the disease. Therefore, we excluded the patients with a gap of 1 month or more between EOS and WSX examinations, as well as those who showed substantial disease condition changes in the first month. EOS is a non-radial X-ray system, whereas WSX is a radial X-ray system. As the object moves further from the center of the source, measurement distortion may occur; however, this concern was insufficient in our research. To reduce the amount of distortion, multiple WSX X-rays should be obtained and combined.
In conclusions, sagittal parameters of patients with sagittal imbalance were different according to EOS or WSX. Pelvic anteversion with reduced PT and increased SS was more pronounced in EOS compared to WSX. Less sagittal parameters could show differences according to EOS or WSX in sagittally balanced patients. This difference could be the result of the limited EOS space. Our finding suggests that EOS is a better reflection than WSX of the patient compensatory mechanism in maintaining standing balance.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yoon Ha and Kyung Hyun Kim.
- Data curation: Dong Kyu Chin, Keun Su Kim, and Yong Eun Cho.
- Formal analysis: Hyun Jun Jang and Kyung Hyun Kim.
- Methodology: Jeong Yoon Park and Sung Uk Kuh.
- Project administration: Hyun Jun Jang and Dong Kyu Chin.
- Visualization: Hyun Jun Jang and Kyung Hyun Kim.
- Writing—original draft: Hyun Jun Jang and Kyung Hyun Kim.
- Writing—review & editing: Hyun Jun Jang and Kyung Hyun Kim.
- Approval of final manuscript: all authors.
References
- 1.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 2.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 3.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 4.Berjano P, Langella F, Ismael MF, Damilano M, Scopetta S, Lamartina C. Successful correction of sagittal imbalance can be calculated on the basis of pelvic incidence and age. Eur Spine J. 2014;23 Suppl 6:587–596. doi: 10.1007/s00586-014-3556-8. [DOI] [PubMed] [Google Scholar]
- 5.Dubousset J, Charpak G, Skalli W, de Guise J, Kalifa G, Wicart P. [Skeletal and spinal imaging with EOS system] Arch Pediatr. 2008;15:665–666. doi: 10.1016/S0929-693X(08)71868-2. French. [DOI] [PubMed] [Google Scholar]
- 6.Lazennec JY, Brusson A, Folinais D, Zhang A, Pour AE, Rousseau MA. Measuring extension of the lumbar-pelvic-femoral complex with the EOS® system. Eur J Orthop Surg Traumatol. 2015;25:1061–1068. doi: 10.1007/s00590-015-1603-8. [DOI] [PubMed] [Google Scholar]
- 7.Dubousset J. In: The pediatric spine: principles and practice. Weinstein SL, editor. New York: Raven Press; 1994. Three-dimensional analysis of the scoliotic deformity; pp. 479–496. [Google Scholar]
- 8.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976) 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 9.Vanneuville G, Garcier JM, Poumarat G, Guillot M, Chazal J. Mechanisms of orientation of the pelvifemoral base during static loading of the lumbar spine in weight-lifters. Surg Radiol Anat. 1992;14:29–33. doi: 10.1007/BF01628040. [DOI] [PubMed] [Google Scholar]
- 10.Legaye J, Duval-Beaupère G. Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg. 2005;71:213–220. [PubMed] [Google Scholar]
- 11.Barrey C, Roussouly P, Le Huec JC, D’Acunzi G, Perrin G. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013;22 Suppl 6:S834–S841. doi: 10.1007/s00586-013-3030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferrero E, Liabaud B, Challier V, Lafage R, Diebo BG, Vira S, et al. Role of pelvic translation and lower-extremity compensation to maintain gravity line position in spinal deformity. J Neurosurg Spine. 2016;24:436–446. doi: 10.3171/2015.5.SPINE14989. [DOI] [PubMed] [Google Scholar]
- 13.Janssen MM, Drevelle X, Humbert L, Skalli W, Castelein RM. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine (Phila Pa 1976) 2009;34:E826–E832. doi: 10.1097/BRS.0b013e3181a9fd85. [DOI] [PubMed] [Google Scholar]
- 14.Hey HWD, Lau ET, Tan KA, Lim JL, Choong D, Lau LL, et al. Lumbar spine alignment in six common postures. Spine (Phila Pa 1976) 2017;42:1447–1455. doi: 10.1097/BRS.0000000000002131. [DOI] [PubMed] [Google Scholar]
- 15.Hey HWD, Tan KA, Chin BZ, Liu G, Wong HK. Comparison of whole body sagittal alignment during directed vs natural, relaxed standing postures in young, healthy adults. Spine J. 2019;19:1832–1839. doi: 10.1016/j.spinee.2019.06.017. [DOI] [PubMed] [Google Scholar]
- 16.Marks M, Stanford C, Newton P. Which lateral radiographic positioning technique provides the most reliable and functional representation of a patient’s sagittal balance? Spine (Phila Pa 1976) 2009;34:949–954. doi: 10.1097/BRS.0b013e318199650a. [DOI] [PubMed] [Google Scholar]
- 17.Vidal C, Ilharreborde B, Azoulay R, Sebag G, Mazda K. Reliability of cervical lordosis and global sagittal spinal balance measurements in adolescent idiopathic scoliosis. Eur Spine J. 2013;22:1362–1367. doi: 10.1007/s00586-013-2752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scheer JK, Lenke L, Smith JS, Passias PG, Kim HJ, Bess S, et al. Outcomes of surgical treatment for one hundred and thirty-eight patients with severe sagittal deformity at a minimum 2-year follow-up. Neurosurgery. 2019;66:310–408. doi: 10.1093/ons/opab153. [DOI] [PubMed] [Google Scholar]
- 19.Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 2017;14:126–132. doi: 10.14245/kjs.2017.14.4.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kyrölä KK, Salme J, Tuija J, Tero I, Eero K, Arja H. Intra- and interrater reliability of sagittal spinopelvic parameters on full-spine radiographs in adults with symptomatic spinal disorders. Neurospine. 2018;15:175–181. doi: 10.14245/ns.1836054.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Protopsaltis T, Schwab F, Bronsard N, Smith JS, Klineberg E, Mundis G, et al. TheT1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Joint Surg Am. 2014;96:1631–1640. doi: 10.2106/JBJS.M.01459. [DOI] [PubMed] [Google Scholar]
- 22.Horton WC, Brown CW, Bridwell KH, Glassman SD, Suk SI, Cha CW. Is there an optimal patient stance for obtaining a lateral 36" radiograph? A critical comparison of three techniques. Spine (Phila Pa 1976) 2005;30:427–433. doi: 10.1097/01.brs.0000153698.94091.f8. [DOI] [PubMed] [Google Scholar]
- 23.Kaneko K, Aota Y, Sekiya T, Yamada K, Saito T. Validation study of arm positions for evaluation of global spinal balance in EOS imaging. Eur J Orthop Surg Traumatol. 2016;26:725–733. doi: 10.1007/s00590-016-1813-8. [DOI] [PubMed] [Google Scholar]