Abstract
Objective The authors describe a novel solution to the challenges of lengthy notes and poor note readability by creating an unobtrusive clinical decision support tool named “disappearing help text.”
Methods We designed this tool in Pediatric Hospital Medicine (PHM) note templates to provide in-line decision support on best documentation practices, note bloat reduction, billing compliance, and provider workflow enhancement.
Results After template changes that utilized disappearing help text, we reduced the percent of notes utilizing any laboratory SmartLink from 90.2 to 15.3% for admission notes ( p <0.001), 92.6 to 17.8% for progress notes ( p <0.001), and 14 to 7.2% for discharge summaries ( p <0.001). In admission and progress notes, this correlated with a significant reduction in the median note length as a proxy of note bloat reduction, with a 18.7% character count reduction in progress notes ( p <0.001) and a 6.4% reduction in admission notes ( p <0.001). PHM coding queries decreased from an average of 42 per month to 36 per month, and there was no change in PHM attending billing compliance audit performance.
Discussion Note template changes that utilized disappearing help text significantly reduced the length of both progress and admission notes, a proxy for note bloat reduction, without negatively impacting coding query frequency or internal billing audit performance. One factor that likely contributed to this reduction in note length is the reduced usage of laboratory SmartLinks prompted by disappearing help text.
Conclusion We present the use of in-line disappearing help text embedded into note templates as a clinical decision support tool to improve note readability, educate trainees on note documentation, and protect confidential teen information. Help text implementation correlated with a reduction in the automatic insertion of laboratories into notes and a decrease in note character count.
Keywords: clinical documentation and communications, encounter level, notes, discharge summary, electronic health record, confidentiality, clinical decision support, physician
Background and Significance
Electronic health record (EHR) documentation burden, poor note readability, and “note bloat” are common problems cited with EHRs and have been associated with increased provider stress and burnout. 1 2 3 4 5 Several factors have contributed to the propagation of lengthy notes that can be not only difficult to read and write, but also inaccurate. 6 7 8 These factors include the ease of copy-forward functionality, the ability to automatically populate data into notes, the use of the note rather than native sections for information review, and the misinterpretation of billing compliance as requiring that all information referenced be included in the note itself. 6 7 9 10 11 Moving from a SOAP (subjective, objective, assessment, plan) to an APSO (assessment, plan, subjective, objective) format 10 12 and collapsing the individual SOAP sections 13 have been suggested as ways to improve note readability. However, these interventions do not address the underlying issues: long notes which contain superfluous information, rendering important clinical data difficult to locate and making the patient story difficult to follow. Options for clinical decision support (CDS) tools to improve provider note documentation practices have previously been limited.
Objective
We sought to shift the note paradigm from a repository of copied data to a succinct summary of the patient story with a focus on medical decision making. As a tertiary pediatric academic teaching hospital with an obligation to educate trainees on note writing, we wanted to embed in-line education on note best practices within the note. Additionally, with an expectation that notes will be shared with patients, we wanted to create more readable notes while also protecting confidential teen information from inadvertently being shared with caregivers. We describe our novel solution to these challenges by creating an unobtrusive CDS tool named “disappearing help text” and inserting it into inpatient note templates used by the Pediatric Hospital Medicine (PHM) service.
Methods
The tool was created using existing functionality within the EHR (Epic Systems, Verona, Wisconsin, United States) and applied to note templates. Text to guide clinicians is displayed when a note is being written which disappears upon note signature, hence the name “disappearing help text.” This tool does not interfere with existing functionality in the note, including keyboard navigation and wildcard selection. The tool provides guidance on best documentation practices, enhances provider workflow while reducing need for auto-populated data in the note via hyperlinks to recommended activities, and enables targeted CDS by displaying specific help text based on patient characteristics.
Providing In-line Guidance for Note Best Practices
We utilized disappearing help text to deliver in-line guidance at the point of care to note authors for PHM admission, progress, and discharge summary notes. Best practice guidance included summarizing significant laboratory results rather than auto-populating entire lists of results into the note via SmartLinks, a tool within Epic that can automatically populate data from the patient record into a note ( Fig. 1-1 ).
Fig. 1.
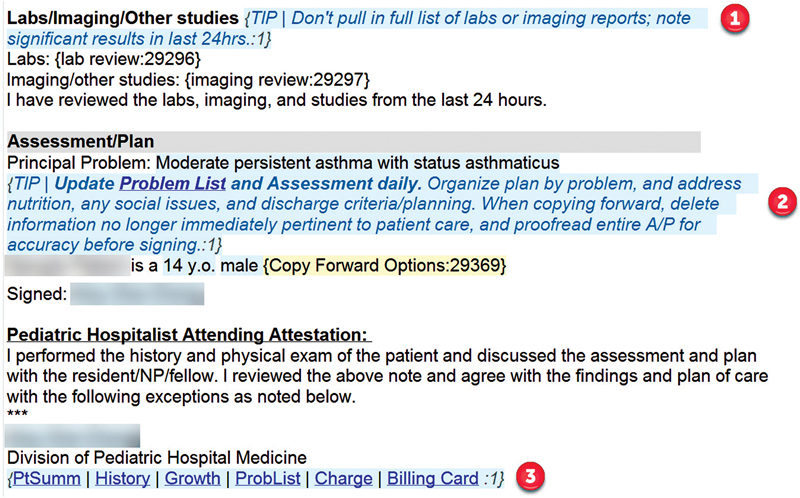
Disappearing help text examples in progress note template. (1) Labs and imaging best practice documentation; (2) Assessment and plan best practice documentation with problem list activity hyperlink. (3) Attending attestation activity hyperlinks and billing reference hyperlink. (c) 2021 Epic Systems Corporation.
Providing In-line Guidance for Billing Compliance
Billing compliance is a frequently cited reason for writing lengthy notes. Disappearing help text added activity hyperlinks to note templates and instructed providers that review of the information in the hyperlinks with appropriate linking language would meet billing requirements without needing to pull the information into the note itself. Activity hyperlinks are hyperlinks in notes that, when clicked, open a specified activity page in the EHR. Help text also added a billing guideline reference hyperlink to the PHM attending attestation template ( Fig. 1-3 ).
Enhancing Provider Workflow via Activity Hyperlinks
The activity hyperlinks in help text additionally enhanced provider workflows by promoting review of patient and encounter level data in appropriate sections of the EHR, rather than directly in the note. The hyperlinks aimed to reduce note bloat by reducing the automatic import of non-relevant information into the note for the purposes of review. They also had secondary aims of (1) promoting structured data entry which could trigger CDS and enhance reporting, (2) encouraging completion of required documentation, (3) decreasing EHR documentation burden by reducing clicks, mouse moves, and screen jumps, (4) allowing other clinicians to easily find patient-level information rather than searching through notes, and (5) protecting confidential teen information.
Help text and hyperlinks directing providers to EHR activities promoted review and completion of patient-level items such as past history and medication reconciliation in shared sections outside of the note ( Figs. 2-2 3 ). To protect confidential teen information and assist release of information staff, help text linked to a shared teen history section and guided clinicians to enter confidential teen history in this section rather than the note unless directly related to the patient's reason for hospitalization ( Fig. 2-2 ).
Fig. 2.
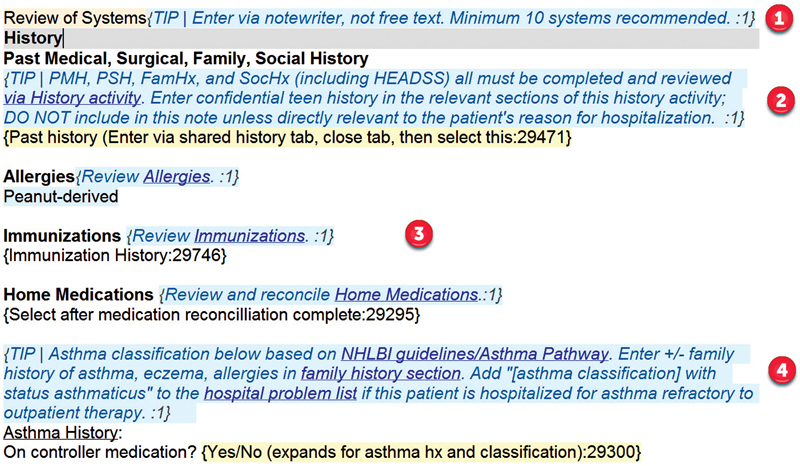
Disappearing help text examples in admission note template. (1) In-line guidance on billing compliance. (2) Rule-based help text for teens with hyperlink to patient-level shared history activity. (3) Activity hyperlinks to allergies, immunizations, and home medication reconciliation activities. (4) Rule-based help text for asthma patients with clinical guideline hyperlink, activity hyperlink, and in-line guidance on best practice documentation. (c) 2021 Epic Systems Corporation.
Fig. 3.
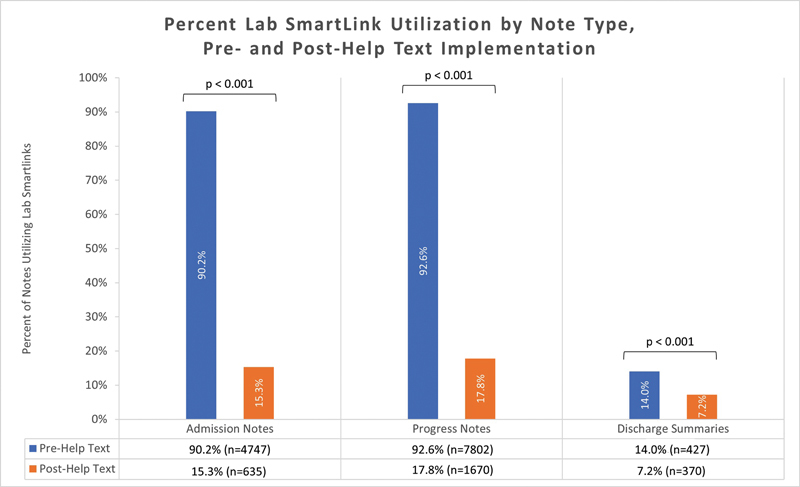
Percent SmartLink utilization by note type, pre- and post-help text implementation. For pediatric hospital medicine admission notes (pre: July 2018–June 2019, post: July 2019–Feb 2020), progress notes (pre: Sept 2017–Aug 2018, post: Sept 2018–Aug 2019), and discharge summaries (pre: May 2017–Apr 2018, post: May 2018–Apr 2019).
Enhancing Attending Review via Activity Hyperlinks
As an academic teaching hospital, another barrier to note bloat reduction is the common practice of attendings using the note as a record review tool. Help text-based hyperlinks to EHR activities requiring attending review (shared history, results, and problem list) were included in the templated attending addendum ( Fig. 1-3 ). This facilitated ease of review of the most up-to-date information by the attending directly in the medical record, while minimizing note bloat.
Rule-Based Help Text for Clinical Decision Support
We designed the help text to interface with patient-based rules, enabling targeted CDS by displaying help text that varied based on patient characteristics. For example, to promote note sharing, we provided CDS by displaying a message at the top of inpatient note templates to elucidate who would have access to the note via the patient portal based on pediatric patient age and diminished capacity status. Rule-based help text also provides CDS an appropriate developmental and teen history capture based on age. We also used patient-based rules to link to clinical guidelines for patients with specific diagnoses ( Fig. 2-4 ).
Data Collection
We evaluated characteristics of first authors admission, progress, and discharge summary notes before and after help text implementation. The first author is the one who first signed the note and, after help text implementation, viewed the help text. To evaluate the impact of disappearing help text on note bloat, we compared pre- and post-intervention median character count per note and the percent of PHM notes utilizing any laboratory SmartLink. We analyzed data in the 12 months before and after the addition of help text to note templates (implemented April 30, 2018 for discharge summaries, September 7, 2018 for progress notes, and June 28, 2019 for admission notes). Due to practice pattern changes related to the COVID-19 pandemic starting in March 2020, we discontinued data collection after February 29, 2020. hence, data for admission notes were only evaluated for 8 months after the addition of help text. As a proxy for note quality, we evaluated frequency of total coding queries sent to PHM attendings and internal billing compliance audit performance by PHM attendings during the periods before and after help text implementation. We also measured incomplete problem list coding queries to evaluate problem list utilization. Pre- and post-statistical comparisons were made using STATA 16.1 (College Station, Texas, United States). Chi-square analyses were performed for percent SmartLink utilization and Wilcoxon Rank Sum test was performed for median note character count.
Results
In total, 223 distinct providers viewed disappearing help text in PHM notes and consisted of pediatric and family medicine residents (81%), fellows (4%), nurse practitioners (4%), and attendings (11%) ( Table 1 ). Of all PHM notes evaluated, 73% were first authored by residents or fellows (72% pre-intervention, 74% post-intervention). After template changes that utilized help text, the percent of notes utilizing any laboratory SmartLink decreased from 90.2 to 15.3% for admission notes ( p <0.001); 92.6 to 17.8% for progress notes ( p <0.001); and 14 to 7.2% for discharge summaries ( p <0.001) ( Fig. 3 ). The median progress note length decreased by 1,251 characters per note (18.7% reduction, p <0.001), and the median admission note length decreased by 720 characters per note (6.4% reduction, p <0.001). The median length of discharge summaries did not significantly change ( Fig. 4 ). After help text implementation, the average number of all coding queries sent to PHM attendings decreased from 41.5 to 36.4 queries per month, and the average number of problem list coding queries sent decreased from 3.5 to 0.4 queries per month ( Table 2 ). Pass rates on internal billing compliance audits for PHM attendings were high at baseline and did not change after help text implementation.
Table 1. Note author characteristics. Characteristics of distinct first authors for notes evaluated in the pre- and post-help text implementation period. The first author is the author who first signed the note and, after help text implementation, the author who viewed the disappearing help text.
| Pre-help text n (%) |
Post-help text n (%) |
|
|---|---|---|
| Provider type | ||
| Resident | 185 (82%) | 180 (81%) |
| Fellow | 8 (4%) | 9 (4%) |
| Nurse practitioner | 9 (4%) | 9 (4%) |
| Attending | 23 (10%) | 24 (11%) |
| Sex | ||
| Female | 155 (69%) | 149 (67%) |
| Male | 70 (31%) | 73 (33%) |
| Specialty | ||
| Pediatrics | 133 (59%) | 135 (61%) |
| Family medicine | 66 (29%) | 61 (27%) |
| Pediatric hospital medicine | 26 (12%) | 26 (12%) |
Fig. 4.
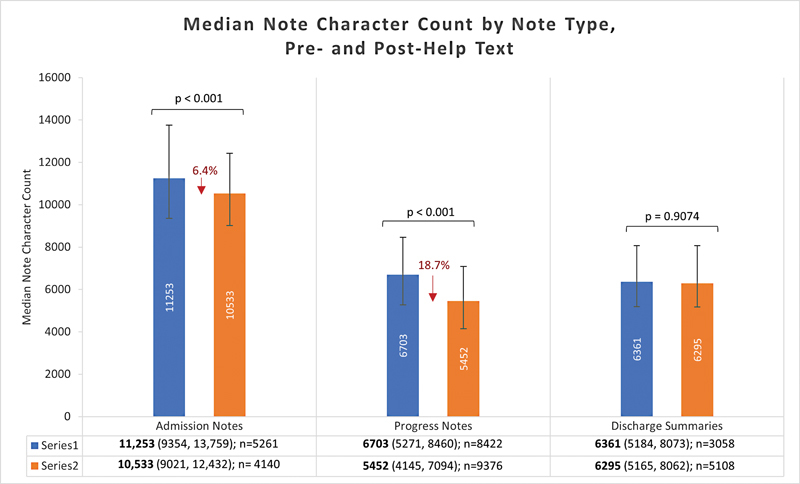
Median note character count by note type, pre- and post-help text implementation. For pediatric hospital medicine admission notes (pre: July 2018–June 2019, post: July 2019–Feb 2020), progress notes (pre: Sept 2017–Aug 2018, post: Sept 2018–Aug 2019), and discharge summaries (pre: May 2017–Apr 2018, post: May 2018–Apr 2019).
Table 2. Average coding queries per month. By phase of help text implementation and by coding query type (all types of coding queries and problem list-specific coding queries).
| Pre-help text (July 2017–April 2018) |
Help text added to discharge summary (May 2018–Aug 2018 |
Help text added to discharge summary and progress note (Sept 2018–July 2019) |
Post-help text, all note templates (July 2019–Feb 2020) |
|
|---|---|---|---|---|
| All coding queries | 41.5 | 45.5 | 36.4 | 35.9 |
| Problem list coding queries | 3.5 | 3.3 | 2.5 | 0.4 |
Discussion
Note template changes that utilized disappearing help text significantly reduced the length of progress and admission notes, a proxy for note bloat reduction. One factor that likely contributed to note length reduction is the reduced usage of laboratory SmartLinks, prompted by help text which encouraged authors to only note significant laboratories rather than using laboratory SmartLinks to automatically import all recent laboratories. After help text implementation, SmartLink usage was reduced in all three note types. The decrease in note length did not negatively impact internal billing compliance audit performance or coding query frequency for PHM attendings, suggesting that the shorter notes did not degrade note quality.
Notably, we did not see a reduction in character count in discharge summaries even as the usage of laboratory SmartLinks was reduced by half. This is likely due to a concomitant change in our Discharge Summary template that added a “Suggested Next Steps for Primary Care Provider” section, 14 which highlighted significant follow-up needs and would be considered relevant note information rather than note bloat.
There are several limitations in our analyses. We did not directly evaluate note quality, and we did not control for the potential impact of concomitant interventions such as trainee education. Additionally, the notes we evaluated were predominantly trainee-written notes and limited only to the PHM service, and may not be generalizable to notes written by attending physicians or notes written by other specialties. Finally, we did not evaluate the potential contribution of help text to cognitive load.
Within the framework of the five “rights,” quality CDS should be delivered with the right information to the right person, in the right interventional format, through the right channel, at the right time in the workflow. 15 Opportunities to provide note-based CDSin EHRs have previously remained limited, and our disappearing help text tool presents a method for non-interruptive CDS to be delivered in real time to a provider within the note workflow itself. As with other forms of CDS, help text should be concise, pertinent, and thoughtfully curated to minimize contribution to cognitive load and alert fatigue. Directions on replicating our build have been shared via presentation at the EHR vendor's annual user meeting, archived tip sheet and presentation on the EHR vendor's user website, and personal correspondence with the author. Further integration of this tool into EHR platforms may expand accessibility and utilization of this note-based decision support tool.
Conclusion
We present the novel use of in-line disappearing help text embedded into existing note templates to improve note readability and accuracy, educate trainees on note documentation, enhance provider workflow, support billing compliance, and protect confidential teen information from being inadvertently shared. Our data demonstrate that help text drove a reduction in the automatic insertion of laboratories into notes which correlated with a decrease in character count and did not negatively impact billing compliance or coding queries. Guidance directing clinicians to document confidential teen information in the shared history section which cannot be pulled into notes may promote note sharing with both teens and their caregivers while maintaining teen confidentiality. Further study is warranted into the impact of help text on protecting teen confidentiality, note quality, documentation accuracy and completeness, trainee education and compliance with billing regulations. Further study should also explore the value of help text for providers at differing levels of training and experience, generalizability to other specialties and contexts, and potential contribution to cognitive load and alert fatigue.
Clinical Relevance Statement
Disappearing help text is a non-interruptive in-line tool that can provide CDS within note templates for clinicians at the point of care. This tool can be used to improve note readability, decrease note bloat, educate trainees on note documentation, protect confidential teen information from being inadvertently shared, and enhance provider workflows.
Multiple Choice Questions
-
Disappearing help text can be used to address all of the following factors that may contribute to “note bloat” EXCEPT:
Ease of copy-forward functionality.
Automatic import of data into notes.
The use of the note rather than native sections for information review.
-
Misinterpretation of billing compliance as requiring that all information be included in the note itself.
Correct Answer: The answer is option a. Disappearing help text encouraged summarizing significant laboratory and radiology results rather than auto-populating entire lists of results into the note, directed providers to review information in native sections via embedded activity hyperlinks rather than in the note, and included guidance on billing and compliance requirements in the note. Help text did not directly address the ease of copy-forward functionality.
-
All of the following describe functionality of disappearing help text EXCEPT:
Displaying targeted ruled-based clinical decision support in a note based on patient characteristics.
Promoting entry and review of patient and encounter level data outside the note via activity hyperlinks.
Defaulting an APSO note format instead of a SOAP format.
Providing in-line guidance on note best practices.
Correct Answer: The answer is option c. Disappearing help text can interface with patient rules to display targeted clinical decision support in a note based on patient characteristics. Activity hyperlinks in help text can enhance provider workflow and promote entry and review of patient and encounter level data outside the note. Help text can provide in-line guidance on note best practices. While disappearing help text could recommend a particular note format such as APSO, it does not cause this format to be defaulted in the note.
Acknowledgments
The following people contributed to content development of disappearing help text in PHM note templates: Elizabeth Mannino Avila, MD, Melissa Cameron, MD, Annie Larrow, MD, and Treavor Robison, MD.
Conflict of Interest None declared.
Protection of Human and Animal Subjects
There were no human subjects involved in the project.
References
- 1.Frintner M P, Kaelber D C, Kirkendall E S, Lourie E M, Somberg C A, Lehmann C U. The effect of electronic health record burden on pediatricians' work-life balance and career satisfaction. Appl Clin Inform. 2021;12(03):697–707. doi: 10.1055/s-0041-1732402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sinsky C, Colligan L, Li L. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753–760. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 3.Overhage J M, McCallie D., Jr Physician time spent using the electronic health record during outpatient encounters: a descriptive study. Ann Intern Med. 2020;172(03):169–174. doi: 10.7326/M18-3684. [DOI] [PubMed] [Google Scholar]
- 4.Arndt B G, Beasley J W, Watkinson M D. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(05):419–426. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kroth P J, Morioka-Douglas N, Veres S. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Netw Open. 2019;2(08):e199609. doi: 10.1001/jamanetworkopen.2019.9609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang M D, Khanna R, Najafi N. Characterizing the source of text in electronic health record progress notes. JAMA Intern Med. 2017;177(08):1212–1213. doi: 10.1001/jamainternmed.2017.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsou A Y, Lehmann C U, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR. systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017;8(01):12–34. doi: 10.4338/ACI-2016-09-R-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Donnell H C, Kaushal R, Barrón Y, Callahan M A, Adelman R D, Siegler E L. Physicians' attitudes towards copy and pasting in electronic note writing. J Gen Intern Med. 2009;24(01):63–68. doi: 10.1007/s11606-008-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downing N L, Bates D W, Longhurst C A. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med. 2018;169(01):50–51. doi: 10.7326/M18-0139. [DOI] [PubMed] [Google Scholar]
- 10.Shoolin J, Ozeran L, Hamann C, Bria W., II Association of medical directors of information systems consensus on inpatient electronic health record documentation. Appl Clin Inform. 2013;4(02):293–303. doi: 10.4338/ACI-2013-02-R-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siegler E L, Adelman R. Copy and paste: a remediable hazard of electronic health records. Am J Med. 2009;122(06):495–496. doi: 10.1016/j.amjmed.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Lin C T, McKenzie M, Pell J, Caplan L. Health care provider satisfaction with a new electronic progress note format: SOAP vs APSO format. JAMA Intern Med. 2013;173(02):160–162. doi: 10.1001/2013.jamainternmed.474. [DOI] [PubMed] [Google Scholar]
- 13.Belden J L, Koopman R J, Patil S J, Lowrance N J, Petroski G F, Smith J B. Dynamic electronic health record note prototype: seeing more by showing less. J Am Board Fam Med. 2017;30(06):691–700. doi: 10.3122/jabfm.2017.06.170028. [DOI] [PubMed] [Google Scholar]
- 14.Larrow A, Chong A, Robison T. A quality improvement initiative to improve discharge timeliness and documentation. Pediatr Qual Saf. 2021;6(04):e440. doi: 10.1097/pq9.0000000000000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jerome A, Osheroff J MT, Levick D. Healthcare Information Management Systems Society; 2012. Improving Outcomes with Clinical Decision Support: An Implementer's Guide. 2nd ed. [Google Scholar]


